Contents
Excess sleepiness
Excessive sleepiness also known as excessive daytime sleepiness, is defined by having an increased pressure to fall asleep during typical wake hours 1. Excessive Daytime Sleepiness is a common complaint of many adults and children. It is the most common symptoms of people with sleep disorders. Excessive Daytime Sleepiness is a leading cause of fatalities from motor vehicle accident. Sleep problems contribute to more than 100,000 motor vehicle incidents that result in 71,000 personal injuries and 1,500 deaths annually 2. According to the National Transportation Safety Board, up to 52 percent of single vehicle crashes involving heavy trucks are fatigue-related, with the driver falling asleep in 17.6 percent of cases 3. Most sleep-related crashes involve adolescent and young adult male drivers 4. Sleepy adolescents also have significantly lower levels of academic performance, increased school tardiness, and lower graduation rates than other students 5. Daytime sleepiness has been linked to poor health on several standardized measurements, including impairment in all domains of the Medical Outcomes Study short form health survey (36 items) 6. It has also been associated with compromised professional performance, including that of physicians and judges 7. Reduced cognitive function related to excessive daytime sleepiness can affect the ability to gain or maintain employment, because patients with excessive daytime sleepiness may be misperceived as lazy or unmotivated.
Excessive Daytime Sleepiness is one of the most common sleep-related symptoms and it affects an estimated 20 percent of adults in the United States 8. People who have excessive sleepiness feel drowsy and sluggish most days, and these symptoms often interfere with their work, school, activities, or relationships. Although patients with excessive daytime sleepiness often complain of “fatigue,” excessive sleepiness is different from fatigue which is characterized by low energy and the need to rest (not necessarily sleep). Excessive sleepiness is also different from depression, in which a person may have a reduced desire to do normal activities, even the ones they used to enjoy. Persons with excessive daytime sleepiness are at risk of motor vehicle and work-related incidents, and have poorer health than comparable adults 9. The prevalence of excessive daytime sleepiness is highest in adolescents, older persons, and shift workers 10, but assessment of its true prevalence is difficult because of the subjective nature of the symptoms, inconsistencies in terminology, and a lack of consensus on methods of diagnosis and assessment. Some persons use subjective terminology (e.g., drowsiness, languor, inertness, fatigue, sluggishness) when describing symptoms of excessive daytime sleepiness 11.
Excessive sleepiness is not a disorder in itself, it is a serious symptom that can have many different causes. If you feel excessively sleepy, you and your doctor should investigate it further. The most common causes of excessive daytime sleepiness are sleep deprivation or poor sleep habits, such as reduced opportunity for sleep or irregular sleep schedule, a sleep disorder like obstructive sleep apnea and side effects from certain medications (sedating medications). Other potential causes of excessive daytime sleepiness include certain medical and psychiatric conditions and sleep disorders, such as narcolepsy. Obstructive sleep apnea is a particularly significant cause of excessive daytime sleepiness. An estimated 26 to 32 percent of adults are at risk of or have obstructive sleep apnea, and the prevalence is expected to increase. The evaluation and management of excessive daytime sleepiness is based on the identification and treatment of underlying conditions (particularly obstructive sleep apnea), and the appropriate use of activating medications.
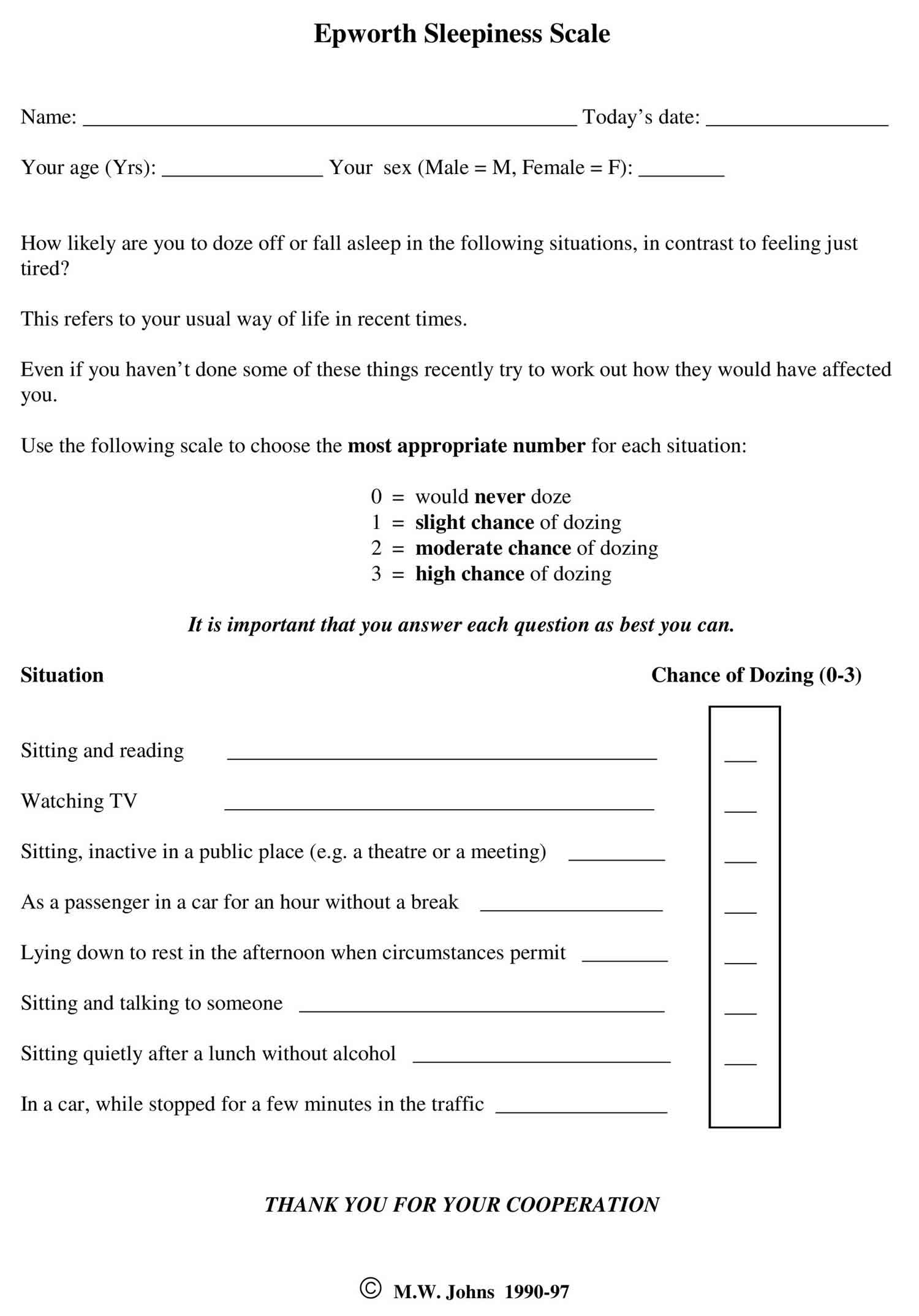
There are several questionnaires available to assess excessive daytime sleepiness. One of the most popular questionnaires is the Epworth Sleepiness Scale (see Figure 1 below). This scale uses eight questions composed of eight scenarios. The user rates the likelihood of falling asleep from 0 -3 points per scenario. The total is tallied up to a highest sleepiness score of 24. Once you and your doctor have determined the cause of excessive sleepiness, you can create a treatment plan together. For most people, that involves changing sleep habits and improving behaviors and elements of the sleep environment. For others, further medical tests or sleep studies may be indicated.
If you are frequently tired, work less productively, make mistakes, have lapses in judgment or wakefulness, or feel unable to enjoy or fully participate in life’s activities, don’t just “push through.” If you’ve been excessively tired for a long time, it may feel normal to you, but poor sleep and resulting excessive sleepiness can have drastic, long-term effects on your health (for example reduced sleep is tied to cardiovascular problems and weight gain), as well as how you think and feel. Not only that, when you go about your day overtired, you put yourself and others at risk, since motor vehicle accidents and other dangerous errors are often caused by sleepiness. If you’re feeling the symptom of excessive sleepiness, talk to your doctor so the two of you can take a closer look at your sleep habits and take steps to improve your health, and ultimately get you on the road to sleeping and feeling better.
Epworth sleepiness scale
Epworth Sleepiness Scale (ESS) is a scale intended to measure ‘daytime sleepiness’ that is measured by use of a very short questionnaire. This can be helpful in diagnosing sleep disorders. Epworth Sleepiness Scale was introduced in 1991 by Dr Murray Johns of Epworth Hospital in Melbourne, Australia and subsequently modified it slightly in 1997.
Epworth Sleepiness Scale is a self-administered questionnaire with 8 questions. The questionnaire asks the subject to rate his or her probability of falling asleep on a scale of increasing probability from 0 to 3 (0 = no chance of dozing 1 = slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing) for eight different situations that most people engage in during their daily lives, though not necessarily every day. The scores for the eight questions are added together to obtain a single number. A number in the 0–9 range is considered to be normal while a number in the 10–24 range indicates that expert medical advice should be sought. For instance, scores of 11-15 are shown to indicate the possibility of mild to moderate sleep apnea, where a score of 16 and above indicates the possibility of severe sleep apnea or narcolepsy. Certain questions in the scale were shown to be better predictors of specific sleep disorders, though further tests may be required to provide an accurate diagnosis.
Figure 1. Epworth Sleepiness Scale (ESS)
Epworth Sleepiness Scale score
Epworth Sleepiness Scale is a scale intended to measure daytime sleepiness that is measured by use of a very short questionnaire. Epworth Sleepiness Scale can be helpful in diagnosing sleep disorders.
Sitting and reading
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Watching television
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Sitting, inactive in a public place (e.g. a theater or meeting)
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
As a passenger in a car for an hour without a break
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Lying down to rest in the afternoon when circumstances permit
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Sitting and talking to someone
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Sitting quietly after a lunch without alcohol
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
In a car, while stopped for a few minutes in the traffic
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Add up all the scores and write in the designated “total score box”.
Interpret the results as per the scale below.
- Score: 1- 6 = Enough Sleep
- Score: 7-8 = Tend to be sleepy during the day
- Score: 9- 15 = Very sleepy
- Score: 16+ = Dangerously sleepy
Your Score is less than 9 and in considered normal
Your Score is above 9 and its recommended that you should seek medical advice.
Epworth Sleepiness Scale interpretation
Epworth Sleepiness Scale is a self-administered questionnaire with 8 questions. Respondents are asked to rate, on a 0-3 scale (0 = no chance of dozing 1 = slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing), their usual chances of dozing off or falling asleep while engaged in eight different activities. Most people engage in those activities at least occasionally, although not necessarily every day. The Epworth Sleepiness Scale score (the sum of 8 item scores, 0-3) can range from 0 to 24. The higher the Epworth Sleepiness Scale score, the higher that person’s average sleep propensity in daily life, or their ‘daytime sleepiness’. A number in the 0–9 range is considered to be normal while a number in the 10–24 range indicates that expert medical advice should be sought. For instance, scores of 11-15 are shown to indicate the possibility of mild to moderate sleep apnea, where a score of 16 and above indicates the possibility of severe sleep apnea or narcolepsy. Certain questions in the Epworth Sleepiness Scale were shown to be better predictors of specific sleep disorders, though further tests may be required to provide an accurate diagnosis.
Sleep Stages
Sleep occurs in 2 main phases, Non-Rapid Eye Movement (NREM) sleep, which has three stages (N1, N2, and N3), and Rapid Eye Movement (REM) sleep 12. Each sleep phase and stage of sleep includes variations in muscle tone, brain wave patterns, and eye movements. Your body cycles through all stages approximately 4 to 6 times each night, averaging 90 minutes for each cycle 13. Each sleep stage serves different functions, from the light transition into sleep (N1), to the restorative deep sleep (N3) and the active dreaming of REM sleep.
- Stage 1 (N1 or light sleep) is the lightest stage of sleep and occurs as a person first falls asleep. This brief stage is when your drowsiness gives way to falling asleep. Your heartbeat and breathing start to slow down, but it’s still pretty easy to wake you up during this stage. Average length 1 to 7 minutes.
- Stage 2 (N2 or intermediate sleep) is where the body starts to relax more deeply. Your body temperature drops, your muscles relax, and your breathing and heart rate slow even more. Average length 10 to 25 minutes.
- Stage 3 (N3 or deep sleep) is the deepest and more restorative sleep, allowing your body to recover and grow. In stage 3 sleep, your breathing and pulse are slow and steady. Average length 20 to 40 minutes.
- Stage 4 (REM Sleep) is where most dreaming occurs, brain activity increases almost as if you were awake, and your muscles become temporarily paralyzed. Your heart rate and respiration speed up and become more erratic, and your eyes move quickly behind your eyelids. Dreams are most vivid during the REM stage. Average length 10 to 60 minutes.
Although the sleep stages are described numerically, you don’t always progress through them in this exact order. For example, in many sleep cycles, you transition from stage 3 sleep back to stage 2 sleep before beginning a period of REM sleep.
Sleep occurs in 5 stages: Wake, Non-Rapid Eye Movement (NREM) stage N1, then progress through N2 and N3, and after N3 you enter REM sleep 12. You then return to NREM stages, often starting again at N2. Throughout the night, the REM periods lengthen, and deep N3 sleep decreases, with most N3 sleep occurring in the first half of the night, with each stage leading to progressively deeper sleep. Approximately 75% of sleep is spent in the NREM (Non-Rapid Eye Movement) stages, with the majority spent in the N2 stage 16. A typical night’s sleep consists of 4 to 5 sleep cycles, with the progression of sleep stages in the following order: N1, N2, N3, N2, REM 17. A complete sleep cycle takes roughly 90 to 120 minutes. The first REM period is short, and as the night progresses, longer periods of REM and decreased time in deep sleep (NREM) occur 12. With each new cycle, you spend increasing amounts of time in REM sleep, so most of your REM sleep takes place in the second half of the night.
Sleep isn’t uniform. Sleep cycles can vary from person to person and from night to night based on a wide range of factors such as your age, recent sleep patterns, and alcohol consumption. Over the course of the night, you go through several rounds of the sleep cycle, which is composed of four stages. In a typical night, a person goes through four to six sleep cycles 12. Not all sleep cycles are the same length, but on average they last about 90 minutes each.
The first sleep cycle is often the shortest, ranging from 70 to 100 minutes, while later cycles tend to fall between 90 and 120 minutes. In addition, the composition of each cycle — how much time is spent in each phase of sleep — changes as the night goes along.
Figure 2. Sleep Stages
Footnotes: A sleep episode begins with a short period of NREM stage N1 progressing through stage N2, followed by stage N3 and finally to REM. However, individuals do not remain in REM sleep the remainder of the night but, rather, cycle between stages of NREM and REM throughout the night. NREM sleep constitutes about 75 to 80 percent of total time spent in sleep, and REM sleep constitutes the remaining 20 to 25 percent. The average length of the first NREM-REM sleep cycle is 70 to 100 minutes. The second, and later, cycles are longer lasting—approximately 90 to 120 minutes 18. In normal adults, REM sleep increases as the night progresses and is longest in the last one-third of the sleep episode. As the sleep episode progresses, stage 2 begins to account for the majority of NREM sleep, and stages 3 and 4 may sometimes altogether disappear.
[Source 14 ]Figure 3. Typical Sleep Pattern in Young Adults
Footnotes: Average times and sequences of sleep cycles during the night. Over the course of a period of sleep, NREM and REM sleep alternate cyclically. The function of alternations between these two types of sleep is not yet understood, but irregular cycling and/or absent sleep stages are associated with sleep disorders 19. For example, instead of entering sleep through NREM, as is typical, individuals with narcolepsy enter sleep directly into REM sleep 20. Rapid eye movement (REM) sleep occurs cyclically throughout the night every 90 to 120 minute. Brief periods of wakefulness (stage W) occur periodically. Sleep time is spent as follows:
- Stage N1: 2–5%
- Stage N2: 45–55%
- Stage N3: 13–23%
- REM: 20–25%
Figure 4. EEG activity of the four stages of sleep
Footnotes: EEG activity during wakefulness with eyes open and closed and during the different stages of sleep. Brainwave activity changes drastically over the course of the different stages of sleep. REM sleep brain activity most closely resembles brain activity while awake.
- Alpha activity is a smooth electrical activity of 8-12 Hz recorded from the brain; generally associated with a state of relaxation during wakefulness.
- Beta activity is a irregular electrical activity of 13-30 Hz recorded from the brain; generally associated with a state of alertness during wakefulness.
- Theta activity is EEG activity of 3.5-7.5 Hz that occurs intermittently during lighter stages of NREM sleep.
- Delta activity is a regular, synchronous electrical activity of less than 4 Hz recorded from the brain; occurs during the deepest stages of slow-wave sleep.
- Sleep spindle is a short burst of 12 to 14 cycle per-second waves observed during NREM sleep, decrease brain’s sensitivity to sensory input and keeps person asleep.
- K complex are single delta waves, sudden sharp wave forms, 1 per minute but can be triggered by noise.
Your sleep-wake cycle is regulated by the circadian rhythm (your body’s natural internal 24-hour clock that manages your sleep-wake cycle and other vital functions, like hormone release and body temperature, by synchronizing with the day-night cycle), which is driven by the suprachiasmatic nucleus (SCN) of the hypothalamus that acts as a “master clock” or “circadian pacemaker”, receiving light cues from your eyes to control the circadian rhythm 23, 24, 25. The circadian rhythm also controls the nocturnal release of adrenocorticotropic hormone (ACTH), prolactin, melatonin, and norepinephrine (NE) 26. External factors like light exposure, meal timing, and activity can influence the circadian rhythm, and disruptions to the circadian rhythm, such as from shift work or jet lag, can negatively affect your health.
The suprachiasmatic nucleus (SCN) of the hypothalamus receives input from nerve cells in the retina that detect light to regulate the circadian rhythm and sleep via multiple pathways that cause the nocturnal release of adrenocorticotropic hormone (ACTH), prolactin, melatonin, and norepinephrine 27. One of the most commonly recognized pathways by which this occurs is via the stimulation of norepinephrine release by the suprachiasmatic nucleus (SCN), which in turn stimulates the pineal gland to release melatonin 28, 25. Wakefulness is maintained by subcortical structures and pathways activating the cortical system 28. This system is termed the “ascending arousal system” and utilizes several major neurochemicals, including:
- Norepinephrine (locus ceruleus)
- Serotonin (midline raphe nuclei)
- Histamine (tuberomammillary nucleus)
- Dopamine (ventral periaqueductal gray matter)
- Acetylcholine (pedunculopontine tegmentum and laterodorsal tegmentum of the pons)
- Orexin (perifornical area)
Transitions between sleep and wake states are influenced by multiple brain structures, including 12:
- Hypothalamus: controls onset of sleep
- Hippocampus: memory region active during dreaming
- Amygdala: emotion center active during dreaming
- Thalamus: prevents sensory signals from reaching the cortex
- Reticular formation: regulates the transition between sleep and wakefulness
- Pons: helps initiate REM sleep. The extraocular movements (eye movements) that occur during REM sleep are due to the activity of PPRF (paramedian pontine reticular formation/conjugate gaze center).
Although it is apparent that humans need sleep, the current understanding of why sleep is an essential part of life is still yet to be determined 12. The current hypotheses on the function of sleep include 29:
- Neural maturation
- Facilitation of learning or memory
- Targeted erasure of synapses to “forget” unimportant information that might clutter the synaptic network
- Cognition
- Clearance of metabolic waste products generated by neural activity in the awake brain
- Conservation of metabolic energy.
Wake or Alert Stage
The first stage is the wake stage or stage W, which further depends on whether your eyes are open or closed. During wakefulness, the EEG is characterized by waves of low amplitude and high frequency. This kind of EEG pattern is known as low-voltage fast activity or activated. During eye-open wakefulness, beta waves predominate. Alpha waves (8–13 Hz) become the predominant pattern as you become drowsy and close your eyes, particularly in occipital regions 30. The Electromyography (EMG, a test that measures the electrical activity of muscles) reveals tonic muscle activity with additional phasic activity related to voluntary movements.
EEG recording: beta waves – highest frequency, lowest amplitude (alpha waves are seen during quiet/relaxed wakefulness)
Non-Rapid Eye Movement (NREM) Sleep Stages
- Stage N1 (Light Sleep): This is the transition between wakefulness and sleep, characterized by slowing heart rate and breathing.
- Stage N2 (Intermediate Sleep): Your heart rate and body temperature decrease further, and your body relaxes.
- Stage N3 (Deep Sleep): This is the deepest stage of Non-Rapid Eye Movement (NREM) sleep, when your body performs restorative work, and it is crucial for feeling rested.
Stage 1 or N1 Sleep
NREM Stage 1 (N1) or Light Sleep serves a transitional role in sleep-stage cycling. This is the lightest stage of sleep and begins when more than 50% of the alpha waves are replaced with low-amplitude mixed-frequency (LAMF) activity. Muscle tone is present in the skeletal muscle, and breathing occurs regularly. This stage lasts around 1 to 7 minutes in the initial cycle, comprising 5% of total sleep time and is easily interrupted by a disruptive noise.
Brain activity on the EEG in stage 1 transitions from wakefulness (marked by rhythmic alpha waves) to low-voltage, mixed-frequency waves. Alpha waves are associated with a wakeful relaxation state and are characterized by a frequency of 8 to 13 cycles per second 20.
EEG recording: Theta waves – low voltage.
Stage 2 or N2 Sleep
NREM Stage 2 (N2) represents deeper sleep as the heart rate and body temperature drop 12. The presence of sleep spindles, K-complexes, or both characterizes it 12. Sleep spindles are brief, powerful bursts of neuronal firing in the superior temporal gyri, anterior cingulate, insular cortices, and thalamus, inducing calcium influx into cortical pyramidal cells. This mechanism is believed to be integral to synaptic plasticity. Numerous studies suggest that sleep spindles are essential in memory consolidation, specifically procedural and declarative memory 31. Individuals who learn a new task have a significantly higher density of sleep spindles than those in a control group 32.
K-complexes are long delta waves that last approximately one second and are known to be the longest and most distinct of all brain waves. K-complexes are shown to function in maintaining sleep and memory consolidation 33.
Stage 2 sleep lasts approximately 10 to 25 minutes in the initial cycle and lengthens with each successive cycle, eventually constituting between 45 to 55 percent of the total sleep episode. Stage 2 sleep is when bruxism (teeth grinding) occurs. An individual in stage 2 sleep requires more intense stimuli than in stage 1 to awaken. Brain activity on an EEG shows relatively low-voltage, mixed-frequency activity characterized by the presence of sleep spindles and K-complexes.
EEG recording: Sleep spindles and K complexes.
Stage 3 or N3 Sleep (Deepest Non-REM Sleep)
Sleep stage 3 or N3 sleep is also known as slow-wave sleep (SWS). This is considered the deepest stage of sleep and is characterized by signals with lower frequencies and higher amplitudes, known as delta waves 12. Sleep stage 3 or N3 sleep is the most difficult to awaken from; for some people, loud noises (> 100 decibels) will not lead to an awake state 12. As people age, they spend less time in this slow, delta-wave sleep and more time in stage N2 sleep 12. Although this stage has the greatest arousal threshold, if someone is awoken during this stage, they will have a transient phase of mental fogginess, known as sleep inertia 12. Cognitive testing shows that individuals awakened during this stage tend to have moderately impaired mental performance for 30 minutes to 1 hour 34. Sleep stage 3 or N3 sleep stage is when the body repairs and regrows tissues, builds bone and muscle, and strengthens the immune system. Sleep stage 3 or N3 sleep is also the stage when sleepwalking, night terrors, and bedwetting occur 35.
Sleep stage 3 or N3 sleep lasts only a few minutes and constitutes about 3 to 8 percent of sleep. The EEG shows increased high-voltage, slow-wave activity.
EEG recording: Delta waves – lowest frequency, highest amplitude.
Rapid Eye Movement (REM) Sleep Stage
Rapid eye movement sleep or REM sleep is the fourth and final stage of sleep and is when you have your most vivid and intense dreams. During REM sleep your brain activity increases to near-waking levels, your eyes dart quickly under your eyelids with fluctuating in your breathing and heart rate and most vivid dreams occur in this phase of sleep. Your muscles become limp (atonia) to prevent you from acting out your dreams. EEG recording shows beta waves – similar to brain waves during wakefulness. You experience your first period of REM sleep about 60 to 90 minutes after falling asleep 27.
REM sleep is defined by the presence of desynchronized (low-voltage, mixed-frequency) brain wave activity, muscle atonia, and bursts of rapid eye movements 20. “Sawtooth” wave forms, theta activity (3 to 7 counts per second), and slow alpha activity also characterize REM sleep 18. During the initial cycle, the REM period may last only 1 to 5 minutes; however, it becomes progressively prolonged as the sleep episode progresses 18.
Most adults need about 2 hours of REM sleep each night, which contributes to brain development, brain function, memory consolidation, and emotional health 36, 37.
Infants and children need more REM sleep, because their brains are still rapidly developing. For example, newborn babies spend around eight hours in REM sleep each day.
How much time you actually spend in REM sleep can vary from night to night. On a night when you’re short of sleep, your total REM time can get cut short. This can trigger your brain to initiate more REM sleep the following night, which is known as a REM rebound 38. Some research also suggests that REM sleep may increase after learning new information 39.
Because REM sleep enables better brain function, memory, and emotional regulation, a lack of REM sleep can cause a range of issues. On top of that, a lack of REM sleep circumvents healthy sleep overall, contributing to sleep deprivation. In the short term, signs of sleep deprivation can include 40:
- Difficulty concentrating
- Excessive daytime sleepiness
- Forgetfulness or poor memory
- Irritability or frustration
- Greater risk of accidents
Over the long term, insufficient sleep can weaken your immune system and raise your risk of conditions like heart disease, diabetes, depression, and anxiety.
How Much Deep Sleep Do I Need?
Different people need different amounts of sleep. Most adults need 7 to 8 hours of sleep a night for good health and mental functioning. Some adults need up to 9 hours a night 41. During a healthy night’s sleep for most adults, deep sleep (stage 3 or N3 sleep) makes up between 10% and 20% of total sleeping time 42. People who sleep less than approximately 7 hours a night are at a greater risk for heart disease, stroke, asthma, arthritis, depression, and diabetes. Nearly 20% of all car crashes, both fatal and nonfatal, are attributed to drowsy driving. Without enough sleep, your brain may struggle to perform basic functions. You may find it hard to concentrate or remember things. You may become moody and lash out at co-workers or people you love.
If you’re not sure about how much sleep you really need, you can use an online Sleep Calculator (https://www.sleepfoundation.org/sleep-calculator). However, your doctor is in the best position to make a detailed sleep recommendation for you based on your age, your overall health and your unique situation.
Table 1. Recommended Sleep Duration
| Age Range | Recommended Daily Sleep | |
|---|---|---|
| Infant | 4–12 months | 12-16 hours (including naps) |
| Toddler | 1–2 years | 11-14 hours (including naps) |
| Preschool | 3–5 years | 10-13 hours (including naps) |
| School-age | 6-12 years | 9-12 hours |
| Teens | 13-18 years | 8-10 hours |
| Adults | 18 years and older | 7 or more hours |
Just as your brain needs sleep to restore itself, so does your body. When you do not have enough sleep, your risk goes up for several illnesses.
- Diabetes. Your body does not do as well controlling blood sugar when you do not get enough sleep.
- Heart disease. Lack of sleep can lead to high blood pressure and inflammation, two things that can damage your heart.
- Obesity. When you do not get enough rest from sleep, you are more prone to overeat. It is also harder to resist foods high in sugar and fat.
- Infection. Your immune system needs you to sleep so it can fight colds and keep you healthy.
- Mental health. Depression and anxiety often make it hard to sleep. They also can become worse after a string of sleepless nights.
The cancer research branch of the World Health Organization has determined that disruption of regular sleep is “probably carcinogenic to humans”, putting it in the same risk category as the infectious agents malaria and human papillomavirus (HPV), as well as the biochemical weapon mustard gas. Sexual health is affected by sleep deprivation as well, as men with the worst sleeping habits have significantly lower sperm counts, decreased circulating testosterone, and even testicular shrinkage.
Adults generally need about 1.5 to 2 hours of deep sleep per night, which equates to roughly 13-23% of their total recommended sleep time. This stage of sleep is crucial for physical recovery, immune function, and cognitive health, so ensure you are getting sufficient overall sleep and practicing healthy sleep habits to obtain enough deep sleep
Why Deep Sleep is Important?
While all stages of sleep are necessary for good health, deep sleep is important because it is when your body undergoes essential physical restoration, immune system strengthening, and hormone production, while your brain processes and stores memories, consolidates learning, and clears waste products 15. During deep sleep, your body works to build and repair tissue, muscles, and bones, including by producing high levels of growth hormone 44. Achieving sufficient deep sleep helps you wake feeling refreshed, promotes long-term physical and mental health, and supports healthy weight and cardiovascular function 15. Deep sleep also promotes immune system functioning. Research suggests that it helps you build stronger immune responses and reduce unwanted chronic inflammation 45.
Slow-wave sleep also helps regulate blood sugar levels. As a result, the risk of developing type 2 diabetes may be higher if you don’t get enough deep sleep 46. And a shortage of deep sleep has also been linked to high blood pressure 47.
Deep sleep is important for cognitive function and memory. Although brain activity slows during deep sleep, this may actually facilitate learning by keeping the brain from becoming oversaturated with information. Evidence suggests that deep sleep also helps eliminate waste material from the brain, which may help protect against dementia 48.
Because deep sleep is an essential component of your nightly rest, a shortage of deep sleep contributes to broader impacts of sleep deprivation. In addition to causing tiredness, a shortage of deep sleep can cause general symptoms of sleep deprivation, including 49:
- Reduced alertness and attention
- Trouble learning and remembering things
- Irritability
- Symptoms of depression or anxiety
- Increased likelihood of accidents and injuries
On top of these immediate effects, a chronic lack of quality sleep can increase the likelihood of multiple health problems, such as:
- Infections and reduced immune system function
- Obesity
- Type 2 diabetes
- Cardiovascular problems, including high blood pressure, stroke, and heart disease
- Kidney disease
If you want to get more deep sleep, focus on enhancing your overall sleep. If your sleep quality and quantity are good, it usually means you’re getting plenty of restorative deep sleep. You get the most deep sleep during the early part of the night.
One of the most reliable ways to improve your sleep is by practicing good sleep hygiene. Good habits include 50:
- Establishing a consistent bedtime and wake-up time
- Ensuring you have a quiet, cool, and dark sleep environment
- Creating a relaxing bedtime routine to wind down in the evening
- Reducing caffeine intake in the afternoon and evening
- Limiting use of mobile devices, tablets, laptops, and other screens for 30 minutes or more before bedtime
There are some additional steps you can try to encourage more deep sleep:
- Take a warm bath: Some research suggests that heating your body with a warm bath before bedtime may induce more slow-wave sleep 51. A warm bath raises body temperature, which promotes blood circulation, and the subsequent cooling may help ease the transition to sleep.
- Change your diet: What you eat and drink before bedtime impacts your sleep. One small study found that people eating a diet high in saturated fats obtained less slow-wave sleep 52. People who ate more fiber were more likely to have increased amounts of deep sleep.
- Listen to binaural beats: Binaural beats are created by listening to two slightly different tones, one in each ear. The difference between the frequencies of those tones creates a perceived third tone, or binaural beat. Limited research suggests that listening to certain binaural beats may contribute to more stage 3 sleep 53.
Excessive daytime sleepiness causes
Excessive daytime sleepiness can occur secondary to sleep deprivation, medication effects, illicit substance use, obstructive sleep apnea (OSA), and other medical and psychiatric conditions 54. Excessive sleepiness caused by a primary hypersomnia of central origin (e.g., narcolepsy, idiopathic hypersomnia) is less common.
Common causes of excessive daytime sleepiness:
- Primary hypersomnias of central origin
- Narcolepsy (0.02 to 0.18 percent of population)
- Idiopathic hypersomnia (10 percent of patients with suspected narcolepsy)
- Other rare primary hypersomnias (example: Kleine-Levin syndrome)
- Secondary hypersomnias
- Sleep disorders
- Sleep-related breathing disorders
- Excessive daytime sleepiness secondary to obstructive sleep apnea (general population prevalence is 2 percent of women and 4 percent of men)
- Behavioral sleep deprivation
- Especially common in adolescents and shift workers
- Other sleep disorders: Includes circadian rhythm sleep disorders, sleep-related movement disorders
- Sleep disorders
- Medical or psychiatric conditions
- Medication effects: Includes prescription, nonprescription, and drugs of abuse
- Psychiatric conditions: Especially depression
- Medical conditions: Includes head trauma, stroke, cancer, inflammatory conditions, encephalitis, neurodegenerative conditions
Hypersomnia due to secondary causes is much more common than primary hypersomnia 54.
Sleep deprivation
Sleep deprivation is probably the most common cause of excessive daytime sleepiness. Symptoms can occur in healthy persons after even mild sleep restriction. Studies that restricted healthy adults to six hours of sleep per night for 14 successive nights showed a cumulative significant impairment of neurobiological functions 55. Symptoms of sleep deprivation can occur after only one night of sleep loss 55 and persons who are chronically sleep deprived are often unaware of their increasing cognitive and performance deficits 6. Paradoxically, most types of chronic insomnia (including primary insomnia, psychopathological insomnia, and paradoxical insomnia) are associated with daytime hyperarousal rather than excessive daytime sleepiness. The presence of excessive daytime sleepiness in a patient with insomnia suggests a comorbidity such as a sleep-related breathing disorder or a mood disorder 56.
Medication and drug side effects
Sleepiness is the most commonly reported side effect of pharmacologic agents that act on the central nervous system. The modulation of sleep and wakefulness is a complex process involving multiple factors and systems. Although no single chemical neurotransmitter has been identified as necessary or sufficient in the control of sleep, most drugs with clinical sedative or hypnotic actions affect one or more of the central neurotransmitters implicated in the neuromodulation of sleep and wakefulness, including dopamine, epinephrine, norepinephrine, acetylcholine, serotonin, histamine, glutamate, γ-aminobutyric acid, and adenosine 57.
Ethanol is the most widely used agent with sedative effects 58. Nonprescription sleeping pills and other medications containing sedating H1 antihistamines, such as diphenhydramine (Benadryl), hydroxyzine (Atarax, brand no longer available in the United States), or triprolidine (Zymine) are also commonly used. Sedating antihistamines, longer-acting benzodiazepines, and sedating antidepressants are associated with decreased performance on driving tests and increased rates of next-day motor vehicle incidents attributed to daytime sleepiness 56. Of the antihypertensive medications in widespread use, tiredness, fatigue, and daytime sleepiness are side effects commonly associated with beta blockers such as propranolol (Inderal), but sedation is also the most common side effect reported for the alpha2-agonists clonidine (Catapres) and methyldopa (Aldomet, brand no longer available in the United States). Sedation is also commonly reported by patients taking anticonvulsant or antipsychotic medications. Among drugs of abuse, marijuana has significant sedating effects. Adolescents abusing stimulants such as amphetamines and cocaine may experience persistent daytime sedation after long episodes of drug-induced wakefulness.
Medication classes commonly associated with daytime sleepiness 57:
- Alpha-adrenergic blocking agents
- Anticonvulsants (e.g., hydantoins, succinimides)
- Antidepressants (monoamine oxidase inhibitors, tricyclics, selective serotonin reuptake inhibitors)
- Antidiarrhea agents
- Antiemetics
- Antihistamines
- Antimuscarinics and antispasmodics
- Antiparkinsonian agents
- Antipsychotics
- Antitussives
- Barbiturates
- Benzodiazepines, other gamma-aminobutyric acid affecting agents, and other anxiolytics
- Beta-adrenergic blocking agents
- Genitourinary smooth muscle relaxants
- Opiate agonists and partial opiate agonists
- Skeletal muscle relaxants
Obstructive sleep apnea
Excessive daytime sleepiness is the most common symptom of obstructive sleep apnea. A sleep disorder caused by blockage of the upper airway, obstructive sleep apnea results in episodes of cessation of breathing (apneas) or a reduction in airflow (hypopneas), and is defined as greater than or equal to five apneic or hypopneic episodes per hour of sleep. These events induce recurrent hypoxia and repetitive arousals from sleep. For adults 30 to 60 years of age, the prevalence of obstructive sleep apnea has been estimated to be 9 percent for women and 24 percent for men. In patients with obstructive sleep apnea, approximately 23 percent of women and 16 percent of men experience excessive daytime sleepiness 59. Sleep-related breathing disorders may be significantly under-recognized as causes of excessive daytime sleepiness. One study estimated that 93 percent of women and 82 percent of men with moderate to severe obstructive sleep apnea are undiagnosed 60. Furthermore, 26 to 32 percent of U.S. adults are at risk of developing or currently have obstructive sleep apnea. Because increasing age and obesity are significant risk factors for obstructive sleep apnea, the prevalence of obstructive sleep apnea is set to increase rapidly. By 2025, obesity will affect 18% of men and over 21% of women worldwide, and that severe obesity will affect 6% of all men and 9% of all women around the world. In some nations, obesity is already present in more than one-third of the adult population and contributes significantly to overall poor health and high annual medical costs 61.
Persons with obstructive sleep apnea have an increased risk of motor vehicle incidents because of their impaired vigilance 60. In 2000, more than 800,000 drivers in the United States were involved in obstructive sleep apnea-related motor vehicle collisions, resulting in 1,400 deaths 62. Approximately 25 percent of persons with untreated obstructive sleep apnea report frequently falling asleep while driving 63. Because of associated daytime sleepiness, reduced vigilance, and inattention, persons with obstructive sleep apnea may have work performance difficulties and are at a high risk of being involved in occupational incidents 64.
Other secondary hypersomnias
Many medical conditions can cause secondary excessive daytime sleepiness, including head trauma, stroke, tumors, inflammatory conditions, encephalitis, and genetic and neurodegenerative diseases. Psychiatric conditions, especially depression, can also result in excessive daytime sleepiness. Sleep disorders such as circadian rhythm disorders (e.g., jet lag, shift work disorder), periodic limb movement disorder, and restless legs syndrome can also contribute to significant levels of daytime sleepiness in some persons.
Primary hypersomnias
Narcolepsy, the most common of the primary hypersomnias, is reported to affect 0.02 to 0.18 percent of the adult population, but may be significantly underdiagnosed. Approximately 25 to 30 percent of patients with narcolepsy have associated cataplexy (i.e., sudden and transient loss of muscle tone associated with emotions) 65. Less common are the other primary hypersomnias of central origin, including idiopathic hypersomnia, menstrual hypersomnia, and Kleine-Levin syndrome (a rare form of recurrent hypersomnia most common in male adolescents) 54.
Excessive daytime sleepiness symptoms
Excessive sleepiness or excessive daytime sleepiness is defined by having an increased pressure to fall asleep during typical wake hours 1. People who have excessive sleepiness feel drowsy and sluggish most days, and these symptoms often interfere with their work, school, activities, or relationships. Although patients with excessive daytime sleepiness often complain of “fatigue,” excessive sleepiness is different from fatigue which is characterized by low energy and the need to rest (not necessarily sleep). Excessive sleepiness is also different from depression, in which a person may have a reduced desire to do normal activities, even the ones they used to enjoy. Persons with excessive daytime sleepiness are at risk of motor vehicle and work-related incidents, and have poorer health than comparable adults 9. The prevalence of excessive daytime sleepiness is highest in adolescents, older persons, and shift workers 10, but assessment of its true prevalence is difficult because of the subjective nature of the symptoms, inconsistencies in terminology, and a lack of consensus on methods of diagnosis and assessment. Some persons use subjective terminology (e.g., drowsiness, languor, inertness, fatigue, sluggishness) when describing symptoms of excessive daytime sleepiness 11.
Excessive daytime sleepiness diagnosis
To diagnose your excessive daytime sleepiness, your doctor may make an evaluation based on your signs and symptoms, an examination, and tests. Your doctor may refer you to a sleep specialist in a sleep center for further evaluation. Your doctor also may refer you to an ear, nose and throat doctor to rule out any anatomic blockage in your nose or throat.
You’ll have a physical examination, and your doctor will examine the back of your throat, mouth and nose for extra tissue or abnormalities. Your doctor may measure your neck and waist circumference and check your blood pressure.
A sleep specialist may conduct additional evaluations to diagnose your condition, determine the severity of your condition and plan your treatment. The evaluation may involve overnight monitoring of your breathing and other body functions as you sleep.
There are several tests that can be done to diagnose sleepiness, which will determine whether the individual has primary (originating in the brain) or secondary (originating as a result of another disease) sleepiness. First, the physician will look for other obvious sleep disorders that could be causing the excessive sleepiness, with the primary goal being to determine if there are treatable medical conditions present. These tests could include polysomnography, subjective scales such as the Epworth Sleepiness Scale and the Stanford Sleepiness Scale, as well as objective tests like the multiple sleep latency test. The physician will usually make the diagnosis when symptoms have been present for three consecutive months and there are no other underlying diseases.
Tests to detect dyssomnias include:
- Polysomnography. During this sleep study, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep. You may have a full-night study, in which you’re monitored all night, or a split-night sleep study. In a split-night sleep study, you’ll be monitored during the first half of the night. If you’re diagnosed with obstructive sleep apnea, staff may wake you and give you continuous positive airway pressure for the second half of the night. Polysomnography can help your doctor diagnose obstructive sleep apnea and adjust positive airway pressure therapy, if appropriate. This sleep study can also help rule out other sleep disorders that can cause excessive daytime sleepiness but require different treatments, such as leg movements during sleep (periodic limb movements) or sudden bouts of sleep during the day (narcolepsy).
- The Multiple Sleep Latency Test (MSLT) and Maintenance of Wakefulness Test (MWT) are tests that are performed in a sleep center. The patient is instructed to try to fall asleep (MSLT) or try to stay awake (MWT). These tests are usually performed during the daytime after a nighttime sleep study. They usually consist of 4 or 5 nap time tests.
- Home sleep apnea testing. Under certain circumstances, your doctor may provide you with an at-home version of polysomnography to diagnose obstructive sleep apnea. This test usually involves measurement of airflow, breathing patterns and blood oxygen levels, and possibly limb movements and snoring intensity.
Changes in Centers for Medicare and Medicaid Services Regulations for Obstructive Sleep Apnea Home Sleep Testing and CPAP (continuous positive airway pressure) Treatment 66
- Obstructive sleep apnea diagnosis is based on an apnea-hypopnea index (AHI) > 15 or an AHI > 5 to 15 associated with daytime sleepiness, impaired cognition, mood disorders, or insomnia, or documented hypertension, ischemic heart disease, or history of smoking
- Apnea-hypopnea index (AHI) is based on standard polysomnography or home sleep testing
- Home sleep testing must only be performed by a physician with board certification in sleep medicine or a physician who is an active staff member of a sleep laboratory or clinic accredited by the American Academy of Sleep Medicine or the Joint Commission
- CPAP is initially limited to a 12-week period, with coverage extended for persons whose symptoms improve based on follow-up physician re-evaluation and with objective evidence of CPAP utilization.
Figure 5. Excessive daytime sleepiness diagnostic algorithm
Footnote: Algorithm for the diagnosis and treatment of conditions that cause excessive daytime sleepiness.
Abbreviations: CPAP = continuous positive airway pressure; OSA = obstructive sleep apnea
Quantifying excessive daytime sleepiness
Subjective assessment of symptoms using questionnaires and clinical assessment of behavioral impact may not accurately reflect the degree of physiologic sleepiness 67. The effects of sleepiness on daytime performance can be assessed by tests of complex reaction time and coordination, or by tests that assess complex behavioral tasks likely to be affected by sleepiness (e.g., driving performance) 68. Performance measures are susceptible to influences that are not task related (e.g., motivation, distraction, comprehension of instructions); therefore, the results of performance tests and questionnaires do not always correlate 11.
The most common tests for assessing psychological variations in daytime sleepiness are the Multiple Sleep Latency Test (MSLT) and the Maintenance of Wakefulness Test (MWT). Both of these tests use modified polysomnography to assess sleep onset latency (i.e., the amount of time it takes to fall asleep) during a series of waking nap periods. Overnight polysomnography is required before the MSLT or MWT to assess the disordered sleep pattern and test for significant obstructive sleep apnea. To diagnose narcolepsy without cataplexy, the Multiple Sleep Latency Test (MSLT) must demonstrate hypersomnolence and early onset of rapid eye movement sleep. The Maintenance of Wakefulness Test (MWT) can be used to assess improvements in waking performance after treatment in persons with excessive daytime sleepiness who could potentially be dangerous to self and others, such as commercial drivers and airplane pilots 69.
Excessive daytime sleepiness treatment
Excessive daytime sleepiness treatment will depend greatly on the underlying cause of sleepiness and whether it is a primary or secondary sleep disorder. Sometimes treatment of excessive daytime sleepiness can be as simple as discontinuing or modifying the use of medication (all prescription and nonprescription medications) and drugs of abuse. Other times, catching up on sleep will alleviate the excessive sleepiness; however, more often than not, it is more appropriate to treat the underlying cause than it is to treat the symptom. Most common treatments include the use of stimulant medications like amphetamines to help the individual stay awake throughout the day. In addition, behavioral therapy, sleep hygiene, and education are usually added to a treatment regimen.
In obstructive sleep apnea—the most dangerous and physiologically disruptive cause of excessive daytime sleepiness—treatment with positive pressure devices (e.g., CPAP) during sleep improves symptoms of daytime sleepiness for most patients 70. The effects of other treatments for obstructive sleep apnea (e.g., medications, dental appliances, surgery) on daytime sleepiness have not been well documented 71.
Modafinil (Provigil) is considered to be the first-line activating agent for the treatment of excessive daytime sleepiness. It is indicated for the treatment of persistent sleepiness associated with obstructive sleep apnea in patients already being treated with CPAP, and for the treatment of daytime sleepiness in patients with shift work disorder 72. Modafinil is pharmacologically distinct from and has a much lower potential for abuse (Schedule IV) than the amphetamines, and has a generally benign side-effect profile. Other medications that must be used with caution to induce alertness in somnolent patients include the amphetamines (dextroamphetamine [Dexedrine], methylphenidate [Ritalin]) and pemoline (Cylert, not available in the United States). The amphetamines are Schedule II prescription drugs and are considered to have a high potential for abuse. Side effects of amphetamines include personality changes, tremor, hypertension, headaches, and gastroesophageal reflux 73. Pemoline can cause hepatic toxicity in susceptible patients. The use of activating agents is inappropriate in hypersomnolent patients with untreated obstructive sleep apnea—although daytime sleepiness may be improved with these agents, the patient remains at risk from the pathophysiologic consequences of untreated obstructive sleep apnea.
Medical and legal considerations
Legal requirements for reporting excessive daytime sleepiness that may impair driving vary from state to state 74. The physician treating patients with excessive daytime sleepiness (or patients using drugs likely to affect driving performance) has the responsibility to make a clinical assessment of the patient’s overall risk of unsafe driving, and to document driving recommendations and precautions. A physician should report patients who fail to comply with treatment, particularly high-risk persons such as airline pilots, truck, bus, and occupational drivers, and those with a history of recent sleepiness-associated incidents.
- https://www.sleepassociation.org/sleep-disorders/more-sleep-disorders/excessive-daytime-sleepiness/[↩][↩]
- National Sleep Foundation. State of the states report on drowsy driving. November 2007.[↩]
- NTSB. Factors that affect fatigue in heavy truck accidents safety study. Washington, DC: National Transportation Safety Board; 1995.[↩]
- Masa JF, Rubio M, Findley LJ. Habitually sleepy drivers have a high frequency of automobile crashes associated with respiratory disorders during sleep. Am J Respir Crit Care Med. 2000;162(4 pt 1):1407–1412.[↩]
- Pagel JF, Forister N, Kwiatkowki C. Adolescent sleep disturbance and school performance: the confounding variable of socioeconomics. J Clin Sleep Med. 2007;3(1):19–23.[↩]
- Sforza E, de Saint Hilaire Z, Pelissolo A, Rochat T, Ibanez V. Personality, anxiety and mood traits in patients with sleep-related breathing disorders: effect of reduced daytime alertness. Sleep Med. 2002;3(2):139–145.[↩][↩]
- Chen I, Vorona R, Chiu R, Ware JC. A survey of subjective sleepiness and consequences in attending physicians. Behav Sleep Med. 2008;6(1):1–15.[↩]
- Johnson EO. Sleep in America: 2000. Results from the National Sleep Foundation’s 2000 Omnibus sleep poll. Washington, DC: The National Sleep Foundation; 2000.[↩]
- Excessive Daytime Sleepiness. Am Fam Physician. 2009 Mar 1;79(5):391-396. https://www.aafp.org/afp/2009/0301/p391.html[↩][↩]
- Friedman NS. Determinants and measurements of daytime sleepiness. In: Pagel JF, Pandi-Perumal SR, eds. Primary Care Sleep Medicine: A Practical Guide. Totowa, N.J.: Humana Press; 2007:61–82.[↩][↩]
- Buysse DJ. Drugs affecting sleep, sleepiness, and performance. In: Monk TH, ed. Sleep, Sleepiness, and Performance. Chichester: Wiley; 1991:4–31.[↩][↩][↩]
- Patel AK, Reddy V, Shumway KR, et al. Physiology, Sleep Stages. [Updated 2024 Jan 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526132[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Memar P, Faradji F. A Novel Multi-Class EEG-Based Sleep Stage Classification System. IEEE Trans Neural Syst Rehabil Eng. 2018 Jan;26(1):84-95. doi: 10.1109/TNSRE.2017.2776149[↩]
- Stages of Sleep: What Happens in a Normal Sleep Cycle? https://www.sleepfoundation.org/stages-of-sleep[↩][↩]
- How Much Deep Sleep Do You Need? https://www.sleepfoundation.org/stages-of-sleep/deep-sleep[↩][↩][↩]
- Malik J, Lo YL, Wu HT. Sleep-wake classification via quantifying heart rate variability by convolutional neural network. Physiol Meas. 2018 Aug 20;39(8):085004. doi: 10.1088/1361-6579/aad5a9[↩]
- Feinberg I, Floyd TC. Systematic trends across the night in human sleep cycles. Psychophysiology. 1979 May;16(3):283-91. doi: 10.1111/j.1469-8986.1979.tb02991.x[↩]
- Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. 2, Sleep Physiology. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19956[↩][↩][↩]
- Zepelin H, Siegel JM, Tobler I. Mammalian sleep. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier/Saunders; 2005. pp. 91–100.[↩]
- Carskadon M, Dement W. Normal human sleep: An overview. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: Elsevier Saunders; 2005. pp. 13–23.[↩][↩][↩]
- Approach to the Patient With a Sleep or Wakefulness Disorder. https://www.msdmanuals.com/professional/neurologic-disorders/sleep-and-wakefulness-disorders/approach-to-the-patient-with-a-sleep-or-wakefulness-disorder[↩]
- Electroencephalogram (EEG) techniques measuring sleep activity and sleep stages. https://quizlet.com/au/336073417/electroencephalogram-eeg-techniques-measuring-sleep-activity-and-sleep-stages-diagram[↩]
- Reddy S, Reddy V, Sharma S. Physiology, Circadian Rhythm. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519507[↩]
- Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014 Jan 8;81(1):12-34. doi: 10.1016/j.neuron.2013.12.025[↩]
- España RA, Scammell TE. Sleep neurobiology from a clinical perspective. Sleep. 2011 Jul 1;34(7):845-58. doi: 10.5665/SLEEP.1112[↩][↩]
- Zajac A, Skowronek-Bała B, Wesołowska E, Kaciński M. Napadowe zaburzenia snu u dzieci w wideo/polisomnografii [Sleep paroxysmal events in children in video/polysomnography]. Przegl Lek. 2010;67(9):762-9. Polish.[↩]
- Feriante J, Araujo JF. Physiology, REM Sleep. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531454[↩][↩]
- Carley DW, Farabi SS. Physiology of Sleep. Diabetes Spectr. 2016 Feb;29(1):5-9. doi: 10.2337/diaspect.29.1.5[↩][↩]
- Frank, M.G., Heller, H.C. (2018). The Function(s) of Sleep. In: Landolt, HP., Dijk, DJ. (eds) Sleep-Wake Neurobiology and Pharmacology . Handbook of Experimental Pharmacology, vol 253. Springer, Cham. https://doi.org/10.1007/164_2018_140[↩]
- Varga B, Gergely A, Galambos Á, Kis A. Heart Rate and Heart Rate Variability during Sleep in Family Dogs (Canis familiaris). Moderate Effect of Pre-Sleep Emotions. Animals (Basel). 2018 Jul 2;8(7):107. doi: 10.3390/ani8070107[↩]
- Antony JW, Schönauer M, Staresina BP, Cairney SA. Sleep Spindles and Memory Reprocessing. Trends Neurosci. 2019 Jan;42(1):1-3. doi: 10.1016/j.tins.2018.09.012[↩]
- Gais S, Mölle M, Helms K, Born J. Learning-dependent increases in sleep spindle density. J Neurosci. 2002 Aug 1;22(15):6830-4. doi: 10.1523/JNEUROSCI.22-15-06830.2002[↩]
- Gandhi MH, Emmady PD. Physiology, K Complex. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557469[↩]
- Hilditch CJ, McHill AW. Sleep inertia: current insights. Nat Sci Sleep. 2019 Aug 22;11:155-165. doi: 10.2147/NSS.S188911[↩]
- El Shakankiry HM. Sleep physiology and sleep disorders in childhood. Nat Sci Sleep. 2011 Sep 6;3:101-14. doi: 10.2147/NSS.S22839[↩]
- Blumberg MS, Lesku JA, Libourel PA, Schmidt MH, Rattenborg NC. What Is REM Sleep? Curr Biol. 2020 Jan 6;30(1):R38-R49. doi: 10.1016/j.cub.2019.11.045[↩]
- Peever J, Fuller PM. The Biology of REM Sleep. Curr Biol. 2017 Nov 20;27(22):R1237-R1248. doi: 10.1016/j.cub.2017.10.026[↩]
- Feriante J, Singh S. REM Rebound Effect. [Updated 2024 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560713[↩]
- Rasch B, Born J. About sleep’s role in memory. Physiol Rev. 2013 Apr;93(2):681-766. doi: 10.1152/physrev.00032.2012[↩]
- Sleep and your health. https://medlineplus.gov/ency/patientinstructions/000871.htm[↩]
- Consensus Conference Panel; Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015 Jun 15;11(6):591-2. doi: 10.5664/jcsm.4758[↩]
- Normal Sleep, Sleep Physiology, and Sleep Deprivation. https://emedicine.medscape.com/article/1188226-overview#showall[↩]
- https://www.sleepfoundation.org/sleep-calculator[↩]
- Dijk DJ. Regulation and functional correlates of slow wave sleep. J Clin Sleep Med. 2009 Apr 15;5(2 Suppl):S6-15. https://pmc.ncbi.nlm.nih.gov/articles/PMC2824213[↩]
- Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012 Jan;463(1):121-37. doi: 10.1007/s00424-011-1044-0[↩]
- Vlahoyiannis A, Aphamis G, Bogdanis GC, Sakkas GK, Andreou E, Giannaki CD. Deconstructing athletes’ sleep: A systematic review of the influence of age, sex, athletic expertise, sport type, and season on sleep characteristics. J Sport Health Sci. 2021 Jul;10(4):387-402. doi: 10.1016/j.jshs.2020.03.006[↩]
- Javaheri S, Zhao YY, Punjabi NM, Quan SF, Gottlieb DJ, Redline S. Slow-Wave Sleep Is Associated With Incident Hypertension: The Sleep Heart Health Study. Sleep. 2018 Jan 1;41(1):zsx179. doi: 10.1093/sleep/zsx179[↩]
- Zhang Y, Gruber R. Can Slow-Wave Sleep Enhancement Improve Memory? A Review of Current Approaches and Cognitive Outcomes. Yale J Biol Med. 2019 Mar 25;92(1):63-80. https://pmc.ncbi.nlm.nih.gov/articles/PMC6430170[↩]
- Healthy Sleep. https://medlineplus.gov/healthysleep.html[↩]
- Changing your sleep habits. https://medlineplus.gov/ency/patientinstructions/000757.htm[↩]
- Maeda T, Koga H, Nonaka T, Higuchi S. Effects of bathing-induced changes in body temperature on sleep. J Physiol Anthropol. 2023 Sep 8;42(1):20. doi: 10.1186/s40101-023-00337-0[↩]
- St-Onge MP, Roberts A, Shechter A, Choudhury AR. Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep. J Clin Sleep Med. 2016 Jan;12(1):19-24. doi: 10.5664/jcsm.5384[↩]
- Lee M, Song CB, Shin GH, Lee SW. Possible Effect of Binaural Beat Combined With Autonomous Sensory Meridian Response for Inducing Sleep. Front Hum Neurosci. 2019 Dec 2;13:425. doi: 10.3389/fnhum.2019.00425[↩]
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic & Coding Manual. 2nd ed. Westchester, Ill.: American Academy of Sleep Medicine; 2005.[↩][↩][↩]
- Van Dongen H, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation [published correction appears in Sleep. 2004; 27(4):600]. Sleep. 2003;26(2):117–126.[↩][↩]
- Pagel JF. Sleep disorders in primary care: evidence-based clinical practice. In: Pagel JF, Pandi-Perumal SR, eds. Primary Care Sleep Medicine: A Practical Guide. Totowa, N.J.: Humana Press; 2007:1–14.[↩][↩]
- Pagel JF. Medications that induce sleepiness. In: Lee-Chiong TL, ed. Sleep: A Comprehensive Handbook. Hoboken, N.J.: Wiley-Liss; 2006:175–182.[↩][↩]
- Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An Amerrican Academy of Sleep Medicine review. Sleep. 2000;23(2):243–308.[↩]
- Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20(9):705–706.[↩]
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239.[↩][↩]
- World Kidney Day 10 March 2017. https://www.who.int/life-course/news/events/world-kidney-day-2017/en/[↩]
- Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27(3):453–458.[↩]
- Findley LJ, Levinson MP, Bonnie RJ. Driving performance and automobile accidents in patients with sleep apnea. Clin Chest Med. 1992;13(3):427–435.[↩]
- Lindberg E, Carter N, Gislason T, Janson C. Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med. 2001;164(11):2031–2035.[↩]
- Thorpy MJ. Cataplexy associated with narcolepsy: epidemiology, pathophysiology and management. CNS Drugs. 2006;20(1):43–50.[↩]
- https://www.cms.gov/Medicare/Coverage/Coverage-with-Evidence-Development/CPAP[↩]
- Roehrs T, Carskadon MA, Dement WC, Roth T. Daytime sleepiness and alertness. In: Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. 3rd ed. Philadelphia, Pa.: Saunders; 2000:43–52.[↩]
- George CF. Vigilance impairment: assessment by driving simulators. Sleep. 2000;23(suppl 4):S115–S118.[↩]
- Kreiger J. Clinical approach to excessive daytime sleepiness. Sleep. 2000;23(suppl 4):S95–S98.[↩]
- Findley L, Smith C, Hooper J, Dineen M, Suratt PM. Treatment with nasal CPAP decreases automobile accidents in patients with sleep apnea. Am J Respir Crit Care Med. 2000;161(3 pt 1):857–859.[↩]
- Veasey SC, Guilleminault C, Strohl KP, Sanders MH, Ballard RD, Magalang UJ. Medical therapy for obstructive sleep apnea: a review by the Medical Therapy for Obstructive Sleep Apnea Task Force of the Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 2006;29(8):1036–1044.[↩]
- Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder [published correction appears in N Engl J Med. 2005;353(10):1078]. N Engl J Med. 2005;353(5):476–486.[↩]
- Wilens TE, Biederman J. The stimulants. Psychiatr Clin North Am. 1992;15(1):191–222.[↩]
- Boehlecke BA. Medicolegal aspects of obstructive sleep apnea/hypopnea syndrome. In: Pagel JF, Pandi-Perumal SR, eds. Primary Care Sleep Medicine: A Practical Guide. Totowa, N.J.: Humana Press; 2007:155–160.[↩]