Contents
What is AMH
AMH is short for antimullerian hormone, also known as mullerian-inhibiting substance, is a dimeric glycoprotein hormone produced by reproductive tissues, including the testicles in males and the ovaries in females. AMH is produced by Sertoli cells of the testis in males and by ovarian granulosa cells in developing egg sacs (follicles) in females. The role of AMH and the amount normally present varies depending upon sex and age. Because of the gender differences in AMH concentrations, its changes in circulating concentrations with sexual development, and its specificity for Sertoli and granulosa cells, measurement of AMH has utility in the assessment of gender, gonadal function, fertility, and as a gonadal tumor marker.
Women are born with their lifetime supply of eggs, and these gradually decrease in both quality and quantity with age. The level of AMH in a woman’s blood is generally a good indicator of her ovarian reserve. AMH does not change during your menstrual cycle, so the blood sample can be taken at any time of the month – even while you are using oral contraception. Since AMH is produced continuously at a relatively steady rate in the granulosa cells of growing follicles during the menstrual cycle, it is superior to the episodically released gonadotropins [follicle-stimulating hormone (FSH) and luteinizing hormone (LH)] and ovarian steroids as a marker of ovarian reserve. Furthermore, unlike other female hormones fluctuate with a woman’s monthly cycle, AMH concentrations are unaffected by pregnancy or use of oral or vaginal estrogen- or progestin-based contraceptives.
Some experts in the medical community are advocating the use of AMH as a more routine test, for predicting the end of fertility and the onset of menopause, but there is not a consensus on this use. AMH test is not considered a diagnostic or “stand-alone” test, but one that supports the diagnosis of one of the conditions mentioned (e.g., assessment of gender, gonadal function, fertility, and as a gonadal tumor marker).
AMH is important for a woman during her childbearing years. At birth, a female has about one million eggs (oocytes), which then decrease naturally in number during childhood to about 500,000. Only a tiny number of these remaining eggs will go through follicle maturation – one at a time as part of a woman’s monthly menstrual cycle. AMH has a balancing effect on the monthly cyclical actions of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) during the process of egg maturation and release (ovulation). The amount of AMH present is a reflection of this follicular growth.
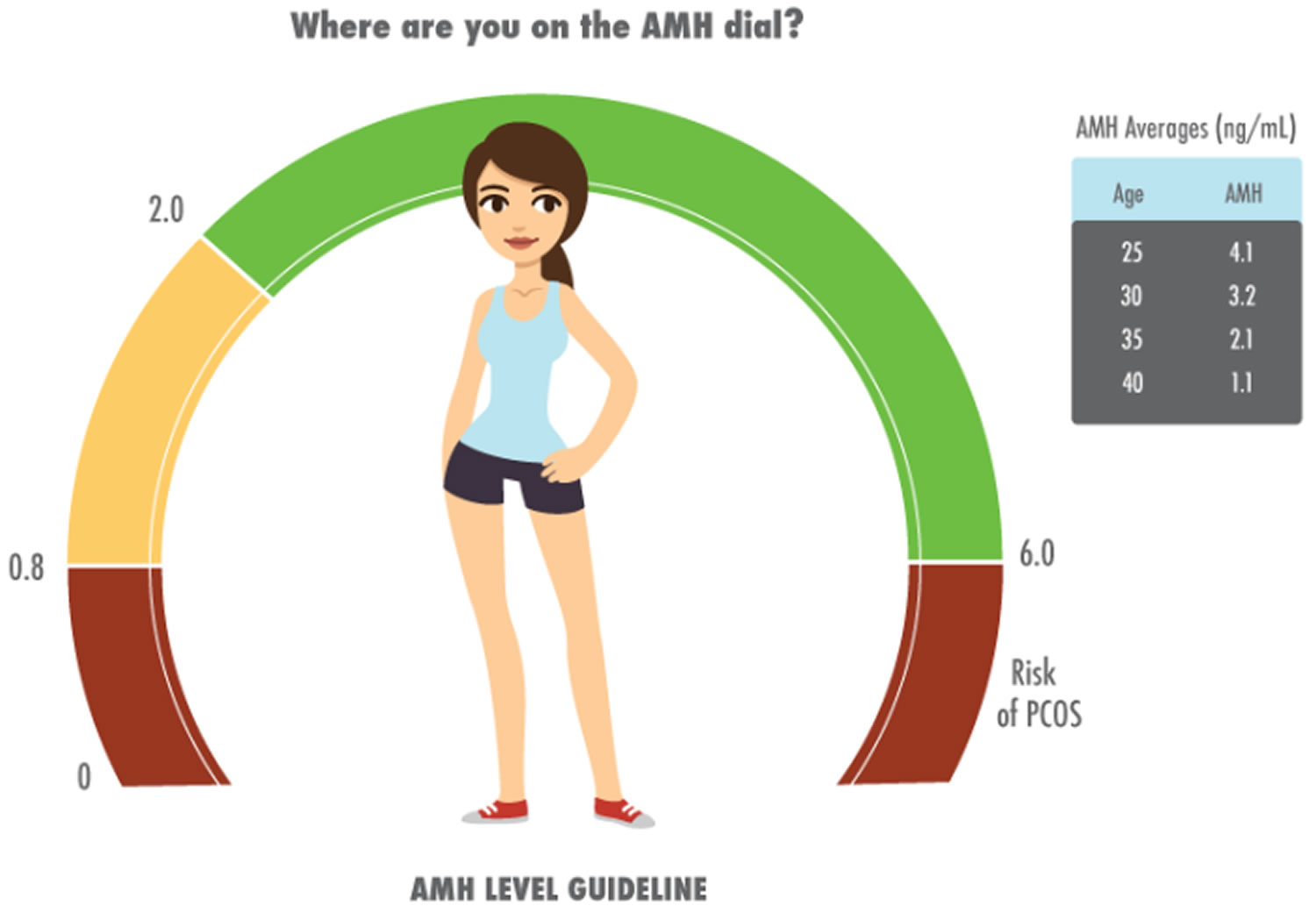
Studies in fertility clinics have shown that the AMH level may be useful in determining a woman’s remaining egg maturation potential (ovarian reserve) and her likelihood of conceiving. AMH declines over time during childbearing years, drops significantly as menopause approaches, and typically becomes almost undetectable after menopause. Determining the AMH level may be useful in evaluating a woman’s current fertility status and may predict the onset of menopause. Women with higher concentrations of AMH have a better response to ovarian stimulation and tend to produce more retrievable oocytes than women with low or undetectable AMH. Females at risk of ovarian hyperstimulation syndrome after gonadotropin administration can have significantly elevated AMH concentrations.
Elevated AMH levels have been associated with a condition affecting the ovaries known as polycystic ovarian syndrome (PCOS). The large numbers of small follicles that occur in polycystic ovarian syndrome (PCOS) produce abnormally large amounts of AMH.
AMH may be elevated in some ovarian tumors (benign or cancerous). If a tumor produces the hormone, then the AMH test can be used as a tumor marker to monitor the effectiveness of treatment and to monitor for recurrence.
AMH also plays a vital part in sexual differentiation in the fetus. During the first few weeks of pregnancy, a developing baby has the potential to develop either male or female reproductive organs. Production of AMH and androgens by the two testicles that are present in a baby boy inhibits development of female reproductive organs (the Müllerian ducts found in both male and female fetuses) and promotes the formation of other male reproductive organs. If a sufficient amount of AMH is not available or absent during this process, then both male and basic female organs may develop. A baby born with ambiguous genitalia may not be instantly recognized as either male or female.
Very early in the development of a baby boy, AMH is produced by the testicles, inhibiting the development of female reproductive organs while promoting the development of other male reproductive organs. Expression during male fetal development prevents the mullerian ducts from developing into the uterus, resulting in development of the male reproductive tract. In the absence of AMH, the mullerian ducts and structures develop into the female reproductive tract. In males, AMH serum concentrations are elevated in males under 2 years old and then progressively decrease until puberty, when there is a sharp decline.
In females, AMH is produced by the granulosa cells of small growing follicles from the 36th week of gestation onwards until menopause when levels become undetectable. In girls, low levels of AMH are produced, thus allowing the development of female reproductive structures. The AMH level in young girls remains low until puberty, when the ovaries begin to produce it and levels increase. AMH will then steadily decline in women over their reproductive years, becoming very low and eventually undetectable after menopause.
AMH measurements are commonly used to evaluate testicular presence and function in infants with intersex conditions or ambiguous genitalia, and to distinguish between cryptorchidism (testicles present but not palpable) and anorchia (testicles absent) in males. In minimally virilized phenotypic females, AMH helps differentiate between gonadal and nongonadal causes of virilization.
Serum AMH concentrations are increased in some patients with ovarian granulosa cell tumors, which comprise approximately 10% of ovarian tumors. AMH, along with related tests including inhibin A and B, estradiol, and CA-125 (Cancer Antigen 125), can be useful for diagnosing and monitoring these patients.
Should every woman of child-bearing years have an AMH test?
For most women, the AMH test is not considered necessary unless they are having fertility issues. Most women will not need to have this test performed.
Do I need an AMH test?
The AMH test is useful if:
- you have been trying to conceive for over six months, and want to check your ovarian reserve is appropriate for your age
- you are considering IVF or other fertility treatments, as low levels of AMH could indicate a potentially poor response to in-vitro fertilization (IVF). Conversely, a high level may indicate an exaggerated response to the IVF medication
- you have had chemotherapy or ovarian surgery and want to know if it has affected your future fertility
- you suspect an ovarian tumor
- you would like to conceive in the future, and just want to understand your current position
Should every male child have an AMH test?
No, testing is not routinely needed. It is only indicated when there are questions about a baby’s sexual development.
Can an AMH test be performed in my doctor’s office?
No, AMH test requires specialized equipment and must be performed in a laboratory. Your blood may need to be sent to a reference laboratory.
AMH test
Anti-Mullerian hormone (AMH) test is not a routinely ordered test but may be useful in specific circumstances.
AMH test in women
- Assessment of menopausal status, including premature ovarian failure
- Assessing ovarian status, including ovarian reserve and ovarian responsiveness, as part of an evaluation for infertility and assisted reproduction protocols such as in vitro fertilization (IVF).
- Assessing ovarian function in patients with polycystic ovarian syndrome (PCOS).
- Monitoring patients with antimullerian hormone-secreting ovarian granulosa cell tumors.
Women of childbearing age may have an AMH test ordered along with other hormone tests, such as estradiol and FSH, to estimate the remaining time left to conceive (ovarian reserve). These tests are also useful in evaluating ovarian function and possibly in predicting the onset of menopause.
AMH may sometimes be ordered for a woman who will be undergoing assisted reproduction procedures such as in vitro fertilization (IVF); the concentration of AMH present is related to her likely responsiveness to treatment. A low level of AMH reflects poor ovarian response, indicating that a decreased number of eggs would be retrieved after ovarian stimulation. For this purpose, it is typically ordered along with other hormone tests and a transvaginal ultrasound (to count the number of follicles as a reflection of the woman’s egg supply).
An AMH test may be used to evaluate polycystic ovarian syndrome (PCOS). AMH may be elevated due to the increased number of follicles present.
Some ovarian cancers produce increased levels of AMH. If the hormone is initially elevated, then the test can be used as a tumor marker to help evaluate response to treatment and monitor for recurrence.
AMH test in infants
- Evaluation of infants with ambiguous genitalia and other intersex conditions
- Evaluating testicular function in infants and children
In an infant with external genitals that are not clearly male or female (ambiguous genitalia), an AMH test may be ordered along with chromosome testing, hormone testing, and sometimes imaging scans to help determine the sex of the baby.
In an infant boy born with no visible testicles, low levels of AMH may account for the ambiguity of genitalia. If the testicles have not descended but are present in the abdomen, this test may be used to help determine whether they are functioning normally by measuring the AMH level.
When is AMH test ordered?
An AMH test may be ordered in women when evaluating ovarian function, fertility issues, especially when considering assisted reproduction procedures such as in vitro fertilization (IVF), and when a health practitioner wants to determine a woman’s likelihood of entering menopause.
AMH test may be ordered when a woman has signs and symptoms of polycystic ovarian syndrome (PCOS). Some of these include:
- Abnormal uterine bleeding
- Acanthosis nigricans
- Acne
- Absence of menstrual cycle (amenorrhea)
- Decreased breast size
- Enlarged ovaries
- Excess face and body hair (hirsutism) involving male hair growth patterns, such as hair on the face, sideburn area, chin, upper lip, lower abdominal midline, chest, areola, lower back, buttock, and inner thigh
- Weight gain/obesity, with fat distribution in center of the body
- Skin tags in the armpits or neck
- Thinning hair, with male pattern baldness
AMH may be ordered periodically for a woman with an AMH-producing ovarian cancer to monitor the effectiveness of treatment and to monitor for recurrence.
An AMH test may be ordered when an infant has ambiguous genitalia or when a male child’s testicles have not descended properly.
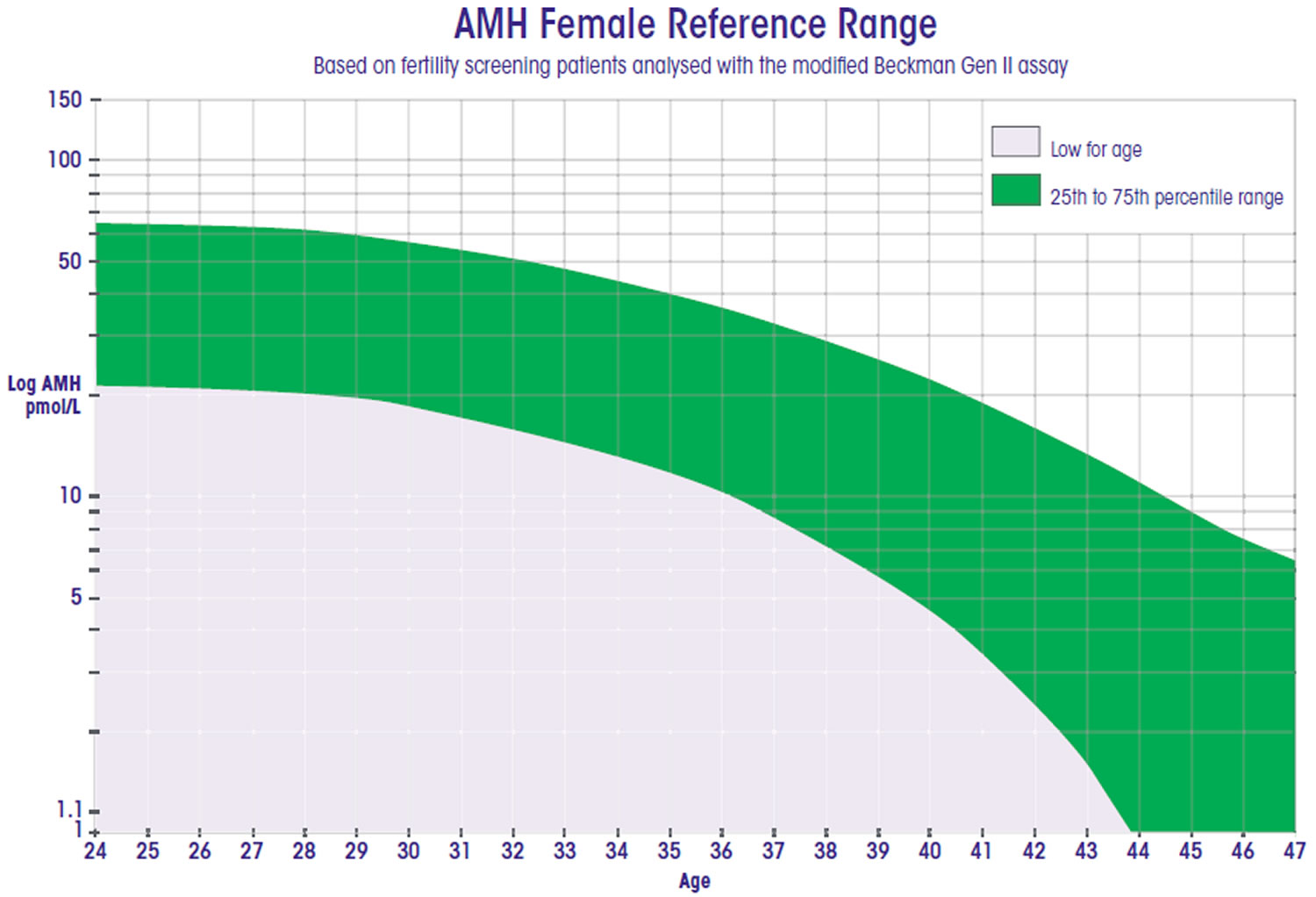
Normal AMH levels by age
Males
- Age <24 months: 14-466 ng/mL
- Age 24 months-12 years: 7.4-243 ng/mL
- Age >12 years: 0.7-19 ng/mL
Females
- Age <24 months: <4.7 ng/mL
- Age 24 months-12 years: <8.8 ng/mL
- Age 13-45 years: 0.9-9.5 ng/mL
- Age >45 years: <1.0 ng/mL
Figure 1. AMH female reference range
What does abnormal AMH blood test result mean?
Like all laboratory tests, antimullerian hormone (AMH) measurement alone is seldom sufficient for diagnosis and results should be interpreted in the light of clinical findings and other relevant test results, such as ovarian ultrasonography (antral follicle count for fertility evaluation), abdominal or testicular ultrasound (intersex and testicular function applications) and measurements of sex steroids (estradiol, testosterone, progesterone), follicle-stimulating hormone (FSH), inhibin B (for fertility), and inhibin A and B (for tumor workup).
Elevated AMH is not specific for malignancy, and the assay should not be used exclusively to diagnose or exclude an AMH-secreting ovarian tumor.
AMH assay demonstrates no cross reactivity with, Inhibin A, Inhibin B, Activin A, Activin B at concentrations of approximately 1,000 pg/mL.
As with other immunoassays, the AMH assay can be susceptible to false-low results at extremely high analyte concentrations (hooking effect).
Heterophilic antibody interferences, that are not blocked by AMH assay’s blocking regents, may also rarely occur, typically false-high results. If AMH test results are inconsistent with the clinical picture, the laboratory should be contacted.
Women
During a woman’s childbearing years, a decreased level of AMH may indicate a low number and quality of eggs (low ovarian reserve) with diminishing fertility, resulting in minimal or less responsiveness to IVF treatment. It can also indicate that the ovaries are not functioning normally (premature ovarian failure).
A decreasing level and/or significant decline in AMH may signal the imminent onset of menopause. Negative to low levels of AMH are normal in a female during infancy and after menopause.
- Menopausal women or women with premature ovarian failure of any cause, including after cancer chemotherapy, have very low antimullerian hormone (AMH) levels, often below the current assay detection limit of 0.1 ng/mL.
- While the optimal AMH concentrations for predicting response to in-vitro fertilization (IVF) are still being established, it is accepted that AMH concentrations in the perimenopausal to menopausal range indicate minimal to absent ovarian reserve. Depending on patient age, ovarian stimulation is likely to fail in such patients By contrast, if serum AMH concentrations exceed 3 ng/mL, hyper-response to ovarian stimulation may result. For these patients, a minimal stimulation would be recommended.
An increased level of AMH is often seen with PCOS but is not diagnostic of this condition. Increased AMH may also indicate an increased or even excessive responsiveness to IVF and a need to tailor the procedure accordingly.
- In patients with polycystic ovarian syndrome (PCOS), AMH concentrations may be 2- to 5-fold higher than age-appropriate reference range values. Such high levels predict anovulatory and irregular cycles.
When AMH is used as a tool to monitor an AMH-producing ovarian cancer, then a decrease in AMH indicates a response to treatment while an increase may indicate cancer recurrence.
- Granulosa cell tumors of the ovary may secrete AMH, inhibin A, and inhibin B. Elevated levels of any of these markers can indicate the presence of such a neoplasm in a woman with an ovarian mass. Levels should fall with successful treatment. Rising levels indicate tumor recurrence or progression.
Infants
In a male infant, absence or low levels of AMH may indicate a problem with the AMH gene located on chromosome 19 that directs AMH production and may be seen with absent or dysfunctional testicles. Lack of male hormones may result in ambiguous genitalia and may cause abnormal internal reproductive structures. Normal levels of AMH and androgens in a male infant whose testicles have not descended indicate that they are present and functional but not physically located where they are supposed to be.
- In children with intersex conditions, an AMH result above the normal female range is predictive of the presence of testicular tissue, while an undetectable value suggests its absence.
- In boys with cryptorchidism, a measurable AMH concentration is predictive of undescended testes, while an undetectable value is highly suggestive of anorchia (without testes) or functional failure of the abnormally sited gonad.