Contents
What is a bone cyst
Bone cyst is a fluid-filled hole that forms in bones. Bone cyst mainly affect children and teenagers. Bone cysts are not usually serious, but they sometimes need to be treated with surgery. However, a bone cyst may not need treatment if it’s small and not causing any problems. Bone cysts often get better on their own, especially in children and teenagers. You may have regular X-rays for a few years to check your bone is healing and the cyst isn’t getting bigger.
Bone cysts are inclusive of but not limited to:
- Unicameral bone cysts – fluid-filled holes that may form if fluid doesn’t drain properly from a bone as it’s growing. Grossly, unicameral bone cyst fluid appears clear yellow and serous unless there is a pathological fracture causing bleeding. Unicameral bone cyst fluid contains inflammatory mediators like prostaglandin, free radicals, interleukins, metalloproteins, and cytokines. The cyst wall lacks epithelial lining and forms from the fibrovascular stroma. Deep to this membrane lie fragments of immature bone, osteoclast giant cells, and mesenchymal cells. Fracture thickens the cyst wall with fibroblast, hemosiderin and reactive woven bone. Calcified cementum-like material in the cyst wall is found to be immature bone on immunohistochemistry 1.
- Aneurysmal bone cysts – blood-filled holes that may be caused by a problem with the blood vessels in a bone (possibly due to an injury or a non-cancerous growth). Aneurysmal bone cyst is a locally aggressive indeterminate tumor. Grossly aneurysmal bone cyst is blood filled cavitary lesion with septations surrounded by a thin layer of cortical bone. Microscopically, it shows hemorrhagic tissue with cavernous spaces and cellular stroma. Lining consists of compressed fibroblast and histiocytes. The fluid contains chronic inflammatory cells, prostaglandins, and giant cells. A solid variant of aneurysmal bone cyst, called giant cell reparative granuloma, is also known.
Unicameral bone cyst is a common lesion. Most commonly, these lesions occur during the second decade of life (approximately 85%), with a male to female ratio of 2 to 1 2.
Aneurysmal bone cyst is rarer, at 1.4 per 10000 population per year, and accounts for 9.1% of all bone tumors 3. There is a female preponderance, and 80% of these lesions occur in the second decade. Most occur in patients younger than 20 years. It is rare after 30 years of age.
A benign bone cyst which may be unicameral (single chamber) or septated 2.
Figure 1. Unicameral bone cyst
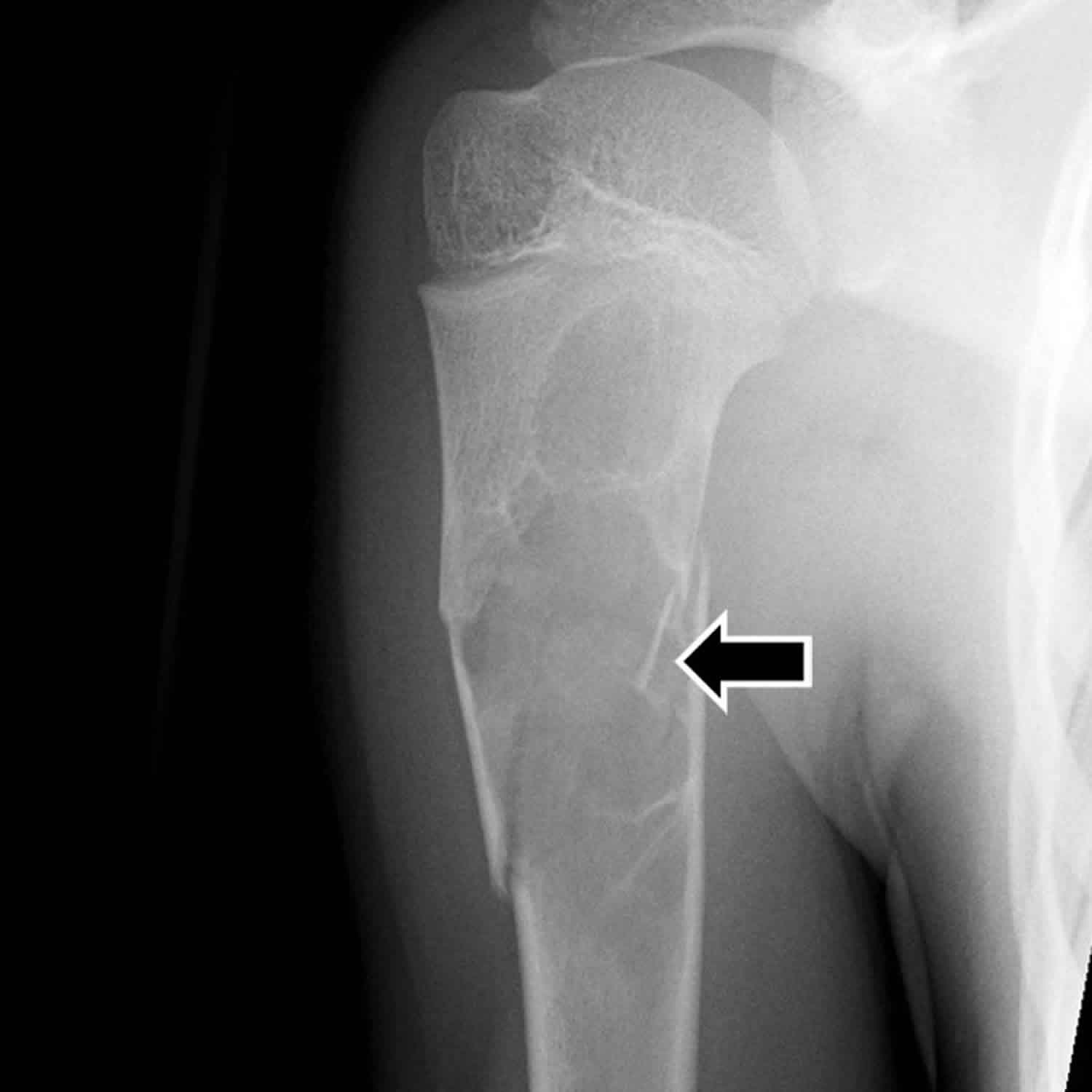
Figure 2. Aneurysmal bone cyst
Aneurysmal bone cyst
An aneurysmal bone cyst is a rare, locally destructive, blood-filled, benign cystic bone tumor. Aneurysmal bone cysts are made up of multiple blood-filled sacs that are packed together. Aneurysmal bone cysts can involve any bone, but the most common sites are the distal femur, proximal tibia, proximal humerus, and spine 2. Aneurysmal bone cysts tend to grow slowly. Most cases present with mild to moderate pain and swelling are common. The aneurysmal bone cyst may be present for a few weeks to a year before diagnosis. The rapid growth of aneurysmal bone cyst may mimic cancer. Spinal lesions may cause radicular pain or neurologic deficits. They often involve posterior elements of the vertebral bodies. Exceptionally, aneurysmal bone cyst can also arise in soft tissue.
Approximately 70% of primary aneurysmal bone cyst lesions are associated with recurrent chromosomal translocations causing gene fusions between ubiquitin specific peptidase 6 (USP6) and multiple genes 4. Secondary aneurysmal bone cyst has correlations with a plethora of benign and malignant primary bone lesions like chondroblastoma, osteosarcoma, simple bone cyst, giant cell tumor, and telangiectatic osteosarcoma. These secondary aneurysmal bone cyst lesions lack chromosomal translocations 5.
Aneurysmal bone cysts usually develop before people reach age 25, it involves the metaphysis of long bones (upper arm and thigh bones) in children and young adults and the cause is not known 6.
Aneurysmal bone cysts can show three different forms of evolutivity; quiescent, active, and aggressive. In some cases, aneurysmal bone cyst may undergo spontaneous resolution while in others they may become more aggressive mimicking fears of malignancy.
- Primary aneurysmal bone cyst: Comprising 70% of cases, aneurysmal bone cyst arises de-novo.
- Secondary aneurysmal bone cyst: In the other 30% of cases, aneurysmal bone cyst occurs in underlying bone tumors like giant cell tumor, simple bone cyst, chondroblastomas, osteoblastomas, fibrous dysplasia, nonossifying fibroma, and chondromyxoid fibromas 7.
The classification and staging of aneurysmal bone cyst are according to morphological characteristics and behavior of lesions.
Enneking staging for benign bone tumors according to the behavior of lesion 8:
- Inactive form: most benign, expansion is rare, minimal inflammation
- Active: Expansile lesion with cortical thinning, reactive bone formation, mild pain clinically
- Aggressive: Rapidly expansile, destructive, severely symptomatic
Capanna morphologic types of aneurysmal bone cyst 9:
- Type 1: Central well contained a metaphyseal lesion
- Type 2: Lesion involving an entire segment of bone with cortical expansion and thinning
- Type 3: Eccentric metaphyseal lesion with no or minimal cortical expansion
- Type 4: Subperiosteal reaction with no or minimal cortical erosion
- Type 5: Periosteum displaced with the erosion of cortex and extension into cancellous bone
Long bones and spine are mostly involved. Mild to moderate pain, present for weeks to months is the most common symptom which brings patients to the clinic 10. Spinal lesion presents with back pain, scoliosis or torticollis. Soft tissue swelling may be present. Sometimes the patient presents with a fracture.
To diagnose aneurysmal bone cysts, doctors usually do x-rays and magnetic resonance imaging (MRI). Doctors also remove a tissue sample for examination under a microscope (biopsy).
Surgical removal of the entire cyst is the most successful treatment, but sometimes the cysts return, particularly if they are not removed completely. Radiation should be avoided when possible because cancerous tumors occasionally develop later. However, radiation may be the treatment of choice for cysts that cannot be treated surgically and are putting pressure on the spinal cord.
Unicameral bone cyst
Unicameral bone cysts (simple bone cysts) can involve any bone of extremities, the most common site being proximal humerus and proximal femur 7. Unicameral bone cysts occur near the growth plates or physis in the arms or legs in children. Growth plates (physis) are what enable children to grow. As the years progress, it gradually grows away from the physis, and may remain as a static bone defect in diaphysis, or may resolve completely with time. In adults, the ilium and calcaneus are common locations. These lesions are most active during growth spurts and are known to heal spontaneously after bone maturity. Two-thirds of unicameral bone cysts present with a fracture. Unicameral bone cysts in flat bones are often asymptomatic unless detected incidentally on imaging.
Unicameral bone cysts often cause nearby bones to thin, which can lead to a break (fracture). Cysts that are less than 2 inches (about 5 centimeters) long or wide may heal and may disappear as the fracture heals. Cysts that are more than 2 inches long or wide, particularly in children, may require treatment.
Unicameral bone cyst seems to be a reactive bone lesion rather than a true bone tumor. Unicameral bone cyst forms secondary to venous stasis in cancellous bone. Bone resorption occurs secondary to venous stasis, a buildup of pressure and increased inflammatory mediators in cyst fluid 11. There are reports of a reduced partial pressure of oxygen in bone cyst as compared to arterial and venous blood which further supports the hypothesis of venous stasis 12.
Unicameral bone cyst is often asymptomatic. Incidentally detected unicameral bone cyst in the femur or humerus is common. On occasions, pain can arise due to spontaneous fracture through the cyst.
To diagnose unicameral bone cysts, doctors usually do x-rays. Most of the time, x-rays are enough to make the diagnosis, but sometimes other imaging tests, such as magnetic resonance imaging (MRI) or occasionally computed tomography (CT), are done.
Most often, unicameral bone cysts are treated with injections of corticosteroids (often repeatedly), with processed bone putty, or with synthetic bone substitutes. Sometimes treatment is surgery to remove the contents of the cyst from the bone by scraping it with a scoop-shaped instrument (curettage) and transplantation of bone from one site to another (bone grafting). Regardless of treatment, the cyst remains or returns in about 10 to 15% of people.
Bone cyst causes
The exact cause of bone cysts is unknown. Bone cysts are not cancer and don’t spread to other parts of your body.
Bone cyst symptoms
Bone cysts are often asymptomatic and found incidentally on radiographs 2. Sometimes, bone cysts may present with pain due to repeated bleeding into the cyst or pathological fracture.
Bone cyst complications
The following complications may accompany bone cysts 7:
- Pathological fracture: The main complication of simple bone cyst is a fracture. Pain, younger age of presentation, proximal humeral lesion, change in the size of a cavity with age, distance from growth plate, multiple septations, and early recurrence are signs of an active cyst and increased fracture risk
- Pain
- Malignant transformation is rare in unicameral bone cyst. Rare cases of malignancies have been reported several years after the treatment of aneurysmall bone cyst
- Arthritis
- Pressure symptoms
- Growth disorder: Limb length discrepancy or axial deviation may be induced in children if cysts transgress the physis or involve the epiphysis
- Recurrence: No treatment guarantees complete cure except for complete surgical resection – the post-treatment recurrence rate in case of unicameral bone cyst is about 10 to 30%; hence, the least aggressive treatment is the initial option
- Aggressive surgical treatment for femoral neck lesions has generally been advocated given the dreaded complications associated with pathological femur neck fractures (like avascular necrosis, residual coxa vara, etc.).
- General risks related to management of cysts: Unanticipated residual structural deformity and functional disability, and injury to adjacent vital structures (e.g., neurovascular) can occur
Bone cyst diagnosis
Physical examination shows tenderness, local swelling, and torticollis/scoliosis or neurological deficits in case of a spine bone cyst.
Unicameral bone cyst diagnosis
- Plain Radiograph: Well marginated, metaphyseal, juxtaepiphyseal, central cystic, purely lytic, moderately expansile lesion along the long axis of the long bone are usually diagnostic of unicameral bone cyst. The cyst never causes a cortical breach; prominent inner wall cortical ridges may give it the multiloculated appearance. There is no periosteal reaction. In case of fracture, there may be a small cortical fragment on the floor of cyst called a fallen fragment sign, which is considered pathognomonic of unicameral bone cyst with a fracture. unicameral bone cyst starts as a metaphyseal lesion, abutting the epiphysis in children. With time it moves into diaphysis. The lesion is considered as active when it is within 1 cm of the physis, and stable when closer to the diaphysis.
- CT scan: shows thick-walled cysts with pseudoseptations. It is useful in assessing the fracture risk of cysts and imaging of adjacent involved structures.
- MRI scan: shows T2 hyperintense cysts and gadolinium enhancement of cyst wall and septa.
- Cystography: is done to study venous drainage within the cyst.
Bone scintigraphy (bone scan) and positron emission tomography (PET scan) are inconclusive.
Aneurysmal bone cyst diagnosis
Suspect aneurysmal bone cyst on clinical examination and imaging:
- Imaging characteristics: Radiograph reveals an expansile lytic, eccentric metaphyseal lesion, that remains contained by a thin cortical wall. The cyst can be well-marginated or mildly permeative mimicking malignancy. A smooth periosteal reaction usually covers the cyst. Bone scan shows peripheral tracer uptake and a central area of decreased uptake called “doughnut sign.”
- CT and MRI scans further help in delineating cyst characteristics, soft tissue involvement, and aggressiveness of a tumor. CT is particularly useful in delineating cysts in areas like spine and pelvis. When differentiating unicameral bone cyst and aneurysmal bone cyst on MRI, the presence of the double density fluid and intralesional septations indicates aneurysmal bone cyst. Imaging further helps in planning surgical management.
Diagnosis: Biopsy should take place in all cases for confirmation 6. An optimal biopsy specimen is necessary for diagnosis. However, fine needle aspiration cytology is performed at some facilities by radiologists which are often inconclusive. Indication for biopsy is high clinical and radiological suspicion for aneurysmal bone cyst. Uncorrected coagulopathy disorders are relative contraindications.
Bone cyst treatment
A bone cyst might need to be treated if it’s:
- large or getting bigger – this could make the bone weaker and more likely to break (fracture) if you injure it
- causing problems like pain, swelling or a lump
The main treatments are:
- draining the fluid with a needle and injecting medicine into the bone to help it heal – this may need to be done several times over a few months
- cutting or scraping out the bone cyst – the hole may be filled with small pieces of bone taken from another part of your body or from someone who donated bone after they died
Treatment is done under general anesthetic. You won’t usually need to stay in hospital overnight.
Recovering after treatment
It normally takes at least a few months for the bone to heal.
You may need to avoid activities or sports that could damage the bone until it has healed.
You’ll have regular X-rays for a few years to check it’s getting better.
Unicameral bone cyst treatment
Nonoperative management is the choice for mild symptoms.
Small asymptomatic lesions in upper extremities are usually followed up with serial plain radiographs. Larger lesions at risk for fracture, symptomatic lesions, and lower extremity lesions typically receive treatment with curettage or aspiration and injection (corticosteroids, bone marrow aspirates, bone matrix, and other materials). Pathological fractures in the upper extremity generally have conservative treatment. The priority of therapy is to treat the fracture first, typically by immobilization for 4 to 6 weeks. However, unstable fracture or fracture in weight-bearing areas like in the lower extremity, treatment involves both fracture fixation and treatment of the bone cyst 13.
Treatment of all the other lesions is via non-aggressive options; techniques associated with preventive osteosynthesis. Injection of corticosteroid is one such option. The cyst is punctured with two needles and its contents aspirated with one needle, and radiological contrast is injected with the another, which is followed by injection with methylprednisone after emptying the contents. This also helps to differentiate from aneurysmal bone cyst. Cryptographic assessment showing the absence of venous drainage in the cyst rather than the presence of rapid venous outflow is a good prognostic indicator for treatment outcome with former showing better cyst healing 14. This technique works by either its antiprostaglandin effect or by decreasing intracystic pressure. It demonstrates a success rate of more than 90%.
Bone marrow aspirate and demineralized bone matrix injection avoids open bone curettage and grafting in 78% of cases with proximal humerus unicameral bone cyst, can be considered as an adjuvant to curettage 15.
Elastic stable intramedullary nailing in case of long bones of children has shown promising results for the treatment of unicameral bone cyst 16.
Current treatment concepts include a combination of decompressions, cyst wall disruption, injection with corticosteroid/demineralized bone matrix/bone marrow aspirate, and internal fixation in the weight-bearing region 17.
Diagnosis is either incidental or prompted by a fracture. In both scenarios, aneurysmal bone cyst and underlying malignancy must be ruled before further management.
Aneurysmal bone cyst treatment
Treatment goal for aneurysmal bone cyst is the eradication of disease, prevention of recurrence and reduction of pain/ functional impairment. Surgical curettage and bone grafting with or without adjuvant therapy was classically the primary mode of treatment. However need for wide resection, disability, cost of rehabilitation post surgery and the benign nature of cyst has prompted to look for less aggressive treatment options.
Several minimally invasive treatments have emerged as an alternative to curettage including sclerotherapy with polidocanol, selective embolization of feeding vessel to the cyst and medical therapy with denosumab. Radionuclide ablation is also an option 18. Preoperative embolizations also help to minimize surgical bleeding for lesions involving the spine and pelvis. When curettage is not possible due to difficult anatomy, arterial embolization can be an option. Low dose radiation can cause rapid ossification of the lesion. However, it is less popular due to the risk of malignant transformation. However, it is sometimes used in surgically inaccessible recurrent spinal tumors.
Percutaneous injection of calcitonin and steroids under CT guidance has shown positive results. Repeated recurrences or development of any suspicious findings on imaging necessitate a more aggressive treatment 19. Injection with an alcoholic solution of zein (corn protein), which possesses thrombogenic and fibrogenic properties, is a simple alternative; it makes open surgical treatment unnecessary by stopping the cyst growth and inducing new bone formation along the inner endosteal layer of the cyst 20. Absolute alcohol also shows comparable treatment efficacy with a low complication rate. It may require repeated injections.
Bone cyst prognosis
Unicameral bone cyst prognosis
Unicameral bone cyst develops in the metaphysis and gradually grows away from the physis and is known for spontaneous resolution, as evidenced by the fact that unicameral bone cyst is rare in adults.
Active cysts are those that are very near the growth plate while inactive cysts are those that have grown away from growth or not in direct contact with growth plate 21. High-risk areas are those which may lead to significant disability like femur neck cyst, which if fractured may lead to necrosis and limb length discrepancy. Asymptomatic lesions with low risk for pathological fractures/inactive cyst are usually left alone. Most children present with pain due to pathological fractures through cyst. Growth discrepancy due to cyst pressure into growth plates, as a complication of cyst treatment very near growth plate, or fracture through femoral neck cyst may occur. All these may cause limb length discrepancy and deformities. Hence, the appropriate treatment protocol is crucial for the management of cysts. Curettage and bone grafting with internal fixation are reserved for larger, symptomatic lesions in high-risk areas like the femur. Other lesions are treated with percutaneous injections as described above. Poor prognostic factors for recurrence following percutaneous treatment include large size, multilocation, active lesions, and age younger than 10 years.
Aneurysmal bone cyst prognosis
Recurrence rate after curettage of aneurysmal bone cyst is approximately 10 to 20%. Age younger than 15 years, central location, and incomplete removal of the cystic cavity are known risk factors for recurrence. Complete surgical resection is reserved for more dispensible bones like the clavicle and fibula, where partial bone excision does not cause any significant long term morbidity.
- Tariq MU, Din NU, Ahmad Z, Kayani N, Ahmed R. Cementum-like matrix in solitary bone cysts: a unique and characteristic but yet underrecognized feature of promising diagnostic utility. Ann Diagn Pathol. 2014 Feb;18(1):1-4[↩]
- Subramanian S, Viswanathan VK. Bone Cyst. [Updated 2019 Mar 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539849[↩][↩][↩][↩]
- Cottalorda J, Bourelle S. Current treatments of primary aneurysmal bone cysts. J Pediatr Orthop B. 2006 May;15(3):155-67[↩]
- Warren M, Xu D, Li X. Gene fusions PAFAH1B1-USP6 and RUNX2-USP6 in aneurysmal bone cysts identified by next generation sequencing. Cancer Genet. 2017 Apr;212-213:13-18[↩]
- Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, Neff JR, Demetri GD, Rosenberg AE, Bridge JA, Fletcher JA. Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes. Oncogene. 2005 May 12;24(21):3419-26[↩]
- Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg. 2012 Apr;20(4):233-41[↩][↩]
- Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015 Feb;101(1 Suppl):S119-27[↩][↩][↩]
- Enneking WF. A system of staging musculoskeletal neoplasms. Clin. Orthop. Relat. Res. 1986 Mar;(204):9-24.[↩]
- Capanna R, Bettelli G, Biagini R, Ruggieri P, Bertoni F, Campanacci M. Aneurysmal cysts of long bones. Ital J Orthop Traumatol. 1985 Dec;11(4):409-17[↩]
- Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: a review of 150 patients. J. Clin. Oncol. 2005 Sep 20;23(27):6756-62[↩]
- Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res. 2015 Feb;101(1 Suppl):S119-27.[↩]
- Chigira M, Maehara S, Arita S, Udagawa E. The aetiology and treatment of simple bone cysts. J Bone Joint Surg Br. 1983 Nov;65(5):633-7[↩]
- Wilke B, Houdek M, Rao RR, Caird MS, Larson AN, Milbrandt T. Treatment of Unicameral Bone Cysts of the Proximal Femur With Internal Fixation Lessens the Risk of Additional Surgery. Orthopedics. 2017 Sep 01;40(5):e862-e867[↩]
- Ramirez A, Abril JC, Touza A. Unicameral bone cyst: radiographic assessment of venous outflow by cystography as a prognostic index. J Pediatr Orthop B. 2012 Nov;21(6):489-94[↩]
- Gundle KR, Bhatt EM, Punt SE, Bompadre V, Conrad EU. Injection of Unicameral Bone Cysts with Bone Marrow Aspirate and Demineralized Bone Matrix Avoids Open Curettage and Bone Grafting in a Retrospective Cohort. Open Orthop J. 2017;11:486-492[↩]
- de Sanctis N, Andreacchio A. Elastic stable intramedullary nailing is the best treatment of unicameral bone cysts of the long bones in children?: Prospective long-term follow-up study. J Pediatr Orthop. 2006 Jul-Aug;26(4):520-5[↩]
- Donaldson S, Wright JG. Recent developments in treatment for simple bone cysts. Curr. Opin. Pediatr. 2011 Feb;23(1):73-7[↩]
- Tsagozis P, Brosjö O. Current Strategies for the Treatment of Aneurysmal Bone Cysts. Orthop Rev (Pavia). 2015 Dec 28;7(4):6182[↩]
- Chang CY, Kattapuram SV, Huang AJ, Simeone FJ, Torriani M, Bredella MA. Treatment of aneurysmal bone cysts by percutaneous CT-guided injection of calcitonin and steroid. Skeletal Radiol. 2017 Jan;46(1):35-40[↩]
- George HL, Unnikrishnan PN, Garg NK, Sampath JS, Bass A, Bruce CE. Long-term follow-up of Ethibloc injection in aneurysmal bone cysts. J Pediatr Orthop B. 2009 Nov;18(6):375-80.[↩]
- Norman A, Schiffman M. Simple bone cysts: factors of age dependency. Radiology. 1977 Sep;124(3):779-82.[↩]