Contents
- Hypocalcemia
- What is calcium?
- Hypocalcemia causes
- Calcium deficiency prevention
- Hypocalcemia signs and symptoms
- Hypocalcemia diagnosis
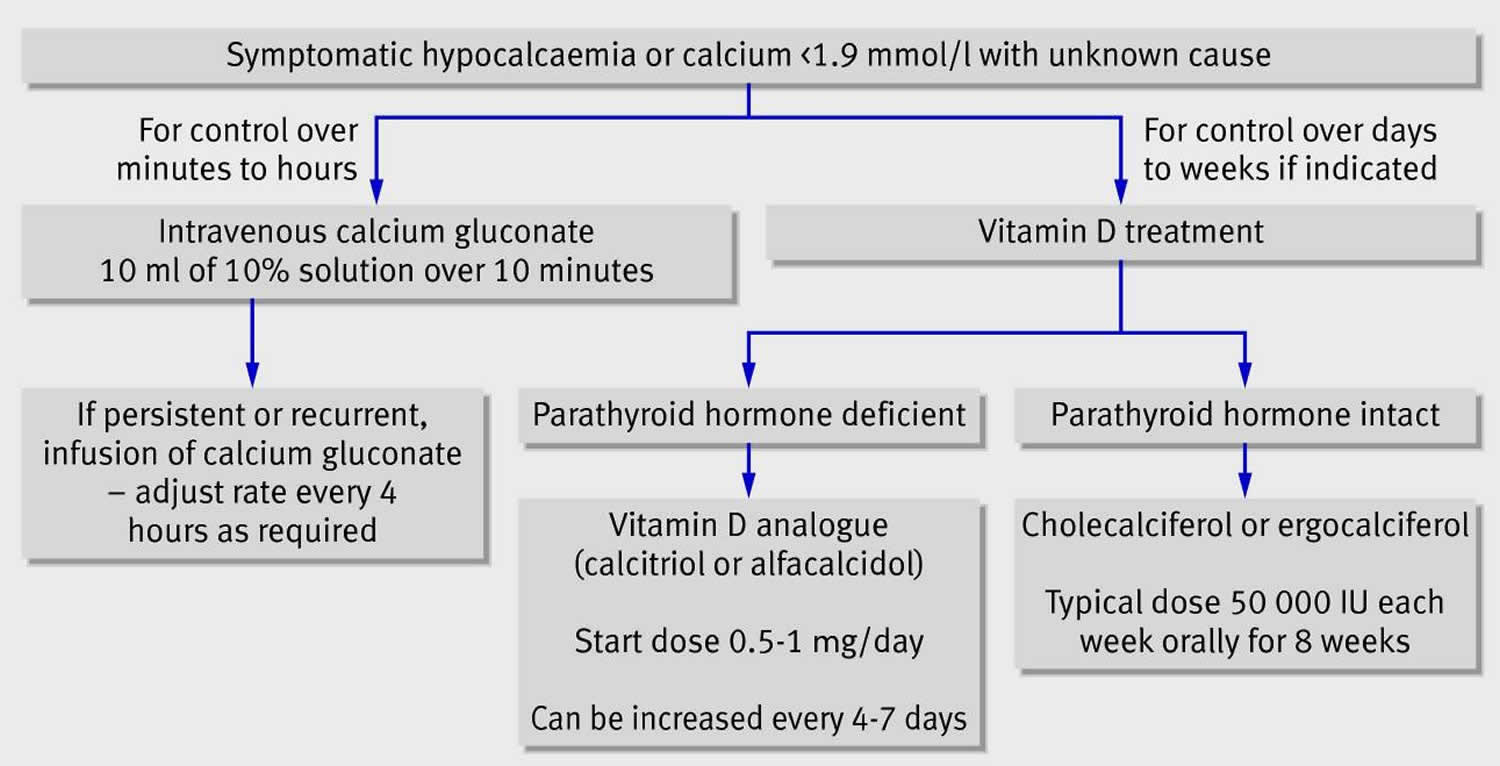
- Hypocalcemia treatment
- Hypocalcemia prognosis
Hypocalcemia
Hypocalcemia is a condition where blood levels of calcium are low. Hypocalcemia is a total serum calcium concentration < 8.5 mg/dL (< 2.13 mmol/L) in the presence of normal plasma protein concentrations or a serum ionized calcium concentration < 4.7 mg/dL (< 1.17 mmol/L) 1. Normal calcium values range from 8.5 to 10.2 mg/dL (2.13 to 2.55 millimol/L). Hypocalcemia can present as an asymptomatic laboratory finding or as a severe, life-threatening condition 2. Symptoms of hypocalcemia include numbness and tingling in the fingers, muscle cramps, convulsions, lethargy, poor appetite, and abnormal heart rhythms 3. Hypocalcemia is frequently encountered in patients who are hospitalized. Depending on the cause, unrecognized or poorly treated hypocalcemic emergencies can lead to significant morbidity or death 4.
Common causes of hypocalcemia include the following 5, 6, 7, 8, 9:
- Vitamin D inadequacy or vitamin D resistance
- Hypoparathyroidism following surgery
- Hypoparathyroidism owing to autoimmune disease or genetic causes
- Renal disease or end-stage liver disease causing vitamin D inadequacy
- Pseudohypoparathyroidism or pseudopseudohypoparathyroidism
- Metastatic or heavy metal (copper, iron) infiltration of the parathyroid gland
- Hypomagnesemia or hypermagnesemia
- Sclerotic metastases
- Hungry bone syndrome postparathyroidectomy
- Infusion of phosphate or citrated blood transfusions
- Critical illness
- Drugs (eg, high-dose intravenous bisphosphonates)
- Fanconi syndrome
- Past radiation of parathyroid glands
Hypocalcemia may be transient, reversing with addressing the underlying cause expeditiously, or chronic and even lifelong, when due to a genetic disorder or the result of irreversible damage to the parathyroid glands after surgery or secondary to autoimmune destruction 10. Prolonged hypocalcemia can result in poor bone formation, which may result in brittle bones that are prone to fractures. Calcium, the most abundant mineral in the body, is found in some foods, added to others, available as a dietary supplement, and present in some medicines (such as antacids). Calcium is required for vascular contraction and vasodilation, muscle function, nerve transmission, intracellular signaling and hormonal secretion, though less than 1% of total body calcium is needed to support these critical metabolic functions 11. Serum calcium is very tightly regulated and does not fluctuate with changes in dietary intakes; the body uses bone tissue as a reservoir for, and source of calcium, to maintain constant concentrations of calcium in blood, muscle, and intercellular fluids 11. Calcium homeostasis in the body is a complex interplay between several different hormones or hormone-like substances, such as parathyroid hormone (PTH), Vitamin D, and calcitonin 4.
About 99% of calcium of your body’s calcium supply is stored in your bones and teeth where it supports their structure and function, while the remaining 1% circulates in the blood 11. Bone itself undergoes continuous remodeling, with constant resorption and deposition of calcium into new bone. The balance between bone resorption and deposition changes with age. Bone formation exceeds resorption in periods of growth in children and adolescents, whereas in early and middle adulthood both processes are relatively equal. In aging adults, particularly among postmenopausal women, bone breakdown exceeds formation, resulting in bone loss that increases the risk of osteoporosis over time 11.
A 70-kg person has approximately 1.2 kg of calcium in the body, more than 99% of which is stored as hydroxyapatite in bones 12. Less than 1% (5-6 g) of calcium is located in the intracellular (inside the cell) and extracellular (oustide the cell) compartments, with only 1.3 g located extracellularly 13. The total calcium concentration in the plasma is 4.5-5.1 mEq/L (9-10.2 mg/dL). Fifty percent of plasma calcium is ionized, 40% is bound to proteins (90% of which binds to albumin), and 10% circulates bound to anions (eg, phosphate, carbonate, citrate, lactate, sulfate). Ionized calcium is the necessary plasma fraction for normal physiologic processes. In the neuromuscular system, ionized calcium facilitates nerve conduction, muscle contraction, and muscle relaxation. Calcium is necessary for bone mineralization and is an important cofactor for hormonal secretion in endocrine organs. At the cellular level, calcium is an important regulator of ion transport and membrane integrity.
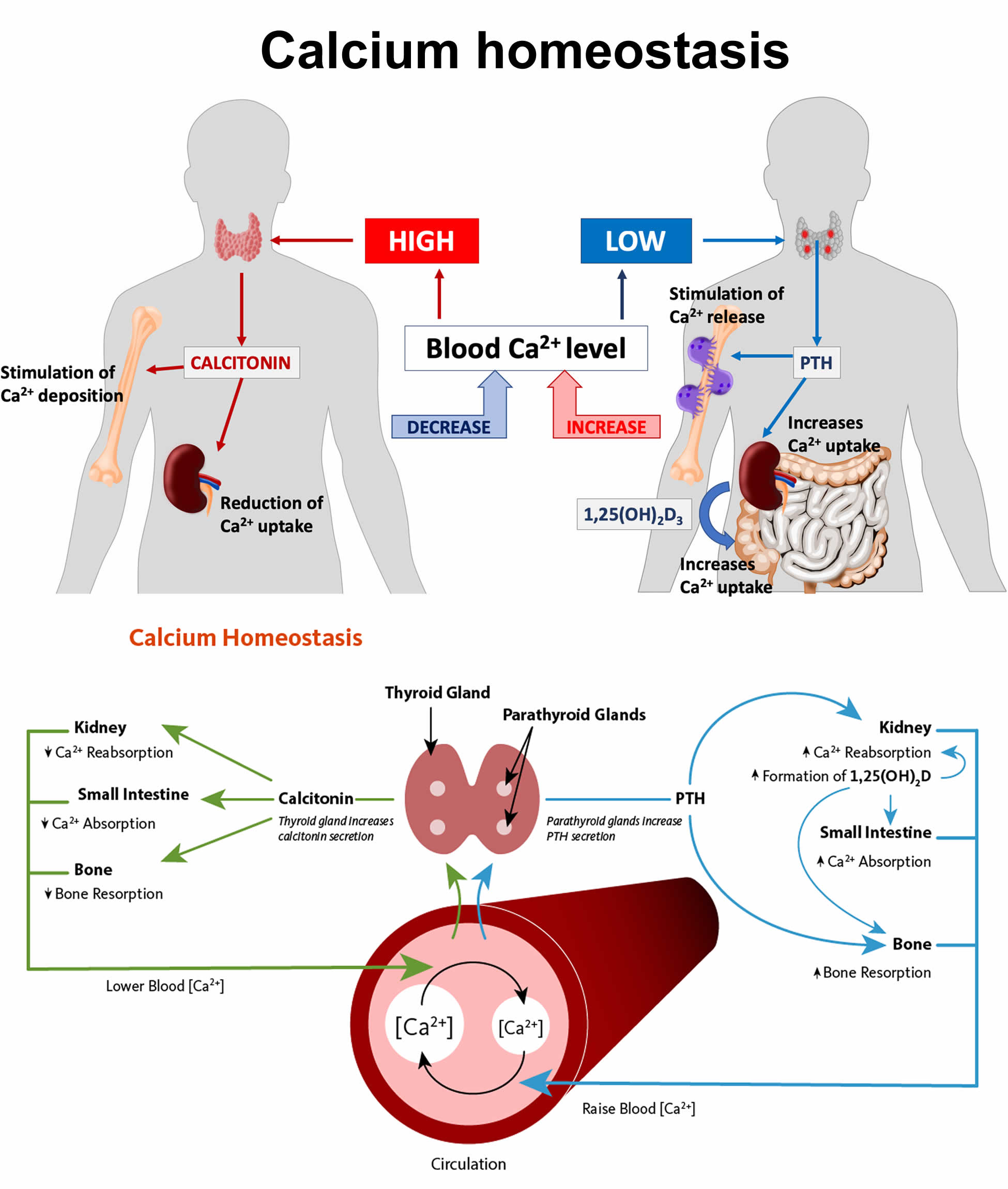
Approximately 500 mg of calcium is removed from the bones daily and replaced by an equal amount 13. Normally, the amount of calcium absorbed by the intestines is matched by urinary calcium excretion. Despite these enormous fluxes of calcium, the levels of ionized calcium remain stable because of the rigid control maintained by parathyroid hormone (PTH), vitamin D, and calcitonin through complex feedback loops (see Figure 1). These compounds act primarily at bone, renal, and gastrointestinal sites. Calcium levels are also affected by magnesium and phosphorus 14.
At a plasma pH of 7.4, each gram of albumin binds 0.8 mg/dL of calcium. This bond is dependent on the carboxyl groups of albumin and is highly dependent on pH. Acute acidemia decreases calcium binding to albumin, whereas alkalemia increases binding, which decreases ionized calcium. Clinical signs and symptoms are observed only with decreases in ionized calcium concentration (normally 4.5-5.5 mg/dL) 15.
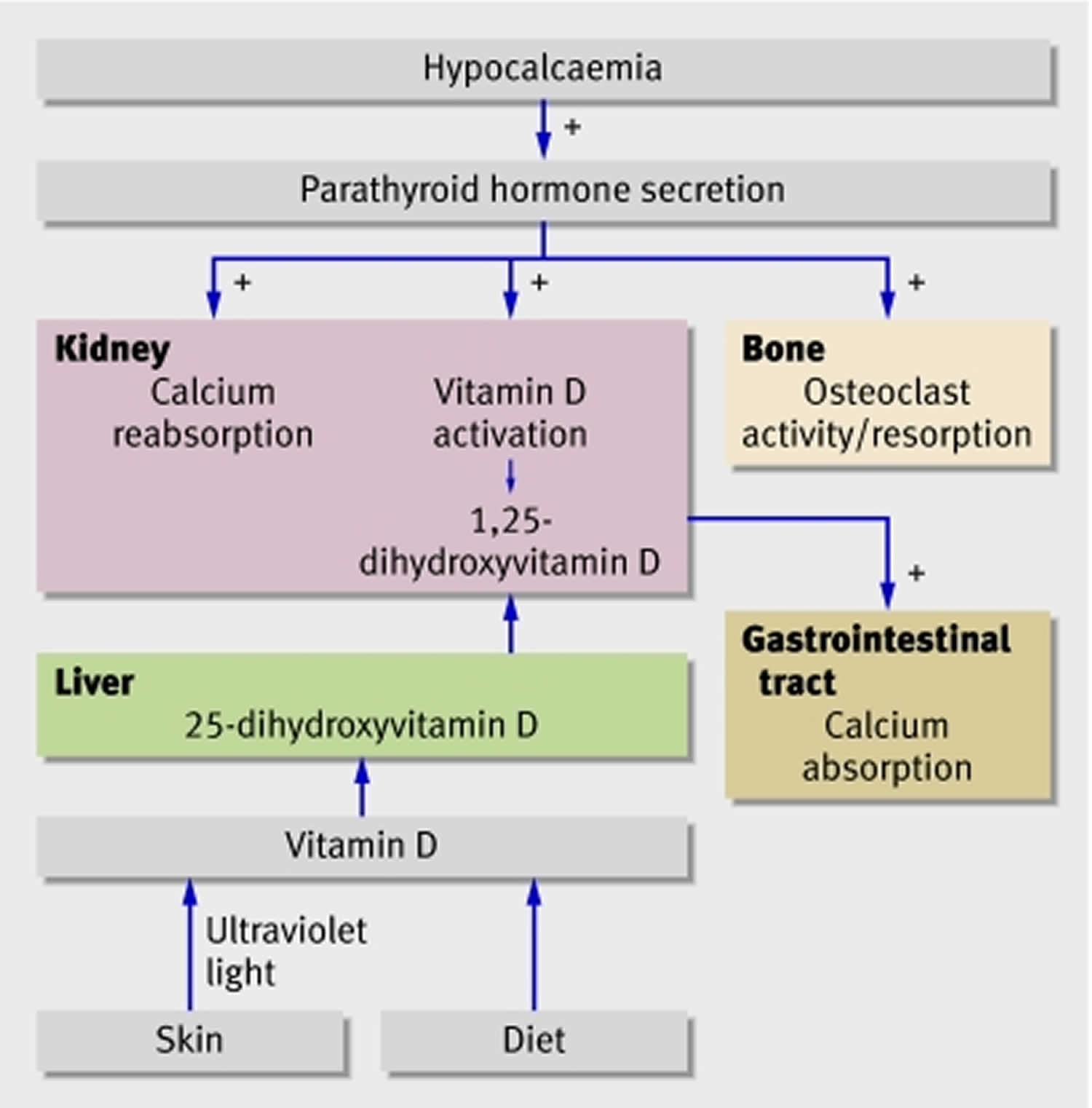
Serum calcium levels are regulated within a narrow range (2.1 to 2.6 mmol/L) by 3 main calcium-regulating hormones—parathyroid hormone (PTH), vitamin D, and to a lesser extent, calcitonin (Figure 1)—through their specific effects on the bowel, kidneys, and skeleton 5. Approximately half of the total serum calcium is bound to protein, and the remaining free ionized calcium is physiologically active 5. When your blood calcium levels are low, your parathyroid glands secrete parathyroid hormone (PTH) (Figure 1). The parathyroid hormone (PTH) helps your bones release calcium into the blood. Parathyroid hormone (PTH) also increases serum calcium by stimulating conversion of vitamin D to its most active form, calcitriol also known as 1,25-dihydroxycholecalciferol or 1,25-dihydroxyvitamin D. Calcitriol also known as 1,25-dihydroxycholecalciferol (1,25-dihydroxyvitamin D), which is actually a hormone, helps your body absorb calcium by increasing the percentage of dietary calcium absorbed by your intestines. Despite increased calcium absorption, long-term increases in parathyroid hormone (PTH) secretion generally result in further bone resorption by inhibiting osteoblastic function and promoting osteoclastic activity. PTH and vitamin D both function as important regulators of bone growth and bone remodeling. Together, parathyroid hormone (PTH) and vitamin D, along with other hormones and minerals, help move calcium in or out of body tissues to keep your blood calcium at a normal level. Serum calcium levels must be corrected for the albumin level before confirming the diagnosis of hypercalcemia or hypocalcemia 16.
Parathyroid hormone (PTH) has several actions, but the most important is to defend against low blood calcium or hypocalcemia. Parathyroid cells sense decreases in serum calcium and, in response, release preformed PTH into your bloodstream. Parathyroid hormone (PTH) increases serum calcium within minutes by increasing kidney and intestinal absorption of calcium and by rapidly mobilizing calcium and phosphate from bone (bone resorption) (Figure 1). Kidney calcium excretion generally parallels sodium excretion and is influenced by many of the same factors that govern sodium transport in the proximal tubule. However, PTH enhances distal tubular calcium reabsorption independently of sodium.
Parathyroid hormone (PTH) raises blood calcium levels by 17:
- Effects of parathyroid hormone (PTH) on your bones, where most of your body’s calcium is stored, to release calcium into the blood.
- In your bones, parathyroid hormone (PTH) stimulates the release of calcium in an indirect process through osteoclasts which ultimately leads to the resorption of your bones. However, before osteoclast activity, PTH directly stimulates osteoblasts which increases their expression of RANKL, a receptor activator for nuclear factor kappa-B ligand, allowing for the differentiation of osteoblasts into osteocytes. PTH also inhibits the secretion of osteoprotegerin, allowing for preferential differentiation into osteoclasts. Osteoprotegerin normally competitively binds with RANKL diminishing the ability to form osteoclasts. Osteoclasts possess the ability to remodel the bones (resorption) by dissolution and degradation of hydroxyapatite and other organic material, releasing calcium into the blood.
- Effects of parathyroid hormone (PTH) on your kidneys helping your kidneys hold on to calcium and return it to your blood instead of flushing it out in urine.
- In your kidneys, the parathyroid hormone (PTH) has 3 functions in increasing serum calcium levels. Most of the physiologic calcium reabsorption in the nephron takes place in the proximal convoluted tubule and additionally at the ascending loop of Henle. Circulating parathyroid hormone (PTH) targets the distal convoluted tubule and collecting duct, directly increasing calcium reabsorption. Parathyroid hormone (PTH) decreases phosphate reabsorption at the proximal convoluted tubule. Phosphate ions in the serum form salts with calcium that are insoluble, resulting in decreased plasma calcium. The reduction of phosphate ions, therefore, results in more ionized calcium in the blood.
- Also in your kidneys, parathyroid hormone (PTH) stimulates the production of 1-alpha-hydroxylase in the proximal convoluted tubule. This enzyme, 1-alpha-hydroxylase, is required to catalyze the synthesis of active vitamin D called “calcitriol” or 1,25 dihydroxyvitamin D (1,25-dihydroxycholecalciferol) from the inactive form 25-hydroxycholecalciferol 18. The main effect of calcitriol or 1,25 dihydroxyvitamin D (1,25-dihydroxycholecalciferol) is to increase calcium absorption from your gut 19. Calcitriol or 1,25 dihydroxyvitamin D (1,25-dihydroxycholecalciferol) binds to the vitamin D receptor in the epithelial cells of the duodenum causing the synthesis of calcium binding proteins that regulate active intestinal calcium absorption 19, 20. In the small intestine, vitamin D allows the absorption of calcium through an active transcellular pathway and a passive paracellular pathway. The transcellular pathway requires energy, while the paracellular pathway allows for the passage of calcium through tight junctions. Calcitriol or 1,25 dihydroxyvitamin D (1,25-dihydroxycholecalciferol) also stimulates calcium reabsorption in your kidneys.
- PTH indirect effects on your small intestines by helping your intestines absorb calcium from food
Insufficient intakes of calcium do not produce obvious symptoms in the short term because the body maintains calcium levels in the blood by taking it from bone. Over the long term, intakes of calcium below recommended levels have health consequences, such as causing low bone mass (osteopenia) and increasing the risks of osteoporosis and bone fractures. Chronically low calcium intakes in growing individuals may prevent the attainment of optimal peak bone mass. Once peak bone mass is achieved, inadequate calcium intake may contribute to accelerated bone loss and ultimately to the development of osteoporosis 21.
Getting too little calcium can cause several conditions, including the following:
- Osteopenia is a condition that begins as you lose bone mass and your bones get weaker. Osteopenia happens when the inside of your bones become brittle from a loss of calcium. Osteopenia is very common as you age. Total bone mass peaks around age 35. Sometimes, osteopenia is a precursor to osteoporosis. People who have osteopenia are at a higher risk of having osteoporosis.
- Osteoporosis, a condition in which bones become weak and brittle, increasing the chance they may break and increases the risk of falling.
- Rickets, a condition in children in which bones become soft and deformed because they don’t have enough calcium and phosphorus. It is caused by not having enough vitamin D in the diet or by not getting enough sunlight. In adults, this condition is called osteomalacia.
- Osteomalacia, a condition in adults in which bones become soft and deformed because they don’t have enough calcium and phosphorus. It is usually caused by not having enough vitamin D in the diet, not getting enough sunlight, or a problem with the way the body uses vitamin D. Symptoms include bone pain and muscle weakness. When the condition occurs in children, it is called rickets.
- Patients with severe low blood calcium or hypocalcemia of less than 7 mg/dL and those with an acute drop in calcium level can develop seizures or life-threatening arrhythmia 22.
Over the long term, inadequate calcium intake causes osteopenia which if untreated can lead to osteoporosis, which is characterized by fragile bones and an increased risk of falling 21. The risk of bone fractures also increases, especially in older individuals. Calcium deficiency can also cause rickets, though it is more commonly associated with vitamin D deficiency 23, 24, 25, 26. In children with rickets, the growth cartilage does not mineralize normally, which can lead to irreversible changes in the skeletal structure (Figure 3) 21. Another effect of chronic calcium deficiency is osteomalacia, or defective bone mineralization and bone softening, which can occur in adults and children 21. For rickets and osteomalacia, the requirements for calcium and vitamin D appear to be interrelated in that the lower the serum vitamin D level (measured as 25-hydroxyvitamin D [25(OH)D]), the more calcium is needed to prevent these diseases 27.
Calcium is absorbed passively (no cellular energy required) in the intestines by diffusing through the spaces between cells. It is also absorbed actively (cellular energy required) through intestinal cells by binding to a transport protein known as calbindin. The production of calbindin is dependent on vitamin D 28. Not all calcium consumed is actually absorbed in the gut. Humans absorb about 30% of the calcium in foods, but this varies depending upon the type of food consumed 11. Other factors also affect calcium absorption including the following:
- Amount consumed: the efficiency of absorption decreases as calcium intake increases 11.
- Age and life stage: net calcium absorption is as high as 60% in infants and young children, who need substantial amounts of the mineral to build bone 29. Absorption decreases to 15%–20% in adulthood (though it is increased during pregnancy) and continues to decrease as people age; compared with younger adults, recommended calcium intakes are higher for females older than 50 years and for both males and females older than 70 years 29.
- Vitamin D intake: this nutrient, obtained from food and produced by skin when exposed to sunlight of sufficient intensity, improves calcium absorption 11.
- Other components in food: phytic acid and oxalic acid, found naturally in some plants, bind to calcium and can inhibit its absorption. Foods with high levels of oxalic acid include spinach, collard greens, sweet potatoes, rhubarb, and beans. Among the foods high in phytic acid are fiber-containing whole-grain products and wheat bran, beans, seeds, nuts, and soy isolates 11. The extent to which these compounds affect calcium absorption varies. Research shows, for example, that eating spinach and milk at the same time reduces absorption of the calcium in milk. In contrast, wheat products (with the exception of wheat bran) do not appear to lower calcium absorption 30. For people who eat a variety of foods, these interactions probably have little or no nutritional consequence and, furthermore, are accounted for in the overall calcium Dietary Reference Intakes (DRIs), which factor in differences in absorption of calcium in mixed diets.
Some absorbed calcium is eliminated from the body in urine, feces, and sweat. This amount is affected by such factors as the following:
- Sodium and protein intakes: high sodium intake increases urinary calcium excretion 31. High protein intake also increases calcium excretion and was therefore thought to negatively affect calcium status 31. However, more recent research suggests that high protein intake also increases intestinal calcium absorption, effectively offsetting its effect on calcium excretion, so whole body calcium retention remains unchanged 32.
- Caffeine intake: this stimulant in coffee and tea can modestly increase calcium excretion and reduce absorption 33. One cup of regular brewed coffee, for example, causes a loss of only 2–3 mg of calcium. Moderate caffeine consumption (1 cup of coffee or 2 cups of tea per day) in young women has no negative effects on bone 34.
- Alcohol intake: alcohol intake can affect calcium status by reducing its absorption 35 and by inhibiting enzymes in the liver that help convert vitamin D to its active form 36. However, the amount of alcohol required to affect calcium status and whether moderate alcohol consumption is helpful or harmful to bone is unknown.
- Phosphorus intake: the effect of this mineral on calcium excretion is minimal. Several observational studies suggest that consumption of carbonated soft drinks with high levels of phosphate is associated with reduced bone mass and increased fracture risk. However, the effect is probably due to replacing milk with soda rather than the phosphorus itself 37.
- Fruit and vegetable intakes: metabolic acids produced by diets high in protein and cereal grains increase calcium excretion 38. Fruits and vegetables, when metabolized, shift the acid/base balance of the body towards the alkaline by producing bicarbonate, which reduces calcium excretion. However, it is unclear if consuming more fruits and vegetables affects bone mineral density. These foods, in addition to reducing calcium excretion, could possibly reduce calcium absorption from the gut and therefore have no net effect on calcium balance.
Certain groups of people are more likely than others to have trouble getting enough calcium 39:
- Postmenopausal women. The body absorbs and retains less calcium after menopause. Over time, this can lead to fragile bones.
- People who don’t drink milk or eat other dairy products. Dairy products are rich sources of calcium, but people with lactose intolerance, people with milk allergies, and vegans (people who don’t consume any animal products) must find other sources of calcium. Options include lactose-free or reduced-lactose dairy products; canned fish with bones; certain vegetables, such as kale, broccoli, and Chinese cabbage; calcium-fortified fruit juices and milk substitutes such as soy and almond beverages, tofu, and ready-to-eat cereals; and dietary supplements that contain calcium.
- People who have lactose intolerance and avoid dairy products
- Women who have an eating disorder (for example, anorexia)
- People who do not eat animal, fish, or dairy products (vegans)
- People who take certain medicines for osteoporosis
- People who have parathyroid disorders, inflammatory bowel disease, or liver or kidney disease
A substantial proportion of people in the United States consume less than recommended amounts of calcium. An analysis of 2007–2010 data from the National Health and Nutrition Examination Survey (NHANES) found that 49% of children aged 4–18 years and 39% of all individuals aged 4 and older consume less than the Estimated Average Requirement (average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals) for calcium from foods and supplements 40.
Average daily intakes of calcium from foods and beverages are 1,083 mg for men aged 20 and older and 842 mg for women 41. For children aged 2–19, mean daily intakes of calcium from foods and beverages range from 965 to 1,015 mg 41. Approximately 22% of men, 32% of women, and 4 to 8% of children take a dietary supplement containing calcium 41. Average daily calcium intakes from both foods and supplements are 1,156 mg for men, 1,009 mg for women, and 968 to 1,020 mg for children 41.
According to 2009–2012 National Health and Nutrition Examination Survey data, rates of calcium inadequacy (intakes below the Estimated Average Requirement) are higher among non-Hispanic Blacks and non-Hispanic Asians (47–48%) than among Hispanics (30%) and non-Hispanic Whites (24%) in the United States 42. Poverty is also associated with a higher risk of inadequacy. National Health and Nutrition Examination Survey data from 2007 to 2014 show that the risk of inadequate calcium intakes (less than 800 to 1,100 mg) is 11.6% higher among adults aged 50 and older in households earning less than $20,000 per year than other households 43.
Unfortunately, getting more calcium than your body needs can cause adverse (negative) effects. This includes kidney stones, frequent urination, belly pain, nausea/vomiting, and fatigue. It is rare to get too much calcium from food alone. There is an amount of calcium that most people can take each day without developing problems. This is called the tolerable upper intake level (UL). Doctors recommend the following tolerable upper intake levels by age:
- Ages 0-6 months: 1,000 mg per day
- Ages 7-12 months: 1,500 mg per day
- Ages 1-8: 2,500 mg per day
- Ages 9-18: 3,000 mg per day
- Ages 19-50: 2,500 mg per day
- Ages 51 and older: 2,000 mg per day
- Pregnant and breastfeeding teens: 3,000 mg per day
- Pregnant and breastfeeding adults: 2,500 mg per day
In addition, research shows that high intakes of calcium may provide health benefits in lowering the risk of colon cancer, preeclampsia (pregnancy related complication in which affected women develop high blood pressure [hypertension]; they can also have abnormally high levels of protein in their urine [proteinuria]), and metabolic syndrome such as diabetes. Other research shows that high calcium intake may raise the risk of prostate cancer. Conflicting research suggests that a high intake of calcium may or may not provide a protection against heart disease 44, 45.
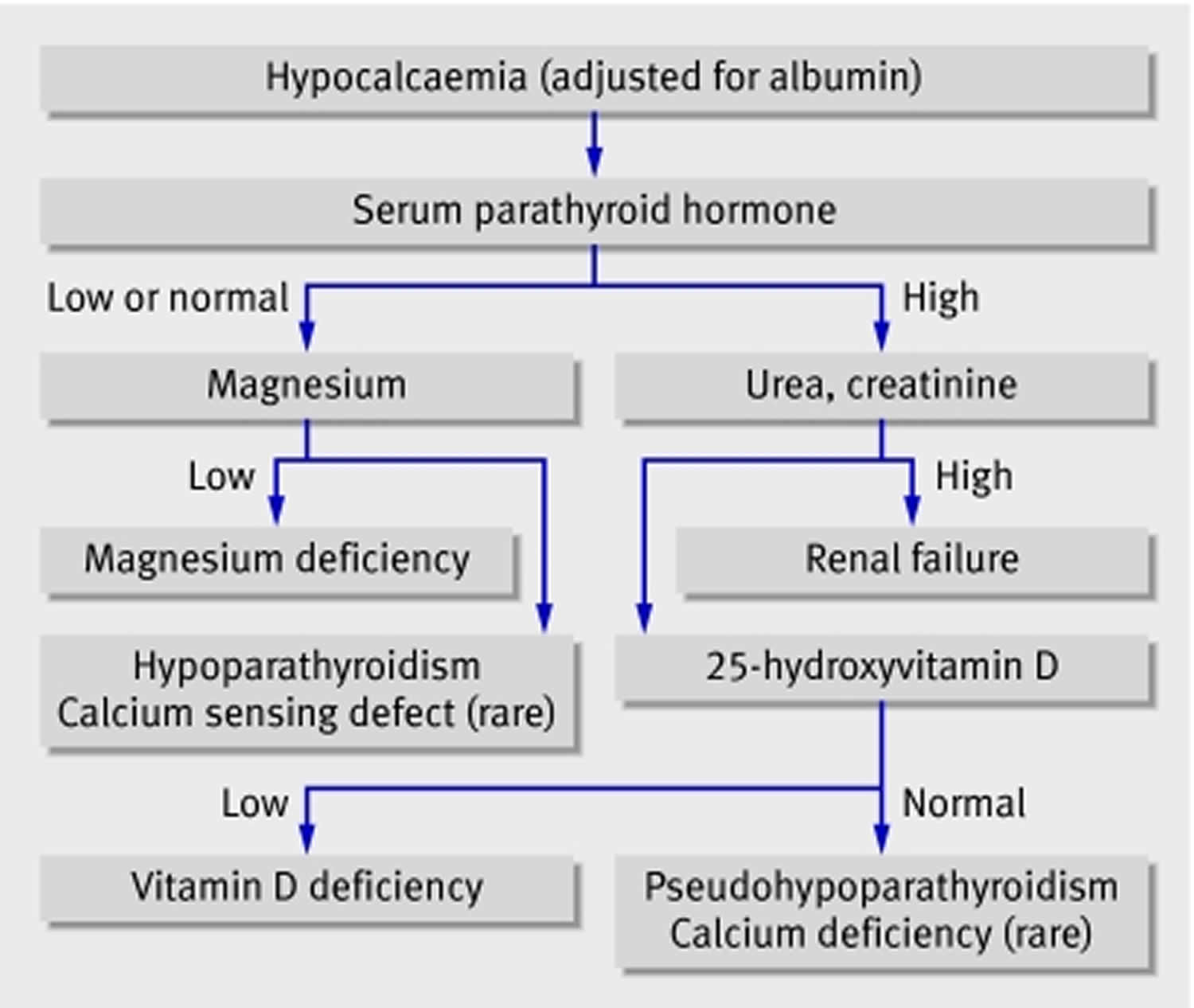
Hypocalcemia basic investigations include 5, 6, 7, 8:
- Serum calcium (corrected for albumin)
- Phosphate
- Magnesium
- Electrolytes
- Creatinine
- Alkaline phosphatase
- Parathyroid hormone
- 25-hydroxyvitamin D
- Serum pH
- Complete blood count
Hypocalcemia further investigations include 5, 6, 7, 8:
- Ionized calcium
- 24-hour urinary phosphate, calcium, magnesium, and creatinine
- 1,25-dihydroxyvitamin D
- Renal ultrasonography to assess for nephrolithiasis
- DNA sequencing to exclude genetic mutations
- Biochemistry in first-degree family members
Hypocalcemia (corrected serum total calcium level < 2.12 mmol/L) is most commonly a consequence of vitamin D inadequacy or hypoparathyroidism, or a resistance to these hormones 46. Hypocalcemia has also been associated with many drugs, including bisphosphonates, cisplatin, antiepileptics, aminoglycosides, diuretics, and proton pump inhibitors (level III evidence); as well, there are other causes 46.
The treatment of hypocalcemia depends on the cause, the severity, the presence of symptoms, and how rapidly the hypocalcemia developed. Most cases of hypocalcemia are clinically mild and require only supportive treatment and further laboratory evaluation 12. Oral calcium repletion may be indicated for outpatient treatment of mild cases. On occasion, severe hypocalcemia may result in seizures, tetany, refractory hypotension, or arrhythmias that require a more aggressive approach, including intravenous infusions of calcium.
Figure 1. Calcium homeostasis (regulation of serum calcium)
Figure 2. Calcium deficiency
Footnote: Parathyroid hormone (PTH) and vitamin D normally interact to protect against low calcium in blood (hypocalcemia). Problems at any level can lead to low serum calcium, but the most common problems are vitamin D deficiency and hypoparathyroidism
[Source 6 ]Figure 3. Calcium deficiency Rickets
Footnote: A 17‐year‐old patient with marked genu valgum deformities due to dietary calcium deficiency.
[Source 23 ]What is calcium?
Calcium (Ca or Ca2+) is the most abundant mineral in your body that is found in bones and teeth, in some foods, added to others, available as a dietary supplement, and present in some medicines (such as gastric antacids e.g. calcium phosphate) 47. Calcium is a mineral that your body needs for numerous functions, including building and maintaining bones and teeth, blood clotting, the transmission of nerve impulses, and the regulation of the heart’s rhythm 48. About 99% of the calcium in your body is stored in your bones and teeth in the form of calcium hydroxyapatite [Ca10(PO4)6(OH)2] crystals, an inorganic matrix of calcium and phosphate 21, 49, 50, 45. While the other 1% of the calcium in your body is found in your blood and soft tissue. Calcium concentrations in your blood and fluid surrounding the cells (extracellular fluid) must be maintained within a narrow concentration range for normal physiological functioning. And your body uses your bones as a reservoir for, and source of, calcium to maintain calcium homeostasis (the state of steady or stable equilibrium of internal physical and chemical conditions) 21. Because the physiological functions of calcium are so vital for survival, your body will stimulate bone resorption (demineralization) to maintain normal blood calcium concentrations when calcium intake is inadequate 45. Thus, adequate intake of calcium is a critical factor in maintaining a healthy skeleton 51.
Calcium is required for narrowing of blood vessels (vascular contraction) and widening of blood vessels (vasodilation), muscle function, nerve transmission, intracellular signaling and hormonal secretion, though less than 1% of total body calcium is needed to support these critical metabolic functions 21. Serum calcium is very tightly regulated and does not fluctuate with changes in dietary intakes; your body uses bone tissue as a reservoir for, and source of calcium, to maintain constant concentrations of calcium in blood, muscle, and intercellular fluids 21. Unlike your teeth, your bone undergoes continuous remodeling, with constant resorption and deposition of calcium into new bone 49. Bone remodeling is required to change bone size during growth, repair damage, maintain serum calcium levels, and provide a source of other minerals 49.
The balance between bone resorption and deposition changes with age. Bone formation exceeds resorption in periods of growth in children and adolescents, whereas in early and middle adulthood both processes are relatively equal. At birth, the body contains about 26 to 30 g calcium 44. This amount rises quickly after birth, reaching about 1,200 g (1.2 kg) in women and 1,400 g (1.4 kg) in men by adulthood 21. These levels remain constant in men, but they start to drop in women as a result of increases in bone remodeling due to decreased estrogen production at the start of menopause 21. In aging adults, particularly among postmenopausal women, bone breakdown exceeds formation, resulting in bone loss that increases the risk of osteoporosis over time 21.
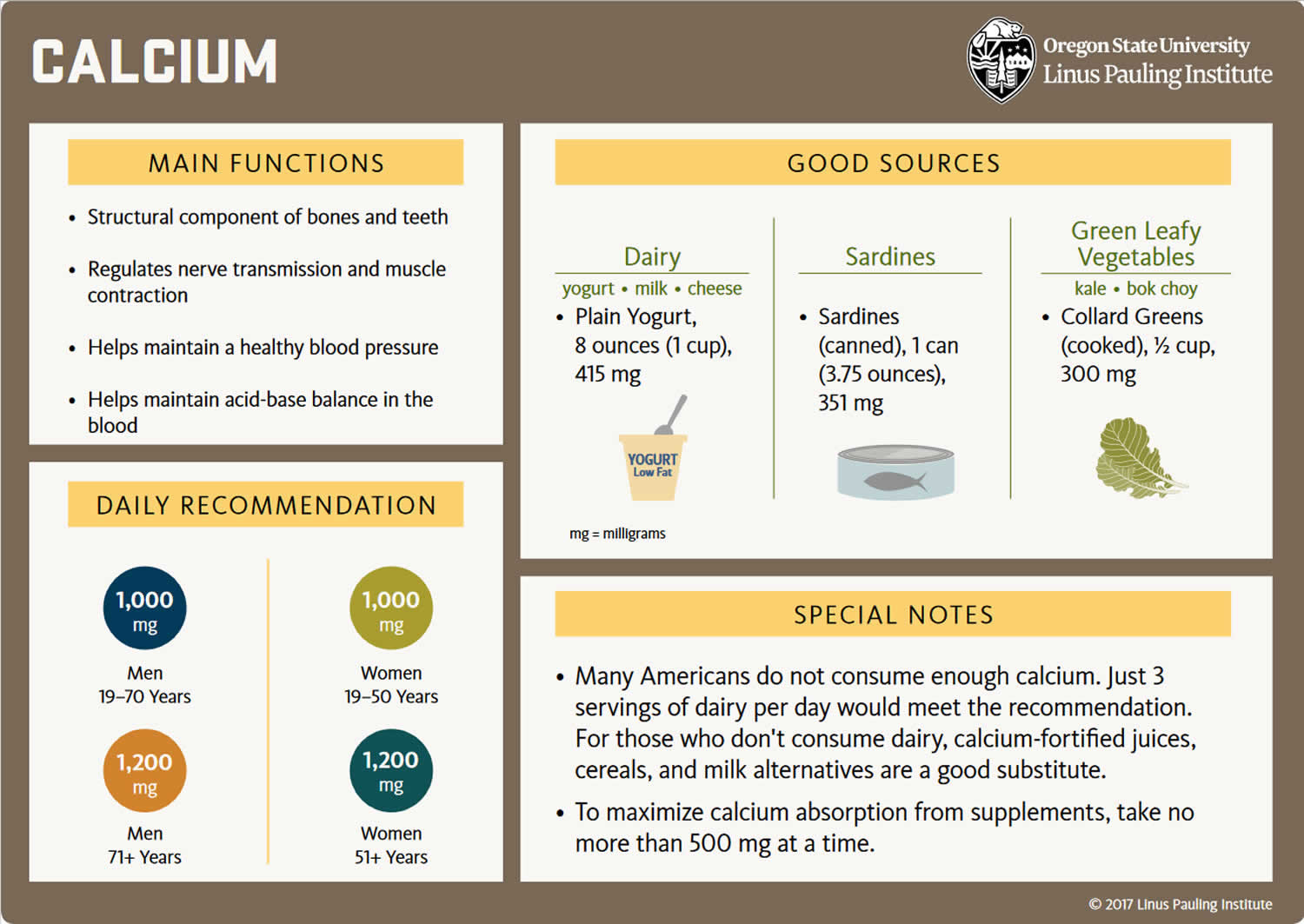
Your body gets the calcium you need in two ways. One is by eating foods or supplements that contain calcium. Good sources include dairy products, which have the highest concentration per serving of highly absorbable calcium, and dark leafy greens or dried beans, which have varying amounts of absorbable calcium. Calcium supplements often contain vitamin D; taking calcium paired with vitamin D seems to be more beneficial for bone health than taking calcium alone 48.
Calcium is found in many foods. It is important to get plenty of calcium in the foods you eat. You can get recommended amounts of calcium by eating a variety of foods, including the following 39:
- Dairy products such as milk, cheese, and yogurt are the main food sources of calcium for most people in the United States.
- Fish with soft bones that you eat, such as canned sardines and salmon.
- Certain vegetables, such as kale, broccoli, and Chinese cabbage (bok choi) also contain calcium.
- Calcium is added to some breakfast cereals and beverages, including many fruit juices and milk substitutes such as soy and almond beverages, as well as some brands of tofu and ready-to-eat cereals. To find out whether these foods have calcium added, check the product labels.
- Most grains (such as breads, pastas, and unfortified cereals) do not have high amounts of calcium. However, because people eat them often, what they contribute adds up.
The other way your body gets calcium is by pulling it from your bones. This happens when the blood levels of calcium drop too low (hypocalcemia), usually when it’s been awhile since having eaten a meal containing calcium. Ideally, the calcium that is “borrowed” from the bones will be replaced at a later point. But, this doesn’t always happen. Most important, this payback can’t be accomplished simply by eating more calcium 48.
The exact amount of calcium you need depends on your age, sex and other factors 39. Growing children and teenagers need more calcium than young adults. Older women need plenty of calcium to prevent osteoporosis. People who do not eat enough high-calcium foods should take a calcium supplement.
An inverse relationship exists between calcium intake and absorption 44. Absorption of calcium from food is about 45% at intakes of 200 mg/day but only 15% when intakes are higher than 2,000 mg/day 52. Age can also affect absorption of dietary calcium 21, 49. Net absorption of dietary calcium is as high as 60% in infants and young children, who need substantial amounts to build bone, but it decreases to about 25% in adulthood and continues to decline with age 21.
Total calcium levels can be measured in serum or plasma; serum levels are typically 8.8 to 10.4 mg/dL (2. 2 to 2.6 mmol/L) in healthy people 53, 21. However, serum calcium levels do not reflect nutritional status because of their tight homeostatic control 49. Levels of ionized or free calcium (Ca2+), the biologically active form, in serum are also used to measure calcium status. The normal range of ionized calcium (Ca2+) in healthy people is 4.6 to 5.3 mg/dL (1.15 to 1.33 mmol/L) 53. Dual x-ray absorptiometry (DEXA) testing of bone mineral density (BMD) can be used to assess cumulative calcium status over the lifetime because the skeleton stores almost all calcium in the body 54.
Calcium and phosphate concentrations are linked by their ability to chemically react to form calcium phosphate. The product of concentrations of calcium and phosphate (in mEq/L) is estimated to be < 60 normally; when the product exceeds 70, precipitation of calcium phosphate crystals in soft tissue is much more likely. Calcification of vascular tissue accelerates arteriosclerotic vascular disease and may occur when the calcium and phosphate product is even lower (> 55), especially in patients with chronic kidney disease.
What does calcium do?
Calcium is a mineral your body needs to build and maintain strong bones and to carry out many important functions. Your body needs calcium for muscles to move and for nerves to carry messages between your brain and every part of your body. Calcium also helps blood vessels move blood throughout your body and helps release hormones that affect many functions in your body. Vitamin D helps your body absorb calcium.
Calcium plays a role in:
- strengthening bones and teeth
- regulating muscle functioning, such as contraction and relaxation
- regulating heart functioning
- blood clotting
- transmission of nervous system messages
- enzyme function.
Structural element in bones and teeth
Calcium is a major structural element in bones and teeth. The mineral component of bone consists mainly of hydroxyapatite [Ca10(PO4)6(OH)2] crystals, which contain large amounts of calcium, phosphorus, and oxygen. Bone is a dynamic tissue that is remodeled throughout life. Bone cells called osteoclasts begin the process of remodeling by dissolving or resorbing bone. Bone-forming cells called osteoblasts then synthesize new bone to replace the bone that was resorbed. During normal growth, bone formation exceeds bone resorption. Osteoporosis may result when bone resorption chronically exceeds formation 21.
Calcium homeostasis
Calcium concentrations in the blood and fluid that surround cells are tightly controlled in order to preserve normal physiological function. A slight drop in blood calcium concentration (e.g., in the case of inadequate calcium intake) is sensed by the parathyroid glands, resulting in their increased secretion of parathyroid hormone (PTH). In the kidneys, PTH stimulates the conversion of vitamin D into its active form (1,25-dihydroxyvitamin D; calcitriol), which rapidly decreases urinary excretion of calcium but increases urinary excretion of phosphorus. Elevations in PTH also stimulates bone resorption, resulting in the release of bone mineral (calcium and phosphate) — actions that also contribute to restoring serum calcium concentrations. Increased circulating calcitriol (1,25-dihydroxyvitamin D) also triggers intestinal absorption of both calcium and phosphorus. Like PTH, calcitriol (1,25-dihydroxyvitamin D) stimulates the release of calcium from bone by activating osteoclasts (bone-resorbing cells). When blood calcium rises to normal levels, the parathyroid glands stop secreting PTH. A slight increase in blood calcium concentration stimulates the production and secretion of the peptide hormone, calcitonin, by the thyroid gland. Calcitonin inhibits PTH secretion, decreases both bone resorption and intestinal calcium absorption, and increases urinary calcium excretion (Figure 1). Finally, acute changes in blood calcium concentrations do not seem to elicit the secretion of the phosphaturic hormone fibroblast growth factor 23 (FGF-23), which is produced by bone-forming cells (osteoblasts/osteocytes) in response to increases in phosphorus intake 55. While this complex system allows for rapid and tight control of blood calcium concentrations, it does so at the expense of the skeleton 21.
Cell signaling
Calcium plays a role in mediating the constriction and relaxation of blood vessels (vasoconstriction and vasodilation), nerve impulse transmission, muscle contraction, and the secretion of hormones like insulin 21. Excitable cells, such as skeletal muscle and nerve cells, contain voltage-dependent calcium channels in their cell membranes that allow for rapid changes in calcium concentrations. For example, when a nerve impulse stimulates a muscle fiber to contract, calcium channels in the cell membrane open to allow calcium ions into the muscle cell. Within the cell, these calcium ions bind to activator proteins, which help release a flood of calcium ions from storage vesicles of the endoplasmic reticulum (ER) inside the cell. The binding of calcium to the protein troponin-c initiates a series of steps that lead to muscle contraction. The binding of calcium to the protein calmodulin activates enzymes that break down muscle glycogen to provide energy for muscle contraction. Upon completion of the action, calcium is pumped outside the cell or into the endoplasmic reticulum (ER) until the next activation 56.
Regulation of protein function
Calcium is necessary to stabilize a number of proteins, including enzymes, optimizing their activities. The binding of calcium ions is required for the activation of the seven “vitamin K-dependent” clotting factors in the coagulation cascade. The term, “coagulation cascade,” refers to a series of events, each dependent on the other that stops bleeding through clot formation.
How much calcium do I need per day?
Intake recommendations for calcium and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by the Food and Nutrition Board at the Institute of Medicine of the National Academies 11. Dietary Reference Intake (DRI) is the general term for a set of reference values used for planning and assessing the nutrient intakes of healthy people. These values, which vary by age and gender, include:
- Recommended Dietary Allowance (RDA): average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals.
- Adequate Intake (AI): established when evidence is insufficient to develop an RDA and is set at a level assumed to ensure nutritional adequacy.
- Estimated Average Requirement (EAR): average daily level of intake estimated to meet the requirements of 50% of healthy individuals. It is usually used to assess the adequacy of nutrient intakes in populations but not individuals.
- Tolerable Upper Intake Level (UL): maximum daily intake unlikely to cause adverse health effects.
The Food and Nutrition Board established Recommended Dietary Allowances (RDAs) for the amounts of calcium required for bone health and to maintain adequate rates of calcium retention in healthy people. They are listed in Table 1 in milligrams (mg) per day.
Many people in the United States don’t get recommended amounts of calcium from the foods they eat especially:
- Children and teens aged 4 to 18 years
- People who are Black or Asian
- Adults aged 50 years and older living in poverty
When total intakes of calcium from both food and supplements are considered, many people—particularly adolescent girls—still fall short of getting enough calcium, while some older women likely get more than the upper limit.
Certain groups of people are more likely than others to have trouble getting enough calcium, including:
- Postmenopausal women. The body absorbs and retains less calcium after menopause. Over time, this can lead to fragile bones.
- People who don’t drink milk or eat other dairy products. Dairy products are rich sources of calcium, but people with lactose intolerance, people with milk allergies, and vegans (people who don’t consume any animal products) must find other sources of calcium. Options include lactose-free or reduced-lactose dairy products; canned fish with bones; certain vegetables, such as kale, broccoli, and Chinese cabbage; calcium-fortified fruit juices and milk substitutes such as soy and almond beverages, tofu, and ready-to-eat cereals; and dietary supplements that contain calcium.
People should get most of their nutrients from food, advises the federal government’s Dietary Guidelines for Americans 57. Foods contain vitamins, minerals, dietary fiber and other substances that benefit health. In some cases, fortified foods and dietary supplements may provide nutrients that otherwise may be consumed in less-than-recommended amounts. For more information about building a healthy diet, refer to the Dietary Guidelines for Americans (https://www.dietaryguidelines.gov) and the U.S. Department of Agriculture’s MyPlate (https://www.myplate.gov).
In its food guidance system, the U.S. Department of Agriculture’s MyPlate (https://www.myplate.gov) recommends that persons aged 9 years and older eat 3 cups of foods from the milk group per day 58. A cup is equal to 1 cup (8 ounces) of milk, 1 cup of yogurt, 1.5 ounces of natural cheese (such as Cheddar), or 2 ounces of processed cheese (such as American).
Table 1. Recommended Dietary Allowances (RDAs) for Calcium
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months | 200 mg |
| Infants 7–12 months | 260 mg |
| Children 1–3 years | 700 mg |
| Children 4–8 years | 1,000 mg |
| Children 9–13 years | 1,300 mg |
| Teens 14–18 years | 1,300 mg |
| Adults 19–50 years | 1,000 mg |
| Adult men 51–70 years | 1,000 mg |
| Adult women 51–70 years | 1,200 mg |
| Adults 71 years and older | 1,200 mg |
| Pregnant and breastfeeding teens | 1,300 mg |
| Pregnant and breastfeeding adults | 1,000 mg |
Footnote: *Adequate Intake (intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an Recommended Dietary Allowance (RDA).
[Source 39 ]What foods provide calcium?
Calcium is found in many foods. It is important to get plenty of calcium in the foods you eat. You can get recommended amounts of calcium by eating a variety of foods, including the following 39:
- Dairy products such as milk, cheese, and yogurt are the main food sources of calcium for most people in the United States.
- Fish with soft bones that you eat, such as canned sardines and salmon.
- Certain vegetables, such as kale, broccoli, and Chinese cabbage (bok choi) also contain calcium.
- Calcium is added to some breakfast cereals and beverages, including many fruit juices and milk substitutes such as soy and almond beverages, as well as some brands of tofu and ready-to-eat cereals. To find out whether these foods have calcium added, check the product labels.
- Most grains (such as breads, pastas, and unfortified cereals) do not have high amounts of calcium. However, because people eat them often, what they contribute adds up.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central website (https://fdc.nal.usda.gov) lists the nutrient content of many foods with Calcium arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/Calcium-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/Calcium-Food.pdf).
Milk, yogurt, and cheese are rich natural sources of calcium and are the major food contributors of this nutrient to people in the United States 11. Nondairy sources include vegetables, such as Chinese cabbage, kale, and broccoli. Spinach provides calcium, but its bioavailability is poor. Most grains do not have high amounts of calcium unless they are fortified; however, they contribute calcium to the diet because they contain small amounts of calcium and people consume them frequently. Foods fortified with calcium include many fruit juices and drinks, tofu, and cereals. Selected food sources of calcium are listed in Table 2.
Calcium absorption varies by type of food. The absorption of calcium from dairy products and fortified foods is about 30% 21. Certain compounds in plants (e.g., oxalic acid, phytic acid) can decrease calcium absorption by forming indigestible salts with calcium, decreasing its absorption 54. As a result, absorption of calcium is only 5% for spinach, whereas it is much higher, at 27%, for milk 54. In addition to spinach, foods with high levels of oxalic acid include collard greens, sweet potatoes, rhubarb, and beans 21. The bioavailability of calcium from other plants that do not contain these compounds—including broccoli, kale, and cabbage—is similar to that of milk, although the amount of calcium per serving is much lower 54. When people eat many different types of foods, these interactions with oxalic or phytic acid probably have little or no nutritional consequence. Net absorption of dietary calcium is also reduced to a small extent by intakes of caffeine and phosphorus and to a greater extent by low status of vitamin D 59, 60, 61.
Table 2. Calcium Rich Foods
| Food* | Milligrams (mg) per serving | Percent DV* |
|---|---|---|
| Yogurt, plain, low fat, 8 ounces | 415 | 32 |
| Orange juice, calcium fortified, 1 cup | 349 | 27 |
| Yogurt, fruit, low fat, 8 ounces | 344 | 27 |
| Mozzarella, part skim, 1.5 ounces | 333 | 26 |
| Sardines, canned in oil, with bones, 3 ounces | 325 | 25 |
| Milk, nonfat, 1 cup** | 299 | 23 |
| Soymilk, calcium fortified, 1 cup | 299 | 23 |
| Milk, whole (3.25% milk fat), 1 cup** | 276 | 21 |
| Tofu, firm, made with calcium sulfate, ½ cup*** | 253 | 19 |
| Salmon, pink, canned, solids with bones, 3 ounces | 181 | 14 |
| Cottage cheese, 1% milk fat, 1 cup | 138 | 11 |
| Tofu, soft, made with calcium sulfate, ½ cup*** | 138 | 11 |
| Soybeans, cooked, ½ cup | 131 | 10 |
| Breakfast cereals, fortified with 10% of the DV for calcium, 1 serving | 130 | 10 |
| Spinach, boiled, drained, ½ cup | 123 | 9 |
| Frozen yogurt, vanilla, soft serve, ½ cup | 103 | 8 |
| Turnip greens, fresh, boiled, ½ cup | 99 | 8 |
| Kale, fresh, cooked, 1 cup | 94 | 7 |
| Chia seeds, 1 tablespoon | 76 | 6 |
| Chinese cabbage (bok choi), raw, shredded, 1 cup | 74 | 6 |
| Beans, pinto, canned, drained, ½ cup | 54 | 4 |
| Tortilla, corn, one, 6” diameter | 46 | 4 |
| Sour cream, reduced fat, 2 tablespoons | 31 | 2 |
| Bread, whole-wheat, 1 slice | 30 | 2 |
| Kale, raw, chopped, 1 cup | 24 | 2 |
| Broccoli, raw, ½ cup | 21 | 2 |
| Apple, golden delicious, with skin, 1 medium | 10 | 0 |
Footnote: * DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The Daily Value (DV) for calcium is 1,300 mg for adults and children age 4 years and older 62. FDA requires food labels to list calcium content. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
** Calcium content varies slightly by fat content; the more fat in the food, the less calcium it contains.
*** Calcium content is for tofu processed with a calcium salt. Tofu processed with other salts does not provide significant amounts of calcium.
Hypocalcemia causes
Hypocalcemia usually implies abnormal parathyroid function since the skeleton provides a large reserve of calcium for maintaining normal blood levels, especially in the case of low dietary calcium intake 45. Other causes of abnormally low blood calcium concentrations include chronic kidney failure, vitamin D deficiency usually associated with iatrogenic hypoparathyroidism in a post-thyroidectomy patient, and low blood magnesium levels often observed in cases of severe alcoholism 45, 64. Magnesium deficiency can impair parathyroid hormone (PTH) secretion by the parathyroid glands and lower the responsiveness of osteoclasts to PTH 45. Therefore, magnesium supplementation is required to correct hypocalcemia in people with low serum magnesium concentrations 45. In general, kidney failure remains by far the most common cause of hypocalcemia, followed by vitamin D deficiency, magnesium deficiency and acute pancreatitis 22.
Common causes of hypocalcemia 6:
- Vitamin D deficiency as a result of limited exposure to ultraviolet light or low dietary intake
- Vitamin D deficiency as a result of malabsorption
- Hypoparathyroidism as a result of surgery
- Hypoparathyroidism as a result of autoimmune disease
- Kidney disease
Rare causes of hypocalcemia 6:
- Parathyroid hormone resistance
- Vitamin D resistance
- Autosomal dominant hypocalcemia
- Hypomagnesemia
- Sclerotic metastases
Other causes of hypocalcemia 6:
- Hungry bone syndrome after parathyroidectomy for hyperparathyroidism 65
- Infusion of phosphate or calcium chelators, such as citrate, with massive blood transfusion
- Critical illness
- After intravenous treatment with bisphosphonates, especially high dose treatment in vitamin D deficient patients.
Parathyroid hormone (PTH) deficiency (low or low normal serum PTH)
Parathyroid Hormone (PTH) Deficiency occurs as a result of decreased PTH secretion, which can be due to destruction of the parathyroid glands (postsurgical or autoimmune), abnormal regulation of PTH production and secretion, or abnormal development of the parathyroid gland. Post-surgical is the most common cause of hypoparathyroidism 22.
- Post thyroidectomy, parathyroidectomy, or radical neck surgery – Post thyroidectomy, parathyroidectomy, or radical neck surgery is the most common cause of transient or permanent hypoparathyroidism leading to hypocalcemia 22. The normal parathyroid gland is made up of about 30% capillary cells. This makes the parathyroid gland very sensitive to disruption of arterial blood supply or venous drainage, which can result from mechanical, thermal, or electrical injury during thyroidectomy. The resulting hypoparathyroidism is usually transient but can also be permanent with subsequent transient or permanent hypocalcemia. Accidental removal of all 4 parathyroid glands during thyroidectomy, though not common, is also a major cause of hypoparathyroidism. Hypoparathyroidism after parathyroidectomy is usually a result of suppression of the remaining parathyroid glands by hypercalcemia from parathyroid adenoma before surgery. This is also transient in most cases but is usually permanent if all 4 glands are removed without autotransplantation of the parathyroid gland. In cases of severe hyperparathyroidism with significantly elevated PTH levels before surgery, as in tertiary hyperparathyroidism in kidney disease, the abrupt drop in PTH levels after surgery can lead to severe hypocalcemia due to unopposed osteoblast activity causing significant calcium uptake into the bones. This condition is termed “hungry bone syndrome” 66, 67, 68
- Autoimmune – Autoantibodies against the parathyroid gland are the main cause of autoimmune hypoparathyroidism which can be a manifestation of polyglandular autoimmune syndrome type 1 along with chronic mucocutaneous candidiasis and adrenal insufficiency.
- Abnormal parathyroid gland development: X-linked or autosomal recessive hypoparathyroidism causes abnormal parathyroid gland development. This can be isolated or associated with complex congenital syndromes like DiGeorge syndrome.
- Parathyroid gland destruction: Parathyroid gland destruction can also be due to rare causes such as infiltrative diseases of the parathyroid glands like granulomatous diseases, hemochromatosis, Wilson disease, or irradiation. Human immunodeficiency virus (HIV) infection is also a rare cause of symptomatic hypoparathyroidism. Lastly, activating mutation of calcium-sensing receptors (CaSR) decreases the setpoint of CaSR, causing hypoparathyroidism and hypocalcemia.
Acquired hypoparathyroidism may result from the following:
- Neck irradiation/radioiodine therapy 69
- Postparathyroidectomy in dialysis patients 70
- Inadvertent surgical removal (can be transient or permanent)
- Infiltrative disease (eg, hemochromatosis, granulomatous disease [sarcoidosis], thalassemia, amyloidosis, or metastatic malignant infiltration
Late-onset hypoparathyroidism can be seen as a part of a complex autoimmune disorder involving ovarian failure and adrenal failure. Mucocutaneous candidiasis, alopecia, vitiligo, and pernicious anemia are associated with this disorder, which is referred to as polyglandular autoimmune disease (PGA 1).
Hereditary hypoparathyroidism may be familial or sporadic, and it can occur as an isolated entity or can be associated with other endocrine manifestations. The familial forms include autosomal dominant and autosomal recessive, as well as a sex-linked form of early onset, for which the gene has been located on the long arm of the X chromosome.
Sporadic, late-onset hypoparathyroidism is a feature of several hereditary syndromes. These syndromes, and their associated features, are as follows:
- DiGeorge syndrome: congenital heart disease, cleft palate/lip, and abnormal facies
- Kearns-Sayre syndrome: heart block, retinitis pigmentosa, and ophthalmoplegia
- Kenny-Caffey syndrome: medullary stenosis of the long bones and growth retardation
Hypoparathyroidism
Hypoparathyroidism is characterized by hypocalcemia and hyperphosphatemia and often causes chronic tetany. Hypoparathyroidism results from deficient parathyroid hormone (PTH), which can occur in autoimmune disorders or after the accidental removal of or damage to several parathyroid glands during thyroidectomy. Transient hypoparathyroidism is common after subtotal thyroidectomy, but permanent hypoparathyroidism occurs after < 3% of such thyroidectomies done by experienced surgeons. Manifestations of hypocalcemia usually begin about 24 to 48 hours postoperatively but may occur after months or years. Parathyroid hormone (PTH) deficiency is more common after radical thyroidectomy for cancer or as the result of surgery on the parathyroid glands (subtotal or total parathyroidectomy). Risk factors for severe hypocalcemia after subtotal parathyroidectomy include:
- Severe preoperative hypercalcemia
- Removal of a large adenoma
- Elevated alkaline phosphatase
- Chronic kidney disease
Idiopathic hypoparathyroidism is an uncommon sporadic or inherited condition in which the parathyroid glands are absent or atrophied. It manifests in childhood. The parathyroid glands are occasionally absent and thymic aplasia and abnormalities of the arteries arising from the brachial arches (DiGeorge syndrome) are present. Other inherited forms include polyglandular autoimmune failure syndrome, autoimmune hypoparathyroidism associated with mucocutaneous candidiasis, and X-linked recessive idiopathic hypoparathyroidism.
High parathyroid hormone (PTH)
- Chronic Kidney Disease (CKD) – Chronic kidney disease (CKD) leads to impaired phosphate excretion and impaired hydroxylation of 25 hydroxyvitamin D to 1,25-dihydroxy vitamin D. This drives PTH secretion and can cause secondary hyperparathyroidism. However, due to impaired vitamin D metabolism and high phosphorus level, the serum calcium remains low despite the high PTH.
- Absolute or relative vitamin D defeciency – Vitamin D maintains normal calcium by enhancing intestinal calcium absorption and bone resorption. Vitamin D deficiency could be from decreased intake or malabsorption, inadequate sun exposure, liver disease, kidney disease results, and decrease conversion to its active metabolite (1,25-dihydroxy vitamin D). This can lead to decreased calcium absorption and bone resorption. The resulting hypocalcemia leads to a compensatory increase in PTH secretion (secondary hyperparathyroidism).
- Pseudohypoparathyroidism – This is a genetic disorder that causes end-organ resistance to the action of PTH and is characterized by hypocalcemia, hyperphosphatemia, and elevated PTH concentration.
Kidney disease
Renal tubular disease, including acquired proximal renal tubular acidosis due to nephrotoxins (eg, heavy metals, cadmium in particular) and distal renal tubular acidosis, can cause severe hypocalcemia due to abnormal renal loss of calcium and decreased renal conversion of vitamin D to active 1,25-dihydroxyvitamin D [1,25(OH)2D also known as “calcitriol”], particularly when the glomerular filtration rate (GFR) falls below 30 mL/min. This results in an increase in PTH. Ultimately, the increased absorption of phosphorus and calcium can lead to calcium-phosphorus mineral deposition in the soft tissues. In the early stages of renal failure, hypocalcemia can occur because of the decrease in calcitriol production and a subsequent decrease in the intestinal absorption of calcium.
Renal failure can result in diminished formation of 1,25-dihydroxyvitamin D [1,25(OH)2D also known as “calcitriol”] due to:
- Direct renal cell damage
- Suppression of 1-alpha-hydroxylase (needed for the vitamin D conversion) by hyperphosphatemia.
Vitamin D deficiency and dependency
Vitamin D is a necessary cofactor for the normal response to PTH, and vitamin D deficiency renders PTH ineffective. Poor nutritional intake, chronic renal insufficiency, or reduced exposure to sunlight may cause vitamin D deficiency.
Vitamin D deficiency is common worldwide. It is a common cause of rickets and osteomalacia, but these disorders may also result from other conditions, such as chronic kidney disease, various renal tubular disorders, familial hypophosphatemic (vitamin D–resistant) rickets, chronic metabolic acidosis, hyperparathyroidism, hypoparathyroidism, inadequate dietary calcium, and disorders or drugs that impair the mineralization of bone matrix.
Vitamin D deficiency causes hypocalcemia, which stimulates production of PTH, causing hyperparathyroidism. Hyperparathyroidism increases absorption, bone mobilization, and renal conservation of calcium but increases excretion of phosphate. As a result, the serum level of calcium may be normal, but because of hypophosphatemia, bone mineralization is impaired.
Vitamin D deficiency may result from the following:
- Inadequate exposure to sunlight
- Inadequate intake of vitamin D
- Reduced absorption of vitamin D
- Abnormal metabolism of vitamin D
- Resistance to the effects of vitamin D
Current Recommended Dietary Allowances (RDAs) for vitamin D are 600 IU (15 mcg) of vitamin D per day for adults for individuals from 14 to 70 years of age and 800 IU per day for those over 70 years (20 mcg) 71. Studies have demonstrated that despite adequate intake, that vitamin D insufficiency can still occur and lead to an increased PTH and subsequent bone turnover. Studies have also shown that dietary intake of vitamin D varies greatly by race and age. In a review of National Health and Nutrition Examination Survey (NHANES) III data from 2001-2006, 32% of African-American women were at risk for vitamin D deficiency—defined as serum 25-hydroxyvitamin D (24[OH]D) levels < 30 nmol/L—as compared with only 3% of white women 72.
An observational study in elderly adults found that 74% of those studied were deficient in vitamin D, defined as 25(OH)D concentrations < 32 ng/mL, despite intake of more than 400-600 IU/d, which was the recommended RDA at the time 72. The authors of this study suggested that elderly individuals may require as much as 1000 IU per day.
Mild hypovitaminosis D may not be trivial. In an elderly population with an increased PTH and osteoporosis, response to alendronate was attenuated. This attenuation was improved when vitamin D was administered 73.
Inadequate exposure or intake
Inadequate direct sunlight exposure or sunscreen use and inadequate intake usually occur simultaneously to result in clinical deficiency. Susceptible people include:
- The elderly (who are often undernourished and are not exposed to enough sunlight)
- Certain communities (eg, women and children who are confined to the home or who wear clothing that covers the entire body and face)
Inadequate vitamin D stores are common among the elderly, particularly those who are housebound, institutionalized, or hospitalized or who have had a hip fracture.
Recommended direct sunlight exposure is 5 to 15 min (suberythemal dose) to the arms and legs or to the face, arms, and hands, at least 3 times a week. However, many dermatologists do not recommend increased sunlight exposure because risk of skin cancer is increased.
Reduced absorption
- Malabsorption can deprive the body of dietary vitamin D; only a small amount of 25(OH)D is recirculated enterohepatically. Numerous conditions can impair the absorption of vitamin D. Small bowel diseases, such as celiac disease, gastric bypass (particularly long limb Roux-en-Y gastric bypass), steatorrhea, and pancreatic diseases can all lead to low vitamin D levels 74.
Abnormal metabolism
Vitamin D deficiency may result from defects in the production of 25(OH)D or 1,25(OH)2D. People with chronic kidney disease commonly develop rickets or osteomalacia because renal production of 1,25 (OH)2D is decreased and phosphate levels are elevated. Hepatic dysfunction can also interfere with production of active vitamin D metabolites.
Type I hereditary vitamin D–dependent rickets is an autosomal recessive disorder characterized by absent or defective conversion of 25(OH)D to 1,25(OH)2D in the kidneys. X-linked familial hypophosphatemia reduces vitamin D synthesis in the kidneys.
Many anticonvulsants and use of glucocorticoids increase the need for vitamin D supplementation.
Resistance to effects of vitamin D
Type II hereditary vitamin D–dependent rickets has several forms and is due to mutations in the 1,25(OH)2D receptor. This receptor affects the metabolism of gut, kidney, bone, and other cells. In this disorder, 1,25(OH)2D is abundant but ineffective because the receptor is not functional.
Pseudovitamin D deficiency rickets
This condition is secondary to an autosomal mutation of the 1-hydroxylase gene. Ultimately, calcidiol is not hydroxylated to calcitriol, and calcium is not absorbed appropriately. This condition is considered a pseudovitamin D deficiency because high doses of vitamin D can overcome the clinical and biochemical findings of this disease.
Hereditary vitamin D resistance rickets
This condition is extremely rare and is caused by a mutation in the vitamin D receptor. Typically, this condition presents within the first 2 years of life.
Pseudohypoparathyroidism
Pseudohypoparathyroidism is an uncommon group of disorders characterized not by hormone deficiency but by target organ resistance to PTH. Pseudohypoparathyroidism is classified into types I and II. Type I is further subdivided into Ia, Ib, and Ic 75. Complex genetic transmission of these disorders occurs.
- Type Ia pseudohypoparathyroidism (Albright hereditary osteodystrophy) is caused by a mutation in the stimulatory Gs-alpha1 protein of the adenylyl cyclase complex (GNAS1). The result is failure of normal renal phosphaturic response or increase in urinary cAMP to PTH. Patients are usually hypocalcemic and hyperphosphatemic. Secondary hyperparathyroidism and hyperparathyroid bone disease can occur. Type Ia pseudohypoparathyroidism comprises the biochemical features of pseudohypoparathyroidism along with the following somatic features of Albright hereditary osteodystrophy:
- Short stature
- Mental retardation with calcification of the basal ganglia
- Obesity
- Round-shaped face
- Brachymetacarpia (shortened metacarpal bones)
- Brachymetatarsia (shortened metatarsal bones)
- Subcutaneous bone formation
- Mild hypothyroidism, and other subtle endocrine abnormalities.
- Because only the maternal allele for GNAS1 is expressed in the kidneys, patients whose abnormal gene is paternal, although they have many of the somatic features of the disease, do not have hypocalcemia, hyperphosphatemia, or secondary hyperparathyroidism; this condition is sometimes described as pseudopseudohypoparathyroidism.
- Laboratory findings in Albright hereditary osteodystrophy include hypocalcemia, hyperphosphatemia (with normal or high PTH levels), and low calcitriol. Vitamin D may be decreased because of inhibition by elevated levels of phosphorus and by decreased PTH stimulation of 25-hydroxyvitamin D 1-alpha-hydroxylase. The low calcitriol levels, in turn, may cause the resistance to the hypercalcemic effects of PTH in the bone.
- The defect of the Gs-alpha protein is not confined to the effects of PTH but also affects other hormonal systems (eg, resistance to glucagon, thyroid-stimulating hormone, gonadotropins). The gene for the Gs-alpha protein is located on chromosome 20. Some family members carry the mutation and display the Albright hereditary osteodystrophy phenotype but do not have pseudohypoparathyroidism. This is termed pseudo-pseudohypoparathyroidism.
- Type Ib pseudohypoparathyroidism is less well known. Affected patients have hypocalcemia, hyperphosphatemia, and secondary hyperparathyroidism but do not have the other associated abnormalities.
- In type Ic pseudohypoparathyroidism, patients present with resistance to multiple hormonal receptors. However, Gs-alpha protein expression is normal.
- Type II pseudohypoparathyroidism is even less common than type 1. In affected patients, exogenous PTH raises the urinary cAMP normally but does not raise serum calcium or urinary phosphate. An intracellular resistance to cAMP or defect is located downstream of the generation of cAMP has been proposed. These patients present with hypocalcemia, hypophosphaturia, and elevated immunoreactive PTH (iPTH) levels. These findings also occur in vitamin D deficiency, but in patients with a vitamin D deficiency, all parameters return to normal after vitamin D administration.
Other Causes
- Pseudohypocalcemia– Serum calcium is normally bound to protiens in the blood most prominently albumin and therefore low albumin states (hypoalbuminemia) can give a falsely low total serum calcium level. Ionized calcium level is usually normal in these states and thus to correct for hypoalbuminemia add 0.8 mg/dL to the total serum calcium for each 1.0 g/dL decrease in albumin below 4.0 g/dL.
- Corrected calcium (mg/dL) = 0.8 x (4.0 g per dL –[plasma albumin]) + [serum calcium (mg/dL)]
- For example, a calcium concentration of 8.22 mg/dL (2.05 mmol/L) with an albumin concentration of 35 g/L would be corrected to 8.62 mg/dL (2.15 mmol/L) [40 g/L – 35 g/L = 5 X 0.08 mg/dL = 0.4 mg/dL], which would correct the hypocalcemic value to normal. This estimation is often used, but it can be unreliable in some situations, such as critical illness 76. If it is doubtful whether total calcium reflects ionized calcium or free calcium, the ionized value can be checked directly. Other situations in which the assessment of serum calcium may be inappropriately low include recent use of certain gadolinium contrast agents and contamination of blood samples by EDTA 6.
- Note that calcium correction based on the above calculation may be inaccurate, particularly in geriatric patients. Ionized calcium levels should be obtained if hypocalcemia is considered to be clinically significant.
- Hypoalbuminemia is the most common cause of hypocalcemia. Causes include cirrhosis, nephrosis, malnutrition, burns, chronic illness, and sepsis. In patients who are critically ill, low calcium levels can be simply due to hypoalbuminemia, which has no clinical significance because the active fraction (ionized) is not affected. However, to prevent missing a second hypocalcemic disorder, measure the ionized calcium level whenever the albumin level is low.
- Acidosis/Aklalosis – Calcium binding to albumin is dependent on the serum pH, and thus in states of severe acidosis, ionized calcium is increased and vice-versa decreased in severe alkalosis. There is no reliable correction factor to estimate this shift in ionized calcium level, so direct measurement of ionized calcium is recommended in these cases to guide therapy.
- Acute pancreatitis – Hypocalcemia is often seen in the setting of acute pancreatitis due to calcium deposition in the abdominal cavity as a result of ongoing inflammation 77.
- Severe sepsis – Severe sepsis can lead to hypocalcemia through unclear mechanisms. Impaired PTH secretion, dysregulation of magnesium metabolism, and impaired calcitriol secretion have been identified as potential mechanisms, but none have been proven as of yet 78. In gram-negative sepsis, there is a reduction in total and ionized serum calcium. The mechanism for this remains unknown, but it appears to be associated with multiple factors, including elevated levels of cytokines (eg, interleukin-6, interleukin-1, TNF-alpha), hypoparathyroidism, and vitamin D deficiency or resistance. Mortality rates are increased in patients with sepsis and hypocalcemia, compared with patients who are normocalcemic 79. More recent reports also indicated hypocalcemia related to severe Covid-19 infection 80. However, there is no clear evidence that treating critically ill patients with supplemental calcium alters outcomes 81.
- Hypomagnesemia and hypermagnesemia
- Low serum magnesium (hypomagnesemia) can be commonly associated with hypocalcemia can cause relative parathyroid hormone deficiency and end-organ (bone and kidneys) resistance to PTH action, usually when serum magnesium concentrations are 0.8 mEq/L (1 mg/dL or 0.4 mmol/L). Decreased PTH secretion can occur in more severe hypomagnesemia 82. It is uncommon above a serum magnesium level of 1 mg/dL. The usual cause of hypomagnesemia is loss via the kidneys (eg, osmotic diuresis, drugs) or the gastrointestinal tract (eg, chronic diarrhea, severe pancreatitis, bypass or resection of small bowel). These patients present with low or inappropriately normal PTH levels in the presence of hypocalcemia. Acute magnesium restoration rapidly corrects the PTH level, suggesting the hypomagnesemia affects the release of PTH, rather than its synthesis.
- Severe hypermagnesemia although rare, can also cause hypocalcemia by suppressing PTH secretion thorough a decreased sensitivity of calcium-sensing receptors.
- Acute hyperphosphatemia – This is an uncommon cause of hypocalcemia which is likely precipitated because of extravascular deposition of calcium phosphate products. Hyperphosphatemia may be seen in critical illness and in patients who have ingested phosphate-containing enemas. Phosphate binds calcium avidly, causing acute hypocalcemia. Acute hypocalcemia secondary to hyperphosphatemia may also result from renal failure or excess tissue breakdown because of rhabdomyolysis or tumor lysis. In acute hyperphosphatemia, calcium is deposited mostly in the bone but also in the extraskeletal tissue. In contrast, in chronic hyperphosphatemia, which is nearly always from chronic renal failure, calcium efflux from the bone is inhibited and the calcium absorption is low, because of reduced renal synthesis of 1,25-dihydroxyvitamin D. However, other consequences of renal failure, including a primary impairment in calcitriol synthesis, also contribute to hypocalcemia.
- Drugs– Bisphosphonates, cinacalcet, phenytoin, phenobarbital, rifampin, denosumab and foscarnet can all cause hypocalcemia which can be severe in some cases. Concomitant vitamin D deficiency makes hypocalcemia more likely to occur in patients treated with those drugs. Patients receiving the calcimimetic agent cinacalcet that works by stimulating the calcium-sensing receptors (CaSR) and thus decreasing PTH secretion to help control both primary and secondary hyperparathyroidism in renal failure may experience hypocalcemia as a result of acute inhibition of PTH release. The resulting decrease in PTH secretion can cause hypocalcemia. Clinically significant hypocalcemia occurs in approximately 5% of patients treated with cinacalcet 83. Hypocalcemia can also occur in patients treated with some chemotherapeutic drugs. For example, cisplatin can induce hypocalcemia by causing hypomagnesemia, and combination therapy with 5-fluorouracil and leucovorin can cause mild hypocalcemia (65% of patients in one series), possibly by decreasing calcitriol production 84. In addition, acute kidney injury and hypocalcemia have been reported as adverse effects in patients receiving the programmed cell death protein 1 (PD-1) inhibitors nivolumab and pembrolizumab 85. Hypocalcemia may result from the treatment of hypercalcemia with bisphosphonates, particularly zoledronic acid, which is significantly more potent than other bisphosphonates in suppressing the formation and function of osteoclasts. Patients who are affected appear to lack an adequate PTH response to decreasing serum calcium levels 86. Hypocalcemia and osteomalacia have been described with prolonged therapy with anticonvulsants (eg, phenytoin, phenobarbital) 87. The mechanisms differ according to the class of anticonvulsants; for example, phenytoin induces cytochrome P450 enzymes and enhances vitamin D catabolism. Patients being treated with these agents should have their calcium and vitamin D levels checked, and low levels should be corrected before initiation of treatment. Cisplatin, a chemotherapeutic drug, can also cause hypocalcemia through hypomagnesemia. Foscarnet can cause hypocalcemia by forming complexes with ionized calcium, thereby reducing levels of ionized calcium. It is therefore important to regularly monitor calcium levels during treatment with all of the above-mentioned drugs 46, 88.
- Foscarnet is a drug used to treat refractory cytomegalovirus and herpes infections in patients who are immunocompromised, and it complexes ionized calcium and, therefore, lowers ionized calcium concentrations, potentially causing symptomatic hypocalcemia. Therefore, the ionized calcium concentration should be measured at the end of an infusion of foscarnet.
- Denosumab is a fully human monoclonal antibody to the receptor activator of nuclear factor kappaB ligand (RANKL), an osteoclast differentiating factor. It inhibits osteoclast formation, decreases bone resorption, increases bone mineral density (BMD), and reduces the risk of fracture. In the denosumab trials, all women were supplemented with daily calcium (1000 mg) and vitamin D (400-800 U). A small proportion of women in the denosumab trials had a decrease in the serum calcium level to less than 8.5 mg/dL. However, in patients with conditions that predispose to hypocalcemia, such as chronic kidney disease, malabsorption syndromes, or hypoparathyroidism, symptomatic hypocalcemia may occur. The nadir in serum calcium occurs approximately 10 days after administration. Thus, denosumab should not be given to patients with preexisting hypocalcemia until it is corrected. In addition, patients with conditions predisposing to hypocalcemia (ie, chronic kidney disease and creatinine clearance < 30 mL/min) should be monitored for hypocalcemia 89.
- Symptomatic hypocalcemia during transfusion of citrated blood or plasma is rare, because healthy patients rapidly metabolize citrate in the liver and kidney. However, a clinically important fall in serum ionized calcium concentration can occur if citrate metabolism is impaired due to hepatic or renal failure or if large quantities of citrate are given rapidly, for example, during plasma exchange or massive blood transfusion.
- Sodium phosphate preparations, which come in aqueous and tablet forms, are used to cleanse the bowel prior to GI procedures such as colonoscopy. In certain populations, these agents can lead to acute hyperphosphatemia and subsequent hypocalcemia 90. Risk factors include the following:
- Renal failure
- Advanced age
- Chronic heart failure
- Hepatic insufficiency
- Volume depletion
- Use of angiotensin-converting enzyme (ACE) inhibitors or nonsteroidal anti-inflammatory drugs (NSAIDS)
- Some radiographic contrast dyes may contain ethylenediaminetetraacetic acid (EDTA), which chelates calcium in serum, thereby reducing serum ionized calcium concentration, resulting in hypocalcemia. Gadolinium-based contrast material can falsely lower serum calcium levels and should be considered if levels are drawn shortly after magnetic resonance imaging.
- Rarely, an excess intake of fluoride can cause hypocalcemia; this effect is presumably mediated by inhibition of bone resorption. Overfluorinated public water supplies and ingestion of fluoride-containing cleaning agents have been associated with low serum calcium levels. In this case, hypocalcemia is thought to be due to excessive rates of skeletal mineralization secondary to formation of calcium difluoride complex.
- Proton pump inhibitors (PPIs) and histamine-2 receptor blockers (eg, cimetidine) reduce gastric acid production; this slows fat breakdown, which is necessary to complex calcium for gut absorption. An association with these medicines and an increased risk for hip fractures in elderly patients has been made because of decreased calcium absorption.
- Other medication effects that may lead to hypocalcemia are as follows:
- Calcitonin and bisphosphonates cause chelation and end-organ inhibition
- Ethylene glycol complexes with calcium
- Estrogen inhibits bone resorption
- Aluminum and alcohol suppress PTH
- Massive Blood transfusion – Transfusion of > 10 units of citrate-anticoagulated blood. Massive blood transfusion can cause an acute decline in ionized calcium due to calcium binding with citrate which is used to prevent the stored blood from clotting 91.
- Hypoproteinemia reduces the protein-bound fraction of serum calcium; hypocalcemia due to diminished protein binding is asymptomatic—because ionized calcium is unchanged, this entity has been termed factitious hypocalcemia.
- Hungry bone syndrome persistent hypocalcemia and hypophosphatemia occurring after surgical or medical correction of moderate to severe hyperparathyroidism (primary or secondary hyperparathyroidism) in patients in whom serum calcium concentrations had been supported by high bone turnover induced by greatly elevated PTH—hungry bone syndrome has been described after parathyroidectomy, after renal transplantation, and rarely in patients with end-stage renal disease treated with calcimimetics. Hungry bone syndrome may be associated with severe hypocalcemia due to a rapid increase in bone remodeling. Hypocalcemia results if the rate of skeletal mineralization exceeds the rate of osteoclast-mediated bone resorption. A less severe picture is also observed after correction of thyrotoxicosis, after institution of vitamin D therapy for osteomalacia, and with tumors associated with bone formation (eg, prostate, breast, leukemia). All of these disease states result in hypocalcemia due to mineralization of large amounts of unmineralized osteoid 92.
- Liver disease with decreased synthetic function can cause vitamin D deficiency from several sources, as follows:
- Impaired 25-hydroxylation of vitamin D
- Decreased bile salts with malabsorption of vitamin D
- Decreased synthesis of vitamin D–binding protein
- Other factors
- Patients with cirrhosis and osteomalacia have low or normal levels of calcitriol, suggesting that other factors may interfere with vitamin D function or are synergistic with malabsorption or decreased sun exposure. These patients require administration of calcidiol or calcitriol for the treatment of hypocalcemia.
- Use of radiocontrast agents containing the divalent ion-chelating agent ethylenediaminetetraacetate (EDTA) can decrease the concentration of bioavailable ionized calcium while total serum calcium concentrations remain unchanged.
- Infusion of gadolinium may spuriously lower calcium concentration.
- Postsurgical effects. The following surgical procedures may result in hypocalcemia:
- Parathyroidectomy causes a transient hypocalcemia due to end-organ PTH resistance in the first postoperative day; in addition, vascular/parathyroid injury may occur as an operative mishap; postoperative oral calcium supplementation, with dosing based on a protocol that considers patient variables affecting risk can prevent postoperative hypocalcemia in almost all cases 93.
- Pancreatectomy prevents calcium absorption in the duodenum and the jejunum by eliminating necessary enzymes
- Bowel resection may cause hypocalcemia by reducing the surface available to absorb fatty acids and calcium
- Although excessive secretion of calcitonin might be expected to cause hypocalcemia, calcitonin actually has only a minor effect on serum calcium. For example, low serum calcium concentrations rarely occur in patients with large amounts of circulating calcitonin due to medullary carcinoma of the thyroid.
- Enhanced protein binding and anion chelation: Protein binding is enhanced by elevated pH and free fatty acid release in high catecholamine states. Anion chelation is seen in high phosphate states (eg, renal failure, rhabdomyolysis, mesenteric ischemia, oral administration of phosphate-containing enemas); high citrate states (eg, massive blood transfusion, radiocontrast dyes); and high bicarbonate, lactate, and oxalate levels.
- Critical illness: Acute illness may lead to hypocalcemia for multiple reasons. In one study, the 3 most common factors identified in patients with hypocalcemia associated with acute illness were hypomagnesemia, acute renal failure, and transfusions.
- Pregnancy: There are reports of hypocalcemia during pregnancy, mostly related to poor diet, hyperemesis gravidarum, or underline diseases 94.
- Osteoblastic metastasis, as in prostate cancer, can cause hypocalcemia which can be severe in rare cases. This is a result of increased calcium uptake into the bones from increased osteoblastic activity.
- Hypocalcemia in the emergency department. Multifactorial causes are probably the most clinically relevant in hypocalcemic emergencies in the emergency department (ED). These include the following:
- Rhabdomyolysis: increased phosphates from creatine phosphokinase (CPK) and other anions (ie, lactate, bicarbonate) chelate calcium
- Toxic shock syndrome can cause hypocalcemia
- High calcitonin levels cause low calcium
- Malignancy: osteoblastic metastases (eg, breast cancer, prostate cancer) and tumor lysis syndrome may cause hypocalcemia (by differing mechanisms)
- Infiltrative disease: sarcoidosis, tuberculosis, and hemochromatosis may infiltrate the parathyroids, causing dysfunction
- Toxicologic causes include hydrofluoric acid burn or ingestion
- Trauma patients with massive transfusion will have hemostasis impairment as one effect of hypocalcemia 95
Hypocalcemia in pancreatitis
Pancreatitis can be associated with lipid abnormalities, hypocalcemia, and even tetany. With the development of animal models, the mechanism of hypocalcemia is known 96. When the pancreas is damaged, free fatty acids are generated by the action of pancreatic lipase. There are insoluble calcium salts present in the pancreas, and the free fatty acids avidly chelate the salts resulting in calcium deposition in the retroperitoneum. In addition, hypoalbuminemia may be part of the clinical picture so that there is a reduction in total serum calcium. If there is concomitant alcohol abuse, emesis or poor nutrition, hypomagnesemia may augment the problem. PTH levels can be normal, suppressed or elevated. If PTH levels are normal or suppressed, hypomagnesemia may be present. If PTH levels are elevated, this is a reflection of the hypocalcemia. In the treatment of these patients, parenteral calcium and magnesium replacements are indicated. Vitamin D status should be assessed to rule out malabsorption or nutritional deficiencies.
Groups at Risk of Calcium Deficiency
The following groups of people are more likely than others to have trouble getting enough calcium.
Postmenopausal women
Menopause leads to bone loss because decreases in estrogen production reduce calcium absorption and increase urinary calcium loss and calcium resorption from bone 21. On average, women lose approximately 1% of their bone mineral density (BMD) per year after menopause 97. Over time, these changes lead to decreased bone mass and fragile bones 21. About 30% of postmenopausal women in the United States and Europe have osteoporosis, and at least 40% of those with this condition develop at least one fragility fracture (a fracture that occurs after minor trauma, such as a fall from standing height or lower) 98. The calcium Recommended Dietary Allowance (average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals) is 1,200 mg for women older than 50 years (vs. 1,000 mg for younger women) to lessen bone loss after menopause 21.
Women of childbearing age whose menstrual periods stop
Women of childbearing age whose menstrual periods stop (amenorrhea) because they exercise heavily, eat too little, or both. They need sufficient calcium to cope with the resulting decreased calcium absorption, increased calcium losses in the urine, and slowdown in the formation of new bone.
Amenorrhea, the condition in which menstrual periods stop or fail to initiate in women of childbearing age, results from reduced circulating estrogen levels that, in turn, have a negative effect on calcium balance. Amenorrheic women with anorexia nervosa have decreased calcium absorption and higher urinary calcium excretion rates, as well as a lower rate of bone formation than healthy women 99. The “female athlete triad” refers to the combination of disordered eating, amenorrhea, and osteoporosis. Exercise-induced amenorrhea generally results in decreased bone mass 100, 101. In female athletes and active women in the military, low bone-mineral density, menstrual irregularities, certain dietary patterns, and a history of prior stress fractures are associated with an increased risk of future stress fractures 102. Such women should be advised to consume adequate amounts of calcium and vitamin D. Supplements of these nutrients have been shown to reduce the risk of stress fractures in female Navy recruits during basic training 103.
Individuals who avoid dairy products
People with lactose intolerance, those with an allergy to milk, and those who avoid eating dairy products (including vegans) have a higher risk of inadequate calcium intakes because dairy products are rich sources of calcium 21, 104. Options for increasing calcium intakes in individuals with lactose intolerance include consuming lactose-free or reduced-lactose dairy products, which contain the same amounts of calcium as regular dairy products 21, 54. Those who avoid dairy products because of allergies or for other reasons can obtain calcium from non-dairy sources, such as some vegetables (e.g., kale, broccoli, and Chinese cabbage [bok choi]), canned fish with bones, or fortified foods (e.g., fruit juices, breakfast cereals, and tofu) 21. However, these individuals typically need to eat foods fortified with calcium or take supplements to obtain recommended amounts 105.
People with lactose intolerance
People with lactose intolerance cannot digest this natural sugar found in milk and experience symptoms like bloating, gas, and diarrhea when they drink more than small amounts at a time. They usually can eat other calcium-rich dairy products that are low in lactose, such as yogurt and many cheeses, and drink lactose-reduced or lactose-free milk.
Lactose intolerance refers to symptoms (such as bloating, flatulence, and diarrhea) that occur when one consumes more lactose, the naturally occurring sugar in milk, than the enzyme lactase produced by the small intestine can hydrolyze into its component monosaccharides, glucose and galactose 106. The symptoms vary, depending on the amount of lactose consumed, history of consumption of lactose-containing foods, and type of meal. Although the prevalence of lactose intolerance is difficult to discern 107, some reports suggest that approximately 25% of U.S. adults have a limited ability to digest lactose, including 85% of Asians, 50% of African Americans, and 10% of Caucasians 108, 109, 110.
Lactose-intolerant individuals are at risk of calcium inadequacy if they avoid dairy products. Research suggests that most people with lactose intolerance can consume up to 12 grams of lactose, such as that present in 8 ounces of milk, with minimal or no symptoms, especially if consumed with other foods; larger amounts can frequently be consumed if spread over the day and eaten with other foods. Other options to reduce symptoms include eating low-lactose dairy products including aged cheeses (such as Cheddar and Swiss), yogurt, or lactose-reduced or lactose-free milk. Some studies have examined whether it is possible to induce adaptation by consuming incremental lactose loads over a period of time 111, 112, but the evidence in support of this strategy is inconsistent 107.
Cow’s milk allergy is less common than lactose intolerance, affecting 0.6% to 0.9% of the population 113. People with this condition are unable to consume any products containing cow’s milk proteins and are therefore at higher risk of obtaining insufficient calcium.
To ensure adequate calcium intakes, lactose-intolerant individuals and those with cow’s milk allergy can choose nondairy food sources of the nutrient (such as kale, bok choy, Chinese cabbage, broccoli, collards and fortified foods) or take a calcium supplement.
Vegans and ovo-vegetarians
Vegans (vegetarians who eat no animal products) and ovo-vegetarians (vegetarians who eat eggs but no dairy products), because they avoid the dairy products that are a major source of calcium in other people’s diets.
Vegetarians might absorb less calcium than omnivores because they consume more plant products containing oxalic and phytic acids. Lacto-ovo vegetarians (who consume eggs and dairy) and nonvegetarians have similar calcium intakes 114, 115. However, vegans, who eat no animal products and ovo-vegetarians (who eat eggs but no dairy products), might not obtain sufficient calcium because of their avoidance of dairy foods 116, 117. In the Oxford cohort of the European Prospective Investigation into Cancer and Nutrition, bone fracture risk was similar in meat eaters, fish eaters and vegetarians, but higher in vegans, likely due to their lower mean calcium intake 118. It is difficult to assess the impact of vegetarian diets on calcium status because of the wide variety of eating practices and thus should be considered on a case by case basis.
Calcium deficiency prevention
Men and women between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn 50 and men turn 70.
You can prevent calcium deficiency by eating a variety of foods. Good sources of calcium include the following 39:
- Milk, yogurt, and cheese are the main food sources of calcium for most people in the United States.
- Canned sardines and salmon with bones contain calcium.
- Dark green leafy vegetables, such as kale, broccoli, and Chinese cabbage (bok choi) also contain calcium.
- Calcium is added to some beverages, including many fruit juices and milk substitutes such as soy and almond beverages, as well as some brands of tofu and ready-to-eat cereals. To find out whether these foods have calcium added, check the product labels.
- Most grains (such as breads, pastas, and unfortified cereals) do not have high amounts of calcium. However, because people eat them often, what they contribute adds up.
If you find it difficult to get enough calcium from your diet, consider taking calcium supplements. However, too much calcium has been linked to kidney stones. Although yet unclear, some experts suggest that too much calcium, especially in supplements, can increase the risk of heart disease.
The Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine recommends that total calcium intake, from supplements and diet combined, should be no more than 2,000 milligrams daily for people older than 50 21.
However, many people in the United States get less than recommended amounts of calcium from food and supplements, especially 39:
- Children and teens aged 4 to 18 years
- People who are Black or Asian
- Adults aged 50 years and older living in poverty
Calcium supplements
Calcium is found in many multivitamin-mineral supplements, in calcium supplements, and in supplements that contain calcium and other nutrients such as vitamin D. Check the Supplement Facts label to determine the amount of calcium in the supplement.
The two main forms of calcium in dietary supplements are calcium carbonate and calcium citrate. Calcium carbonate is absorbed best when taken with food. Calcium citrate is well absorbed on an empty stomach or a full stomach. People with low levels of stomach acid—a condition most common in older people—absorb calcium citrate more easily than calcium carbonate.
Other forms of calcium in supplements and fortified foods include calcium sulfate, calcium ascorbate, calcium microcrystalline hydroxyapatite, calcium gluconate, calcium lactate, and calcium phosphate.
Calcium is absorbed best when you take 500 mg or less at one time. If you take 1,000 mg/day of calcium from supplements, for example, it is better to take a smaller dose twice a day than to take it all at once.
Calcium supplements might cause gas, bloating, and constipation in some people. If you have any of these symptoms, try spreading out the calcium dose throughout the day, taking the supplement with meals, or switching the form of calcium you take.
Vitamin D
Vitamin D improves your body’s ability to absorb calcium and improves bone health in other ways. The amount of vitamin D you need each day depends on your age. Average daily recommended amounts from the Food and Nutrition Board (a national group of experts) for different ages are listed below in International Units (IU). People can get some of their vitamin D from sunlight, but this might not be a good source if you live in a high latitude, if you’re housebound, or if you regularly use sunscreen or avoid the sun because of the risk of skin cancer.
Dietary sources of vitamin D include cod liver oil, trout and salmon. Many types of milk and cereal have been fortified with vitamin D.
Most people need at least 600 international units (IU) of vitamin D a day. That recommendation increases to 800 IU a day after age 70.
People without other sources of vitamin D and especially with limited sun exposure might need a supplement. Most multivitamin products contain between 600 and 800 IU of vitamin D. Up to 4,000 IU of vitamin D a day is safe for most people.
Table 3. Recommended Dietary Allowances (RDAs) for Vitamin D
| Life Stage | Recommended Amount |
|---|---|
| Birth to 12 months | 400 IU (10 mcg) |
| Children 1–13 years | 600 IU (15 mcg) |
| Teens 14–18 years | 600 IU (15 mcg) |
| Adults 19–70 years | 600 IU (15 mcg) |
| Adults 71 years and older | 800 IU (20 mcg) |
| Pregnant and breastfeeding women | 600 IU (15 mcg) |
Footnote: The amount of vitamin D contained in supplements is sometimes expressed in international units (IU) where 40 IU is equal to one microgram (1 mcg) of vitamin D.
[Source 71 ]Exercise
Exercise can help you build strong bones and slow bone loss. Exercise will benefit your bones no matter when you start, but you’ll gain the most benefits if you start exercising regularly when you’re young and continue to exercise throughout your life.
Combine strength training exercises with weight-bearing and balance exercises. Strength training helps strengthen muscles and bones in your arms and upper spine. Weight-bearing exercises — such as walking, jogging, running, stair climbing, skipping rope, skiing and impact-producing sports — affect mainly the bones in your legs, hips and lower spine. Balance exercises such as tai chi can reduce your risk of falling especially as you get older.
Hypocalcemia signs and symptoms
Extracellular calcium concentrations are important for normal physiological functions, including those involving muscles, nerves, blood vessels and the release of hormones and enzymes. Hypocalcemia can present as an asymptomatic laboratory finding or as a severe, life-threatening condition 2. Initially, if your body doesn’t get enough calcium and vitamin D to support these important functions, it takes calcium from your bones. This is called losing bone mass (osteopenia). Losing bone mass makes the inside of your bones become weak and porous. This puts you at risk for the bone disease osteoporosis.
In the short term, most symptoms of calcium deficiency are subtle that you may not notice them at all. But if left unaddressed, chronic hypocalcemia can have detrimental effects on different body systems, including contributing to low bone mass (osteopenia) and risk for osteoporosis.
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture
- A bone that breaks much more easily than expected.
Your bones are in a constant state of renewal — new bone is made and old bone is broken down. When you’re young, your body makes new bone faster than it breaks down old bone and your bone mass increases. After the early 20s this process slows, and most people reach their peak bone mass by age 30. As people age, bone mass is lost faster than it’s created.
Distinguishing acute from chronic hypocalcemia and asymptomatic from severely symptomatic hypocalcemia is critical for determining appropriate therapy. In the setting of acute hypocalcemia, rapid treatment may be necessary. In contrast, chronic hypocalcemia may be well tolerated, but treatment is necessary to prevent long-term complications.
Symptoms of serious calcium deficiency almost always occur in people with serious health problems, patients who are hospitalized or in people who are undergoing certain medical treatments where serum calcium levels drop to dangerous levels.
Potential signs and symptoms of hypocalcemia may include 119, 2:
- Seizures – Can be the sole manifestation or a part of the whole myriad of clinical presentation.
- Tetany – Generally induced by a rapid decline in serum ionized calcium. Tetany is usually most dangerous and most commonly seen in the presence of respiratory alkalosis causing hypocalcemia.
- Paresthesias – can be perioral or otherwise
- Psychiatric manifestations – Can be associated with anxiety/depression/emotional lability
- Carpopedal spasm – Also referred to as Trousseau’s sign. It represents increased neuromuscular excitability which may be related to the gating function of calcium ion for ion channels at a cellular level (particularly in neurons). This manifests as a spasm of hand upon routine BP check.
- Chvostek’s sign – Another manifestation of heightened neuromuscular excitability. It is the spasm of facial muscles in response to tapping the facial nerve near the angle of the jaw. Chvostek sign is an involuntary twitching of the facial muscles elicited by a light tapping of the facial nerve just anterior to the exterior auditory meatus. It is present in ≤ 10% of healthy people and in most people with acute hypocalcemia but is often absent in chronic hypocalcemia.
- Trousseau sign is the precipitation of carpal spasm by reduction of the blood supply to the hand with a tourniquet or blood pressure cuff inflated to 20 mm Hg above systolic blood pressure applied to the forearm for 3 min. Trousseau sign also occurs in alkalosis, hypomagnesemia, hypokalemia, and hyperkalemia and in about 6% of people with no identifiable electrolyte disturbance.
- QTc prolongation – Can lead to Torsades de pointes although extremely rare, it can be fatal.
- Many other abnormalities may occur in patients with chronic hypocalcemia, such as dry and scaly skin, brittle nails, and coarse hair.
- Candida infections occasionally occur in hypocalcemia but most commonly occur in patients with idiopathic hypoparathyroidism.
- Cataracts occasionally occur with long-standing hypocalcemia and are not reversible by correction of serum calcium.
Neuromuscular irritability
- Chvostek’s sign
- Trousseau’s sign
- Paresthesias
- Tetany
- Seizures (focal, petit mal, grand mal)
- Muscle cramps
- Muscle weakness
- Laryngospasm
- Bronchospasm
Neurological signs and symptoms
- Extrapyramidal signs due to calcification of basal ganglia
- Calcification of cerebral cortex or cerebellum
- Personality disturbances
- Irritability
- Impaired intellectual ability
- Nonspecific EEG changes
- Increased intracranial pressure
- Parkinsonism
- Choreoathetosis
- Dystonic spasms
Mental status
- Confusion
- Disorientation
- Psychosis
- Fatigue
- Anxiety
- Poor memory
- Reduced concentration
Ectodermal changes
- Dry skin
- Coarse hair
- Brittle nails
- Alopecia
- Enamel hypoplasia
- Shortened premolar roots
- Thickened lamina dura
- Delayed tooth eruption
- Increased dental caries
- Atopic eczema
- Exfoliative dermatitis
- Psoriasis
- Impetigo herpetiformis
Smooth muscle involvement
- Dysphagia
- Abdominal pain
- Biliary colic
- Dyspnea
- Wheezing
Ophthalmologic manifestations
- Subcapsular cataracts
- Papilledema
Cardiac
- Prolonged QT interval on EKG
- Congestive heart failure
- Cardiomyopathy
The hallmark of acute hypocalcemia is neuromuscular irritability. Patients often complain of numbness and tingling in their fingertips, toes, and the perioral region. Paresthesias of the extremities may occur, along with fatigue and anxiety. Muscle cramps can be very painful and progress to carpal spasm or tetany. In extreme cases of hypocalcemia, bronchospasm and laryngospasm with stridor may occur. Muscle symptoms can be so severe as to present with a polymyositis-like picture with elevated muscle isoenzymes. These symptoms are corrected by calcium replacement. Clinically, neuromuscular irritability can be demonstrated by eliciting Chvostek’s or Trousseau’s signs. Chvostek’s sign is elicited by tapping the skin over the facial nerve anterior to the external auditory meatus. Ipsilateral contraction of the facial muscles occurs in individuals with hypocalcemia. Chvostek’s sign is also present in 10% of normal individuals. Trousseau’s sign is elicited by inflation of a blood pressure cuff to 20 mm Hg above the patient’s systolic blood pressure for 3-5 minutes. Carpal spasm presents as flexion of the wrist and of the metacarpal phalangeal joints, extension of the interphalangeal joints, and abduction of the thumb. It can be very painful.
Acute hypocalcemia may have cardiac manifestations. Prolongation of the QT-interval due to lengthening of the ST-segment on electrocardiogram is fairly common in hypocalcemic patients. T-waves are abnormal in approximately 50% of patients 120. A pattern of acute anteroseptal injury on EKG without infarction has been associated with hypocalcemia and other electrolyte abnormalities 121. Hypomagnesemia in concert with hypocalcemia may magnify the EKG abnormalities. Rarely, congestive heart failure may occur 122. Reversible cardiomyopathy due to hypocalcemia has been reported 123. In patients with mild, asymptomatic hypocalcemia, calcium replacement can result in improved cardiac output, and exercise tolerance 124.
Chronic hypocalcemia may have an entirely different presentation 125. Patients with idiopathic hypoparathyroidism or pseudohypoparathyroidism may develop neurological complications, including calcifications of the basal ganglia and other areas of the brain 126, and extrapyramidal symptoms. Grand mal, petit mal, or focal seizures have been described. Increased intracranial pressure and papilledema may be present. If the patient has pre-existing subclinical epilepsy, hypocalcemia may lower the excitation threshold for seizures 127. Electroencephalographic changes may be acute and nonspecific or present with distinct changes in the electroencephalogram (EEG). EEG changes may be present with or without symptoms of hypocalcemia. The relationship between calcification of basal ganglia 126, cerebral cortex, or cerebellum with pre-existing epileptic or convulsive disorders is not well understood.
Epidermal changes are frequently found in patients with chronic hypocalcemia. These include dry skin, coarse hair, and brittle nails. If hypocalcemia has occurred prior to the age of 5, dental abnormalities may be present. Dental abnormalities include enamel hypoplasia, defects in dentin, shortened premolar roots, thickened lamina dura, delayed tooth eruption, and an increase in the number of dental caries. Alopecia has been noted following surgically-induced hypoparathyroidism and is also associated with autoimmune hypoparathyroidism. Other skin lesions reported in patients with hypoparathyroidism include atopic eczema, exfoliative dermatitis, impetigo herpetiformis, and psoriasis. Restoration of normocalcemia is reported to improve these skin disorders.
Changes in smooth muscle function with low serum levels of calcium may cause irritability of the autonomic ganglia and can result in dysphagia, abdominal pain, biliary colic, wheezing, and dyspnea. Subscapular cataracts occur in chronic, longstanding hypocalcemia 128 and with treatment, especially when the calcium x phosphate product is chronically elevated. Paravertebral ligamentous ossification has been noted in 50% of cases with hypoparathyroidism, and antalgic gait may be noted. In some cases of chronic hypoparathyroidism, psychoses, organic brain syndrome, and subnormal intelligence have been noted. Treatment of the hypocalcemia may improve mental functioning and personality, but amelioration of psychiatric symptoms is inconsistent. Delayed development, subnormal IQ, and poor cognitive function could also be a component of a syndrome that includes hypoparathyroidism as one of its features 129. This is critically important to consider in young patients being evaluated for the condition. In the elderly population, disorientation or confusion may be manifestations of hypocalcemia.
Figure 4. Chvostek’s sign
Trousseau’s sign
Trousseau’s sign is a carpopedal spasm induced by ischemia through inflation of a sphygmomanometer cuff to a suprasystolic blood pressure. Trousseau’s sign emerged at 25 seconds after the start of cuff inflation, with a maximal spasm at 60 seconds. Trousseau sign reported sensitivity and specificity for hypocalcemia are 94% and 99%, respectively 130.
Test for the Trousseau sign by placing a blood pressure cuff on the patient’s arm and inflating to 20 mm Hg above systolic blood pressure for 3-5 minutes 131. This increases the irritability of the nerves, and a flexion of the wrist and metacarpal phalangeal joints can be observed with extension of the interphalangeal joints and adduction of the thumb (carpal spasm). The Trousseau sign is more specific than the Chvostek sign but has incomplete sensitivity.
Neurologic manifestations
Muscle cramps involving the back and legs are common.
Insidious hypocalcemia may cause mild, diffuse encephalopathy and should be suspected in patients with unexplained dementia, depression, or psychosis.
Papilledema occasionally occurs.
Severe hypocalcemia with serum calcium < 7 mg/dL (< 1.75 mmol/L) may cause hyperreflexia, tetany, laryngospasm, or generalized seizures.
Tetany characteristically results from severe hypocalcemia but can result from reduction in the ionized fraction of serum calcium without marked hypocalcemia, as occurs in severe alkalosis. Tetany is characterized by the following:
- Sensory symptoms consisting of paresthesias of the lips, tongue, fingers, and feet
- Carpopedal spasm, which may be prolonged and painful
- Generalized muscle aching
- Spasm of facial musculature
Tetany may be overt with spontaneous symptoms or latent and requiring provocative tests to elicit. Latent tetany generally occurs at less severely decreased serum calcium concentrations: 7 to 8 mg/dL (1.75 to 2.20 mmol/L).
Fatigue
Fatigue reduces your energy, your ability to do things and your ability to focus. Ongoing fatigue affects quality of life and state of mind. In the case of hypocalcemia, fatigue is the result of your cells being undernourished.
Poor oral health
If your body is leeching calcium from your bones to stay functional, it’s going to make your teeth more susceptible to decay and loosening — and possibly even periodontal disease.
Muscle pain and spasms
Calcium doesn’t just make our bones strong: It also ensures our muscles function properly. Specifically, it helps our muscles contract and relax. Put differently, hypocalcemia will, quite literally, make you weaker. You’ll also experience more aches, pains, stiffness and spasms.
Cognitive issues
If your cells are being deprived of calcium, you can encounter a range of cognitive symptoms, from brain fog to dizziness and confusion. There’s even preliminary evidence to suggest that calcium intake affects our mental health.
Numbness and tingling in your fingers
Calcium plays a vital role in many different parts of your central nervous system; if you’re deficient, you may see those nerves impacted, particularly in your extremities (hands, fingers, feet and toes).
Seizures
Nutritional deficiencies can sometimes trigger seizures.
Abnormal heart rhythm
Calcium is crucial to muscle function and your heart is a muscle. There is a well-established connection between calcium dysregulation and ventricular arrhythmias, which can be serious and potentially even deadly.
Regardless of calcium levels, you should go to the emergency room (ER) immediately if you’re experiencing chest pain (angina) along with other symptoms like shortness of breath, lightheadedness or fainting.
Hypocalcemia diagnosis
Distinguishing acute from chronic hypocalcemia and asymptomatic from severely symptomatic hypocalcemia is critical for determining appropriate therapy. In the setting of acute hypocalcemia, rapid treatment may be necessary. In contrast, chronic hypocalcemia may be well tolerated, but treatment is necessary to prevent long-term complications. Figure 5 shows an algorithm for investigating hypocalcemia.
Work up of hypocalcemia can be thought of in following parts:
- Confirming the hypocalcemia: First part of evaluation should focus on confirming the hypocalcemia and requires checking a serum albumin level to correct the total calcium, or measuring directly the ionized calcium level (where available). An EKG should also be obtained for all suspected cases of hypocalcemia to look for QTc prolongation which if present is a risk factor for Torsades de pointes. Sometimes further testing, including measurement of magnesium, PTH, phosphate, alkaline phosphatase, and vitamin D concentrations in blood and cAMP and phosphate concentrations in urine
- Finding the cause of hypocalcemia: This part can be driven by the clinical picture obtained during previous steps. Usually entails checking electrolytes such as serum magnesium and phosphorus levels and at least a serum PTH level. If suspicion for vitamin D deficiency is high based on history then vitamin D2 level should be measured as vitamin D3 can be affected by PTH levels. Other biomarkers may be obtained as indicated by history and physical eg. serum lipase in suspected pancreatitis.
In order to diagnose hypocalcemia, initial laboratory testing involves measuring serum calcium, phosphate, magnesium, intact parathyroid hormone (PTH), 25-hydroxyvitamin D, and 1,25-dihydroxyvitamin D levels. Albumin, liver function studies, and coagulation parameters should be aslo obtained to assess liver dysfunction and hypoalbuminemia. Blood urea nitrogen (BUN) and serum creatinine should be measured, as elevated levels may indicate kidney dysfunction. An electrocardiogram (ECG) is also indicated. Imaging studies may include plain radiography or computed tomography (CT) scans. On radiographs, disorders associated with rickets or osteomalacia present with the pathognomonic Looser zones, which are better observed in the pubic ramus, upper femoral bone, and ribs. Radiography will also disclose osteoblastic metastases from certain tumors (eg, breast, prostate, lung), which can cause hypocalcemia. CT scans of the head may show basal ganglia calcification and extrapyramidal neurologic symptoms (in idiopathic hypoparathyroidism) 132.
Total calcium levels can be measured in serum or plasma; serum levels are typically 8.8 to 10.4 mg/dL (2. 2 to 2.6 mmol/L) in healthy adults 53, 21. However, serum calcium levels do not reflect nutritional status because of their tight homeostatic control 49. Furthermore, serum calcium concentration must be interpreted in relation to serum albumin. Serum calcium exists in an ionized form (∼50%) or is bound to albumin or other ions. Only ionized calcium or free calcium is biologically important. Various factors alter the ratio of ionized calcium to bound calcium, but the most important factor is the albumin concentration. Many medical conditions cause a decrease in serum albumin. Serum calcium concentrations are therefore “corrected” to a reference albumin concentration of 40 g/L, and for every 1 g/L of albumin above or below this value, the calcium is adjusted by decreasing or increasing by 0.08 mg/dL (0.02 mmol/L) 133. For example, a calcium concentration of 8.22 mg/dL (2.05 mmol/L) with an albumin concentration of 35 g/L would be corrected to 8.62 mg/dL (2.15 mmol/L) [40 g/L – 35 g/L = 5 X 0.08 mg/dL = 0.4 mg/dL], which would correct the hypocalcemic value to normal. This estimation is often used, but it can be unreliable in some situations, such as critical illness 76. If it is doubtful whether total calcium reflects ionized calcium or free calcium, the ionized value can be checked directly. Other situations in which the assessment of serum calcium may be inappropriately low include recent use of certain gadolinium contrast agents and contamination of blood samples by EDTA 6.
Levels of ionized or free calcium, the biologically active form, in serum are also used to measure calcium status and the normal range of ionized calcium in healthy adults is 4.6 to 5.3 mg/dL (1.15 to 1.33 mmol/L) 53, 21.
Hypocalcemia is defined as a total serum calcium concentration < 8.8 mg/dL (< 2.20 mmol/L) in the presence of normal plasma protein concentrations or as a serum ionized calcium concentration < 4.7 mg/dL (< 1.17 mmol/L) 134.
Hypocalcemic patients should undergo measurement of renal function (eg, BUN, creatinine), serum phosphate, magnesium, and alkaline phosphatase.
When no cause (eg, alkalosis, renal failure, drugs, or massive blood transfusion) is obvious, further testing is needed.
Additional testing begins with serum concentrations of magnesium, phosphate, parathyroid hormone, alkaline phosphatase, and occasionally vitamin D levels, both 25-hydroxyvitamin D, and 1,25-dihydroxyvitamin D. Urinary phosphate and cAMP concentrations are measured when pseudohypoparathyroidism is suspected.
PTH concentration should be measured as an assay of the intact molecule. Because hypocalcemia is the major stimulus for PTH secretion, PTH normally should be elevated in response to hypocalcemia. Thus,
- Low or even low-normal PTH concentrations are inappropriate and suggest hypoparathyroidism.
- An undetectable PTH concentration suggests idiopathic hypoparathyroidism.
- A high PTH concentration suggests pseudohypoparathyroidism or an abnormality of vitamin D metabolism.
Hypoparathyroidism is further characterized by high serum phosphate and normal alkaline phosphatase.
In true hypocalcemia, parathyroid hormone (PTH) concentrations should be high if the parathyroids are responding appropriately to the reduced negative feedback of calcium or low if the parathyroid glands are the cause of the problem. “Normal” concentrations of parathyroid hormone (PTH) in this context are inappropriate and thus abnormal. A high concentration of parathyroid hormone (PTH) in the presence of normal kidney function suggests vitamin D deficiency or calcium malabsorption. A low parathyroid hormone (PTH) concentration usually indicates hypoparathyroidism. Parathyroid hormone (PTH) concentrations can be normal in hypoparathyroidism, but they are usually within the lower part of the reference range. Parathyroid hormone (PTH) concentrations can also be inappropriately normal in hypomagnesemia or when the extracellular calcium sensing receptor has increased sensitivity (an autosomal dominant genetic disorder) 135.
A raised serum alkaline phosphatase (ALP) suggests osteomalacia as a result of vitamin D deficiency. If the diagnosis of osteomalacia is suspected, a bone biopsy can determine the final diagnosis. The possibility of metastatic cancer, with sclerotic metastases causing rapid absorption of calcium into the skeleton, should also be excluded. Parathyroid hormone (PTH) stimulates renal phosphate clearance, so serum phosphate should be low in non-parathyroid disease but high in parathyroid hormone deficiency. Measuring phosphate has limited value because it varies diurnally and is affected by food intake. Kidney function should be measured because the kidney is central to several aspects of calcium homoeostasis.
Other tests may be needed in some situations. Serum 25-hydroxyvitamin D concentrations are useful in confirming vitamin D deficiency when it presents atypically, and it should be assessed in patients with possible pseudohypoparathyroidism. Serum magnesium is important for the synthesis and release of parathyroid hormone 136. In hypomagnesaemia, the release of parathyroid hormone is inhibited, leading to (potentially severe) hypocalcaemia. The prevalence of hypomagnesaemia in a large primary care cohort was 2% 137, but in intensive care patients it can be up to 65% 138. Poor nutrition associated with chronic alcohol use, prolonged diarrhea, and treatment with diuretics and certain chemotherapeutics (such as cisplatin) causes hypomagnesemia. Recognition of hypomagnesemia is important because in this setting it is difficult to reverse hypocalcemia without magnesium repletion.
In type I pseudohypoparathyroidism, despite the presence of a high concentration of circulating PTH, urinary cAMP and urinary phosphate are absent. Provocative testing by injection of parathyroid extract or recombinant human PTH fails to raise serum or urinary cAMP. Patients with type Ia pseudohypoparathyroidism frequently also have skeletal abnormalities, including short stature and shortened 1st, 4th, and 5th metacarpals. Patients with type Ib disease have renal manifestations without skeletal abnormalities.
In vitamin D deficiency, osteomalacia or rickets may be present, usually with typical skeletal abnormalities on x-ray.
Severe hypocalcemia can affect the ECG. It typically shows prolongation of the QTc and ST intervals. Changes in repolarization, such as T-wave peaking or inversion, also occur. ECG may show arrhythmia or heart block occasionally in patients with severe hypocalcemia. However, evaluation of isolated hypocalcemia does not mandate ECG testing.
Imaging studies may include plain radiography or computed tomography (CT) scans. On radiographs, disorders associated with rickets or osteomalacia present with the pathognomonic Looser zones, which are better observed in the pubic ramus, upper femoral bone, and ribs. Radiography will also disclose osteoblastic metastases from certain tumors (eg, breast, prostate, lung), which can cause hypocalcemia. CT scans of the head may show basal ganglia calcification and extrapyramidal neurologic symptoms (in idiopathic hypoparathyroidism).
In order to diagnose osteopenia, your doctor will do a bone density test to assess cumulative calcium status over the lifetime because the skeleton stores almost all calcium in the body 54. Bone density measures bone mass and bone strength. One type of bone density test is a dual-energy X-ray absorptiometry (DEXA or DXA). It measures bone density in your hips, spine, and wrist. The result can tell if you have osteopenia or osteoporosis, or if your bones are normal. The lower your score, the higher your risk of bone breakage. A T-score between -1 and -2.5 is labeled osteopenia. A T-score lower than -2.5 is labeled osteoporosis.
According to the U.S. Preventive Services Task Force, all women over 65 years old should have a bone density test 139. Women under 65 years old should be tested as well if they’re at high risk 139.
Figure 5. Calcium deficiency diagnostic algorithm
[Source 6 ]Hypocalcemia test
Critical initial laboratory testing involves measuring serum phosphate, magnesium, intact parathyroid hormone (PTH), 25-hydroxyvitamin D, and 1,25-dihydroxyvitamin D levels. Further evaluation is directed by the clinical and laboratory profiles that emerge.
Estimation of ionized calcium concentration
Ionized calcium concentration can be estimated from routine laboratory tests, usually with reasonable accuracy.
In hypoalbuminemia, measured serum calcium is often low, mainly reflecting a low concentration of protein-bound calcium, while ionized calcium can be normal. Measured total serum calcium decreases or increases by about 0.8 mg/dL (0.2 mmol/L) for every 1 g/dL decrease or increase in albumin. Thus, an albumin concentration of 2.0 g/dL (normal, 4.0 g/dL) should itself reduce measured serum calcium by 1.6 mg/dL (0.4 mmol/L).
Similarly, increases in serum proteins, as occur in multiple myeloma, can raise total serum calcium. Acidosis increases ionized calcium by decreasing protein binding, whereas alkalosis decreases ionized calcium.
Parathyroid hormone (PTH)
The parathyroid hormone (PTH) level should be checked as early as possible. The parathyroid hormone (PTH) test is an antibody-mediated radioimmunoassay. Low-to-normal PTH levels occur in patients with hereditary or acquired hypoparathyroidism and in patients with severe hypomagnesemia.
Patients with ineffective PTH have elevated PTH levels. The PTH elevation is a result of hypocalcemia.
Vitamin D blood test
Doctors test for vitamin D levels because low levels are common in people with primary hyperparathyroidism.
In the blood, a form of vitamin D known as 25-hydroxyvitamin D [25(OH)D] or “calcidiol” is measured in either nanomoles per liter (nmol/L) or nanograms per milliliter (ng/mL). One nmol/L is equal to 0.4 ng/mL. So, for example, 50 nmol/L is the same as 20 ng/mL.
- Levels of 50 nmol/L (20 ng/mL) or above are adequate for most people for bone and overall health.
- Levels below 30 nmol/L (12 ng/mL) are too low and might weaken your bones and affect your health.
- Levels above 125 nmol/L (50 ng/mL) are too high and might cause health problems.
In patients with primary hyperparathyroidism, the low vitamin D level can further stimulate the parathyroid glands to make even more parathyroid hormone (PTH). Also, a very low vitamin D level may cause a secondary form of hyperparathyroidism, which resolves when vitamin D levels are returned to normal.
- A low 25-hydroxyvitamin D [25(OH)D] or “calcidiol” level suggests vitamin D deficiency from poor nutritional intake, lack of sunlight, or malabsorption.
- Low levels of 1,25-dihydroxyvitamin D [1,25(OH)2D] or “calcitriol” in association with high PTH suggest ineffective PTH from a lack of vitamin D, as observed in patients with chronic kidney failure, vitamin D–dependent rickets type 1 (VDDR-I), and pseudohypoparathyroidism 140.
Assessing vitamin D status by measuring serum 25-hydroxyvitamin D [25(OH)D] or “calcidiol” concentrations is complicated by the considerable variability of the available assays (the two most common ones involve antibodies or chromatography) used by laboratories that conduct the analyses 141, 142. As a result, a finding can be falsely low or falsely high, depending on the assay used and the laboratory. The international Vitamin D Standardization Program has developed procedures for standardizing the laboratory measurement of 25-hydroxyvitamin D [25(OH)D] or “calcidiol” to improve clinical and public health practice 143, 144, 145.
In contrast to 25-hydroxyvitamin D [25(OH)D], circulating 1,25-dihydroxyvitamin D [1,25(OH)2D] or “calcitriol” is generally not a good indicator of vitamin D status because it has a short half-life measured in hours, and serum levels are tightly regulated by parathyroid hormone, calcium, and phosphate 21. Levels of 1,25-dihydroxyvitamin D [1,25(OH)2D] do not typically decrease until vitamin D deficiency is severe 146.
Urinary cyclic adenosine monophosphate (cAMP) may help differentiate hypoparathyroidism from pseudohypoparathyroidism types 1 and 2. Urinary cAMP levels are generally elevated in hypoparathyroidism 140.
Electrocardiogram
Acute hypocalcemia causes prolongation of the QT interval, which may lead to ventricular dysrhythmias 147. It also causes decreased myocardial contractility, which can lead to heart failure, hypotension, and angina 147. Cardiomyopathy and ventricular tachycardia may be reversible with treatment.
Kidney imaging tests
Doctors may use one of the following imaging tests to look for kidney stones.
- Ultrasound. Ultrasound uses a device called a transducer that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician does the procedure. A radiologist reads the images, which can show kidney stones.
- Abdominal x-ray. An abdominal x-ray is a picture of the abdomen that uses low levels of radiation and is recorded on film or on a computer. During an abdominal x-ray, you lie on a table or stand up. A technician positions the x-ray machine close to your abdomen and asks you to hold your breath so the picture won’t be blurry. A radiologist reads the x-ray, which can show the location of kidney stones in the urinary tract. Not all stones are visible on an abdominal x-ray.
- Computed tomography (CT) scans. CT scans use a combination of x-rays and computer technology to create images of your urinary tract. CT scans sometimes use a contrast medium—a dye or other substance that makes structures inside your body easier to see. Contrast medium isn’t usually needed to see kidney stones. For the scan, you’ll lie on a table that slides into a tunnel-shaped machine that takes the x-rays. A radiologist reads the images, which can show the size and location of a kidney stone.
Bone mineral density test
Bone mineral density (BMD) at specific locations of your hip and spine is measured by dual-energy X-ray absorptiometry, also called a DXA or DEXA scan, which uses low-dose x-rays to measure bone density. During the DEXA test, you will lie on a padded table while a technician moves the scanner over your body. A bone expert or radiologist will read the scan.
The DEXA provides a T-score that is used for diagnostic purposes. Clinically, a T-score of -2.5 standard deviations (SD) or below gives a diagnosis of osteoporosis in postmenopausal women and men aged ≥50 years (Table 4).
Table 4. Bone mineral density DEXA test T-score cutoffs
| Normal bone mass | T-score equal to or above -1 standard deviation (SD) |
| Low bone mass (osteopenia) | T-score between -1 SD and -2.5 SD |
| Osteoporosis | T-score equal to or below -2.5 SD |
Risk of Fracture
The burden of osteoporosis lies primarily in the fractures that arise. Osteoporotic fractures are often precipitated by falls from standing height, although vertebral fractures can occur in the absence of a fall during daily, routine activities. About 70% of osteoporotic fractures affect women. Worldwide, 1 in 3 women and 1 in 5 men aged >50 years will suffer from a fracture.
The risk of osteoporotic fracture is influenced by bone mass, bone structure (microarchitecture, geometry), and propensity to fall (balance, mobility, muscular strength). The Fracture Risk Assessment Tool (https://frax.shef.ac.uk/FRAX/index.aspx) is an online tool that helps estimate your probability of fracture over the next 10 years, taking bone mineral density (BMD) measurement and additional risk factors into account (Table 5).
Table 5. 10-year Fracture Risk Probability
| Age (between 40 and 90 years) |
| Sex |
| Weight and height |
| Previous osteoporotic fracture |
| Parental history of hip fracture |
| Current tobacco smoking |
| Use of glucocorticoids (>3 months of doses equivalent to 5 mg/day of prednisolone) |
| Confirmed diagnosis of rheumatoid arthritis |
| Conditions associated with secondary osteoporosis (type 1 diabetes mellitus, osteogenesis imperfecta, untreated long-standing hyperparathyroidism, hypogonadism or premature menopause [<45 years], chronic malnutrition, or malabsorption and chronic liver disease) |
| Alcohol intake: ≥3 units (drinks)/day |
| Low femoral neck BMD |
Hypocalcemia treatment
The treatment of hypocalcemia depends on the cause, the severity, the presence of symptoms, and how rapidly the hypocalcemia developed 6. Management of Hypocalcemia can be divided into two broad categories 148:
- Symptomatic hypocalcemia: intravenous calcium is recommended for rapid repletion if there is any evidence of neuromuscular excitability. If the symptoms are mild such as paresthesias or psychiatric oral calcium can be attempted. Calcium gluconate is the preferred solution and can be given over 10-30 minutes depending on the severity of symptoms. Calcium chloride can be used if central venous access is available. Alkaline solution like bicarbonate and phosphorus containing solution need to be avoided through the same iv to avoid precipitation of calcium salts.
- Asymptomatic hypocalcemia: if corrected total serum calcium is below 7.5mg/dL, iv calcium should still be the preferred method. However, if corrected serum calcium is >7.5 mg/dL and patient is asymptomatic oral calcium can be used. Vitamin D supplementation is often recommended with calcium to promote absorption and because vitamin D deficiency is commonly encountered in most clinical scenarios leading to hypocalcemia. It is also important to address disease-specific problems and correct co-exiting electrolyte disturbances eg. hypomagnesemia.
The decision to treat is dependent on presenting symptoms, and the severity and rapidity with which hypocalcemia develops. All treatment requires close monitoring. If intravenous infusions are contemplated, hospitalization in an intensive care unit or specialized unit with access to cardiac monitoring and rapid ionized calcium determinations is ideal for optimal management and safety.
Most cases of hypocalcemia are clinically mild and require only supportive treatment and further laboratory evaluation. Oral calcium repletion may be indicated for outpatient treatment of mild cases. On occasion, severe hypocalcemia may result in seizures, tetany, refractory hypotension, or arrhythmias that require a more aggressive approach, including prompt management in hospital and treatment with intravenous infusions of calcium.
Asymptomatic patients with corrected serum calcium less than 1.9 mmol/L may develop serious complications and admission should be considered. Figure 6 shows an algorithm for managing acute hypocalcemia in adults that is based on clinical experience and expert recommendations 149. Calcium gluconate is the preferred form of intravenous calcium because calcium chloride is more likely to cause local irritation 6. One or two 10 ml ampoules of 10% calcium gluconate should be diluted in 50-100 ml of 5% dextrose and infused slowly over 10 minutes 6. Electrocardiographic (ECG) monitoring is recommended because arrhythmias can occur if correction is too rapid 6. Treatment can be repeated until symptoms have cleared. Often this offers only temporary relief, and continuous administration of a dilute solution of calcium may be needed to prevent recurrence of hypocalcemia. Ten 10 ml ampoules of 10% calcium gluconate in 1 litre of 5% dextrose or 0.9% saline may be given at an initial infusion rate of 50 ml/hour, with the aim of maintaining serum calcium at the lower end of the reference range 149. An infusion of 10 ml/kg of this solution over four to six hours will increase serum calcium by 0.3-0.5 mmol/l. Oral calcium supplements should be given concurrently, and—if parathyroid hormone is deficient or non-functional—calcitriol should be given (for example, 1 mcg/day).
Patients taking digoxin have increased cardiac sensitivity to fluctuations in serum calcium, so intravenous calcium administration should be more cautious in this setting, with careful electrocardiographic monitoring. Patients with hypocalcemia related to hypomagnesemia will need magnesium replacement 6.
Figure 6. Hypocalcemia treatment algorithm
Footnote: In an emergency setting parenteral calcium is likely to be needed. If medium or long term treatment is needed, vitamin D or one of its analogues should be given 136
[Source 6 ]Acute Hypocalcemia
Acute hypocalcemia can be life-threatening, as patients may present with tetany, seizures, cardiac arrhythmias, laryngeal spasm, or altered mental status. Intravenous calcium is given if serum calcium levels fall below 1.9 mmol/L, or ionized calcium levels are less than 1 mmol/L, or if patients are symptomatic 6, 5, 150. Calcium gluconate via a central venous catheter is the preferred intravenous calcium salt as calcium chloride often causes local irritation 6, 5, 151, 152, 153. Calcium gluconate contains 90 mg of elemental calcium per 10 mL ampule, and usually 1 to 2 ampules 10-mL ampoules of 10% calcium gluconate (180 mg of elemental calcium) diluted in 50 to 100 mL of 5% dextrose is infused over 5 to 10 minutes 6, 5. This can be repeated until the patient’s symptoms have cleared. To avoid precipitation of calcium salts, phosphate and bicarbonate should not be infused with the calcium 152. Patients should also receive oral calcium supplements and calcitriol (0.25 to 1 mcg/day) as needed 6.
With persistent hypocalcemia, administration of a calcium gluconate drip over longer periods of time may be necessary. The goal should be to raise the serum ionized calcium concentration into the low normal range (~1.0 mM), maintain it there, and control the patient’s symptoms. Drip rates of 0.5-2.0 mg/kg/hour are recommended. As soon as possible, oral calcium supplementation should be initiated and, if warranted, therapy with vitamin D or its analogues.
Local vein irritation can occur with solutions >200 mg/100 mL of elemental calcium. If local extravasation into soft tissues occurs, calcifications due to the precipitation of calcium phosphate crystals can occur 154. Calcium phosphate deposition can occur in any organ and is more likely to occur if the calcium-phosphate product exceeds 55. Calcium phosphate deposition in the lungs, kidney or other soft tissue may occur in patients receiving intravenous calcium especially in the presence of high serum phosphate levels.
Calcium chloride 10% solution delivers higher amounts of calcium and is advantageous when rapid correction is needed, but it should be administered via central venous access. Calcium infusion drips should be started at 0.5 mg/kg/hr and increased to 2 mg/kg/hr as needed, with an arterial line placed for frequent measurement of ionized calcium.
Rapid correction of hypocalcemia can contribute to cardiac arrhythmias so intravenous administration should be carefully monitored 6, 46. Cardiac monitoring during intravenous calcium supplementation is necessary, particularly in patients taking digoxin therapy 6, 151, 155.
Measure serum calcium every 4-6 hours to maintain serum calcium levels at 8-9 mg/dL. If low albumin is also present, ionized calcium should be monitored. Admit the patient for further evaluation and observation.
It is essential to measure serum magnesium in any patient who is hypocalcemic, as correction of hypomagnesemia must occur to overcome PTH resistance before serum calcium will return to normal.
Magnesium deficiency or alkalosis should be corrected if present 5, 151, 155. Acutely, magnesium supplementation therapy will not elevate serum PTH or calcium, as peripheral PTH resistance can last for several days 152.
Patients with cardiac arrhythmias or patients on digoxin therapy need continuous electrocardiographic (ECG) monitoring during calcium replacement because calcium potentiates digitalis toxicity. Identify and treat the cause of hypocalcemia and taper the infusion.
Start oral calcium and vitamin D treatment early. Patients with postparathyroidectomy hungry bone disease, especially those with osteitis fibrosa cystica, can present with a dramatic picture of hypocalcemia. Treatment with calcium and vitamin D for 1-2 days prior to parathyroid surgery may help prevent the development of severe hypocalcemia.
Tetany
For tetany, calcium gluconate 10 mL of 10% solution IV over 10 min is given. Response can be dramatic but may last for only a few hours. Repeated boluses or a continuous infusion with 20 to 30 mL of 10% calcium gluconate in 1 L of 5% dextrose in water over the next 12 to 24 h may be needed. Infusions of calcium are hazardous in patients receiving digoxin and should be given slowly and with continuous ECG monitoring after checking for (and correcting) hypokalemia.
When tetany is associated with hypomagnesemia, it may respond transiently to calcium or potassium administration but is permanently relieved only by repletion of magnesium, typically given as a 10% magnesium sulfate solution (1 g/10 mL) IV, followed by oral magnesium salts (eg, magnesium gluconate 500 to 1000 mg oral three times daily).
Chronic Hypocalcemia
In chronic hypocalcemia, patients can often tolerate remarkably severe hypocalcemia and remain asymptomatic. For patients who are asymptomatic or with mildly symptomatic hypocalcemia, calcium homeostasis can be restored with oral calcium and vitamin D or an activated vitamin D metabolite such as calcitriol 125.
Oral calcium carbonate is often the most commonly administered salt, although many different calcium salts exist. Oral doses calcium should be in the amount of 1 to 3 grams of elemental calcium in 3 to 4 divided doses with meals to ensure optimal absorption. Calcium carbonate contains 40% elemental calcium by weight and is relatively inexpensive. Lower amounts of elemental calcium are present in other types of calcium such as calcium lactate (13%), calcium citrate (21%) and calcium gluconate (9%), requiring a larger number of tablets. There are expensive forms of calcium supplements that have relatively few additional advantages. Liquid calcium supplements are available such as calcium glubionate that contains 230 mg of calcium per 10 mL or liquid forms of calcium carbonate. In patients with achlorhydria, a solution of 10% calcium chloride (1- to 30 ml) every 8 hours can also effectively raise calcium levels. Calcium phosphate salts should be avoided.
In patients without renal failure, vitamin D is given as a standard oral supplement (eg, cholecalciferol 800 IU once/day). Vitamin D therapy is not effective unless adequate dietary or supplemental calcium and phosphate are also supplied. For patients with renal failure, calcitriol or another 1,25(OH)2D analog is used because these drugs require no renal metabolic alteration. Patients with hypoparathyroidism have difficulty converting cholecalciferol to its active form and also usually require calcitriol, usually 0.5 to 2 mcg po once/day. Pseudohypoparathyroidism can occasionally be managed with oral calcium supplementation alone. When used, calcitriol requires 1 to 3 mcg/day.
Vitamin D analogs include dihydrotachysterol (usually given orally at 0.8 to 2.4 once/day for a few days, followed by 0.2 to 1.0 mg once/day) and calcidiol (eg, 4000 to 6000 IU po once/wk). Use of vitamin D analogs, particularly the longer-acting calcidiol, can be complicated by vitamin D toxicity, with severe symptomatic hypercalcemia. Serum calcium concentration should be monitored weekly at first and then at 1- to 3-mo intervals after calcium concentrations have stabilized. The maintenance dose of calcitriol or its analog, dihydrotachysterol, usually decreases with time.
The overall goal of therapy is to maintain serum calcium in the low normal range, especially in patients with hypoparathyroidism 156. Serum calcium should be tested every 3 to 6 months or when any changes in the medical regimen are made. One potential side effect of therapy in patients with hypoparathyroidism is hypercalciuria which can be complicated by nephrocalcinosis, nephrolithiasis, and or renal insufficiency. A 24-hour urine calcium along with creatinine determination should be done at least annually, once stable doses of supplements are established. The target for urinary calcium excretion is <4 mg/kg/24 hr. Serum levels of calcium are poor indicators of the presence of hypercalciuria and nephrocalcinosis 156. The patient should also regularly see an ophthalmologist to screen for cataracts. When treating hypocalcemia in the presence of hyperphosphatemia, special care must be taken (sometimes with the use of a phosphate binder) to avoid soft tissue calcium phosphate precipitation. Soft tissue calcification can occur in any tissue, but involvement of vital organs such as the lungs, kidney, heart, blood vessels, or brain can result in substantial morbidity or mortality 126.
For patients with hypoparathyroidism, vitamin D2 or D3 (ergocalciferol or cholecalciferol, respectively) or vitamin D metabolites [calcitriol or 1,25-(OH)2 vitamin D or 1 alpha-OH vitamin D (not available in the US)] are often required. Calcitriol, the active metabolite of vitamin D, is rapid-acting and physiologic and is often used for initial therapy. Where rapid dose adjustment is necessary, such as growing children, this may be the most convenient approach 157. Most patients require 0.25 mcg twice daily and may require up to 0.5 mcg 4 times a day of calcitriol. Among other options, ergocalciferol is a less expensive choice and has a long duration of action. The usual dose is 50,000 to 100,000 IU/day. When therapy needs to be administered acutely, calcitriol should be given for the first 3 weeks but then tapered off as the dose of ergocalciferol becomes effective. If calcitriol is the vitamin D metabolite administered, then the serum 25 (OH) vitamin D level should be checked periodically to assure that vitamin D sufficiency is maintained. Serum 25 (OH) vitamin D levels should be kept stable at >20 ng/mL.
Thiazide diuretics can increase renal calcium reabsorption in patients with hypoparathyroidism. This approach may be needed to achieve a urinary calcium of <4 mg/kg/day. Furosemide and other loop diuretics can depress serum calcium levels and should be avoided. Other factors that may precipitate hypocalcemia are glucocorticoids since they can antagonize the action of vitamin D and its analogues.
Administration or withdrawal of exogenous estrogen can also influence calcium and vitamin D replacement therapy. Estrogen increases calcium absorption at the level of the intestine and indirectly through stimulation of renal 1-alpha-hydroxylase activity. Dose adjustment may be required after changes in estrogen therapy due to alteration in calcium homeostasis. During the pre- and postpartum period in pregnant patients with hypoparathyroidism, doses of vitamin D often need frequent adjustments. This is due to placental production of 1,25-(OH)2 vitamin D in pregnancy, the increasing levels of PTH-rP from placental, maternal and fetal tissues later in pregnancy, and the high levels of PTH-rP in conjunction with the estrogen-deficient state of lactation 156.
How well current treatment strategies (calcium salts, vitamin D and its metabolites) maintain quality of life in patients with hypoparathyroidism has been assessed to a limited extent 158. In a cross-sectional, controlled study, 25 women with postsurgical hypoparathyroidism on stable calcium and vitamin D treatment were compared to 25 control subjects with a history of thyroid surgery. Quality of life, urinary calcium excretion and renal calcifications, serum creatinine, and the presence of cataracts by slit lamp examination were assessed. Serum calcium was in the therapeutic target range in 18 of 25 hypoparathyroid patients. Urinary calcium was elevated (>8 mmol/day) in 5 of 23 patients. Eleven of 25 hypoparathyroid patients had cataracts, and 2 of 25 had renal stones 158. Compared to the control group, those with hypoparathyroidism had higher global complaint scores with predominant increases in anxiety and phobic anxiety subscores and their physical equivalents using validated questionnaires. Thus, by both physical and psychologic assessments, there were several parameters that were reduced compared to control subjects.
The long-term complications of standard treatment of hypoparathyroidism were recently examined in a cohort of 120 patients (73% women, average age 52 years, 66% post-surgical) followed at a tertiary medical center 156. The time-weighted average for serum calcium (maintained between 7.5 and 9.5 mg/dL) occurred in 88% of patients. Patients were estimated to be in this range ~86% of the time. Just 53 of 120 patients had any 24-hour urine calcium level determined. Of those patients, 38% had at least one elevated measurement (>300 mg/24 hours). Among the 54 of 120 with renal imaging, intrarenal calcifications were detected in 31%. Of those with brain imaging (31/120 patients), 52% had basal ganglia calcifications. Analysis of renal function showed rates of chronic kidney disease (stage 3 or greater) of 2- to 17-fold higher than age-adjusted normal subjects 156. Overall, it was concluded that patients with hypoparathyroidism suffer excess morbidity, especially with regard to renal outcomes.
Underbjerg et al 159 examined clinical outcomes in a case-control study of 688 Danish patients with hypoparathyroidism compared to age- and gender-matched controls. Patients with postsurgical hypoparathyroidism demonstrated increased risk of renal complications and hospitalizations due to seizures, compared to controls 160. No increased cardiovascular complications or deaths were seen. Using the same cohort, Underbjerg et al 159 further reported greater risks of hospitalization for infections and of depression/bipolar affective disorder. Risks of cataracts, cancers, spinal stenosis, and fractures were not increased.
The same investigators assessed the epidemiologic features of nonsurgical hypoparathyroidism in Danish patients 161. Based on data from 180 patients (collected from 1977 to 2012), these investigators found a marked increased in renal insufficiency, as well as almost 2-fold increased risk of cardiovascular disease. Neuropsychiatric complications and risks of infections, seizures, cataracts and upper extremity fractures were also increased. This was thought to be due to the longer duration (lifetime) of the genetic condition responsible for the nonsurgical hypoparathyroidism in these patients.
Long-term management of chronic hypocalcemia
Oral calcium and vitamin D and its metabolites are essential in management, in addition to correction of hypomagnesemia 5. Calcium carbonate has 40% elemental calcium and calcium citrate has 28% elemental calcium and are easily absorbed; they are considered the calcium supplements of choice 162, 151, 163. Calcium supplement dosages are 1 to 2 g of elemental calcium 3 times daily 151. Elemental calcium supplements can be started at 500 to 1000 mg 3 times daily and titrated upward 151. Asymptomatic electrocardiography changes usually normalize with calcium and calcitriol supplementation 164.
Hypercalciuria is a complication of vitamin D therapy, particularly for patients with hypoparathyroidism, as the absence of PTH enhances urinary calcium losses 5. If hypocalcemia is due to malabsorption of vitamin D, physicians should treat the underlying cause (eg, implementing a gluten-free diet for patients with celiac disease) 165. Magnesium supplementation corrects hypomagnesemia-related hypocalcemia 46.
Vitamin D deficiency
Vitamin D deficiency requires correction with either ergocalciferol (vitamin D2) or cholecalciferol (vitamin D3). Ergocalciferol (vitamin D2) can be given in doses of 50,000 IU weekly or twice a week with assessment of levels 3 months later, titrating up until a normal 25(OH)D level is reached 6, 7, 166, 167, 168, 169. Alternatively, 300,000 IU of ergocalciferol (vitamin D2) can be administered intramuscularly, with the first 2 injections spaced 3 months apart, followed by regular injections every 6 months 6, 5.
Cholecalciferol (vitamin D3) is more potent than ergocalciferol (vitamin D2) 7, 162, 151, 170, 171. Administrating 100,000 IU of cholecalciferol (vitamin D3) once every 3 months is also effective in maintaining adequate 25(OH)D levels 172. Further study is needed to evaluate the use of tanning beds in correcting vitamin D inadequacy 7, 173.
Hypoparathyroidism
The treatment of hypoparathyroidism requires careful evaluation of the patient and consideration of the treatment options other than calcium supplementation. The primary goals of management with calcium and vitamin D supplementation include symptom control, maintaining serum calcium in the low-normal range (2.00 to 2.12 mmol/L), maintaining serum phosphorus within a normal range, and maintaining a calcium-phosphate product below 4.4 mmol/L (55 mg/dL) without developing hypercalciuria, nephrocalcinosis, or precipitation of calcium-phosphate salts in soft tissues 5, 174, 151, 155.
Vitamin D analogues, particularly calcitriol or alfacalcidol, can be used 5. Usual starting doses are 0.5 μg of calcitriol or 1 μg of alfacalcidol daily.1 Upward titration with increases in the doses every 4 to 7 days is advised until a low-normal serum calcium level is achieved 6 Calcitriol is preferable as it is relatively more potent, and has a rapid onset and offset of action attributable to its short half-life 5, 162, 151. Vitamin D treatment in patients with gain-of-function mutations of the calcium-sensing receptors results in further hypercalciuria, nephrocalcinosis, and renal impairment; thus, asymptomatic patients can simply be followed 5.
Thiazide diuretics decrease urinary calcium excretion by increasing distal renal tubular calcium reabsorption 5, 151, 175. Combining diuretics with a low-salt, low-phosphate diet and phosphate binders is beneficial 162.
Serum calcium, phosphorus, and creatinine should be measured weekly to monthly during initial dose adjustments, with quarterly or twice-yearly measurements once the therapy protocol has stabilized 162, 151, 6.
Unfortunately, patients with hypoparathyroidism have poor quality of life as measured on standard scales, which illustrates the limitations of therapy 176.
Replacement therapy with PTH is a viable option, as it corrects hypercalciuria and potentially reduces the risk of nephrocalcinosis, nephrolithiasis, and renal insufficiency. It can also reduce the wide fluctuation in serum calcium as well as the need to administer very large doses of calcium and vitamin D metabolites. Also, PTH 1-34 reduces urinary calcium excretion 177, 178, 179, 180, 181 possibly allowing reductions in the dose of calcium and vitamin D; PTH 1-84 has also been studied and might become a valuable addition to current treatment options 182. Hypoparathyroidism is the only remaining hormonal insufficiency that is currently not being treated with direct replacement of the deficient hormone 183. At this time, PTH supplementation has not been approved by Health Canada for the treatment of hypoparathyroidism 5.
Replacement with PTH for Hypoparathyroidism
In hypoparathyroidism, ideal treatment would theoretically be to replace the hormone itself in a physiologic manner. Several clinical studies have evaluated PTH and PTH as replacement therapy for hypoparathyroidism. In a trial of hypoparathyroid patients, once daily administration of PTH 184 normalized serum and urine calcium levels, but the action lasted only 12 hours 185. With twice-daily administration of PTH 186 compared to twice-daily calcitriol for 3 years in 27 patients, Winer et al 187 reported stabilization of serum calcium levels just below the lower limit of normal and a normalization of urinary calcium excretion (at the target level of 1.25-6.25 mmol/24 hours). Patients on calcitriol in this trial had urinary calcium levels above normal. Serum creatinine levels were stable over time in both groups of patients, and biochemical markers of bone turnover increased with PTH treatment compared to control levels at baseline. Bone mineral density (BMD) by dual energy x-ray absorptiometry (DXA) increased slightly but significantly at the lumbar spine and whole body in the calcitriol-treated patients and remained stable over 3 years in the PTH-treated group. These studies in adults 187 included patients with a variety of different etiologies for their hypoparathyroidism including patients with activating Casr mutations. Two other studies done in children 188 demonstrated stabilization of serum calcium levels with twice-daily treatment and normalization of urinary calcium excretion on both PTH and calcitriol. The most promising results for lowering urinary calcium into an acceptable range was seen during continuous PTH infusion. This approach achieved urinary calcium levels of ~4 mmol calcium/24 hours vs ~9.7 mmol/24 hours with twice-daily injections (normal range, 1.25-6.25 mmol/24 hours) in 8 adults with hypoparathyroidism 189. Serum calcium, phosphorus, and magnesium concentrations were comparable with the two modes of PTH delivery. These findings suggest that renal PTH receptors may require more continuous exposure to the hormone to reabsorb calcium adequately.
Three recent trials have tested the ability of PTH therapy to permit lowering of calcium and calcitriol supplements safely while maintaining serum calcium homeostasis in patients with chronic hypoparathyroidism 190. Rubin et al 191 gave PTH (100 mcg every other day) to hypoparathyroid patients and was able to lower both calcium and calcitriol supplements substantially (30-40%), while maintaining serum calcium within the target range and mildly lowering urinary calcium excretion. Since there was no placebo control group in this study, reports of improved quality of life parameters 190 must be interpreted cautiously.
Two other clinical trials, which included placebo treatment arms, further assessed the safety and efficacy of PTH therapy in hypoparathyroid subjects 192. In the first, using a randomized, placebo-controlled trial design, Sikjaer et al 193 added PTH (fixed dose of 100 mcg/day) or placebo injections to 62 patients on a chronic regimen of calcium and active vitamin D supplements for 24 weeks. As serum calcium levels rose, supplements were reduced. A substantial percentage of serum calcium measurements in patients receiving PTH were elevated during the trial (~20%), and ~96% of those episodes in the PTH-treated subjects versus the placebo-treated group. This outcome may have affected the quality of life during the study because no differences were noted between the PTH- and placebo-treated groups in those assessments.
In the second randomized, placebo-controlled trial, PTH or placebo was administered for 24 weeks to 134 patients with chronic hypoparathyroidism as calcium supplements and activated vitamin D (calcitriol or alphacalcidol) were actively down-titrated 192. Dose escalations of PTH were made starting at 50 mcg/day and then up to 75 and 100 mcg/day as calcium and activated vitamin D metabolites were dose-reduced. This study met its primary end-point, defined as a 50% or greater reduction in calcium supplements and in active vitamin D metabolites while maintaining a serum calcium concentration within the optimized range of 2.0-2.5 mM. Urinary calcium levels did not differ substantially between PTH(1-84)- compared to placebo-treated groups. Extension studies are in progress from two of these trials 192 to determine long-term safety and efficacy of PTH in this patient population. Based on these findings, the Food and Drug Administration of the US approved recombinant human PTH in 2015 for the treatment of hypoparathyroidism in patients not well controlled on conventional therapy with calcium supplements and activated vitamin D analogues. Future research is being directed toward designing ideal treatment regimens with PTH.
Persistent hypocalcemia
With milder degrees of hypocalcemia, treatment depends on the underlying cause 6. In vitamin D deficiency, treatment should be with vitamin D, either ergocalciferol (vitamin D2) or cholecalciferol (vitamin D3; these two forms of vitamin D can be considered identical in this setting) 6. Most available vitamin D preparations include calcium, and two tablets of calcium with vitamin D, each containing 400 IU vitamin D, are usually given daily 6. This dose of vitamin D is relatively low, and patients with symptomatic vitamin D deficiency or those who fail to respond can be treated in the short term with higher doses, such as 50 000 IU orally once a week for eight weeks or 300 000 IU intramuscularly every three months 167.
In patients with hypoparathyroidism, the above doses of vitamin D are ineffective because parathyroid hormone (PTH) is needed for conversion to 1,25-dihydroxyvitamin D 6. Thus calcitriol or alfacalcidol is needed. Typical starting doses are 0.5 mcg of calcitriol or 1 mcg of alfacalcidol each day, with doses being increased every four to seven days to achieve a serum calcium in the lower part of the reference range 6. Once a stable calcium concentration is achieved, concentrations should be monitored every three to six months. The main long term risk is the development of nephrocalcinosis as a result of hypercalciuria. Urinary calcium excretion should be monitored annually and if high the dose of vitamin D may need to be reduced.
In hypocalcemia caused by malabsorption, the underlying problem should be treated if possible. Patients with celiac disease should receive calcium and vitamin D orally and should comply with a gluten free diet 165.
Diet
Treatment for calcium deficiency starts with changes to your diet and lifestyle. Your doctor will suggest ways for you to get more calcium and vitamin D in your diet. Nonfat and low-fat dairy products, such as yogurt, cheese, and milk, are good sources of calcium. Other sources of calcium include dried beans, salmon, spinach, and broccoli. Some foods, such as orange juice, breads, and dry cereals, may be fortified with calcium, vitamin D, or both. Very few foods naturally contain vitamin D. Fatty fish (like trout, salmon, tuna, and mackerel) and fish liver oils are among the best natural sources of vitamin D. Fortified foods provide most of the vitamin D in the diets of people in the United States 194. Check the Nutrition Facts label for the amount of vitamin D in a food or beverage. Almost all of the U.S. milk supply is fortified with about 3 mcg (120 IU) vitamin D per cup. Many plant-based alternatives such as soy milk, almond milk, and oat milk are similarly fortified. But foods made from milk, like cheese and ice cream, are usually not fortified. If you don’t get enough calcium and vitamin D from the food you eat, your doctor may suggest taking a vitamin D or calcium supplement as well.
You also should stop smoking and limit alcohol. Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis. The exact role tobacco plays in osteoporosis isn’t clear, but it has been shown that tobacco use contributes to weak bones.
An increase in dietary calcium to greater than 1 g/day is an important part of the treatment of chronic hypocalcemia, particularly in cases of vitamin D deficiency. Women 50 years of age and younger and men 70 years of age and younger should get 1,000 mg of calcium per day. Women older than 50 years of age and men older than 70 years of age should get 1,200 mg of calcium per day. Women who are post-menopausal may need 1,500 mg of calcium per day. It is best to get your calcium from food.
In patients with hypocalcemia and chronic renal failure, the dietary intake of phosphate should be lowered to 400-800 mg/day to prevent hyperphosphatemia.
Patients with chronic hypocalcemia should be educated about the early symptoms of hypocalcemia, such as paresthesias and muscle weakness, so that they can obtain care before more severe symptoms develop.
Many countries around the world and some professional societies have somewhat different guidelines for vitamin D intakes 195. Serum concentration of 25-Hydroxyvitamin D [25(OH)D] is currently the main indicator of vitamin D status. It reflects vitamin D produced endogenously and that obtained from foods and supplements 21. The Endocrine Society states, for example, that to maintain serum 25-Hydroxyvitamin D [25(OH)D] levels above 75 nmol/L (30 ng/mL), adults might need at least 37.5 to 50 mcg (1,500–2,000 IU)/day of supplemental vitamin D, and children and adolescents might need at least 25 mcg (1,000 IU)/day 196. In contrast, the United Kingdom Scientific Advisory Committee on Nutrition recommends intakes of 10 mcg (400 IU)/day for its citizens aged 4 years and older 197.
And to prevent bone loss or osteopenia, your doctor will want you to increase your physical activity. Weight-bearing exercise can help strengthen your bones and increase your bone mass. It also can build muscle and improve your balance, which help prevent against broken bones. This is why it’s important to begin an active lifestyle at a young age. Examples of weight-bearing exercise include walking, jogging, and climbing steps. Try to do a mix of strength training and weight-bearing exercises.
If you’re at risk for falls, reduce your risk by getting rid of tripping hazards in your home. For example, remove rugs, avoid slippery surfaces, move electrical cords and wear low-heeled shoes with nonslip soles. You can install grab bars in certain places, such as your bathroom and shower. The grab bars can help you move around more easily and safely.
Your doctor may prescribe medicine(s) to help treat osteoporosis. Treatment recommendations are often based on an estimate of your risk of breaking a bone in the next 10 years using information such as the bone density test (see Tables 3 and 4 above). The Fracture Risk Assessment Tool (https://frax.shef.ac.uk/FRAX/index.aspx) is an online tool that helps estimate your probability of fracture over the next 10 years, taking bone mineral density (BMD) measurement and additional risk factors into account (https://frax.shef.ac.uk/FRAX/index.aspx).
If your risk of fracture is low, you might not need medication and instead might focus on modifying your risk factors for bone loss and falls.
Medicines to help treat osteoporosis
Biophosphonates
Biophosphonates helps reduce your risk of breaks and fractures. Biophosphonates also increases bone density. Biophosphonates comes in oral (pill) form or intravenous (IV or injection) form. Side effects can include nausea and stomach pain. You may have heartburn-like symptoms with irritation of your esophagus (the tube that connects your mouth and stomach). These are less likely to occur if the medicine is taken properly. Intravenous forms of bisphosphonates don’t cause stomach upset but can cause fever, headache and muscle aches.
A very rare complication of bisphosphonates is a break or crack in the middle of the thighbone. A second rare complication is delayed healing of the jawbone (osteonecrosis of the jaw). This can occur after an invasive dental procedure, such as removing a tooth.
Some people cannot take biophosphonates. This includes people who have kidney disease or low levels of calcium in their blood, and women who are pregnant or nursing.
For both men and women at increased risk of fracture, the most widely prescribed osteoporosis medications are bisphosphonates. Examples include:
- Alendronate (Binosto, Fosamax). Alendronate is used to help prevent and treat osteoporosis. Alendronate helps reduce your risk of fractures by decreasing the rate of bone loss. Alendronate is available in pill form. Alendronate most common side effect is an upset stomach.
- Ibandronate (Boniva). Ibandronate helps to slow bone loss and increase bone density. It is available as a pill or injection. You have 2 options for the pill. You can take it daily or monthly. For the injection, your doctor or nurse will give you a shot every 3 months. Side effects may include lower back or side pain, shortness of breath, tightness in your chest, and bloody or cloudy urine.
- Risedronate (Actonel, Atelvia). Risedronate is used to help prevent and treat osteoporosis. Risedronate helps reduce your risk of fractures by decreasing the rate of bone loss. Risedronate is available in pill form. Risedronate most common side effect is an upset stomach.
- Zoledronic acid (Reclast, Zometa). Zoledronic acid is given through IV once a year.
Denosumab
Denosumab (Prolia, Xgeva) is used when other drugs don’t work or if you can’t tolerate other treatment options. Denosumab increases your bone density. It can be used by both women and men. Denosumab is delivered via a shot under the skin every six months. Side effects can include lower calcium levels, skin rash, or pain in the arms and legs.
Compared with bisphosphonates, denosumab produces similar or better bone density results and reduces the chance of all types of fractures.
Similar to bisphosphonates, denosumab has the same rare complication of causing breaks or cracks in the middle of the thighbone and osteonecrosis of the jaw. If you take denosumab, you might need to continue to do so indefinitely. Recent research indicates there could be a high risk of spinal column fractures after stopping the drug.
Estrogen, especially when started soon after menopause, can help maintain bone density. However, estrogen therapy can increase the risk of breast cancer and blood clots, which can cause strokes. Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms also require treatment.
Raloxifene (Evista) mimics estrogen’s beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen. Taking Raloxifene can reduce the risk of some types of breast cancer. Hot flashes are a possible side effect. Raloxifene also may increase your risk of blood clots.
In men, osteoporosis might be linked with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help improve symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and thus are recommended alone or in addition to testosterone.
Bone-building medications
If you have severe osteoporosis or if the more common treatments for osteoporosis don’t work well enough, your doctor might suggest trying:
- Teriparatide (Bonsity, Forteo). Teriparatide is a synthetic form of parathyroid hormone (PTH) and stimulates new bone growth. Both women and men can use it. Teriparatide is given by daily injection under the skin for up to two years. You inject it in your thigh or stomach once a day. Common side effects are nausea, stomach pain, headache, muscle weakness, fatigue, and loss of appetite.
- Abaloparatide (Tymlos) is another drug similar to parathyroid hormone (PTH). This drug can be taken for only two years.
- Romosozumab (Evenity). This is the newest bone-building medication to treat osteoporosis. It is given as an injection every month at your doctor’s office and is limited to one year of treatment.
After you stop taking any of these bone-building medications, you generally will need to take another osteoporosis drug to maintain the new bone growth.
Calcitonin
Calcitonin is a hormone that helps slow down bone loss. It is available as an injection or nasal spray. Side effects of Calcitonin injection include diarrhea, stomach pain, nausea, and vomiting. Side effects of Calcitonin nose spray include headache and irritation of your nose lining.
Hypocalcemia prognosis
The overall prognosis of hypocalcemia is good as it can be easily corrected 22. In rare cases, patients with complete parathyroidectomy require very high doses of calcium and vitamin D supplements to maintain calcium in the normal range 22. Patients who have undergone gastric bypass surgery usually have malabsorption and may also require very high doses of calcium and vitamin D to correct hypocalcemia 22.
Bone fractures, particularly in the spine or hip, are the most serious complications of osteoporosis 198. Osteoporotic fractures often lead to a reduced quality of life and premature death 199. Hip fractures are the most serious of all osteoporotic fractures since 12-20% of women suffering from a hip fracture die during the following 2 years, and 50% of those surviving lose their independence and require long-term nursing care 199. The risk of death after hip fracture is higher in men than women. Fractures at other sites can also be debilitating.
In some cases, spinal fractures can occur even if you haven’t fallen. The bones that make up your spine (vertebrae) can weaken to the point of collapsing, which can result in back pain, lost height and a hunched forward posture. Multiple and/or severe vertebral fractures can lead to loss of height and abnormal bending of the upper and middle back (thoracic spine), reducing lung function and affecting digestion. Vertebral and non-hip, non-vertebral fractures are also associated with premature death.
- Hypocalcemia. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/electrolyte-disorders/hypocalcemia?query=Hypocalcemia[↩]
- Schafer AL, Shoback DM. Hypocalcemia: Diagnosis and Treatment. [Updated 2016 Jan 3]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://ncbi.nlm.nih.gov/sites/books/NBK279022[↩][↩][↩]
- Weaver CM, Heaney RP. Calcium. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ. Modern Nutrition in Health and Disease. 10th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2006:194-210.[↩]
- Goyal A, Singh S. Hypocalcemia. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430912[↩][↩]
- Murphy E, Williams GR. Hypocalcaemia. Medicine. 2009;37(9):465–468. doi: 10.1016/j.mpmed.2009.06.003[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia. BMJ. 2008 Jun 7;336(7656):1298-302. doi: 10.1136/bmj.39582.589433.BE. Erratum in: BMJ. 2008 Jun 28;336(7659): doi: 10.1136/bmj.a334[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81. doi: 10.1056/NEJMra070553[↩][↩][↩][↩][↩][↩]
- Bilezikian JP, Khan A, Potts JT Jr, Brandi ML, Clarke BL, Shoback D, Jüppner H, D’Amour P, Fox J, Rejnmark L, Mosekilde L, Rubin MR, Dempster D, Gafni R, Collins MT, Sliney J, Sanders J. Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res. 2011 Oct;26(10):2317-37. doi: 10.1002/jbmr.483[↩][↩][↩]
- Fong J, Khan A. Hypocalcemia: updates in diagnosis and management for primary care. Can Fam Physician. 2012 Feb;58(2):158-62 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267[↩]
- Schafer AL, Shoback DM. Hypocalcemia: Diagnosis and Treatment. [Updated 2016 Jan 3]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279022[↩]
- Committee to Review Dietary Reference Intakes for Vitamin D and Calcium, Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Hypocalcemia. https://emedicine.medscape.com/article/241893-overview[↩][↩]
- Hypocalcemia. https://emedicine.medscape.com/article/241893-overview#a5[↩][↩]
- Sarko J. Bone and mineral metabolism. Emerg Med Clin North Am. 2005 Aug;23(3):703-21, viii. doi: 10.1016/j.emc.2005.03.01[↩]
- Pedersen KO. Binding of calcium to serum albumin. I. Stoichiometry and intrinsic association constant at physiological pH, ionic strength, and temperature. Scand J Clin Lab Invest. 1971 Dec. 28(4):459-69.[↩]
- Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia. BMJ. 2008;336(7656):1298–302.[↩]
- Khan M, Jose A, Sharma S. Physiology, Parathyroid Hormone. [Updated 2022 Oct 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499940[↩]
- Dirk Vanderschueren and others, Active Vitamin D (1,25-Dihydroxyvitamin D) and Bone Health in Middle-Aged and Elderly Men: The European Male Aging Study (EMAS), The Journal of Clinical Endocrinology & Metabolism, Volume 98, Issue 3, 1 March 2013, Pages 995–1005, https://doi.org/10.1210/jc.2012-2772[↩]
- Lips P. Vitamin D physiology. Prog Biophys Mol Biol. 2006 Sep;92(1):4-8. doi: 10.1016/j.pbiomolbio.2006.02.016[↩][↩]
- Lieben L, Carmeliet G, Masuyama R. Calcemic actions of vitamin D: effects on the intestine, kidney and bone. Best Pract Res Clin Endocrinol Metab. 2011 Aug;25(4):561-72. doi: 10.1016/j.beem.2011.05.008[↩]
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, et al., editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): National Academies Press (US); 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56070/ doi: 10.17226/13050[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Goyal A, Anastasopoulou C, Ngu M, et al. Hypocalcemia. [Updated 2022 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430912[↩][↩][↩][↩][↩][↩][↩]
- Schnitzler CM, Pettifor JM. Calcium Deficiency Rickets in African Adolescents: Cortical Bone Histomorphometry. JBMR Plus. 2019 Feb 11;3(6):e10169. doi: 10.1002/jbm4.10169[↩][↩]
- Kooh SW, Fraser D, Reilly BJ, Hamilton JR, Gall DG, Bell L. Rickets due to calcium deficiency. N Engl J Med. 1977;297:1264–1266. doi: 10.1056/NEJM197712082972307[↩]
- Thacher TD, Fischer PR, Pettifor JM. Rickets: vitamin D and calcium deficiency. J Bone Miner Res. 2007;22:638–638. doi: 10.1359/jbmr.070118[↩]
- Pettifor JM. Nutritional rickets: deficiency of vitamin D, calcium, or both? Am J Clin Nutr. 2004 Dec;80(6 Suppl):1725S-9S. doi: 10.1093/ajcn/80.6.1725S[↩]
- Sempos CT, Durazo-Arvizu RA, Fischer PR, Munns CF, Pettifor JM, Thacher TD. Serum 25-hydroxyvitamin D requirements to prevent nutritional rickets in Nigerian children on a low-calcium diet-a multivariable reanalysis. Am J Clin Nutr. 2021 Jul 1;114(1):231-237. doi: 10.1093/ajcn/nqab048[↩]
- Bronner F. Mechanisms of intestinal calcium absorption. Journal of Cellular Biochemistry 2003; 88(2):387–393. https://www.ncbi.nlm.nih.gov/pubmed/12520541[↩]
- Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA. Clarification of DRIs for calcium and vitamin D across age groups. J Am Diet Assoc. 2011 Oct;111(10):1467. doi: 10.1016/j.jada.2011.08.022[↩][↩]
- Weaver CM, Heaney RP. Isotopic exchange of ingested calcium between labeled sources. Evidence that ingested calcium does not form a common absorptive pool. Calcif Tissue Int. 1991 Oct;49(4):244-7. doi: 10.1007/BF02556212[↩]
- Weaver CM, Proulx WR, Heaney R. Choices for achieving adequate dietary calcium with a vegetarian diet. Am J Clin Nutr. 1999 Sep;70(3 Suppl):543S-548S. doi: 10.1093/ajcn/70.3.543s[↩][↩]
- Kerstetter JE, O’Brien KO, Caseria DM, Wall DE, Insogna KL. The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. J Clin Endocrinol Metab. 2005 Jan;90(1):26-31. doi: 10.1210/jc.2004-0179[↩]
- Barrett-Connor E, Chang JC, Edelstein SL. Coffee-associated osteoporosis offset by daily milk consumption. The Rancho Bernardo Study. JAMA. 1994 Jan 26;271(4):280-3. doi: 10.1001/jama.1994.03510280042030[↩]
- Massey LK, Whiting SJ. Caffeine, urinary calcium, calcium metabolism and bone. J Nutr. 1993 Sep;123(9):1611-4. doi: 10.1093/jn/123.9.1611[↩]
- Hirsch PE, Peng TC. Effects of alcohol on calcium homeostasis and bone. In: Anderson J, Garner S, eds. Calcium and Phosphorus in Health and Disease. Boca Raton, FL: CRC Press, 1996:289-300.[↩]
- U.S. Department of Agriculture. Results from the United States Department of Agriculture’s 1994-96 Continuing Survey of Food Intakes by Individuals/Diet and Health Knowledge Survey, 1994-96.[↩]
- Heaney RP, Rafferty K. Carbonated beverages and urinary calcium excretion. Am J Clin Nutr. 2001 Sep;74(3):343-7. doi: 10.1093/ajcn/74.3.343[↩]
- Fenton TR, Eliasziw M, Lyon AW, Tough SC, Hanley DA. Meta-analysis of the quantity of calcium excretion associated with the net acid excretion of the modern diet under the acid-ash diet hypothesis. Am J Clin Nutr. 2008 Oct;88(4):1159-66. doi: 10.1093/ajcn/88.4.1159[↩]
- Calcium. https://ods.od.nih.gov/factsheets/Calcium-Consumer[↩][↩][↩][↩][↩][↩][↩]
- Wallace TC, McBurney M, Fulgoni VL 3rd. Multivitamin/mineral supplement contribution to micronutrient intakes in the United States, 2007-2010. J Am Coll Nutr. 2014;33(2):94-102. doi: 10.1080/07315724.2013.846806[↩]
- U.S. Department of Agriculture, Agricultural Research Service. Food Surveys Research Group: Beltsville, MD. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/wweia-data-tables/[↩][↩][↩][↩]
- Blumberg JB, Frei B, Fulgoni VL III, Weaver CM, Zeisel SH. Contribution of Dietary Supplements to Nutritional Adequacy in Race/Ethnic Population Subgroups in the United States. Nutrients. 2017 Nov 28;9(12):1295. doi: 10.3390/nu9121295[↩]
- Marshall K, Teo L, Shanahan C, Legette L, Mitmesser SH. Inadequate calcium and vitamin D intake and osteoporosis risk in older Americans living in poverty with food insecurities. PLoS One. 2020 Jul 8;15(7):e0235042. doi: 10.1371/journal.pone.0235042[↩]
- Calcium. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional[↩][↩][↩]
- Calcium. https://lpi.oregonstate.edu/mic/minerals/calcium[↩][↩][↩][↩][↩][↩][↩]
- Liamis G, Milionis HJ, Elisaf M. A review of drug-induced hypocalcemia. J Bone Miner Metab. 2009;27(6):635-42. doi: 10.1007/s00774-009-0119-x[↩][↩][↩][↩][↩]
- Gilman, A. G., L. S. Goodman, and A. Gilman. (eds.). Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 6th ed. New York: Macmillan Publishing Co., Inc. 1980., p. 1528[↩]
- Harvard University, Harvard School of Public Health. Calcium: What’s Best for Your Bones and Health ? https://www.hsph.harvard.edu/nutritionsource/calcium-full-story/[↩][↩][↩]
- Weaver CM. Calcium. In: Marriott BP, Birt DF, Stallings VA, Yates AA, eds. Present Knowledge in Nutrition. 11th ed. Cambridge, Massachusetts: Wiley-Blackwell; 2020:321-48.[↩][↩][↩][↩][↩][↩]
- Wawrzyniak N, Suliburska J. Nutritional and health factors affecting the bioavailability of calcium: a narrative review. Nutr Rev. 2021 Nov 10;79(12):1307-1320. doi: 10.1093/nutrit/nuaa138[↩]
- Weaver CM. Calcium. In: Erdman JJ, Macdonald I, Zeisel S, eds. Present Knowledge in Nutrition. 10th ed: John Wiley & Sons, Inc.; 2012:434-446.[↩]
- Fairweather-Tait SJ, Teucher B. Iron and calcium bioavailability of fortified foods and dietary supplements. Nutr Rev. 2002 Nov;60(11):360-7. doi: 10.1301/00296640260385801[↩]
- Song L. Calcium and Bone Metabolism Indices. Adv Clin Chem. 2017;82:1-46. doi: 10.1016/bs.acc.2017.06.005[↩][↩][↩][↩]
- Weaver CM, Heaney RP. Calcium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:133-49.[↩][↩][↩][↩][↩][↩]
- Wesseling-Perry K, Wang H, Elashoff R, Gales B, Jüppner H, Salusky IB. Lack of FGF23 response to acute changes in serum calcium and PTH in humans. J Clin Endocrinol Metab. 2014 Oct;99(10):E1951-6. doi: 10.1210/jc.2014-2125[↩]
- Clapham DE. Calcium signaling. Cell. 2007 Dec 14;131(6):1047-58. doi: 10.1016/j.cell.2007.11.028[↩]
- Dietary Guidelines for Americans. https://www.dietaryguidelines.gov[↩]
- U.S. Department of Agriculture, Center for Nutrition Policy and Promotion. ChooseMyPlate.gov 2011. https://www.myplate.gov[↩]
- Wongdee K, Rodrat M, Teerapornpuntakit J, Krishnamra N, Charoenphandhu N. Factors inhibiting intestinal calcium absorption: hormones and luminal factors that prevent excessive calcium uptake. J Physiol Sci. 2019 Sep;69(5):683-696. doi: 10.1007/s12576-019-00688-3[↩]
- Wikoff D, Welsh BT, Henderson R, Brorby GP, Britt J, Myers E, Goldberger J, Lieberman HR, O’Brien C, Peck J, Tenenbein M, Weaver C, Harvey S, Urban J, Doepker C. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food Chem Toxicol. 2017 Nov;109(Pt 1):585-648. doi: 10.1016/j.fct.2017.04.002[↩]
- Gallagher JC, Yalamanchili V, Smith LM. The effect of vitamin D on calcium absorption in older women. J Clin Endocrinol Metab. 2012 Oct;97(10):3550-6. doi: 10.1210/jc.2012-2020[↩]
- Food Labeling: Revision of the Nutrition and Supplement Facts Labels. https://www.federalregister.gov/documents/2016/05/27/2016-11867/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels[↩]
- The USDA Food DataCentral. https://fdc.nal.usda.gov[↩]
- Manappallil RG, Krishnan R, Veetil PP, Nambiar H, Karadan U, Anil R, Josephine B. Hypocalcemic Seizure Due to Vitamin D Deficiency. Indian J Crit Care Med. 2020 Sep;24(9):882-884. doi: 10.5005/jp-journals-10071-23586[↩]
- Chen Z, Zhao Q, Du J, Wang Y, Han R, Xu C, Chen X, Shu M. Risk factors for postoperative hypocalcaemia after thyroidectomy: A systematic review and meta-analysis. J Int Med Res. 2021 Mar;49(3):300060521996911. doi: 10.1177/0300060521996911[↩]
- Kakava K, Tournis S, Papadakis G, Karelas I, Stampouloglou P, Kassi E, Triantafillopoulos I, Villiotou V, Karatzas T. Postsurgical Hypoparathyroidism: A Systematic Review. In Vivo. 2016 May-Jun;30(3):171-9.[↩]
- Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. 2014 Mar;101(4):307-20. doi: 10.1002/bjs.9384[↩]
- Mathur A, Nagarajan N, Kahan S, Schneider EB, Zeiger MA. Association of Parathyroid Hormone Level With Postthyroidectomy Hypocalcemia: A Systematic Review. JAMA Surg. 2018 Jan 1;153(1):69-76. doi: 10.1001/jamasurg.2017.3398[↩]
- Burch WM, Posillico JT. Hypoparathyroidism after I-131 therapy with subsequent return of parathyroid function. J Clin Endocrinol Metab. 1983 Aug. 57(2):398-401.[↩]
- Cruz DN, Perazella MA. Biochemical aberrations in a dialysis patient following parathyroidectomy. Am J Kidney Dis. 1997 May. 29(5):759-62.[↩]
- Vitamin D. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional[↩][↩]
- Linnebur SA, Vondracek SF, Vande Griend JP, Ruscin JM, McDermott MT. Prevalence of vitamin D insufficiency in elderly ambulatory outpatients in Denver, Colorado. Am J Geriatr Pharmacother. 2007 Mar. 5(1):1-8.[↩][↩]
- Barone A, Giusti A, Pioli G, Girasole G, Razzano M, Pizzonia M, et al. Secondary hyperparathyroidism due to hypovitaminosis D affects bone mineral density response to alendronate in elderly women with osteoporosis: a randomized controlled trial. J Am Geriatr Soc. 2007 May. 55(5):752-7.[↩]
- Johnson JM, Maher JW, DeMaria EJ, Downs RW, Wolfe LG, Kellum JM. The long-term effects of gastric bypass on vitamin D metabolism. Ann Surg. 2006 May. 243(5):701-4; discussion 704-5.[↩]
- Shoback DM, Bilezikian JP, Costa AG, Dempster D, Dralle H, Khan AA, et al. Presentation of Hypoparathyroidism: Etiologies and Clinical Features. J Clin Endocrinol Metab. 2016 Jun. 101 (6):2300-12.[↩]
- Slomp J, van der Voort PH, Gerritsen RT, Berk JA, Bakker AJ. Albumin-adjusted calcium is not suitable for diagnosis of hyper- and hypocalcemia in the critically ill. Crit Care Med. 2003 May;31(5):1389-93. doi: 10.1097/01.CCM.0000063044.55669.3C[↩][↩]
- Muhammed H, Jain A, Irfan M, Charles S, Dwivedi P, Chavan PP, Khubchandani R, Sharma A, Phatak S, Shukla AN, Shah R, Subramanian N, Pandya SC, Singh YP, Chengappa KG, Thabah M, Rajasekhar L, Shobha V, Negi VS, Dhir V, Sharma A, Misra R, Aggarwal A; SLE-SIG of IRA. Clinical features, severity and outcome of acute pancreatitis in systemic lupus erythematosus. Rheumatol Int. 2022 Aug;42(8):1363-1371. doi: 10.1007/s00296-021-04834-2[↩]
- Kelly A, Levine MA. Hypocalcemia in the critically ill patient. J Intensive Care Med. 2013 May-Jun;28(3):166-77. doi: 10.1177/0885066611411543[↩]
- Zivin JR, Gooley T, Zager RA, Ryan MJ. Hypocalcemia: a pervasive metabolic abnormality in the critically ill. Am J Kidney Dis. 2001 Apr. 37(4):689-98.[↩]
- Martha JW, Wibowo A, Pranata R. Hypocalcemia is associated with severe COVID-19: A systematic review and meta-analysis. Diabetes Metab Syndr. 2021 Jan-Feb;15(1):337-342. doi: 10.1016/j.dsx.2021.01.003[↩]
- Forsythe RM, Wessel CB, Billiar TR, Angus DC, Rosengart MR. Parenteral calcium for intensive care unit patients. Cochrane Database Syst Rev. 2008. (4):CD006163.[↩]
- Jacob J, Raghothama S, Subramanyam K, Johny D. Hypomagnesaemia causing functional hypoparathyroidism in rheumatic mitral stenosis leading to sudden cardiac arrest in a young woman. BMJ Case Rep. 2021 Jul 19;14(7):e244176. doi: 10.1136/bcr-2021-244176[↩]
- Szczech LA. The impact of calcimimetic agents on the use of different classes of phosphate binders: results of recent clinical trials. Kidney International. 2004. 90:S46-48.[↩]
- Kido Y, Okamura T, Tomikawa M, Yamamoto M, Shiraishi M, Okada Y. Hypocalcemia associated with 5-fluorouracil and low dose leucovorin in patients with advanced colorectal or gastric carcinomas. Cancer. 1996 Oct 15. 78(8):1794-7.[↩]
- Manohar S, Kompotiatis P, Thongprayoon C, Cheungpasitporn W, Herrmann J, Herrmann SM. Programmed cell death protein 1 inhibitor treatment is associated with acute kidney injury and hypocalcemia: meta-analysis. Nephrol Dial Transplant. 2019 Jan 1. 34 (1):108-117.[↩]
- Recker RR, Lewiecki EM, Miller PD, Reiffel J. Safety of bisphosphonates in the treatment of osteoporosis. Am J Med. 2009 Feb. 122(2 Suppl):S22-32.[↩]
- Stamp TC, Round JM, Rowe DJ, Haddad JG. Plasma levels and therapeutic effect of 25-hydroxycholecalciferol in epileptic patients taking anticonvulsant drugs. Br Med J. 1972 Oct 7. 4(5831):9-12.[↩]
- Marlow CF, Sharma S, Babar F, Lin J. Severe Hypocalcemia and Hypomagnesemia with Denosumab in Advanced Chronic Kidney Disease: Case Report and Literature Review. Case Rep Oncol Med. 2018 Oct 14;2018:2059364. doi: 10.1155/2018/2059364[↩]
- McCormick BB, Davis J, Burns KD. Severe hypocalcemia following denosumab injection in a hemodialysis patient. Am J Kidney Dis. 2012 Oct. 60(4):626-8.[↩]
- Niemeijer ND, Rijk MC, van Guldener C. Symptomatic hypocalcemia after sodium phosphate preparation in an adult with asymptomatic hypoparathyroidism. Eur J Gastroenterol Hepatol. 2008 Apr. 20(4):356-8.[↩]
- Vasudeva M, Mathew JK, Groombridge C, Tee JW, Johnny CS, Maini A, Fitzgerald MC. Hypocalcemia in trauma patients: A systematic review. J Trauma Acute Care Surg. 2021 Feb 1;90(2):396-402. doi: 10.1097/TA.0000000000003027[↩]
- Brasier AR, Nussbaum SR. Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med. 1988 Apr. 84(4):654-60.[↩]
- Norman JG, Politz DE. Safety of immediate discharge after parathyroidectomy: a prospective study of 3,000 consecutive patients. Endocr Pract. 2007 Mar-Apr. 13(2):105-13.[↩]
- Almaghamsi A, Almalki MH, Buhary BM. Hypocalcemia in Pregnancy: A Clinical Review Update. Oman Med J. 2018 Nov;33(6):453-462. doi: 10.5001/omj.2018.85[↩]
- Lier H, Krep H, Schroeder S, Stuber F. Preconditions of hemostasis in trauma: a review. The influence of acidosis, hypocalcemia, anemia, and hypothermia on functional hemostasis in trauma. J Trauma. 2008 Oct. 65(4):951-60.[↩]
- Dettelbach MA, Deftos LJ, Stewart AF: Intraperitoneal free fatty acids induce severe hypocalcemia in rats: A model for the hypocalcemia of pancreatitis. J Bone Miner Res 5:1249-1255, 1990[↩]
- Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ. 2015 Sep 29;351:h4183. doi: 10.1136/bmj.h4183[↩]
- Cano A, Chedraui P, Goulis DG, Lopes P, Mishra G, Mueck A, Senturk LM, Simoncini T, Stevenson JC, Stute P, Tuomikoski P, Rees M, Lambrinoudaki I. Calcium in the prevention of postmenopausal osteoporosis: EMAS clinical guide. Maturitas. 2018 Jan;107:7-12. doi: 10.1016/j.maturitas.2017.10.004[↩]
- Abrams SA, Silber TJ, Esteban NV, Vieira NE, Stuff JE, Meyers R, Majd M, Yergey AL. Mineral balance and bone turnover in adolescents with anorexia nervosa. J Pediatr. 1993 Aug;123(2):326-31. doi: 10.1016/s0022-3476(05)81714-7[↩]
- Drinkwater BL, Bruemner B, Chesnut CH 3rd. Menstrual history as a determinant of current bone density in young athletes. JAMA. 1990 Jan 26;263(4):545-8.[↩]
- Marcus R, Cann C, Madvig P, Minkoff J, Goddard M, Bayer M, Martin M, Gaudiani L, Haskell W, Genant H. Menstrual function and bone mass in elite women distance runners. Endocrine and metabolic features. Ann Intern Med. 1985 Feb;102(2):158-63. doi: 10.7326/0003-4819-102-2-158[↩]
- Nattiv A. Stress fractures and bone health in track and field athletes. J Sci Med Sport. 2000 Sep;3(3):268-79. doi: 10.1016/s1440-2440(00)80036-5[↩]
- Lappe J, Cullen D, Haynatzki G, Recker R, Ahlf R, Thompson K. Calcium and vitamin d supplementation decreases incidence of stress fractures in female navy recruits. J Bone Miner Res. 2008 May;23(5):741-9. doi: 10.1359/jbmr.080102[↩]
- Boaventura RM, Mendonça RB, Fonseca FA, Mallozi M, Souza FS, Sarni ROS. Nutritional status and food intake of children with cow’s milk allergy. Allergol Immunopathol (Madr). 2019 Nov-Dec;47(6):544-550. doi: 10.1016/j.aller.2019.03.003[↩]
- Bakaloudi DR, Halloran A, Rippin HL, Oikonomidou AC, Dardavesis TI, Williams J, Wickramasinghe K, Breda J, Chourdakis M. Intake and adequacy of the vegan diet. A systematic review of the evidence. Clin Nutr. 2021 May;40(5):3503-3521. doi: 10.1016/j.clnu.2020.11.035[↩]
- Wilt TJ, Shaukat A, Shamliyan T, Taylor BC, MacDonald R, Tacklind J, Rutks I, Schwarzenberg SJ, Kane RL, and Levitt M. Lactose Intolerance and Health. No. 192 (Prepared by the Minnesota Evidence-based Practice Center under Contract No. HHSA 290-2007-10064-I.) AHRQ Publication No. 10-E004. Rockville, MD. Agency for Healthcare Research and Quality. February 2010.[↩]
- Suchy FJ, Brannon PM, Carpenter TO, Fernandez JR, Gilsanz V, Gould JB, Hall K, Hui SL, Lupton J, Mennella J, Miller NJ, Osganian SK, Sellmeyer DE, Wolf MA. NIH Consensus Development Conference Statement: Lactose Intolerance and Health. NIH Consens State Sci Statements. 2010 Feb 22–24; 27(2):1–27. https://consensus.nih.gov/2010/lactosestatement.htm[↩][↩]
- Johnson AO, Semenya JG, Buchowski MS, Enwonwu CO, Scrimshaw NS. Correlation of lactose maldigestion, lactose intolerance, and milk intolerance. Am J Clin Nutr. 1993 Mar;57(3):399-401. doi: 10.1093/ajcn/57.3.399[↩]
- Nose O, Iida Y, Kai H, Harada T, Ogawa M, Yabuuchi H. Breath hydrogen test for detecting lactose malabsorption in infants and children. Prevalence of lactose malabsorption in Japanese children and adults. Arch Dis Child. 1979 Jun;54(6):436-40. doi: 10.1136/adc.54.6.436[↩]
- Rao DR, Bello H, Warren AP, Brown GE. Prevalence of lactose maldigestion. Influence and interaction of age, race, and sex. Dig Dis Sci. 1994 Jul;39(7):1519-24. doi: 10.1007/BF02088058[↩]
- Hertzler SR, Savaiano DA. Colonic adaptation to daily lactose feeding in lactose maldigesters reduces lactose intolerance. Am J Clin Nutr. 1996 Aug;64(2):232-6. doi: 10.1093/ajcn/64.2.232[↩]
- Pribila BA, Hertzler SR, Martin BR, Weaver CM, Savaiano DA. Improved lactose digestion and intolerance among African-American adolescent girls fed a dairy-rich diet. J Am Diet Assoc. 2000 May;100(5):524-8; quiz 529-30. doi: 10.1016/S0002-8223(00)00162-0[↩]
- Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, Sigurdardottir ST, Lindner T, Goldhahn K, Dahlstrom J, McBride D, Madsen C. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol. 2007 Sep;120(3):638-46. doi: 10.1016/j.jaci.2007.05.026[↩]
- Marsh AG, Sanchez TV, Midkelsen O, Keiser J, Mayor G. Cortical bone density of adult lacto-ovo-vegetarian and omnivorous women. J Am Diet Assoc. 1980 Feb;76(2):148-51.[↩]
- Reed JA, Anderson JJ, Tylavsky FA, Gallagher PN Jr. Comparative changes in radial-bone density of elderly female lacto-ovovegetarians and omnivores. Am J Clin Nutr. 1994 May;59(5 Suppl):1197S-1202S. doi: 10.1093/ajcn/59.5.1197S. Erratum in: Am J Clin Nutr 1994 Dec;60(6):981.[↩]
- Janelle KC, Barr SI. Nutrient intakes and eating behavior scores of vegetarian and nonvegetarian women. J Am Diet Assoc. 1995 Feb;95(2):180-6, 189, quiz 187-8. doi: 10.1016/s0002-8223(95)00045-3[↩]
- American Dietetic Association; Dietitians of Canada. Position of the American Dietetic Association and Dietitians of Canada: Vegetarian diets. J Am Diet Assoc. 2003 Jun;103(6):748-65. doi: 10.1053/jada.2003.50142[↩]
- Appleby P, Roddam A, Allen N, Key T. Comparative fracture risk in vegetarians and nonvegetarians in EPIC-Oxford. Eur J Clin Nutr. 2007 Dec;61(12):1400-6. doi: 10.1038/sj.ejcn.1602659[↩]
- Schafer AL and Shoback D: Hypocalcemia: definition, etiology, pathogenesis, diagnosis and management. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, C. J. Rosen (ed), John Wiley and Sons, Eighth Edition. pp 572-578, 2013[↩]
- Rallidis LS, Gregoropoulos PP, Papasteriadis EG: A case of severe hypocalcaemia mimicking myocardial infarction. Int J Cardiol 61:89-91, 1997[↩]
- Lehmann G, Deisenhofer I, Ndrepepa G, et al: ECG changes in a 25-year-old woman with hypocalcemia due to hypoparathyroidism: Hypocalcemia mimicking acute myocardial infarction. Chest 119:668-669, 2001[↩]
- RuDusky BM: ECG abnormalities associated with hypocalcemia. Chest 119:668-669, 2001[↩]
- Suzuki T, Ikeda U, Fujikawa H, et al: Hypocalcemic heart failure: A reversible form of heart muscle disease. Clin Cardiol 21:227-228, 1998[↩]
- Wong CK, Lau CP, Cheng CH, et al: Hypocalcemic myocardial dysfunction: Short- and long-term improvement with calcium replacement. Am Heart J 120:381-386, 1990[↩]
- Bilezikian JP, Khan A, Potts JT Jr, et al: Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment and challenges for future research. J Bone Min Res 26: 2317-37, 2011[↩][↩]
- Mitchell DM, Regan S, Cobley MR, et al: Long-term followup of patients with hypoparathyroidism. J Clin Endo Metab 97: 4507-4514, 2012[↩][↩][↩]
- Basser LS, Neale FC, Ireland AW, et al: Epilepsy and electroencephalographic abnormalities in chronic surgical hypoparathyroidism. Ann Intern Med 71:507-515, 1969[↩]
- Faig JC, Kalinyak J, Marcus R, et al: Chronic atypical seizure disorder and cataracts due to delayed diagnosis of pseudohypoparathyroidism. West J Med 157:64-65, 1992[↩]
- Shoback D: Clinical practice: hypoparathyroidism. N Engl J Med 359: 391-403, 2008[↩]
- Jesus JE, Landry A. Images in clinical medicine. Chvostek’s and Trousseau’s signs. N Engl J Med 2012;367:e15. doi:10.1056/NEJMicm1110569[↩]
- Urbano FL. Signs of hypocalcemia: Chvostek’s and Trousseau’s. Hosp Physician 2000;36:43-5.[↩]
- Hypocalcemia Workup. https://emedicine.medscape.com/article/241893-workup[↩]
- Bushinsky DA, Monk RD. Electrolyte quintet: Calcium. Lancet. 1998 Jul 25;352(9124):306-11. doi: 10.1016/s0140-6736(97)12331-5. Erratum in: Lancet 2002 Jan 19;359(9302):266.[↩]
- Hypocalcemia. https://emedicine.medscape.com/article/241893-overview#a1[↩]
- Lienhardt A, Bai M, Lagarde JP, Rigaud M, Zhang Z, Jiang Y, Kottler ML, Brown EM, Garabédian M. Activating mutations of the calcium-sensing receptor: management of hypocalcemia. J Clin Endocrinol Metab. 2001 Nov;86(11):5313-23. doi: 10.1210/jcem.86.11.8016[↩]
- Anast CS, Winnacker JL, Forte LR, Burns TW. Impaired release of parathyroid hormone in magnesium deficiency. J Clin Endocrinol Metab. 1976 Apr;42(4):707-17. doi: 10.1210/jcem-42-4-707[↩][↩]
- Schimatschek HF, Rempis R. Prevalence of hypomagnesemia in an unselected German population of 16,000 individuals. Magnes Res. 2001 Dec;14(4):283-90.[↩]
- Ryzen E, Wagers PW, Singer FR, Rude RK. Magnesium deficiency in a medical ICU population. Crit Care Med. 1985 Jan;13(1):19-21. doi: 10.1097/00003246-198501000-00006[↩]
- Osteoporosis to Prevent Fractures: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/osteoporosis-screening[↩][↩]
- Hypocalcemia Workup. https://emedicine.medscape.com/article/241893-workup#c11[↩][↩]
- Sempos CT, Heijboer AC, Bikle DD, Bollerslev J, Bouillon R, Brannon PM, DeLuca HF, Jones G, Munns CF, Bilezikian JP, Giustina A, Binkley N. Vitamin D assays and the definition of hypovitaminosis D: results from the First International Conference on Controversies in Vitamin D. Br J Clin Pharmacol. 2018 Oct;84(10):2194-2207. doi: 10.1111/bcp.13652[↩]
- LeFevre ML; U.S. Preventive Services Task Force. Screening for vitamin D deficiency in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015 Jan 20;162(2):133-40. doi: 10.7326/M14-2450[↩]
- Sempos CT, Binkley N. 25-Hydroxyvitamin D assay standardisation and vitamin D guidelines paralysis. Public Health Nutr. 2020 May;23(7):1153-1164. doi: 10.1017/S1368980019005251[↩]
- Brooks SPJ, Sempos CT. The importance of 25-hydroxyvitamin D assay standardization and the Vitamin D Standardization Program. Journal of AOAC International 2017;100:1223-4.[↩]
- Taylor CL, Sempos CT, Davis CD, Brannon PM. Vitamin D: Moving Forward to Address Emerging Science. Nutrients. 2017 Dec 1;9(12):1308. doi: 10.3390/nu912130[↩]
- Norman AW, Henry HH. Vitamin D. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition, 10th ed. Washington DC: Wiley-Blackwell, 2012.[↩]
- Hypocalcemia Workup. https://emedicine.medscape.com/article/241893-workup#c12[↩][↩]
- Goyal A, Singh S. Hypocalcemia. [Updated 2019 Jan 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430912[↩]
- Thakker RV. Parathyroid disorders and diseases altering calcium metabolism. In: Warrall D, Cox T, Firth J, Benz E, eds. Oxford textbook of medicine 4th ed. Oxford: Oxford University Press, 2003[↩][↩]
- Dickerson RN. Treatment of hypocalcemia in critical illness–part 1. Nutrition. 2007 Apr;23(4):358-61. doi: 10.1016/j.nut.2007.01.011[↩]
- Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008 Jul 24;359(4):391-403. doi: 10.1056/NEJMcp0803050[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Tohme JF, Bilezikian JP. Hypocalcemic emergencies. Endocrinol Metab Clin North Am. 1993 Jun;22(2):363-75.[↩][↩][↩]
- Body JJ, Bouillon R. Emergencies of calcium homeostasis. Rev Endocr Metab Disord. 2003 May;4(2):167-75. doi: 10.1023/a:1022994104070[↩]
- Kagen MH, Bansal MG, Grossman M. Calcinosis cutis following the administration of intravenous calcium therapy. Cutis. 2000 Apr;65(4):193-4.[↩]
- Maeda SS, Fortes EM, Oliveira UM, Borba VC, Lazaretti-Castro M. Hypoparathyroidism and pseudohypoparathyroidism. Arq Bras Endocrinol Metabol. 2006 Aug;50(4):664-73. doi: 10.1590/s0004-27302006000400012[↩][↩][↩]
- Bollerslev J, Rejnmark L, Marcocci C, et al: European Society of Endocrinology Clinical Guideline: treatment of chronic hypoparathyroidism in adults. Eur J Endocrinol 173: G1-G20, 2015[↩][↩][↩][↩][↩]
- Umpaichitra V, Bastian W, Castells S: Hypocalcemia in children: Pathogenesis and management. Clin Pediatr 40:305-312, 2001[↩]
- Arlt W, Fremerey C, Callies F, et al: Well-being, mood and calcium homeostasis in patients with hypoparathyroidism receiving standard treatment with calcium and vitamin D. Eur J Endocrinol 146:215-222, 2002[↩][↩]
- Underbjerg L, Sikjaer T, Mosekilde, Rejnmark L: Postsurgical hypoparathyroidism – risk of fractures, psychiatric diseases, cancer, cataract, and infections. J Bone Min Res 29: 2504-10, 2014[↩][↩]
- Underbjerg L, Sikjaer T, Mosekilde, Rejnmark L: Cardiovascular and renal complications to postsurgical hypoparathyroidism: A Danish nationwide controlled historic follow-up study. J Bone Min Res 28: 2277-2285, 2013[↩]
- Underbjerg L, Sikjaer T, Mosekilde, Rejnmark L: The epidemiology of non-surgical hypoparathyroidism in Denmark: a nationwide case finding study. J Bone Min Res 30: 1738-44, 2015[↩]
- Walker Harris V, Jan De Beur S. Postoperative hypoparathyroidism: medical and surgical therapeutic options. Thyroid. 2009 Sep;19(9):967-73. doi: 10.1089/thy.2008.0306[↩][↩][↩][↩][↩]
- Harvey JA, Zobitz MM, Pak CY. Dose dependency of calcium absorption: a comparison of calcium carbonate and calcium citrate. J Bone Miner Res. 1988 Jun;3(3):253-8. doi: 10.1002/jbmr.5650030303[↩]
- Eryol NK, Colak R, Ozdoğru I, Tanriverdi F, Unal S, Topsakal R, Katlandur H, Bayram F. Effects of calcium treatment on QT interval and QT dispersion in hypocalcemia. Am J Cardiol. 2003 Mar 15;91(6):750-2. doi: 10.1016/s0002-9149(02)03423-9[↩]
- Hopper AD, Hadjivassiliou M, Butt S, Sanders DS. Adult coeliac disease. BMJ. 2007 Sep 15;335(7619):558-62. doi: 10.1136/bmj.39316.442338.AD[↩][↩]
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006 Mar;81(3):353-73. doi: 10.4065/81.3.353[↩]
- Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998 Mar 14;351(9105):805-6. doi: 10.1016/s0140-6736(05)78933-9[↩][↩]
- Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003 Jan;77(1):204-10. doi: 10.1093/ajcn/77.1.204. Erratum in: Am J Clin Nutr. 2003 Nov;78(5):1047.[↩]
- Tangpricha V, Koutkia P, Rieke SM, Chen TC, Perez AA, Holick MF. Fortification of orange juice with vitamin D: a novel approach for enhancing vitamin D nutritional health. Am J Clin Nutr. 2003 Jun;77(6):1478-83. doi: 10.1093/ajcn/77.6.1478[↩]
- Armas LA, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab. 2004 Nov;89(11):5387-91. doi: 10.1210/jc.2004-0360[↩]
- Trang HM, Cole DE, Rubin LA, Pierratos A, Siu S, Vieth R. Evidence that vitamin D3 increases serum 25-hydroxyvitamin D more efficiently than does vitamin D2. Am J Clin Nutr. 1998 Oct;68(4):854-8. doi: 10.1093/ajcn/68.4.854[↩]
- Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ. 2003 Mar 1;326(7387):469. doi: 10.1136/bmj.326.7387.469[↩]
- Bouillon R, Norman AW, Lips P. Vitamin D deficiency. N Engl J Med. 2007 Nov 8;357(19):1980-1; author reply 1981-2. doi: 10.1056/NEJMc072359[↩]
- Noordzij M, Voormolen NM, Boeschoten EW, Dekker FW, Bos WJ, Krediet RT, Korevaar JC; NECOSAD study group. Disordered mineral metabolism is not a risk factor for loss of residual renal function in dialysis patients. Nephrol Dial Transplant. 2009 May;24(5):1580-7. doi: 10.1093/ndt/gfn768[↩]
- Horwitz MJ, Stewart AF. Hypoparathyroidism: is it time for replacement therapy? J Clin Endocrinol Metab. 2008 Sep;93(9):3307-9. doi: 10.1210/jc.2008-1216[↩]
- Arlt W, Fremerey C, Callies F, Reincke M, Schneider P, Timmermann W, Allolio B. Well-being, mood and calcium homeostasis in patients with hypoparathyroidism receiving standard treatment with calcium and vitamin D. Eur J Endocrinol. 2002 Feb;146(2):215-22. doi: 10.1530/eje.0.1460215[↩]
- Winer KK, Yanovski JA, Sarani B, Cutler GB Jr. A randomized, cross-over trial of once-daily versus twice-daily parathyroid hormone 1-34 in treatment of hypoparathyroidism. J Clin Endocrinol Metab. 1998 Oct;83(10):3480-6. doi: 10.1210/jcem.83.10.5185[↩]
- Winer KK, Ko CW, Reynolds JC, Dowdy K, Keil M, Peterson D, Gerber LH, McGarvey C, Cutler GB Jr. Long-term treatment of hypoparathyroidism: a randomized controlled study comparing parathyroid hormone-(1-34) versus calcitriol and calcium. J Clin Endocrinol Metab. 2003 Sep;88(9):4214-20. doi: 10.1210/jc.2002-021736[↩]
- Winer KK, Sinaii N, Peterson D, Sainz B Jr, Cutler GB Jr. Effects of once versus twice-daily parathyroid hormone 1-34 therapy in children with hypoparathyroidism. J Clin Endocrinol Metab. 2008 Sep;93(9):3389-95. doi: 10.1210/jc.2007-2552[↩]
- Winer KK, Yanovski JA, Cutler GB Jr. Synthetic human parathyroid hormone 1-34 vs calcitriol and calcium in the treatment of hypoparathyroidism. JAMA. 1996 Aug 28;276(8):631-6.[↩]
- Winer KK, Sinaii N, Reynolds J, Peterson D, Dowdy K, Cutler GB Jr. Long-term treatment of 12 children with chronic hypoparathyroidism: a randomized trial comparing synthetic human parathyroid hormone 1-34 versus calcitriol and calcium. J Clin Endocrinol Metab. 2010 Jun;95(6):2680-8. doi: 10.1210/jc.2009-2464[↩]
- Rubin MR, Sliney J Jr, McMahon DJ, Silverberg SJ, Bilezikian JP. Therapy of hypoparathyroidism with intact parathyroid hormone. Osteoporos Int. 2010 Nov;21(11):1927-34. doi: 10.1007/s00198-009-1149-x[↩]
- Rubin MR, Bilezikian JP. Hypoparathyroidism: clinical features, skeletal microstructure and parathyroid hormone replacement. Arq Bras Endocrinol Metabol. 2010 Mar;54(2):220-6. doi: 10.1590/s0004-27302010000200019[↩]
- Al-Azem H, Khan AA: Hypoparathyroidism. Best Pract Res Clin Endocrinol Metab 26:517-22, 2012[↩]
- Winer KK, Yanovski JA, Sarani B, Cutler GB Jr: A randomized, cross-over trial of once-daily versus twice-daily parathyroid hormone 1-34 treatment of hypoparathyroidism. J Clin Endocrinol Metab 83: 3480-86, 1998[↩]
- Witteveen JE, van Thiel S, Romijn JA, Hamdy NA: Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol 168:R45-53, 2013[↩]
- Winer KK, Ko CW, Reynolds JC, et al: Long-term treatment of hypoparathyroidism: a randomized controlled study comparing parathyroid hormone-(1-34) versus calcitriol and calcium. J Clin Endocrinol Metab 88: 4214-20, 2003[↩][↩]
- Winer KK, Sinaii N, Reynolds J, et al: Long-term treatment of 12 children with chronic hypoparathyroidism: a randomized trial comparing synthetic human parathyroid hormone 1-34 versus calcitriol and calcium. J Clin Endocrinol Metab 95: 2680-88, 2010[↩]
- Winer KK, Zhang B, Shrader JA, et al: Synthetic human parathyroid hormone 1-34 replacement therapy: a randomized crossover trial comparing pump versus injections in the treatment of chronic hypoparathyroidism. J Clin Endocrinol Metab 97: 391-99, 2012[↩]
- Cusano NE, Rubin MR, McMahon DJ, et al: PTH(1-84) is associated with improved quality of life in hypoparathyroidism through 5 years of therapy. J Clin Endocrinol Metab 99:3694-9, 2014[↩][↩]
- Rubin JR, Sliney J Jr, McMahon DJ, Silverberg SJ, Bilezikian JP: Therapy of hypoparathyroidism with intact parathyroid hormone. Osteo Int 21: 1927-34, 2010[↩]
- Mannstadt M, Clarke BL, Vokes T, et al: Efficacy and safety of recombinant human parathyroid hormone (1-84) in hypoparathyroidism (REPLACE): a double-blind, placebo-controlled, randomised phase 3 study. Lancet Diabetes Endocrinol 1: 275-83, 2014[↩][↩][↩]
- Sikjaer T, Amstrup AK, Rolighed L, et al: PTH(1-84) replacement therapy in hypoparathyroidism: a randomized controlled trial on pharmacokinetic and dynamic effects after 6 months of treatment. J Bone Miner Res 28:2232-43, 2013[↩]
- Vitamin D. https://ods.od.nih.gov/factsheets/VitaminD-Consumer[↩]
- Bouillon R. Comparative analysis of nutritional guidelines for vitamin D. Nat Rev Endocrinol. 2017 Aug;13(8):466-479. doi: 10.1038/nrendo.2017.31[↩]
- Michael F. Holick and others, Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline, The Journal of Clinical Endocrinology & Metabolism, Volume 96, Issue 7, 1 July 2011, Pages 1911–1930, https://doi.org/10.1210/jc.2011-0385[↩]
- SACN vitamin D and health report. https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report[↩]
- Osteoporosis. https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968[↩]
- Osteoporosis. https://lpi.oregonstate.edu/mic/health-disease/osteoporosis[↩][↩]