Contents
Jumper’s knee
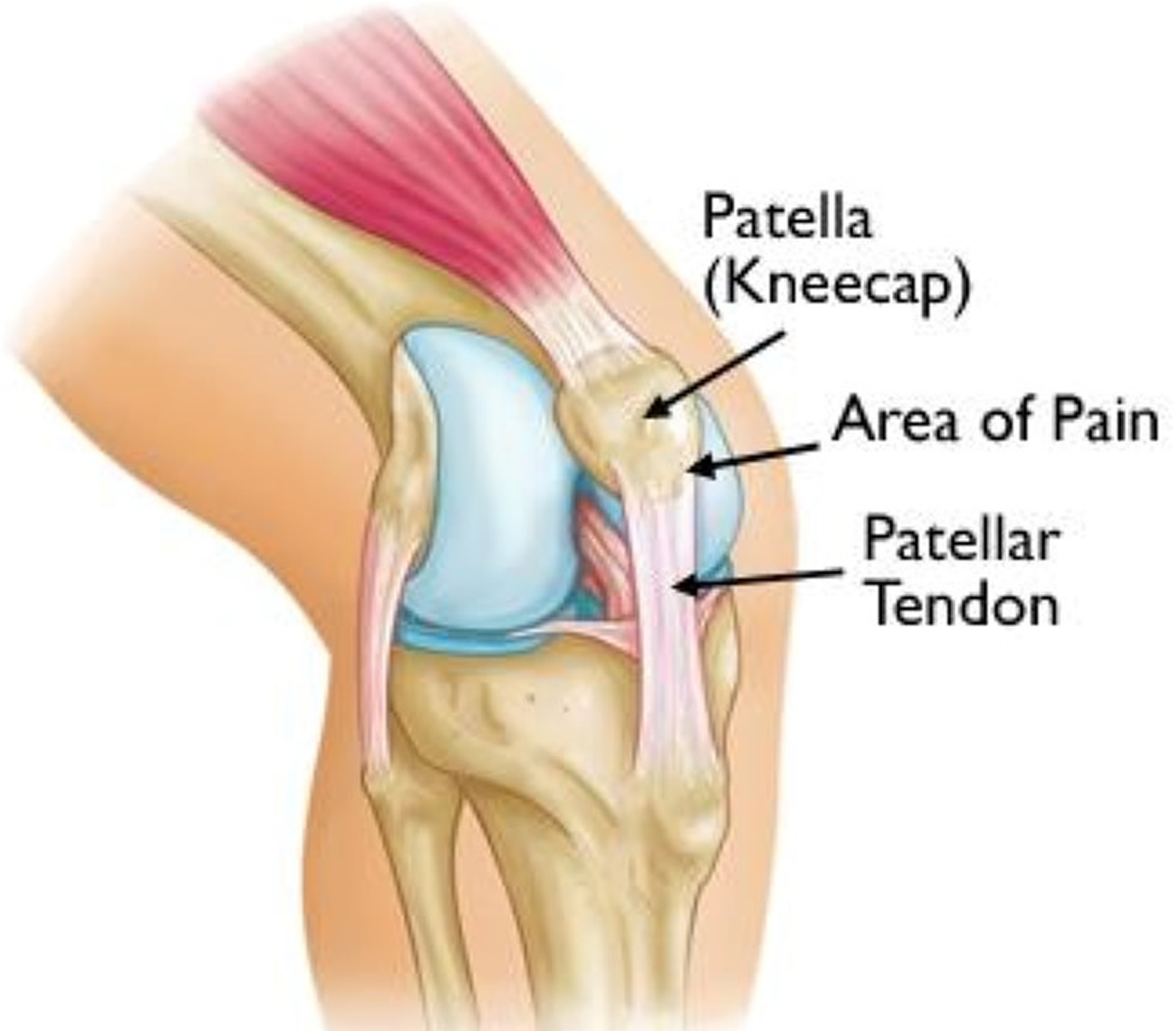
Jumper’s knee also called patellar tendinitis or patellar tendinopathy, is a painful condition of the knee caused by small tears in the patellar tendon that mainly occurs in sports requiring strenuous jumping 1. It is appropriate to mention that patellar “tendinitis” is a misnomer as the condition is felt by many clinicians to be more tendinosis than it is tendinitis 1. In published studies, it is noted that classic inflammatory cells are usually absent 2. The patellar tendon is the cord-like tissue that joins the patella (kneecap) to the tibia (shinbone). The patellar tendon works with the muscles at the front of your thigh to extend your knee so that you can kick, run and jump. The tears are typically caused by accumulated stress on the patellar or quadriceps tendon. As the name implies, jumper’s knee is common in athletes from jumping sports such as volleyball, track (long and high jump), and basketball. Jumper’s knee has a male predominance 3. However, even people who don’t participate in jumping sports can get patellar tendinitis. Contrary to traditional belief, jumper’s knee does not involve inflammation of the knee extensor tendons. Studies dating back 40 years describe jumper’s knee as a degenerative condition. Jumper’s knee is a clinical diagnosis made through detailed history taking and a physical exam. Ultrasound can facilitate the diagnosis, as this imaging study is readily available and affordable. Treatment mainly revolves around conservative measures such as reducing activities that place loading impact on the knee. For knee pain, try self-care measures first, such as icing the area and temporarily reducing or avoiding activities that trigger your symptoms. Once the pain subsides, restoration of function is achieved through physical and exercise therapy. Surgery usually remains the last resort for chronic refractory cases.
Figure 1. Patella tendon (ligament)
Figure 2. Jumper’s knee
Jumper’s knee staging
Blazina et al. 4 first used the term jumper’s knee in 1973. They also classified the pathology by stage according to the onset of pain in relation to physical activity. This classification along with its modifications are still widely employed. Blazina et al. suggest 4 stages 4:
- Pain after sports activity
- Pain at the beginning of sports activity yet disappearing with warm-up and sometimes reappearing with fatigue
- Pain at rest and during activity
- Rupture of the tendon
It may be useful to classify the pathology into 3 stages according to the duration of symptoms 5:
- Acute when symptoms have been present for 0 to 6 weeks
- Sub-acute when symptoms have been present between 6 to 12 weeks
- Chronic after more than 3 months
Jumper’s knee causes
Jumper’s knee is an overuse injury of the knee extensor mechanism due to repetitive mechanical stress from athletic activities requiring movements such as jumping, landing, acceleration, deceleration, and cutting 6. Micro-tearing of the knee extensor tendons can arise after constant repetition of these movements during a single exercise session or if there is insufficient rest between sessions. The component of the knee extensor mechanism most likely to be affected is the inferior pole of the patella where the patellar tendon inserts. Other less frequently involved regions of the knee are at the insertion of the quadriceps tendon to the superior pole of the patella and where the patellar tendon inserts into the tibial tuberosity 7. For purposes of simplicity, and considering that the majority of the cases for jumper’s knee are due to a problem on the patellar tendon at its insertion in the inferior patella, some authors have use the term patellar tendinopathy with jumper’s knee interchangeably.
There are several intrinsic factors of the knee that predispose to this pathology. These include ligamentous laxity, excessive Q-angle of the knee, abnormal patellar height, previous ongoing inflammation of the knee and excessive force generation on the knee. Other factors can also lead to the development of the jumper’s knee such as excessive volume and frequency of training, the athlete’s performance level, and the hardness of the ground where the sport is practiced 8.
Pathophysiology
Overload on the knee extensor tendons will cause it to weaken progressively, eventually leading to failure. Microscopic failure occurs within the tendon at high loads and eventually leads to alterations at the cellular level, which undermine its mechanical properties. Tendon micro-trauma may cause individual fibril degeneration due to stress across the tendon. As the fibril degeneration becomes ongoing, chronic tendinopathy will ensue 9.
Examination of the tendon under ultrasound shows three pathologic changes. At first, there will be edema along the damaged tendon fibers. The affected tissue is swollen and thickened, but still homogenous. The second is a “stage with irreversible anatomical lesions,” the tendon has a heterogeneous appearance with hypoechoic and hyperechoic images without edema (granuloma). At this point, the tendinous envelope is still more or less well defined. In the final stage of the lesion, the tendinous envelope is irregular and thickened. Its fibers appear heterogeneous, yet the swelling has disappeared 6.
Risk factors for jumper’s knee
A combination of factors may contribute to the development of jumper’s knee, including:
- Physical activity. Running and jumping are most commonly associated with jumper’s knee. Sudden increases in how hard or how often you engage in the activity also add stress to the tendon, as can changing your running shoes.
- Tight leg muscles. Tight thigh muscles (quadriceps) and hamstrings, which run up the back of your thighs, can increase strain on your patellar tendon.
- Muscular imbalance. If some muscles in your legs are much stronger than others, the stronger muscles could pull harder on your patellar tendon. This uneven pull could cause tendinitis.
- Chronic illness. Some illnesses disrupt blood flow to the knee, which weakens the tendon. Examples include kidney failure, autoimmune diseases such as lupus or rheumatoid arthritis and metabolic diseases such as diabetes.
Jumper’s knee prevention
To reduce your risk of developing jumper’s knee, take these steps:
- Don’t play through pain. As soon as you notice exercise-related knee pain, ice the area and rest. Until your knee is pain-free, avoid activities that put stress on your patellar tendon.
- Strengthen your muscles. Strong thigh muscles are better able to handle the stresses that can cause jumper’s knee. Eccentric exercises, which involve lowering your leg very slowly after extending your knee, are particularly helpful.
- Improve your technique. To be sure you’re using your body correctly, consider taking lessons or getting professional instructions when starting a new sport or using exercise equipment.
Jumper’s knee symptoms
Pain is the first symptom of jumper’s knee, usually between your kneecap and where the tendon attaches to your shinbone (tibia).
Initially, you may only feel pain in your knee as you begin physical activity or just after an intense workout. Over time, the pain worsens and starts to interfere with playing your sport. Eventually, the pain interferes with daily movements such as climbing stairs or rising from a chair.
Jumper’s knee complications
If you try to work through your pain, ignoring your body’s warning signs, you could cause increasingly larger tears in the patellar tendon. Knee pain and reduced function can persist if you don’t tend to the problem, and you may progress to the more serious patellar tendinopathy.
Athletes, clinicians, coaches, and athletic trainers need to understand that the treatment for patellar tendinopathy can be a slow and sometimes frustrating process. There are multiple pitfalls to be aware of, including the failure to control pain. The athlete’s beliefs about pain and pathology may influence the development and management of unresponsive tendinopathies. Because some athletes may have been told that they have weakened tendons due to tears and degeneration, and hence an increased risk of rupture, they may develop fear-avoidance behavior, which can be associated with poorer functional outcomes in individuals suffering from lower-limb tendinopathy. Over-reliance on non-invasive therapies like shockwave therapy and injections instead of including rehabilitation exercises as part of the treatment plan can also lead to complications. Failure to address the athletes landing kinematics can also bring difficulties. Athletes should have their jump-landing mechanics retrained after adequate rehabilitation 10.
Jumper’s knee diagnosis
During the exam, your doctor may apply pressure to parts of your knee to determine where you hurt. Usually, pain from patellar tendinitis is on the front part of your knee, just below your kneecap.
Imaging tests
Your doctor may suggest one or more of the following imaging tests:
- X-rays. X-rays help to exclude other bone problems that can cause knee pain.
- Ultrasound. This test uses sound waves to create an image of your knee, revealing tears in your patellar tendon.
- Magnetic resonance imaging (MRI). MRI uses a magnetic field and radio waves to create detailed images that can reveal subtle changes in the patellar tendon.
Jumper’s knee treatment
There is no evidence-based, preferred treatment of choice for jumper’s knee. Doctors typically begin with less invasive treatments before considering other options, such as surgery. Refractory response to treatment is also typical for jumper’s knee which often leaves the health professional and patients searching for alternative therapies 11.
Most patients with jumper’s knee are managed through medical and rehabilitative treatment in the initial stages of the disease 12. Early recognition and diagnosis of jumper’s knee are vital as it can have a progressive course. Pain relievers such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others) may provide short-term relief from pain associated with jumper’s knee. Although non-steroidal anti-inflammatory drugs (NSAIDs) were used traditionally, these have recently become less judicious as more physicians come to realize that jumper’s knee is not inflammatory. Hence, NSAIDs may not provide significant long-term benefit in jumper’s knee tendinopathy 2.
Home remedies
If your knee hurts, consider the following:
- Pain relievers. Over-the-counter medications such as ibuprofen and naproxen sodium may provide short-term pain relief.
- Avoid activity that causes pain. You may need to practice your sport less often or temporarily switch to a lower impact sport. Working through pain can further damage your patellar tendon.
- Ice. Apply ice after activity that causes pain. Place ice in a plastic bag and wrap the bag in a towel. Or try an ice massage. Freeze water in a plastic foam cup and hold the cup as you apply the ice directly to your skin.
- Braces. These are sometimes recommended to provide support for the knee. There is no clear evidence if there is a benefit, but it does provide some patients with relief from their symptoms.
Physical therapy
A variety of physical therapy techniques can help reduce the symptoms associated with jumper’s knee, including:
- Stretching exercises. Regular, steady stretching exercises can reduce muscle spasm and help lengthen the muscle-tendon unit. Don’t bounce during your stretch.
- Strengthening exercises. Weak thigh muscles contribute to the strain on your patellar tendon. Exercises that involve lowering your leg very slowly after extending it can be particularly helpful, as can exercises that strengthen all of the leg muscles in combination, such as a leg press.
- Patellar tendon strap. A strap that applies pressure to your patellar tendon can help to distribute force away from the tendon and direct it through the strap instead. This may help relieve pain.
- Iontophoresis. This therapy involves spreading a corticosteroid medicine on your skin and then using a device that delivers a low electrical charge to push the medication through your skin.
Eccentric training has been suggested to play a key role in the rehabilitation of jumper’s knee 13. According to Rodriguez-Merchan 14 eccentric training appears to be the treatment of choice for patients suffering from patellar tendinopathy. Athletes must avoid activities such as excessive jumping or impact loading of the knee which only aggravate the situation. As the pain begins to subside, the intensity of rehabilitation therapy and sport-specific training can be slowly increased 6.
Other procedures
Given the refractory response to many initial treatments, new methods have recently emerged. These include dry-needling, sclerosing injections, platelet-rich plasma therapy, extracorporeal shock wave treatment and hyperthermia thermotherapy 11.
If conservative treatments don’t help, your doctor may suggest other therapies, such as:
- Corticosteroid injection. An ultrasound-guided corticosteroid injection into the sheath around the patellar tendon may help relieve pain. But these types of drugs can also weaken tendons and make them more likely to rupture.
- Platelet-rich plasma injection. This type of injection has been tried in some people with chronic patellar tendon problems. Studies are ongoing. It is hoped the injections might promote new tissue formation and help heal tendon damage.
- Oscillating needle procedure. This outpatient procedure is performed using local anesthesia. Your doctor uses ultrasound imaging to guide a small oscillating needle that cuts away the damaged area while sparing healthy tendon. This is a relatively new procedure, but results have shown promise.
Surgical treatment
Surgery usually remains the last resort for chronic refractory cases. Traditionally, the gold standard for surgical treatment of patellar tendinopathy involved open debridement of the inferior pole of the patella, as well as debridement of the patella tendon. Recently, knee arthroscopy has gained popularity for tissue debridement and release 11.
Jumper’s knee prognosis
Most cases of jumper’s knee will resolve with nonoperative management 9. Nevertheless, mild to moderate pain may persist for 15 years in adult athletes with jumper’s knee but does not appear to limit leisure-time physical activity 15.
Rudavsky and Cook 16 say that the process of returning to sports play is slow. This process is often dependent on a variety of factors ranging from the severity of pain, grade of dysfunction, the sport practiced, the quality of rehabilitation, the athlete’s performance level, and the presence of intrinsic and extrinsic factors. A previous study 17 that used imaging technology to classify the severity of the lesion said that mild pathologies might take anywhere from 20 days for the patient to return to sport, whereas more severe cases might take 90 days. Other experts mention that athletes with severe dysfunction might need anywhere from 6 to 12 months to recover. Lang and coworkers published a study were they analyzed patients who were treated surgically (arthroscopic patellar release). They determined that the meantime to return to play was 4.03 plus or minus 3.18 months 18.
Joshua et al. 19 performed a systemic search of previous studies to compare the efficacy of treatment for commonly used invasive and non-invasive treatment options. The conclusion reached was that eccentric squat-based therapy, shockwave, or platelet-rich plasma could be used as monotherapies or as adjunct therapies to accelerate recovery. Surgery or shockwave can be considered for patients who fail to improve after six months of conservative treatment. Since jumper’s knee is not inflammatory, corticosteroid injections should not be used 19.
Patellar tendinopathy may cause long-lasting symptoms that can lead to the athlete’s early retirement from sport. In a small prospective case-control study, Kettunen et al. 15 found that 53% of their symptomatic subjects with jumper’s knee had quit their sport when compared to their asymptomatic counterpart in which only 7% quit.
- Santana JA, Sherman Al. Jumpers Knee. [Updated 2019 Apr 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532969[↩][↩]
- Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth. BMJ. 2002 Mar 16;324(7338):626-7.[↩][↩]
- Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005 Apr;33(4):561-7.[↩]
- Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ. Jumper’s knee. Orthop. Clin. North Am. 1973 Jul;4(3):665-78.[↩][↩]
- Kaux JF, Forthomme B, Goff CL, Crielaard JM, Croisier JL. Current opinions on tendinopathy. J Sports Sci Med. 2011 Jun 01;10(2):238-53.[↩]
- Fredberg U, Bolvig L. Jumper’s knee. Review of the literature. Scand J Med Sci Sports. 1999 Apr;9(2):66-73.[↩][↩][↩]
- Ferretti A. Epidemiology of jumper’s knee. Sports Med. 1986 Jul-Aug;3(4):289-95.[↩]
- Tibesku CO, Pässler HH. [Jumper’s knee–a review]. Sportverletz Sportschaden. 2005 Jun;19(2):63-71.[↩]
- Schwartz A, Watson JN, Hutchinson MR. Patellar Tendinopathy. Sports Health. 2015 Sep-Oct;7(5):415-20.[↩][↩]
- Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J Orthop Sports Phys Ther. 2015 Nov;45(11):887-98.[↩]
- Christian RA, Rossy WH, Sherman OH. Patellar tendinopathy – recent developments toward treatment. Bull Hosp Jt Dis (2013). 2014;72(3):217-24.[↩][↩][↩]
- Martens M, Wouters P, Burssens A, Mulier JC. Patellar tendinitis: pathology and results of treatment. Acta Orthop Scand. 1982 Jun;53(3):445-50.[↩]
- Van der Worp H, de Poel HJ, Diercks RL, van den Akker-Scheek I, Zwerver J. Jumper’s knee or lander’s knee? A systematic review of the relation between jump biomechanics and patellar tendinopathy. Int J Sports Med. 2014 Jul;35(8):714-22.[↩]
- Rodriguez-Merchan EC. The treatment of patellar tendinopathy. J Orthop Traumatol. 2013 Jun;14(2):77-81.[↩]
- Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper’s knee in male athletes. A prospective follow-up study. Am J Sports Med. 2002 Sep-Oct;30(5):689-92.[↩][↩]
- Rudavsky A, Cook J. Physiotherapy management of patellar tendinopathy (jumper’s knee). J Physiother. 2014 Sep;60(3):122-9.[↩]
- Gemignani M, Busoni F, Tonerini M, Scaglione M. The patellar tendinopathy in athletes: a sonographic grading correlated to prognosis and therapy. Emerg Radiol. 2008 Nov;15(6):399-404.[↩]
- Lang G, Pestka JM, Maier D, Izadpanah K, Südkamp N, Ogon P. Arthroscopic patellar release for treatment of chronic symptomatic patellar tendinopathy: long-term outcome and influential factors in an athletic population. BMC Musculoskelet Disord. 2017 Nov 22;18(1):486.[↩]
- Everhart JS, Cole D, Sojka JH, Higgins JD, Magnussen RA, Schmitt LC, Flanigan DC. Treatment Options for Patellar Tendinopathy: A Systematic Review. Arthroscopy. 2017 Apr;33(4):861-872.[↩][↩]