What is the aorta
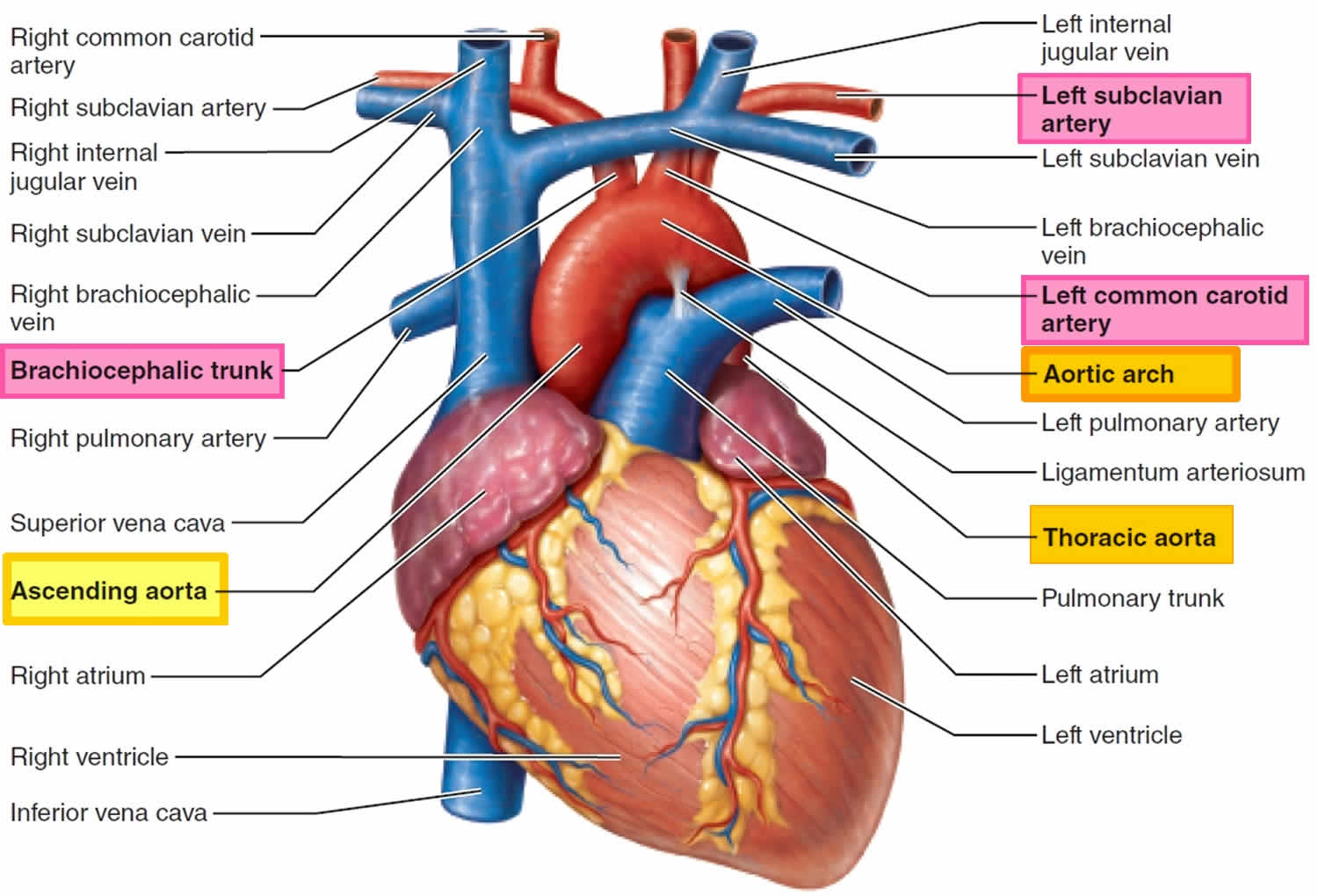
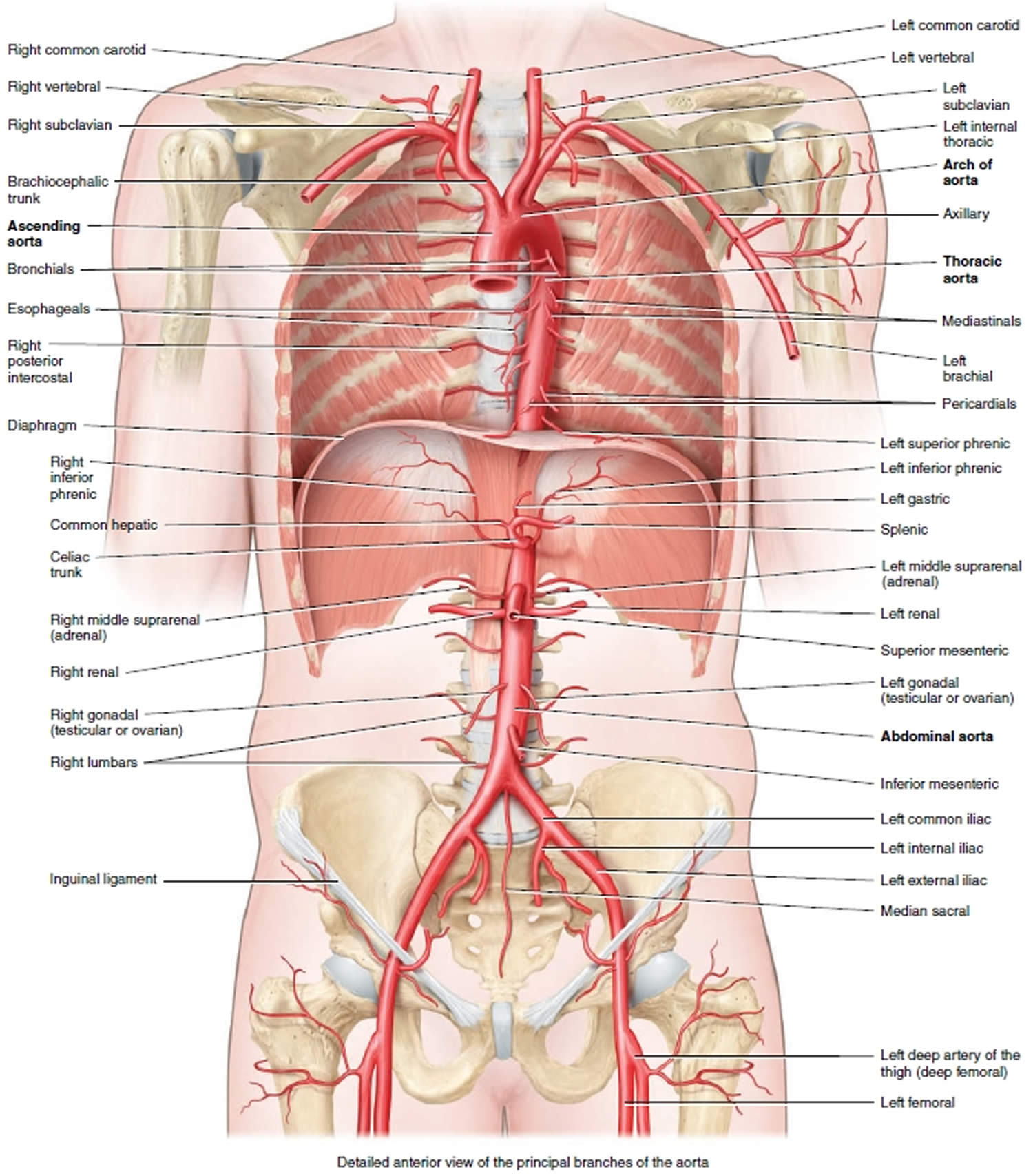
The aorta is the largest artery in your body with a diameter of 2–3 cm (about 1 in.). The aorta four principal divisions are the ascending aorta, arch of the aorta, thoracic aorta, and abdominal aorta (Figures 1 and 2). The portion of the aorta that emerges from the left ventricle posterior to the pulmonary trunk is the ascending aorta (see Figure 1). The beginning of the aorta contains the aortic valve, leaves the heart, arcs superiorly and then descends along the bodies of the vertebrae to the inferior part of the abdomen (see Figure 2). Along this course, the aorta is divided into the following three parts.
Ascending Aorta
The ascending aorta (Figure 1), one of the great vessels leaving the heart, arises from the left ventricle and ascends for only about 5 cm. It begins posterior to the pulmonary trunk, passes to the right of that vessel, and then curves left to become the aortic arch. The only branches of the ascending aorta are the right and left coronary arteries that supply the myocardium of the heart. Then the ascending aorta arches to the left, forming the arch of the aorta, which descends and ends at the level of the intervertebral disc between the fourth and fifth thoracic vertebrae.
Aortic Arch
Arching posteriorly and to the left, the aortic arch lies posterior to the manubrium of the sternum. The ligamentum arteriosum, a fibrous remnant of a fetal artery called the ductus arteriosus, connects the aortic arch and the pulmonary trunk (Figure 1).
Aorta branches
Three arteries branch from the aortic arch and run superiorly (Figure 1).
- The first and largest branch is the brachiocephalic trunk. The brachiocephalic trunk ascends to the right toward the base of the neck where it divides into the right common carotid artery and the right subclavian artery.
- The second branch of the aortic arch is the left common carotid artery.
- The third branch is the left subclavian artery.
These three branches of the aorta supply the head and neck, upper limbs, and the superior part of the thoracic wall. Note that the brachiocephalic trunk on the right has no corresponding artery on the left because the left common carotid and subclavian arteries arise directly from the aorta.
This is the typical branching pattern of these vessels off the aortic arch; however, as with all vessels, there is some variability from this pattern. The most frequent variation is the branching of the left common carotid artery from the brachiocephalic trunk. Less commonly, four large arteries (the right and left common carotids, and the right and left subclavian arteries) arise separately from the aortic arch, or the left common carotid artery and the left subclavian artery arise from a left brachiocephalic trunk.
Figure 1. Aorta and aortic arch branches
Descending Aorta
Continuing from the aortic arch, the descending aorta runs posterior to the heart and continues to descend close to the bodies of the thoracic and lumbar vertebrae. It has two parts, the thoracic aorta and the abdominal aorta.
The thoracic aorta (Figure 1) descends on the bodies of the thoracic vertebrae (T5–T12) just to the left of the midline. Along the way, it sends many small branches to the thoracic organs and body wall.
When the thoracic aorta reaches the bottom of the thorax it passes through the aortic hiatus of the diaphragm at the level of vertebra T12 and enters the abdominal cavity to become the abdominal aorta. The abdominal aorta lies on the lumbar vertebral bodies in the midline. The abdominal aorta ends at the level of vertebra L4, where it divides into two common iliac arteries, the right and left common iliac arteries, which carry blood to the pelvis and lower limbs.
Each division of the aorta gives off arteries that branch into distributing arteries that lead to various organs. Within the organs, the arteries divide into arterioles and then into capillaries that service the systemic tissues (all tissues except the alveoli of the lungs).
Table 1. Aorta and aorta branches
| DIVISION AND BRANCHES | REGION SUPPLIED |
ASCENDING AORTA
| Heart |
| ARCH OF THE AORTA | |
| Right side of head and neck. Right upper limb |
| Left side of head and neck. |
| Left upper limb. |
| THORACIC AORTA (CHEST) | |
| Pericardium. |
| Bronchi of lungs. |
| Esophagus. |
| Structures in mediastinum. |
| Intercostal and chest muscles. |
| Upper abdominal muscles. |
| Superior and posterior surfaces of diaphragm. |
| ABDOMINAL AORTA | |
| Inferior surface of diaphragm. |
| Abdominal muscles. |
| Celiac trunk | |
| Liver, stomach, duodenum, and pancreas. |
| Stomach and esophagus. |
| Spleen, pancreas, and stomach. |
| Superior mesenteric artery | Small intestine, cecum, ascending and transverse colons, and pancreas. |
| Suprarenal arteries | Adrenal (suprarenal) glands. |
| Renal arteries | Kidneys. |
| Gonadal arteries | |
| Testes (male). |
| Ovaries (female). |
| Inferior mesenteric artery | Transverse, descending, and sigmoid colons; rectum. |
| Common iliac arteries | |
| Lower limbs. |
| Uterus (female), prostate (male), muscles of buttocks, and urinary bladder |
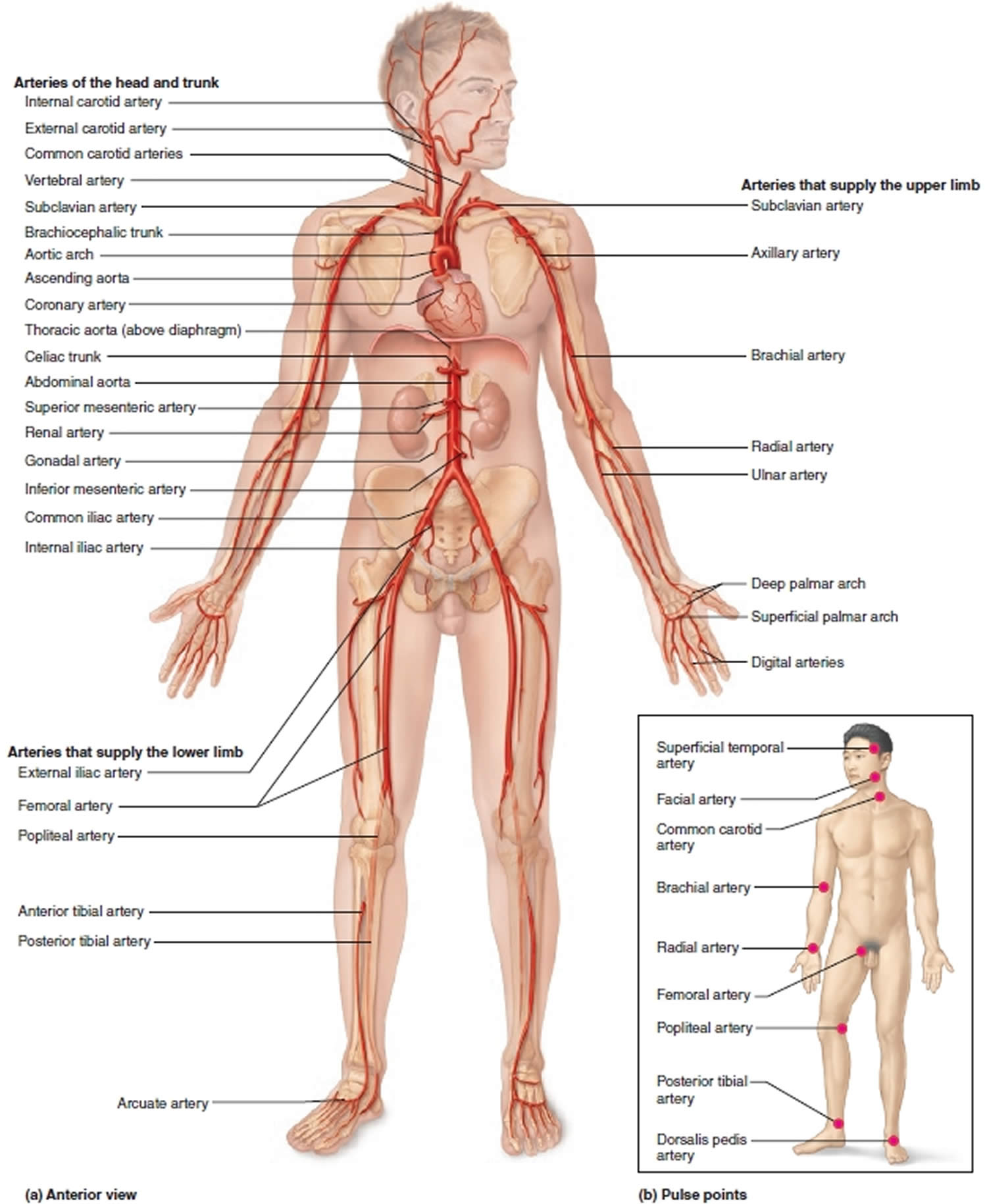
Aorta function
The aorta carries oxygenated blood from your heart to the organs throughout your body. The elastin in the walls of these arteries maintains the pulsatile flow. Arterial pulses can be palpated in the muscular arteries at numerous body locations (Figure 2B) and can be used to determine heart rate and to assess blood flow to a body region after trauma, surgery, or disease. Deep pressure at a pulse point is a first aid technique used to limit blood flow through a vessel that is hemorrhaging and thus limit blood loss.
Aorta problems
Dilated aorta
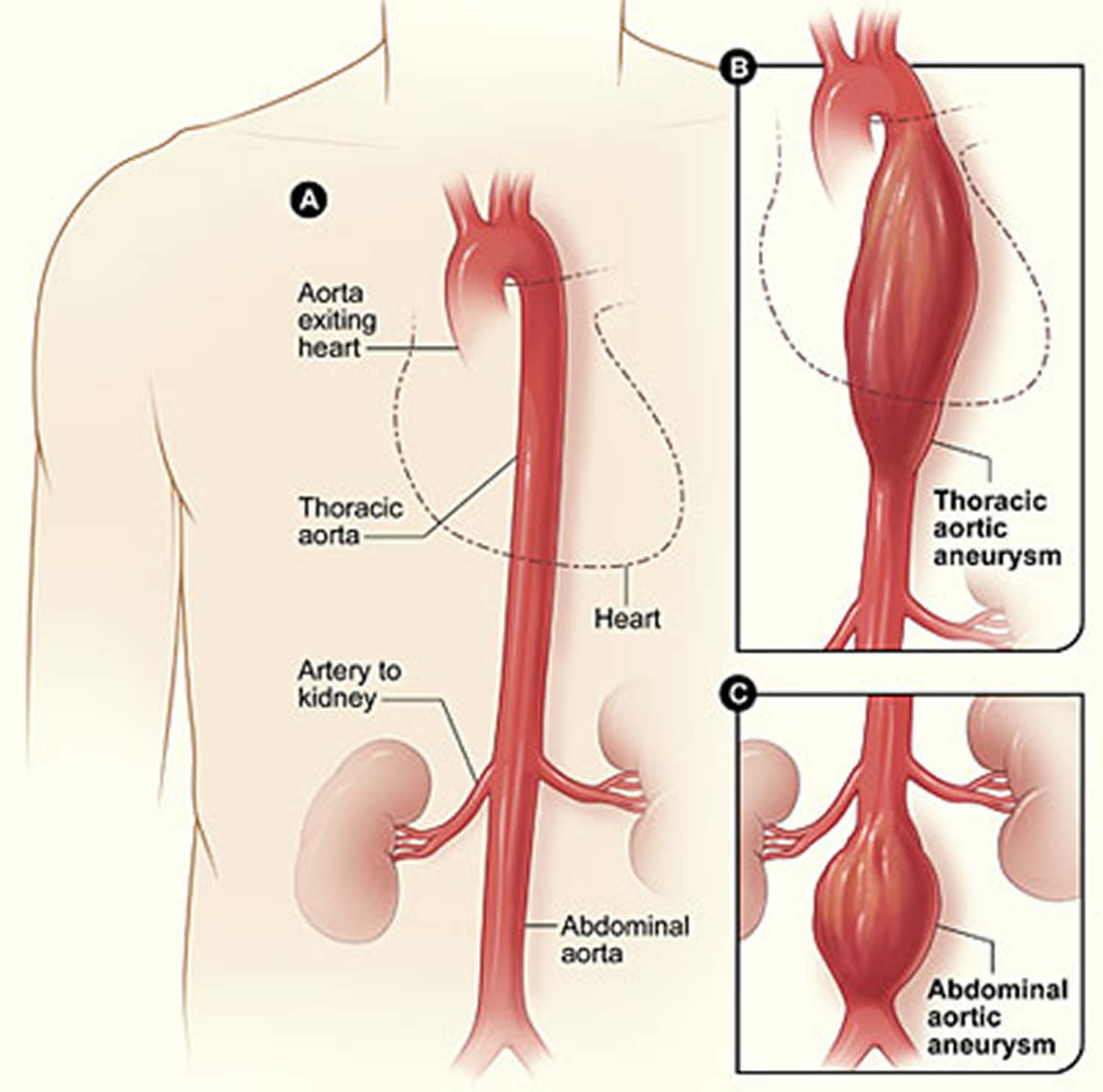
Dilated or enlarged aorta is also called aortic anurysm. An aneurysm is a bulge or “ballooning” in the wall of an artery. Arteries have thick walls to withstand normal blood pressure. However, certain medical problems, genetic conditions, and trauma can damage or injure artery walls. The force of blood pushing against the weakened or injured walls can cause an aneurysm.
An aneurysm can grow large and rupture (burst) or dissect. A rupture causes dangerous bleeding inside your body or even death. A dissection is a split in one or more layers of the artery wall. The split causes bleeding into and along the layers of the artery wall. Both rupture and dissection often are fatal.
About 13,000 Americans die each year from aortic aneurysms. Most of the deaths result from rupture or dissection 1.
Early diagnosis and treatment can help prevent rupture and dissection. However, aneurysms can develop and grow large before causing any symptoms. Thus, people who are at high risk for aneurysms can benefit from early, routine screening.
Most aneurysms are in the aorta, the main artery that runs from the heart through the chest and abdomen.
There are two types of aortic aneurysm:
- Thoracic aortic aneurysms (TAA) – these occur in the part of the aorta running through the chest (thoracic aortic aneurysm). Thoracic aortic aneurysms don’t always cause symptoms, even when they’re large. Only half of all people who have thoracic aortic aneurysms notice any symptoms. thoracic aortic aneurysms are found more often now than in the past because of chest CT scans done for other medical problems. With a common type of thoracic aortic aneurysm, the walls of the aorta weaken and a section close to the heart enlarges. As a result, the valve between the heart and the aorta can’t close properly. This allows blood to leak back into the heart. A less common type of thoracic aortic aneurysm (TAA) can develop in the upper back, away from the heart. A thoracic aortic aneurysm in this location may result from an injury to the chest, such as from a car crash.
- Abdominal aortic aneurysms (AAA) – these occur in the part of the aorta running through the abdomen (abdominal aortic aneurysm). Most aortic aneurysms are abdominal aortic aneurysms. Abdominal aortic aneurysms (AAA) are found more often now than in the past because of computed tomography scans (CT scans), done for other medical problems. Small abdominal aortic aneurysms rarely rupture. However, abdominal aortic aneurysms can grow very large without causing symptoms. Routine checkups and treatment for an abdominal aortic aneurysm can help prevent growth and rupture.
Figure 3. Aortic aneurysms
Most aneurysms are found during tests done for other reasons. Some people are at high risk for aneurysms. It is important for them to get screening, because aneurysms can develop and become large before causing any symptoms. Screening is recommended for people between the ages of 65 and 75 if they have a family history, or if they are men who have smoked. Doctors use imaging tests to find aneurysms. Medicines and surgery are the two main treatments.
Aneurysms along the aortic arch often develop slowly over many years with little or no symptoms, and are usually detected when medical imaging is conducted for unrelated reasons. Some patients experience chest pain, fast pulse, fatigue or shortness of breath. There may also be a marked difference in blood pressure measured in the arms and legs. Should these symptoms occur, it is important to seek urgent medical attention, particularly to rule out aortic dissection, which is life-threatening and demands immediate surgery.
Doctors often can successfully treat aortic aneurysms with medicines or surgery if they’re found in time. Medicines may be given to lower blood pressure, relax blood vessels, and reduce the risk of rupture.
Large aortic aneurysms often can be repaired with surgery. During surgery, the weak or damaged portion of the aorta is replaced or reinforced.
Aortic aneurysm causes
The force of blood pushing against the walls of an artery combined with damage or injury to the artery’s walls can cause an aneurysm.
Many conditions and factors can damage and weaken the walls of the aorta and cause aortic aneurysms. Examples include aging, smoking, high blood pressure, and atherosclerosis. Atherosclerosis is the hardening and narrowing of the arteries due to the buildup of a waxy substance called plaque.
Rarely, infections—such as untreated syphilis (a sexually transmitted infection)—can cause aortic aneurysms. Aortic aneurysms also can occur as a result of diseases that inflame the blood vessels, such as vasculitis.
A family history of aneurysms also may play a role in causing aortic aneurysms.
In addition to the factors above, certain genetic conditions may cause thoracic aortic aneurysms (TAAs). Examples of these conditions include Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome (the vascular type), and Turner syndrome.
These genetic conditions can weaken the body’s connective tissues and damage the aorta. People who have these conditions tend to develop aneurysms at a younger age than other people. They’re also at higher risk for rupture and dissection.
Trauma, such as a car accident, also can damage the walls of the aorta and lead to thoracic aortic aneurysms (TAAs).
Researchers continue to look for other causes of aortic aneurysms. For example, they’re looking for genetic mutations (changes in the genes) that may contribute to or cause aneurysms.
Risk factors for developing aortic aneurysm
Certain factors put you at higher risk for an aortic aneurysm. These factors include:
- Male gender. Men are more likely than women to have aortic aneurysms.
- Age. The risk for abdominal aortic aneurysms increases as you get older. These aneurysms are more likely to occur in people who are aged 65 or older.
- Smoking. Smoking can damage and weaken the walls of the aorta.
- A family history of aortic aneurysms. People who have family histories of aortic aneurysms are at higher risk for the condition, and they may have aneurysms before the age of 65.
- A history of aneurysms in the arteries of the legs.
- Certain diseases and conditions that weaken the walls of the aorta. Examples include high blood pressure and atherosclerosis.
Having a bicuspid aortic valve can raise the risk of having a thoracic aortic aneurysm. A bicuspid aortic valve has two leaflets instead of the typical three.
Car accidents or trauma also can injure the arteries and increase the risk for aneurysms.
If you have any of these risk factors, talk with your doctor about whether you need screening for aneurysms.
Aortic aneurysm screening and prevention
The best way to prevent an aortic aneurysm is to avoid the factors that put you at higher risk for one. You can’t control all aortic aneurysm risk factors, but lifestyle changes can help you lower some risks.
For example, if you smoke, try to quit. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
Another important lifestyle change is following a healthy diet. A healthy diet includes a variety of fruits, vegetables, and whole grains. It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugar.
Be as physically active as you can. Talk with your doctor about the amounts and types of physical activity that are safe for you.
Work with your doctor to control medical conditions such as high blood pressure and high blood cholesterol. Follow your treatment plans and take all of your medicines as your doctor prescribes.
Screening for aortic aneurysms
Although you may not be able to prevent an aneurysm, early diagnosis and treatment can help prevent rupture and dissection.
Aneurysms can develop and grow large before causing any signs or symptoms. Thus, people who are at high risk for aneurysms may benefit from early, routine screening.
Your doctor may recommend routine screening if you’re:
- A man between the ages of 65 and 75 who has ever smoked
- A man or woman between the ages of 65 and 75 who has a family history of aneurysms
If you’re at risk, but not in one of these high-risk groups, ask your doctor whether screening will benefit you.
Aortic aneurysm signs and symptoms
The signs and symptoms of an aortic aneurysm depend on the type and location of the aneurysm. Signs and symptoms also depend on whether the aneurysm has ruptured (burst) or is affecting other parts of the body.
Aneurysms can develop and grow for years without causing any signs or symptoms. They often don’t cause signs or symptoms until they rupture, grow large enough to press on nearby body parts, or block blood flow.
Abdominal Aortic Aneurysms
Most abdominal aortic aneurysms (AAAs) develop slowly over years. They often don’t cause signs or symptoms unless they rupture. If you have an AAA, your doctor may feel a throbbing mass while checking your abdomen.
When symptoms are present, they can include:
- A throbbing feeling in the abdomen
- Deep pain in your back or the side of your abdomen
- Steady, gnawing pain in your abdomen that lasts for hours or days
If an abdominal aortic aneurysm ruptures, symptoms may include sudden, severe pain in your lower abdomen and back; nausea (feeling sick to your stomach) and vomiting; constipation and problems with urination; clammy, sweaty skin; light-headedness; and a rapid heart rate when standing up.
Internal bleeding from a ruptured abdominal aortic aneurysm can send you into shock. Shock is a life-threatening condition in which blood pressure drops so low that the brain, kidneys, and other vital organs can’t get enough blood to work well. Shock can be fatal if it’s not treated right away.
Thoracic Aortic Aneurysms
A thoracic aortic aneurysm (TAA) may not cause symptoms until it dissects or grows large. If you have symptoms, they may include:
- Pain in your jaw, neck, back, or chest
- Coughing and/or hoarseness
- Shortness of breath and/or trouble breathing or swallowing
A dissection is a split in one or more layers of the artery wall. The split causes bleeding into and along the layers of the artery wall.
If a thoracic aortic aneurysm ruptures or dissects, you may feel sudden, severe, sharp or stabbing pain starting in your upper back and moving down into your abdomen. You may have pain in your chest and arms, and you can quickly go into shock.
If you have any symptoms of thoracic aortic aneurysm or aortic dissection, call your local emergency services number for an ambulance. If left untreated, these conditions may lead to organ damage or death.
Aortic aneurysm diagnosis
If you have an aortic aneurysm but no symptoms, your doctor may find it by chance during a routine physical exam. More often, doctors find aneurysms during tests done for other reasons, such as chest or abdominal pain.
If you have an abdominal aortic aneurysm (AAA), your doctor may feel a throbbing mass in your abdomen. A rapidly growing aneurysm about to rupture (burst) can be tender and very painful when pressed. If you’re overweight or obese, it may be hard for your doctor to feel even a large abdominal aortic aneurysm.
If you have an abdominal aortic aneurysm, your doctor may hear rushing blood flow instead of the normal whooshing sound when listening to your abdomen with a stethoscope.
Specialists involved
Your primary care doctor may refer you to a cardiothoracic or vascular surgeon for diagnosis and treatment of an aortic aneurysm.
A cardiothoracic surgeon does surgery on the heart, lungs, and other organs and structures in the chest, including the aorta. A vascular surgeon does surgery on the aorta and other blood vessels, except those of the heart and brain.
Diagnostic Tests and Procedures
To diagnose and study an aneurysm, your doctor may recommend one or more of the following tests.
Ultrasound and Echocardiography
Ultrasound and echocardiography (echo) are simple, painless tests that use sound waves to create pictures of the structures inside your body. These tests can show the size of an aortic aneurysm, if one is found.
Computed Tomography Scan
A computed tomography scan (CT scan), is a painless test that uses x rays to take clear, detailed pictures of your organs.
During the test, your doctor will inject dye into a vein in your arm. The dye makes your arteries, including your aorta, visible on the CT scan pictures.
Your doctor may recommend this test if he or she thinks you have an abdominal aortic aneurysm or a thoracic aortic aneurysm (TAA). A CT scan can show the size and shape of an aneurysm. This test provides more detailed pictures than an ultrasound or echo.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) uses magnets and radio waves to create pictures of the organs and structures in your body. This test works well for detecting aneurysms and pinpointing their size and exact location.
Angiography
Angiography is a test that uses dye and special x rays to show the insides of your arteries. This test shows the amount of damage and blockage in blood vessels.
Aortic angiography shows the inside of your aorta. The test may show the location and size of an aortic aneurysm.
Aortic Aneurysm Treatment
Aortic aneurysms are treated with medicines and surgery. Small aneurysms that are found early and aren’t causing symptoms may not need treatment. Other aneurysms need to be treated.
The goals of treatment may include:
- Preventing the aneurysm from growing
- Preventing or reversing damage to other body structures
- Preventing or treating a rupture or dissection
- Allowing you to continue doing your normal daily activities
Treatment for an aortic aneurysm is based on its size. Your doctor may recommend routine testing to make sure an aneurysm isn’t getting bigger. This method usually is used for aneurysms that are smaller than 5 centimeters (about 2 inches) across.
How often you need testing (for example, every few months or every year) is based on the size of the aneurysm and how fast it’s growing. The larger it is and the faster it’s growing, the more often you may need to be checked.
Medicines
If you have an aortic aneurysm, your doctor may prescribe medicines before surgery or instead of surgery. Medicines are used to lower blood pressure, relax blood vessels, and lower the risk that the aneurysm will rupture (burst). Beta blockers and calcium channel blockers are the medicines most commonly used.
Aorta surgery
Your doctor may recommend surgery if your aneurysm is growing quickly or is at risk of rupture or dissection.
The two main types of surgery to repair aortic aneurysms are open abdominal or open chest repair and endovascular repair.
Open Abdominal or Open Chest Repair
The standard and most common type of surgery for aortic aneurysms is open abdominal or open chest repair. This surgery involves a major incision (cut) in the abdomen or chest.
General anesthesia is used during this procedure. The term “anesthesia” refers to a loss of feeling and awareness. General anesthesia temporarily puts you to sleep.
Aortic arch surgery is a highly complex operation 2. It requires heart-lung bypass, whereby after opening the chest, circulation is diverted from the heart and lungs and oxygenated blood is pumped around the body using an external machine 2. The heart then stops beating. Subsequently, the body is cooled down to around 18-28 °C (64-82 °F), which reduces the metabolic demands of vital organs, allowing general circulation around the body to be stopped (circulatory arrest). Concurrently, blood is selectively pumped to the brain via arteries to maintain neurological function.
Operation on the aortic arch is then performed, which is usually replacement of diseased portions with synthetic material. Once all the blood vessels are satisfactorily replaced and connected, the blood is slowly warmed and introduced into the body, and the heart restarted. During this operation, repairs can also be performed for any concomitant heart anomalies, such as blocked coronary arteries.
During the surgery, the aneurysm is removed. Then, the section of aorta is replaced with a graft made of material such as Dacron® or Teflon.® The surgery takes 3 to 6 hours; you’ll remain in the hospital for 5 to 8 days.
If needed, repair of the aortic heart valve also may be done during open abdominal or open chest surgery.
It often takes a month to recover from open abdominal or open chest surgery and return to full activity. Most patients make a full recovery.
Endovascular Repair
In endovascular repair, the aneurysm isn’t removed. Instead, a graft is inserted into the aorta to strengthen it. Surgeons do this type of surgery using catheters (tubes) inserted into the arteries; it doesn’t require surgically opening the chest or abdomen. General anesthesia is used during this procedure. This minimally-invasive procedure removes the need for open heart surgery in some select cases.
The surgeon first inserts a catheter into an artery in the groin (upper thigh) and threads it to the aneurysm. Then, using an x ray to see the artery, the surgeon threads the graft (also called a stent graft) into the aorta to the aneurysm.
The graft is then expanded inside the aorta and fastened in place to form a stable channel for blood flow. The graft reinforces the weakened section of the aorta. This helps prevent the aneurysm from rupturing.
The recovery time for endovascular repair is less than the recovery time for open abdominal or open chest repair. However, doctors can’t repair all aortic aneurysms with endovascular repair. The location or size of an aneurysm may prevent the use of a stent graft.
Figure 4. Endovascular Aneursym Repair
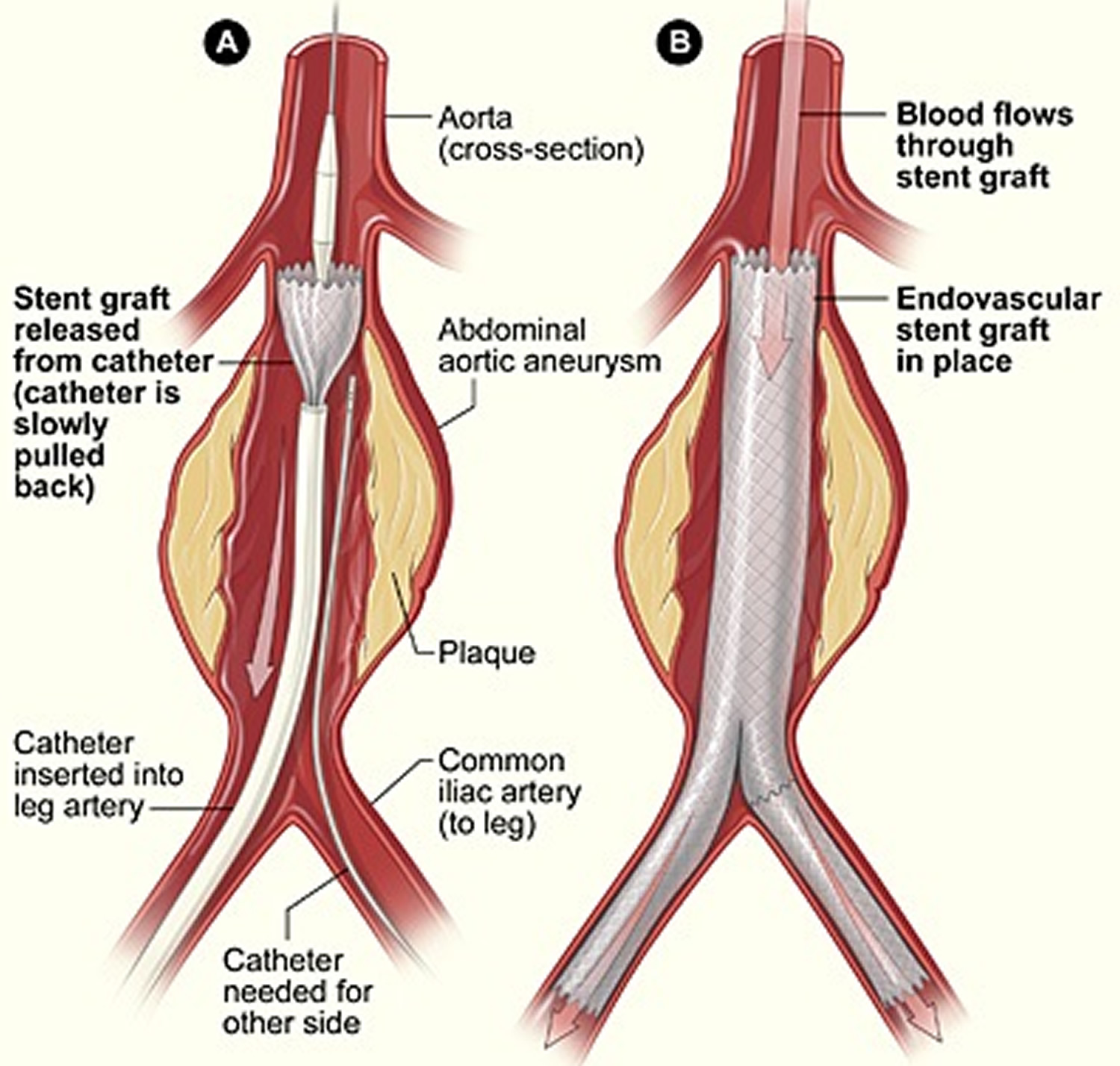
Footnote: The illustration shows the placement of a stent graft in an aortic aneurysm. In figure A, a catheter is inserted into an artery in the groin (upper thigh). The catheter is threaded to the abdominal aorta, and the stent graft is released from the catheter. In figure B, the stent graft allows blood to flow through the aneurysm.
Aortic arch surgery risks
The complexity of aortic arch surgery carries with it serious risk. Complications include 2:
- Stroke
- Damage to spinal cord
- Bleeding
- Heart attacks
- Lung and/or kidney failure
- Bowel necrosis
- Risk to life
However, despite these risks, long term outcome is reasonable, although this is dependent upon the type of arch disorder. Significantly improved quality of life usually follows surgery. Rates of risk vary between institutions, as well as with patient comorbidities and anatomy. Such risks, balanced against potential benefits, should be discussed with your surgeon.
Aortic dissection
An aortic dissection is a serious condition in which there is a tear in the inner layer of the aorta, the large blood vessel branching off the heart. Blood surges through the tear, causing the inner and middle layers of the aorta to separate (dissect). As the tear extends along the wall of the aorta, blood can flow in between the layers of the blood vessel wall (dissection). This can lead to aortic rupture or decreased blood flow (ischemia) to organs. If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is often fatal.
Aortic dissection is relatively uncommon. The condition most frequently occurs in men in their 60s and 70s. Symptoms of aortic dissection may mimic those of other diseases, often leading to delays in diagnosis. However, when an aortic dissection is detected early and treated promptly, the chance of survival greatly improves.
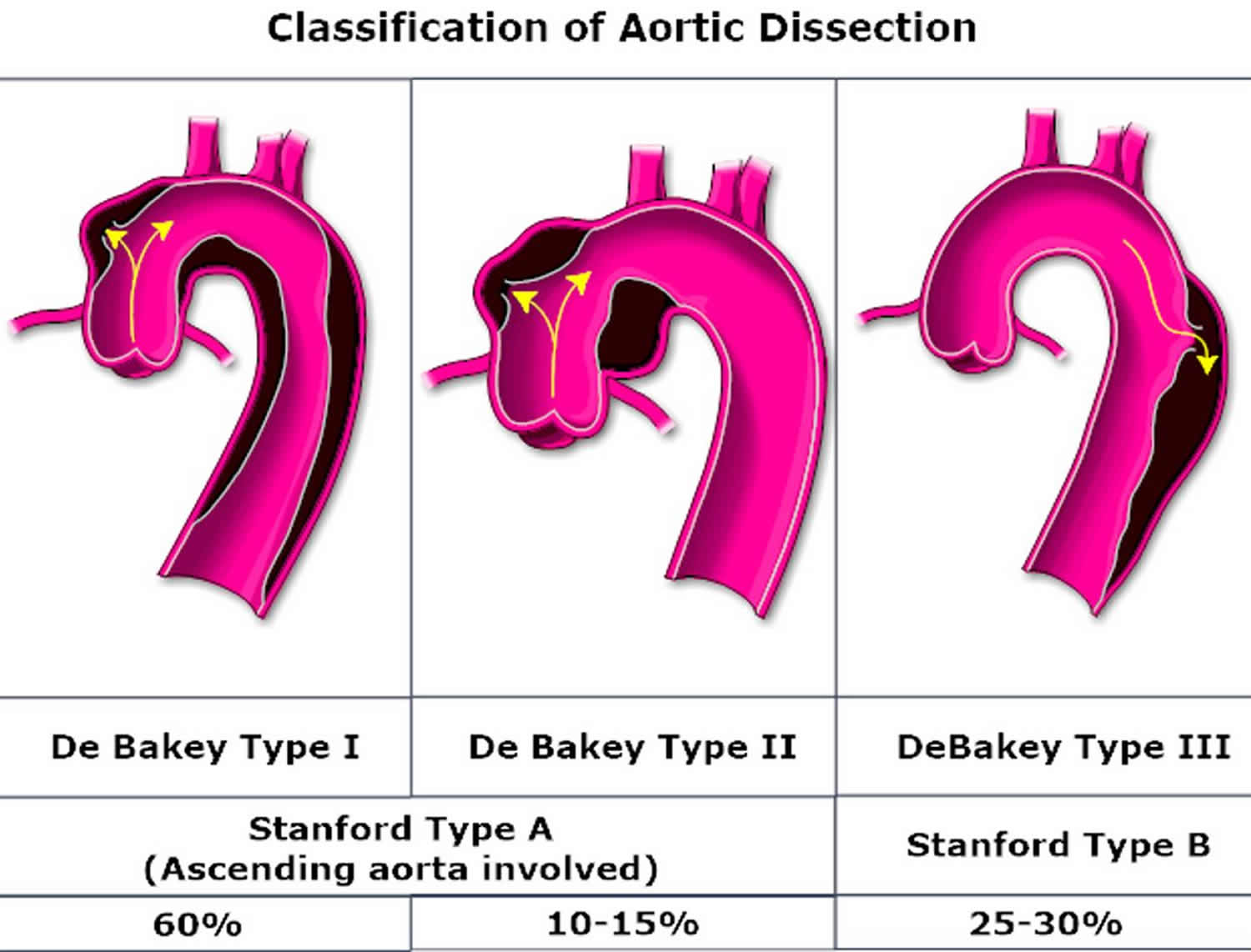
Aortic dissections are divided into two groups, depending on which part of the aorta is affected:
- Type A (ascending aorta). This more common and dangerous type involves a tear in the part of the aorta where it exits the heart or a tear in the upper aorta, which may extend into the abdomen.
- Type B (descending aorta). This involves a tear in the lower aorta only, which may also extend into the abdomen.
An aortic dissection can lead to:
- Death due to severe internal bleeding
- Organ damage, such as kidney failure or life-threatening intestinal damage
- Stroke
- Aortic valve damage (aortic regurgitation) or rupture into the lining around the heart (cardiac tamponade)
Figure 5. Aortic dissection
[Source 3]Aortic dissection symptoms
Aortic dissection symptoms may be similar to those of other heart problems, such as a heart attack. Typical signs and symptoms include:
- Sudden severe chest or upper back pain, often described as a tearing, ripping or shearing sensation, that radiates to the neck or down the back
- Sudden severe abdominal pain
- Loss of consciousness
- Shortness of breath
- Sudden difficulty speaking, loss of vision, weakness or paralysis of one side of your body, similar to those of a stroke
- Weak pulse in one arm or thigh compared with the other
- Leg pain
- Difficulty walking
- Leg paralysis
Aortic dissection causes
An aortic dissection occurs in a weakened area of the aortic wall. Chronic high blood pressure may stress the aortic tissue, making it more susceptible to tearing. You can also be born with a condition associated with a weakened and enlarged aorta, such as Marfan syndrome, bicuspid aortic valve or other rarer conditions associated with weakening of the walls of the blood vessels. Rarely, aortic dissections are caused by traumatic injury to the chest area, such as during motor vehicle accidents.
Risk factors for developing aortic dissection
Risk factors for aortic dissection include:
- Uncontrolled high blood pressure (hypertension)
- Hardening of the arteries (atherosclerosis)
- Weakened and bulging artery (pre-existing aortic aneurysm)
- An aortic valve defect (bicuspid aortic valve)
- A narrowing of the aorta at birth (aortic coarctation)
The most important risk factor for the development of aortic dissection is poorly controlled hypertension. Men are more often affected and the risk increases with age. Other important pathogenic factors are positive family history and genetic history (connective tissue disease, Ehlers-Danlos syndrome, Marfan syndrome), aortic disease and aortic valve diseases, history of cardiac surgery and previous trauma.
Certain genetic diseases increase the risk of having an aortic dissection, including:
- Turner’s syndrome. High blood pressure, heart problems and a number of other health conditions may result from this disorder.
- Marfan syndrome. This is a condition in which connective tissue, which supports various structures in the body, is weak. People with this disorder often have a family history of aneurysms of the aorta and other blood vessels or family history of aortic dissections.
- Other connective tissue disorders. This includes Ehlers-Danlos syndrome, a group of connective tissue disorders characterized by skin that bruises or tears easily, loose joints and fragile blood vessels and Loeys-Dietz syndrome, with twisted arteries, especially in the neck.
- Inflammatory or infectious conditions. These may include giant cell arteritis, which is an inflammation of the arteries, and syphilis, a sexually transmitted infection.
Other potential risk factors include:
- Sex. Men have about double the incidence of aortic dissection.
- Age. The incidence of aortic dissection peaks in the 60s and 80s.
- Cocaine use. This drug may be a risk factor for aortic dissection because it temporarily raises blood pressure.
- Pregnancy. Infrequently, aortic dissections occur in otherwise healthy women during pregnancy.
- High-intensity weightlifting. This and other strenuous resistance training may increase the risk of aortic dissection by increasing blood pressure during the activity.
Aortic dissection prevention
Here are a few tips to reduce your risk of an aortic dissection:
- Control blood pressure. If you have high blood pressure, get a home blood pressure measuring device to help you monitor your blood pressure.
- Don’t smoke. If you do smoke, take steps to stop.
- Maintain an ideal weight. Follow a low-salt diet with plenty of fruits, vegetables and whole grains and exercise regularly.
- Wear a seat belt. This reduces the risk of traumatic injury to your chest area.
Work with your doctor. If you have a family history of aortic dissection, a connective tissue disorder or a bicuspid aortic valve, tell your doctor. If you have an aortic aneurysm, find out how often you need monitoring and if surgery is necessary to repair your aneurysm.
If you have a genetic condition that increases your risk of aortic dissection, your doctor may recommend medications, even if your blood pressure is normal.
Aortic dissection diagnosis
Detecting an aortic dissection can be tricky because the symptoms are similar to those of a variety of health problems. Doctors often suspect an aortic dissection if the following signs and symptoms are present:
- Sudden tearing or ripping chest pain
- Widening of the aorta on chest X-ray
- Blood pressure difference between right and left arms
Although these signs and symptoms suggest aortic dissection, more-sensitive imaging techniques are needed. Frequently used imaging procedures include:
- Transesophageal echocardiogram (TEE). This test uses high-pitched sound waves to produce an image of the heart. A TEE is a special type of echocardiogram in which an ultrasound probe is inserted through the esophagus. The ultrasound probe is placed close to the heart and the aorta, providing a clearer picture of your heart than would a regular echocardiogram.
- Computerized tomography (CT) scan. CT scanning generates X-rays to produce cross-sectional images of the body. A CT of the chest is used to diagnose an aortic dissection, possibly with an injected contrast liquid. Contrast makes the heart, aorta and other blood vessels more visible on the CT pictures.
- Magnetic resonance angiogram (MRA). An MRI uses a magnetic field and pulses of radio wave energy to make pictures of the body. An MRA uses this technique to look at blood vessels.
Aortic dissection treatment
An aortic dissection is a medical emergency requiring immediate treatment. Therapy may include surgery or medications, depending on the area of the aorta involved.
Type A aortic dissection
Treatment for type A aortic dissection may include:
- Surgery. Surgeons remove as much of the dissected aorta as possible, block the entry of blood into the aortic wall and reconstruct the aorta with a synthetic tube called a graft. If the aortic valve leaks as a result of the damaged aorta, it may be replaced at the same time. The new valve is placed within the graft used to reconstruct the aorta.
- Medications. Some medications, such as beta blockers and nitroprusside (Nitropress), reduce heart rate and lower blood pressure, which can prevent the aortic dissection from worsening. They may be given to people with type A aortic dissection to stabilize blood pressure before surgery.
Type B aortic dissection
Treatment of type B aortic dissection may include:
- Medications. The same medications that are used to treat type A aortic dissection may be used without surgery to treat type B aortic dissections.
- Surgery. The procedure is similar to that used to correct a type A aortic dissection. Sometimes stents — small wire mesh tubes that act as a sort of scaffolding — may be placed in the aorta to repair complicated type B aortic dissections.
After treatment, you may need to take blood pressure lowering medication for life. In addition, you may need follow-up CTs or MRIs periodically to monitor your condition.
- Aneurysm. https://www.nhlbi.nih.gov/health-topics/aneurysm[↩]
- Tian DH, Croce B, Hardikar A. Aortic arch surgery. Ann Cardiothorac Surg. 2013;2(2):245. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3741828/[↩][↩][↩]
- Silaschi M, Byrne J, Wendler O. Aortic dissection: medical, interventional and surgical management. Heart 2017;103:78-87. https://heart.bmj.com/content/103/1/78[↩]