Contents
What is twin to twin transfusion syndrome
Twin-to-twin transfusion syndrome is a rare disease of the placenta that occurs only in monozygotic (identical) twins with a monochorionic placenta while they are in the womb. Twin-to-twin transfusion syndrome is the result of an intrauterine blood transfusion from one twin (donor) to another twin (recipient) that share the same placenta. Twin-to-twin transfusion syndrome affects twins or other multiples that share a single placenta containing blood vessels going from one baby to the other. Blood from the smaller “donor” twin is transferred to the larger “recipient” twin through interconnecting vessels causing an unequal exchange of blood. The donor twin is often smaller with a birth weight 20% less than the recipient’s birth weight. The donor twin is often anemic and the recipient twin is often plethoric with hemoglobin differences greater than 5 g/dL. The unequal size of identical twins is referred to as discordant twins.
Although all identical twins share a placenta, twin-to-twin transfusion syndrome develops in about 10 to 15 percent of those pregnancies. Twin-to-twin transfusion syndrome does not occur when the twins are non-identical (fraternal).
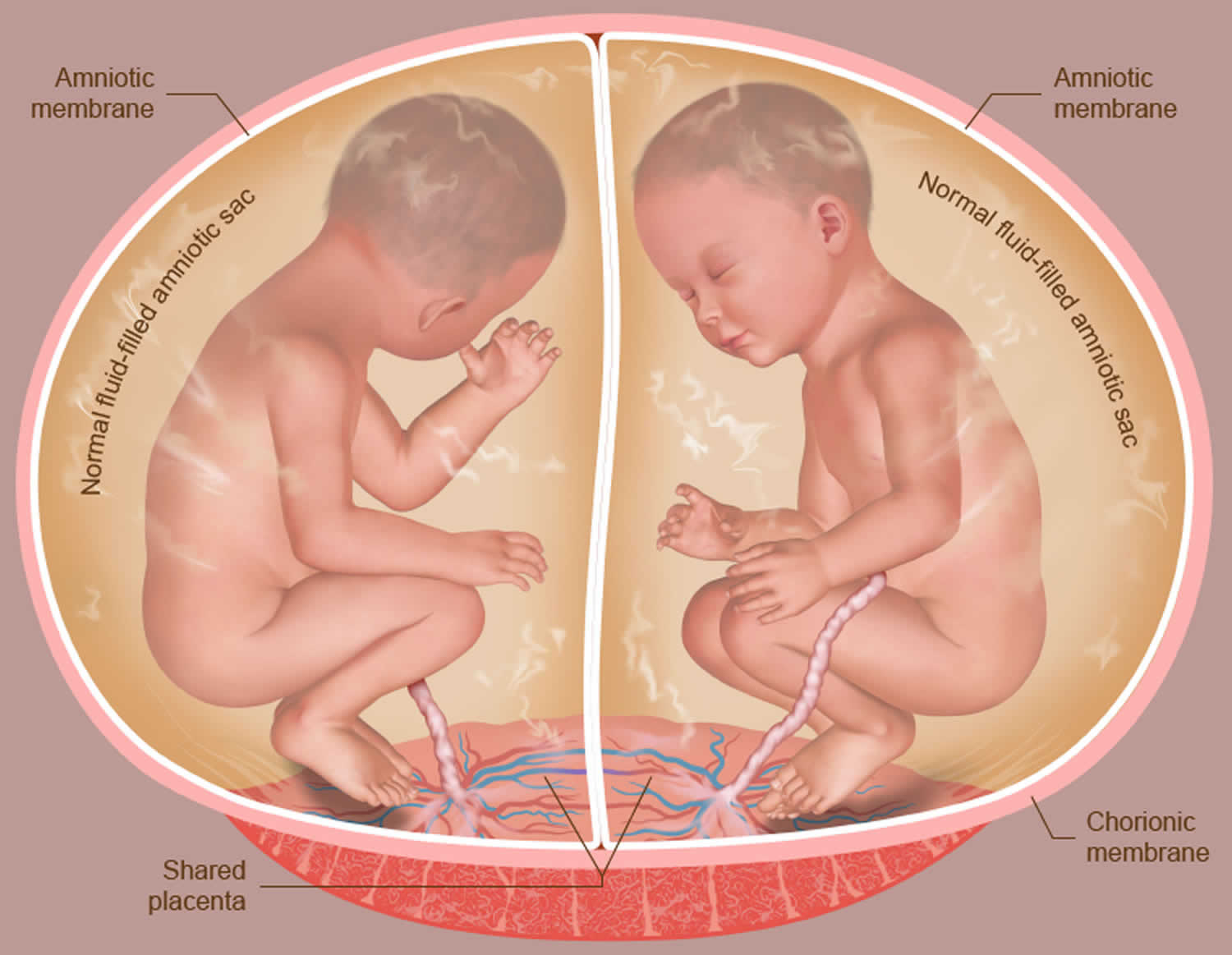
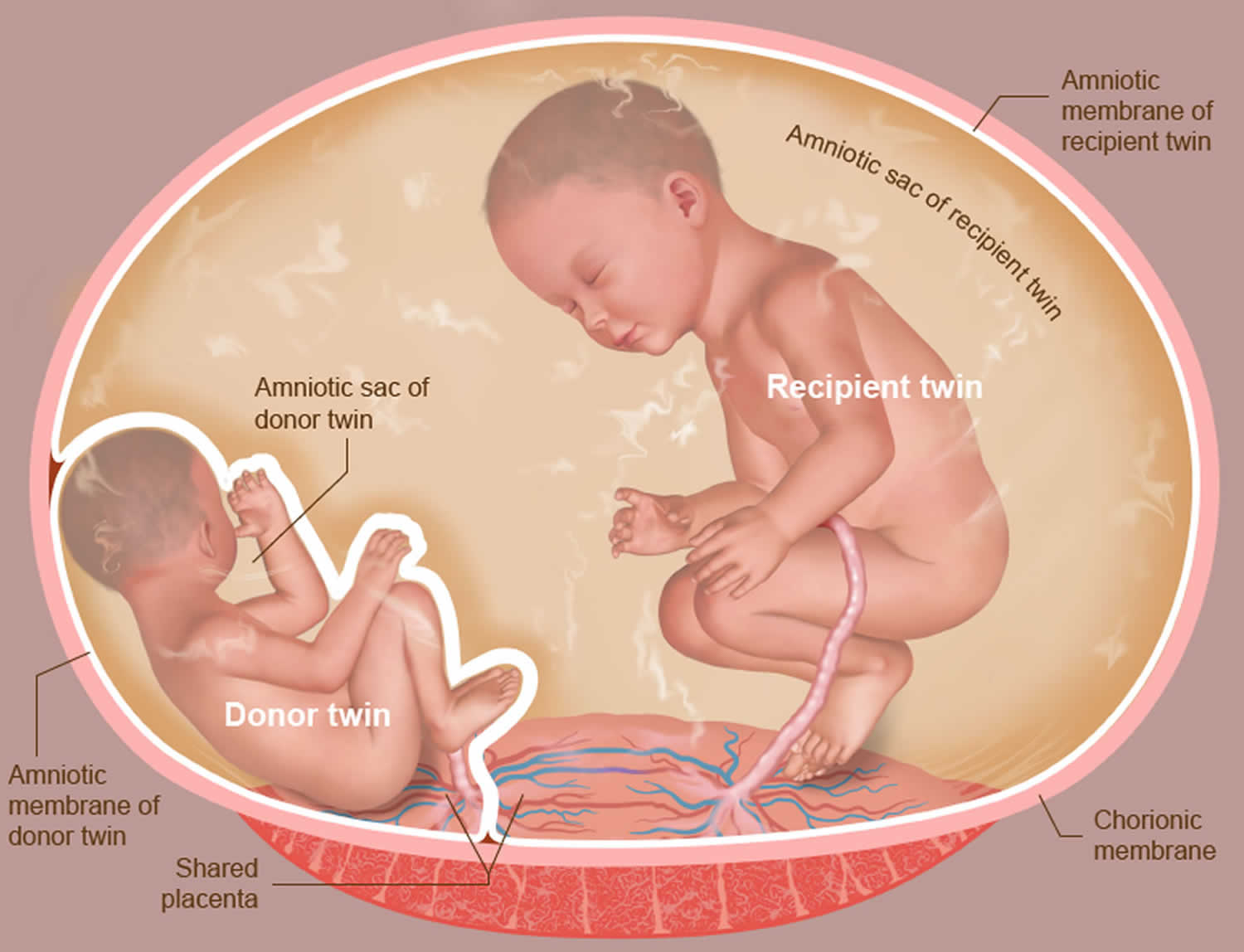
When babies share a placenta they also share connecting blood vessels. Usually the blood flow is equally balanced between them, and the babies are able to grow and develop normally (Figure 1). But in cases of twin-to-twin transfusion syndrome, the flow of blood becomes unbalanced, and one baby will actually donate blood to the other. When this happens, the baby donating the blood (the “donor” twin) becomes dehydrated and stops making urine. This results in a decrease in amniotic fluid, the protective liquid that surrounds the baby in the womb. The baby receiving the extra blood (the “recipient” twin), however, produces higher-than-normal amounts of urine, resulting in excess amniotic fluid (Figure 2).
The recipient twin is at risk for heart failure from receiving too much blood from both the placenta and donor twin, forcing its heart to work harder, while the donor twin is at risk for loss of blood.
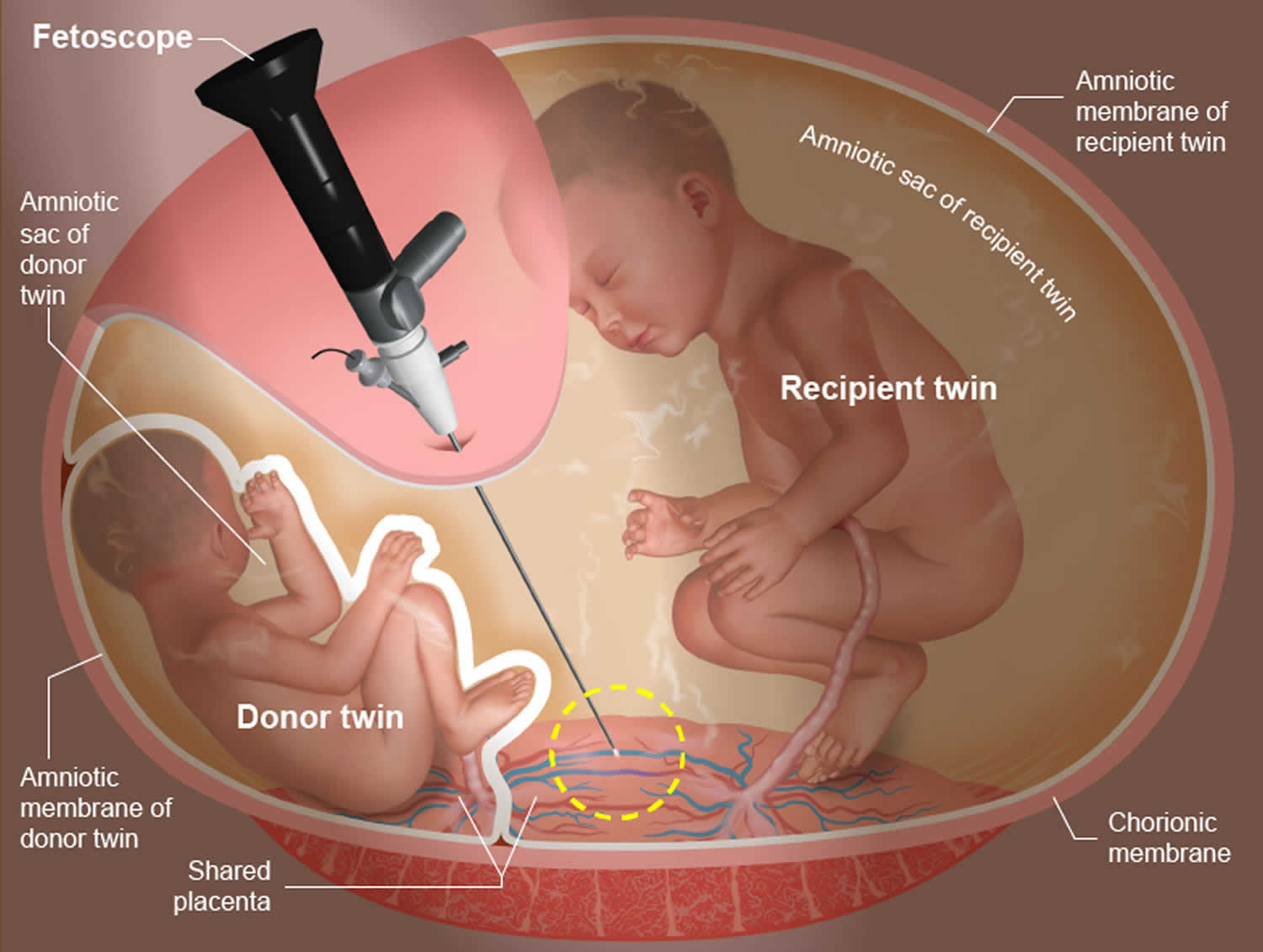
Untreated, twin-to-twin transfusion syndrome can be life-threatening for both babies. Laser surgery may be performed to correct the problem. A laser is endoscopically inserted into the womb to burn and seal the interconnecting blood vessels, restoring the normal flow of blood. Following treatment, the babies are regularly monitored.
Figure 1. Normal monochorionic identical twins
Figure 2. Twin to twin transfusion syndrome
Twin to twin transfusion syndrome causes
The placenta is a very active organ and provides babies with oxygen and nutrients during pregnancy. It grows along with the babies. Sometimes, for reasons that are not well understood, the normal flow of blood in the placenta’s blood vessels develops an abnormal pattern. When unborn babies share a placenta, the result can be an imbalance in blood circulation, with one baby receiving too much blood through the umbilical cord and the other receiving too little. It is this imbalance that leads to twin-to-twin transfusion syndrome.
Twin-to-twin transfusion syndrome occurs when the blood supply of one twin moves to the other through the shared placenta. The twin that loses the blood is called the donor twin. The twin that receives the blood is called the recipient twin.
Both infants may have problems depending on how much blood is passed from one to the other. The donor twin may have too little blood, and the other may have too much blood.
Twin to twin transfusion syndrome symptoms
In twin-twin transfusion syndrome, there is an unequal sharing of blood that passes between twins through blood vessel connections in the placenta. One twin (called the donor twin) pumps blood to the other twin (called the recipient). This causes the recipient twin to receive too much blood and the donor twin to receive too little.
The increased volume of blood causes the recipient twin to produce more than the usual amount of urine, which can result in a large bladder, too much amniotic fluid (known as polyhydramnios) and hydrops, a prenatal form of heart failure. The donor twin, who receives too little blood, produces less than the usual amount of urine. This results in low or no amniotic fluid surrounding it (oligohydramnios) and a small or absent bladder.
Without intervention, the condition can be fatal for both twins.
Twin to twin transfusion syndrome diagnosis
The most important step in evaluating a twin pregnancy for twin-twin transfusion syndrome is to determine whether the twins share a single placenta. A twin to twin transfusion syndrome diagnosis is confirmed by ultrasound during the first trimester. Twin-to-twin transfusion syndrome becomes evident when the ultrasound images show that one child has extra amniotic fluid and the other child has significantly decreased amounts. Abnormalities in the blood-flow patterns in the umbilical cord may also be found. In addition, the mother may experience a rapid enlargement of her uterus — more quickly than is expected during pregnancy.
Because twin-to-twin transfusion syndrome can develop rapidly, women carrying twins who share a placenta should undergo frequent ultrasounds to evaluate amniotic fluid volumes. Typically, ultrasounds are performed every two weeks, starting at 16 weeks. The frequency of ultrasounds then increases during the third trimester.
Your evaluation will involve the following exams:
- High-resolution ultrasound – An examination to rule out structural abnormalities in the twins. This exam will also confirm placental location and umbilical cord insertion into the placenta, as well as assess blood flow patterns in specific blood vessels for each twin.
- Fetal echocardiogram – A focused ultrasound of each twin’s heart to look for any related heart conditions. Twin-twin transfusion syndrome may cause serious cardiac strain in the recipient twin, resulting in enlargement of the heart and cardiac dysfunction. All twins evaluated for twin-to-twin transfusion syndrome should undergo a fetal echocardiogram. Fetal cardiology experts from have developed a cardiac scoring tool to determine how severe the condition has become for the twins. This score helps the medical team determine need for treatment.
- Genetic amniocentesis – A procedure in which a small amount of amniotic fluid is removed from the sacs surrounding the fetuses and tested. In some cases, this genetic test may be needed if imaging studies identify structural malformations in addition to twin-to-twin transfusion syndrome.
Accurate diagnosis is extremely important in distinguishing twin-to-twin transfusion syndrome from other related anomalies, such as selective intrauterine growth restriction (sIUGR). Twin-to-twin transfusion syndrome and selective intrauterine growth restriction (sIUGR) can both occur in monochorionic, diamniotic pregnancies, but are differentiated by the blood flow patterns between the twins. It is important to identify the specific patterns of blood flow to distinguish between the conditions and confirm the diagnosis.
Your test results and specific treatment options will be discussed in detail on the day of your evaluation. If fetal intervention is recommended, you can also expect to meet with an advanced practice nurse to complete preoperative testing, and a social worker to arrange temporary accommodations.
What is high-resolution fetal ultrasonography?
High-resolution fetal ultrasonography is a non-invasive test performed by an ultrasound specialist. The test uses reflected sound waves to create images of your babies within the womb. Doctors will use ultrasonography to follow the development of your babies’ internal organs and overall growth, as well as the volume of amniotic fluid that surrounds them throughout the pregnancy.
What is fetal echocardiogram?
Fetal echocardiography (“echo” for short) is performed by a pediatric cardiologist (a physician who specializes in fetal heart abnormalities). This non-invasive, high-resolution ultrasound procedure looks specifically at how your babies’ hearts are structured and function while in the womb.
Twin to twin transfusion syndrome stages
When twin-to-twin transfusion syndrome is diagnosed, a staging system is used to classify the severity of the condition. This system also known as the Quintero staging system 1 — helps to determine whether an intervention is needed and which treatment option(s) might be most appropriate. Here is an explanation of twin to twin transfusion syndrome stages:
- Stage 1: Polyhydramnios (too much amniotic fluid) in the recipient sac, oligohydramnios (little or no amniotic fluid) in the donor sac. The ultrasound shows an imbalance of amniotic fluid around the twins, but the donor twin’s bladder is still visible. The visibility of the bladder indicates the donor baby is receiving enough nutrients and fluid through the blood to produce urine.
- Stage 2: The ultrasound shows an imbalance of amniotic fluid around the twins, but the donor twin’s bladder is not visible. This finding indicates the bladder is empty — a sign that the baby has stopped making urine.
- Stage 3: In addition to the Stage 1 and 2 indicators, the ultrasound shows significant abnormalities in the flow of blood within the twins’ umbilical cords. Abnormal blood flow patterns, including:
- Absent/reversed umbilical artery end-diastolic velocity
- Reverse flow in ductus venosus
- Stage 4: In addition to the Stages 1-3 indicators, the recipient twin shows signs of heart failure (hydrops fetalis, or extra fluid within the baby). Hydrops or massive fluid retention puts both mother and twins at risk
- Stage 5: Death of one or both twins while still in the uterus.
Twin to twin transfusion syndrome treatment
Twin to twin transfusion syndrome management before birth
Prenatal management of babies with twin-to-twin transfusion syndrome involves monitoring the babies frequently with high-resolution fetal ultrasonography and fetal echocardiography. This testing allows doctors to measure the amount of amniotic fluid around your babies. It also allows doctors to assess how well blood is flowing within your babies’ umbilical cords, as well as within other blood vessels.
The key to twin to twin transfusion syndrome treatment is early diagnosis and intervention. What treatment option will be best for your babies will depend on the stage of the twin-to-twin transfusion syndrome and your babies’ gestational age at diagnosis. Several options are available, including the following:
- Expectant management: In situations where surgery is not yet indicated, close monitoring with periodic ultrasound examinations is used to evaluate the condition of both twins and look for signs of progression. This involves continued close ultrasound surveillance throughout the pregnancy. Doctors currently recommend expectant management for most Stage 1 twin-to-twin transfusion syndrome. In some cases, a follow-up fetal echocardiogram is used as well to look for signs of cardiac changes; these may sometimes be seen before other changes.
- Amnioreduction: This is a procedure that is used to remove excess fluid that has accumulated in the amniotic sac of the recipient (larger) twin. The procedure is similar to that of amniocentesis, with the doctor using “real-time” ultrasound images to guide a long, very fine needle into the uterus to withdraw the fluid. Removal of excess amniotic fluid from the larger twin (recipient) which may help ease any pain or discomfort experienced by the mother due to fluid buildup. This is a temporary treatment option and may need to be repeated. Doctors may recommend this intervention for Stage 1 twin-to-twin transfusion syndrome or when the twin-to-twin transfusion syndrome is diagnosed later in the pregnancy and fetoscopic laser photocoagulation (see below) is no longer an option.
- Fetoscopic laser photocoagulation (also called selective laser photocoagulation): This minimally invasive surgery that uses a laser to ablate (seal) blood vessels that are contributing to the abnormal flow of blood to the babies (Figures 3). This is typically the preferred treatment for twin-to-twin transfusion syndrome, depending on gestational age at presentation, location of the placenta and stage of twin-to-twin transfusion syndrome. Many studies have demonstrated that this procedure for the treatment of twin to twin transfusion syndrome is the most effective therapy for babies with advanced twin-to-twin transfusion syndrome.
- Selective cord occlusion: A minimally invasive surgery that stops the blood flow to one twin in order to maximize the outcome for the other twin. Selective cord occlusion procedures include radiofrequency ablation and bipolar cord coagulation. This is considered a last resort option when the disease is very advanced and the at-risk twin is not going to survive. This intervention can protect the co-twin from neurologic impairment and/or death.
- Delivery: If twin-to-twin transfusion syndrome is discovered later in the pregnancy, delivery of the babies may be the best option.
Figure 3. Fetoscopic laser photocoagulation
Footnote: An operative fetoscope contains a tiny camera that identifies connecting blood vessels between the twins. A tiny fiber then delivers laser energy that seals off the blood vessels so that no further exchange of blood occurs.
Twin to twin transfusion syndrome treatment after birth
Most babies with twin-to-twin transfusion syndrome are born prematurely, but main goal will be to have your babies delivered as close to your due date as possible. Babies who are treated with laser ablation are typically delivered around week 31 or 32 of the pregnancy.
Doctors will recommend that your babies be born at one of a specialized mother-baby center. This means that your babies will be born just a few feet down the hall from our newborn intensive care unit (NICU). If necessary, many of the physicians you have already met may be present during or immediately after your babies’ birth so doctors can care for your babies right away.
Twin to twin transfusion syndrome long term effects
The long-term prognosis for babies with twin-to-twin transfusion syndrome depends on how soon the condition is treated after it has developed, as well as the age of the babies at delivery. The earlier the babies receive treatment and the longer they stay in the womb before birth, the less likely they will experience complications.
When untreated, 90 percent of babies with advanced twin-to-twin transfusion syndrome do not survive to birth. That percentage is dramatically improved for babies who undergo fetoscopic laser photocoagulation. In almost 90 percent of those pregnancies, at least one baby will survive and be healthy after leaving the hospital newborn intensive care unit (NICU). Having both twins survive advanced twin-to-twin transfusion syndrome remains a challenge, however. Across all medical centers in the United States, about half of pregnancies treated for twin-to-twin transfusion syndrome end with two healthy babies.
Because of all the potential health issues associated with twin-to-twin transfusion syndrome, your babies will require long-term follow-up care. Specialist Fetal Care Centers have developed a detailed care plan for babies who experienced twin-to-twin transfusion syndrome during gestation. Your babies’ plan will be implemented by a comprehensive team of specialists, including a pediatrician (who will coordinate your babies’ overall care), a pediatric cardiologist, a developmental specialist, and any other caregiver your baby may require to manage any twin to twin transfusion syndrome long term effects.
- Quintero RA, Morales WJ, et al. Staging of twin-twin transfusion syndrome. J Perinatol. 1999 Dec;19(8Pt1):550-5 https://www.ncbi.nlm.nih.gov/pubmed/10645517[↩]