Contents
What is listeria
Listeriosis the illness from ingesting Listeria also known as listeria infection is a rare but potentially serious infection caused by eating food contaminated with the Gram-positive bacteria Listeria monocytogenes 1, 2, 3. The Listeria monocytogenes bacteria is common in the environment found in water and soil. Vegetables can become contaminated from the soil, and many farm animals and pets can also be carriers. Listeria has been found in uncooked meats, uncooked vegetables, unpasteurized milk, foods made from unpasteurized milk, and processed foods. Listeria is killed by pasteurization and cooking. There is a chance that contamination may occur in ready-to-eat foods such as hot dogs and deli meats because contamination may occur after cooking and before packaging 4. You can be infected by listeria if you eat contaminated food. Some foods are riskier than others – the riskiest are those eaten raw or inadequately cooked.
Unlike most other foodborne pathogens, Listeria monocytogenes can grow in food with fairly low moisture content and high salt concentration 5. Most importantly, Listeria monocytogenes grows at refrigeration temperatures, by contrast with many other foodborne pathogens 5. This ability to persist and multiply in the food environment makes Listeria monocytogenes especially difficult to control 6.
After exposure via eating contaminated food most healthy adults do not develop any symptoms, except in the case of pregnant women or people who have a weakened immune system 7. In healthy people, Listeria infections might cause febrile gastroenteritis, which is usually mild and self-limiting 5. In the case of pregnant women, after an incubation period of about three weeks pregnant women may suffer from a mild influenza-like illness, but it causes severe disease in the fetus or newborn baby 8. In that case, it can lead to death of the fetus (stillbirths) and consequent spontaneous abortions (miscarriages) or to congenital listeriosis in the newborn 9. Preterm birth is also a common consequence of listeriosis in pregnant women 10, 11.
In addition, some people with Listeria infections, most commonly adults 65 years and older and people with weakened immune systems, develop severe infections of the bloodstream (causing sepsis) or brain (causing meningitis or encephalitis) and thereby cause lifelong consequences and even death 12, 13, 14. Listeria infections can sometimes affect other parts of the body, including bones, joints, and sites in the chest and abdomen. Fortunately, all clinical presentations are treatable with prolonged courses of antibiotics, but the prognosis of the most serious ones is poor. The Centers for Disease Control and Prevention (CDC) estimated 1,600 people get listeriosis each year, and about 260 die 4. Early recognition and treatment with ampicillin, penicillin G, or trimethoprim-sulfamethoxazole are very effective in treating Listeria monocytogenes 15.
The Centers for Disease Control and Prevention (CDC) estimates that Listeria is the third leading cause of death from food poisoning in the United States. The annual incidence of laboratory-confirmed listeriosis in the United States is about 0.24 cases per 100,000 population, based on active surveillance by the CDC. About 1,600 people get sick from Listeria each year, and about 260 die. Listeria is the 3rd leading cause of death from food poisoning. Nearly everyone with listeriosis is hospitalized. The case-fatality rate is about 20%. Nearly one-quarter of pregnancy-associated cases result in fetal loss or death of the newborn.
At least 90% of people who get Listeria infections are pregnant women, newborns, older adults, and people with weakened immune systems. Pregnant women are 10 times more likely than other people to get listeriosis.
Although the CDC states that pregnant women are 10 times more likely to become infected than non-pregnant healthy adults, the number of cases of listeriosis in pregnant women is about 17% 16.
- About 1 in 6 cases of listeriosis are associated with pregnancy.
- Pregnant women are 10 times more likely than other people to get Listeria infection.
- Pregnant Hispanic women are 24 times more likely than other people to get Listeria infection.
- Pregnant women with a Listeria infection can pass the infection to their unborn babies.
- Listeria infection can cause miscarriages, stillbirths, and preterm labor.
- Listeria infection can cause serious illness and even death in newborns.
- Older adults are at particular risk – more than half of all Listeria infections occur in people 65 and older.
- Adults who are 65 years and older are 4 times more likely than other people in the United States to get Listeria infections.
- People with weakened immune systems due to underlying medical conditions, such as cancer, diabetes, liver or kidney disease, alcoholism, and HIV or AIDS, are more likely to get a Listeria infection. Treatments that make it more difficult for the body to fight off illness, such as steroids and chemotherapy, also can increase the chance of Listeria infection.
- People with cancer are 10 times more likely than other people to get Listeria infection.
- People on dialysis are 50 times more likely than other people to get Listeria infection.
Most people found to have Listeria infection require hospital care and about 1 in 5 people with the infection die.
Listeria is a deadly germ that is hard to control because Listeria monocytogenes bacteria are widespread in the environment and listeria may be found in the soil, water, on animals and in animal waste. Listeria monocytogenes bacteria can sometimes contaminate certain high risk foods that have not been thoroughly cooked or properly prepared or stored. Listeria can contaminate many foods that you don’t usually cook, like deli meats, cheeses and sprouts. Some foods you might not suspect can be contaminated with Listeria and cause sickness and outbreaks, such as cantaloupe and celery. Listeria can hide unnoticed in the equipment or appliances where food is prepared, including in factories and grocery stores. Listeria is a hardy germ that can even grow on foods that are refrigerated.
Listeriosis is usually caught from eating food containing Listeria monocytogenes bacteria. When someone eats food contaminated with Listeria, sickness or miscarriage may not occur until weeks later when it is difficult to identify which food was the source.
Foods that are most likely to have Listeria include:
- Unpasteurized milk and foods made with it. If milk is pasteurized, it’s been heated to kill germs. Look for the word “pasteurized” on the label.
- Soft cheeses, like feta, Brie, Camembert, Roquefort and Mexican-style cheeses, like queso fresco, queso blanco, Panela and Asadero
- Deli meat, hot dogs, juice from hot dogs and dry sausages that are chilled or at room temperature
- Unwashed fruits, vegetables or sprouts
- Cold salads from delis or salad bars
- Refrigerated patés or meat spreads (Canned meat spreads are safe.)
- Refrigerated smoked seafood, including nova-style, lox, kippered, smoked and jerky
While Listeria infection is uncommon in healthy people, people at greater risk of infection include:
- pregnant women and their unborn or newborn babies
- people whose immune system has been weakened due to chronic illness such as cancer, diabetes or alcoholism
- people taking medications that impair immunity such as steroids and anti-cancer drugs.
Listeriosis is not normally transmitted between people, although it can pass from a pregnant woman to her unborn baby, where listeriosis can cause miscarriage, stillbirth and premature birth, low birthweight and septicemia (whole body infection) and pneumonia in newborn babies.
Foods to avoid or limit during pregnancy
Not every food is safe to eat during pregnancy. Some foods may be harmful to you or your baby because of the way they’re cooked or because of germs or chemicals they contain.
Here’s why:
- Raw meat, fish and eggs can contain harmful germs that can give you food poisoning, like salmonella infection. Cooking them fully kills the germs, which helps keep you and your baby from getting sick.
- Many dairy products, like milk, eggs and cheese, are pasteurized. This means they’re heated to kill any bad germs. If the product label doesn’t say “pasteurized,” pick a different product. Unpasteurized dairy products can give you food poisoning, like listeriosis.
- Some foods contain chemicals, like caffeine or mercury. You can pass these harmful chemicals to your baby during pregnancy.
You can get listeria from lots of types of food, here is a list of foods that are completely off limits during pregnancy:
DON’T eat these foods during pregnancy. They can be really harmful to you and your baby.
Certain meats and fish
- Raw or undercooked meat, including beef, poultry and pork. This includes hotdogs and deli meat (like ham or bologna).
- Raw fish, especially shellfish
- Fish that can be high in mercury, like shark, swordfish, king mackerel and tilefish. Always check with your local health department before you eat any fish you catch yourself.
- Refrigerated pates, meat spreads or smoked seafood
- Chilled ready-to-eat foods, like prepacked sandwiches, pâté and deli meats
Certain dairy products
- Raw or lightly cooked eggs or foods made with them. This includes cake batter and raw cookie dough.
- Soft-scrambled eggs
- Unpasteurized juice
- Unpasteurized milk or any foods made with them
- Unpasteurized soft cheeses, such as brie, feta, Camembert, Roquefort, queso blanco, queso fresco and Panela
Other
- Raw sprouts, especially alfalfa sprouts
- Herbal products, like pills and teas. Herbal products are made from herbs, which are plants used in cooking or medicine. We don’t know enough about herbal products to know if they’re safe to use during pregnancy. So it’s best not to use them while you’re pregnant.
- Nonfood items, like clay, starch, paraffin or coffee grounds. Tell your provider if you crave anything like this that’s not food.
Foods should you LIMIT during pregnancy
These foods are OK to eat during pregnancy in limited amounts:
- Fish that have small amounts of mercury. Mercury is a metal that can harm your baby. Fish get mercury from the water they swim in and from eating other fish that have mercury in them. By eating fish that contain mercury, you can pass the metal to your baby during pregnancy. This can cause brain damage and affect your baby’s hearing and vision. During pregnancy, eat 8 to 12 ounces a week of fish that doesn’t have a lot of mercury, including shrimp, salmon, pollock, catfish and canned light tuna. It’s OK to eat 6 ounces a week of albacore (white) tuna.
- Food and drinks that have caffeine. Limit the caffeine you get each day to 200 milligrams. This is about the amount in 1½ 8-ounce cups of coffee or one 12-ounce cup of coffee. Caffeine amounts in coffee vary a lot and depend on things, like the brand you drink, how it’s made and the size of the cup. Check to see how many ounces your cup has, especially if you’re buying a cup of coffee or tea. Instead of drinking regular coffee, try coffee that’s decaffeinated (has a smaller amount of caffeine). Caffeine is also found in tea, chocolate, soda and some over-the-counter medicine. Read labels on food, drinks and medicine to know how much caffeine you’re getting.
You can also catch listeria from:
- someone else who has it – for example, if you eat food they’ve handled when they haven’t washed their hands
- close contact with farm animals – especially sheep and cows that are giving birth
Listeriosis symptoms
In most people, listeriosis has no symptoms or only causes mild symptoms for a few days, such as:
- a high temperature of 100.4 °F (38 °C) or above
- muscle aches and pains
- chills
- feeling sick or vomiting
- diarrhea
- stiff neck and sensitivity to light
- confusion and drowsiness
- nausea (feeling sick)
- diarrhea.
If you have these symptoms and you are NOT pregnant, you can usually look after yourself at home.
- Symptoms usually occur around 3 weeks after eating contaminated food but the interval can vary between a few days and 2 months.
- Healthy people and pregnant women may have mild or no symptoms, but Listeria infection may still result in miscarriage, premature birth or stillbirth.
- In people at risk, Listeria infection can result in serious illnesses including meningitis (infection of the membrane surrounding the brain and spinal cord) and septicemia (infection of the blood that can spread widely through the body).
- Babies born with Listeria infection can develop septicemia or meningitis.
- If you are pregnant or have a weakened immune system and develop symptoms consistent with Listeria infection, see your doctor as soon as possible.
Footnote: This chart shows those groups most at risk for Listeria food poisoning: Pregnant women and their newborns; older adults, and people with weakened immune systems. It also shows that when it comes to Listeria, some foods are more risky than others. Some foods where Listeria is known to hide include raw sprouts, raw milk (unpasteurized), deli meats and hot dogs (cold, uncooked), soft cheeses and smoked seafood.
See your doctor if you’re pregnant and think you have listeriosis
You may need a blood test to check for the infection. You’ll be given antibiotics if you have listeriosis because it could cause serious problems like a miscarriage if not treated.
Ask for an urgent appointment if:
- you think you have listeriosis and you have a condition that weakens your immune system (like diabetes)
- you think you have listeriosis and you’re having treatment that weakens your immune system (like chemotherapy)
- you think your baby might have listeriosis
If it’s not treated, severe listeriosis can cause serious infections like meningitis in babies and people with a weak immune system.
What is listeria outbreak?
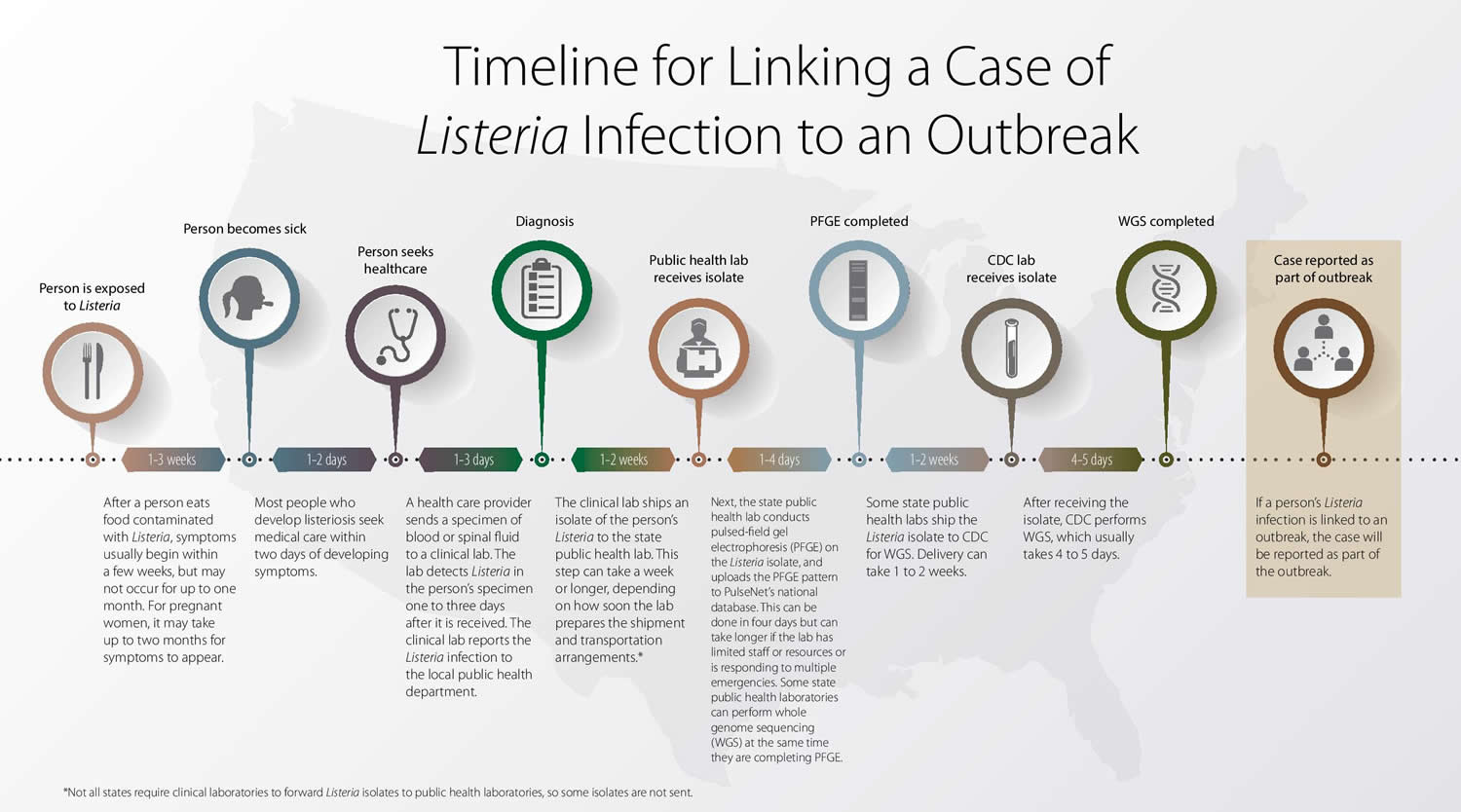
When two or more people get listeriosis from the same contaminated food or drink, the event is called a listeria outbreak. Public health officials investigate outbreaks to control them, so more people do not get sick, and to learn how to prevent similar outbreaks from happening in the future.
A series of events occurs from when someone eats a food contaminated with Listeria to when public health officials can determine that the person is part of an outbreak. This typically takes about 2–10 weeks but can take much longer. So the number of cases linked to an outbreak can continue to increase as more cases are found. Some of them may even have occurred years before.
Figure 1. Timeline for Linking a Case of Listeria Infection to an Outbreak
[Source 17]The following factors contribute to the time it takes to recognize a case of Listeria infection (listeriosis) and report that it is part of an outbreak:
- Time to illness (typically 1–3 weeks): After a person eats food contaminated with Listeria, symptoms usually begin within a few weeks, but may not occur for up to one month. For pregnant women, it may take up to two months for symptoms to appear.
- Time to seek health care (typically 2 days): Most people who develop listeriosis seek medical care within two days of developing symptoms.
- Time to diagnosis (typically 3 days): A health care provider examines the person and sends a specimen of blood or spinal fluid to a clinical lab. The lab detects Listeria in the person’s specimen one to three days after it is received. The clinical lab reports the Listeria infection to the local public health department.
- Time to ship isolate to public health lab (typically 7 days): The clinical lab ships an isolate of the person’s Listeria to the state public health lab. This step can take a week or longer, depending on how soon the lab prepares the shipment and transportation arrangements.*
- Time to complete pulsed-field gel electrophoresis (typically 4 days): Next, the state public health lab conducts pulsed-field gel electrophoresis (a technique used to generate DNA fingerprints of bacteria) on the Listeria isolate, and uploads the pulsed-field gel electrophoresis pattern to PulseNet‘s national database. This can be done in four days but can take longer if the lab has limited staff or resources or is responding to multiple emergencies. Some state public health labs can perform whole genome sequencing at the same time they are completing pulsed-field gel electrophoresis.
- Time to ship to the Centers for Disease Control and Prevention (CDC) lab (typically 1–2 weeks): Some state public health labs ship the Listeria isolate to CDC for whole genome sequencing. Delivery can take 1 to 2 weeks.
- Time to perform whole genome sequencing and analysis (typically 5 days): After receiving the isolate, CDC performs whole genome sequencing, which usually takes 4 to 5 days.
- Report case as part of outbreak: If a person’s Listeria infection is linked to an outbreak, the case will be reported as part of the outbreak.
*Not all states require clinical labs to forward Listeria isolates to public health labs, so some isolates are not sent.
Listeria in pregnancy
Pregnant women and their newborns are much more likely to get a Listeria infection 18. About 1 in 6 cases of listeriosis are associated with pregnancy.
- Pregnant women are 10 times more likely than other people to get Listeria infection.
- Pregnant Hispanic women are 24 times more likely than other people to get Listeria infection.
- Pregnant women with a Listeria infection can pass the infection to their unborn babies.
- Listeria infection can cause miscarriages, stillbirths, and preterm labor.
- Listeria infection can cause serious illness and even death in newborns.
In general, you can protect yourself from listeriosis by following these guidelines:
- Avoid eating cheese made from raw (unpasteurized) milk.
- Soft cheeses made with pasteurized milk, including commercial cottage cheese, cream cheese, and mozzarella, are generally regarded as safe. However, some soft cheeses made with pasteurized milk, including Hispanic-style soft cheeses, have become contaminated with Listeria during processing. This could occur again.
- Avoid raw (unpasteurized) milk and products made from it, such as cheese, ice cream, and yogurt. Look for the word “pasteurized” on the label. If in doubt, don’t buy it!
- Do not eat raw or lightly cooked sprouts of any kind (including alfalfa, clover, radish, and mung bean sprouts).
- Eat cut melon right away or refrigerate it at 40° F (4.4 °C) or colder and for no more than 7 days. Throw away cut melons left at room temperature for more than 4 hours.
- Avoid eating hot dogs, lunch meats, cold cuts, other deli meats (such as bologna), or fermented or dry sausages unless they are heated to an internal temperature of 165°F (73.9 °C) or until steaming hot just before serving. Don’t let juice from hot dog and lunch meat packages get on other foods, utensils, and food preparation surfaces. Wash hands after handling hot dogs, lunch meats, and deli meats.
- Do not eat refrigerated pâté or meat spreads from a deli or meat counter or from the refrigerated section of a store. Foods that do not need refrigeration, like canned or shelf-stable pâté and meat spreads, are safe to eat. Refrigerate these foods after opening.
- Do not eat refrigerated smoked seafood unless it is in a cooked dish, such as a casserole, or unless it is canned or shelf-stable.
If you are pregnant and Hispanic, your risk of getting listeriosis is even greater. Pregnant Hispanic women are about 24 times more likely than other people to get listeriosis. Be aware that some Hispanic-style cheeses, such as queso fresco, that were made from pasteurized milk but were contaminated when the cheese was being made, have caused Listeria infections. Hispanic-style soft cheeses include queso fresco, queso blanco, queso blando, queso Cotija, queso panela, queso ranchero, cuajada en terrón, and others. Learn about additional ways to reduce your risk for listeriosis.
If you are pregnant and have a fever and other symptoms of possible listeriosis, such as fatigue and muscle aches, within two months after eating a possibly contaminated food, you should seek medical care and tell the doctor about eating possibly contaminated food. If you are infected, your health care provider can give you antibiotics that can protect your fetus or newborn. If you ate food possibly contaminated with Listeria and do not feel sick, most experts believe you do not need tests or treatment, even if you are in a group that is more likely to get listeriosis.
Listeria symptoms in pregnancy
Pregnant women typically experience only fever and other “flu-like” symptoms, such as fever, myalgia (muscle ache), backache, and headache, often preceded by diarrhea or other gastrointestinal symptoms 19. Some pregnant women with Listeria infection have no symptoms. The consequences for the baby, however, may be devastating. Listeria infections during pregnancy can lead to miscarriage, stillbirth (baby may die unexpectedly before birth), premature delivery, meningitis, life-threatening infection of the newborn within the first few days after birth or death.
- Some neonates with listeriosis develop granulomatosis infantiseptica, a severe disorder involving the internal organs and skin.
- Neonatal listeriosis is classified as early (within 6 days of birth) or late onset (7–28 days after birth).
- Early-onset neonatal listeriosis is usually acquired through transplacental transmission.
- The sources of late-onset listeriosis are less clear; they may involve exposure during delivery or nosocomial exposure.
As in adults, the signs and symptoms of a listeria infection in a newborn can be subtle, but may include:
- Little interest in feeding
- Irritability
- Fever
- Vomiting
Listeria in pregnancy treatment and management
The following American College of Obstetricians and Gynecologists recommendations provide guidance for the management of pregnant women with presumptive exposure to listeria in three clinical scenarios: women who are 1) asymptomatic, 2) mildly symptomatic but afebrile, and 3) febrile with or without other symptoms of listeriosis (see Figure 2).
Figure 2. Listeria in pregnancy management and treatment
[Source 20]Asymptomatic
No testing, including blood and stool cultures, or treatment is indicated for an asymptomatic pregnant woman who reports consumption of a product that was recalled or implicated during an outbreak of listeria contamination. An asymptomatic patient should be instructed to return if she develops symptoms of listeriosis within 2 months of eating the recalled or implicated product. There is no reason to alter or begin fetal surveillance in asymptomatic women with known or presumptive exposure to listeria.
Mildly Symptomatic but Afebrile
There are no data to guide the management of an exposed, afebrile pregnant woman with mild symptoms that do not strongly suggest listeriosis. A pregnant woman who ate a product that was recalled because of listeria contamination and who is afebrile but has signs and symptoms consistent with a minor gastrointestinal or flu-like illness (such as mild myalgia, mild nausea, vomiting, or diarrhea) can be managed expectantly (i.e, the same as for an exposed, asymptomatic pregnant woman). This is a reasonable approach that limits low-yield testing. Alternatively, such a patient could be tested with blood culture for listeria, but if such a course is elected, specific instruction should be given to the microbiology laboratory. Because the morphology of listeria resembles that of diphtheroids, it may be mistaken for a contaminant 19. Therefore, the laboratory should be alerted to the clinical suspicion of listeriosis. If such diagnostic testing is performed, some experts would withhold antibiotic therapy unless the culture yielded listeria. Others would initiate antibiotic therapy, although no effectiveness data exist to help clinicians and patients evaluate the risks and benefits of such a treatment choice. If testing is undertaken and the blood culture yields listeria, standard antimicrobial treatment for listeriosis, typically including intravenous ampicillin, would be indicated (see following section). Assessments of fetal well-being should be addressed on an individualized basis with consideration given to the degree of concern for infection and the patient’s clinical status.
Febrile With or Without Other Symptoms Consistent With Listeriosis
An exposed pregnant woman with a fever higher than 38.1°C (100.6°F) and signs and symptoms consistent with listeriosis for whom no other cause of illness is known should be simultaneously tested and treated for presumptive listeriosis.
Diagnosis is made primarily by blood culture. Placental cultures should be obtained in the event of delivery. If blood cultures are negative after the recommended antibiotic regimen has begun, the decision about whether or not to continue antibiotics should be made using clinical judgment combined with consultation(s) with an infectious disease specialist, a maternal–fetal medicine specialist, or both.
Listeria survives and grows within host cells, so infection does not respond favorably to bacteriostatic antibiotics. The antimicrobial regimen of choice for treatment of listeriosis is high-dose intravenous ampicillin (at least 6 g/day) for nonallergic patients for at least 14 days 21. Frequently, gentamicin is added to the treatment regimen because it has demonstrated synergism with ampicillin 22, although not all authorities agree that this adds to the effectiveness of the regimen, especially given the toxicity of gentamicin 21. Women who are allergic to penicillin, ampicillin, or both present a clinical conundrum; trimethoprim with sulfamethoxazole is the generally recommended alternative to ampicillin 21. The Centers for Disease Control and Prevention considers listeriosis a nationally notifiable disease, and once diagnosis is confirmed, health care providers should contact their state public health departments to comply with local requirements for reporting.
Although blood cultures are the standard for diagnosis in cases of fever and symptoms consistent with listeriosis, if an amniocentesis has been performed, it usually reveals meconium staining and gram-positive rods 23. This information may help guide management when the diagnosis is uncertain 24.
Initiating a program of fetal surveillance seems prudent for women in whom listeriosis is diagnosed or strongly suspected because of exposure and fever with or without other symptoms, although studies and data do not exist to point to one best plan for such testing.
Stool Culture
In the aforementioned clinical scenarios, management guidance does not include stool culture for listeria because such cultures have not been validated as a screening tool and are not recommended for the diagnosis of listeriosis. Ingestion of listeria occurs frequently because the bacterium is commonly present in the environment. Therefore, intermittent fecal carriage and shedding of listeria are also frequent (approximately 5% in unselected populations, but substantial variation exists) and rarely indicative of infection 25. Furthermore, stool culture for listeria may have low sensitivity and is not available in most clinical laboratories.
What causes listeriosis?
Listeria bacteria can be found in soil, water and animal feces. Humans typically are infected by eating:
- Raw vegetables that have been contaminated from the soil or from contaminated manure used as fertilizer
- Contaminated animal meat
- Unpasteurized milk or foods made with unpasteurized milk
- Certain processed foods — such as soft cheeses, hot dogs and deli meats that have been contaminated after processing
Unborn babies can contract a listeria infection from the mother via the placenta.
Listeria monocytogenes bacteria
Listeria monocytogenes is a facultatively anaerobic, rod-shaped, gram-positive bacterium that can be readily isolated in standard bacterial culture of normally sterile body sites. It is widespread in the environment and can be isolated from soil, water, and decaying vegetation. It is a hardy organism that can withstand a wide range of conditions including freezing, drying, heat, and relatively high levels of acid, salinity, and alcohol. Unlike most foodborne pathogens, it can grow at standard refrigerator temperature (40°F), which makes it a particular problem in ready-to-eat foods that are not cooked before eating.
Serotyping differentiates isolates of Listeria below the species level. Listeria serotypes are designated based on the immunoreactivity of two cell surface structures, the O and H antigens. Twelve serotypes of L. monocytogenes (1/2a, 1/2b, 1/2c, 3a, 3b, 3c, 4a, 4b, 4c, 4d, 4e, and 7) are recognized, three of which (1/2a, 1/2b, and 4b) cause most (95%) human illness; serotype 4b is most commonly associated with outbreaks.
Figure 3. Listeria monocytogenes bacteria
Risk factors for listeriosis
Pregnant women and people who have weak immune systems are at highest risk of contracting a listeria infection.
Pregnant women and their babies
Pregnant women are significantly more susceptible to listeria infections than are other healthy adults. Although a listeria infection may cause only a mild illness in the mother, consequences for the baby may include:
- Miscarriage
- Stillbirth
- Premature birth
- A potentially fatal infection after birth
People who have weak immune systems
This category includes people who:
- Are older than 60
- Have AIDS
- Are undergoing chemotherapy
- Have diabetes or kidney disease
- Take high-dose prednisone or certain rheumatoid arthritis drugs
- Take medications to block rejection of a transplanted organ
Listeria infection complications
Most listeria infections are so mild they may go unnoticed. However, in some cases, a listeria infection can lead to life-threatening complications — including:
- A generalized blood infection (septicemia)
- Inflammation of the membranes and fluid surrounding the brain (meningitis)
Complications of a listeria infection may be most severe for an unborn baby. Early in pregnancy, a listeria infection may lead to miscarriage. Later in pregnancy, a listeria infection may lead to stillbirth, premature birth or a potentially fatal infection in the baby after birth — even if the mother becomes only mildly ill.
Listeria prevention
There are some simple things you can do to reduce your risk of getting listeriosis:
DO
- Wash your hands regularly with soap and water
- Store ready-to-eat foods as recommended by the manufacturer
- Make sure all hot food is steaming hot all the way through
- Use a thermometer to make sure your refrigerator is 40°F (4.4 °C) or lower and your freezer is 0°F (minus 17.8°C) or lower.
- Keep raw meat away from fresh produce and other ready-to-eat food, to avoid contamination.
- Thaw or marinate foods in the refrigerator, never on the counter or in the kitchen sink.
- Wash fruits and vegetables (even if you plan to peel them), but do not wash meat, poultry or eggs!
- Use separate cutting boards for raw produce and for raw meat, poultry, seafood, and eggs.
- Use a food thermometer to be sure food is cooked to its proper temperature.
- Refrigerate leftovers within 2 hours in shallow covered containers and use within 3-4 days.
- Know when to throw food out.
DON’T
- eat food after its use-by date, even if it looks and smells normal
Foods to avoid if you’re pregnant
If you’re pregnant, you should avoid eating foods that have the highest risk of causing listeriosis.
There are some foods to avoid or take care with when you’re pregnant as they might make you ill or harm your baby.
Make sure you know the important facts about which foods you should avoid or take precautions with when you’re pregnant.
- Avoid some raw or partially cooked eggs.
- Avoid all types of pâté, including vegetable pâtés, as they can contain listeria.
- Only consume pasteurized milk and milk products, including soft cheese, ice cream, and yogurt. Look for the word “pasteurized” on the label. If in doubt, don’t eat it!
Cheeses to avoid in pregnancy
- Soft cheeses with white rinds
Don’t eat mould-ripened soft cheese (cheeses with a white rind) such as brie and camembert. This includes mould-ripened soft goats’ cheese, such as chèvre. These cheeses are only safe to eat in pregnancy if they’ve been cooked.
- Soft blue cheeses
You should also avoid soft blue-veined cheeses such as danish blue, gorgonzola and roquefort. Soft blue cheeses are only safe to eat in pregnancy if they’ve been cooked.
It’s advised pregnant women avoid some soft cheeses because they’re less acidic than hard cheeses and contain more moisture, which means they can be an ideal environment for harmful bacteria, such as listeria, to grow in.
Although infection with listeria (listeriosis) is rare, it’s important to take special precautions in pregnancy – even a mild form of the illness in a pregnant woman can lead to miscarriage, stillbirth or severe illness in a newborn baby.
Avoid raw or undercooked meat in pregnancy
Do not eat raw or undercooked meat, including meat joints and steaks cooked rare, because of the potential risk of toxoplasmosis.
Cook all meat and poultry thoroughly so it’s steaming hot and there’s no trace of pink or blood – especially with poultry, pork, sausages and minced meat, including burgers.
Wash all surfaces and utensils thoroughly after preparing raw meat to avoid the spread of harmful bugs. Wash and dry your hands after touching or handling raw meat.
Toxoplasmosis is an infection caused by a parasite found in raw and undercooked meat, unpasteurised goats’ milk, soil, cat poo, and untreated water.
If you’re pregnant, the infection can damage your baby, but it’s important to remember toxoplasmosis in pregnancy is very rare.
Toxoplasmosis often has no symptoms, but if you feel you may have been at risk, discuss it with your doctor or obstetrician. If you’re infected while you’re pregnant, treatment for toxoplasmosis is available.
DON’T eat these foods during pregnancy
They can be really harmful to you and your baby.
Certain meats and fish
- Raw or undercooked meat, including beef, poultry and pork. This includes hotdogs and deli meat (like ham or bologna).
- Raw fish, especially shellfish
- Fish that can be high in mercury, like shark, swordfish, king mackerel and tilefish. Always check with your local health department before you eat any fish you catch yourself.
- Refrigerated pates, meat spreads or smoked seafood
- Chilled ready-to-eat foods, like prepacked sandwiches, pâté and deli meats
Certain dairy products
- Raw or lightly cooked eggs or foods made with them. This includes cake batter and raw cookie dough.
- Soft-scrambled eggs
- Unpasteurized juice
- Unpasteurized milk or any foods made with them
- Unpasteurized soft cheeses, such as brie, feta, Camembert, Roquefort, queso blanco, queso fresco and Panela
Other
- Raw sprouts, especially alfalfa sprouts
- Herbal products, like pills and teas. Herbal products are made from herbs, which are plants used in cooking or medicine. We don’t know enough about herbal products to know if they’re safe to use during pregnancy. So it’s best not to use them while you’re pregnant.
- Nonfood items, like clay, starch, paraffin or coffee grounds. Tell your provider if you crave anything like this that’s not food.
Caffeine in pregnancy
High levels of caffeine can result in babies having a low birthweight, which can increase the risk of health problems in later life. Too much caffeine can also cause miscarriage.
Caffeine is naturally found in lots of foods, such as coffee, tea (including green tea) and chocolate, and is added to some soft drinks and energy drinks.
Some cold and flu remedies also contain caffeine. Talk to your midwife, doctor or pharmacist before taking these remedies.
You don’t need to cut out caffeine completely, but don’t have more than 200mg a day.
The approximate amount of caffeine found in food and drinks is:
- one mug of instant coffee: 95mg
- one mug of filter coffee: 140mg
- one mug of tea: 75mg
- one can of cola: 40mg
- one 250ml can of energy drink: 80mg (larger cans of energy drink may have up to 160mg caffeine)
- one 50g bar of plain (dark) chocolate: most US brands contain less than 25mg
- one 50g bar of milk chocolate: most US brands contain less than 10mg
So, if you have one can of cola and one mug of filter coffee, for example, you have reached almost 200mg of caffeine. Don’t worry if you occasionally have more than this amount – the risks are small.
To cut down on caffeine, try decaffeinated tea and coffee, fruit juice or mineral water instead of regular tea, coffee, cola and energy drinks.
Listeria signs and symptoms
Listeriosis can cause a variety of symptoms, depending on the person and the part of the body affected. Listeria can cause fever and diarrhea similar to other foodborne germs, but this type of Listeria infection is rarely diagnosed. Symptoms in people with invasive listeriosis, meaning the bacteria has spread beyond the gut, depend on whether the person is pregnant.
Signs and symptoms of listeriosis usually start a few days after eating food contaminated by Listeria, but they may not happen for up to 2 months. They’re usually mild and flu-like.
People with invasive listeriosis usually report symptoms starting 1 to 4 weeks after eating food contaminated with Listeria; some people have reported symptoms starting as late as 70 days after exposure or as early as the same day of exposure.
If you ate food possibly contaminated with Listeria and do not feel sick, most experts believe you do not need tests or treatment. Talk with your medical provider if you have questions about what to do after eating possibly contaminated food.
Your health care provider can test your blood to see if you have listeriosis. Listeriosis is usually diagnosed when a bacterial culture (a type of laboratory test) grows Listeria monocytogenes from a body tissue or fluid, such as blood, spinal fluid, or the placenta.
In most people, listeriosis has no symptoms or only causes mild symptoms for a few days, such as:
- a high temperature of 100.4 °F (38 °C) or above
- muscle aches and pains
- chills
- feeling sick or vomiting
- diarrhea
- stiff neck and sensitivity to light
- confusion and drowsiness
- nausea (feeling sick)
- diarrhea.
Symptoms may begin a few days after you’ve eaten contaminated food, but it may take as long as 30 days or more before the first signs and symptoms of infection begin.
If the listeria infection spreads to your nervous system, signs and symptoms may include:
- Being confused or having trouble with balance
- Fever or chills
- Headache
- Muscle aches
- Nausea (feeling sick to your stomach) or diarrhea
- Seizures
- Stiff neck
See your doctor right away if you have any of the above symptoms.
Call your local emergency number or go to emergency room if you get:
- a severe headache and stiff neck
- discomfort when looking at bright lights
- fits (seizures)
- sudden confusion
- a rash that doesn’t fade when a glass is rolled over it – the rash may be blotchy, like bruises or small red pinpricks
These could be symptoms of meningitis caused by listeriosis, which needs to be treated in hospital straight away.
Listeriosis diagnosis
A blood test is often the most effective way to determine whether you have a listeria infection. In some cases, samples of urine or spinal fluid may be tested as well.
Listeriosis is usually diagnosed when a bacterial culture (a type of laboratory test) grows Listeria from a body tissue or fluid, such as blood, spinal fluid, or the placenta.
According to the CDC, stool cultures are neither sensitive nor specific for diagnosing Listeria monocytogenes.
Listeriosis treatment
Treatment of listeria infection varies, depending on the severity of the signs and symptoms. Most people with mild symptoms require no treatment. More-serious infections can be treated with antibiotics.
During pregnancy, prompt antibiotic treatment may help keep the infection from affecting the baby (see Listeria in Pregnancy treatment and management section above). Newborns who have a listeria infection may receive a combination of antibiotics.
Little scientific evidence is available to inform decisions regarding management of people at elevated risk of invasive listeriosis who have been exposed to Listeria monocytogenes and who are either asymptomatic or have mild symptoms that could be consistent with early Listeria infection.
Patient management decisions for asymptomatic or mildly symptomatic people are appropriately made on a case-by-case basis, informed by clinical judgment and the likelihood of exposure of the patient. Consultation with a specialist in infectious disease may be considered.
Exposed, asymptomatic
Most experts believe that no testing or treatment is indicated for an asymptomatic person with elevated risk of invasive listeriosis who ate a product recalled because of Listeria monocytogenes contamination. Such a patient should be instructed to return for medical treatment if he or she develops symptoms of listeriosis within two months after eating the recalled product. Symptoms may include fever and myalgias, often preceded by diarrhea or other gastrointestinal symptoms. In older adults and immunocompromised people, symptoms of listeriosis can include headache, stiff neck, confusion, loss of balance, and convulsions.
Exposed, afebrile, mild symptoms
A person with elevated risk of invasive listeriosis who ate a product recalled because of Listeria monocytogenes contamination, who is afebrile and has signs and symptoms consistent with a minor gastrointestinal or flu-like illness, such as mild myalgias or mild nausea or diarrhea, could be managed expectantly; this approach limits low-yield testing. Alternatively, such a patient could be tested with blood culture. If diagnostic tests are performed, some experts would withhold antibiotic therapy unless cultures yielded Listeria monocytogenes. Others would initiate antibiotic therapy while culture results were pending and then stop treatment if the cultures were negative. The antibiotic regimen could consist of oral ampicillin or amoxicillin, although it is important that both the clinician and the patient know that no effectiveness data exist for this scenario. If the blood culture yielded Listeria, standard antimicrobial treatment for listeriosis, typically including IV ampicillin and gentamicin, would be indicated.
Exposed, fever and symptoms consistent with invasive listeriosis
An exposed person with elevated risk of invasive listeriosis with fever (>100.6° F, >38.1° C) and signs and symptoms consistent with listeriosis, for whom no other cause of illness is known, should be tested and treated for presumptive listeriosis.
- Diagnostic testing should include blood culture and other tests, such as culture of cerebrospinal fluid, as indicated by the clinical presentation.
- The antimicrobial regimen should be the standard therapy for listeriosis, typically including IV ampicillin and gentamicin for 14 to 21 days for nonallergic patients.
- If blood culture is negative and symptoms resolve, antibiotic therapy may be discontinued.
Exposed, history of symptoms in past 4 weeks, currently asymptomatic
Most experts believe that no testing or treatment is indicated for an asymptomatic person with elevated risk of invasive listeriosis who ate a product recalled because of L. monocytogenes contamination and experienced symptoms that have resolved. Any such patient should be instructed to return for medical care if he or she develops symptoms of listeriosis within 2 months after eating the recalled product.
Note: The suggested framework above does not include stool culture for Listeria monocytogenes. Stool culture has not been evaluated as a screening tool and is not recommended for the diagnosis of listeriosis. Ingestion of food contaminated with Listeria occurs frequently because the bacterium is commonly present in the environment. Therefore, intermittent fecal carriage and shedding of Listeria is also frequent (about 5% in unselected populations, but substantial variation exists) and rarely indicative of infection. Stool culture for Listeria may also have low sensitivity and is rarely available in clinical laboratories. Serologic testing for Listeria has poor sensitivity and specificity and is not recommended for diagnosis of listeriosis in individual patients.
Listeriosis prognosis
Studies have shown that Listeria monocytogenes is the third leading cause of death from food-borne illnesses in the United States, with approximately 260 deaths annually 26. Mortality rates with confirmed Listeria monocytogenes infection are around 20% to 30% but can be higher depending on patient status and comorbidities 27. Nearly 25% of pregnancy-related cases have poor outcomes including fetal loss or death of the newborn 28. Early recognition and treatment with ampicillin, penicillin G, or trimethoprim-sulfamethoxazole are very effective in treating Listeria monocytogenes.
- de Noordhout CM, Devleesschauwer B, Angulo FJ, Verbeke G, Haagsma J, Kirk M, et al. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(11):1073–1082. doi: 10.1016/S1473-3099(14)70870-9[↩]
- Wilking H, Lachmann R, Holzer A, Halbedel S, Flieger A, Stark K. Ongoing High Incidence and Case-Fatality Rates for Invasive Listeriosis, Germany, 2010–2019. Emerg Infect Dis. 2021;27(9):2485–2488. doi: 10.3201/eid2709.210068[↩]
- Schlech WF 3rd, Lavigne PM, Bortolussi RA, Allen AC, Haldane EV, Wort AJ, Hightower AW, Johnson SE, King SH, Nicholls ES, Broome CV. Epidemic listeriosis–evidence for transmission by food. N Engl J Med. 1983 Jan 27;308(4):203-6. doi: 10.1056/NEJM198301273080407[↩]
- Listeria (Listeriosis). https://www.cdc.gov/listeria/index.html[↩][↩]
- de Noordhout CM, Devleesschauwer B, Angulo FJ, Verbeke G, Haagsma J, Kirk M, Havelaar A, Speybroeck N. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis. 2014 Nov;14(11):1073-1082. doi: 10.1016/S1473-3099(14)70870-9[↩][↩][↩]
- Havelaar AH, van Rosse F, Bucura C, Toetenel MA, Haagsma JA, Kurowicka D, Heesterbeek JH, Speybroeck N, Langelaar MF, van der Giessen JW, Cooke RM, Braks MA. Prioritizing emerging zoonoses in the Netherlands. PLoS One. 2010 Nov 15;5(11):e13965. doi: 10.1371/journal.pone.0013965[↩]
- Listeriosis. https://www.ecdc.europa.eu/en/listeriosis[↩]
- Lamont RF, Sobel J, Mazaki-Tovi S, Kusanovic JP, Vaisbuch E, Kim SK, Uldbjerg N, Romero R. Listeriosis in human pregnancy: a systematic review. J Perinat Med. 2011 May;39(3):227-36. doi: 10.1515/jpm.2011.035[↩]
- Johnston WH, Morton SA, Wong MH, Roy TE. Septicaemia of the newborn due to Listeria monocytogenes. Can Med Assoc J. 1955;73:402–05. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1826322/pdf/canmedaj00716-0077.pdf[↩]
- Becroft DM, Farmer K, Seddon RJ, Sowden R, Stewart JH, Vines A, Wattie DA. Epidemic listeriosis in the newborn. Br Med J. 1971 Sep 25;3(5777):747-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1798886/pdf/brmedj02667-0039.pdf[↩]
- Awofisayo A, Amar C, Ruggles R, Elson R, Adak GK, Mook P, Grant KA. Pregnancy-associated listeriosis in England and Wales. Epidemiol Infect. 2015 Jan;143(2):249-56. doi: 10.1017/S0950268814000594. Epub 2014 Mar 20. Erratum in: Epidemiol Infect. 2015 Jan;143(2):257. Mook, P [added].[↩]
- Disson O, Lecuit M. Targeting of the central nervous system by Listeria monocytogenes. Virulence. 2012 Mar-Apr;3(2):213-21. doi: 10.4161/viru.19586[↩]
- McLauchlin J, Mitchell RT, Smerdon WJ, Jewell K. Listeria monocytogenes and listeriosis: a review of hazard characterisation for use in microbiological risk assessment of foods. Int J Food Microbiol. 2004 Apr 1;92(1):15-33. doi: 10.1016/S0168-1605(03)00326-X[↩]
- Doganay, M. (2003), Listeriosis: clinical presentation. FEMS Immunology & Medical Microbiology, 35: 173-175. https://doi.org/10.1016/S0928-8244(02)00467-4[↩]
- Rogalla D, Bomar PA. Listeria Monocytogenes. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534838[↩]
- People at Risk – Pregnant Women and Newborns. https://www.cdc.gov/listeria/risk-groups/pregnant-women.html[↩]
- Timeline for Linking a Case of Listeria Infection to an Outbreak. https://www.cdc.gov/listeria/timeline.html[↩]
- People at Risk – Pregnant Women and Newborns. https://www.cdc.gov/listeria/risk-groups/pregnant-women.html[↩]
- Mylonakis E, Paliou M, Hohmann EL, Calderwood SB, Wing EJ. Listeriosis during pregnancy: a case series and review of 222 cases. Medicine 2002;81:260–9. https://journals.lww.com/md-journal/Fulltext/2002/07000/Listeriosis_During_Pregnancy__A_Case_Series_and.2.aspx[↩][↩]
- Management of Pregnant Women With Presumptive Exposure to Listeria monocytogenes. https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Management-of-Pregnant-Women-With-Presumptive-Exposure-to-Listeria-monocytogenes[↩]
- Janakiraman V. Listeriosis in Pregnancy: Diagnosis, Treatment, and Prevention. Reviews in Obstetrics and Gynecology. 2008;1(4):179-185. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2621056/[↩][↩][↩]
- Temple ME, Nahata MC. Treatment of listeriosis. Ann Pharmacother 2000;34:656–61 https://www.ncbi.nlm.nih.gov/pubmed/10852095[↩]
- Mazor M, Froimovich M, Lazer S, Maymon E, Glezerman M. Listeria monocytogenes. The role of transabdominal amniocentesis in febrile patients with preterm labor. Arch Gynecol Obstet 1992;252:109–12. https://www.ncbi.nlm.nih.gov/pubmed/1471911[↩]
- Craig S, Permezel M, Doyle L, Mildenhall L, Garland S. Perinatal infection with Listeria monocytogenes. Aust N Z J Obstet Gynaecol 1996;36:286–90. https://www.ncbi.nlm.nih.gov/pubmed/8883752[↩]
- Lamont RF, Sobel J, Mazaki-Tovi S, Kusanovic JP, Vaisbuch E, Kim SK, et al. Listeriosis in human pregnancy: a systematic review. J Perinat Med 2011;39:227–36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3593057/[↩]
- https://www.cdc.gov/foodnet/pdfs/2014-foodnet-surveillance-report.pdf[↩]
- Choi MH, Park YJ, Kim M, Seo YH, Kim YA, Choi JY, Yong D, Jeong SH, Lee K. Increasing Incidence of Listeriosis and Infection-associated Clinical Outcomes. Ann Lab Med. 2018 Mar;38(2):102-109. doi: 10.3343/alm.2018.38.2.102. Erratum in: Ann Lab Med. 2018 May;38(3):287.[↩]
- Listeria (Listeriosis). Information for Health Professionals and Laboratories. https://www.cdc.gov/listeria/technical.html[↩]