Contents
What is amniotic band syndrome
Amniotic band syndrome also called amniotic band sequence or ADAM (amniotic deformity, adhesions, mutilations) complex, is a rare congenital (present at birth) disorder caused by entrapment of fetal parts by fibrous amniotic bands in utero 1. Amniotic band syndrome fetal malformation ranges from mild deformities to severe anomalies incompatible with post natal life 2. The congenital anomalies seen in amniotic band syndrome vary widely and defects may be isolated or multiple and do not follow a specific pattern. Asymmetric distribution of defects is the hallmark of amniotic band syndrome. The diagnosis of amniotic band syndrome is difficult to make on ultrasound and relies on identification of amniotic bands 1.
Amniotic band syndrome is a rare, sporadic condition with an incidence of 1:1,200 to 1:15,000 live births 3. No gender or ethnic predispositions have been identified with amniotic band syndrome. In the surveillance of almost 300,000 births in a Boston hospital over many years, 40 infants (1 in 7,500) with amniotic band syndrome were identified, including several with recognized causes. Antenatal diagnosis of amniotic band syndrome is difficult because the amniotic bands may be very thin and difficult to identify on ultrasound, unless a thorough search is performed. The exact cause of amniotic band syndrome is unknown. Various causal factors hypothesized are amniocentesis, collagen vascular disease of mother, deformed uterus and drugs as cocaine and mifepristone 3. Various theories have been postulated to explain the pathogenesis. Amniotic disruption theory by Torpin et al. 4 is the most widely accepted theory. This theory suggests that amniotic band syndrome occurs when the inner membrane (amnion) ruptures before 12 weeks of gestation without injury to the outer membrane (chorion), this exposes the baby to mesoblastic fibrous sticky tissue (bands) from the ruptured amnion which can float in the waters of the uterus, these fibrous tissues can entangle the baby reducing blood supply and causing congenital abnormalities 5. In some cases a complete “natural” amputation of a digit(s) or limb may occur before birth or the digit(s) or limbs may be necrotic (dead) and require surgical amputation following birth. A strong relationship between amniotic band syndrome and clubfoot exists. A 31.5% of associated clubfoot deformity and amniotic band syndrome can be correlated with 20% occurring bilaterally. Other abnormalities found with amniotic band syndrome include: clubhands, cleft lip, and/or cleft palate, and hemangioma.
As fetus develops, the amniotic bands can trap extremities causing immobilization, constriction or amputation of structure 3. Early insult results in facial clefts and brain defects, while late insult (after 45 days gestation) results in limb involvement without facial clefting or CNS (central nervous system) involvement 5.
Van Alen 6 proposed the vascular disruption theory that states that this malformation may be caused by events that affect the blood supply to various organs during embryogenesis which may result in abnormal development of structures or damage to preformed structures. This theory has been questioned by various investigators and cannot fully explain all the abnormalities seen in this condition 7. Endogenous theory was described by Streeter in 1930, suggesting that these abnormalities were caused by imperfect histogenesis 8. However, some of the cases of amniotic band syndrome have shown geographical and temporal clustering and cannot be explained by this theory. Differences in regard to the exact cause and pathogenesis still persist.
Although ultrasound is the mainstay of prenatal imaging diagnosis of amniotic band syndrome, fetal magnetic resonance imaging is a complementary imaging modality in cases where fetal surgery is contemplated, given its large field of view and high soft tissue contrast, since it provides excellent 3-D anatomical detail of the entire pregnancy 9.
Figure 1. Amniotic band syndrome ultrasound
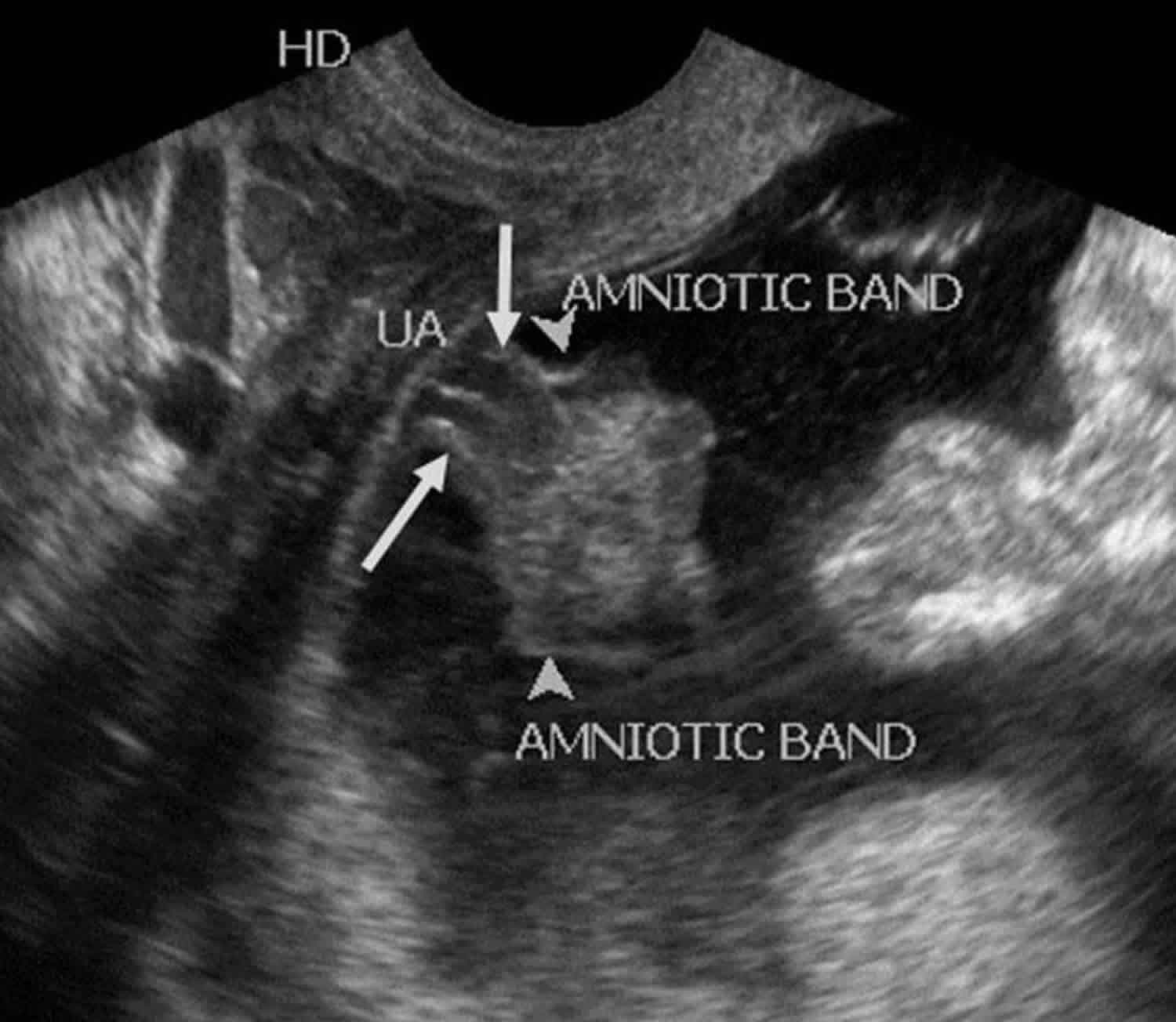
Footnote: Male fetus at 17 weeks of gestation with amniotic band syndrome. Transvaginal sonogram depicting the entrapment of the two vessel umbilical cord (white arrows) by the amniotic bands (white arrowheads). Grayscale ultrasound image of the umbilical cord proximal to its placental end demonstrates well the amniotic bands engulfing the umbilical cord and trapping it.
[Source 1 ]Amniotic band syndrome causes
What causes amniotic band syndrome is still unknown. The underlying mechanisms that cause amniotic band syndrome are complex and controversial. Several different theories have been proposed to explain the complex mechanisms that underlie amniotic band syndrome. Various causal factors hypothesized are chorionic villus sampling (CVS), collagen vascular disease of mother, deformed uterus and drugs as cocaine and misoprostol 3. One estimate of the risk for developing amniotic band syndrome was 1 in 2,000 CVS (chorionic villus sampling) procedures. It has also been reported that intense uterine contractions caused by a drug known as misoprostol (a prostaglandin E1 analogue) has resulted in amniotic band syndrome. Misoprostol is approved by the Food and Drug Administration for the treatment of gastric ulcers. However, the drug has been used to induce abortion. If the pregnancy continues after the use of misoprostol at 6 to 8 weeks of pregnancy, the infant may have the amniotic band syndrome.
The exact cause of impaired fetal blood flow as suggested by the intrinsic theory is unknown. It has been noted, also, that the amniotic band syndrome occurs with greater frequency in first pregnancies, problem pregnancies or premature births. Young women and women of African descent also have higher rates of infants with amniotic band syndrome. Research is ongoing to determine why certain populations have a greater risk of developing the disorder than other populations.
Some recent genetic studies have begun to identify intrinsic, genetic factors that may predispose infants to the development of amniotic band syndrome (genetic predisposition). A genetic predisposition to developing a disorder means that a person carries a gene, or more likely gene(s), for the disorder, but that the disorder is not expressed unless it is triggered or activated under certain circumstances such as particular environmental factors (multifactorial inheritance).
For example, a genetic predisposition to vascular disruption may contribute to the development of amniotic band syndrome in some cases. Two medical journal articles 10, 11 have discussed the possibility that genetic factors influence the development of amniotic band syndrome in certain pregnancies.
Although genetic factors are believed to play a role in the development of infants with some cases of amniotic band syndrome, the risk of recurrence in a subsequent child is extremely low. Most cases of amniotic band syndrome occur sporadically. Current, ongoing research into the potential intrinsic factors associated with amniotic band syndrome should reveal more about the complex causes and development of the disorder.
Various theories have been postulated to explain the pathogenesis. Amniotic disruption theory by Torpin et al. 4 is the most widely accepted theory. This theory suggests that amniotic band syndrome occurs when amnion ruptures before 12 weeks of gestation resulting in chorionic side of amnion emanating numerous mesoblastic fibrous strings which entrap fetal parts 5. As fetus develops, the amniotic bands can trap extremities causing immobilization, constriction or amputation of structure 3. Early insult results in facial clefts and brain defects, while late insult (after 45 days gestation) results in limb involvement without facial clefting or CNS (central nervous system) involvement 5.
Van Alen 6 proposed the vascular disruption theory that states that this malformation may be caused by events that affect the blood supply to various organs during embryogenesis which may result in abnormal development of structures or damage to preformed structures. This theory has been questioned by various investigators and cannot fully explain all the abnormalities seen in this condition 7. Endogenous theory was described by Streeter in 1930, suggesting that these abnormalities were caused by imperfect histogenesis 8. However, some of the cases of amniotic band syndrome have shown geographical and temporal clustering and cannot be explained by this theory. Differences in regard to the exact cause and pathogenesis still persist.
How to prevent amniotic band syndrome
Because the exact cause of amniotic band syndrome is still unknown, currently there is no way to prevent it. However, various causal factors have been hypothesized to cause amniotic band syndrome and they are chorionic villus sampling (CVS), collagen vascular disease of mother, deformed uterus and drugs as cocaine and misoprostol 3. One estimate of the risk for developing amniotic band syndrome was 1 in 2,000 CVS (chorionic villus sampling) procedures. It has also been reported that intense uterine contractions caused by a drug known as misoprostol (a prostaglandin E1 analogue) has resulted in amniotic band syndrome. Misoprostol is approved by the Food and Drug Administration for the treatment of gastric ulcers. However, the drug has been used to induce abortion. If the pregnancy continues after the use of misoprostol at 6 to 8 weeks of pregnancy, the infant may have the amniotic band syndrome.
Damage to the amniotic sac has been implicated as a cause of amniotic band syndrome under the extrinsic theory. The exact reason that the amniotic sac tears or ruptures is not always known and researchers believe that in some cases it may happen as a random occurrence. In some infants, trauma to the abdominal area during pregnancy or blunt trauma to the placenta seemed to have caused the amniotic band syndrome.
Some recent genetic studies have begun to identify intrinsic, genetic factors that may predispose infants to the development of amniotic band syndrome (genetic predisposition). A genetic predisposition to developing a disorder means that a person carries a gene, or more likely gene(s), for the disorder, but that the disorder is not expressed unless it is triggered or activated under certain circumstances such as particular environmental factors (multifactorial inheritance).
For example, a genetic predisposition to vascular disruption may contribute to the development of amniotic band syndrome in some cases. Two medical journal articles 11, 10 have discussed the possibility that genetic factors influence the development of amniotic band syndrome in certain pregnancies.
Although genetic factors are believed to play a role in the development of infants with some cases of amniotic band syndrome, the risk of recurrence in a subsequent child is extremely low. Most cases of amniotic band syndrome occur sporadically. Current, ongoing research into the potential intrinsic factors associated with amniotic band syndrome should reveal more about the complex causes and development of the disorder.
Amniotic band syndrome symptoms
The symptoms associated with amniotic band syndrome vary greatly from one infant to another and depend on the severity and location of the constrictions and no two cases are identical 1. Some infants develop only mild deformities; others develop severe and even life-threatening malformations. It seems likely that the features of amniotic band syndrome develop primarily in the first 12 weeks (first trimester) of pregnancy 12.
Fetal malformations encountered in amniotic band syndrome broadly fall into three main categories 13:
- Limb defects,
- Craniofacial defects (abnormalities of the head and face), and
- Visceral defects.
Most infants with amniotic band syndrome have some form of deformity of the arms and legs or fingers and toes. One or more limbs may be affected. Upper limbs are affected more often than lower limbs. In some patients, one limb or one hand or foot may be the only symptom of the disorder. The specific physical features can include abnormally short fingers or toes with absence of the end (distal) portion, webbing (fusion) of fingers or toes (syndactyly), constriction rings and extra strands of tissue adhering to the fingers. The constriction rings that encircle a limb or digit can alter blood flow.
Another pattern associated with amniotic band syndrome is referred to as the limb-body wall complex, a lethal condition. Affected infants usually have protrusion of a portion of the brain and its surrounding membranes (meninges) through the skull defect (encephalocele), facial clefts, protrusion of the viscera (the soft internal organs of the body including those found in the abdominal or chest cavities) through a fissure in the abdominal wall (abdominoschisis) or the chest wall (thoracoschisis), and a variety of defects affecting the arms and legs.
A third pattern associated with amniotic band syndrome involves craniofacial abnormalities such as incomplete closure of the roof of the mouth (cleft palate), facial clefts, small, underdeveloped eyes (microphthalmia), narrowing of the nasal passages (choanal atresia), and malformations affecting the size and shape of the skull. In some infants, the head is adherent to the placenta.
The mildest constrictions affect only the superficial skin and may not require treatment. Deeper constrictions may block lymphatic vessels, impair blood flow, and require immediate surgical care 14. When the bands affect the limbs, the lower part of the limbs are most often involved, especially the middle, long, and index fingers of the hand. When the feet are involved, the bands most commonly affect the big toe 14.
Pressure from the bands may result in additional abnormalities, such as underdevelopment of a limb, bone abnormalities, amputations, leg-length discrepancy, and club feet. Constriction bands across the head and face may lead to facial clefts. Severe clefts affecting vital organs are often life-threatening 14.
In one case, the fetus had multiple amniotic bands with visceral and limb anomalies and a short umbilical cord with single umbilical artery. Short umbilical cord is a common finding in amniotic band syndrome, possibly due to limited fetal movements and available fetal space 15. Short cord has not been reported in early aborted cases of the amniotic band syndrome, suggesting it is a secondary feature 15. A normal umbilical cord has two umbilical arteries and one umbilical vein, surrounded by Wharton’s Jelly 16. Umbilical cord with only single umbilical artery is associated with increased risk of renal and cardiovascular anomalies. A less common association of single umbilical artery has been described in cases of amniotic band syndrome 15. A topographic correlation of the presence of single umbilical artery has been suggested with regional location of amniotic adhesions in amniotic band syndrome 15. In their study of 48 cases, Belinda et al. reported the presence of finding of single umbilical artery in 64% cases of amniotic band syndrome with caudal adhesions and caudal malformations, however single umbilical artery was not seen in any case of pure cephalo-thoracic malformations 15. A proposed mechanism for this specifically regional association of single umbilical artery with caudal adhesions is the exposure of umbilical cord in the absence of a covering abdominal wall resulting in disruption of one umbilical artery 15.
Amniotic band syndrome diagnosis
Amniotic band syndrome is typically diagnosed at or soon after birth based upon characteristic physical findings. The minimal diagnostic criteria consist of the detection of certain abnormalities of the arms, legs, fingers, and/or toes, i.e., ring-like constriction or amputation defects, fusion (syndactyly) between some digits and/or strands of tissue attached to the ends of affected fingers.
In some cases, the condition may be suspected before birth (prenatally), based upon the results of certain specialized imaging techniques, such as fetal ultrasonography, which may reveal the characteristic defects. During fetal ultrasonography, reflected high-frequency sound waves are used to create an image of the developing fetus.
Amniotic band syndrome treatment
The treatment of infants and children with amniotic band syndrome is symptomatic and supportive. For example, in infants with incomplete development of the lungs and associated respiratory insufficiency, treatment may include oxygen support measures and other supportive therapies as required. Reconstructive surgery or other surgical techniques may be recommended to help correct or repair associated malformations, such as ring-like constrictions of the limbs, webbed fingers and toes, cleft lip or club foot. Physical and occupational therapy may also be necessary to ensure infants can attain the optimal use of affected fingers, toes, arms and legs.
In rare cases, surgery may be performed before birth (fetal surgery) to cut amniotic bands that are tightly constricting and may cause loss of a limb or digit. In-utero surgical correction may be attempted if there is threatened limb amputation or constriction of the umbilical cord. Fetoscopic laser release of amniotic bands has been successfully performed for threatened limb amputation 17. In less severe cases with digital abnormalities, cleft lip or cleft palate, surgical correction can be performed after birth. Extensive abnormalities detected on antenatal ultrasound entail parental counselling and termination of pregnancy.
Amniotic band syndrome prognosis
Prognosis depends on the degree of malformation and location and severity of the constricting bands. There is an increased risk of premature rupture of membranes, prematurity and low birth weight. Bands encircling the head and the umbilical cord can be concerning for fetal demise, with umbilical cord constriction by amniotic bands seen in 10% of cases 18. Entrapment of the umbilical cord may be a precursor to cord strangulation and subsequent derangement of vascular supply to the fetus resulting in fetal demise 19. Therefore, in a case with unusual distribution of fetal defects, careful evaluation for amniotic bands should be done. It is also critical to evaluate the entire length of umbilical cord for entrapment and use color Doppler for evaluation of blood supply to the fetus in these cases.
Because the prognosis of people with amniotic band syndrome can vary from patient to patient, the best person to provide your family with information regarding your child’s prognosis, is your health care providers involved in their care. In general, the outlook for infants with a single band involving the superficial skin of the wrist and/or hand is good. While the family and child will need to adjust to the cosmetic difference, the functional use of the hand is normal. Deeper bands can be associated with complications (i.e., blockage of lymph and blood vessels) that can worsen over time and may require surgery. Some people with amniotic band syndrome are born with acrosyndactyly, a fusion of the fingers that may limit the hand function and cause stiffness of the joints. In many cases a good ability to hold and grasp may be obtained with reconstructive procedures 14.
- Gupta K, Venkatesan B, Chandra T, Rajeswari K, Devi TK. Amniotic band syndrome with sacral agenesis and umbilical cord entrapment: A case report emphasizing the value of evaluation of umbilical cord. J Radiol Case Rep. 2015;9(3):12–19. Published 2015 Mar 31. doi:10.3941/jrcr.v9i3.2115 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4395011[↩][↩][↩][↩]
- Sonographic diagnosis of the amniotic band syndrome. Burton DJ, Filly RA. AJR Am J Roentgenol. 1991 Mar; 156(3):555-8.[↩]
- Cignini P, Giorlandino C, Padula F, et al. Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. J Prenat Med. 2012 Oct;6(4):59–63[↩][↩][↩][↩][↩][↩]
- Torpin R. Amniochorionic mesoblastic fibrous strings and amnionic bands: associated constricting fetal malformations or fetal death. Am J Obstet Gynecol. 1965;91:65–75[↩][↩]
- Peterside Oliemen, Omietimi James E, Adeyemi Oyedeji O. Amniotic band syndrome: a report of two cases and review of the literature. IOSR Journal of Dental and Medical Sciences. 2013 Mar-Apr;5[↩][↩][↩][↩]
- Van Allen MI. Fetal vascular disruptions: mechanisms and some resulting birth defects. Pediatr Ann. 1981 Jun;10(6):219–33[↩][↩]
- Werler MM, Bosco JL, Shapira SK. National Birth Defects Prevention Study. Maternal vasoactive exposures, amniotic bands, and terminal transverse limb defects. Birth Defects Res A Clin Mol Teratol. 2009 Jan;85(1):52–7[↩][↩]
- Streeter GL. Focal deficiencies in fetal tissues and their relation to intrauterine amputations. Contrib Embryol Carnegie Inst. 1930;22:1–44[↩][↩]
- Neuman J, Calvo-Garcia MA, Kline-Fath BM, Bitters C, Merrow AC, Guimaraes CV, Lim FY. Prenatal imaging of amniotic band sequence: utility and role of fetal MRI as an adjunct to prenatal US. Pediatr Radiol. 2012 May;42(5):544–51.[↩]
- Hunter AG. A pilot study of the possible role of familial defects in anticoagulation as a cause for terminal limb reduction malformations. Clin Genet. 2000;57:197-204.[↩][↩]
- Carmichael SL, Shaw GM, Iovannisci DM, et al. Risks of human limb deficiency anomalies associated with 29 SNPs of genes involved in homocysteine metabolism, coagulation, cell-cell interactions, inflammatory response, and blood pressure response, and blood pressure regulation. Am J Med Genet A. 2006;140:2433-2440.[↩][↩]
- Amniotic band syndrome. https://rarediseases.org/rare-diseases/amniotic-band-syndrome/[↩]
- Burton DJ, Filly RA. Sonographic diagnosis of the amniotic band syndrome. AJR Am J Roentgenol. 1991 Mar;156(3):555–8[↩]
- Amniotic Band Syndrome (Streeter Dysplasia). https://emedicine.medscape.com/article/1260337-overview[↩][↩][↩][↩]
- Davies BR, Giménez-Scherer JA, Hernández-Sierra JF. Fetal amniotic adhesions. Their topographic concordance with regionally clustered malformations. Arch Med Res. 2001 Jan-Feb;32(1):48–61[↩][↩][↩][↩][↩][↩]
- De Laat MW, Franx A, van Alderen ED, Nikkels PG, Visser GH. The umbilical coiling index, a review of the literature. J Matern Fetal Neonatal Med. 2005 Feb;17(2):93–100. Review[↩]
- Keswani SG, Johnson MP, Adzick NS, et al. In utero limb salvage: fetoscopic release of amniotic bands for threatened limb amputation. J Pediatr Surg. 2003 Jun;38(6):848–51.[↩]
- Neuman J, Calvo-Garcia MA, Kline-Fath BM, Bitters C, Merrow AC, Guimaraes CV, Lim FY. Prenatal imaging of amniotic band sequence: utility and role of fetal MRI as an adjunct to prenatal US. Pediatr Radiol. 2012 May;42(5):544–51[↩]
- Lurie S, Feinstein M, Mamet Y. Umbilical cord strangulation by an amniotic band resulting in a stillbirth. J Obstet Gynaecol Res. 2008 Apr;34(2):255–7[↩]





