Contents
What is adenomyosis
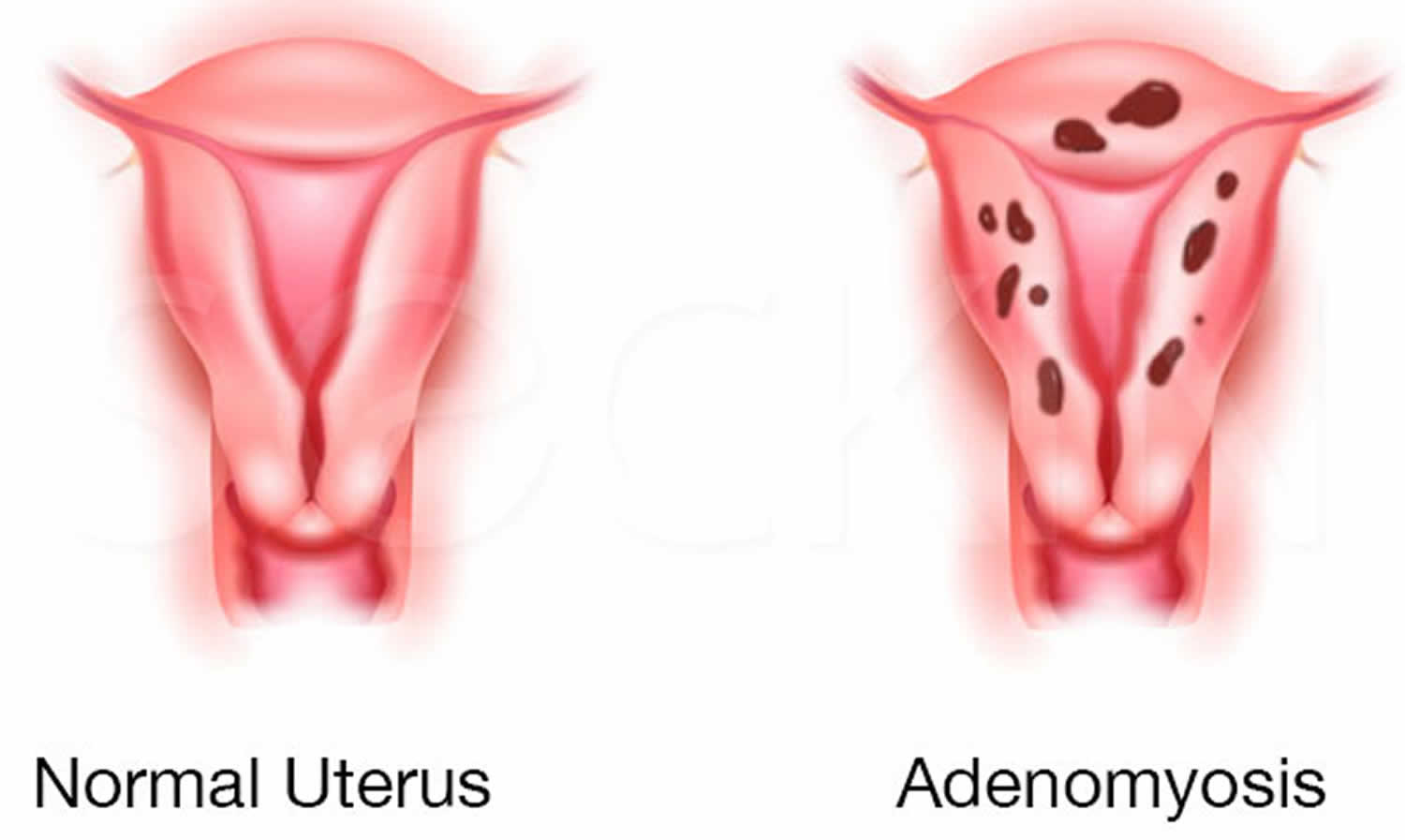
Adenomyosis is a common, benign uterine pathology that occurs when the cells that normally line the uterus (endometrial tissue) also grow into the layer of muscle in the wall of your uterus. Adenomyosis is thought by many to be on the spectrum of endometriosis, with ectopic endometrial tissue in the myometrium 1. The displaced endometrial tissue continues to act normally — thickening, breaking down and bleeding — during each menstrual cycle. An enlarged uterus and painful, heavy periods can result. If adenomyosis is concentrated in one area, it can lead to a mass called an adenomyoma.
Adenomyosis may present with abnormally heavy uterine bleeding (menorrhagia) and painful periods or menstrual cramps (dysmenorrhea).
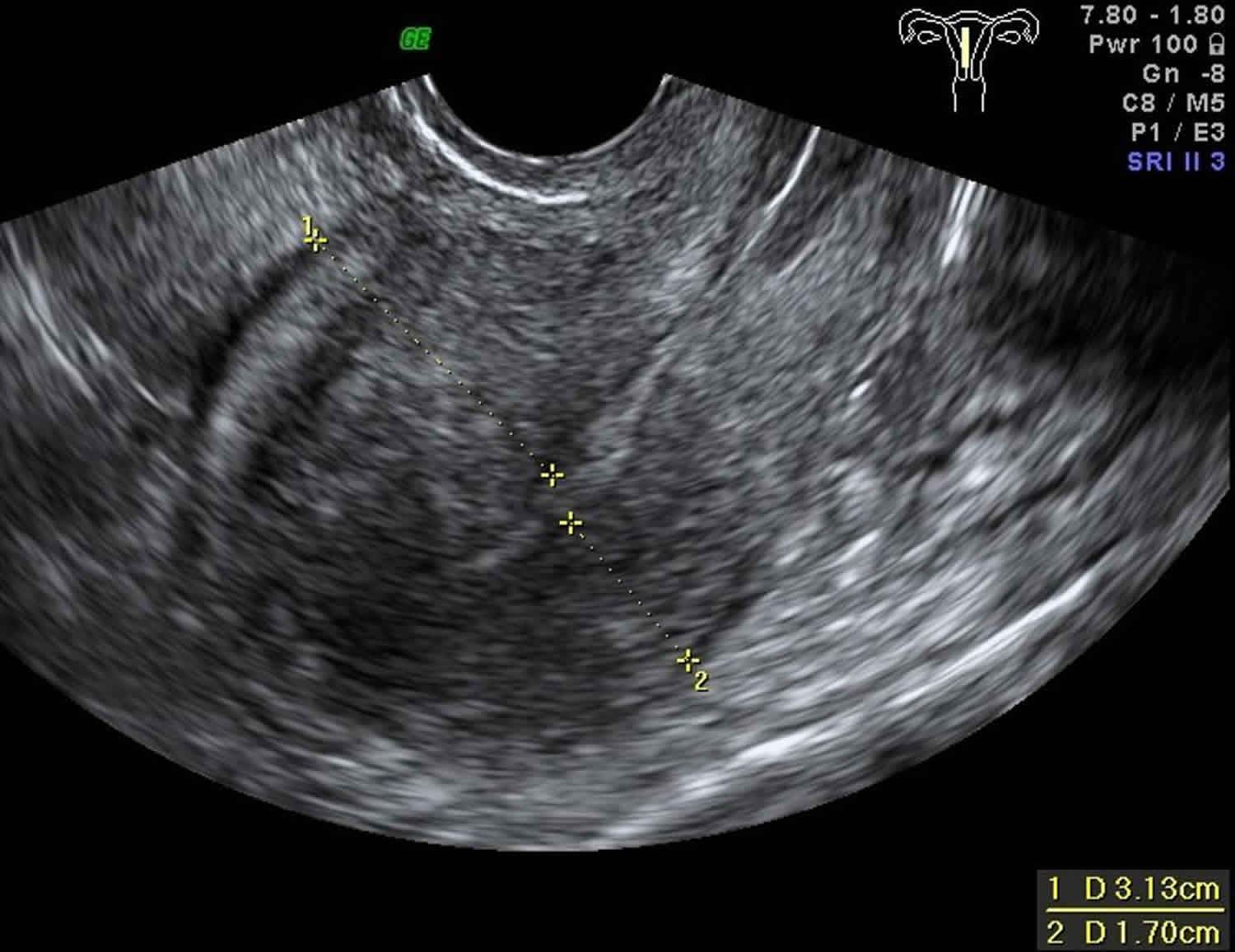
Adenomyosis may be difficult to diagnose. Transvaginal ultrasound (the ultrasound probe is placed in the vagina) and MRI are imaging modalities that may show characteristic findings. The test should preferably be performed by a gynecologist who specializes in ultrasound, as general ultrasonagraphers may be inexperienced in the diagnosis of adenomyosis. Unfortunately, the sonographic features of adenomyosis are variable and may be absent 2. The reported sensitivity and specificity of transabdominal ultrasound are 32-63% and 95-97% respectively 3. However, it has been reported that transvaginal ultrasound is as sensitive (89%) and specific (89%) as MRI in diagnosing adenomyosis. Ultrasound features of adenomyosis, including asymmetrical uterine wall thickening anteriorly with focal heterogeneity and associated increased blood flow, as well as the “venetian blind” pattern of acoustic shadowing. The latter may be seen with either adenomyosis or uterine fibroids 4. However, the only way to confirm adenomyosis is to examine the uterus after hysterectomy.
Imaging features of adenomyosis are variable and in many instances very subtle. Three (some say four) forms can be distinguished 2:
- Diffuse adenomyosis is the most common of uterine adenomyosis 5.
- Focal adenomyosis and adenomyoma: some consider these as separate.
- Cystic adenomyosis is a rare variant of adenomyosis and is believed to the result of repeated focal haemorrhages resulting in cystic spaces filled with altered blood products 6.
- Adenomyotic cyst is an extremely rare variation of cystic adenomyosis 7. The lesion consists of a large hemorrhagic cyst, which is partly or entirely surrounded by a solid wall. It can be entirely within the myometrium, submucosal, or subserosal and frequently is associated with symptoms of menorrhagia and dysmenorrhea.
Adenomyosis association with other gynecological disorders
Coexistence of adenomyosis with other gynecological disorders, such as myomas and endometriosis, has been well established 8.
- If you have adenomyosis, you might have co-existent endometriosis, which has been reported in 27% of women with endometriosis 9. A study evaluating the prevalence of adenomyosis using MRI scans in women diagnosed with endometriosis as compared to two control groups, one without endometriosis, defined as control group, and another without endometriosis but with a partner considered hypofertile, defined as healthy control group, confirmed the presence of adenomyotic lesions, in 79% of the endometriosis group, 28% of the control group, and 9% in the healthy control group 10. Interestingly, the prevalence of adenomyosis reached 90% in the subset of women with endometriosis less than 36 years of age. This study contrasts findings from a previous study, in which adenomyosis diagnosed with MRI was present in only 27% of women with endometriosis 9.
- Leiomyomas: may be present in almost 50% of cases involving adenomyosis of the uterus 11.
- Other reported associations include endometrial hyperplasia and endometrial polyps 11.
The cause of adenomyosis remains unknown, but adenomyosis is only seen in women in their reproductive years because it requires the hormone estrogen to grow. Adenomyosis eventually goes away after menopause when estrogen production drops.
Adenomyosis is difficult to treat and it will disappear after menopause so management will depend on your life stage. For women who have severe discomfort from adenomyosis, hormonal treatments can help. Removal of the uterus (hysterectomy) cures adenomyosis.
What happens when you get a period?
The endometrial tissue in the muscle undergo the same changes as the endometrial cells of the uterus. This means when you have your period, these endometrial tissue also bleed but because they are trapped in the muscle layer they form little pockets of blood within the muscle.
If you have prolonged, heavy bleeding or severe cramping during your periods that interferes with your regular activities, make an appointment to see your doctor.
Other uterine diseases can cause signs and symptoms similar to adenomyosis, making adenomyosis difficult to diagnose. Conditions include fibroid tumors (leiomyomas), uterine cells growing outside the uterus (endometriosis) and growths in the uterine lining (endometrial polyps).
Your doctor might conclude that you have adenomyosis only after ruling out other possible causes for your signs and symptoms.
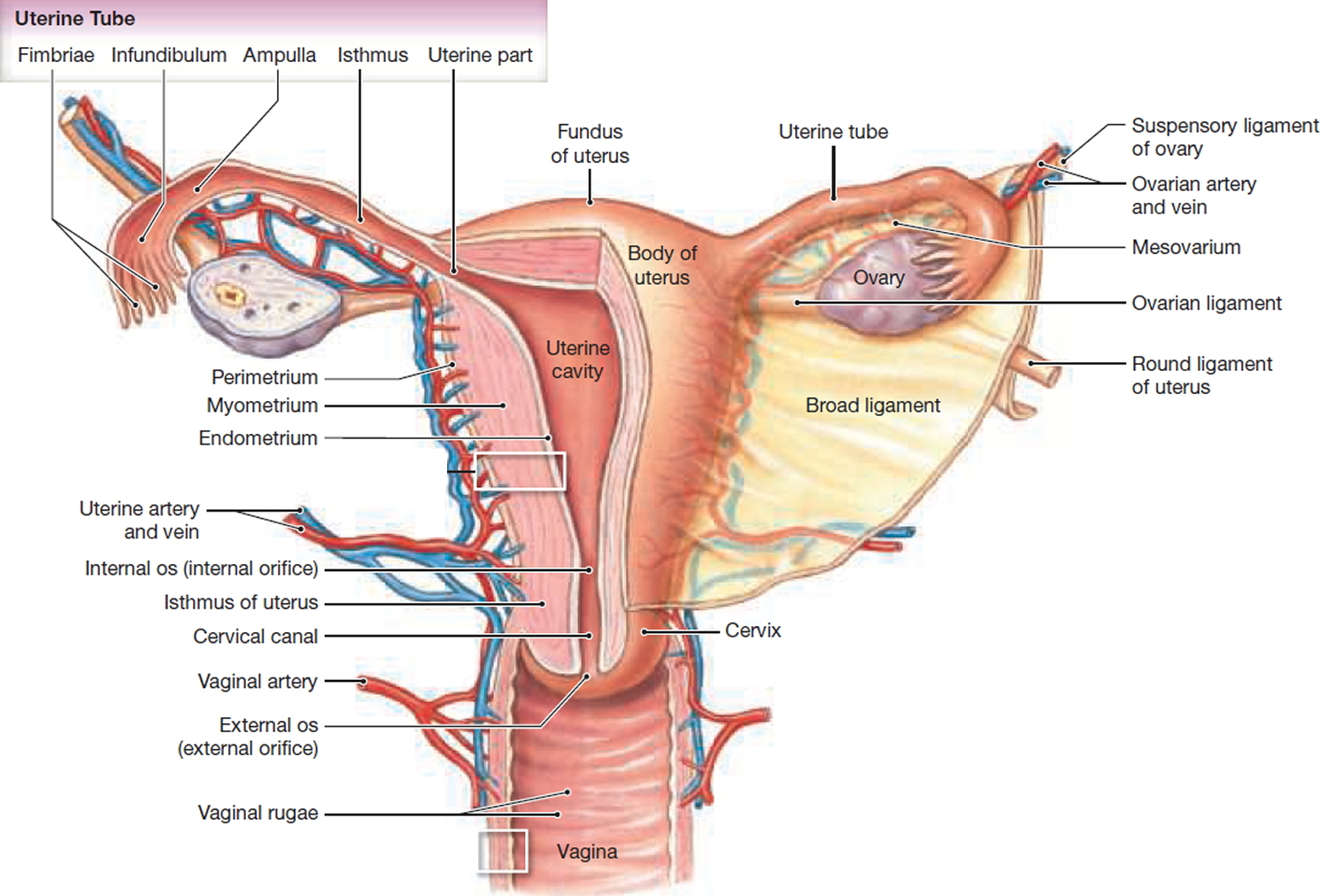
Figure 1. Uterus anatomy
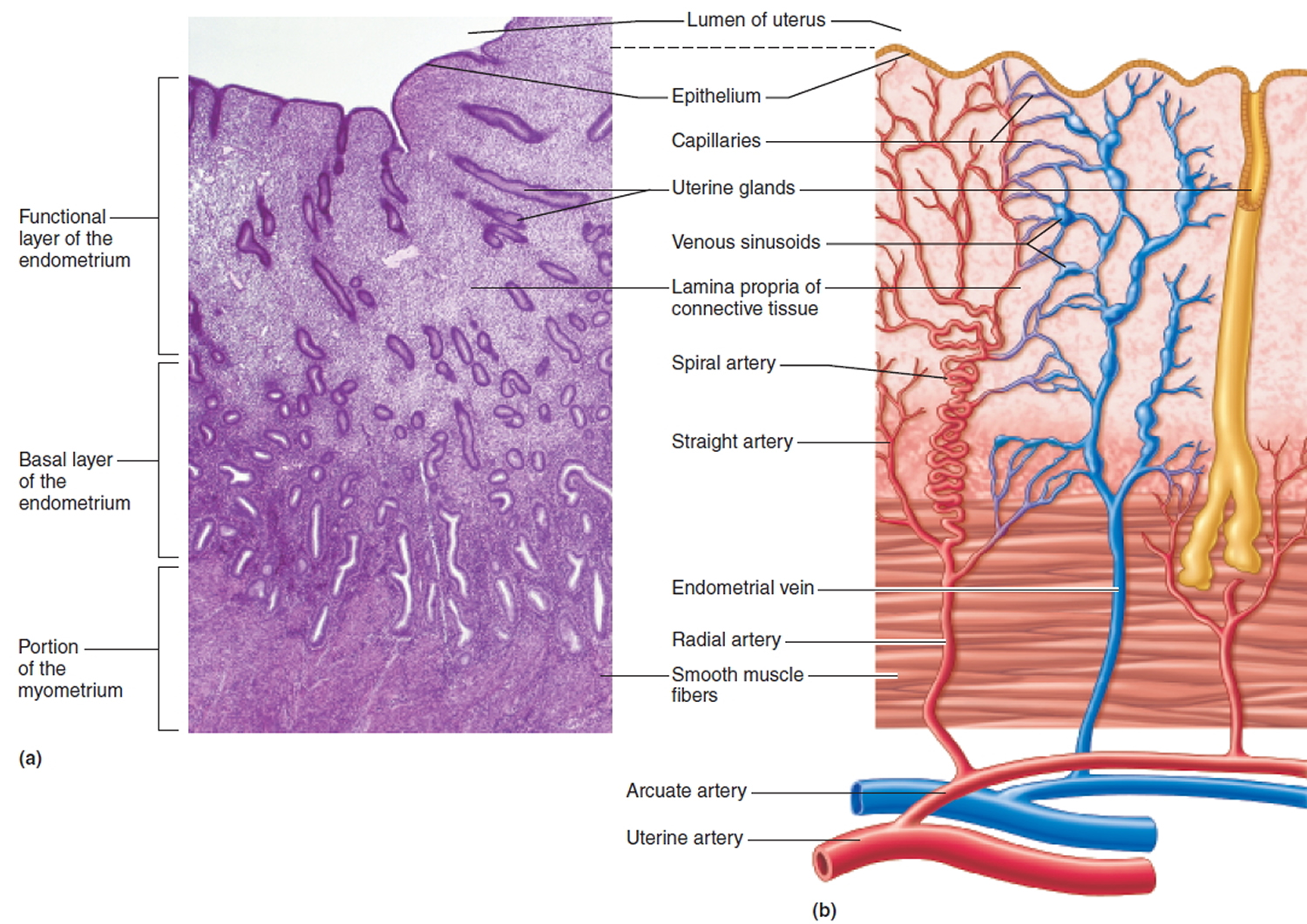
Figure 2. Endometrium of the uterus and its blood supply
Figure 3. Adenomyosis
Figure 4. Adenomyosis ultrasound
Footnote: Asymmetrical uterine wall thickening anteriorly with focal heterogeneity and associated increased blood flow, as well as the “venetian blind” pattern of acoustic shadowing.
[Source 4 ]Adenomyosis vs Endometriosis
Endometriosis occurs when cells similar to those that line the uterus (endometrial tissue) are found in other parts of the body such as the fallopian tubes, the ovaries or the tissue lining the pelvis (the peritoneum). In rare cases, endometriosis may grow outside the pelvic cavity, such as on the lungs or in other parts of the body 12.
About 30% of women with endometriosis with endometriosis have trouble with fertility and struggle to get pregnant. This is likely to affect women in different ways and can create a rollercoaster of emotions. It is thought that the reasons are related to:
- scarring of the tubes and ovaries from endometriosis
- problems with the quality of the egg
- problems with the embryo traveling down the tube and implanting in the wall of the uterus due to damage from endometriosis
- change of the organs in the pelvis such as adhesions with scarred pelvic tissue and blockage of the fallopian tubes
Once pregnant, many women also worry about the effect of their endometriosis on their pregnancy and delivery. Pregnancy does not cure endometriosis, but symptoms appear to improve during pregnancy. This is because higher progesterone levels can suppress the endometriosis. However, the effects of endometriosis after delivery of the baby are unclear. These effects may only be temporary and many women have a recurrence within a few years.
It is important to remember not all women with endometriosis are infertile. Many women have children without difficulty, have children before they are diagnosed, or eventually have a successful pregnancy.
Laparoscopic surgery (keyhole surgery using a thin telescope with a light inserted through a small cut in the belly button to look into the pelvis) is an operation to reduce symptoms and improve fertility by removing endometriotic patches, implants, cysts, nodules and adhesions by cutting them out (excision) or burning them (diathermy).
If treatment is unsuccessful, in vitro fertilisation (IVF) treatments may also be considered. However, before trying this form of treatment, it is important that your endometriosis is properly treated. IVF treatment includes increasing oestrogen levels, which will encourage the development of existing endometriosis.
Fertility treatments
Starting on fertility treatment can lead to a range of different feelings from happiness and excitement to frustration, disappointment and sadness.
If you decide to try fertility treatment, it is important both you and your partner are supported through the process. Most IVF units will have counselors who will support and counsel you through the assessment and treatment time. Getting counseling before starting treatment can help you to:
- prepare for the emotional journey ahead
- cope with any unsuccessful treatments or miscarriages
- develop strategies for coping with other people’s pregnancies/births
- talk through how both you and your partner are feeling throughout the process
Endometriosis, pregnancy and delivery
Recent studies have shown if you have endometriosis, medical care should not stop once you become pregnant. Endometriosis is a risk factor for:
- the baby being born early – before 40 weeks
- bleeding after the 24th week of pregnancy
- high blood pressure (pre-eclampsia)
- delivery by caesarean section
Endometriosis and the risk of premature birth
If you have ovarian cysts (endometriomas) and become pregnant using assisted reproductive technologies (ART), there is a greater risk of the baby:
- being born early – before 40 weeks (preterm birth)
A large study of more than 13,000 births, showed that women who were diagnosed with endometriosis had a higher risk of complications at birth, preterm birth and of having a caesarean section 13. This research information helps obstetricians identify and monitor pregnant women who have been diagnosed with endometriosis at increased risk of premature labor and birth.
Who is at risk of adenomyosis?
The known risks for developing adenomyosis are:
- previous surgery of the uterus such as a caesarean section or fibroid removal
- childbirth
Because of the link with childbirth or uterine surgery, adenomyosis is more likely to occur in women between 30-50 years.
Does adenomyosis affect fertility?
Studies suggest there may be changes in the ability of the uterine muscles to contract appropriately. Also, these endometrial cells inside the muscle may release body chemicals which lead to subfertility.
Mechanisms proposed for fertility impairment on the presence of adenomyosis 14.
- (i) Aberrant uterine contractility, originating from the junctional zone, which is broadened in case of adenomyosis, may impair rapid and sustained directed sperm transport
- (ii) Abnormal myometrial activity during the peri-implantation period may hinder apposition, adhesion, and penetration of the embryonic pole of the blastocyst into the decidualized endometrium
- (iii) Increased endometrial stroma vascularization in the secretory phase may derange the endometrial milieu, thus negatively affecting implantation
- (iv) Alteration in the expression profile of cytokines and growth factors in the endometrium, such as increased expression of hypoxia-inducible factor 1α (HIF-1α) and interleukins (IL-6, IL-8, IL-10) as well as IL-8 receptors CXCR1 and CXCR2, matrix metalloproteinases (MMP2 and MMP9) and vascular endothelial growth factor (VEGF) and decreased expression of leukemia inhibiting factor (LIF), LIF receptor α, and IL-11 may be linked to adenomyosis-associated infertility
- (v) Decreased expression of HOXA-10 gene during the midluteal phase, which is considered a necessary component of endometrial receptivity and peaks during the implantation window, may negatively affect implantation
- (vi) Hyperestrogenic endometrial environment due to the increased expression of cytochrome P450 along with increased aromatase activity in the endometrium sustains the increased expression of the estrogen receptor α during the secretory phase. This in turn adversely affects cell-adhesion molecule expression, such as β3 integrins, which are deemed as key elements for the development of a receptive endometrium.
Besides the rationale for the existence of a link between adenomyosis and infertility, to date a causal relationship between these conditions has not been fully confirmed 15. On the other hand, reports of the incidence of adenomyosis in the infertile women entering an IVF/ICSI (intracytoplasmic sperm injection) program are inconsistent, varying from 6.9% to 34.3% 16. A recent systematic review and meta-analysis on the effect of adenomyosis on IVF outcome reinforced the aspect of a negative impact of this condition on reproductive outcome 16. Clinical pregnancy rates in women with adenomyosis were 28% lower as compared to controls. It is noteworthy that no significant difference was seen when analysis was restricted to women undergoing a single IVF/ICSI (intracytoplasmic sperm injection) cycle. Interestingly, coexistence of endometriosis did not alter these results. Similarly, implantation rates were 23% lower in the adenomyosis group and live birth rates were 30% lower. The miscarriage rate per clinical pregnancy was also significantly increased in women with adenomyosis. The authors concluded that screening for adenomyosis in infertile women entering an IVF program is worthy and thus should be encouraged 16.
For a patient, who has a desire to preserve her reproductive function, various uterine-sparing surgical techniques have been proposed. For patients with focal adenomyosis disease and for selected cases of more diffuse adenomyosis, excision of the adenomyoma or cystectomy for cystic focal adenomyosis has been proposed 15. Partial removal of the abnormal tissue or cytoreductive surgery is reserved for cases of diffuse adenomyosis with special attention to preserve a functional uterus 15. Nonexcisional invasive treatments include laparoscopic (electrocoagulation, uterine artery ligation), hysteroscopic (ablation, transcervical resection), and other treatments, the latter including uterine artery embolization 14 and ablation with MRI-guided focused ultrasound surgery (MRIgFUS), thermoballoon, radiofrequency, or microwave 15.
Conservative medical approaches have also been applied to relieve symptoms and in women wishing to get pregnant. GnRH-analogues, aromatase inhibitors, the levonorgestrel-releasing intrauterine contraception device, a danazol intrauterine contraception device, and the continuous use of estrogen-progestin oral contraceptives are all included in available treatment options 17.
Adenomyosis and pregnancy
Data concerning the association between adenomyosis and pregnancy outcome are scanty. An early study reported a prevalence of adenomyosis of 17.2% in women undergoing cesarean hysterectomy. The authors thought that the presence of adenomyosis could have impair gravid uterus functionality, thereby increasing pregnancy complications, such as postpartum hemorrhage, uterine atony, and uterine rupture 18.
A subsequent and more recent study found an increased risk for preterm birth, more frequent occurrences of fetal growth restriction and fetal malpresentation 19 and preterm premature rupture of membranes in association with adenomyosis 20. Among the pathogenic processes having been proposed so far, the authors pointed at decidual chorioamniotic or systemic inflammation, as the possible underlying mechanism for adenomyosis-related preterm delivery.
A review of the literature regarding pregnancy complications in association to adenomyosis revealed only 29 cases. In particular, uterine rupture, postpartum hemorrhage due to uterine atony, and ectopic pregnancy were reported in relation to adenomyosis in the gravid uterus 21.
What causes adenomyosis?
It is not certain how or why the uterus-lining cells enter the muscle wall. However there are a number of theories for the causes of adenomyosis:
- Invasive tissue growth. Some experts believe that adenomyosis results from the direct invasion of endometrial cells from the lining of the uterus into the muscle that forms the uterine walls. Uterine incisions made during an operation such as a cesarean section (C-section) might promote the direct invasion of the endometrial cells into the wall of the uterus.
- Developmental origins. Other experts suspect that adenomyosis originates within the uterine muscle from endometrial tissue deposited there when the uterus first formed in the fetus.
- Uterine inflammation related to childbirth. Another theory suggests a link between adenomyosis and childbirth. Inflammation of the uterine lining during the postpartum period might cause a break in the normal boundary of cells that line the uterus. Surgical procedures on the uterus can have a similar effect.
- Stem cell origins. A recent theory proposes that bone marrow stem cells might invade the uterine muscle, causing adenomyosis.
Adenomyosis sometimes happens after:
- the birth of a baby
- surgery involving the uterus, such as caesarean section or removal of uterine fibroids.
Regardless of how adenomyosis develops, its growth depends on the circulating estrogen in women’s bodies.
Risk factors for adenomyosis
Risk factors for adenomyosis include:
- Prior uterine surgery, such as a caesarean section (C-section) or fibroid removal
- Childbirth
- Middle age
Most cases of adenomyosis — which depends on estrogen — are found in women in their 40s and 50s. Adenomyosis in these women could relate to longer exposure to estrogen compared with that of younger women. However, current research suggests that the condition might be common in younger women.
Adenomyosis symptoms
Most patients with adenomyosis are asymptomatic 22. Symptoms related to adenomyosis include painful periods (dysmenorrhea), heavy periods (menorrhagia), pain during sex (dyspareunia), chronic pelvic pain, and prolonged or excessive uterine bleeding that occurs irregularly (menometrorrhagia) 23. Pelvic tenderness on examination is associated with diffuse enlargement of the uterus.
Often, symptoms start late in the childbearing years after women have children. Women with adenomyosis might have:
- heavy or prolonged menstrual bleeding
- painful periods
- pain during sex
- bleeding between periods
- tiredness from the anemia caused by blood loss
The symptoms might be mild, but they can be severe enough to interfere with work and your enjoyment of life.
Your uterus might get bigger. Although you might not know if your uterus is enlarged, you may notice that your lower abdomen feels tender or causes pelvic pressure.
Adenomyosis complications
If you often have prolonged, heavy bleeding during your periods, you can develop chronic anemia, which causes fatigue and other health problems.
Although not harmful, the pain and excessive bleeding associated with adenomyosis can disrupt your lifestyle. You might avoid activities you’ve enjoyed in the past because you’re in pain or you worry you might start bleeding.
Adenomyosis diagnosis
Your doctor may suspect adenomyosis based on:
- Signs and symptoms
- A pelvic exam that reveals an enlarged, tender uterus
- Ultrasound imaging of the uterus
- Magnetic resonance imaging (MRI) of the uterus
In some instances, your doctor might collect a sample of uterine tissue for testing (endometrial biopsy) to verify that your abnormal uterine bleeding isn’t associated with another serious condition. But an endometrial biopsy won’t help your doctor confirm a diagnosis of adenomyosis.
The only way to confirm adenomyosis is to examine the uterus after hysterectomy. However, pelvic imaging such as ultrasound and MRI can detect signs of it.
Other uterine diseases can cause signs and symptoms similar to adenomyosis, making adenomyosis difficult to diagnose. Conditions include fibroid tumors (leiomyomas), uterine cells growing outside the uterus (endometriosis) and growths in the uterine lining (endometrial polyps).
Your doctor might conclude that you have adenomyosis only after ruling out other possible causes for your signs and symptoms.
Adenomyosis treatment
Adenomyosis often goes away after menopause, so treatment might depend on how close you are to that stage of life.
Treatment options for adenomyosis include:
- Anti-inflammatory drugs. Your doctor might recommend anti-inflammatory medications, such as ibuprofen (Advil, Motrin IB, others), to control the pain. By starting an anti-inflammatory medicine one to two days before your period begins and taking it during your period, you can reduce menstrual blood flow and help relieve pain.
- Hormone medications. Combined estrogen-progestin birth control pills or hormone-containing patches or vaginal rings might lessen heavy bleeding and pain associated with adenomyosis. Progestin-only contraception, such as an intrauterine device, or continuous-use birth control pills often lead to amenorrhea — the absence of your menstrual periods — which might provide some relief.
- Progestogen releasing intrauterine device (IUD) such as Mirena. The insertion of a progestogen releasing intrauterine device (IUD) can cause:
- a thinning of the endometrium
- a reduction in the size of the uterus
- a reduction in the pain experienced with intercourse
- reduced bleeding
- Gonadotropin-releasing hormone (GnRH) agonists (an artificial hormone used to prevent natural ovulation). Gonadotropin-releasing hormone (GnRH) agonists cause:
- a thinning of the endometrium
- a reduction in the size of the uterus
- suppression of the period
- a temporary chemical menopause
- In the presence of infertility and endometriosis these may be used temporarily.
- Progestogen releasing intrauterine device (IUD) such as Mirena. The insertion of a progestogen releasing intrauterine device (IUD) can cause:
- Hysterectomy. If your pain is severe and no other treatments have worked, your doctor might suggest surgery to remove your uterus. Removing your ovaries isn’t necessary to control adenomyosis.
You can ease adenomyosis pain and cramps by:
- Take an over-the-counter anti-inflammatory medication, such as ibuprofen (Advil, Motrin IB, others).
- Use warm baths and heat packs. Use a heating pad on your abdomen.
- Hormone treatment
- Insertion of an intrauterine device (IUD) that releases the hormone progesterone
Hysterectomy is an option for women with severe adenomyosis.
Treatment for an adenomyoma (mass of adenomyosis in one area):
- Laparoscopy (keyhole surgery): An adenoyoma may be surgically removed using keyhole surgery.
- High intensity focused ultrasound: Guided by an MRI, high intensity focused ultrasound waves cause a localised increase in temperature to the adenomyoma causing the cells to die.
Lifestyle modifications
Some women have found that their pain is improved by exercise and relaxation techniques. Although natural supplements have not been shown to reduce endometriosis-related pain, over-the-counter, nonsteroidal, anti-inflammatory medications, like ibuprofen and naproxen, reduce painful menstrual cramps. When painful intercourse is a problem, changing positions prevents pain caused by deep penetration. In spite of these measures, medical treatment is frequently needed.
- History of adenomyosis. Benagiano G, Brosens I. Best Pract Res Clin Obstet Gynaecol. 2006 Aug; 20(4):449-63. https://www.ncbi.nlm.nih.gov/pubmed/16515887/[↩]
- Adenomyosis. https://radiopaedia.org/articles/adenomyosis[↩][↩]
- Tamai K, Togashi K, Ito T et-al. MR imaging findings of adenomyosis: correlation with histopathologic features and diagnostic pitfalls. Radiographics. 25 (1): 21-40. doi:10.1148/rg.251045060[↩]
- Adenomyosis. https://radiopaedia.org/cases/adenomyosis-4[↩][↩]
- Diffuse uterine adenomyosis. https://radiopaedia.org/articles/diffuse-uterine-adenomyosis[↩]
- Cystic adenomyosis. https://radiopaedia.org/articles/cystic-adenomyosis[↩]
- Adenomyotic cyst. https://radiopaedia.org/articles/adenomyotic-cyst[↩]
- New interventional techniques for adenomyosis. Rabinovici J, Stewart EA. Best Pract Res Clin Obstet Gynaecol. 2006 Aug; 20(4):617-36. https://www.ncbi.nlm.nih.gov/pubmed/16934530/[↩]
- Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Bazot M, Darai E, Hourani R, Thomassin I, Cortez A, Uzan S, Buy JN. Radiology. 2004 Aug; 232(2):379-89. https://www.ncbi.nlm.nih.gov/pubmed/15205479/[↩][↩]
- Adenomyosis in endometriosis–prevalence and impact on fertility. Evidence from magnetic resonance imaging. Kunz G, Beil D, Huppert P, Noe M, Kissler S, Leyendecker G. Hum Reprod. 2005 Aug; 20(8):2309-16. https://www.ncbi.nlm.nih.gov/pubmed/15919780/[↩]
- Agostinho L, Cruz R, Osório F, Alves J, Setúbal A, Guerra A. MRI for adenomyosis: a pictorial review. Insights Imaging. 2017;8(6):549-556. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5707223[↩][↩]
- Office on Women’s Health, U.S. Department of Health and Human Services. (2009). Endometriosis fact sheet. http://www.womenshealth.gov/publications/our-publications/fact-sheet/endometriosis.html[↩]
- Stephansson O, Kieler H, Granath F, Falconer H. Endometriosis assisted reproduction technology, and risk of adverse pregnancy outcome. Human Reproduction. 2009;24(9): 2341-7.[↩]
- Vlahos NF, Theodoridis TD, Partsinevelos GA. Myomas and Adenomyosis: Impact on Reproductive Outcome. Biomed Res Int. 2017;2017:5926470. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5694987/[↩][↩]
- Uterus-sparing operative treatment for adenomyosis. Grimbizis GF, Mikos T, Tarlatzis B. Fertil Steril. 2014 Feb; 101(2):472-87. https://www.ncbi.nlm.nih.gov/pubmed/24289992/[↩][↩][↩][↩]
- Uterine adenomyosis and in vitro fertilization outcome: a systematic review and meta-analysis. Vercellini P, Consonni D, Dridi D, Bracco B, Frattaruolo MP, Somigliana E. Hum Reprod. 2014 May; 29(5):964-77. https://www.ncbi.nlm.nih.gov/pubmed/24622619/[↩][↩][↩]
- Habiba M., Benagiano G. Uterine Adenomyosis. Cham: Springer International Publishing; 2016.[↩]
- Adenomyosis in the gravid uterus at term. SANDBERG EC, COHN F. Am J Obstet Gynecol. 1962 Dec 1; 84():1457-65. https://www.ncbi.nlm.nih.gov/pubmed/13976185/[↩]
- Adverse pregnancy outcomes associated with adenomyosis with uterine enlargement. J Obstet Gynaecol Res. 2015 Apr;41(4):529-33. doi: 10.1111/jog.12604. Epub 2014 Nov 3. https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1111/jog.12604[↩]
- Adenomyosis and risk of preterm delivery. Juang CM, Chou P, Yen MS, Twu NF, Horng HC, Hsu WL. BJOG. 2007 Feb; 114(2):165-9. https://www.ncbi.nlm.nih.gov/pubmed/17169011/[↩]
- Adenomyosis in pregnancy. A review. Azziz R. J Reprod Med. 1986 Apr; 31(4):224-7. https://www.ncbi.nlm.nih.gov/pubmed/3712359/[↩]
- Adenomyosis https://radiopaedia.org/articles/adenomyosis[↩]
- Sakhel K, Abuhamad A. Sonography of adenomyosis. J Ultrasound Med. 2012;31 (5): 805-8. https://www.ncbi.nlm.nih.gov/pubmed/22535729[↩]