Ranson criteria
Ranson criteria are used to predict severity and mortality of acute pancreatitis 1, 2. The original Ranson’s criteria is a scoring system that uses 11 parameters to assess the severity of acute pancreatitis. The 11 parameters are age, white blood cell count (WBC), blood glucose, serum aspartate transaminase (AST), serum lactate dehydrogenase (LDH), serum calcium, fall in hematocrit, arterial oxygen (PaO2), blood urea nitrogen (BUN), base deficit, and sequestration of fluids 3. Five parameters are assessed on admission, and the other six are assessed at 48 hours post admission. One point is given for each positive parameter for a maximum score of 11.
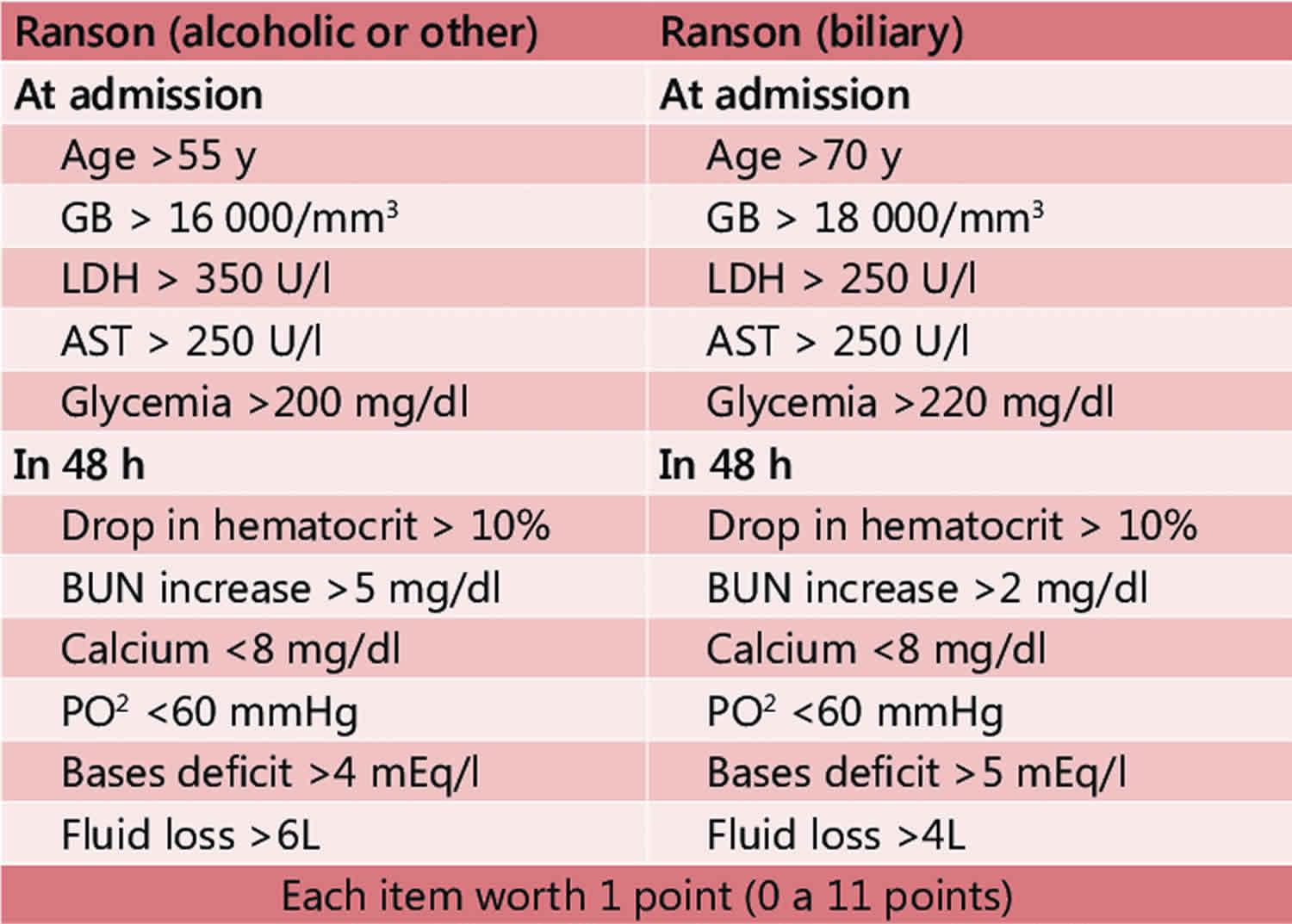
It should be noted that there is also a modified Ranson’s criteria. The modified Ranson criteria have a max score of 10. Five parameters assessed on admission and the other 5 at the 48-hour mark 4. The original Ranson’s criteria with 11 parameters are used to score alcoholic pancreatitis while the modified criteria have 10 parameters that are used to score gallbladder pancreatitis 5.
The Ranson criteria with 11 parameters are used to assess the severity of alcoholic pancreatitis. The 5 parameters on admission are age older than 55 years, WBC count greater than 16,000 cells/mm³, blood glucose greater than 200 mg/dL (11 mmol/L), serum AST greater than 250 IU/L, and serum LDH greater than 350 IU/L. At 48 hours, the remaining 6 parameters are: serum calcium less than 8.0 mg/dL (less than 2.0 mmol/L), hematocrit fall greater than 10%, PaO2 less than 60 mmHg, BUN increased by 5 or more mg/dL (1.8 or more mmol/L) despite intravenous (IV) fluid hydration, base deficit greater than 4 mEq/L, and sequestration of fluids greater than 6 L.
The modified Ranson’s criteria are used to assess gallstone pancreatitis. The five parameters on admission are age older than 70 years, white blood cell count (WBC) greater than 18,000 cells/mm³, blood glucose greater than 220 mg/dL (greater than 12.2 mmol/L), serum AST greater than 250 IU/L, and serum LDH greater than 400 IU/L. At 48 hours, the remaining 5 parameters are serum calcium less than 8.0 mg/dL (less than 2.0 mmol/L), hematocrit fall greater than 10%, BUN increased by 2 or more mg/dL (0.7 or more mmol/L) despite IV fluid hydration, base deficit greater than 5 mEq/L, and sequestration of fluids greater than 4 L.
One limitation of Ranson’s criteria is that other scoring systems are superior in either sensitivity or specificity, In a 2016 meta-analysis, a Ranson’s score greater than 2 had a median sensitivity and specificity of 90% and 67.4% respectively. In this same meta-analysis, other scoring systems had better sensitivity or specificity. For example, APACHE-II score greater than 7 had a 100% median sensitivity, while BISAP score greater than 2 had 87.6% median specificity. Another meta-analysis of acute pancreatitis severity scores showed that a Ranson score of greater than 2 has a sensitivity of 86.6% and specificity of 87.2%. Ranson et al. also showed a Ranson score greater than 2 had a sensitivity of 84.2% and specificity of 89.8%.
The second limitation is that the score and severity of acute pancreatitis cannot be determined until 48 hours have passed since admission. This limits its utility in time-sensitive situations like the emergency department. Also, there are 11 parameters, which makes it difficult to use conveniently. Other scoring systems like APACHE-II can be applied at any time and is the scoring system used in critical care. The Bedside Index of Severity in Acute Pancreatitis (BISAP) is another scoring system that can be used at any time and is utilized by emergency medicine physicians.
The third limitation is that the study group in Ranson et al. 1 consisted of an age range of approximately 30 to 75 years old. As a result, Ranson’s criteria cannot be used for a pediatric or adolescent population. This was studied in Lautz et al., which showed that the Ranson’s criteria had a sensitivity 51.8% and negative predictive value of 83.2%.
The Bedside Index for Severity in Acute Pancreatitis (BISAP) was developed in 2008 and has been shown to be a more accurate prognostic tool that predicts the mortality risk in acute pancreatitis based on the data within the first 24 hour (Table 2) 6. The Bedside Index for Severity in Acute Pancreatitis (BISAP) scoring index is to be used in the first 24 hour of presentation and the variables included in Bedside Index of Severity in Acute Pancreatitis (BISAP) score include 6:
- Blood urea nitrogen (BUN) > 25 mg/dL
- Abnormal mental status (Glasgow coma score <15)
- Evidence of systemic inflammatory response syndrome (SIRS)
- Greater than or equal to 60 years of age
- Presence of pleural effusion
To calculate the BISAP, sum the number of positive variables (0–5). Multiple studies have validated the performance of the BISAP and pooled estimates demonstrate its accuracy in predicting acute pancreatitis severity 7, 8.
Table 1. Ranson criteria for acute pancreatitis based on initial lab values
| Ranson criteria at admission | |
|---|---|
| White blood cell count > 16,000 cells/mm³ | 1 point |
| Age > 55 years of age | 1 point |
| Blood glucose > 200 mg/dL | 1 point |
| Aspartate transaminase (AST) > 250 IU/L | 1 point |
| Lactate dehydrogease (LDH) > 350 IU/L | 1 point |
| Ranson criteria within 48 hours | |
| Serum calcium <8.0 mg/dL | 1 point |
| Hematocrit drop >10% | 1 point |
| PaO2 <60 mmHg | 1 point |
| Blood urea nitrogen (BUN) > 5 mg/dL | 1 point |
| Base deficit > 4.0 mEq/L | 1 point |
| Fluid sequestration > 6L | 1 point |
Footnote: Ranson Criteria for acute pancreatitis total point indicates a prognosis for the patient as follows:
- 0 to 2 points: Severe pancreatitis is unlikely; Mortality 0% to 3%
- 3 to 4 points: Severe pancreatitis is likely; Mortality 15%
- 5 to 6 points: Severe pancreatitis is likely; Mortality 40%
- 7 to 11 points: Severe pancreatitis is likely; Mortality nearly 100%
Table 2. Bedside Index for Severity in Acute Pancreatitis (BISAP) score
| Bedside Index for Severity in Acute Pancreatitis (BISAP) score for pancreatitis mortality | |
|---|---|
| Blood urea nitrogen > 25 mg/dL | 1 point |
| Impaired mental status (disorientation, lethargy, somnolence, coma, stupor) | 1 point |
≥ 2 Systemic Inflammatory Response Syndrome (SIRS) Criteria
| 1 point |
| Age ≥ 60 years old | 1 point |
| Pleural effusion present on imaging | 1 point |
Footnotes: Bedside Index for Severity in Acute Pancreatitis (BISAP) score of 0 has < 1% and scores ≤ 2 have 1.9% mortality risk, respectively.
[Source 10 ]Ranson criteria calculator
Ranson criteria for the severity of acute pancreatitis
On admission
- Age > 55 years old = 1
- White blood cell count (WBC) > 16,000/mcL = 1
- Blood glucose > 200 mg/dL (11 mmol/L) = 1
- Serum AST > 250 IU/L = 1
- Serum LDH > 350 IU/L = 1
After 48 Hours
- Hematocrit fall > 10% = 1
- Blood urea nitrogen (BUN) rise by ≥ 5 mg/dL (≥ 1.8 mmol/L) after IV fluid hydration = 1
- Serum Calcium <8.0 mg/dL (< 2.0 mmol/L) = 1
- Hypoxemia (PO2 < 60 mmHg) = 1
- Base deficit > 4 meq/L = 1
- Estimated fluid sequestration > 6L = 1
Total Ranson Score:
Ranson Score Interpretation 9:
- 0 to 2 points: Severe pancreatitis is unlikely; Mortality 0% to 3%
- 3 to 4 points: Severe pancreatitis is likely; Mortality 15%
- 5 to 6 points: Severe pancreatitis is likely; Mortality 40%
- 7 to 11 points: Severe pancreatitis is likely; Mortality nearly 100%
Ranson criteria score interpretation
Ranson’s criteria are primarily used in the inpatient setting. A Ranson score of 0 or 1 predicts that complications will not develop and that mortality will be negligible. A score of 3 or greater predicts severe acute pancreatitis and possible mortality. Severe acute pancreatitis is defined by the presence of any organ failure or local pancreatic complications such as pseudocyst, abscess, or necrosis.
Ranson Score Interpretation:
- 0 to 2 points: Severe pancreatitis is unlikely; Mortality 0% to 3%
- 3 to 4 points: Severe pancreatitis is likely; Mortality 15%
- 5 to 6 points: Severe pancreatitis is likely; Mortality 40%
- 7 to 11: Severe pancreatitis is likely; Mortality nearly 100%
Because of the drawbacks of the Ranson criteria, other factors are also used to assess the severity of acute pancreatitis. An elevated BUN on admission has been found to be associated with an increase in the severity of acute pancreatitis and/or risk fo death. It is believed that the elevated BUN is a reflection of intravascular volume depletion, which is mediated by inflammatory mediators in response to the acute inflammation. The APACHE score has one major advantage over Ranson criteria in that it can be used to evaluate the patient at any time point of admission. However, the one major drawback of the APACHE score is that it is labor intensive.
The one laboratory parameter which is often used to stage acute pancreatitis is the hematocrit. Hematocrit greater than 47% on admission has been shown to be a good predictor of pancreatic necrosis. Other markers also used to stage acute pancreatitis include levels of CRP and interleukin-6. Many other biological markers have shown promise in predicting the severity of acute pancreatitis (e.g., trypsinogen activation peptide, phospholipase A2, and polymorphonuclear elastase) but not all are better than using CRP.
It is important to understand that imaging is not indicated to assess a patient with mild acute pancreatitis unless the patient is suspected of having a malignancy. However, CT scan of the abdomen is always indicated in patients with severe acute pancreatitis and is the imaging modality of choice in patients with complications. The CT scan is rarely needed within the first three days of admission unless the diagnosis is in doubt because most inflammatory alterations are often not visible on the scan at this time.
Finally, in some patients with severe acute pancreatitis, image-guided aspiration may be required to differentiate sterile necrosis from a purulent infection.
- Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974 Jul;139(1):69-81.[↩][↩]
- Basit H, Ruan GJ, Mukherjee S. Ranson Criteria. [Updated 2019 Jul 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482345[↩]
- Kothari S, Kalinowski M, Kobeszko M, Almouradi T. Computed tomography scan imaging in diagnosing acute uncomplicated pancreatitis: Usefulness vs cost. World J. Gastroenterol. 2019 Mar 07;25(9):1080-1087.[↩]
- Kim YJ, Kim DB, Chung WC, Lee JM, Youn GJ, Jung YD, Choi S, Oh JH. Analysis of factors influencing survival in patients with severe acute pancreatitis. Scand. J. Gastroenterol. 2017 Aug;52(8):904-908.[↩]
- Waller A, Long B, Koyfman A, Gottlieb M. Acute Pancreatitis: Updates for Emergency Clinicians. J Emerg Med. 2018 Dec;55(6):769-779.[↩]
- Papachristou GI, Muddana V, Yadav D, O’Connell M, Sanders MK, Slivka A, Whitcomb DC. Comparison of BISAP, Ranson’s, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol. 2010 Feb;105(2):435-41; quiz 442. doi: 10.1038/ajg.2009.622[↩][↩]
- Chandra S, Murali A, Bansal R, Agarwal D, Holm A. The Bedside Index for Severity in Acute Pancreatitis: a systematic review of prospective studies to determine predictive performance. J Community Hosp Intern Med Perspect. 2017 Sep 19;7(4):208-213. doi: 10.1080/20009666.2017.1361292[↩]
- Pérez Campos A, Bravo Paredes E, Prochazka Zarate R, Bussalleu A, Pinto Valdivia J, Valenzuela Granados V. BISAP-O y APACHE-O: utilidad en la predicción de severidad en la pancreatitis aguda según la clasificación modificada de Atlanta [BISAP-O y APACHE-O: utility in predicting severity in acute pancreatitis in modified Atlanta classification]. Rev Gastroenterol Peru. 2015 Jan;35(1):15-24. Spanish.[↩]
- Ducarme G, Maire F, Chatel P, Luton D, Hammel P. Acute pancreatitis during pregnancy: a review. J Perinatol. 2014 Feb;34(2):87-94. doi: 10.1038/jp.2013.161[↩][↩]
- Kothari S, Kalinowski M, Kobeszko M, Almouradi T. Computed tomography scan imaging in diagnosing acute uncomplicated pancreatitis: Usefulness vs cost. World J Gastroenterol. 2019 Mar 7;25(9):1080-1087. doi: 10.3748/wjg.v25.i9.1080[↩]