Contents
- High blood pressure
- What is blood pressure?
- What is normal blood pressure?
- Types of hypertension
- High blood pressure symptoms and signs
- Side effects of high blood pressure
- Causes of high blood pressure
- High blood pressure prevention
- High blood pressure diagnosis
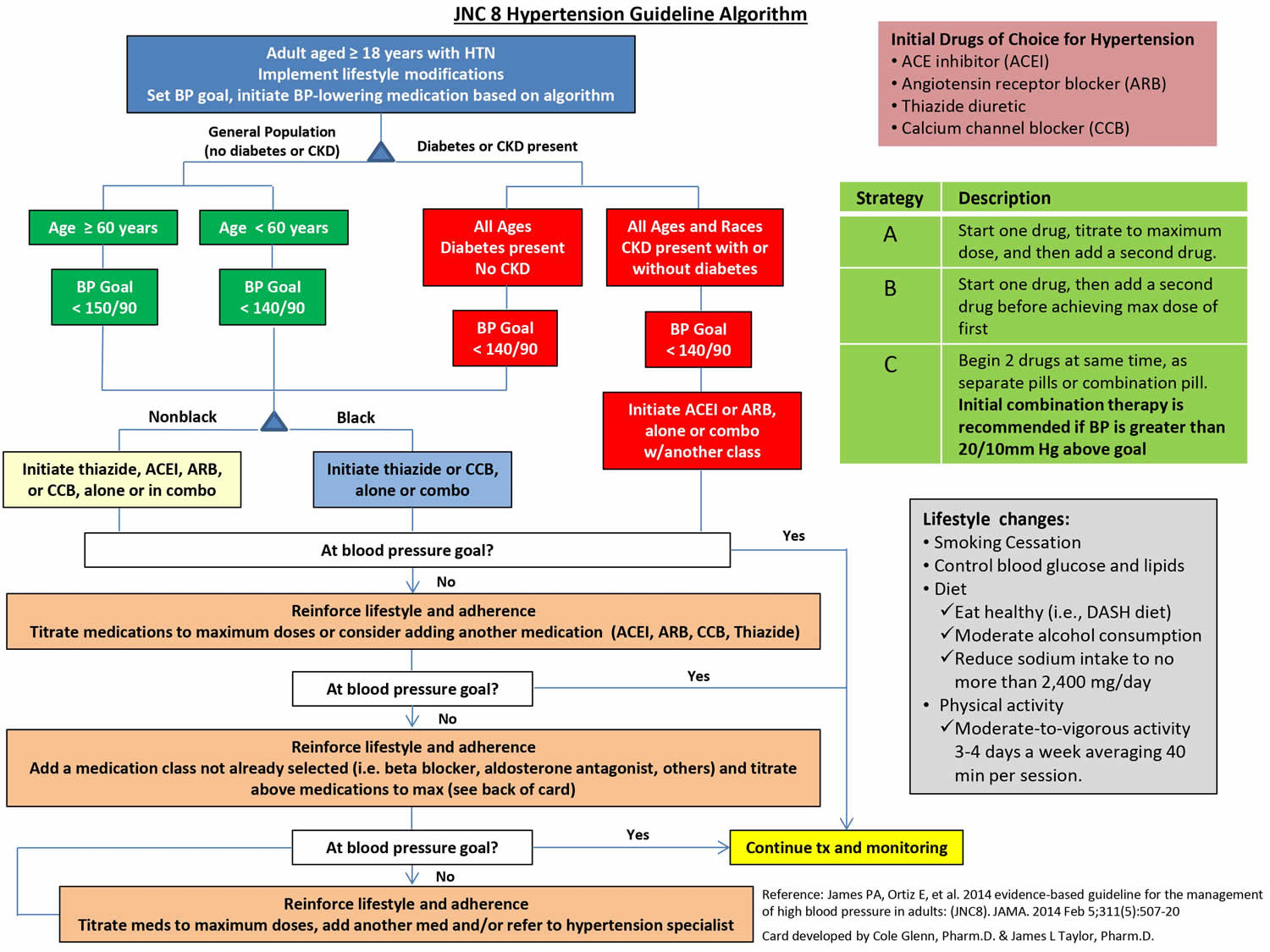
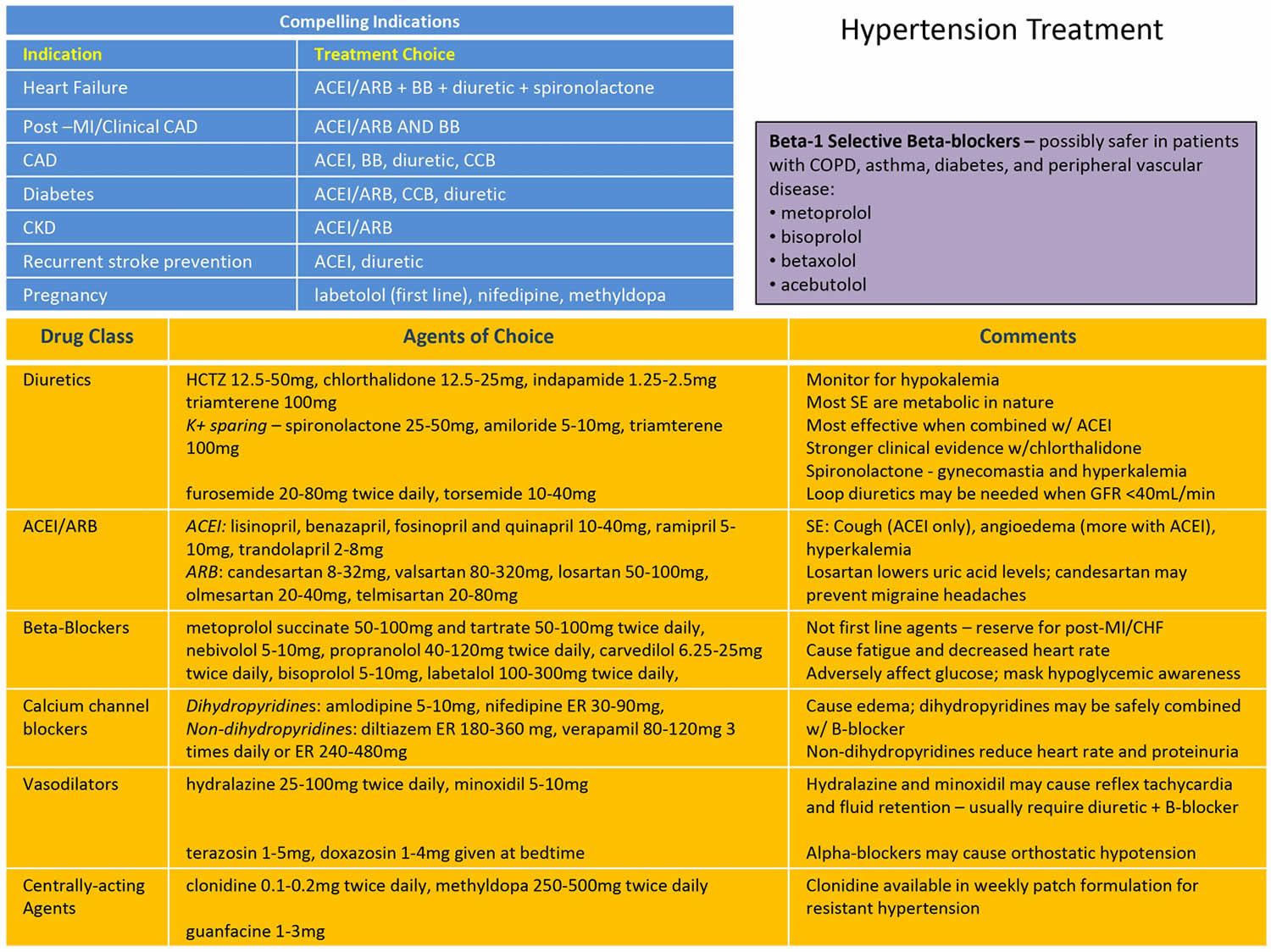
- High blood pressure treatment
- High blood pressure prognosis
High blood pressure
High blood pressure is medically known as hypertension, means your blood pressure is consistently higher-than-normal pressures and that also means your heart has to work harder to pump blood around your body. Your blood pressure is made up of two numbers given in millimeters of mercury (mm Hg): systolic pressure and diastolic pressure. Systolic pressure is the blood pressure when the heart ventricles pump blood out of your heart. Systolic pressure is represented by the top, higher number. Diastolic pressure measures the blood pressure in your arteries between heartbeats when your heart is at rest and is filling with blood and blood is not moving out of your heart. Diastolic pressure is represented by the bottom, lower number. For example, if your blood pressure is “140 over 90” or 140/90 mmHg, it means you have a systolic pressure of 140 mmHg and a diastolic pressure of 90 mmHg. The definition and categories of hypertension have been evolving over the years, high blood pressure is defined as systolic blood pressure 130 mmHg or higher and/or diastolic blood pressure 80 mmHg or higher 1. Your blood pressure is considered high when you have consistent systolic readings of 130 mm Hg or higher or diastolic readings of 80 mm Hg or higher 2. Everyone’s blood pressure will be slightly different. What’s considered low or high for you may be normal for someone else. As a general guide high blood pressure is considered to be 140/90mmHg or higher (or 150/90mmHg or higher if you’re over the age of 80). Readings above 180/120 mm Hg are dangerously high and require immediate medical attention. An ideal blood pressure is usually considered to be between 90/60mmHg and 120/80mmHg. Research have shown that systolic blood pressure greater than 120 mm Hg can be increasingly harmful to health 3, 4. You can have high blood pressure for years without any symptoms. Nearly half of American adults have high blood pressure and are not being treated to control their blood pressure. High blood pressure usually has no symptoms and many people don’t even know they have it 5. So the only way to find out if you have high blood pressure is to get regular blood pressure checks at least once a year from your health care provider. Your doctor will use a gauge, a stethoscope or electronic sensor, and a blood pressure cuff. He or she will take two or more readings at separate appointments before making a diagnosis.
Table 1. Blood pressure classification
| Systolic blood pressure (mmHg) | and/or | Diastolic blood pressure(mmHg) | Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure | American College of Cardiology/American Heart Association 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults |
|---|---|---|---|---|
| <120 | and | <80 | Normal blood pressure | Normal blood pressure |
| 120–129 | and | <80 | Prehypertension | Elevated blood pressure |
| 130–139 | or | 80–89 | Prehypertension | Stage 1 hypertension |
| 140–159 | or | 90–99 | Stage 1 hypertension | Stage 2 hypertension |
| ≥160 | or | ≥100 | Stage 2 hypertension | Stage 2 hypertension |
Footnotes: Blood pressure should be based on an average of ≥2 careful readings on ≥2 occasions. Adults with systolic blood pressure or diastolic blood pressure in 2 categories should be designated to the higher blood pressure category.
[Sources 6, 7 ]The National Heart, Lung, and Blood Institute of the National Institutes of Health has determined 2 levels of high blood pressure for adults (for individuals aged 18 years and above):
- Stage 1 hypertension
- 130 mm Hg to 139 mm Hg systolic pressure
- OR
- 80 mm Hg to 89 mm Hg diastolic pressure
- Stage 2 hypertension
- 140 mm Hg to 159 mm Hg systolic pressure
- OR
- 90 mm Hg to 99 mm Hg diastolic pressure
- Stage 2 hypertension
- Higher than 160 mm Hg systolic pressure
- OR
- Higher than 100 mm Hg diastolic pressure
- Hypertensive crisis
- A blood pressure measurement higher than 180/120 mm Hg is an emergency situation that requires urgent medical care. If you get this result when you take your blood pressure at home, wait five minutes and retest. If your blood pressure is still this high, contact your doctor immediately. If you also have chest pain, vision problems, numbness or weakness, breathing difficulty, or any other signs and symptoms of a stroke (this is when blood flow to your brain stops) or heart attack (also called myocardial infarction), call your local emergency medical number.
The National Heart, Lung, and Blood Institute defines “prehypertension” or “elevated blood pressure” as:
- 120 mm Hg to 129 mm Hg systolic pressure
- AND
- Less than 80 mm Hg diastolic pressure
The National Heart, Lung, and Blood Institute guidelines define “normal blood pressure” as follows:
- Less than 120 mm Hg systolic pressure
- AND
- Less than 80 mm Hg diastolic pressure
Low blood pressure is define as:
- Less than 90 mm Hg systolic pressure
- AND
- Less than 60 mm Hg diastolic pressure
The recent European Society of Cardiology and European Society of Hypertension guidelines for individuals aged 16 years and above came out in 2018 and defined hypertension as 8:
- Optimal: systolic blood pressure less than 120 mmHg and diastolic blood pressure less than 80 mmHg
- Normal: systolic blood pressure 120 to 129 mmHg and/or diastolic blood pressure 80 to 84 mmHg
- High normal: systolic BP 130 to 139 mmHg and/or diastolic BP 85 to 89 mmHg
- Grade 1 hypertension: systolic BP 140 to 159 mmHg and/or diastolic BP 90 to 99 mmHg
- Grade 2 hypertension: systolic BP 160 to 179 mmHg and/or diastolic BP 100 to 109mmHg
- Grade 3 hypertension: systolic BP greater than or equal to 180 mmHg and/or diastolic BP greater than or equal to 110 mmHg
- Isolated systolic hypertension: systolic BP greater than or equal to 140 mmHg and diastolic BP less than 90 mmHg (further classified into Grades as per above ranges of systolic blood pressure)
European Society of Cardiology and European Society of Hypertension recommendations also shed light on home and ambulatory BP measurements and following cut-offs were given 8:
- Daytime (or awake) mean systolic blood pressure greater than or equal to 135mmHg and/or diastolic BP greater than or equal to 85 mmHg
- Night-time (or asleep) mean systolic blood pressure greater than or equal to 120mmHg and/or diastolic BP greater than or equal to 70 mmHg
- 24 hr mean systolic blood pressure greater than or equal to 130mmHg and/or diastolic BP greater than or equal to 80 mmHg
- Home BP mean systolic blood pressure greater than or equal to 135mmHg and/or diastolic BP greater than or equal to 85 mmHg
Isolated systolic hypertension is a condition in which the diastolic pressure is normal (less than 80 mm Hg) but systolic pressure is high (greater than or equal to 130 mm Hg). This is a common type of high blood pressure among people older than 65.
White coat hypertension is an office BP 130/80 mmHg or more but less than 160/100mmHg which comes down to 130/80mmHg or less after at least 3 months of anti-hypertensive therapy 9. Ambulatory or home blood pressure measurement is usually necessary for this diagnosis.
Masked hypertension is an elevated office systolic BP 120 to 129mmHg, and diastolic BP less than 80mmHg but raised BP on ambulatory or home measurements (130/80mmHg or more) 9.
Use these numbers as a guide only. Both numbers in a blood pressure reading are important. But after age 50, the systolic reading is even more important. A single elevated blood pressure measurement is not necessarily an indication of a problem. Because blood pressure normally varies during the day and may increase during a doctor visit (white coat hypertension), your doctor will likely take multiple blood pressure measurements over several days or weeks before making a diagnosis of high blood pressure and starting treatment. If you normally run a lower-than-usual blood pressure, you may be diagnosed with high blood pressure with blood pressure measurements lower than 140/90.
Uncontrolled high blood pressure increases your risk of serious health problems and need urgent treatment in hospital to reduce the risk of a stroke or heart attack. High blood pressure can also cause kidney failure, heart failure, problems with your sight and vascular dementia. Your blood pressure is important because if it is too high, it affects the blood flow to your organs. Over the years, this increases your chances of developing heart disease, stroke, kidney failure, diabetes, eye disease, erectile dysfunction and other conditions. Fortunately, high blood pressure can be easily detected. And once you know you have high blood pressure, you can work with your doctor to control it.
To control or lower high blood pressure, your doctor may recommend that you adopt a heart-healthy lifestyle. This includes choosing heart-healthy foods such as those in the DASH (Dietary Approaches to Stop Hypertension) eating plan. You may also need to take medicines. Controlling or lowering blood pressure can help prevent or delay serious health problems such as chronic kidney disease, heart attack, heart failure, stroke, and possibly vascular dementia.
High blood pressure can often be prevented or reduced by eating healthily, maintaining a healthy weight, taking regular exercise, drinking alcohol in moderation and not smoking.
What is blood pressure?
Blood pressure is the pressure of blood in your arteries or the force of blood pushing against your artery walls – the vessels that carry your blood from your heart to your brain and the rest of your body 10. You need a certain amount of pressure to get the blood moving around your body. Your blood pressure is determined both by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries. The size and elasticity of the artery walls affect blood pressure. The more blood your heart pumps and the narrower your arteries, the higher your blood pressure. High blood pressure, sometimes called hypertension, happens when this force is too high. A blood pressure reading is given in millimeters of mercury (mm Hg). This recording represents how high the mercury column in the blood pressure cuff is raised by the pressure of your blood. Mercury was used in the first accurate pressure gauges and is still used in medicine today as the standard unit of measurement for pressure. Health care workers check blood pressure readings the same way for children, teens, and adults. They use a gauge, stethoscope or electronic sensor, and a blood pressure cuff.
Your blood pressure naturally goes up and down throughout the day and night, and it’s normal for it to go up while you’re moving about. It’s when your overall blood pressure is consistently high, even when you are resting, that you need to do something about it.
Blood pressure is measured in millimeters of mercury (mmHg) and is given as two figures:
- Systolic pressure (the upper number) – the pressure when your heart pushes blood out. The systolic pressure (higher number) is the force at which your heart pumps blood around your body.
- Diastolic pressure (the lower number)– the pressure when your heart rests between beats. The diastolic pressure (lower number) is the resistance to the blood flow in the blood vessels.
For example, if your blood pressure is “140 over 90” or 140/90mmHg, it means you have a systolic pressure of 140mmHg and a diastolic pressure of 90mmHg. Normal blood pressure for adults is defined as a systolic pressure below 120 mmHg and a diastolic pressure below 80 mmHg. It is normal for blood pressures to change when you sleep, wake up, or are excited or nervous. When you are active, it is normal for your blood pressure to increase. However, once the activity stops, your blood pressure returns to your normal baseline range.
Both numbers in a blood pressure reading are important. Typically, more attention is given to systolic blood pressure (the first number) as a major risk factor for cardiovascular disease for people over 50. In most people, systolic blood pressure rises steadily with age due to the increasing stiffness of large arteries, long-term buildup of plaque and an increased incidence of cardiac and vascular disease. However, either an elevated systolic or an elevated diastolic blood pressure reading may be used to make a diagnosis of high blood pressure. According to recent studies, the risk of death from ischemic heart disease and stroke doubles with every 20 mm Hg systolic or 10 mm Hg diastolic increase among people from age 40 to 89. But after age 60, the systolic reading is even more significant. Isolated systolic hypertension is a condition in which the diastolic pressure is normal (less than 90 mm Hg) but systolic pressure is high (greater than 140 mm Hg). This is a common type of high blood pressure among people older than 60.
Your doctor will likely take two to three blood pressure readings each at three or more separate appointments before diagnosing you with high blood pressure. This is because blood pressure normally varies throughout the day, and sometimes specifically during visits to the doctor, a condition called white coat hypertension. Your blood pressure generally should be measured in both arms to determine if there is a difference. It’s important to use an appropriate-sized arm cuff. Your doctor may ask you to record your blood pressure at home and at work to provide additional information.
Blood pressure normally rises with age and body size. Newborn babies often have very low blood pressure numbers that are considered normal for babies, while older teens have numbers similar to adults.
Table 2. Blood Pressure Levels – Adults
| Classification | Systolic and diastolic readings |
|---|---|
| Normal | Systolic: less than 120 mm Hg AND Diastolic: less than 80 mm Hg |
| Elevated | Systolic: 120–129 mm Hg AND Diastolic: less than 80 mm Hg |
| High blood pressure (Stage 1 hypertension) | Systolic: 130–139 mm Hg OR Diastolic: 80–89 mm Hg |
| High blood pressure (Stage 2 hypertension) | Systolic: 140 mm Hg or higher OR Diastolic: 90 mm Hg or higher |
| Hypertensive crisis (you should call your local emergency services number and see a doctor immediately) | Systolic: Higher than 180 mm Hg AND/OR Diastolic: Higher than 120 mm Hg |
Footnote: Healthy and unhealthy blood pressure ranges. A blood pressure reading between 120/80mmHg and 140/90mmHg could mean you’re at risk of developing high blood pressure if you don’t take steps to keep your blood pressure under control. A hypertensive crisis (high blood pressure crisis) is when blood pressure rises quickly and severely with readings of 180/120 or greater. If your blood pressure reading is 180/120 or greater and you are experiencing any other associated symptoms of target organ damage such as chest pain, shortness of breath, back pain, numbness/weakness, change in vision, or difficulty speaking then this would be considered a hypertensive emergency. Do not wait to see if your pressure comes down on its own, call your local emergency number immediately.
The consequences of uncontrolled blood pressure in this range can be severe and include:
- Stroke
- Loss of consciousness
- Memory loss
- Heart attack
- Damage to the eyes and kidneys
- Loss of kidney function
- Aortic dissection
- Angina (unstable chest pain)
- Pulmonary edema (fluid backup in the lungs)
- Eclampsia
An elevated reading may or may not be accompanied by one or more of the following symptoms:
- Severe headache
- Shortness of breath
- Nosebleeds
- Severe anxiety
Table 3. Blood Pressure Categories and Stages – Children
| For children aged 1–13 years | For children aged ≥ 13 years |
|---|---|
| Normal BP: < 90th percentile | Normal BP: < 120/< 80 mm Hg |
| Elevated blood pressure: ≥ 90th percentile to < 95th percentile or 120/80 mm Hg to < 95th percentile (whichever is lower) | Elevated blood pressure: 120/< 80 to 129/< 80 mm Hg |
| Stage 1 hypertension: ≥ 95th percentile to < 95th percentile + 12 mm Hg, or 130/80 to 139/89 mm Hg (whichever is lower) | Stage 1 hypertension: 130/80 to 139/89 mm Hg |
| Stage 2 hypertension: ≥ 95th percentile + 12 mm Hg, or ≥ 140/90 mm Hg (whichever is lower) | Stage 2 hypertension: ≥ 140/90 mm Hg |
- Most of the time there are no obvious symptoms for high blood pressure.
- The only way to find out if your blood pressure is high is to have your blood pressure checked.
- Certain physical traits and lifestyle choices can put you at a greater risk for developing high blood pressure.
- When left untreated, the damage that high blood pressure does to your circulatory system is a significant contributing factor to heart attack, stroke and other health threats.
Ask your doctor for a blood pressure reading at least every two years starting at age 18. If you’re age 40 or older, or you’re age 18-39 with a high risk of high blood pressure, ask your doctor for a blood pressure reading every year.
If you don’t regularly see your doctor, you may be able to get a free blood pressure screening at a health resource fair or other locations in your community. You can also find machines in some stores that will measure your blood pressure for free.
Public blood pressure machines, such as those found in pharmacies, may provide helpful information about your blood pressure, but they may have some limitations. The accuracy of these machines depends on several factors, such as a correct cuff size and proper use of the machines.
What is normal blood pressure?
For most adults, a normal blood pressure is less than 120/80 mmHg 2. An ideal blood pressure is usually considered to be between 90/60mmHg and 120/80mmHg. See your healthcare provider if your blood pressure readings are consistently higher than 120/80 mmHg. Blood pressure readings between 120/80mmHg and 140/90mmHg could mean you’re at risk of developing high blood pressure if you do not take steps to keep your blood pressure under control. For children younger than 13, blood pressure readings are compared with readings common for children of the same, age, sex, and height. In children younger than 13 years, elevated blood pressure is defined as blood pressure in the 90th percentile or higher for age, height, and sex, and hypertension is defined as blood pressure in the 95th percentile or higher 14. In adolescents 13 years and older, elevated blood pressure is defined as blood pressure of 120 to 129 mm Hg systolic and less than 80 mm Hg diastolic, and hypertension is defined as blood pressure of 130/80 mm Hg or higher.
Types of hypertension
There are two types of high blood pressure (hypertension).
Primary (essential) hypertension
For most adults, there’s no identifiable cause (idiopathic) of high blood pressure. This type of high blood pressure, called primary hypertension or essential hypertension, tends to develop gradually over many years. It has long been suggested that an increase in salt intake increases the risk of developing hypertension 15. One of the described factors for the development of essential hypertension is the patient genetic ability to salt response 16. About 50 to 60% of the patients are salt sensitive and therefore tend to develop hypertension 17.
Secondary hypertension
Some people have high blood pressure caused by an underlying condition. This type of high blood pressure, called secondary hypertension, tends to appear suddenly and cause higher blood pressure than does primary hypertension. Various conditions and medications can lead to secondary hypertension, including:
- Obstructive sleep apnea (OSA)
- Kidney disease
- Adrenal gland tumors
- Thyroid problems
- Certain defects you’re born with (congenital) in blood vessels
- Certain medications, such as birth control pills, cold remedies, decongestants, over-the-counter pain relievers and some prescription drugs
- Illegal drugs, such as cocaine and amphetamines
Isolated systolic hypertension
Isolated systolic hypertension is the predominant form of hypertension in the elderly population 18. Based on data from the National Health and Nutrition Examination Survey 1999-2010, approximately 30% of persons aged 60 years and above have untreated isolated systolic hypertension, as compared with 6% in adults aged 40 to 50 years and 1.8% in young adults aged 18 to 39 years 19. As per the Framingham Heart Study, a person aged 65 years with normal blood pressure has a 90% lifetime risk of developing hypertension. Among the elderly group, women and non-Hispanic Blacks have a higher prevalence of hypertensive disorders.
Isolated systolic hypertension is traditionally defined as systolic blood pressure above 140 mmHg with diastolic blood pressure of less than 90 mmHg 20. It is estimated that 15% of people aged 60 years and above have isolated systolic hypertension. Per the 2017 American College of Cardiology/American Heart Association Blood Pressure guidelines, however, a systolic blood pressure of 130 mmHg is now considered hypertensive at all ages 7. The new definition of hypertension will lead to an increased number of elderly being diagnosed with high blood pressure. Isolated systolic hypertension remains an important public health concern as chronically untreated high systolic blood pressure patients carry significant mortality and morbidity.
Most patients with isolated systolic hypertension have primary hypertension, which is also known as essential hypertension. Rarely, isolated systolic hypertension is attributed to other causes of secondary hypertension such as hypothyroidism/hyperthyroidism, chronic kidney disease, peripheral vascular disease, diabetes mellitus, aortic insufficiency, arteriovenous fistula, anemia, Paget disease, and atherosclerotic renal artery stenosis 21.
Isolated systolic hypertension, in most cases, develops as a result of the reduced elasticity of the arterial system 20. This is commonly seen among the elderly as there is increased deposition of calcium and collagen to the arterial wall 22. Hence, this may result in reduced compliance of the arterial vessels, decreased lumen-to-wall ratio, and increased thickening and fibrotic remodeling of the vascular intima and media. As a result, these stiffened conduit arteries lead to an increase in pulse pressure and pulse wave velocity, causing an elevation in systolic blood pressure and a further decline in diastolic blood pressure. Similarly, chronic diseases such as the above causes of secondary hypertension may contribute to the same pathological process by accelerating the deposition of calcium and collagen to the arterial system and the fibrotic remodeling of the vascular walls 23.
Malignant hypertension
Malignant hypertension also known as hypertensive crisis, is a term that has been used to describe patients with elevated blood pressure and multiple complications (end organ damage) with a poor prognosis. Today, the term malignant hypertension or hypertensive crisis is used to describe patients who present with severe BP elevations as follow 24:
- Systolic blood pressure greater than 180 mm Hg
- Diastolic blood pressure greater than 120 mm Hg
To make a diagnosis of malignant hypertension, papilledema has to be present 24. The diagnosis can be further classified as a hypertensive emergency when severe elevation in BP is associated with end-organ damage or hypertensive urgency when severe hypertension occurs without it. Prompt treatment of BP can prevent a hypertensive emergency and, consequently, serious life-threatening complications 25.
There are multiple causes of malignant hypertension (hypertensive crisis), including the following 24:
- Medication noncompliance
- Renovascular diseases, such as renal artery stenosis, polyarteritis nodosa, and Takayasu arteritis
- Renal parenchymal disease including glomerulonephritis, tubulointerstitial nephritis, systemic sclerosis, hemolytic-uremic syndrome, systemic lupus erythematosus
- Endocrine dysfunction, such as pheochromocytoma, Cushing disease, primary hyperaldosteronism, renin-secreting tumor
- Coarctation of aorta; drugs or other exposures, including cocaine, phencyclidine, sympathomimetics, erythropoietin, cyclosporine
- Antihypertensive medication withdrawal
- Amphetamines
- Central nervous system disorders, such as head injury, cerebral infarction, and cerebral hemorrhage
The prognosis of patients with malignant hypertension is guarded. Five-year survivals of 75% to 84% have been reported with treatment; without treatment, the life expectancy is less than 24 months. Most deaths are a result of heart failure, stroke, or renal failure.
Multiple complications can arise from hypertensive crisis when target organs are affected, including encephalopathy, intracerebral hemorrhage, acute myocardial infarction, acute heart failure, pulmonary edema, unstable angina, dissecting aortic aneurysm, acute kidney injury, and vision loss. Fortunately, most patients with malignant hypertension have no acute end-organ damage (hypertensive urgency). Nevertheless, some patients have signs and symptoms of acute, ongoing injury, which is recognized as hypertensive emergency.
In malignant hypertension (hypertensive emergency), the key is to lower the blood pressure within a few hours. However, it is not recommended to decrease the blood pressure too fast or too much, as ischemic damage can occur in vascular territories that have become habituated with the elevated level of blood pressure 24. For most hypertensive emergencies, mean arterial pressure (MAP) should be reduced by approximately 10 to 20% within the first hour and by another 5% to 15% over the next 24 hours 24. This often results in a target blood pressure of less than 180/120 mm Hg for the first hour and less than 160/110 mm Hg for the next 24 hours, but rarely less than 130/80 mm Hg during that time frame.
Common intravenous (IV) medications and doses used to treat malignant hypertension (hypertensive emergencies) include:
- Nicardipine, initial infusion rate 5 mg per hour, increasing by 2.5 mg per hour every 5 minutes to a maximum of 15 mg per hour
- Sodium nitroprusside, 0.3 to 0.5 mcg/kg/minute, increases by 0.5 mcg/kg per minute every few minutes as needed to a maximum dose of 10 mcg/kg per minute.
- Labetalol 10 to 20 mg IV followed by bolus doses of 20 to 80 mg at 10-minute intervals until a target blood pressure is reached to a maximum 300-mg cumulative dose
- Esmolol, initial loading dose 500 mcg/kg/minute over 1 minute, then 50 to 100 mcg/kg/minute to a maximum dose of 300 mcg/kg per minute.
If there is any possibility of over or underestimating BP using frequent noninvasive cuff measurements or if the end-organ damage is life-threatening, consider arterial catheterization for precise, second-to-second measurements allowing for more careful medication titration.
The major exceptions to gradual BP lowering over the first day are:
- Acute phase of an ischemic stroke: The BP is usually not treated unless it is greater than 185/110 mmHg in patients whose reperfusion therapy could be an option or greater than 220/120 mm Hg in patients who might not qualify for it. Consider labetalol or nicardipine infusion.
- Acute aortic dissection: The SBP should be lowered to 120 mm Hg within 20 minutes, and a target heart rate around 60 beats per minute to reduce aortic shearing forces. Treatment usually requires a beta-blocker and a vasodilator. Options include esmolol, nicardipine, or nitroprusside.
- An intracerebral hemorrhage: The goals of therapy are different and depend on the location and surgical approach.
- Acute myocardial ischemia: Nitroglycerin is the drug of choice; do not use if the patient has taken phosphodiesterase inhibitors, including sildenafil or tadalafil, within the past 48 hours.
After a suitable period, often 8 to 24 hours of BP control at a target, oral medications are usually given, and the initial intravenous therapy is tapered and discontinued.
Renovascular hypertension
Renovascular hypertension is one of the most common causes of secondary hypertension and often leads to resistant hypertension. Renovascular hypertension is defined as systemic hypertension that manifests secondary to the compromised blood supply to the kidneys, usually due to an occlusive lesion in the main renal artery 26. It is important to realize that any condition that compromises blood flow to the kidneys can contribute to renovascular hypertension 27. The underlying mechanism in renovascular hypertension involves decreased perfusion to the kidney and activation of the renin-angiotensin-aldosterone (RAAS) pathway. Renin secretion by the kidneys is stimulated by three main pathways, 1) renal baroreceptors that sense decreased perfusion to the kidney, 2) low sodium chloride levels detected by the macula densa and 3) beta-adrenergic stimulation. Prolonged kidney ischemia also increases the number of renin expressing cells in the kidney in a process called ‘juxtaglomerular (JG) recruitment’ 28. When renin is secreted into the blood, it acts on angiotensinogen (produced by the liver). Renin cleaves angiotensinogen to angiotensin 1, which is then converted to angiotensin 2 by angiotensin-converting enzyme (ACE) that is primarily found in the vascular endothelium of lungs and kidney. Angiotensin 2 raises blood pressure by multiple mechanisms, which include:
- Vasoconstriction, mostly in the heart, kidney, and vascular smooth muscle 29
- Sympathetic nervous stimulation causing a presynaptic release of norepinephrine
- Stimulates secretion of aldosterone by the adrenal cortex, which in turn causes sodium and water retention, thereby raising blood pressure.
- It also causes the increased synthesis of collagen type I and III in fibroblasts, leading to thickening of the vascular wall and myocardium, and fibrosis
- It has been shown to have a growth effect on renal cells, which has been implicated in the development of glomerulosclerosis and tubulointerstitial fibrosis
The most common causes of renovascular hypertension include 26:
- Renal artery stenosis (RAS), mostly secondary to atherosclerosis
- Fibromuscular dysplasia (FMD)
- Arteritides such as Takayasu’s arteritis, antiphospholipid antibody (APLA), or mid aortic syndrome 30
- Extrinsic compression of a renal artery
- Renal artery dissection or infarction
- Radiation fibrosis
- Obstruction from aortic endovascular grafts
The dominant cause (at least 85%) of renovascular hypertension in western countries is atherosclerotic renal artery stenosis (ARAS) and is mostly seen in older adults (>65 years) 27. This often develops as part of systemic atherosclerotic disease affecting multiple vascular beds, including coronary, cerebral and peripheral vessels. Community based studies suggest that up to 6.8% of individuals older than 65 have atherosclerotic renal artery stenosis (ARAS) more than 60% occlusion 31. Renal artery stenosis secondary to atherosclerosis has a higher prevalence in patients with known atherosclerotic disease (such as those with coronary artery disease, peripheral artery disease, or carotid artery stenosis) and autopsy studies have revealed that “greater than 25% of all patients who die of cardiovascular disease have some degree of renal artery stenosis” 32. Screening studies indicate rising prevalence of detectable atherosclerotic renal artery stenosis (ARAS) in hypertensive subjects from 3% (ages 50-59) to 25% (above age 70) with older ages 33. Clinically significant atherosclerotic renovascular disease often is manifest by worsening or accelerating blood pressure elevations in older individuals with pre-existing hypertension.
Fibromuscular dysplasia (FMD) is usually seen in young women and accounts for around 10% of renovascular hypertension and 5.8% of secondary hypertension 34. Fibromuscular dysplasia (FMD) can affect any arterial bed but most commonly affects the distal two-thirds of the renal artery 35.
Salient points in the history that suggest the presence of renovascular hypertension include:
- Resistant hypertension: Uncontrolled blood pressure necessitating the use of 2 or 3 antihypertensive agents of different classes, one of which is a diuretic
- Trial of multiple medications to control blood pressure
- History of multiple hospital admissions for hypertensive crisis
- Elevation in creatinine of more than 30% after starting an angiotensin-converting enzyme inhibitor (ACE-I)
- Patients with renal artery stenosis secondary to atherosclerosis are usually older and might have the presence of other atherosclerotic diseases such as carotid artery stenosis, peripheral artery stenosis, or coronary artery disease
- A premenopausal female (15-50 years) with hypertension is most likely to have fibromuscular dysplasia (FMD) 30
- Long term history of smoking
- Patients with systemic vasculitis can develop vasculitis of renal arteries and present with renovascular hypertension
- Recurrent episodes of flash pulmonary edema and/or unexplained congestive heart failure
- Unexplained azotemia
- Elevation in serum creatinine upon starting angiotensin-converting enzyme (ACE) inhibitor, which occurs due to interference with autoregulation and post glomerular arterial tone
- Unexplained hypokalemia and metabolic alkalosis
- Unilateral small or atrophic kidney
Physical examination may reveal an abdominal bruit, indicating the presence of renal artery stenosis.
Patients with renovascular hypertension often undergo an extensive evaluation to find a cause for uncontrolled hypertension.
Laboratory Tests include:
- Urine analysis: To check for proteinuria, hematuria, and casts. The presence of proteinuria (protein in urine) indicates the presence of renal parenchymal disorder, whereas the presence of hematuria (blood in urine) or red blood cell (RBC) casts indicates the presence of glomerulonephritis.
- Blood urea nitrogen and serum creatinine: To assess baseline kidney function.
- Basal metabolic profile: To assess for electrolyte disturbances and acid-base balance.
- Complement levels and autoimmune profile: In suspected cases of autoimmune diseases affecting the renal vasculature.
- Plasma free metanephrines or 24-hour urinary fractionated metanephrines and normetanephrine to rule out pheochromocytoma
- Plasma renin-aldosterone ratio to rule out hyperaldosteronism
- 24 hour urinary free cortisol or low dose dexamethasone suppression test to rule out Cushing’s syndrome
Imaging studies
There are multiple imaging modalities available to evaluate renovascular hypertension. Since the most common cause of renovascular hypertension is renal artery stenosis, renal arteriography remains the gold standard diagnostic test 35. However, catheter angiography is invasive, costly, time-consuming, and can lead to complications such as renal artery dissection or cholesterol embolization. Other imaging tests that can be done to evaluate the renal vessels include duplex ultrasonography, computed tomography with angiography (CTA), and magnetic resonance angiography (MRA). The type of imaging test used often depends on the suspicion for high-grade lesions, and the need for intervention 30.
Duplex ultrasonography is the initial imaging test of choice to evaluate the renal arteries. It is relatively inexpensive, non-invasive, and does not involve administration of contrast or exposure to radiation. A duplex scan has been shown to have an excellent correlation with contrast-enhanced angiography 36. Though there are several criteria to assess the presence of renal artery stenosis, the most important sign is peak systolic velocity (PSV). A peak systolic velocity (PSV) higher than 180 cm/s suggests the presence of stenosis of greater than 60% 37.
Duplex ultrasonography can also measure the resistive index (RI), which is calculated as (PSV-End diastolic velocity)/PSV. A value of more than 0.7 indicates the presence of pathological resistance to flow, and studies have shown that a value >0.8 predicts poor response to revascularization treatments 37. The most significant setbacks for duplex ultrasonography are its reduced sensitivity in obese patients, hindrance by overlying bowel gas, and operator dependence.
CT angiography (CTA) involves the administration of intravenous contrast and acquiring detailed images of blood vessels or tissues by moving the beam in a helical manner across the area being studied. In a study by Wittenberg et al 38, the sensitivity and specificity for hemodynamically significant renal artery stenosis (>50%) by CTA was found to be 96% and 99%. Computed tomography with angiography (CTA) also has a comparable negative predictive value to magnetic resonance angiography (MRA) in ruling out renal artery stenosis 39.
It can also diagnose extrinsic compression of renal arteries, fibromuscular dysplasia (FMD), arterial dissection, and help in evaluating surrounding structures. However, CT angiography (CTA) can only provide an anatomical assessment of the lesion and is not able to evaluate the degree of obstruction to renal blood flow. Exposure to radiation, allergy to contrast, and acute kidney injury are other downfalls of CT angiography (CTA).
Magnetic resonance angiography (MRA) uses a powerful magnetic field, pulses of radio waves, and intravenous gadolinium to evaluate the renal blood vessels and surrounding structures. Several studies have shown the sensitivity and specificity of magnetic resonance angiography (MRA) to be around 97% and 92% in diagnosing renal artery stenosis 39. MRA does not involve radiation, and gadolinium contrast is less likely to cause an allergic reaction as compared to the iodine contrast used in CTA. However, MRA has been shown to overestimate the grade of stenosis and is often affected by motion artifacts or opacification of renal veins, leading to difficulty visualizing the renal arteries 39. Also, gadolinium has been shown to induce a rare, progressively fatal disease called nephrogenic systemic fibrosis (NSF). NSF can affect the skin, joints, and multiple organs leading to progressive, irreversible fibrosis and eventual death. This occurs due to a transmetalation reaction that displaces gadolinium ion from its chelate, resulting in the deposition of gadolinium in the skin and soft tissues. The 1-year incidence of NSF has been reported to be around 4.6% and almost all cases occurred in patients with a glomerular filtration rate < 30 mL/min/1.73 m² 40.
In comparative studies, the positive predictive value of MRA was found to be higher than CTA due to increased false-positive rates with CTA. Negative predictive values are high for both CTA and MRA (>98% for both) 39. Both modalities can exclude significant renal artery lesions with a high degree of certainty. Both MRA and CTA have also shown to be effective for the diagnosis of FMD, with the sensitivity of CTA being the best (84.2%) when compared to angiography 41.
Nuclear medicine ACE-inhibitor (ACE-I) renography is another non-invasive, relatively safe imaging method that uses radioactive material, a special camera, and a computer to evaluate for renovascular hypertension. It involves the administration of an ACE-inhibitor (ACE-I) to determine if the cause of hypertension is due to the narrowing of the renal arteries. The sensitivity and specificity of this test have shown to be variable, with values between 74% – 94% for sensitivity and 59% – 95% for specificity 42. It is a time-consuming procedure, and there is a risk of radiation exposure and irritation or pain from the injection of the radiotracer. The sensitivity of ultrasound has shown to be higher than captopril renography which makes it a better choice for an initial diagnostic test 43.
Catheter angiography is the gold standard test to evaluate for renovascular hypertension and provides the best temporal and spatial resolution. Catheter angiography has the added advantage of measuring translesional pressure gradients to assess the hemodynamic significance of anatomically severe lesions 44. Catheter angiography is most useful in:
- Patients with a disparity between imaging modalities
- Patients with a high index of suspicion and negative imaging findings
- Patients anticipated of needing an intervention
Catheter angiography can also evaluate anatomical abnormalities of the kidney, renal arteries, aorta, and can be followed by endovascular intervention for the treatment of significant lesions. Also, the surrounding tissues and bones can be removed or subtracted from the final image revealing only the arterial framework. This method is known as digital subtraction angiography (DSA). However, the radiation doses are higher than CTA, and because it is an invasive procedure, there are risks of complications such as arterial dissection, tear, rupture, or thromboembolic phenomenon 44.
The management of renovascular hypertension aims to treat the underlying cause. Several options are available, which include pharmacological and invasive therapy. Renovascular hypertension due to atherosclerotic renal artery stenosis should be primarily managed medically as multiple studies have failed to show renal or cardiovascular benefits with invasive management.
Pharmacological therapy entails the use of antihypertensive medications to control blood pressure. The American College of Cardiology and the American Heart Association advocates pharmacological therapy as the first-line treatment for renal artery stenosis 45. Since renin-angiotensin-aldosterone (RAAS) is the most prominent pathway contributing to hypertension in these disorders, ACE-inhibitors (ACE-Is) and angiotensin II receptor blockers (ARBs) form the cornerstone of managing renovascular hypertension. Often more than one medication will be needed to control the blood pressure. Calcium channel blockers, thiazides, beta-blockers, and hydralazine have been shown to be effective to control blood pressure in patients with renal artery stenosis 46. Direct renin inhibitors such as aliskiren have been studied as monotherapy or in combination with ACE-inhibitors (ACE-Is) and angiotensin 2 receptor blockers (ARBs) to treat hypertension. Though it has been shown to be effective for the treatment of hypertension there is not enough data to prove its efficacy in treating renovascular hypertension 47.
ACE-inhibitors (ACE-Is) and angiotensin II receptor blockers (ARBs) inhibit the action of angiotensin II, thereby causing vasodilation and promote sodium and water excretion. However, these medications are contraindicated in patients with a single functioning kidney or bilateral lesions as they can cause efferent arteriolar vasodilatation leading to interruption in autoregulation and thereby decreasing glomerular filtration. While these medications are effective in controlling blood pressure, they can also lead to worsening renal function.
Percutaneous angioplasty is the treatment of choice for renovascular hypertension due to fibromuscular dysplasia (FMD) and for patients with atherosclerotic renal artery stenosis that is not controlled with medications 48. The American College of Cardiology and the American Heart Association guidelines recommend revascularization for renal artery disease in the following scenarios 46:
- Patients with hemodynamically significant renal artery stenosis and recurrent, unexplained congestive heart failure or sudden, unexplained pulmonary edema
- Hemodynamically significant renal artery stenosis and accelerated hypertension, resistant hypertension, malignant hypertension or hypertension with an unexplained unilateral small kidney, and hypertension with intolerance to medication
- Patients with bilateral renal artery stenosis and progressive chronic kidney disease or a renal artery stenosis to a solitary functioning kidney
- Patients with hemodynamically significant renal artery stenosis and unstable angina
- Asymptomatic bilateral or solitary viable kidney with hemodynamically significant renal artery stenosis
- Patients with renal artery stenosis and chronic renal insufficiency with unilateral renal artery stenosis
- In addition to angioplasty, renal stent placement is indicated for patients with ostial atherosclerotic lesions
Patients with fibromuscular dysplasia (FMD) and renovascular hypertension are also treated with percutaneous intervention with or without a stent 48. Multiple studies have shown a decrease in baseline blood pressure after intervention for fibromuscular dysplasia (FMD) 49. However, there remains an ongoing debate about the benefit of revascularization when compared to medical management in patients with atherosclerotic renal artery stenosis (ARAS). Several studies have failed to show a significant decrease in blood pressure or the number of antihypertensive agents between angioplasty and medical treatment groups. A meta-analysis of 7 trials by Zhu et al. 50 revealed that medical management is as effective as percutaneous revascularization in the treatment of renal artery stenosis. Three recent trials: the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) 51, Cardiovascular Outcomes in Renal Atherosclerotic Lesions (CORAL) 52, and STAR 53 found no difference between stenting and medical therapy in patients with atherosclerotic renal artery stenosis. Thus it can be established that revascularization does not reverse renal damage or decrease blood pressure in patients with atherosclerotic renal artery stenosis.
In the case of recurrent renal artery stenosis or blood pressure not controlled with medication and or/angioplasty, renal bypass surgery may be an option. In this procedure, the surgeon uses a vein or synthetic tube to connect the kidney to the aorta, to create an alternate route for blood to flow around the blocked artery into the kidney. This is a complex procedure and rarely used. The American College of Cardiology and the American Heart Association guidelines recommend surgery for renal artery stenosis in 46:
- Patients with renal artery stenosis secondary to fibromuscular dysplasia (FMD), especially those with complex disease and/or those having microaneurysms
- Patients with atherosclerotic renal artery stenosis involving multiple vessels or involvement of early primary branch of the main renal artery
- Patients with atherosclerotic renal artery stenosis who require pararenal aortic reconstructions (such as with aortic aneurysms or severe aortoiliac obstruction)
Several studies have also evaluated the role of unilateral nephrectomy in patients with renovascular hypertension and have shown improvement in blood pressure control, renal function, and a decrease in the use of anti-hypertensives 54. However, this is an invasive procedure with inherent risks and the long-term consequences of such a procedure are unclear.
Untreated renovascular hypertension can also lead to end-stage renal failure with a median survival time of 25 months and a 4-year mortality rate of 35% 26.
Hypertension in pregnancy
Some women have high blood pressure before they get pregnant. Others have high blood pressure for the first time during pregnancy. About 8 in 100 women (8 percent) have some kind of high blood pressure during pregnancy. If you have high blood pressure, talk to your health care provider. Managing your blood pressure can help you have a healthy pregnancy and a healthy baby.
Two kinds of high blood pressure that can happen during pregnancy:
- Chronic hypertension. Chronic hypertension is high blood pressure that you have before you get pregnant or that develops before 20 weeks of pregnancy. Chronic hypertension doesn’t go away once you give birth. Chronic hypertension is diagnosed per American College of Cardiology and the American Heart Association and American College of Obstetricians and Gynecologists guidelines as an in-office measurement with systolic blood pressure greater than 140 mmHg or diastolic blood pressure greater than 90mmHg confirmed with either ambulatory blood pressure monitoring, home blood pressure monitoring, or blood pressure evaluation with serial office visits, with elevated pressures at least 4 hours apart prior to 20 weeks gestation 55, 56, 57. About 1 in 4 women with chronic hypertension (25 percent) has preeclampsia during pregnancy. If you’re at high risk for preeclampsia, your health care provider may treat you with low-dose aspirin to prevent it. Your health care provider will check your blood pressure and urine at each prenatal care visit. You may need to check your blood pressure at home, too. Your health care provider may also use ultrasound and fetal heart rate testing to check your baby’s growth and health. Your health care provider also checks for signs of preeclampsia. If you were taking medicine for chronic hypertension before pregnancy, your health care provider makes sure it’s safe to take during pregnancy. If it’s not, he/she switches you to a safer medicine. Some blood pressure medicines, called ACE inhibitors (ACE-I) and angiotensin II receptor blockers (ARBs), can harm your baby during pregnancy. During the first half of pregnancy, blood pressure often falls. If you have mild hypertension and took medicine for it before pregnancy, your health care provider may lower the dose of medicine you take. Or you may be able to stop taking medicine during pregnancy. Don’t stop taking any medicine before you talk to your health care provider. Even if you didn’t take blood pressure medicine in the past, you may need to start taking it during pregnancy.
- Gestational hypertension. Gestational hypertension is high blood pressure that only pregnant women can get. Gestational hypertension is defined per American College of Obstetricians and Gynecologists guidelines as blood pressure greater than or equal to 140 mmHg systolic or 90mmHg diastolic on two separate occasions at least four hours apart after 20 weeks of pregnancy when previous blood pressure was normal with no excess protein in their urine or other signs of organ damage. Alternatively, a patient with systolic blood pressure greater than 160 mmHg or diastolic blood pressure greater than 110 mmHg can be confirmed to have gestational hypertension if they have a similar pressure after a short interval. This is in order to ensure timely antihypertensive treatment. Gestational hypertension starts after 20 weeks of pregnancy and usually goes away after you give birth. It usually causes a small rise in blood pressure, but some women develop severe hypertension and may be at risk for more serious complications later in pregnancy, like preeclampsia.
- Chronic hypertension with superimposed preeclampsia. This condition occurs in women who have been diagnosed with chronic high blood pressure before pregnancy, but then develop worsening high blood pressure and protein in the urine or other health complications during pregnancy.
Hypertensive disorders of pregnancy includes chronic hypertension, with or without superimposed pre-eclampsia/eclampsia, gestational hypertension, HELLP syndrome, preeclampsia with or without severe features or eclampsia present a significant risk of morbidity to both mother and fetus. HELLP stands for hemolysis (H), elevated liver enzymes (EL), low platelet count (LP) syndrome.
High blood pressure in pregnancy can cause problems for you and your baby during pregnancy, including 58:
- Problems for moms include:
- Preeclampsia. Preeclampsia is a complication of pregnancy in which affected women develop high blood pressure (hypertension); they can also have abnormally high levels of protein in their urine (proteinuria) and signs of damage to another organ system, most often the liver and kidneys. Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had been normal or after giving birth (called postpartum preeclampsia). Signs and symptoms of preeclampsia include having protein in the urine, changes in vision and severe headaches. Preeclampsia can be a serious medical condition. Even if you have mild preeclampsia, you need treatment to make sure it doesn’t get worse. Without treatment, preeclampsia can cause serious health problems, including kidney, liver and brain damage. In rare cases, it can lead to life-threatening conditions called eclampsia and HELLP syndrome. Eclampsia causes seizures and can lead to coma. HELLP syndrome stands for hemolysis (H) which is the destruction of red blood cells, elevated liver enzymes (EL), low platelet count (LP) syndrome. HELLP syndrome is a more severe form of preeclampsia, and can rapidly become life-threatening for both you and your baby. Left untreated, preeclampsia can lead to serious — even fatal — complications for both you and your baby. If you have preeclampsia, the most effective treatment is delivery of your baby. Even after delivering the baby, it can still take a while for you to get better.
- Gestational diabetes. This is a kind of diabetes that only pregnant women get. It’s a condition in which your body has too much sugar (also called glucose). Most women get a test for gestational diabetes at 24 to 28 weeks of pregnancy.
- Heart attack (also called myocardial infarction).
- Kidney failure. This is a serious condition that happens when the kidneys don’t work well and allow waste to build up in the body.
- Placental abruption. This is a serious condition in which the placenta separates from the wall of the uterus before birth. If this happens, your baby may not get enough oxygen and nutrients in the womb. You also may have serious bleeding from the vagina. The placenta grows in the uterus and supplies the baby with food and oxygen through the umbilical cord.
- Postpartum hemorrhage (PPH). This is when a woman has heavy bleeding after giving birth. It’s a serious but rare condition. It usually happens 1 day after giving birth, but it can happen up to 12 weeks after having a baby.
- Pulmonary edema. This is when fluid fills the lungs and leads to shortness of breath.
- Stroke. This is when blood flow to your brain stops. Stroke can happen if a blood clot blocks a vessel that brings blood to the brain or when a blood vessel in the brain bursts open.
- Pregnancy related death. This is when a woman dies during pregnancy or within 1 year after the end of her pregnancy from health problems related to pregnancy.
If you have high blood pressure during pregnancy, you’re also more likely have a cesarean birth (also called c-section). This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
- Problems for babies include:
- Premature birth. This is birth that happens too early, before 37 weeks of pregnancy. Even with treatment, a pregnant woman with severe high blood pressure or preeclampsia may need to give birth early to avoid serious health problems for her and her baby.
- Fetal growth restriction. High blood pressure can narrow blood vessels in the umbilical cord. This is the cord that connects the baby to the placenta. It carries food and oxygen from the placenta to the baby. If you have high blood pressure, your baby may not get enough oxygen and nutrients, causing him to grow slowly.
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces.
- Fetal death. When a baby dies spontaneously in the womb at any time during pregnancy.
- Neonatal death. This is when a baby dies in the first 28 days of life.
To manage high blood pressure during pregnancy:
- Go to all your prenatal care checkups, even if you’re feeling fine.
- If you need medicine to control your blood pressure, take it every day. Your doctor can help you choose one that’s safe for you and your baby.
- If you have severe preeclampsia or HELLP syndrome, corticosteroid medications can temporarily improve liver and platelet function to help prolong your pregnancy. Corticosteroids can also help your baby’s lungs become more mature in as little as 48 hours — an important step in preparing a premature baby for life outside the womb.
- If your preeclampsia is severe, your doctor may prescribe an anticonvulsant medication, such as magnesium sulfate, to prevent a first seizure.
- Do not take any extra vitamins, calcium, aspirin, or other medicines without talking with your doctor first.
- Check your blood pressure at home. Ask your doctor what to do if your blood pressure is high.
- Eat healthy foods. Don’t eat foods that are high in salt, like soup and canned foods. They can raise your blood pressure.
- Stay active. Being active for 30 minutes each day can help you manage your weight, reduce stress and prevent problems like preeclampsia.
- Don’t smoke, drink alcohol or use street drugs or abuse prescription drugs.
- Contact your doctor immediately or go to an emergency room if you have severe headaches, blurred vision or other visual disturbance, severe pain in your abdomen, or severe shortness of breath. Because headaches, nausea, and aches and pains are common pregnancy complaints, it’s difficult to know when new symptoms are simply part of being pregnant and when they may indicate a serious problem — especially if it’s your first pregnancy. If you’re concerned about your symptoms, contact your doctor.
Pulmonary hypertension
Pulmonary hypertension is a potentially life-threatening condition caused by high blood pressure in the arteries of the lungs (pulmonary arteries), which leads to damage to the right side of the heart. In pulmonary hypertension the walls of the pulmonary arteries become thick and stiff, and cannot expand as well to allow blood to flow through. The reduced blood flow into your lungs makes it harder for the right side of your heart to pump blood through the pulmonary arteries. This increase in pressure can damage your heart. If the right side of your heart has to continually work harder, it can gradually become weaker. This can lead to heart failure. Pulmonary hypertension can also cause other symptoms such as shortness of breath, chest pain, tiredness, a racing heartbeat (palpitations), swelling (edema) in the legs, ankles, feet or tummy (abdomen) and lightheadedness. These symptoms often get worse during exercise, which can limit your ability to take part in physical activities.
Pulmonary hypertension can occur alone or be caused by another disease or condition 59:
- One type of pulmonary hypertension is pulmonary arterial hypertension (PAH). Pulmonary arterial hypertension (PAH) is caused by changes in the smaller branches of the pulmonary arteries.
- Left heart diseases, such as left heart failure, which may be caused by high blood pressure throughout your body or coronary heart disease
- Other heart and blood vessel diseases such as congenital (inherited) heart defects
- Lung diseases or a shortage of oxygen in the body (hypoxia)
- Blood clots that cause narrowing or a blockage in the pulmonary arteries
- Other medical conditions such as liver disease, sickle cell disease or connective tissue disorders like scleroderma
Several factors can increase your risk of developing pulmonary hypertension:
- Age: Pulmonary hypertension can occur at any age, but your risk increases as you get older. The condition is usually diagnosed between ages 30 and 60.
- Environment: You may be at an increased risk of pulmonary hypertension if you have or are exposed to asbestos or certain infections caused by parasites.
- Family history and genetics: Certain genetic disorders, such as Down syndrome, congenital heart disease, and Gaucher disease, can increase your risk of pulmonary hypertension. A family history of blood clots also increases your risk.
- Lifestyle habits: Unhealthy lifestyle habits such as smoking and illegal drug use can raise your risk of developing pulmonary hypertension.
- Medicine: Some prescribed medicines used to treat cancer and depression may increase your risk of pulmonary hypertension.
- Sex: Pulmonary hypertension is more common in women than in men. Pulmonary hypertension with certain types of heart failure is also more common in women.
In the United States, the most common cause of pulmonary hypertension is left heart disease, such as left heart failure. There are several other medical conditions and environmental factors that can increase the risk of developing pulmonary hypertension. As a disease on its own pulmonary hypertension is rare – affecting between 10 and 57 people per million – but it leads to heart damage. Pulmonary hypertension can lead to death from heart failure within a few years. Some patients will need a lung transplant, or heart-lung transplant.
To diagnose pulmonary hypertension, your doctor may ask you questions about your medical history and do a physical exam. Based on your symptoms and risk factors, your doctor may refer you to a lung specialist (pulmonologist) or a heart and blood vessel specialist (cardiologist). Your doctor will diagnose you with pulmonary hypertension if tests show higher-than-normal pressure in the arteries of the lungs (pulmonary arteries).
The most common tests that doctors use to diagnose pulmonary hypertension is to measure the pressure in your pulmonary arteries using cardiac catheterization and echocardiography. Normal pressure in the pulmonary arteries is between 11 and 20 mm Hg. If the pressure is too high, you may have pulmonary hypertension. A pressure of 25 mmHg or greater measured by cardiac catheterization or 35 to 40 mmHg or greater on echocardiography suggests pulmonary hypertension.
Other tests use to diagnose pulmonary hypertension may include:
- Blood tests look for blood clots, stress on the heart, or anemia.
- Heart imaging tests, such as cardiac MRI, take detailed pictures of the structure and functioning of the heart and surrounding blood vessels.
- Lung imaging tests, such as chest X-ray, looks at the size and shape of the heart and surrounding blood vessels, including the pulmonary arteries.
- Electrocardiogram (ECG or EKG) looks for changes in the electrical activity of your heart. This can help detect if certain parts of the heart are damaged or working too hard. In pulmonary hypertension, the heart can become overworked due to damage or changes in the pulmonary arteries.
Pulmonary hypertension treatment
Treatments for pulmonary hypertension will depend on the cause of the condition. Pulmonary hypertension usually gets worse over time. Left untreated, it may cause heart failure, which can be fatal, so it’s important treatment is started as soon as possible.
Many times, there is not a cure for pulmonary hypertension, but your healthcare provider can work with you to manage the symptoms and help you manage your condition. This may include medicine or healthy lifestyle changes.
If another condition is causing pulmonary hypertension, the underlying condition should be treated first. This can sometimes prevent the pulmonary arteries being permanently damaged.
Medicines to treat pulmonary hypertension may include:
- Anticoagulant medicines or blood thinners to prevent blood clots in people whose pulmonary hypertension is caused by chronic blood clots in the lungs. These blood thinners also can help some people who have pulmonary arterial hypertension (PAH), heart failure, or other risk factors for blood clots.
- Digitalis or digoxin to control the rate blood is pumped throughout the body. Digoxin can improve your symptoms by strengthening your heart muscle contractions and slowing down your heart rate
- Vasodilator therapy to relax blood vessels and lower blood pressure in the pulmonary artery most affected in people who have pulmonary arterial hypertension. This includes calcium channel blockers such as nifedipine, diltiazem, nicardipine and amlodipine, as well as newer groups of medicines called endothelin receptor antagonists (bosentan, ambrisentan and macitentan), phosphodiesterase type 5 inhibitors (sildenafil and tadalafil), prostaglandins (epoprostenol, iloprost and treprostinil) and soluble guanylate cyclase stimulators (riociguat).
- Diuretics (water tablets) to remove excess fluid as a result of heart failure
Home oxygen treatment may also be prescribed if the level of oxygen in your blood is low.
Your doctor may recommend a procedure or surgery to treat pulmonary hypertension:
- Pulmonary endarterectomy – a surgery to remove old blood clots from the pulmonary arteries in the lungs of people with chronic thromboembolic pulmonary hypertension.
- Balloon pulmonary angioplasty – a new procedure where a tiny balloon is guided into the pulmonary arteries and inflated for a few seconds to push the blockage aside and restore blood flow to the lung; it may be considered if pulmonary endarterectomy is not suitable, and has been shown to lower blood pressure in the lung arteries, improve breathing, and increase the ability to exercise.
- Atrial septostomy to decrease pressure in the right heart chambers and improve the output of the left heart and oxygenation of the blood. In this procedure, a small hole is made in the wall between the right and left atria to allow blood to flow from the right to the left atrium.
- Transplant surgery – in severe cases, a lung transplant or a heart-lung transplant may be needed; this type of surgery is rarely used because effective medicine is available
Your doctor may also recommend medicines or procedures to treat the condition that is causing your pulmonary hypertension:
- Blood pressure medicines such as angiotensin-converting enzymes inhibitors (ACE-I), beta blockers, or calcium channel blockers (CCB) when left heart disease is the cause
- Blood transfusions or hydroxyurea to treat sickle cell disease
- Heart valve repair
- Iron supplements to increase blood iron levels and improve anemia
The outlook for pulmonary hypertension varies, depending on factors such as:
- what’s causing it
- how quickly it’s diagnosed
- how advanced your symptoms are
- whether you have another underlying health condition
The specialist in charge of your care will be able to give you more detailed information.
Having pulmonary hypertension can affect your ability to carry out everyday activities. Your doctor may recommend the following to monitor your condition and treatment response:
- Six-minute walk test to monitor your ability to exercise
- Blood tests to check hemoglobin, iron, and electrolyte levels; kidney, liver, and thyroid function; your blood’s ability to clot; and signs of stress on the heart
- Cardiac catheterization
- Cardiac MRI to monitor your heart’s size and how well it is working
- Chest X-ray
- Echocardiography to monitor your heart’s size and how well it is working, and measure the pressure in your right heart chambers
- Electrocardiogram to check for irregular heartbeats
- Lung function tests to check for any change in your lung function
If your pulmonary hypertension is severe or does not respond to treatment, your doctor may talk to you about a lung transplant or a heart and lung transplant.
Portal hypertension
Portal hypertension is abnormally high blood pressure in the portal vein (the large vein that brings blood from the intestine to the liver) and its branches. The portal vein receives blood from the entire intestine and from the spleen, pancreas, and gallbladder and carries that blood to the liver. After entering the liver, the portal vein divides into right and left branches and then into tiny channels that run through the liver. When blood leaves the liver, it flows back into the general circulation through the hepatic vein.
Portal hypertension is a common complication of cirrhosis and, less commonly, alcoholic hepatitis. When the liver becomes severely scarred, it’s harder for blood to move through it. This leads to an increase in the pressure of blood around the intestines.
The blood must also find a new way to return to your heart. It does this by using smaller blood vessels. Most often it goes through blood vessels in your stomach, esophagus, or intestines. But these blood vessels are not designed to carry the weight of blood, so they can become stretched out and weakened. These weakened blood vessels are known as varices. If the blood pressure rises to a certain level, it can become too high for the varices to cope with, causing the walls of the varices to split and bleed. Bleeding from esophageal varices is a medical emergency and can be fatal. The bleeding can be rapid and massive, causing you to vomit blood and pass stools that are very dark or tar-like. Alternatively, long-term bleeding can lead to anemia.
Usually, doctors can recognize portal hypertension based on symptoms and findings during the physical examination. Doctors can usually feel an enlarged spleen when they examine the abdomen. They can detect fluid in the abdomen by noting abdominal swelling and by listening for a dull sound when tapping (percussing) the abdomen.
Ultrasonography may be used to examine blood flow in the portal vein and nearby blood vessels and to detect fluid in the abdomen. Ultrasonography, magnetic resonance imaging (MRI), or computed tomography (CT) can be used to look for and examine collateral vessels.
Less commonly, a catheter is inserted through an incision in the neck and threaded through blood vessels into the liver to measure pressure in the portal blood vessels.
Treatment of portal hypertension
- For bleeding from esophageal varices, drugs to slow bleeding, blood transfusions, and/or endoscopy. Drugs such as vasopressin or octreotide may be given intravenously to make the bleeding veins contract and thus slow the bleeding. Blood transfusions are given to replace lost blood. Doctors usually use a flexible viewing tube (endoscope), inserted through the mouth into the esophagus to confirm that the bleeding is from varices. Working through the endoscope, doctors can use rubber bands to tie off the veins or hardened chemicals in the swollen blood vessels to block them off. To reduce the risk of bleeding from esophageal varices, doctors may try to reduce pressure in the portal vein. One way is to give beta-blocker drugs, such as timolol, propranolol, nadolol, or carvedilol.
- Sometimes surgery to reroute blood flow (portosystemic shunting). Portosystemic shunting may be done to connect the portal vein or one of its branches to a vein in the general circulation. This procedure reroutes most of the blood that normally goes to the liver so that it bypasses the liver. This bypass (called a shunt) lowers pressure in the portal vein because pressure is much lower in the general circulation. There are various types of portosystemic shunt procedures. In one type, called transjugular intrahepatic portosystemic shunting (TIPS), doctors, using x-rays for guidance, insert a catheter with a needle into a vein in the neck and thread it to veins in the liver. The catheter is used to create a passage (shunt) that connects the portal vein (or one of its branches) directly with one of the hepatic veins. Less commonly, portosystemic shunts are created surgically.
- If surgery doesn’t work or you have liver failure, you may need a liver transplant.
Intracranial hypertension
Intracranial hypertension is a general term for the neurological disorders in which cerebrospinal fluid (CSF) pressure within the skull is too high. “Intracranial” means “within the skull.” “Hypertension” means “high fluid pressure.” Intracranial hypertension in adults is generally defined as intracranial pressure that reaches 250 millimeters of water (mm H2O) or above. Old names for intracranial hypertension include Benign Intracranial Hypertension and Pseudotumor Cerebri 60.
For adults:
- Normal intracranial pressure readings are generally below 200 mm H2O
- Borderline high intracranial pressure readings are between 200-250 mm H2O
- Anything above 250 mm H2O is considered a high pressure reading.
For young children:
- Anything above 200 mm H2O is considered a high pressure reading.
Cerebrospinal fluid (CSF) is one of three major components inside the skull; the other two are the blood supply (the arteries and veins known as the vasculature) that the brain requires to function and the brain itself. Cerebrospinal fluid (CSF) has several important functions. It cushions the brain within the skull, transports nutrients to brain tissue and carries waste away. CSF is produced at a site within the brain called the choroid plexus, which generates about 400-500 ml (one pint) of the fluid each day or approximately 0.3 cc per minute. The total volume of CSF in the skull at any given time is around 140 ml. That means the body produces, absorbs and replenishes the total volume of CSF about 3-4 times daily.
Cerebrospinal fluid (CSF) flows from the choroid plexus through the brain’s four, interconnecting ventricles before finally entering the sub-arachnoid space, which surrounds the brain and spinal cord. The fluid then flows over the brain and spinal cord and is eventually absorbed into the venous blood system through tiny, one-way channels called arachnoid granulations or villi. When this continuous cycle of CSF production, circulation and absorption functions normally, it regulates the volume of CSF in the skull and the fluid pressure remains at a constant level. In other words, the CSF production rate remains equal to the CSF absorption rate. Intracranial pressure is determined by the three main components within the skull —brain tissue, blood and cerebrospinal fluid (CSF)— working together. Under normal circumstances, these three components maintain a dynamic equilibrium. In order for this balance to be maintained, it is believed that CSF, which is produced at approximately 0.3 cc per minute, must also exit the skull at the same rate. But when the body cannot effectively absorb or drain CSF, intracranial pressure increases within the skull, which is made of bone and cannot expand. And since the brain and the vasculature can only be compressed so far, intracranial pressure must rise. Intracranial hypertension in adults is defined as CSF pressure at 250 mmH2O or above. In chronic intracranial hypertension, the exiting (or egress) of CSF is thought to be impaired while simultaneously the CSF productions continues, which leads to elevated intracranial pressure.
Intracranial hypertension can be divided into two categories:
- Acute intracranial hypertension
- Chronic intracranial hypertension
Acute intracranial hypertension often occurs as the result of severe head injury or intracranial bleeding from an aneurysm or a stroke. It is characterized by a very rapid onset after the initial injury and extremely high intracranial pressure that can be fatal. The underlying cause of acute intracranial hypertension is brain-swelling or intracranial bleeding into the sub-arachnoid space that surrounds the brain. In many cases, a piece of skull is surgically removed to accommodate brain swelling and lower intracranial pressure. This can be life-saving.
In contrast, chronic intracranial hypertension is a neurological disorder in which the increased cerebrospinal fluid (CSF) pressure has generally arisen and remains elevated over a sustained period of time. It can either occur without a detectable cause (idiopathic intracranial hypertension or pseudotumor cerebri) or be triggered by an identifiable cause such as an underlying disease or disorder, injury, drug or cerebral blood clot (secondary intracranial hypertension). Chronic intracranial hypertension is frequently a life-long illness with significant physical, financial and emotional impact. Chronic intracranial hypertension can cause both rapid and progressive changes in vision. Vision loss and blindness due to chronic intracranial hypertension are usually related to optic nerve swelling (papilledema), which is caused by high CSF pressure on the nerve and its blood supply. In addition, individuals with chronic intracranial hypertension often suffer severe pain. The most common form is a chronic headache, which is generally unresponsive to the most potent pain medication.
Anyone can develop chronic intracranial hypertension, regardless of age, gender, ethnicity, race or body type. While the chronic form of intracranial hypertension is not usually fatal, current treatments for the disorder can result in serious, sometimes life-threatening complications.
Researchers are eager to identify the mechanism that underlies chronic intracranial hypertension. While no one is sure why intracranial hypertension happens, some researchers believe that the answer may involve resistance or obstruction of CSF outflow through the exiting pathways from the brain.
Symptoms of chronic intracranial hypertension can include 61:
- Constant throbbing headaches that are generally nonspecific in location, type and frequency and can be associated with nausea and vomiting. Headaches may be worse in the morning, or when coughing or straining; it may improve when standing up
- Pulsatile tinnitus is a rhythmic or pulsating ringing heard in one or both ears.
- Horizontal double vision can be a sign of pressure on the 6th cranial nerve(s).
- Nonspecific radiating pain in the arms or legs (radicular pain).
- Transient obscurations of vision, which are temporary dimming or complete blacking out of vision. Your vision may become dark or “greyed out” for a few seconds at a time; this can be triggered by coughing, sneezing or bending down
- Visual field defects. These defects can occur in the central as well as the peripheral vision.
- Loss of color vision.
- Feeling and being sick
- Feeling sleepy
- Feeling irritable
Chronic intracranial hypertension can sometimes result in permanent vision loss, although treatment can help to reduce the chances of this happening.
The cause of chronic intracranial hypertension is usually not known (idiopathic intracranial hypertension). A common explanation for increased intracranial pressure is a problem with the reabsorption of cerebrospinal fluid (CSF) back into the body, which causes the pressure to increase. Sometimes the cause is found and then it is called secondary intracranial hypertension.
Possible causes of chronic intracranial hypertension include:
- a blood clot on the surface of your brain, known as a chronic subdural hematoma
- a brain tumor
- an infection in your brain, such as meningitis or encephalitis
- hydrocephalus, where fluid builds up around and inside your brain
- abnormal blood vessel, such as an arteriovenous fistula or arteriovenous malformation
- a blood clot in one of the veins of your brain, known as a venous sinus thrombosis
Rare causes include a blockage in the circulation of fluid at the bottom of the skull (Chiari malformation), inflammation of the blood vessels in the brain (vasculitis) and abnormal skull growth in children (craniosynostosis).
Causes of secondary intracranial hypertension include:
- Certain medications such as oral contraceptives, steroids, vitamin A, Isotretinoin, lithium, growth hormone, nitrofurantoin, phenytoin, sulfa drugs, minocycline, Tamoxifen, naladixic acid, thyroid replacement, tetracycline, and some chemotherapeutic drugs.
- Medical conditions such as dural venous sinus thrombosis, kidney disease, head injuries, Lyme disease, lupus, acute sinusitis or mastoiditis, measles, blood clotting disorders, anemia, leukemia, periodic fever and meningitis.
In many cases, the cause of chronic intracranial hypertension is unclear. This is known as idiopathic intracranial hypertension or benign intracranial hypertension (pseudotumor cerebri). It mainly affects women in their 20s and 30s, and has been associated with:
- being overweight or obese – most cases happen in overweight women, although it’s not clear why
- hormone problems such as Cushing’s syndrome, hypoparathyroidism, an underactive thyroid (hypothyroidism) or an overactive thyroid (hyperthyroidism)
- certain medicines including some antibiotics, steroids and the combined contraceptive pill
- a lack of red blood cells (iron deficiency anaemia) or too many red blood cells (polycythaemia)
- chronic kidney disease
- lupus – a problem with the immune system
But these are only linked with idiopathic intracranial hypertension, they’re not necessarily causes.
A doctor may suspect you have intracranial hypertension if you have symptoms of increased pressure on your brain, such as vision problems and headaches.
You may have several different tests to diagnose intracranial hypertension, such as:
- an examination to check functions such as your muscle strength, reflexes and balance. Any problems could be a sign of an issue with your brain or nerves
- an assessment of your eyes and vision
- a CT scan or MRI scan of your brain
- a lumbar puncture, where a needle is inserted into your spine to check for high pressure in the fluid that surrounds your brain and spinal cord. The typical position for a spinal tap is to lie on your side, with knees slightly bent forward. Local anesthesia is given to numb the lower back. Sometimes, an x-ray (fluoroscopy) may be used to help guide the needle connected to the manometer, the device used to measure intracranial pressure, into the subarachnoid space. Once the spinal needle is inserted, the physician may have you extend your legs and ask you to relax in order to obtain an accurate reading. Holding your breath, bearing down (Valsalva maneuver), or sitting, rather than lying on your side, can produce an inaccurate reading. The opening pressure must be measured before any CSF is removed. The amount of CSF drained during a spinal tap depends on several factors: the opening pressure, the desired closing pressure and the amount of CSF the physician requires for lab studies. Many find that the headache and pulse synchronous tinnitus associated with intracranial hypertension disappears during a spinal tap. While spinal taps can provide important diagnostic information, their therapeutic effects are temporary since spinal fluid regenerates quickly.
Idiopathic intracranial hypertension may be diagnosed if you have increased pressure on your brain and no other cause can be found.
The Modified Dandy Criteria for Idiopathic Intracranial Hypertension is the official criteria used to diagnose idiopathic intracranial hypertension (benign intracranial hypertension). According to the Dandy criteria, an idiopathic intracranial hypertension diagnosis is appropriate if a person 62:
- has signs and symptoms of increased intracranial pressure, such as papilledema and headache;
- has no localizing findings on neurological examination. Localizing findings are findings that point to injury of specific brain areas. For instance, a localizing finding could be the inability to move a certain muscle;
- has a normal MRI/CT scan with no evidence of venous obstructive disease;
- has high intracranial pressure of 250mm/H2O or above on a spinal tap, with no abnormalities of cerebrospinal fluid;
- is awake and alert;
- has no other cause of increased intracranial pressure found.
Chronic intracranial hypertension can be life threatening if it remains undiagnosed and the causes are not treated. You should be referred to a specialist (neurologist) as soon as possible if a your healthcare provider suspects it.
Treatment for intracranial hypertension depends on the cause, if this is known.
The main treatments for idiopathic intracranial hypertension are:
- losing weight if you’re overweight. This can often help to reduce your symptoms and may sometimes relieve them altogether
- stopping any medicine that may be causing your symptoms, including contraception methods. You will need to use a barrier form of contraception as an alternative, such as condoms
- medicine to remove excess fluid from the body (diuretics)
- medicine to reduce the production of cerebrospinal fluid in your brain
- a short course of steroid medicine to relieve headaches and reduce the risk of vision loss
- regular lumbar punctures to remove excess fluid from your spine and help reduce the pressure on your brain
Surgery
Surgery may be considered if other treatments do not help.
The main types of surgery for chronic intracranial hypertension are:
- shunt surgery – a thin, flexible tube is inserted into the fluid-filled space in your skull or spine to divert excess fluid to another part of your body
- optic nerve sheath fenestration – the protective layer surrounding your optic nerve (the nerve connecting the eye to the brain), is opened up to relieve pressure on it and allow fluid to drain away
These procedures can provide relief from your symptoms, but they also carry a risk of potentially serious complications. Talk to the surgeon about what your operation involves and what the risks are.
While many people find their symptoms are relieved with treatment, but the symptoms can come back and can have a significant impact on your life. There’s also a risk that you could lose your vision, even though treatment can help reduce this risk. Permanent vision loss is estimated to happen to 1 in every 5 to 20 people with idiopathic intracranial hypertension.
High blood pressure symptoms and signs
Most people with high blood pressure have no signs or symptoms, even if blood pressure readings reach dangerously high levels.
A few people with high blood pressure may have headaches, shortness of breath or nosebleeds, but these signs and symptoms aren’t specific and usually don’t occur until high blood pressure has reached a severe or life-threatening stage.
Side effects of high blood pressure
If your blood pressure is too high, it puts extra strain on your blood vessels, heart and other organs and can damage your blood vessels as well as your organs, such as the brain, kidneys and eyes. The higher your blood pressure and the longer it goes uncontrolled, the greater the damage.
Persistent high blood pressure can increase your risk of a number of serious and potentially life-threatening health conditions, such as:
- Heart disease
- Coronary heart disease
- Heart attacks. High blood pressure can cause hardening and thickening of the arteries (atherosclerosis), which can lead to a heart attack, stroke or other complications.
- Strokes
- Aneurysm. Increased blood pressure can cause your blood vessels to weaken and bulge, forming an aneurysm. If an aneurysm ruptures, it can be life-threatening.
- Heart failure. To pump blood against the higher pressure in your vessels, the heart has to work harder. This causes the walls of the heart’s pumping chamber to thicken (left ventricular hypertrophy). Eventually, the thickened muscle may have a hard time pumping enough blood to meet your body’s needs, which can lead to heart failure.
- Peripheral arterial disease
- Aortic aneurysms
- Atrial fibrillation
- Kidney disease. Weakened and narrowed blood vessels in your kidneys. This can prevent your kidneys from functioning normally.
- Eye disease. Thickened, narrowed or torn blood vessels in the eyes. This can result in vision loss.
- Metabolic syndrome. This syndrome is a group of disorders of your body’s metabolism, including increased waist size, high triglycerides, decreased high-density lipoprotein (HDL) cholesterol (the “good” cholesterol), high blood pressure and high insulin levels. These conditions make you more likely to develop diabetes, heart disease and stroke.
- Vascular dementia. Narrowed or blocked arteries can limit blood flow to the brain, leading to a certain type of dementia (vascular dementia). A stroke that interrupts blood flow to the brain also can cause vascular dementia.
- Trouble with memory or understanding (hypertensive encephalopathy). Uncontrolled high blood pressure may also affect your ability to think, remember and learn. Trouble with memory or understanding concepts is more common in people with high blood pressure.
- Death (usually due to coronary heart disease, vascular disease, stroke-related)
If you have high blood pressure, reducing it even a small amount can help lower your risk of these health conditions.
Causes of high blood pressure
In most cases, it’s not clear exactly what causes high blood pressure, but there are things that can increase your risk.
You might be more at risk of high blood pressure if you:
- Are overweight or obese. The more you weigh, the more blood you need to supply oxygen and nutrients to your tissues. As the amount of blood flow through your blood vessels increases, so does the pressure on your artery walls.
- Eat too much salt (sodium) and do not eat enough fruit and vegetables. Too much sodium in your diet can cause your body to retain fluid, which increases blood pressure.
- Have too little potassium in your diet. Potassium helps balance the amount of sodium in your cells. A proper balance of potassium is critical for good heart health. If you don’t get enough potassium in your diet, or you lose too much potassium due to dehydration or other health conditions, sodium can build up in your blood.
- Do not do enough exercise. People who are inactive tend to have higher heart rates. The higher your heart rate, the harder your heart must work with each contraction and the stronger the force on your arteries. Lack of physical activity also increases the risk of being overweight.
- Drink too much alcohol or coffee (or other caffeine-based drinks). Over time, heavy drinking can damage your heart. Having more than one drink a day for women and more than two drinks a day for men may affect your blood pressure. If you drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and two drinks a day for men. One drink equals 12 ounces of beer, 5 ounces of wine or 1.5 ounces of 80-proof liquor.
- Smoke or use tobacco. Not only does smoking or chewing tobacco immediately raise your blood pressure temporarily, but the chemicals in tobacco can damage the lining of your artery walls. This can cause your arteries to narrow and increase your risk of heart disease. Secondhand smoke also can increase your heart disease risk.
- Use illegal drugs such as cocaine, “bath salts,” and methamphetamine.
- Do not get much sleep or have disturbed sleep
- Have certain chronic conditions. Certain chronic conditions also may increase your risk of high blood pressure, including kidney disease, diabetes, sleep apnea, metabolic syndrome, thyroid problems and certain tumors.
- Age over 65. The risk of high blood pressure increases as you age. Until about age 64, high blood pressure is more common in men. Women are more likely to develop high blood pressure after age 65.
- Have a relative or family history with high blood pressure. High blood pressure tends to run in families.
- Are of African American or Hispanic descent. High blood pressure is particularly common among people of African heritage, often developing at an earlier age than it does in whites. Serious complications, such as stroke, heart attack and kidney failure, also are more common in people of African heritage.
- Experience stress in your life. High levels of stress can lead to a temporary increase in blood pressure. Stress-related habits such as eating more, using tobacco or drinking alcohol can lead to further increases in blood pressure.
- Use medicines. Some prescription and over-the-counter medicines can make it more difficult for your body to control your blood pressure. Antidepressants, decongestants (medicines to relieve a stuffy nose), hormonal birth control pills, and non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen can all raise your blood pressure.
- Live in a deprived area. Research now shows that factors such as income, your education, where you live, and the type of job you have may contribute to your risk of high blood pressure. Working early or late shifts is one example of a social factor that can raise your risk. Additionally, some research has shown that experiencing danger, harm, or trauma as a child has links to a higher risk of developing high blood pressure.
- Sometimes pregnancy contributes to high blood pressure as well. During pregnancy, African American women are more likely than white women to develop preeclampsia. Preeclampsia is a pregnancy disorder that causes sudden high blood pressure and problems with the kidneys and liver. Women who have high blood pressure during pregnancy are more likely to have high blood pressure later in life.
- Men are more likely than women to develop high blood pressure throughout middle age. But in older adults, women are more likely than men to develop high blood pressure.
In about 1 in 20 cases, high blood pressure happens as the result of an underlying health condition or taking a certain medicine.
- Health conditions that can cause high blood pressure include:
- kidney disease
- diabetes
- long-term kidney infections
- obstructive sleep apnea – where the walls of the throat relax and narrow during sleep, interrupting normal breathing
- glomerulonephritis – damage to the tiny filters inside the kidneys
- narrowing of the arteries supplying the kidneys
- hormone problems – such as an underactive thyroid, an overactive thyroid, Cushing’s syndrome, acromegaly, increased levels of the hormone aldosterone (hyperaldosteronism), and pheochromocytoma
- lupus – a condition in which the immune system attacks parts of the body, such as the skin, joints and organs
- scleroderma – a condition that causes thickened skin, and sometimes problems with organs and blood vessels
- Medicines that can increase your blood pressure include:
- the contraceptive pill
- steroids
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen and naproxen
- some pharmacy cough and cold remedies
- some herbal remedies – particularly those containing liquorice
- some recreational drugs – such as cocaine and amphetamines
- some selective serotonin-noradrenaline reuptake inhibitor (SSNRI) antidepressants – such as venlafaxine
In these cases, your blood pressure may return to normal once you stop taking the medicine or drug.
Although high blood pressure is most common in adults, children may be at risk, too. For some children, high blood pressure is caused by problems with the kidneys or heart. But for a growing number of kids, poor lifestyle habits — such as an unhealthy diet and lack of exercise — contribute to high blood pressure.
Making healthy lifestyle changes can sometimes help reduce your chances of getting high blood pressure and help lower your blood pressure if it’s already high.
Risk factors for high blood pressure
Nearly one-third of all Americans have high blood pressure, but it is particularly prevalent in:
- People who have diabetes, gout, or kidney disease
- African Americans (particularly those who live in the southeastern U.S.)
- People in their early to middle adult years; men in this age group have higher blood pressure more often than women in this age group
- People in their middle to later adult years; women in this age group have higher blood pressure more often than men in this age group (more women have high blood pressure after menopause than men of the same age)
- Middle-aged and elderly people; more than half of all Americans age 60 and older have high blood pressure
- People with a family history of high blood pressure
- People consuming a high salt diet
- Overweight or obese people
- Heavy drinkers of alcohol
- Women who are taking oral contraceptives
- People with depression
- A lack of exercise and physical activity
High blood pressure prevention
A heart-healthy lifestyle can help prevent high blood pressure from developing. To live a healthy lifestyle:
- Choose heart-healthy foods that are lower in sodium (salt) and are rich in potassium. Fruits and vegetables are high in potassium. For more ways to limit your sodium, visit the DASH eating plan page.
- Avoid or limit alcohol.
- Get regular physical activity. Even modest amounts can make a difference.
- Aim for a healthy weight.
- Quit smoking.
- Manage stress.
- Get enough good-quality sleep.
The DASH eating plan requires no special foods and instead provides daily and weekly nutritional goals. DASH eating plan recommends 63:
- Eating vegetables, fruits, and whole grains
- Including fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils
- Limiting foods that are high in saturated fat, such as fatty meats, full-fat dairy products, and tropical oils such as coconut, palm kernel, and palm oils
- Limiting sugar-sweetened beverages and sweets
When following the DASH eating plan, it is important to choose foods that are:
- Low in saturated and trans fats
- Rich in potassium, calcium, magnesium, fiber, and protein
- Lower in sodium
Table 4. DASH Diet Eating Plan—Number of Food Servings by Calorie Level
| Food Group | 1,200 Calories | 1,400 Calories | 1,600 Calories | 1,800 Calories | 2,000 Calories | 2,600 Calories | 3,100 Calories |
| Grains a | 4–5 | 5–6 | 6 | 6 | 6–8 | 10–11 | 12–13 |
| Vegetables | 3–4 | 3–4 | 3–4 | 4–5 | 4–5 | 5–6 | 6 |
| Fruits | 3–4 | 4 | 4 | 4–5 | 4–5 | 5–6 | 6 |
| Fat-free or low-fat dairy products b | 2–3 | 2–3 | 2–3 | 2–3 | 2–3 | 3 | 3–4 |
| Lean meats, poultry, and fish | 3 or less | 3–4 or less | 3–4 or less | 6 or less | 6 or less | 6 or less | 6–9 |
| Nuts, seeds, and legumes | 3 per week | 3 per week | 3–4 per week | 4 per week | 4–5 per week | 1 | 1 |
| Fats and oils c | 1 | 1 | 2 | 2–3 | 2–3 | 3 | 4 |
| Sweets and added sugars | 3 or less per week | 3 or less per week | 3 or less per week | 5 or less per week | 5 or less per week | ≤2 | ≤2 |
| Maximum sodium limit d | 2,300 mg/day | 2,300 mg/day | 2,300 mg/day | 2,300 mg/day | 2,300 mg/day | 2,300 mg/day | 2,300 mg/day |
Footnotes:
a Whole grains are recommended for most grain servings as a good source of fiber and nutrients.
b For lactose intolerance, try either lactase enzyme pills with dairy products or lactose-free or lactose-reduced milk.
c Fat content changes the serving amount for fats and oils. For example, 1 Tbsp regular salad dressing = one serving; 1 Tbsp low-fat dressing = one-half serving; 1 Tbsp fat-free dressing = zero servings.
d The DASH diet eating plan has a salt (sodium) limit of either 2,300 mg or 1,500 mg per day. 1,500 milligrams (mg) sodium lowers blood pressure even further than 2,300 mg sodium daily.
Tips for a lower-salt diet
Too much salt can raise your blood pressure, which puts you at increased risk of health problems such as heart disease and stroke. But a few simple steps can help you to cut your salt intake.
Salt (Sodium) Equivalents
Sodium chloride or table salt is approximately 40 percent sodium. It’s important to understand just how much sodium is in salt so you can take measures to control your intake. These amounts are approximate.
- 1/4 teaspoon salt = 575 mg sodium
- 1/2 teaspoon salt = 1,150 mg sodium
- 3/4 teaspoon salt = 1,725 mg sodium
- 1 teaspoon salt = 2,300 mg sodium
Sodium Sources
Sodium can be sneaky. Taking control of your sodium means checking labels and reducing preservatives. Other foods to be aware of include:
- Processed foods
- Natural foods with a higher-than-average sodium content, including cheese, seafood, olives and some legumes
- Table salt, sea salt and kosher salt (sodium chloride)
- Some over-the-counter drugs
- Some prescription medications
You don’t have to add salt to food to be eating too much – 75% of the salt we eat is already in everyday foods such as bread, breakfast cereal and ready meals.
A diet that is high in salt can cause raised blood pressure, which currently affects more than one third of adults in the US.
High blood pressure often has no symptoms, and it is estimated that in America about one in every three people who have high blood pressure don’t know it. But if you have it, you are more likely to develop heart disease or have a stroke.
Increasing Daily Potassium
The DASH diet eating plan is designed to be rich in potassium, with a target of 4,700 mg potassium daily, to enhance the effects of reducing sodium on blood pressure. The following are examples of potassium-rich foods.
Table 5. Sample Foods and Potassium Levels
| Food Groups | Potassium (mg) |
| Vegetables | |
| Potato, 1 medium | 926 |
| Sweet Potato, 1 medium | 540 |
| Spinach, cooked, 1/2 cup | 290 |
| Zucchini, cooked, 1/2 cup | 280 |
| Tomato, fresh, 1/2 cup | 210 |
| Kale, cooked, 1/2 cup | 150 |
| Romaine lettuce, 1 cup | 140 |
| Mushrooms, 1/2 cup | 110 |
| Cucumber, 1/2 cup | 80 |
| Fruit | |
| Banana, 1 medium | 420 |
| Apricots, 1/4 cup | 380 |
| Orange, 1 medium | 237 |
| Cantaloupe chunks, 1/2 cup | 214 |
| Apple, 1 medium | 150 |
| Nuts, seeds, and legumes | |
| Cooked soybeans, 1/2 cup | 440 |
| Cooked lentils, 1/2 cup | 370 |
| Cooked kidney beans, 1/2 cup | 360 |
| Cooked split peas, 1/2 cup | 360 |
| Almonds, roasted, 1/3 cup | 310 |
| Walnuts, roasted, 1/3 cup | 190 |
| Sunflower seeds, roasted, 2 Tbsp | 124 |
| Peanuts, roasted, 1/3 cup | 120 |
| Low-fat or fat-free milk and milk products | |
| Milk, 1 cup | 380 |
| Yogurt, 1 cup | 370 |
| Lean meats, fish, and poultry | |
| Fish (cod, halibut, rockfish, trout, tuna), 3 oz | 200-400 |
| Pork tenderloin, 3 oz | 370 |
| Beef tenderloin, chicken, turkey, 3 oz | 210 |
Footnote: Before you increase the potassium in your diet or use salt substitutes (which often contain potassium), check with your doctor. People who have kidney problems or who take certain medicines must be careful about how much potassium they consume.
[Source 64 ]High blood pressure diagnosis
The only way of knowing whether you have high blood pressure is to have a blood pressure test. Ask your doctor for a blood pressure reading at least every two years starting at age 18. If you’re age 40 or older, or you’re 18 to 39 with a high risk of high blood pressure, ask your doctor for a blood pressure reading every year. Children age 3 and older will usually have blood pressure measured as a part of their yearly checkups. Getting this done is easy and could save your life.
Blood pressure generally should be checked in both arms to determine if there’s a difference. It’s important to use an appropriate-sized arm cuff. Your readings can be different if the arm cuff is too small or too big.
You can get your blood pressure tested at a number of places, including:
- at your doctor
- at some pharmacies
- as part of your health check
- in some workplaces
You can also check your blood pressure yourself with a home blood pressure monitor.
Your doctor will ask questions about your medical history and do a physical examination. Because blood pressure normally varies during the day and may increase during a doctor visit (white coat hypertension), your doctor will likely take several blood pressure readings at three or more separate appointments before diagnosing you with high blood pressure.
Your doctor will also likely recommend more-frequent readings if you’ve already been diagnosed with high blood pressure or have other risk factors for cardiovascular disease.
If you don’t regularly see your doctor, you may be able to get a free blood pressure screening at a health resource fair or other locations in your community. You can also find machines in some stores that will measure your blood pressure for free.
Public blood pressure machines, such as those found in pharmacies, may provide helpful information about your blood pressure, but they may have some limitations. The accuracy of these machines depends on several factors, such as a correct cuff size and proper use of the machines. Ask your doctor for advice on using public blood pressure machines.
Taking your blood pressure at home
Your doctor may ask you to record your blood pressure at home to provide additional information and confirm if you have high blood pressure. Home monitoring is an important way to confirm if you have high blood pressure, to check if your blood pressure treatment is working or to diagnose worsening high blood pressure.
Home blood pressure monitors are widely available and inexpensive, and you don’t need a prescription to buy one. Home blood pressure monitoring isn’t a substitute for visits to your doctor, and home blood pressure monitors may have some limitations.
Make sure to use a validated device, and check that the cuff fits. Bring the monitor with you to your doctor’s office to check its accuracy once a year. Talk to your doctor about how to start checking your blood pressure at home.
Devices that measure your blood pressure at your wrist or finger aren’t recommended by the American Heart Association because they can provide less reliable results.
High blood pressure tests
If you have high blood pressure, your doctor may recommend tests to confirm the diagnosis and check for underlying conditions that can cause hypertension.
- Ambulatory (24-hour) blood pressure monitoring. This 24-hour blood pressure monitoring test is used to confirm if you have high blood pressure. The device used for this test measures your blood pressure at regular intervals over a 24-hour period and provides a more accurate picture of blood pressure changes over an average day and night. However, these devices aren’t available in all medical centers, and they may not be reimbursed.
- Lab tests. Your doctor may recommend a urine test (urinalysis) and blood tests, including a cholesterol test.
- Blood workup including complete blood count, ESR, creatinine, eGFR, electrolytes, HbA1c, thyroid profile, blood cholesterol levels, and serum uric acid
- Urine albumin to creatinine ratio
- Electrocardiogram (ECG or EKG). This quick and painless test measures your heart’s electrical activity.
- Echocardiogram. Depending on your signs and symptoms and test results, your doctor may order an echocardiogram to check for more signs of heart disease. An echocardiogram uses sound waves to produce images of the heart.
- Ankle-brachial pressure index – ABI (if symptoms suggestive of peripheral arterial disease)
High blood pressure treatment
Doctors can help you keep your blood pressure to a safe level using:
- lifestyle changes
- medicines
What works best is different for each person. Talk to your doctor to help you decide about treatment.
Your doctor may recommend that you make lifestyle changes including:
- Eating a heart-healthy diet with less salt
- Getting regular physical activity
- Maintaining a healthy weight or losing weight if you’re overweight or obese
- Limiting the amount of alcohol you drink
But sometimes lifestyle changes aren’t enough. If diet and exercise don’t help, your doctor may recommend medication to lower your blood pressure. Have your blood pressure checked routinely and see your healthcare provider to monitor your blood pressure.
Eighth Joint National Committee (JNC 8) recommends the following 65:
- Starting pharmacological therapy for individuals with diabetes mellitus and chronic kidney disease (CKD) with blood pressure greater than or equal to 140/90 mmHg to therapeutic target blood pressure less than 140/90 mmHg
- Starting pharmacological therapy for individuals 60 years of age and over with blood pressure greater than or equal to 150/90 mmHg to therapeutic target blood pressure less than 150/90mmHg
- Starting pharmacological therapy for individuals 18 to 59 years of age with systolic blood pressure greater than or equal to 140mmHg to therapeutic target systolic blood pressure less than 140mmHg
- Individuals with diabetes mellitus and non-black population, treatment should include a thiazide diuretic, calcium channel blocker, and an angiotensin-converting enzyme inhibitors/angiotensin receptor blocker
- Individuals in the black population, including those with diabetes mellitus, treatment should include a thiazide diuretic and calcium channel blocker
- Individuals with chronic kidney disease, treatment should be started with or include angiotensin-converting enzyme inhibitors/angiotensin receptor blocker, and this applies to all chronic kidney disease patients irrespective of race or diabetes mellitus status
American College of Cardiology recommends the following 66:
- Ten-year atherosclerotic cardiovascular disease risk should be estimated
- Anti-hypertensive medications are usually initiated when blood pressure readings are persistently greater than or equal to 140/90 mmHg
- High-risk population (diabetics, chronic kidney disease, individuals with atherosclerotic cardiovascular disease) or in those individuals with 10-year atherosclerotic cardiovascular disease risk greater than or equal to 10%, therapy can be initiated at lower blood pressure cutoffs
- The goal of treatment is to keep blood pressures in as close to normal range as possible, i.e., blood pressure less than or equal to 130/80 mmHg
European Society of Cardiology and European Society of Hypertension recommends the following 8:
- Starting pharmacological therapy for grade 2 or 3 hypertension regardless of the level of risk
- Starting pharmacological therapy for grade 1 hypertension when there is hypertension mediated end-organ damage
- Grade 1 hypertension in the absence of hypertension mediated end-organ damage requires either high risk for cardiovascular disease or failure of lifestyle interventions, for initiating pharmacological therapy
- Starting pharmacological therapy for individuals greater than or equal to 80 years of age with blood pressure greater than or equal to 160/90mmHg to therapeutic target less than 160/90mmHg regardless of diabetes mellitus, chronic kidney disease, coronary artery disease or transient ischemia attack (TIA)/ stroke (cerebrovascular accident)
- Starting pharmacological therapy for individuals 18 to 79 years of age with blood pressure greater than or equal to 140/90mmHg to therapeutic target less than 140/90 mmHg regardless of diabetes mellitus, chronic kidney disease, coronary artery disease or transient ischemia attack (TIA)/ stroke (cerebrovascular accident)
Figure 1. Eighth Joint National Committee (JNC 8) Hypertension Guideline Algorithm
Abbreviations: CKD = chronic kidney disease; BP = blood pressure; HTN = hypertension
[Source 65 ]Natural ways to lower blood pressure
Changing your lifestyle can help control and manage high blood pressure. These lifestyle changes can help prevent and lower your high blood pressure:
- Reduce the amount of salt you eat and have a generally healthy diet. Eat a heart-healthy diet. Try the Dietary Approaches to Stop Hypertension (DASH) diet, which emphasizes fruits, vegetables, whole grains, poultry, fish and low-fat dairy foods.
- Choose foods that are low in sodium (salt). Aim to limit sodium to less than 2,300 milligrams (mg) a day or less. However, a lower sodium intake — 1,500 mg a day or less — is ideal for most adults. While you can reduce the amount of salt you eat by putting down the saltshaker, you generally should also pay attention to the amount of salt that’s in the processed foods you eat, such as canned soups or frozen dinners.
- Get plenty of potassium, which can help prevent and control high blood pressure.
- Choose foods low in calories and saturated fat and trans fat
- Choose foods high in fiber
- Cut back on alcohol or omit alcoholic beverages. Even if you’re healthy, alcohol can raise your blood pressure. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women, and up to two drinks a day for men. One drink equals 12 ounces of beer, 5 ounces of wine or 1.5 ounces of 80-proof liquor.
- Maintain a healthy weight, or lose weight if you’re overweight. Keeping a healthy weight, or losing weight if you’re overweight or obese, can help you control your high blood pressure and lower your risk of related health problems. In general, you may reduce your blood pressure by about 1 mm Hg with each kilogram (about 2.2 pounds) of weight you lose.
- Limit serving sizes
- Exercise regularly. Regular physical activity can help lower your blood pressure, manage stress, keep your weight under control and reduce your risk of many health conditions. If you have high blood pressure, consistent moderate- to high-intensity workouts can lower your top blood pressure reading by about 11 mm Hg and the bottom number by about 5 mm Hg. Aim for at least 150 minutes a week of moderate aerobic activity or 75 minutes a week of vigorous aerobic activity, or a combination of moderate and vigorous activity. For example, try brisk walking for about 30 minutes most days of the week. Or try interval training, in which you alternate short bursts of intense activity with short recovery periods of lighter activity. Aim to do muscle-strengthening exercises at least two days a week.
- Cut down on caffeine. Drinking more than 4 cups of coffee a day may increase your blood pressure. If you’re a big fan of coffee, tea or other caffeine-rich drinks, such as cola and some energy drinks, consider cutting down. It’s fine to drink tea and coffee as part of a balanced diet, but it’s important that these drinks are not your main or only source of fluid.
- Stop smoking. Tobacco can injure blood vessel walls and speed up the process of buildup of plaque in the arteries. If you smoke, ask your doctor to help you quit.
- Manage stress. Reduce stress as much as possible. Practice healthy coping techniques, such as muscle relaxation, deep breathing or mindfulness. Getting regular physical activity and plenty of sleep can help, too.
- Practice relaxation or slow, deep breathing. Practice taking deep, slow breaths to help relax. Some research shows that slow, paced breathing (five to seven deep breaths per minute) combined with mindfulness techniques can reduce blood pressure. There also are some devices available that promote slow, deep breathing. According to the American Heart Association, device-guided breathing may be a reasonable nondrug option for lowering blood pressure, especially if you have anxiety with high blood pressure or can’t tolerate standard treatments well.
- Control blood pressure during pregnancy. Women with high blood pressure should discuss with their doctors how to control their blood pressure during pregnancy.
- Monitor your blood pressure at home. Home blood pressure monitoring allows you to keep a daily log of blood pressure measurements. Your doctor can review the information to determine if your medication is working or if you’re having complications. Home blood pressure monitoring isn’t a substitute for visits to your doctor. Even if you get normal readings, don’t stop or change your medications or alter your diet without talking to your doctor first.
Some people with high blood pressure may also need to take 1 or more medicines to stop their blood pressure getting too high. If your blood pressure is under control, ask your doctor about how often you need to check it.
Natural remedies for high blood pressure
Although diet and exercise are the most appropriate ways to lower your blood pressure, some supplements also may help lower it. However, more research is needed to determine the potential benefits. These supplements include:
- Fiber, such as blond psyllium and wheat bran
- Minerals, such as magnesium, calcium and potassium
- Folic acid
- Supplements or products that increase nitric oxide or widen blood vessels (vasodilators), such as cocoa, coenzyme Q10, L-arginine and garlic
- Omega-3 fatty acids, found in fatty fish, high-dose fish oil supplements and flaxseed
Researchers are also studying whether vitamin D can reduce blood pressure, but evidence is conflicting. More research is needed.
While it’s best to include these supplements in your diet as foods, you can also take supplement pills or capsules. Talk to your doctor before adding any of these supplements to your blood pressure treatment. Some supplements can interact with medications, causing harmful side effects, such as an increased bleeding risk that could be life-threatening.
You can also practice relaxation techniques, such as deep breathing or mindfulness, to help you relax and reduce your stress level. These practices may temporarily reduce your blood pressure.
High blood pressure medicine
The type of medication your doctor prescribes for high blood pressure depends on your blood pressure measurements and overall health. Two or more blood pressure drugs often work better than one. Sometimes finding the most effective medication or combination of drugs is a matter of trial and error.
Common blood pressure medicines include:
- ACE inhibitors (ACEI) – such as enalapril, lisinopril, perindopril and ramipril
- Angiotensin-2 receptor blockers (ARBs) – such as candesartan, irbesartan, losartan, valsartan and olmesartan
- Calcium channel blockers (CCB) – such as amlodipine, felodipine and nifedipine or diltiazem and verapamil
- Diuretics – such as indapamide and bendroflumethiazide
- Beta blockers (BB) – such as atenolol and bisoprolol
- Alpha blockers – such as doxazosin
- Other diuretics – such as amiloride and spironolactone
You should aim for a blood pressure treatment goal of less than 130/80 mm Hg if:
- You’re a healthy adult age 65 or older
- You’re a healthy adult younger than age 65 with a 10% or higher risk of developing cardiovascular disease in the next 10 years
- You have chronic kidney disease, diabetes or coronary artery disease
Ask your doctor what your blood pressure treatment goal should be. Also, the ideal blood pressure treatment goal can vary with age and health conditions, particularly if you’re older than age 65.
Figure 2. High blood pressure medicine
[Source 65 ]Best medicine for high blood pressure
Medications used to treat high blood pressure include:
- Diuretics sometimes called water pills, are medications that help your kidneys eliminate sodium and water from the body. These drugs are often the first medications tried to treat high blood pressure. There are different classes of diuretics, including thiazide, loop and potassium sparing. Which one your doctor recommends depends on your blood pressure measurements and other health conditions, such a kidney disease or heart failure. Diuretics commonly used to treat blood pressure include chlorthalidone, hydrochlorothiazide (Microzide) and others. A common side effect of diuretics is dizziness when standing up, increased thirst, a rash and increased urination, which could reduce potassium levels. If you have a low potassium level, your doctor may add a potassium-sparing diuretic — such as triamterene (Dyazide, Maxide) or spironolactone (Aldactone) — to your treatment.
- Angiotensin-converting enzyme (ACE) inhibitors. These medications — such as lisinopril (Prinivil, Zestril), benazepril (Lotensin), captopril and others — help relax blood vessels by blocking the formation of a natural chemical that narrows blood vessels. The most common side effect of angiotensin-converting enzyme (ACE) inhibitors is a persistent dry cough. Other possible side effects include headaches, dizziness and a rash.
- Angiotensin II receptor blockers (ARBs). These medications relax blood vessels by blocking the action, not the formation, of a natural chemical that narrows blood vessels. ARBs include candesartan (Atacand), losartan (Cozaar) and others. Possible side effects of angiotensin-2 receptor blockers (ARBs) include dizziness, headaches, and cold or flu-like symptoms.
- Calcium channel blockers (CCB). These medications — including amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and others — help relax the muscles of your blood vessels. Some slow your heart rate. Calcium channel blockers may work better for older people and people of African heritage than do ACE inhibitors alone. Don’t eat or drink grapefruit products when taking calcium channel blockers. Grapefruit increases blood levels of certain calcium channel blockers, which can be dangerous. Talk to your doctor or pharmacist if you’re concerned about interactions.
The medicine recommended for you will depend on things like how high your blood pressure is, your age and your ethnicity.
Additional medications sometimes used to treat high blood pressure
If you’re having trouble reaching your blood pressure goal with combinations of the above medications, your doctor may prescribe:
- Alpha blockers. These medications reduce nerve signals to blood vessels, lowering the effects of natural chemicals that narrow blood vessels. Alpha blockers include doxazosin (Cardura), prazosin (Minipress) and others.
- Alpha-beta blockers. Alpha-beta blockers block nerve signals to blood vessels and slow the heartbeat to reduce the amount of blood that must be pumped through the vessels. Alpha-beta blockers include carvedilol (Coreg) and labetalol (Trandate).
- Beta blockers (BB). These medications reduce the workload on your heart and widen your blood vessels, causing your heart to beat slower and with less force. Beta blockers include acebutolol, atenolol (Tenormin) and others. Beta blockers aren’t usually recommended as the only medication you’re prescribed, but they may be effective when combined with other blood pressure medications. Possible side effects of beta blockers include dizziness, headaches, tiredness, and cold hands and feet.
- Aldosterone antagonists. These drugs also are considered diuretics. Examples are spironolactone and eplerenone (Inspra). These drugs block the effect of a natural chemical that can lead to salt and fluid buildup, which can contribute to high blood pressure. They may be used to treat resistant hypertension.
- Renin inhibitors. Aliskiren (Tekturna) slows the production of renin, an enzyme produced by your kidneys that starts a chain of chemical steps that increases blood pressure. Due to a risk of serious complications, including stroke, you shouldn’t take aliskiren with ACE inhibitors or ARBs.
- Vasodilators. These medications include hydralazine and minoxidil. They work directly on the muscles in the walls of your arteries, preventing the muscles from tightening and your arteries from narrowing.
- Central-acting agents. These medications prevent your brain from telling your nervous system to increase your heart rate and narrow your blood vessels. Examples include clonidine (Catapres, Kapvay), guanfacine (Intuniv) and methyldopa.
Potential future treatments
Researchers continue to study catheter-based ultrasound and radiofrequency ablation of the kidney’s sympathetic nerves (renal denervation) as a treatment for resistant hypertension (where adequate blood pressure control is not achieved despite adequate compliance to two or three anti-hypertensive drugs and lifestyle measures). Early studies showed some benefit, but more-robust studies found that the therapy does not significantly lower blood pressure in people with resistant hypertension, so this remains an investigational therapy. More research is underway to determine what role, if any, this therapy may have in treating hypertension.
Resistant hypertension treatment
If your blood pressure remains stubbornly high despite taking at least three different types of high blood pressure drugs, one of which usually should be a diuretic, you may have resistant hypertension. You’re also considered to have resistant hypertension if you have controlled high blood pressure but are taking four different types of medications at the same time to achieve that control. If you do, your doctor should investigate the possibility of a secondary cause of the high blood pressure.
Having resistant hypertension doesn’t mean your blood pressure will never get lower. If you and your doctor can determine the cause, a more effective treatment plan can be created to help you meet your goal blood pressure.
Treating resistant hypertension may involve many steps, including:
- Changing your high blood pressure medications to determine which combinations and doses work best
- Reviewing all the medications you take, including those that you take for other conditions or buy without a prescription
- Monitoring your blood pressure at home to see if going to the doctor causes your blood pressure to increase (white coat hypertension)
- Making healthy lifestyle changes, such as eating a healthy diet with less salt, maintaining a healthy weight and limiting alcohol
You should always take blood pressure medications as prescribed. Never skip a dose or abruptly stop taking your blood pressure medication. Suddenly stopping certain blood pressure drugs, such as beta blockers, can cause a sharp increase in blood pressure (rebound hypertension).
If you skip doses because you can’t afford the medications, because you have side effects or because you simply forget to take your medications, talk to your doctor about solutions. Don’t change your treatment without your doctor’s guidance.
High blood pressure in people over 80
The target blood pressure reading for the over-80s is below 150/90 mmHg when it’s measured in the clinic or surgery, and below 145/85 mmHg for home readings.
While there are definite benefits from taking medicines to reduce blood pressure if you’re under the age of 80, it’s less clear it’s useful if you’re over 80. It’s now thought that if you reach 80 while you’re taking medicine for high blood pressure, it’s fine to continue treatment provided it’s still helping you and is not causing side effects.
If you’re diagnosed with high blood pressure and you’re aged over 80, your doctor will also consider your other health risk factors when deciding whether to give you treatment for the high blood pressure.
High blood pressure prognosis
Mild to moderate hypertension may be associated with a risk of atherosclerotic disease if left untreated in 30% of people and organ damage in 50% of people within 8-10 years after onset. Large scale meta analyses have also shown the rising cardiovascular disease and vascular disease risk with a rise in systolic and diastolic blood pressures, with almost doubling of risk of death from coronary heart disease or heart failure and stroke with rising systolic blood pressure of as much as 20 and diastolic blood pressure of 10 mmHg 67. Patients with resistant hypertension also have a higher risk for poor outcomes, especially for those with certain comorbidities (e.g., chronic kidney disease and ischemic heart disease).
The prognosis depends on blood pressure control and is favorable only if the blood pressures attain adequate control; however, complications may develop in some patients as hypertension is a progressive disease.
Adequate control and lifestyle measures only serve to delay the development and progression of complications such as chronic kidney disease and renal failure.
- What Is High Blood Pressure (Hypertension). https://www.nhlbi.nih.gov/health/high-blood-pressure[↩]
- High Blood Pressure Diagnosis. https://www.nhlbi.nih.gov/health/high-blood-pressure/diagnosis[↩][↩]
- Zhou, B., Perel, P., Mensah, G. A., & Ezzati, M. (2021). Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nature reviews. Cardiology, 18(11), 785–802. https://doi.org/10.1038/s41569-021-00559-8[↩]
- Casey, D. E., Jr, Thomas, R. J., Bhalla, V., Commodore-Mensah, Y., Heidenreich, P. A., Kolte, D., Muntner, P., Smith, S. C., Jr, Spertus, J. A., Windle, J. R., Wozniak, G. D., & Ziaeian, B. (2019). 2019 AHA/ACC Clinical Performance and Quality Measures for Adults With High Blood Pressure: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circulation. Cardiovascular quality and outcomes, 12(11), e000057. https://doi.org/10.1161/HCQ.0000000000000057[↩]
- The Facts About High Blood Pressure. http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/GettheFactsAboutHighBloodPressure/The-Facts-About-High-Blood-Pressure_UCM_002050_Article.jsp[↩]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003 Dec;42(6):1206-52. https://www.ahajournals.org/doi/epub/10.1161/01.HYP.0000107251.49515.c2[↩]
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018 Jun;71(6):e13-e115. https://www.ahajournals.org/doi/epub/10.1161/HYP.0000000000000065[↩][↩]
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339. Erratum in: Eur Heart J. 2019 Feb 1;40(5):475.[↩][↩][↩]
- Iqbal AM, Jamal SF. Essential Hypertension. [Updated 2022 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539859[↩][↩]
- High blood pressure. https://www.bhf.org.uk/informationsupport/risk-factors/high-blood-pressure[↩]
- Understanding Blood Pressure Readings. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings[↩]
- Lenfant C, Chobanian AV, Jones DW, Roccella EJ; Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003 Jun;41(6):1178-9. doi: 10.1161/01.HYP.0000075790.33892.AE[↩]
- Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents [published correction appears in Pediatrics. 2017;140(6):e20173035]. Pediatrics. 2017;140(3):e20171904. https://doi.org/10.1542/peds.2017-1904[↩]
- High Blood Pressure in Children and Adolescents. Am Fam Physician. 2018 Oct 15;98(8):486-494. https://www.aafp.org/afp/2018/1015/p486.html[↩]
- Frost, C. D., Law, M. R., & Wald, N. J. (1991). By how much does dietary salt reduction lower blood pressure? II–Analysis of observational data within populations. BMJ (Clinical research ed.), 302(6780), 815–818. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1669173/pdf/bmj00120-0021.pdf[↩]
- Fagard R, Brguljan J, Staessen J, Thijs L, Derom C, Thomis M, Vlietinck R. Heritability of conventional and ambulatory blood pressures. A study in twins. Hypertension. 1995 Dec;26(6 Pt 1):919-24. doi: 10.1161/01.hyp.26.6.919[↩]
- Warren, H. R., Evangelou, E., Cabrera, C. P., Gao, H., et al. UK Biobank CardioMetabolic Consortium BP working group (2017). Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nature genetics, 49(3), 403–415. https://doi.org/10.1038/ng.3768[↩]
- Bavishi C, Goel S, Messerli FH. Isolated Systolic Hypertension: An Update After SPRINT. Am J Med. 2016 Dec;129(12):1251-1258. doi: 10.1016/j.amjmed.2016.08.032. Epub 2016 Sep 14. Erratum in: Am J Med. 2017 Sep;130(9):1128.[↩]
- Liu, X., Rodriguez, C. J., & Wang, K. (2015). Prevalence and trends of isolated systolic hypertension among untreated adults in the United States. Journal of the American Society of Hypertension : JASH, 9(3), 197–205. https://doi.org/10.1016/j.jash.2015.01.002[↩]
- Tan JL, Thakur K. Systolic Hypertension. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482472[↩][↩]
- Diagnosis of Secondary Hypertension: An Age-Based Approach. Am Fam Physician. 2010 Dec 15;82(12):1471-1478. https://www.aafp.org/afp/2010/1215/p1471.html[↩]
- AlGhatrif, M., & Lakatta, E. G. (2015). The conundrum of arterial stiffness, elevated blood pressure, and aging. Current hypertension reports, 17(2), 12. https://doi.org/10.1007/s11906-014-0523-z[↩]
- Chobanian AV. Clinical practice. Isolated systolic hypertension in the elderly. N Engl J Med. 2007 Aug 23;357(8):789-96. doi: 10.1056/NEJMcp071137[↩]
- Naranjo M, Chauhan S, Paul M. Malignant Hypertension. [Updated 2021 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507701[↩][↩][↩][↩][↩]
- Riemekasten G. Fortschritte bei der Systemischen Sklerose [Progress in Systemic Sclerosis – Early, Targeted and Intensive Therapy is the Key to Success]. Dtsch Med Wochenschr. 2019 Feb;144(3):189-193. German. doi: 10.1055/a-0652-2488[↩]
- Nair R, Vaqar S. Renovascular Hypertension. [Updated 2021 Nov 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551587[↩][↩][↩]
- Textor S. C. (2017). Renal Arterial Disease and Hypertension. The Medical clinics of North America, 101(1), 65–79. https://doi.org/10.1016/j.mcna.2016.08.010[↩][↩]
- Sparks, M. A., Crowley, S. D., Gurley, S. B., Mirotsou, M., & Coffman, T. M. (2014). Classical Renin-Angiotensin system in kidney physiology. Comprehensive Physiology, 4(3), 1201–1228. https://doi.org/10.1002/cphy.c130040[↩]
- Morris DL, Sanghavi D, Kahwaji CI. Angiotensin II. [Updated 2021 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499912[↩]
- Baumgartner, I., & Lerman, L. O. (2011). Renovascular hypertension: screening and modern management. European heart journal, 32(13), 1590–1598. https://doi.org/10.1093/eurheartj/ehq510[↩][↩][↩]
- Hansen KJ, Edwards MS, Craven TE, Cherr GS, Jackson SA, Appel RG, Burke GL, Dean RH. Prevalence of renovascular disease in the elderly: a population-based study. J Vasc Surg. 2002 Sep;36(3):443-51. doi: 10.1067/mva.2002.127351[↩]
- Bloch, M. J., & Basile, J. (2007). Diagnosis and management of renovascular disease and renovascular hypertension. Journal of clinical hypertension (Greenwich, Conn.), 9(5), 381–389. https://doi.org/10.1111/j.1524-6175.2007.06573.x[↩]
- Coen G, Manni M, Giannoni MF, Bianchini G, Calabria S, Mantella D, Pigorini F, Taggi F. Ischemic nephropathy in an elderly nephrologic and hypertensive population. Am J Nephrol. 1998;18(3):221-7. doi: 10.1159/000013340[↩]
- Ralapanawa, D. M., Jayawickreme, K. P., & Ekanayake, E. M. (2016). A case of treatable hypertension: fibromuscular dysplasia of renal arteries. BMC research notes, 9, 6. https://doi.org/10.1186/s13104-015-1835-z[↩]
- Weber, B. R., & Dieter, R. S. (2014). Renal artery stenosis: epidemiology and treatment. International journal of nephrology and renovascular disease, 7, 169–181. https://doi.org/10.2147/IJNRD.S40175[↩][↩]
- Lee HY, Grant EG. Sonography in renovascular hypertension. J Ultrasound Med. 2002 Apr;21(4):431-41. doi: 10.7863/jum.2002.21.4.431[↩]
- Granata, A., Fiorini, F., Andrulli, S., Logias, F., Gallieni, M., Romano, G., Sicurezza, E., & Fiore, C. E. (2009). Doppler ultrasound and renal artery stenosis: An overview. Journal of ultrasound, 12(4), 133–143. https://doi.org/10.1016/j.jus.2009.09.006[↩][↩]
- Wittenberg G, Kenn W, Tschammler A, Sandstede J, Hahn D. Spiral CT angiography of renal arteries: comparison with angiography. Eur Radiol. 1999;9(3):546-51. doi: 10.1007/s003300050707[↩]
- Rountas C, Vlychou M, Vassiou K, Liakopoulos V, Kapsalaki E, Koukoulis G, Fezoulidis IV, Stefanidis I. Imaging modalities for renal artery stenosis in suspected renovascular hypertension: prospective intraindividual comparison of color Doppler US, CT angiography, GD-enhanced MR angiography, and digital substraction angiography. Ren Fail. 2007;29(3):295-302. doi: 10.1080/08860220601166305[↩][↩][↩][↩]
- Perez-Rodriguez, J., Lai, S., Ehst, B. D., Fine, D. M., & Bluemke, D. A. (2009). Nephrogenic systemic fibrosis: incidence, associations, and effect of risk factor assessment–report of 33 cases. Radiology, 250(2), 371–377. https://doi.org/10.1148/radiol.2502080498[↩]
- Louis, R., Levy-Erez, D., Cahill, A. M., & Meyers, K. E. (2018). Imaging studies in pediatric fibromuscular dysplasia (FMD): a single-center experience. Pediatric nephrology (Berlin, Germany), 33(9), 1593–1599. https://doi.org/10.1007/s00467-018-3983-6[↩]
- Huot SJ, Hansson JH, Dey H, Concato J. Utility of captopril renal scans for detecting renal artery stenosis. Arch Intern Med. 2002 Sep 23;162(17):1981-4. doi: 10.1001/archinte.162.17.1981[↩]
- Eklöf H, Ahlström H, Magnusson A, Andersson LG, Andrén B, Hägg A, Bergqvist D, Nyman R. A prospective comparison of duplex ultrasonography, captopril renography, MRA, and CTA in assessing renal artery stenosis. Acta Radiol. 2006 Oct;47(8):764-74. doi: 10.1080/02841850600849092[↩]
- Lao, D., Parasher, P. S., Cho, K. C., & Yeghiazarians, Y. (2011). Atherosclerotic renal artery stenosis–diagnosis and treatment. Mayo Clinic proceedings, 86(7), 649–657. https://doi.org/10.4065/mcp.2011.0181[↩][↩]
- Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Apr 2;127(13):1425-43. doi: 10.1161/CIR.0b013e31828b82aa[↩]
- Hirsch AT, Haskal ZJ, et al.; American Association for Vascular Surgery; Society for Vascular Surgery; Society for Cardiovascular Angiography and Interventions; Society for Vascular Medicine and Biology; Society of Interventional Radiology; ACC/AHA Task Force on Practice Guidelines Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease; American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; Vascular Disease Foundation. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006 Mar 21;113(11):e463-654. doi: 10.1161/CIRCULATIONAHA.106.174526[↩][↩][↩]
- Verdecchia P, Angeli F, Mazzotta G, Martire P, Garofoli M, Gentile G, Reboldi G. Aliskiren versus ramipril in hypertension. Ther Adv Cardiovasc Dis. 2010 Jun;4(3):193-200. doi: 10.1177/1753944710369682. Epub 2010 Apr 23. Erratum in: Ther Adv Cardiovasc Dis. 2010 Aug;4(4):277.[↩]
- Chrysant, S. G., & Chrysant, G. S. (2014). Treatment of hypertension in patients with renal artery stenosis due to fibromuscular dysplasia of the renal arteries. Cardiovascular diagnosis and therapy, 4(1), 36–43. https://doi.org/10.3978/j.issn.2223-3652.2014.02.01[↩][↩]
- Barrier P, Julien A, Guillaume C, Philippe O, Hervé R, Francis J. Technical and clinical results after percutaneous angioplasty in nonmedial fibromuscular dysplasia: outcome after endovascular management of unifocal renal artery stenoses in 30 patients. Cardiovasc Intervent Radiol. 2010 Apr;33(2):270-7. doi: 10.1007/s00270-010-9818-x[↩]
- Zhu Y, Ren J, Ma X, Chen MH, Zhou Y, Jin M, Liu Z. Percutaneous Revascularization for Atherosclerotic Renal Artery Stenosis: A Meta-Analysis of Randomized Controlled Trials. Ann Vasc Surg. 2015 Oct;29(7):1457-67. doi: 10.1016/j.avsg.2015.06.062[↩]
- ASTRAL Investigators, Wheatley K, Ives N, Gray R, Kalra PA, Moss JG, Baigent C, Carr S, Chalmers N, Eadington D, Hamilton G, Lipkin G, Nicholson A, Scoble J. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009 Nov 12;361(20):1953-62. doi: 10.1056/NEJMoa0905368[↩]
- Gupta R, Assiri S, Cooper CJ. Renal Artery Stenosis: New Findings from the CORAL Trial. Curr Cardiol Rep. 2017 Sep;19(9):75. doi: 10.1007/s11886-017-0894-2[↩]
- Bax L, Woittiez AJ, Kouwenberg HJ, Mali WP, Buskens E, Beek FJ, Braam B, Huysmans FT, Schultze Kool LJ, Rutten MJ, Doorenbos CJ, Aarts JC, Rabelink TJ, Plouin PF, Raynaud A, van Montfrans GA, Reekers JA, van den Meiracker AH, Pattynama PM, van de Ven PJ, Vroegindeweij D, Kroon AA, de Haan MW, Postma CT, Beutler JJ. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med. 2009 Jun 16;150(12):840-8, W150-1. doi: 10.7326/0003-4819-150-12-200906160-00119[↩]
- Thomaz MJ, Lucon AM, Praxedes JN, Bortolotto LA, Srougi M. The role of nephrectomy of the atrophic kidney in bearers of renovascular hypertension. Int Braz J Urol. 2010 Mar-Apr;36(2):159-70. doi: 10.1590/s1677-55382010000200005[↩]
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50. doi: 10.1097/AOG.0000000000003020[↩]
- Katigbak C, Fontenot HB. A Primer on the New Guideline for the Prevention, Detection, Evaluation, and Management of Hypertension. Nurs Womens Health. 2018 Aug;22(4):346-354. doi: 10.1016/j.nwh.2018.06.003[↩]
- Gonzalez Suarez, M. L., Kattah, A., Grande, J. P., & Garovic, V. (2019). Renal Disorders in Pregnancy: Core Curriculum 2019. American journal of kidney diseases : the official journal of the National Kidney Foundation, 73(1), 119–130. https://doi.org/10.1053/j.ajkd.2018.06.006[↩]
- High blood pressure during pregnancy. https://www.marchofdimes.org/complications/high-blood-pressure-during-pregnancy.aspx[↩]
- Pulmonary Hypertension Causes and Risk Factors. https://www.nhlbi.nih.gov/health/pulmonary-hypertension/causes[↩]
- What is IH? https://ihrfoundation.org/what-is-ih[↩]
- Idiopathic Intracranial Hypertension (Pseudotumor Cerebri). https://www.aapos.org/glossary/idiopathic-intracranial-hypertension-pseudotumor-cerebri[↩]
- How is Diagnosis Made? https://ihrfoundation.org/what-is-ih/diagnosis[↩]
- Getting Started on DASH. https://www.nhlbi.nih.gov/sites/default/files/publications/GettingStarted.pdf[↩]
- National Institutes of Health. National Heart, Blood and Lung Institute. Your Guide to Lowering Your Blood Pressure With DASH. https://www.nhlbi.nih.gov/health/resources/heart/hbp-dash-how-to[↩]
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014 Feb 5;311(5):507-20. https://jamanetwork.com/journals/jama/fullarticle/1791497 Erratum in: JAMA. 2014 May 7;311(17):1809.[↩][↩][↩]
- Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS, Chalmers J, Mant J, Salam A, Rahimi K, Perkovic V, Rodgers A. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016 Jan 30;387(10017):435-43. doi: 10.1016/S0140-6736(15)00805-3[↩]
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002 Dec 14;360(9349):1903-13. doi: 10.1016/s0140-6736(02)11911-8. Erratum in: Lancet. 2003 Mar 22;361(9362):1060.[↩]