Contents
- What is atropine
- How does atropine work?
- What is atropine used for?
- Atropine special precautions
- Atropine contraindications
- Atropine dose
- Adult dose for bradycardia
- Adult dose for anesthesia
- Adult dose for anticholinesterase poisoning
- Adult dose for rhinorrhea
- Adult dose for AV heart block
- Adult dose for head injury
- Adult dose for peptic ulcer
- Adult dose for organophosphate poisoning
- Adult dose for nerve agent poisoning
- Adult dose for radiographic exam
- Pediatric dose for anesthesia
- Pediatric dose for anticholinesterase poisoning
- Pediatric dose for bradycardia
- Use: To overcome severe bradycardia and syncope due to a hyperactive carotid sinus reflex
- Pediatric dose for AV heart block
- Pediatric dose for head injury
- Pediatric dose for peptic ulcer
- Pediatric dose for organophosphate poisoning
- Pediatric dose for nerve agent poisoning
- Atropine side effects
What is atropine
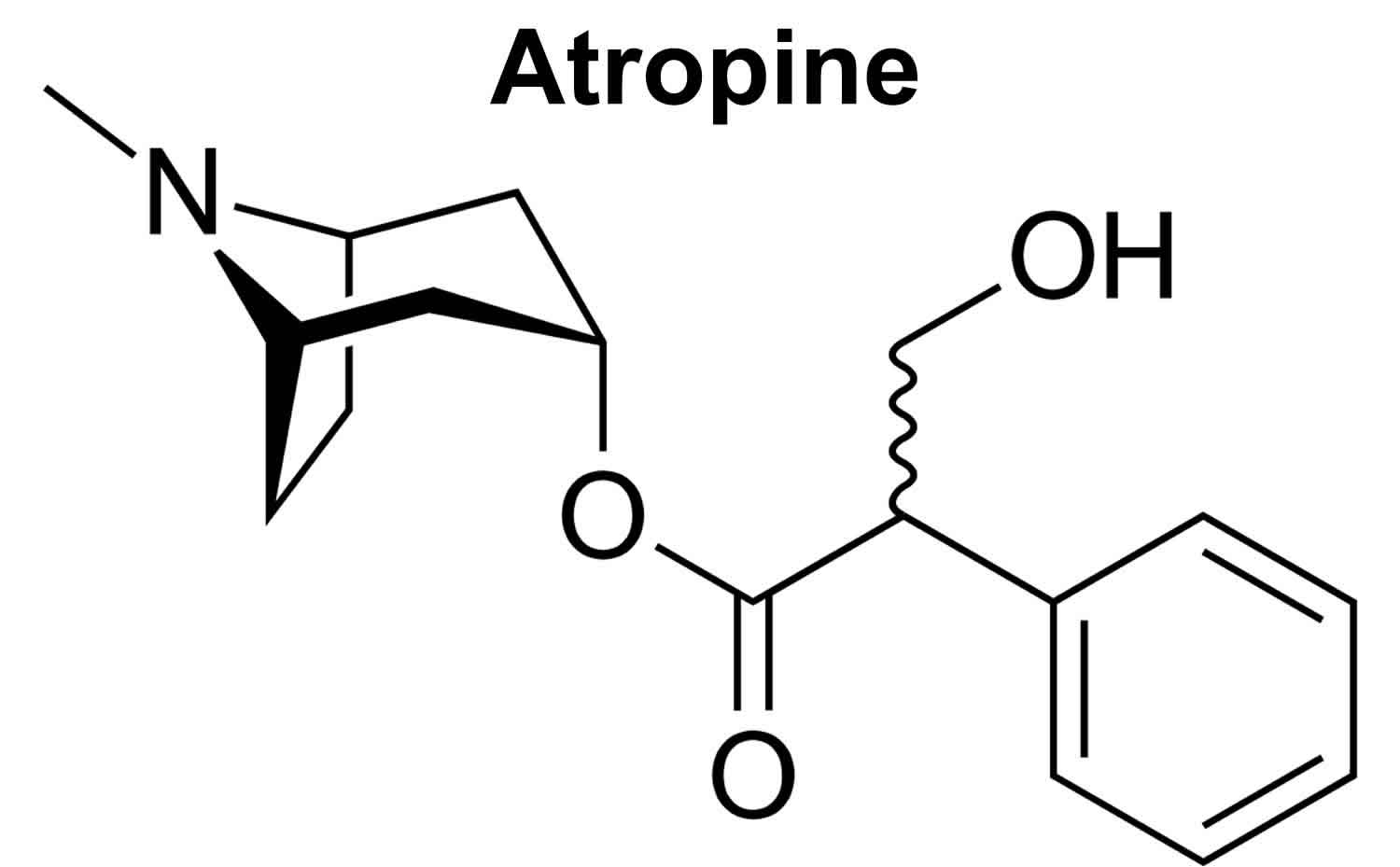
Atropine is a natural alkaloid anticholinergic agent found as a secondary metabolite in plants of the Solanaceae family, including deadly nightshade (Atropa belladonna) for which it is named. Atropine has potent and broad, nonspecific antimuscarinic activity and is used by injection. Because of atropine rapid onset of action and short half-life, atropine is used parenterally in management of medical emergencies including cardiac bradycardia, during anesthesia to prevent vagal reflexes and to decrease secretions, for acute severe bronchospasm, and for anticholinesterase overdose or poisoning. Atropine is injected into a muscle, under the skin, or into a vein through an IV. A healthcare provider will give you this injection.
Oral formulations of atropine are present in many over the counter and combination products used for allergic rhinitis and symptoms of peptic ulcer disease. Atropine has been in use in medicine for decades, but has not been formally approved for many of its broadly accepted indications. Atropine is used in low doses (1 mg or less) and usually for short periods of time.
Homatropine is a synthetic derivative of atropine and is less potent and has a shorter half-life, which makes it appropriate as a cycloplegic eye drops to dilate the pupils. It is also used in combination with opiate drugs for its aversive side effects to prevent abuse of high doses.
Common side effects of atropine are those of parasympathetic stimulation and include dryness of the mouth and eyes, decreased sweating, hyperthermia, headache, visual blurring, constipation, urinary retention, impotence, tachycardia and palpitations, anxiety, restlessness and in some instances agitation and hallucinations. Anticholinergic agents can precipitate acute narrow angle glaucoma and acute urinary retention.
How does atropine work?
Atropine functions as a sympathetic, competitive antagonist (blocker) of muscarinic postganglionic acetylcholine receptors, thereby abolishing the effects of parasympathetic stimulation. Atropine may induce tachycardia, inhibit secretions, and relax smooth muscles 1. This leads to parasympathetic inhibition of the acetylcholine receptors in smooth muscle. The end effect of increased parasympathetic inhibition allows for preexisting sympathetic stimulation to predominate creating increased cardiac output and other associated antimuscarinic side effects 2.
What is atropine used for?
Atropine or atropine sulfate carries U.S. Food and Drug Administration (FDA) indications to reduce saliva, mucus, or other secretions in your airway during a surgery (anti-sialagogue), treat symptomatic bradycardia, severe bronchospasm and to reduce vagal stimulation 3. Atropine is also used to treat spasms in the stomach, intestines, bladder, or other organs. Atropine is sometimes used as an antidote to treat certain types of organophosphate or anticholinergic poisoning.
Ophthalmic atropine is used before eye examinations to dilate (open) the pupil, the black part of the eye through which you see. It is also used to relieve pain caused by swelling and inflammation of the eye.
Antisialagogue
While atropine can be used independently for anti-salivation effects, it most commonly is secondary to anticholinergic or antimuscarinic poisoning which is discussed below. It is not formally recommended for routine use in controlled airways, though can be used off-label for minimizing secretions in the intubated patient.
Organophosphate or anticholinergic poisoning
Acetylcholine works on three different receptors that must be addressed in nerve agent poisonings. Atropine is only useful to counter muscarinic effects (pralidoxime and benzodiazepines address the others). If there are local symptoms to the eyes or respiratory tract, atropine is not indicated. Intravenous (IV) atropine is indicated for patients with hypersalivation, bronchial secretions, or bradycardia. Large doses and repeat doses may be required. Ingestions especially require higher doses (up to 20 mg). Titrate to effect by monitoring the patient’s ability to clear excess secretions. Pupils and heart rate are poor indications of appropriate dosing in these patients.
Bradycardia
Atropine is the first-line therapy for symptomatic bradycardia in the absence of reversible causes. Treatments for bradydysrhythmias are indicated when there is a structural disease of the infranodal system or if the heart rate is less than 50 beats/min with unstable vital signs. Approximately 20% of bradydysrhythmias are due to endogenous cardiac electrical systems. The structural disease may or may not require resuscitation and should be closely monitored with medication and pacing readily available. If there is no improvement in the clinical state after repeat doses of atropine, additional treatments with atropine are unlikely to be effective. However, transient improvements with repeat dosing are an indication to continue treatment with atropine (which may exceed standard cumulative dosing maximums). Pediatric bradycardia is rarely cardiac and often secondary to hypoxia and hypoventilation. If bradycardia persists despite adequate respiratory support, atropine is indicated.
Rapid Sequence Intubation Pretreatment
Although not recommended as a routine agent, atropine may be used 3-5 minutes prior to initiation of rapid sequence intubation to prevent bradycardia. In the setting of post-intubation related bradycardia, atropine is indicated. Post induction bradycardia is seen more commonly in the pediatric population due to the predominance of vagal response, even without the use of succinylcholine.
Atropine/Diphenoxylate (Lomotil) is an antimotility agent that can be used in the treatment of diarrhea as a second-line therapy. This allows the central acting opioid effect of diphenoxylate and capitalization on its anticholinergic side effect of constipation to slow motility. Subtherapeutic amounts of atropine are included in the dosage form to discourage diphenoxylate abuse. It may potentiate barbiturates, alcohol, or tranquilizers and therefore must be used with caution.
Under current advanced cardiac life support protocols, atropine is indicated for symptomatic bradycardia and not in a pulseless patient. All indications for atropine in the pulseless patient have been removed by the American Heart Association 1.
Atropine is not indicated in beta-blocker-induced bradycardias or hypotension, though its use is unlikely to be harmful. Glucagon is first line to treat beta-blockade-induced symptoms.
Atropine special precautions
Before taking atropine
To make sure atropine is safe for you, tell your doctor if you have:
- asthma or other breathing disorder;
- glaucoma;
- enlarged prostate;
- urination problems,
- a heart rhythm disorder;
- liver or kidney disease;
- myasthenia gravis; or
- blockage in your digestive tract (stomach or intestines).
Pregnancy Class B: It does cross the placenta and may lead to fetal tachycardia 4. It is not known whether atropine will harm an unborn baby. However, some forms of this medicine contain a preservative that may be harmful to a newborn. Tell your doctor if you are pregnant.
It is not known whether atropine passes into breast milk or if it could harm a nursing baby. Tell your doctor if you are breast-feeding a baby.
Use with caution in patients with coronary heart disease, acute myocardial ischemia, congestive heart failure, tachycardia, or hypertension as the increased cardiac demand and possible further worsening of tachycardia and hypertension can prove detrimental to patient outcomes.
Furthermore, caution is advised in use with elderly patients, chronic lung disease patients, acute angle glaucoma, obstructive diseases (uropathy, toxic megacolon, paralytic ileus, pyloric stenosis, prostatic hypertrophy), myasthenia gravis, or in situations with environmental heat exposure.
Atropine contraindications
Atropine does not carry a FDA Boxed Warning nor any absolute indications. There are multiple conditions that carry a cautionary status, however, relative contraindications are overridden by the clinical need, especially in the unstable or poisoning patient.
Use with caution in patients with coronary heart disease, acute myocardial ischemia, congestive heart failure, tachycardia, or hypertension as the increased cardiac demand and possible further worsening of tachycardia and hypertension can prove detrimental to patient outcomes.
Furthermore, caution is advised in use with elderly patients, chronic lung disease patients, acute angle glaucoma, obstructive diseases (uropathy, toxic megacolon, paralytic ileus, pyloric stenosis, prostatic hypertrophy), myasthenia gravis, or in situations with environmental heat exposure.
Atropine dose
Atropine can be administered by intravenous (IV), subcutaneous, intramuscular, or endotracheal method; IV is preferred. For endotracheal administration dilute 1 mg to 2 mg in 10 mL of sterile water or normal saline prior to administration. For pediatric endotracheal, double the usual IV dose and dilute in 3 to 5 mL.
- Antisialagogue/antivagal: 0.5 mg to 1 mg every 1 to 2 hours
- Organophosphate or muscarinic poisoning: 2 mg to 3 mg every 20 to 30 minutes (may require dosing up to 20 mg, titrate to effect of secretion control)
- Bradycardia: 1 mg every 3 to 5 minutes (3 mg max), repeat until desired heart rate is obtained, most effective for sinus and AV nodal disease.
- Pediatric: 0.01 mg/kg to 0.03 mg/kg every 3 to 5 minutes. Pediatric minimum dose 0.1 mg, maximum dose 0.5 mg (child) and 1.0 mg (adolescent); maximum cumulative dose 1 mg (child) and 2 mg (adolescent).
- Rapid Sequence Intubation Pretreatment: 0.01 mg/kg IV for adults with bradycardia secondary to repeat dosing of succinylcholine. Pediatric 0.02 mg/kg IV, minimum dose 0.1 mg. Not recommended as routine.
In general, dosing of atropine can be repeated every 5 minutes until a maximum of 0.04 mg/kg is reached.
Dosing in adults to greater than 0.5 mg and slow IV pushes have been associated with paradoxical bradycardia (though likely transient) and ventricular fibrillation (VF).
Adult dose for bradycardia
Use: To overcome severe bradycardia and syncope due to a hyperactive carotid sinus reflex
- 0.4 to 1 mg, IV, every 1 to 2 hours as needed
- Larger doses, up to a maximum of 2 mg, may be required
Adult dose for anesthesia
- 0.4 mg to 0.6 mg, IV, intramuscularly, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- In anesthesia to control excessive salivation and bronchial secretions
Adult dose for anticholinesterase poisoning
0.4 mg to 0.6 mg, IV, intramuscularly, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Treatment of parkinsonism; rigidity and tremor relieved by the apparently selective depressant action
- Relieve pylorospasm, hypertonicity of the small intestine, and hypermotility of the colon
- Relieve hypertonicity of the uterine muscle
- Relax the spasm of biliary and ureter colic and bronchial spasm
- Diminish the tone of the detrusor muscle of the urinary bladder in the treatment of urinary tract disorders
- Control the crying and laughing episode in patients with brain lesions
- Closed head injuries which cause acetylcholine to be released or present in the cerebrospinal fluid, causing abnormal EEG patterns, stupor, and neurological signs
- Management of peptic ulcer
- In anesthesia to control excessive salivation and bronchial secretions
- Control rhinorrhea of acute rhinitis or hay fever
- Antidote for pilocarpine, physostigmine, isoflurophate, choline esters, certain species of Aminata mushrooms, and anticholinesterase insecticide poisoning
- To lessen the degree of atrioventricular heart block when increased vagal tone is a major factor in the conduction defect, as in some cases due to digitalis
Adult dose for rhinorrhea
- 0.4 mg to 0.6 mg, IV, intramuscularly, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Control rhinorrhea of acute rhinitis or hay fever
Adult dose for AV heart block
- 0.4 mg to 0.6 mg, IV, intramuscularly, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- To lessen the degree of atrioventricular heart block when increased vagal tone is a major factor in the conduction defect, as in some cases due to digitalis
Adult dose for head injury
- 0.4 mg to 0.6 mg, IV, intramuscularly, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Control the crying and laughing episode in patients with brain lesions
- Closed head injuries which cause acetylcholine to be released or present in the cerebrospinal fluid, causing abnormal EEG patterns, stupor, and neurological signs
Adult dose for peptic ulcer
- 0.4 mg to 0.6 mg, IV, intramuscularly, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Management of peptic ulcer
Adult dose for organophosphate poisoning
Uses: Treatment of poisoning by susceptible organophosphorous nerve agents having cholinesterase activity as well as organophosphorous or carbamate insecticides.
- 0.8 mg, IM
- If no apparent effect within 30 minutes OR definite poisoning symptoms occur (nausea, vomiting, diarrhea, pupillary constriction, pulmonary edema, fasciculations of eyelids and tongue, jerky ocular movements and excessive sweating, salivation and bronchial secretion): Give 2 mg, IM, every hour, until signs of atropinization are seen
- The 2 mg dose may need to be given 2 or 3 times (4 to 6 mg total) in severe cases
Auto-injector:
- 2 or more mild symptoms of exposure: One 2 mg dose
- Severe symptoms: One 2 mg dose, followed by two additional 2 mg injections given in rapid succession 10 minutes after the first dose
or - Severe symptoms or unconscious: Three 2 mg doses into the mid-lateral thigh in rapid succession
Mild symptoms:
- Blurred vision, miosis
- Excessive unexplained teary eyes
- Excessive unexplained runny nose
- Increased salivation such as sudden unexplained excessive drooling
- Chest tightness or difficulty breathing
- Tremors throughout the body or muscular twitching
- Nausea and/or vomiting
- Unexplained wheezing or coughing
- Acute onset of stomach cramps
- Tachycardia or bradycardia
Severe symptoms:
- Strange or confused behavior
- Severe difficulty breathing or severe secretions from the lungs/airway
- Severe muscular twitching and general weakness
- Involuntary urination and defecation
- Convulsions
- Unconsciousness
Comments:
- These doses may be considerably exceeded in certain cases.
- Protective garments, including masks, designed specifically for protection against exposure to chemical nerve agents and insecticide poisoning should be worn as primary protection.
- Patients should not rely solely on the availability of antidotes for protection against chemical nerve agent and insecticide poisoning.
- Immediate evacuation from the contaminated environment is essential.
- Decontaminate the poisoned individual as soon as possible.
- The auto-injector should be used by persons with adequate training in recognizing and treating nerve agent or insecticide intoxication.
- Pralidoxime chloride may serve as an important adjunct to atropine therapy.
- The auto-injector is intended as initial treatment of muscarinic symptoms of nerve agent or insecticide poisoning; definitive medical care should be sought immediately.
- Administer as soon as symptoms of poisoning occur (usually tearing, excessive oral secretions, wheezing, muscle fasciculations, etc.).
- In severe poisonings, an anticonvulsant may be concurrently administered if seizure is suspected in the unconscious individual as the classic tonic-clonic jerking may not be apparent due to the effects of the poison.
- It is recommended that 3 auto-injectors be available for each person at risk of nerve agent or organophosphate insecticide poisoning: 1 for mild symptoms, plus 2 more for severe symptoms. Do not administer more than 3 injections unless under supervision of trained medical providers.
- Administering atropine in the absence of actual nerve agent or insecticide poisoning may cause an overdose of atropine which could result in temporary incapacitation (inability to walk properly, see or think clearly for several or more hours); patients with cardiac disease risk severe adverse events, including death.
Adult dose for nerve agent poisoning
Uses: Treatment of poisoning by susceptible organophosphorous nerve agents having cholinesterase activity as well as organophosphorous or carbamate insecticides.
- 0.8 mg, IM
- If no apparent effect within 30 minutes OR definite poisoning symptoms occur (nausea, vomiting, diarrhea, pupillary constriction, pulmonary edema, fasciculations of eyelids and tongue, jerky ocular movements and excessive sweating, salivation and bronchial secretion): Give 2 mg, IM, every hour, until signs of atropinization are seen
- The 2 mg dose may need to be given 2 or 3 times (4 to 6 mg total) in severe cases
Auto-injector:
- 2 or more mild symptoms of exposure: One 2 mg dose
- Severe symptoms: One 2 mg dose, followed by two additional 2 mg injections given in rapid succession 10 minutes after the first dose
or - Severe symptoms or unconscious: Three 2 mg doses into the mid-lateral thigh in rapid succession
Mild symptoms:
- Blurred vision, miosis
- Excessive unexplained teary eyes
- Excessive unexplained runny nose
- Increased salivation such as sudden unexplained excessive drooling
- Chest tightness or difficulty breathing
- Tremors throughout the body or muscular twitching
- Nausea and/or vomiting
- Unexplained wheezing or coughing
- Acute onset of stomach cramps
- Tachycardia or bradycardia
Severe symptoms:
- Strange or confused behavior
- Severe difficulty breathing or severe secretions from the lungs/airway
- Severe muscular twitching and general weakness
- Involuntary urination and defecation
- Convulsions
- Unconsciousness
Comments:
- These doses may be considerably exceeded in certain cases.
- Protective garments, including masks, designed specifically for protection against exposure to chemical nerve agents and insecticide poisoning should be worn as primary protection.
- Patients should not rely solely on the availability of antidotes for protection against chemical nerve agent and insecticide poisoning.
- Immediate evacuation from the contaminated environment is essential.
- Decontaminate the poisoned individual as soon as possible.
- The auto-injector should be used by persons with adequate training in recognizing and treating nerve agent or insecticide intoxication.
- Pralidoxime chloride may serve as an important adjunct to atropine therapy.
- The auto-injector is intended as initial treatment of muscarinic symptoms of nerve agent or insecticide poisoning; definitive medical care should be sought immediately.
- Administer as soon as symptoms of poisoning occur (usually tearing, excessive oral secretions, wheezing, muscle fasciculations, etc.).
- In severe poisonings, an anticonvulsant may be concurrently administered if seizure is suspected in the unconscious individual as the classic tonic-clonic jerking may not be apparent due to the effects of the poison.
- It is recommended that 3 auto-injectors be available for each person at risk of nerve agent or organophosphate insecticide poisoning: 1 for mild symptoms, plus 2 more for severe symptoms. Do not administer more than 3 injections unless under supervision of trained medical providers.
- Administering atropine in the absence of actual nerve agent or insecticide poisoning may cause an overdose of atropine which could result in temporary incapacitation (inability to walk properly, see or think clearly for several or more hours); patients with cardiac disease risk severe adverse events, including death.
Adult dose for radiographic exam
- 1 mg, IM
Use: Relaxation of the upper gastrointestinal tract and colon during radiography
Pediatric dose for anesthesia
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- In anesthesia to control excessive salivation and bronchial secretions
Pediatric dose for anticholinesterase poisoning
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
Doses may be considerably exceeded in certain cases.
Uses:
- Relieve pylorospasm, hypertonicity of the small intestine, and hypermotility of the colon
- Relieve hypertonicity of the uterine muscle
- Relax the spasm of biliary and ureter colic, and bronchial spasm
- Diminish the tone of the detrusor muscle of the urinary bladder in the treatment of urinary tract disorders
- Control the crying and laughing episodes in patients with brain lesions
- Closed head injuries which cause acetylcholine to be released or present in the cerebrospinal fluid, causing abnormal EEG patterns, stupor, and neurological signs
- Management of peptic ulcer
- In anesthesia to control excessive salivation and bronchial secretions
- Control rhinorrhea of acute rhinitis or hay fever
- Antidote for pilocarpine, physostigmine, isoflurophate, choline esters, certain species of Aminata mushrooms, and anticholinesterase insecticide poisoning
- Treatment of parkinsonism; rigidity and tremor relieved by the apparently selective depressant action
Pediatric dose for bradycardia
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
Doses may be considerably exceeded in certain cases.
Use: To overcome severe bradycardia and syncope due to a hyperactive carotid sinus reflex
Pediatric dose for rhinorrhea
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Control rhinorrhea of acute rhinitis or hay fever
Pediatric dose for AV heart block
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- To lessen the degree of atrioventricular heart block when increased vagal tone is a major factor in the conduction defect, as in some cases due to digitalis
Pediatric dose for head injury
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Control the crying and laughing episodes in patients with brain lesions
- Closed head injuries which cause acetylcholine to be released or present in the cerebrospinal fluid, causing abnormal EEG patterns, stupor, and neurological signs
Pediatric dose for peptic ulcer
- 7 to 16 pounds: 0.1 mg, IV, IM, or subcutaneously
- 17 to 24 pounds: 0.15 mg, IV, IM, or subcutaneously
- 24 to 40 pounds: 0.2 mg, IV, IM, or subcutaneously
- 40 to 65 pounds: 0.3 mg, IV, IM, or subcutaneously
- 65 to 90 pounds: 0.4 mg, IV, IM, or subcutaneously
- Over 90 pounds: 0.4 to 0.6 mg, IV, IM, or subcutaneously
Comments:
- Doses may be considerably exceeded in certain cases.
Uses:
- Management of peptic ulcer
Pediatric dose for organophosphate poisoning
Use: Treatment of poisoning by susceptible organophosphorous nerve agents having cholinesterase activity as well as organophosphorous or carbamate insecticides.
Auto-injector:
- Children weighing over 90 pounds: 2 mg dose
- 40 to 90 pounds: 1 mg dose
- 15 to 40 pounds: 0.5 mg dose
- Less than 15 pounds: 0.25 mg dose (bunch up thigh to provide a thicker area for injection)
2 or more mild symptoms of exposure: One dose (see weight guide above)
Severe symptoms: One dose, followed by two additional doses given in rapid succession 10 minutes after the first dose
or
Severe symptoms or unconscious: Three doses into the mid-lateral thigh in rapid succession
Mild symptoms:
- Blurred vision, miosis
- Excessive unexplained teary eyes
- Excessive unexplained runny nose
- Increased salivation such as sudden unexplained excessive drooling
- Chest tightness or difficulty breathing
- Tremors throughout the body or muscular twitching
- Nausea and/or vomiting
- Unexplained wheezing or coughing
- Acute onset of stomach cramps
- Tachycardia or bradycardia
Severe symptoms:
- Strange or confused behavior
- Severe difficulty breathing or severe secretions from the lungs/airway
- Severe muscular twitching and general weakness
- Involuntary urination and defecation
- Convulsions
- Unconsciousness
Comments:
- These doses may be considerably exceeded in certain cases.
- Protective garments, including masks, designed specifically for protection against exposure to chemical nerve agents and insecticide poisoning should be worn as primary protection.
- Patients should not rely solely on the availability of antidotes for protection against chemical nerve agent and insecticide poisoning.
- Immediate evacuation from the contaminated environment is essential.
- Decontaminate the poisoned individual as soon as possible.
- The auto-injector should be used by persons with adequate training in recognizing and treating nerve agent or insecticide intoxication.
- Pralidoxime chloride may serve as an important adjunct to atropine therapy.
- The auto-injector is intended as initial treatment of muscarinic symptoms of nerve agent or insecticide poisoning; definitive medical care should be sought immediately.
- Administer as soon as symptoms of poisoning occur (usually tearing, excessive oral secretions, wheezing, muscle fasciculations, etc.).
- In severe poisonings, an anticonvulsant may be concurrently administered if seizure is suspected in the unconscious individual as the classic tonic-clonic jerking may not be apparent due to the effects of the poison.
- It is recommended that 3 auto-injectors be available for each person at risk of nerve agent or organophosphate insecticide poisoning: 1 for mild symptoms, plus 2 more for severe symptoms. Do not administer more than 3 injections unless under supervision of trained medical providers.
- Administering atropine in the absence of actual nerve agent or insecticide poisoning may cause an overdose of atropine which could result in temporary incapacitation (inability to walk properly, see or think clearly for several or more hours); patients with cardiac disease risk severe adverse events, including death.
Pediatric dose for nerve agent poisoning
Use: Treatment of poisoning by susceptible organophosphorous nerve agents having cholinesterase activity as well as organophosphorous or carbamate insecticides.
- Children weighing over 90 pounds: 2 mg dose
- 40 to 90 pounds: 1 mg dose
- 15 to 40 pounds: 0.5 mg dose
- Less than 15 pounds: 0.25 mg dose (bunch up thigh to provide a thicker area for injection)
2 or more mild symptoms of exposure: One dose (see weight guide above)
Severe symptoms: One dose, followed by two additional doses given in rapid succession 10 minutes after the first dose
or
Severe symptoms or unconscious: Three doses into the mid-lateral thigh in rapid succession
Mild symptoms:
- Blurred vision, miosis
- Excessive unexplained teary eyes
- Excessive unexplained runny nose
- Increased salivation such as sudden unexplained excessive drooling
- Chest tightness or difficulty breathing
- Tremors throughout the body or muscular twitching
- Nausea and/or vomiting
- Unexplained wheezing or coughing
- Acute onset of stomach cramps
- Tachycardia or bradycardia
Severe symptoms:
- Strange or confused behavior
- Severe difficulty breathing or severe secretions from the lungs/airway
- Severe muscular twitching and general weakness
- Involuntary urination and defecation
- Convulsions
- Unconsciousness
Comments:
- These doses may be considerably exceeded in certain cases.
- Protective garments, including masks, designed specifically for protection against exposure to chemical nerve agents and insecticide poisoning should be worn as primary protection.
- Patients should not rely solely on the availability of antidotes for protection against chemical nerve agent and insecticide poisoning.
- Immediate evacuation from the contaminated environment is essential.
- Decontaminate the poisoned individual as soon as possible.
- The auto-injector should be used by persons with adequate training in recognizing and treating nerve agent or insecticide intoxication.
- Pralidoxime chloride may serve as an important adjunct to atropine therapy.
- The auto-injector is intended as initial treatment of muscarinic symptoms of nerve agent or insecticide poisoning; definitive medical care should be sought immediately.
- Administer as soon as symptoms of poisoning occur (usually tearing, excessive oral secretions, wheezing, muscle fasciculations, etc.).
- In severe poisonings, an anticonvulsant may be concurrently administered if seizure is suspected in the unconscious individual as the classic tonic-clonic jerking may not be apparent due to the effects of the poison.
- It is recommended that 3 auto-injectors be available for each person at risk of nerve agent or organophosphate insecticide poisoning: 1 for mild symptoms, plus 2 more for severe symptoms. Do not administer more than 3 injections unless under supervision of trained medical providers.
- Administering atropine in the absence of actual nerve agent or insecticide poisoning may cause an overdose of atropine which could result in temporary incapacitation (inability to walk properly, see or think clearly for several or more hours); patients with cardiac disease risk severe adverse events, including death.
Atropine side effects
The most common side effect effects of atropine are related to the antimuscarinic properties including dryness of the mouth and eyes (xerostomia), blurred vision, photophobia, tachycardia, flushing, and hot skin.
Common atropine side effects may include:
- dry mouth, nose, or throat;
- dry eyes, blurred vision;
- dizziness; or
- headache, drowsiness.
Tachycardia is the most common side effect; titrate dose to effect when treating bradycardia in patients with coronary artery disease. Atropine may precipitate acute angle glaucoma, pyloric obstruction, urinary retention due to benign prostatic hyperplasia, or viscid plugs in patients with chronic lung diseases.
Constipation, difficulty with urination, and anhidrosis can occur especially in at-risk populations (most notably, the elderly). In rare cases, delirium or coma may occur. Hypersensitivity reactions may occur and are usually limited to a skin rash that could progress to exfoliation 5.
Atropine decreases the rate of mexiletine absorption that can be prevented by combined IV delivery of metoclopramide with atropine before anesthesia.
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Tell your caregivers right away if you have:
- a light-headed feeling, like you might pass out;
- pounding heartbeats or fluttering in your chest;
- restlessness;
- speech problems, trouble swallowing;
- confusion, hallucinations;
- weakness, loss of balance;
- hot, dry skin; or
- a severe skin rash.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
Atropine overdose
Atropine overdose can lead to increased antimuscarinic side effects presenting with dilated pupils, warm, dry skin, tachycardia, tremor, ataxia, delirium, and coma. In extreme toxicity, circulatory collapse secondary to respiratory failure may occur after paralysis and coma. Ten milligrams or less may be fatal to a child, while there is no known adult fatal dose.
All Datura plant species have endogenous atropine and other assorted anticholinergic alkaloids. This includes Jimson weed and angel’s trumpet, which is typically seen in warm or temperate climate areas. It may be accidental ingestion or intentionally smoked or ingested for the goal effect of hallucinations. While treatment for ingestions is similar to other toxic overdoses of anticholinergics, whole-bowel irrigation is recommended after a large quantity of seed ingestion. Avoid phenothiazines in these patients. Physostigmine is the basis of reversal.
Treatment of atropine overdose includes a short-acting barbiturate or diazepam as needed for convulsions or excitement. Avoid dosing for sedation as it can cause respiratory collapse. Physostigmine is useful as an antidote to treat delirium and coma. Repeat doses may be required as physostigmine has a shorter half-life. Monitor respiratory effort and supplement, if necessary 6.
- McLendon K, Preuss CV. Atropine. [Updated 2018 Nov 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470551[↩][↩]
- Drugs and Lactation Database (LactMed) [Internet]. National Library of Medicine (US); Bethesda (MD): 2006. Belladonna.[↩]
- Smulyan H. The Beat Goes On: The Story of Five Ageless Cardiac Drugs. Am. J. Med. Sci. 2018 Nov;356(5):441-450.[↩]
- Drugs and Lactation Database (LactMed) [Internet]. National Library of Medicine (US); Bethesda (MD): 2006. Atropine[↩]
- Wu PC, Chuang MN, Choi J, Chen H, Wu G, Ohno-Matsui K, Jonas JB, Cheung CMG. Update in myopia and treatment strategy of atropine use in myopia control. Eye (Lond). 2019 Jan;33(1):3-13[↩]
- Menezes RG, Usman MS, Hussain SA, Madadin M, Siddiqi TJ, Fatima H, Ram P, Pasha SB, Senthilkumaran S, Fatima TQ, Luis SA. Cerbera odollam toxicity: A review. J Forensic Leg Med. 2018 Aug;58:113-116[↩]