Contents
What is MDMA
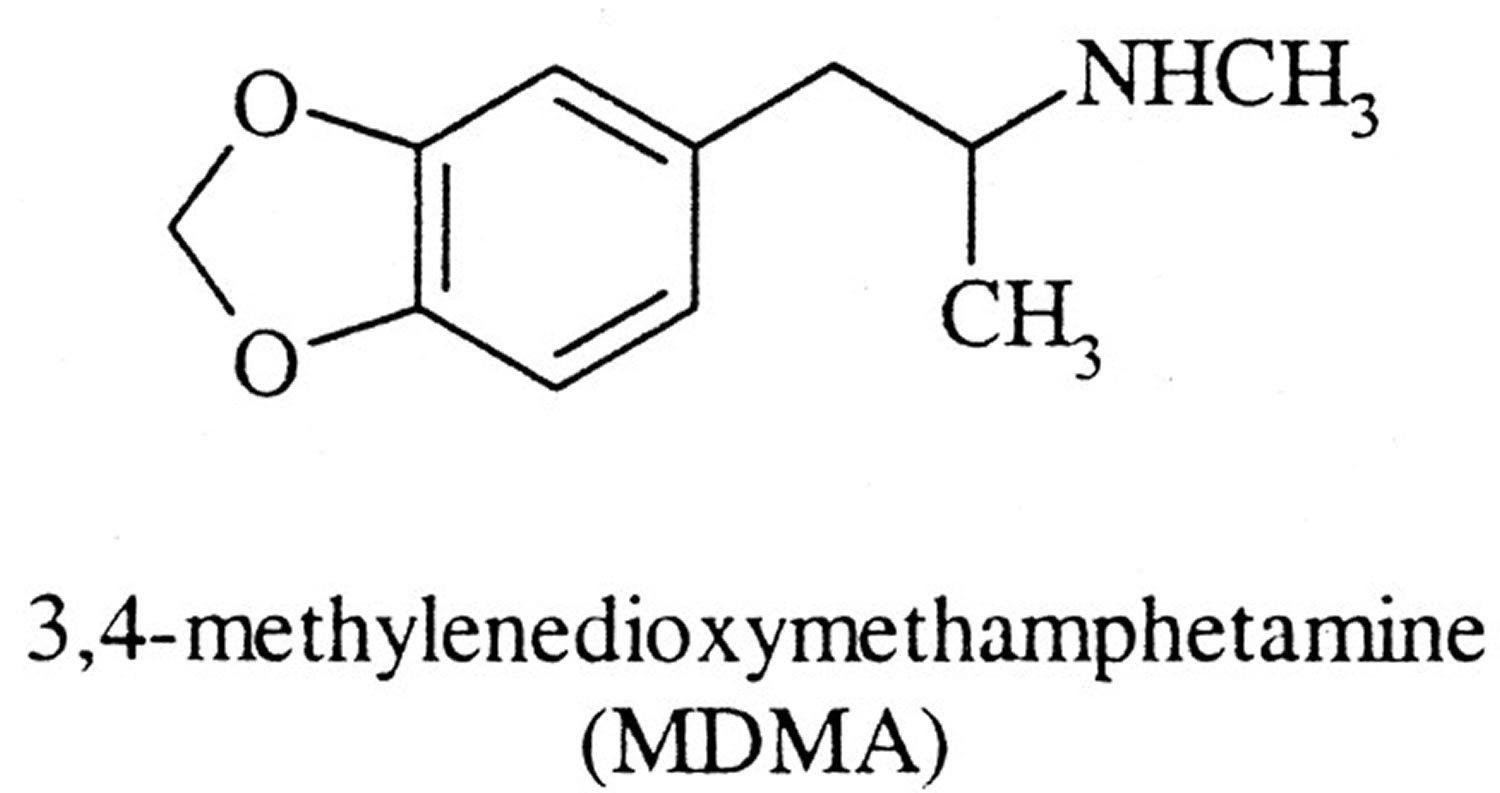
MDMA also known as methylenedioxymethamphetamine, 3,4-methylenedioxymethamphetamine, Ecstasy, Molly, Emma, “love drug“, “E“, “eckies“, “pingers” and “caps” is a man-made or synthetic drug that has effects similar to stimulants like methamphetamine and in higher doses, MDMA can cause hallucinogenic-like effects or psychedelic properties 1, 2, 3, 4. Psychedelics also known as hallucinogens are a class of psychoactive substances (psychotropic substances) that alters your brain function and can change your perception, mood, consciousness, awareness, thoughts, feelings and behavior 5, 6. MDMA’s acts as a central nervous system stimulant (psychostimulant properties) causing you to feel more energetic and alert and having an increased feeling of empathy and compassion towards others and increases your motivation to socialize, which may facilitate social connection 7, 8, 9. MDMA is commonly taken as an illicit drug as a mood enhancer at parties and nightclubs. MDMA is usually swallowed as a tablet but can come in powder, liquid or crystal form. Pills are usually different colors and have pictures or logos stamped on them. Most people take pills, but some may snort (inhaled through the nose), smoke or inject ecstasy. In high doses, MDMA can cause seizures and vomiting. In some cases, MDMA can contribute to death as a result of heart attack, stroke, overheating or if a person drinks too much water.
MDMA influences the activity of at least 3 neurotransmitters (chemical messengers in the brain) that can strongly influence people’s mood and behavior: serotonin, dopamine, and norepinephrine (noradrenaline) and may act directly on some adrenergic, cholinergic, and serotonergic receptors 10, 11, 12. For example, serotonin is a neurotransmitter that plays an important role in the regulation of mood, sleep, pain, and appetite. Like amphetamines, which are chemically similar, MDMA enhances the release of these neurotransmitters and/or blocks their reuptake into nerve cells that send and receive signals in the brain. This increases levels of these neurotransmitters in the brain, which likely causes changes in mood, energy and visual hallucinations, or perceiving things other than reality 13.
Researchers are studying MDMA in supervised clinical research trials as a potential treatment for severe post-traumatic stress disorder (PTSD) and depression 14, 15, 16. “Trauma-focused” psychotherapies that involve focusing on details of the trauma or associated cognitive and emotional effects and cognitive behavioral therapy (CBT) are considered to be the gold standard treatments for PTSD 17. Only two drugs, the selective serotonin reuptake inhibitors (SSRIs) sertraline hydrochloride (Zoloft) and paroxetine hydrochloride (Paxil), are Food and Drug Administration (FDA)-approved first-line oral medications for the treatment of PTSD 18, 19, 20. However, an estimated 40–60% of patients do not respond to these drugs 21. In a meta-analysis evaluating psychotherapy versus drug therapy, trauma-focused psychotherapies resulted in greater and longer lasting improvements than medications 22. Analysis of six phase 2 trials of MDMA-assisted psychotherapy for PTSD have now shown promising safety and efficacy findings 23.
MDMA stimulates the release of neurotransmitters, such as serotonin and norepinephrine, from brain neurons producing a high that lasts from 3 to 6 hours, but the length of a high is variable based on the user. The effects of MDMA are usually felt about 20 minutes to an hour after it is taken and last for around 3-4 hours. MDMA rewarding effects vary with the individual taking it, the dose taken, purity of the MDMA, and the environment in which it is taken. MDMA can produce stimulant effects such as an enhanced sense of pleasure and self-confidence and increased energy. Its psychedelic effects include feelings of peacefulness, acceptance, and empathy. If taking MDMA, think about your setting, who you are with, and your dosage. It is helpful to have a plan in place in case of emergency or if you start to feel unwell.
MDMA comedown or return to normal as the drug leaves the body may last one to 2 days or up to a week.
MDMA mechanism of action
MDMA is a ring-substituted phenethylamine with structural similarities to amphetamine and mescaline that is classified as an entactogen in the Merck Index due to its properties that can promote empathy and compassion for self and others 24, 25, 26, 27. MDMA stimulates the release of at least 3 neurotransmitters (chemical messengers in the brain) that can strongly influence people’s mood and behavior: serotonin, dopamine, and norepinephrine (noradrenaline) and may act directly on some adrenergic, cholinergic, and serotonergic receptors 10, 11, 12. MDMA elevates levels of the neurohormone oxytocin, an effect likely mediated through direct or indirect action on 5HT1A, 5HT2A, and 5HT4 receptors 28, 29, 30, as well as elevating levels of prolactin, arginine vasopressin (AVP), adrenocorticotrophic hormone (ACTH), and cortisol 31, 32, 33, 34. The effects of MDMA are believed to be mediated by a number of mechanisms, including monoamine release, serotonin and norepinephrine transporter reuptake inhibition, monoamine oxidase inhibition, partial agonism of serotonin receptors (5-HT2A, 5-HT1A, and 5-HT2C receptors), and increase in blood concentrations of oxytocin 35, 36, 37, 38, 39.
MDMA is classified as an “empathogen”, which means it increases feelings of empathy and compassion towards others 7. MDMA possesses a unique pharmacodynamic profile in humans that includes increased emotional empathy, an increase in feelings of interpersonal closeness, greater prosocial behavior, and an increased ability to tolerate distressing memories, greater reward from pleasant memories, and less distress in response to social exclusion 40, 41, 42, 43, 44. In laboratory studies in healthy human volunteers, MDMA enhances subjective feelings of sociability, friendliness, and confidence, in addition to positive affective responses to social cues 45, 46, 47, 48, 49. Furthermore, MDMA reduces responses to negative social input, such as blunting neural responses to threatening social stimuli and alleviating social anxiety 46, 50. It is perhaps partly as a result of these prosocial effects that MDMA has shown promise as an adjunct to psychotherapy in the treatment of PTSD 14.
Imaging studies found that MDMA reduced activity in brain areas associated with anxiety, including the amygdala, and increased activity in prefrontal cortex 51, 52, 53. Hypotheses for MDMA’s therapeutic action include enhanced fear extinction, memory reconsolidation, enhanced therapeutic alliance, widening a window of tolerance for distressing thoughts or experiences, and re-opening or enhancing a critical period for experiencing social reward 54, 55, 30. It is likely through these effects that MDMA augments and enhances effectiveness of psychotherapy 15.
MDMA also acts as a psychostimulant, since it speeds up the workings of the central nervous system (brain and spinal cord) and at high doses can also alter someone’s perception of reality giving it hallucinogenic qualities.
MDMA works by stimulating the central nervous system. This means people can feel a burst of energy.
MDMA can also heighten and distort your senses (sight and sound), and can increase feelings of love and happiness. This is often caused by the increase in brain chemicals such as serotonin (happy) and dopamine (reward).
The effects of MDMA can vary from person to person and depend on factors such as:
- the amount and strength of the dose
- your physical make-up and state of mind
- how you respond to the drug (for example, a first-time user may experience different effects to someone who has used it before)
- whether it has been mixed with other drugs.
Generally, MDMA effects begin around 20 minutes and will last around 3 to 4 hours. They may include:
- Euphoria and feeling energetic and confident
- Accelerated heart rate and breathing
- Rise in blood pressure
- Sweating and dehydration
- Nausea
- Jaw clenching and teeth grinding
- Tingling skin and muscle aches and pains
- Dilated pupils
- Loss of appetite
- Heightened senses
- Sleep problems
- Feeling affectionate and an increased sex drive (libido)
- Loss of inhibitions
- Excessive thirst – drinking large amounts of water, which can result in death (approximately 250-500 ml of water per hour is okay).
In addition to these symptoms, people who take MDMA in large or strong doses, may experience further effects such as:
- Changes in perception (such as auditory and visual hallucinations)
- Irrational behavior that seems out of character – aggression, paranoia
- Anxiety and irritability
- Vomiting.
After experiencing a high, “coming down” from MDMA can be an unpleasant experience, but rarely dangerous. Typically, you should feel better in 2 to 3 days.
Your comedown experience will depend on a range of factors. Symptoms may include:
- Sleep problems and fatigue
- Aching muscles
- Anxiety, agitation, depression
- Trouble concentrating.
MDMA effect in the brain
MDMA exerts its primary effects in the brain on neurons that use the chemicals serotonin, dopamine and norepinephrine to communicate with other neurons.
Serotonin is most likely responsible for the feelings of empathy, elevated mood, and emotional closeness experienced with this drug. Overall, these neurotransmitter systems play an important role in regulating:
- mood
- energy/activity and the reward system
- appetite
- aggression
- sexual activity
- sleep
- sensitivity to pain
- heart rate, blood pressure
Research in animals indicates that MDMA is neurotoxic and may affect the brain. Clinical studies suggest that MDMA may increase the risk of long-term or permanent problems with memory and learning.
Can I get addicted to MDMA?
Research suggests MDMA is potentially addictive, although more research is needed. Some people who use MDMA say that it is hard to stop taking MDMA and report symptoms of an MDMA-related substance use disorder, indicating that it is possible to become psychologically dependent 56. These symptoms include continued use despite negative side effects, tolerance—which is needing to take increasingly larger amounts of a drug for the same effects—withdrawal side effects, and craving 56. Like many other drugs, someone can build up a tolerance to MDMA. This means they need to take larger and larger doses to try and achieve the same effect. However, this can also increase the intensity of MDMA unpleasant side effects. Almost 60% of people who use Ecstasy report some withdrawal symptoms, including fatigue, loss of appetite, depressed feelings, and trouble concentrating.
MDMA users may encounter problems similar to those experienced by amphetamine and cocaine users, including addiction. Research has shown that animals will self-administer MDMA, an important indicator of a drug’s addictive potential. However, those studies show that animals did not take MDMA as much as some other addictive drugs such as cocaine 57.
Some people who use MDMA do report symptoms of addiction, including continued use despite negative consequences, tolerance, withdrawal, and craving.
After moderate use of MDMA over one week, psychological and physical effects due to withdrawal may include:
- irritability
- depression
- confusion
- agression and impulsiveness
- muscle cramps
- problems with sleep
- anxiety
- memory deficits
- loss of attention
- nausea and decreased appetite
- loss of interest in sex
What is MDMA used to treat?
The U.S. Food and Drug Administration (FDA) has not approved MDMA as a treatment for any medical condition. MDMA therapies have only been approved for research purposes, with no widely accepted medical indications. In 2016, the United States Food and Drug Administration (FDA) approved the Multidisciplinary Association for Psychedelic Studies (MAPS, a nonprofit organization that was founded in 1986 to increase the knowledge base of psychedelic substances) investigators’ design for two phase 3 clinical trials investigating MDMA for the treatment of post-traumatic stress disorder (PTSD) 58. In 2017, the FDA designated MDMA-assisted psychotherapy as a “breakthrough therapy” based on its use in assisting psychotherapy for the treatment of post-traumatic stress disorder (PTSD), giving it priority consideration in the regulatory process 59. MDMA-assisted psychotherapy involves talk therapy (psychotherapy) alongside the ingestion of MDMA 60. Pilot studies indicate that MDMA-assisted psychotherapy may be beneficial in treating social anxiety in autistic adults 50, 61. In these pilot studies, the vast majority of participants reported increased feelings of empathy that persisted after the therapy sessions 62.
Researchers are studying MDMA in supervised clinical research trials as a potential treatment for severe post-traumatic stress disorder (PTSD) and depression 14, 15, 16. Analysis of six phase 2 trials of MDMA-assisted psychotherapy for PTSD have now shown promising safety and efficacy findings 23. Across six phase 2 trials (105 participants) following MDMA-assisted psychotherapy, 54% of participants did not meet the criteria for PTSD, compared to 23% in the control group 63. At long-term follow-up, this increased to 67.0%. Most participants also reported other benefits, including improved relationships and well-being, better sleep quality, and post-traumatic growth 63.
The first phase 3 trial of any psychedelic-assisted therapy (MAPP1), participants who received MDMA-assisted therapy reported a significant reduction in severe PTSD symptoms compared to those who received placebo with therapy 64. 67% of the group who received MDMA, compared to 32% of the group who received a placebo, no longer qualified for a PTSD diagnosis after three treatment sessions 64. In addition, participants treated with MDMA-assisted therapy had statistically significant reductions for the key secondary endpoint of functional impairment relative to placebo with therapy 64.
The second phase 3 MDMA trial (MAPP2) produced data that confirmed the findings of the first Phase 3 trial (MAPP1), which suggests that MDMA-assisted therapy can benefit a broader range of people who have PTSD 65. It’s important to emphasize that this trial included participants with both moderate and severe PTSD, and about half of the participants were from diverse racial and ethnic backgrounds.
Participants in the phase 3 MDMA trial (MAPP2) MDMA-assisted therapy group experienced a significant reduction in PTSD symptoms versus participants receiving a placebo with therapy as measured by a change from baseline in the Clinician-Administered PTSD Scale for DSM-5 (“CAPS-5”) total severity score 65. The data also demonstrated that MDMA-assisted therapy significantly reduced clinician-rated functional impairment as measured by change from baseline in the modified Sheehan Disability Scale (“SDS”) 65. When compared with conventional treatments, phase 3 results of MDMA-assisted therapy (MAPP2) demonstrated lower dropout rates (7.6%), as well as very high response rates (80%), with only ~1/3 of participants meeting diagnostic criteria for PTSD at trial completion 14.
Most common treatment emergent adverse event in the phase 3 MDMA trial (MAPP2) include 65:
- Muscle tightness
- Nausea
- Decreased appetite
- Hyperhidrosis
- Feeling hot
- Feeling cold
- Paresthesia
- Chest discomfort
- Dry mouth
- Chills
- Feeling jittery
- Restlessness
- Vision blurred
- Bruxism
- Nystagmus
- Mydriasis
- Tremor.
Rates of cardiac treatment emergent adverse events were low, and increases in blood pressure and pulse were mild, transient and consistent with MDMA’s sympathomimetic effects 66, 67, 68. Consistent with PTSD, suicidal ideation was observed in both groups. MDMA did not appear to increase this risk, and no suicidal behavior was observed. There were no deaths or serious treatment emergent adverse event in the phase 3 MDMA trial (MAPP2) 65. These data suggest that MDMA-assisted therapy reduced PTSD symptoms and functional impairment in a diverse population with moderate to severe PTSD and was generally well tolerated (although there have not yet been head-to-head trials comparing MDMA to conventional treatments) 65.
Is MDMA safe?
MDMA was originally developed in Germany in 1912 by the Merck chemical company as a potential therapeutic agent to decrease clotting time and to prevent bleeding 61. MDMA did not prove efficacious for use as a blood clotting drug, but its psychoactive properties were recognized. Chemist Alexander Shulgin resynthesized MDMA in 1976, and the first published report characterizing the psychoactive effects of MDMA appeared in 1978 69. These psychoactive properties encouraged MDMA’s use as a recreational drug. Pure MDMA used in approved clinical settings is far safer than recreational use of Ecstasy or Molly. Today, MDMA is generally made in illegal laboratories, which means the person taking it has no idea if the dose will be strong or weak, or even if it will contain any MDMA at all. It is possible for pills sold as ecstasy tablets to contain little or no MDMA. They may contain other chemicals such as amphetamines, paramethoxyamphetamine (PMA), paramethoxymethamphetamine (PMMA) or ketamine or ‘fillers’ such as household products which may have unexpected or dangerous side effects.
MDMA can be dangerous if it is mixed with other drugs including alcohol, cocaine, amphetamines, ice and some prescription medications such as antidepressants.
MDMA can cause negative health effects, some potentially serious. People with certain conditions such as epilepsy, high blood pressure, heart disease, diabetes, kidney disease or mood or psychiatric disorders are at greater risk of harm if they take MDMA.
MDMA use can lead to serious harm including:
- cardiac arrest
- stroke
- kidney failure
- overheating (hyperthermia) and dehydration
- dilutional hyponatremia – where a person’s brain swells from drinking too much water and can lead to coma.
- death.
MDMA’s effects depend on the amount used, the purity of MDMA taken, and where and how a person is taking it. Using MDMA with other substances such as alcohol or some prescription drugs, including selective serotonin reuptake inhibitors (SSRIs), may increase the risk of negative health effects 1.
Health risks associated with using MDMA
Negative health effects of taking MDMA may include higher blood pressure, involuntary jaw clenching, nausea, vomiting, and restless legs. While deaths associated with MDMA use are rare, taking MDMA can also lead to more severe side effects. People can experience a dangerously steep rise in body temperature called hyperpyrexia, particularly if they are very physically active or are in a warm environment such as a club 70. Long-term MDMA use can also lead to heart problems or liver damage 57.
Changes in Mood and Brain Function
MDMA use has been associated with anxiety and panic attacks 13. Studies have shown that people who regularly use MDMA may experience poor sleep, a lack of appetite, confusion, depression, anxiety, paranoia, and memory or attention problems 57.
Contamination With Other Drugs
Chemical analyses of drugs sold as MDMA have shown that they may be adulterated, meaning they contain other types of drugs, perhaps without the buyer knowing it. These hidden ingredients have included ketamine, amphetamine, synthetic cathinones (“bath salts”), 3,4-methylinedioxy-amphetamine (MDA), and methamphetamine 71.
Taking an adulterated drug can lead to unexpected and unwelcome side effects and may increase its potential health risks. Over the past decade, illegally made opioids like fentanyl have been increasingly found in the drug supply, and have contributed to a dramatic rise in drug overdose deaths in the United States.
Harms During Pregnancy
MDMA is a moderately teratogenic drug (i.e., it is toxic to the fetus) 72, 73. Only a few studies have examined the effects of prenatal MDMA exposure, but evidence suggests that children born to people who took MDMA during pregnancy had an increased risk of birth defects, including heart problems and developmental delays in motor skills like standing and walking 74, 75, 76. The severity of these developmental delays increases with heavier MDMA use 76, 77.
MDMA side effects
In high doses, MDMA can cause hallucinations and floating sensations, as well as seizures and vomiting. In some cases, MDMA can contribute to death as a result of heart attack, stroke, overheating or if a person drinks too much water.
MDMA side effect may include:
- nausea
- muscle cramping
- involuntary teeth clenching
- blurred vision
- chills
- sweating / hyperthermia
Also, there is evidence that people who develop a rash that looks like acne after using MDMA may be at risk of severe side effects, including liver damage, if they continue to use MDMA.
Because MDMA use promotes trust, closeness, empathy, and enhances sexual desire, the risk of unsafe sexual practices may increase, resulting in HIV/AIDS, hepatitis, or other sexually transmitted diseases.
Damage to brain serotonin neurons can occur; serotonin is thought to play a role in regulating mood, memory, sleep, and appetite. Studies are conflicting on MDMA use and its affects on memory and cognition.
MDMA overdose
If the strength of MDMA dose is high or if MDMA is taken in large amounts, it can cause bad reactions or overdose. Signs to watch for include:
- seizures (‘fits’) and vomiting
- a sharp rise in body temperature and blood pressure
- dizziness and confusion
- anxiety
- paranoia
- aggression
- muscle twitching or cramps
- heart palpitations.
MDMA-related fatalities at raves have been reported. The stimulant effects of MDMA, which enable the user to dance for extended periods, combined with the hot, crowded conditions usually found at raves can lead to dehydration, hyperthermia (dangerous increase in body temperature), and heart or kidney failure.
Repeated use within a short timeframe can be dangerous because MDMA cannot be adequately removed from the body.
Other drugs chemically similar to MDMA, such as MDA (methylenedioxyamphetamine, the parent drug of Ecstasy) and PMA (paramethoxyamphetamine) have been associated with fatalities in the U.S. and Australia and are sometimes sold as Ecstasy. These drugs can be toxic to the brain or create additional health risks to the user.
Additionally, the illegal sale of Ecstasy or Molly makes it prone to being “cut” with other illicit and potentially toxic or deadly chemicals. Ecstasy or Molly may contain other substances in addition to MDMA, including:
- ketamine (an anesthetic used mostly by veterinarians that also has phencyclidine (PCP)-like effects)
- caffeine
- bath salts (synthetic cathinones)
- cocaine
- methamphetamine
While the combination of Ecstasy with one or more of these drugs may be inherently dangerous, users might also voluntarily combine them with substances, such as marijuana, alcohol, or opioids, putting themselves at further risk of physical harm, overdose, or death.
In addition, fentanyl has been increasingly found cut into other street drugs, often unknown by the user and leading to fatalities.
MDMA dependence, tolerance and withdrawal
Some people who use MDMA say that it is hard to stop taking MDMA, indicating that it is possible to become psychologically dependent. Like many other drugs, someone can build up a tolerance to MDMA. This means they need to take larger and larger doses to try and achieve the same effect. However, this can also increase the intensity of MDMA unpleasant side effects.
MDMA long-term effects
Research on the long-term effects of MDMA is limited, however studies suggest that regular long-term use can cause:
- Liver damage
- Memory and concentration problems
- Colds or flu
- Depression
- Risk of HIV, hepatitis, blood poisoning or skin abscesses if MDMA is injected using shared needles
- Increased use of other drugs such as benzodiazepines, alcohol or cannabis.
- Papaseit E, Pérez-Mañá C, Torrens M, Farré A, Poyatos L, Hladun O, Sanvisens A, Muga R, Farré M. MDMA interactions with pharmaceuticals and drugs of abuse. Expert Opin Drug Metab Toxicol. 2020 May;16(5):357-369. https://doi.org/10.1080/17425255.2020.1749262[↩][↩]
- Dumont GJ, Verkes RJ. A review of acute effects of 3,4-methylenedioxymethamphetamine in healthy volunteers. J Psychopharmacol. 2006 Mar;20(2):176-87. doi: 10.1177/0269881106063271[↩]
- Liechti ME, Vollenweider FX. Which neuroreceptors mediate the subjective effects of MDMA in humans? A summary of mechanistic studies. Hum Psychopharmacol. 2001 Dec;16(8):589-598. doi: 10.1002/hup.348[↩]
- Schmid Y, Hysek CM, Simmler LD, Crockett MJ, Quednow BB, Liechti ME. Differential effects of MDMA and methylphenidate on social cognition. J Psychopharmacol. 2014 Sep;28(9):847-56. doi: 10.1177/0269881114542454[↩]
- Green AR, Mechan AO, Elliott JM, O’Shea E, Colado MI. The pharmacology and clinical pharmacology of 3,4-methylenedioxymethamphetamine (MDMA, “ecstasy”). Pharmacol Rev. 2003 Sep;55(3):463-508. doi: 10.1124/pr.55.3.3[↩]
- Luethi D, Liechti ME. Monoamine Transporter and Receptor Interaction Profiles in Vitro Predict Reported Human Doses of Novel Psychoactive Stimulants and Psychedelics. Int J Neuropsychopharmacol. 2018 Oct 1;21(10):926-931. doi: 10.1093/ijnp/pyy047[↩]
- Bershad AK, Hsu DT, de Wit H. MDMA enhances positive affective responses to social feedback. J Psychopharmacol. 2024 Mar;38(3):297-304. doi: 10.1177/02698811231224153[↩][↩]
- Bershad AK, Miller MA, Baggott MJ, de Wit H. The effects of MDMA on socio-emotional processing: Does MDMA differ from other stimulants? J Psychopharmacol. 2016 Dec;30(12):1248-1258. doi: 10.1177/0269881116663120[↩]
- Kamilar-Britt P, Bedi G. The prosocial effects of 3,4-methylenedioxymethamphetamine (MDMA): Controlled studies in humans and laboratory animals. Neurosci Biobehav Rev. 2015 Oct;57:433-46. doi: 10.1016/j.neubiorev.2015.08.016[↩]
- Feduccia, A.A., Holland, J. & Mithoefer, M.C. Progress and promise for the MDMA drug development program. Psychopharmacology 235, 561–571 (2018). https://doi.org/10.1007/s00213-017-4779-2[↩][↩]
- Liechti M. Novel psychoactive substances (designer drugs): overview and pharmacology of modulators of monoamine signaling. Swiss Med. Wkly. 2015:3. doi: 10.4414/smw.2015.14043[↩][↩]
- Avram, M., Fortea, L., Wollner, L. et al. Large-scale brain connectivity changes following the administration of lysergic acid diethylamide, d-amphetamine, and 3,4-methylenedioxyamphetamine. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02734-y[↩][↩]
- Michael White C. How MDMA’s pharmacology and pharmacokinetics drive desired effects and harms. J Clin Pharmacol. 2014 Mar;54(3):245-52. doi: 10.1002/jcph.266[↩][↩]
- Mitchell JM, Bogenschutz M, Lilienstein A, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med. 2021 Jun;27(6):1025-1033. doi: 10.1038/s41591-021-01336-3[↩][↩][↩][↩]
- Feduccia AA, Jerome L, Yazar-Klosinski B, Emerson A, Mithoefer MC, Doblin R. Breakthrough for Trauma Treatment: Safety and Efficacy of MDMA-Assisted Psychotherapy Compared to Paroxetine and Sertraline. Front Psychiatry. 2019 Sep 12;10:650. doi: 10.3389/fpsyt.2019.00650[↩][↩][↩]
- Reiff CM, Richman EE, Nemeroff CB, Carpenter LL, Widge AS, Rodriguez CI, Kalin NH, McDonald WM; the Work Group on Biomarkers and Novel Treatments, a Division of the American Psychiatric Association Council of Research. Psychedelics and Psychedelic-Assisted Psychotherapy. Am J Psychiatry. 2020 May 1;177(5):391-410. doi: 10.1176/appi.ajp.2019.19010035[↩][↩]
- Watkins LE, Sprang KR, Rothbaum BO. Treating PTSD: A Review of Evidence-Based Psychotherapy Interventions. Front Behav Neurosci. 2018 Nov 2;12:258. doi: 10.3389/fnbeh.2018.00258[↩]
- Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA (2000) 283:1837–44. 10.1001/jama.283.14.1837[↩]
- Davidson JR, Rothbaum BO, Van Der Kolk BA, Sikes CR, Farfel GM. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry (2001) 58:485–92. 10.1001/archpsyc.58.5.485[↩]
- Friedman MJ, Marmar CR, Baker DG, Sikes CR, Farfel GM. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry (2007) 68:711–20. 10.4088/JCP.v68n0508[↩]
- Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for Military-Related PTSD: A Review of Randomized Clinical Trials. JAMA. 2015;314(5):489–500. doi:10.1001/jama.2015.8370[↩]
- Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, Hoge CW. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety (2016) 33:792–806. doi: 10.1002/da.22511[↩]
- Mithoefer MC, Feduccia AA, Jerome L, Mithoefer A, Wagner M, Walsh Z, Hamilton S, Yazar-Klosinski B, Emerson A, Doblin R. MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials. Psychopharmacology (Berl). 2019 Sep;236(9):2735-2745. doi: 10.1007/s00213-019-05249-5. Epub 2019 May 7. Retraction in: Psychopharmacology (Berl). 2024 Nov;241(11):2405. doi: 10.1007/s00213-024-06666-x[↩][↩]
- O’neil MJ. The Merck index: an encyclopedia of chemicals, drugs, and biologicals. 15th edition Whitehouse Station, NJ: RSC Publishing; (2013).[↩]
- Harris DS, Baggott M, Mendelson JH, Mendelson JE, Jones RT. Subjective and hormonal effects of 3,4-methylenedioxymethamphetamine (MDMA) in humans. Psychopharmacology (Berl). 2002 Aug;162(4):396-405. doi: 10.1007/s00213-002-1131-1[↩]
- Cami J, Farré M, Mas M, Roset PN, Poudevida S, Mas A, San L, de la Torre R. Human pharmacology of 3,4-methylenedioxymethamphetamine (“ecstasy”): psychomotor performance and subjective effects. J Clin Psychopharmacol. 2000 Aug;20(4):455-66. doi: 10.1097/00004714-200008000-00010[↩]
- Kirkpatrick MG, Baggott MJ, Mendelson JE, Galloway GP, Liechti ME, Hysek CM, de Wit H. MDMA effects consistent across laboratories. Psychopharmacology (Berl). 2014 Oct;231(19):3899-905. doi: 10.1007/s00213-014-3528-z[↩]
- Thompson MR, Hunt GE, Mcgregor IS. Neural correlates of MDMA (“Ecstasy”)-induced social interaction in rats. Soc Neurosci (2009) 4:60–72. 10.1080/17470910802045042[↩]
- Curry DW, Berro LF, Belkoff AR, Sulima A, Rice KC, Howell LL. Sensitization to the prosocial effects of 3,4-methylenedioxymethamphetamine (MDMA). Neuropharmacology (2019) 151:13–20. 10.1016/j.neuropharm.2019.03.017[↩]
- Nardou R, Lewis EM, Rothhaas R, Xu R, Yang A, Boyden E, et al. Oxytocin-dependent reopening of a social reward learning critical period with MDMA. Nature (2019) 569 (7754):116–20. 10.1038/s41586-019-1075-9[↩][↩]
- Grob CS, Poland RE, Chang L, Ernst T. Psychobiologic effects of 3,4-methylenedioxymethamphetamine in humans: methodological considerations and preliminary observations. Behav Brain Res (1996) 73:103–7. 10.1016/0166-4328(96)00078-2[↩]
- Dumont GJ, Sweep FC, Van Der Steen R, Hermsen R, Donders AR, Touw DJ, et al. Increased oxytocin concentrations and prosocial feelings in humans after ecstasy (3,4-methylenedioxymethamphetamine) administration. Soc Neurosci (2009) 4:359–66. 10.1080/17470910802649470[↩]
- Simmler LD, Hysek CM, Liechti ME. Sex differences in the effects of MDMA (ecstasy) on plasma copeptin in healthy subjects. J Clin Endocrinol Metab (2011) 96:2844–50. 10.1210/jc.2011-1143[↩]
- Hysek CM, Domes G, Liechti ME. MDMA enhances “mind reading” of positive emotions and impairs “mind reading” of negative emotions. Psychopharmacology (Berl) (2012) 222:293–302. 10.1007/s00213-012-2645-9[↩]
- Simmler LD, Liechti ME. Pharmacology of MDMA- and Amphetamine-Like New Psychoactive Substances. Berlin, Heidelberg, Springer, pp 1-22[↩]
- Dumont GJ, Sweep FC, van der Steen R, Hermsen R, Donders AR, Touw DJ, van Gerven JM, Buitelaar JK, Verkes RJ. Increased oxytocin concentrations and prosocial feelings in humans after ecstasy (3,4-methylenedioxymethamphetamine) administration. Soc Neurosci. 2009;4(4):359-66. doi: 10.1080/17470910802649470[↩]
- Young MB, Norrholm SD, Khoury LM, Jovanovic T, Rauch SAM, Reiff CM, Dunlop BW, Rothbaum BO, Howell LL. Inhibition of serotonin transporters disrupts the enhancement of fear memory extinction by 3,4-methylenedioxymethamphetamine (MDMA). Psychopharmacology (Berl). 2017 Oct;234(19):2883-2895. doi: 10.1007/s00213-017-4684-8[↩]
- Kuypers KPC, Dolder PC, Ramaekers JG, Liechti ME. Multifaceted empathy of healthy volunteers after single doses of MDMA: A pooled sample of placebo-controlled studies. J Psychopharmacol. 2017 May;31(5):589-598. doi: 10.1177/0269881117699617[↩]
- Setola V, Hufeisen SJ, Grande-Allen KJ, Vesely I, Glennon RA, Blough B, Rothman RB, Roth BL. 3,4-methylenedioxymethamphetamine (MDMA, “Ecstasy”) induces fenfluramine-like proliferative actions on human cardiac valvular interstitial cells in vitro. Mol Pharmacol. 2003 Jun;63(6):1223-9. doi: 10.1124/mol.63.6.1223[↩]
- Carhart-Harris RL, Wall MB, Erritzoe D, Kaelen M, Ferguson B, De Meer I, et al. The effect of acutely administered MDMA on subjective and BOLD-fMRI responses to favourite and worst autobiographical memories. Int J Neuropsychopharmacol (2014) 17:527–40. 10.1017/S1461145713001405[↩]
- Frye CG, Wardle MC, Norman GJ, De Wit H. MDMA decreases the effects of simulated social rejection. Pharmacol Biochem Behav (2014) 117:1–6. 10.1016/j.pbb.2013.11.030[↩]
- Hysek CM, Schmid Y, Simmler LD, Domes G, Heinrichs M, Eisenegger C, et al. MDMA enhances emotional empathy and prosocial behavior. Soc Cogn Affect Neurosci (2014) 9:1645–52. 10.1093/scan/nst161[↩]
- Kirkpatrick MG, Baggott MJ, Mendelson JE, Galloway GP, Liechti ME, Hysek CM, et al. MDMA effects consistent across laboratories. Psychopharmacology (Berl) (2014) 231:3899–905. 10.1007/s00213-014-3528-z[↩]
- Bershad AK, Miller MA, Baggott MJ, De Wit H. The effects of MDMA on socio-emotional processing: does MDMA differ from other stimulants? J Psychopharmacol (2016) 30:1248–58. 10.1177/0269881116663120[↩]
- Baggott MJ, Coyle JR, Siegrist JD, Garrison KJ, Galloway GP, Mendelson JE. Effects of 3,4-methylenedioxymethamphetamine on socioemotional feelings, authenticity, and autobiographical disclosure in healthy volunteers in a controlled setting. J Psychopharmacol. 2016 Apr;30(4):378-87. doi: 10.1177/0269881115626348[↩]
- Bedi G, Phan KL, Angstadt M, de Wit H. Effects of MDMA on sociability and neural response to social threat and social reward. Psychopharmacology (Berl). 2009 Nov;207(1):73-83. doi: 10.1007/s00213-009-1635-z[↩][↩]
- Bershad AK, Mayo LM, Van Hedger K, McGlone F, Walker SC, de Wit H. Effects of MDMA on attention to positive social cues and pleasantness of affective touch. Neuropsychopharmacology. 2019 Sep;44(10):1698-1705. doi: 10.1038/s41386-019-0402-z[↩]
- Kirkpatrick MG, Lee R, Wardle MC, Jacob S, de Wit H. Effects of MDMA and Intranasal oxytocin on social and emotional processing. Neuropsychopharmacology. 2014 Jun;39(7):1654-63. doi: 10.1038/npp.2014.12[↩]
- Wardle MC, de Wit H. MDMA alters emotional processing and facilitates positive social interaction. Psychopharmacology (Berl). 2014 Oct;231(21):4219-29. doi: 10.1007/s00213-014-3570-x[↩]
- Danforth AL, Grob CS, Struble C, Feduccia AA, Walker N, Jerome L, Yazar-Klosinski B, Emerson A. Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: a randomized, double-blind, placebo-controlled pilot study. Psychopharmacology (Berl). 2018 Nov;235(11):3137-3148. doi: 10.1007/s00213-018-5010-9[↩][↩]
- Gamma A, Buck A, Berthold T, Liechti ME, Vollenweider FX. 3,4-Methylenedioxymethamphetamine (MDMA) modulates cortical and limbic brain activity as measured by [H(2)(15)O]-PET in healthy humans. Neuropsychopharmacology (2000) 23:388–95. 10.1016/S0893-133X(00)00130-5[↩]
- Bedi G, Phan KL, Angstadt M, De Wit H. Effects of MDMA on sociability and neural response to social threat and social reward. Psychopharmacology (Berl) (2009) 207:73–83. 10.1007/s00213-009-1635-z[↩]
- Carhart-Harris RL, Murphy K, Leech R, Erritzoe D, Wall MB, Ferguson B, et al. The Effects of Acutely Administered 3,4-methylenedioxymethamphetamine on spontaneous brain function in healthy volunteers measured with arterial spin labeling and blood oxygen level-dependent resting state functional connectivity. Biol Psychiatry (2015) 78:554–62. 10.1016/j.biopsych.2013.12.015[↩]
- Mithoefer MC, Grob CS, Brewerton TD. Novel psychopharmacological therapies for psychiatric disorders: psilocybin and MDMA. Lancet Psychiatry (2016) 3 (5):481–88. 10.1016/S2215-0366(15)00576-3[↩]
- Feduccia AA, Mithoefer MC. MDMA-assisted psychotherapy for PTSD: are memory reconsolidation and fear extinction underlying mechanisms? Prog Neuropsychopharmacol Biol Psychiatry (2018) 84:221–8. 10.1016/j.pnpbp.2018.03.003[↩]
- Wu LT, Ringwalt CL, Weiss RD, Blazer DG. Hallucinogen-related disorders in a national sample of adolescents: the influence of ecstasy/MDMA use. Drug Alcohol Depend. 2009 Sep 1;104(1-2):156-66. doi: 10.1016/j.drugalcdep.2009.04.014[↩][↩]
- Dunlap LE, Andrews AM, Olson DE. Dark Classics in Chemical Neuroscience: 3,4-Methylenedioxymethamphetamine. ACS Chem Neurosci. 2018 Oct 17;9(10):2408-2427. doi: 10.1021/acschemneuro.8b00155[↩][↩][↩]
- Multidisciplinary Association for Psychedelic Studies (MAPS): FDA agrees to phase 3 trials of MDMA-assisted psychotherapy for PTSD. November 29, 2016. https://maps.org/2016/11/29/fda-agrees-to-phase-3-trials-of-mdma-assisted-psychotherapy-for-ptsd/[↩]
- Multidisciplinary Association for Psychedelic Studies (MAPS): A phase 3 program of MDMA-assisted psychotherapy for the treatment of severe posttraumatic stress disorder. 2017. https://maps.org/research/mdma/ptsd/phase3[↩]
- MDMA-Assisted Therapy Guide. https://psychedelic.support/resources/mdma-assisted-therapy-guide[↩]
- Danforth AL, Struble CM, Yazar-Klosinski B, Grob CS. MDMA-assisted therapy: A new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016 Jan 4;64:237-49. doi: 10.1016/j.pnpbp.2015.03.011[↩][↩]
- Psychedelic Support: First Clinical Trial: Social Anxiety in Autistic Adults Successfully Treated with MDMA Therapy. https://maps.org/news/media/psychedelic-support-first-clinical-trial-social-anxiety-in-autistic-adults-successfully-treated-with-mdma-therapy[↩]
- Mithoefer, M.C., Feduccia, A.A., Jerome, L. et al. RETRACTED ARTICLE: MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials. Psychopharmacology 236, 2735–2745 (2019). https://doi.org/10.1007/s00213-019-05249-5[↩][↩]
- Mitchell, J.M., Bogenschutz, M., Lilienstein, A. et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med 27, 1025–1033 (2021). https://doi.org/10.1038/s41591-021-01336-3[↩][↩][↩]
- Mitchell, J.M., Ot’alora G., M., van der Kolk, B. et al. MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial. Nat Med 29, 2473–2480 (2023). https://doi.org/10.1038/s41591-023-02565-4[↩][↩][↩][↩][↩][↩]
- Feduccia AA, Mithoefer MC. MDMA-assisted psychotherapy for PTSD: Are memory reconsolidation and fear extinction underlying mechanisms? Prog Neuropsychopharmacol Biol Psychiatry. 2018 Jun 8;84(Pt A):221-228. doi: 10.1016/j.pnpbp.2018.03.003[↩]
- Lester SJ, Baggott M, Welm S, Schiller NB, Jones RT, Foster E, Mendelson J. Cardiovascular effects of 3,4-methylenedioxymethamphetamine. A double-blind, placebo-controlled trial. Ann Intern Med. 2000 Dec 19;133(12):969-73. doi: 10.7326/0003-4819-133-12-200012190-00012[↩]
- Vizeli P, Liechti ME. Safety pharmacology of acute MDMA administration in healthy subjects. J Psychopharmacol. 2017 May;31(5):576-588. doi: 10.1177/0269881117691569[↩]
- Holland J, Weil A, Metzner R, et al: Ecstasy: The Complete Guide. Edited by Holland J. Rochester, Vermont, Park Street Press, 2001[↩]
- Rigg, Khary K., and Amanda Sharp. 2018. “Deaths Related to MDMA (Ecstasy/Molly): Prevalence, Root Causes, and Harm Reduction Interventions.” Journal of Substance Use 23 (4): 345–52. https://doi.org/10.1080/14659891.2018.1436607[↩]
- Palamar JJ, Salomone A, Massano M, Cleland CM. Trends in reported and biologically confirmed drug use among people who use ecstasy in the nightclub/festival-attending population, 2016-2022. Drug Alcohol Depend Rep. 2023 Nov 2;9:100198. doi: 10.1016/j.dadr.2023.100198[↩]
- Meamar R, Karamali F, Sadeghi HM, Etebari M, Nasr-Esfahani MH, Baharvand H. Toxicity of ecstasy (MDMA) towards embryonic stem cell-derived cardiac and neural cells. Toxicol In Vitro. 2010 Jun;24(4):1133-8. doi: 10.1016/j.tiv.2010.03.005[↩]
- Vorhees CV. Methods for detecting long-term CNS dysfunction after prenatal exposure to neurotoxins. Drug Chem Toxicol. 1997 Nov;20(4):387-99. doi: 10.3109/01480549709003895[↩]
- McElhatton PR, Bateman DN, Evans C, Pughe KR, Thomas SH. Congenital anomalies after prenatal ecstasy exposure. Lancet. 1999 Oct 23;354(9188):1441-2. doi: 10.1016/s0140-6736(99)02423-x[↩]
- Singer LT, Moore DG, Min MO, Goodwin J, Turner JJ, Fulton S, Parrott AC. Motor delays in MDMA (ecstasy) exposed infants persist to 2 years. Neurotoxicol Teratol. 2016 Mar-Apr;54:22-8. doi: 10.1016/j.ntt.2016.01.003[↩]
- Singer LT, Moore DG, Fulton S, Goodwin J, Turner JJ, Min MO, Parrott AC. Neurobehavioral outcomes of infants exposed to MDMA (Ecstasy) and other recreational drugs during pregnancy. Neurotoxicol Teratol. 2012 May-Jun;34(3):303-10. doi: 10.1016/j.ntt.2012.02.001[↩][↩]
- Parrott AC. The potential dangers of using MDMA for psychotherapy. J Psychoactive Drugs. 2014 Jan-Mar;46(1):37-43. doi: 10.1080/02791072.2014.873690[↩]