Contents
What is bladder exstrophy
Bladder exstrophy is a complex, rare birth defect in which the bladder develops outside the fetus. As the bladder is developing the abdominal wall does not fully form, leaving the pubic bones separated and the bladder exposed to the outside skin surface through an opening in the lower abdominal wall. Because the bladder and urethra are not closed, the bladder is unable to store urine. Urine produced by the kidneys drains into this open area.
Bladder exstrophy is more common in males than in females. Bladder exstrophy is more common in males with male-to-female ratio 2:1. Bladder exstrophy occurs in approximately 1 in every 50,000 live births.
Bladder exstrophy may occur in varying degrees and may involve other organs including the bowel, external genitalia and pelvic bones.
Bladder exstrophy is the most common of a larger group of birth defects called the bladder exstrophy-epispadias complex. As the fetus grows, a structure called the cloaca — where reproductive, urinary and digestive openings all come together — does not develop properly. The resulting defects can range greatly in severity depending on the age of the fetus when the developmental error occurs. Defects resulting from this complex range from mild to severe. Bladder exstrophy itself also has a range of severity and, in addition to the abnormalities in the bladder, genitals and pelvic bones, may include defects in the intestines and reproductive organs.
Often doctors will identify bladder exstrophy on an ultrasound during pregnancy. Sometimes, though, the defect isn’t visible until after the baby is born.
Treatment for bladder exstrophy includes surgical repair. The goal of treatment is to optimize urinary control, to preserve normal renal function, and to optimize the appearance and function of the external genitalia. If left untreated, normal urine continence does not occur and normal sexual function is compromised.
Surgeons treat bladder exstrophy after birth. Surgical repair is usually done at age 3 months or later. Sometimes two or more procedures are needed. Some children require additional surgery around age 4.
With surgery, and sometimes with medication, many children achieve bladder control (continence).
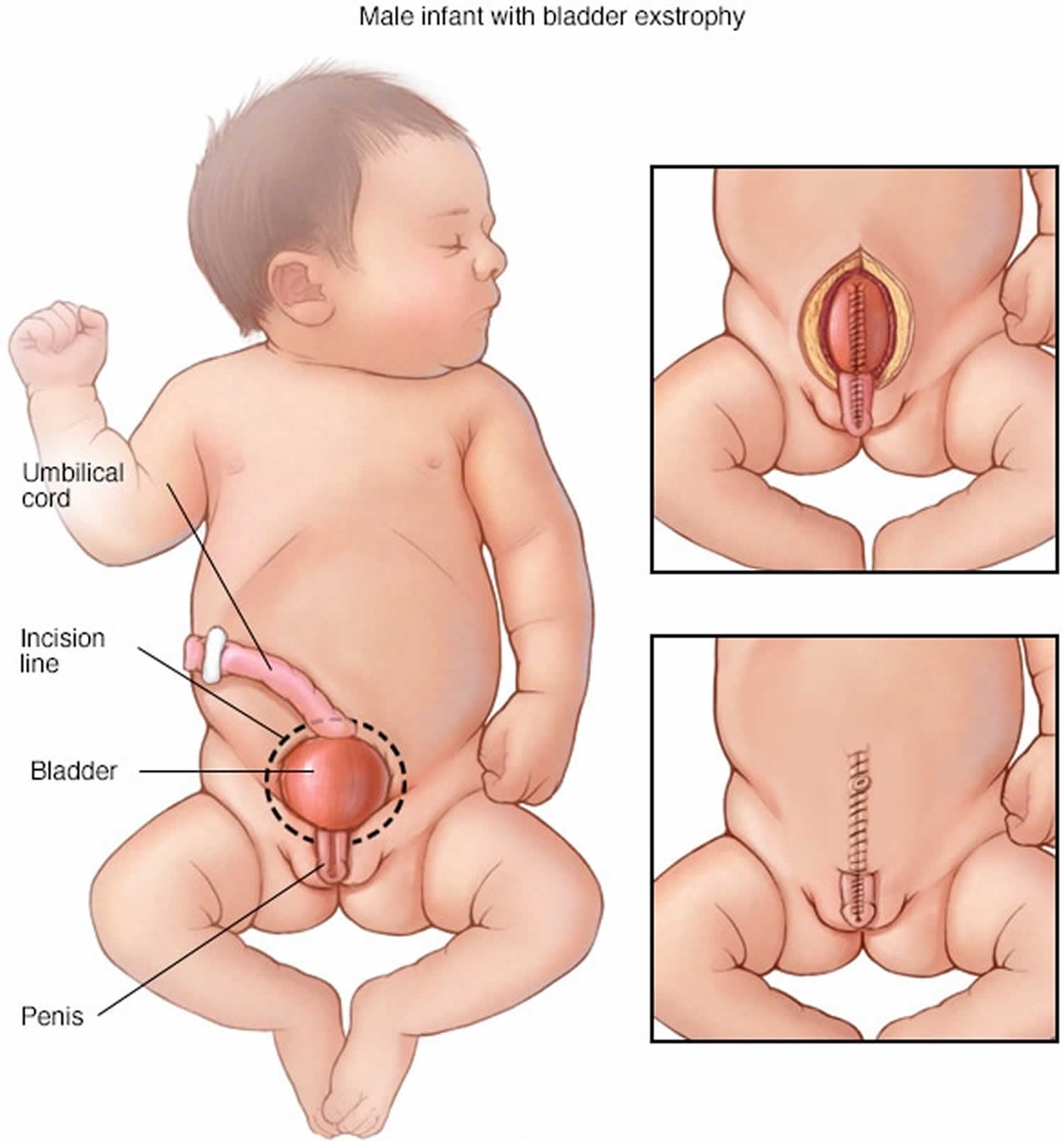
Figure 1. Bladder exstrophy
[Source 1 ]Figure 2. Bladder exstrophy female infant
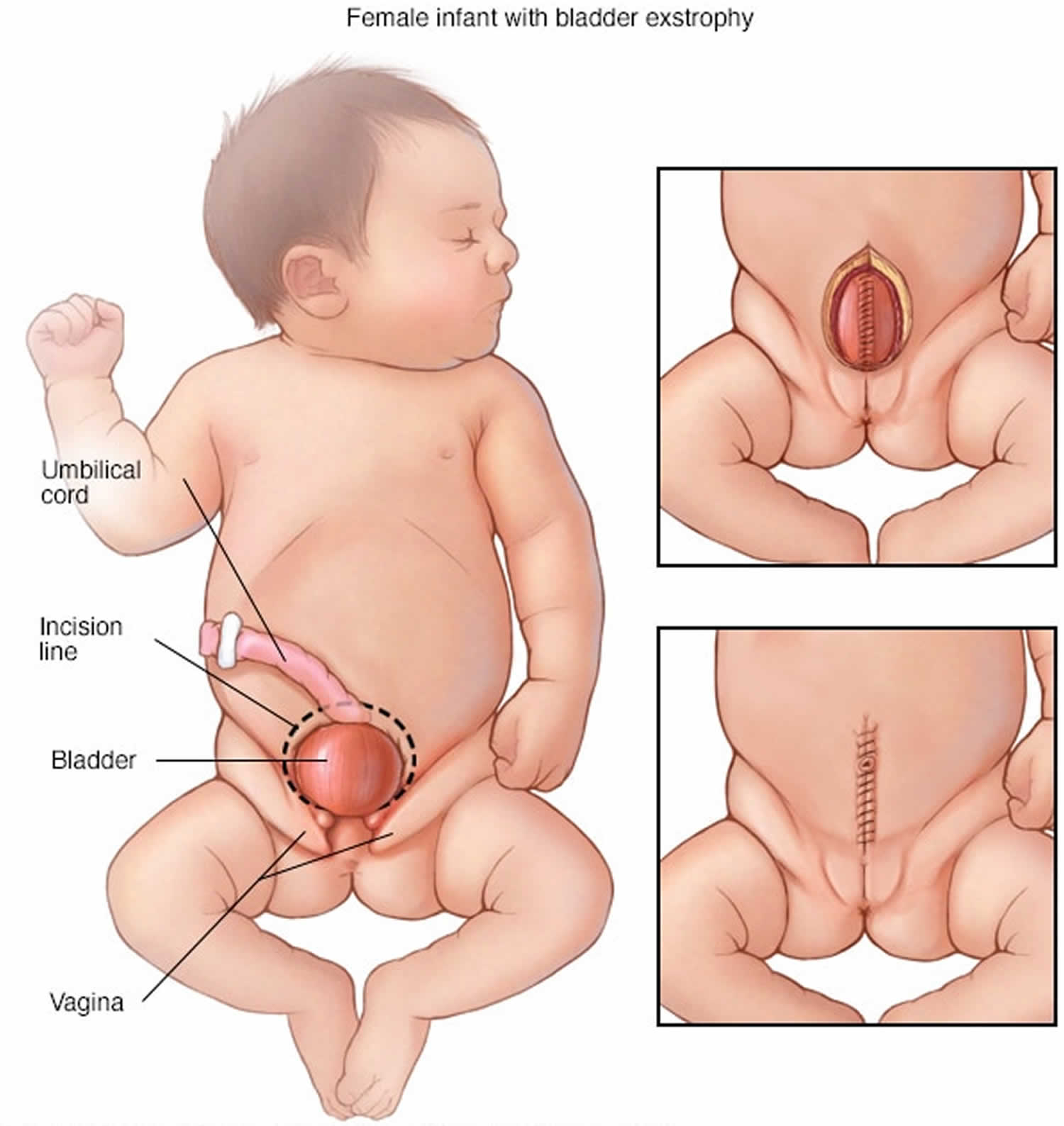 Footnote: In girls born with bladder exstrophy, the bladder is on the outside of the body and the vagina is not fully formed. Surgeons will close the bladder (top right) and then close the abdomen and skin (bottom right).
Footnote: In girls born with bladder exstrophy, the bladder is on the outside of the body and the vagina is not fully formed. Surgeons will close the bladder (top right) and then close the abdomen and skin (bottom right).Figure 3. Bladder exstrophy male infant
Footnote: In boys born with bladder exstrophy, the bladder is on the outside of the body and the penis and the urine tube (urethra) are not fully closed. Surgeons will close the penis and bladder (top right) and then close the abdomen and skin (bottom right).
Bladder exstrophy causes
Doctors aren’t sure what causes bladder exstrophy. As with similar problems, it appears to result from a combination of genetic and environmental risk factors.
- Genetic factors. Recent studies indicate that the master control gene ISL1 is probably a susceptibility gene for bladder exstrophy. A susceptibility gene is one that is likely the cause of a specific disease or disorder. This gene is also important in regulating urinary tract development.
- Environmental factors. Some research suggests associations with the age of the mother, assisted reproduction, use of the hormone progesterone during pregnancy and smoking during pregnancy, but no cause and effect has been determined.
Risk factors for bladder exstrophy
Factors that increase the risk of bladder exstrophy include:
- Family history. Firstborn children, children of a parent with bladder exstrophy or siblings of a child with bladder exstrophy have an increased chance of being born with the condition.
- Race. Bladder exstrophy is more common in whites than in other races.
- Sex. More males than females are born with bladder exstrophy.
Bladder exstrophy signs and symptoms
The signs and symptoms of bladder exstrophy can vary from child to child, but may include:
- Abnormal development of the bladder: The bladder is open in the front and exposed on the abdominal wall (bladder is outside the body). The bladder neck has not developed properly and the bladder itself is usually small. These factors make it difficult for the bladder to hold urine initially after correction surgery until the bladder has time to grow and develop.
- Epispadias: The urethra, which is the hollow tube that drains urine from the bladder to the outside of the body, is not formed completely. In males, the urethra is open on the top of the penis and not the tip. In girls, the urethral opening may be positioned further up between the divided clitoris and labia minora.
- Widening of the pubic bones: The pubic bones usually join to protect and support the bladder, urethra and abdominal muscles. In children with exstrophy, the pubic bones do not join, leaving a wide opening. This causes the hips to be outwardly rotated.
- Vesicoureteral reflux (VUR): Normally the kidneys make urine and drain down the ureters (drainage tubes) into the bladder. VUR is a condition where urine travels back up into the kidneys. This may develop after the bladder is closed.
- Abnormal development of genitalia:
- Boys: The penis may appear shorter and curved in an upward direction. The testicles may not be in a normal position in the scrotum and a hernia may be seen.
- Girls: The clitoris and labia minora are separated and spread apart; the vagina and urethra are shorter. The uterus, fallopian tubes and ovaries are generally normal.
- Displacement of the umbilicus (belly button) and/or an umbilical hernia
Bladder exstrophy is the most common of a larger group of birth defects called the bladder exstrophy-epispadias complex. If your child has bladder exstrophy-epispadias complex, he or she will have one of the following:
- Epispadias. This is the least severe form of bladder exstrophy-epispadias complex, in which the tube to expel urine (urethra) does not fully develop.
- Bladder exstrophy. This is the most common form of bladder exstrophy-epispadias complex. Bladder exstrophy means that the bladder is formed on the outside of the body and is turned inside out. Usually bladder exstrophy will involve organs of the urinary tract, as well as the digestive and reproductive systems. The condition can include specific defects of the abdominal wall, bladder, genitals, pelvic bones, final section of the large intestine (rectum) and opening at the end of the rectum (anus). Children with bladder exstrophy will also have a condition called vesicoureteral reflux, in which urine flows the wrong way — from the bladder back up into the tubes that connect to the kidneys (ureters). Children with bladder exstrophy also have epispadias. These defects are treated through surgical procedures that repair the affected organs, muscles and bones.
- Cloacal exstrophy. Cloacal exstrophy is the most serious form of bladder exstrophy-epispadias complex, in which the rectum, bladder and genitals did not fully separate as the fetus developed. These organs may not be correctly formed. The pelvic bones are more severely affected as well. The backbone and spinal cord may be affected, as well as the kidneys. Children born with protruding abdominal organs (omphalocele) likely have cloacal exstrophy. However, an omphalocele may occasionally be associated with bladder exstrophy as well. Most children with cloacal exstrophy have spinal abnormalities, including spina bifida.
Bladder exstrophy complications
If not treated, children with bladder exstrophy will have an inability to hold urine (urinary incontinence) and an increased risk of bladder cancer. They’re also at risk of sexual dysfunction.
Surgical treatment can reduce complications, depending on the severity of defects. Many children who have surgical repair are able to hold urine (continent). Young children with bladder exstrophy may walk with their legs turned somewhat outward, due to the separation of their pelvic bones.
People born with bladder exstrophy can go on to have normal sexual function, including the ability to have children. However, pregnancy will be high risk for both mother and baby. It’s possible for pregnant women with bladder exstrophy to choose a vaginal birth, although it may be complicated by the condition of her cervical tissue. A planned cesarean section is likely to be the preferable option.
Bladder exstrophy diagnosis
Bladder exstrophy can usually be diagnosed by fetal ultrasound before an infant is born. Bladder exstrophy is suspected when ultrasound shows that the baby’s bladder is not filling and emptying normally.
Signs the doctor will look for in the images include:
- Bladder doesn’t fill or empty correctly
- Umbilical cord is placed low on the abdomen
- Pubic bones — part of the hipbones that form the pelvis — are separated
- Smaller than normal genitals
Fetal imaging experts will look for several other indicators to confirm the diagnosis, including a low umbilical cord with an abdominal bulge below the cord insertion (representing the opened bladder halves, or bladder plate) and unclear male or female genitalia. Bladder exstrophy is not usually associated with other ultrasound findings or chromosomal or genetic syndromes. However, for gender identification, an amniocentesis may be recommended.
Sometimes bladder exstrophy can’t be seen until after the baby is born. In a newborn, doctors look for:
- Size of the portion of the bladder that is open and exposed to air (bladder template)
- Position of the testicles
- Intestine bulging through the abdominal wall (inguinal hernia)
- Anatomy of the area around the navel
- Position of opening at the end of the rectum (anus)
- How much the pubic bones are separated, and how easily the pelvis moves
Prenatal evaluation
If doctors believe your unborn baby has bladder exstrophy, they will schedule you for a comprehensive prenatal evaluation.
During your prenatal evaluation, you will undergo a variety of diagnostic tests which may include:
- Targeted, high-resolution fetal ultrasound
- Fetal echocardiogram (specialized ultrasound that evaluates the structure and function of the fetal heart)
- Ultrafast fetal MRI
- Consultation with an obstetric specialist and a pediatric urologist
Your healthcare team will meet with you to review all studies and make a plan tailored to your unique needs. They will provide extensive information about your baby’s condition and answer your questions about the diagnosis, prenatal care and delivery, what to expect before and after surgery, and plans for long-term follow-up care.
Bladder exstrophy treatment
The goals of bladder exstrophy treatment are to improve quality of life, continence and body image for children born with bladder exstrophy.
Children born with bladder exstrophy are treated with reconstructive surgery following birth. The overall goals of reconstruction are to provide enough space for urine storage, create outer sex organs (external genitalia) that look and function acceptably, establish bladder control (continence), and preserve kidney function.
Bladder exstrophy surgery
Bladder exstrophy can be repaired with reconstructive surgery.
Doctors will choose one of two basic approaches:
- Complete primary repair of bladder exstrophy. Complete primary repair of exstrophy surgery is performed in one procedure, usually after the baby is three months old 2. Surgeons close the bladder and the abdomen and repair the urethra and outer sex organs. Most surgery for newborns will include repair to the pelvic bones (pelvic osteotomy). However, doctors may choose not to perform an osteotomy if the baby is less than 72 hours old, the pelvic separation (pubic diastasis) is small, and the infant’s bones are flexible.
- Modern staged repair of bladder exstrophy. Modern staged repair of bladder exstrophy involves three operations, usually within 72 hours after birth, at age 6 to 12 months and again at 4 to 5 years. The first closes the bladder and the abdomen, and the second repairs the urethra and sex organs. Then, when the child is old enough for toilet training and can participate in a “voiding program,” surgeons will perform bladder neck reconstruction. Most, but not all, children will be able to achieve continence, but they sometimes may need to have a tube inserted into their bladder to drain urine (catheterization).
After surgery, doctors will need to keep your child immobilized and will manage his or her pain.
- Immobilization. Following surgery, infants will need to be held still in traction while healing. The amount of time a child needs to be immobilized varies. Infants undergoing initial surgery to close their bladder may be immobilized for three to six weeks. Children who are older or having a second bladder closure may need to be immobilized up to eight weeks, but may be able to recover at home.
- Pain management. New, regional anesthesia techniques allow doctors to place a thin tube (catheter) into the spinal canal (epidural space) during surgery and leave it in place for up to 30 days. This approach provides more consistent pain control and requires less use of opioid medications than previously.
Complete primary repair of exstrophy
Complete primary repair of exstrophy allows doctors to achieve the goals of surgical correction all in one operation:
- Bladder closure (moving it inside the body)
- Epispadias repair with reconstruction of the genitalia
- Bladder neck reconstruction (reconstruction of the urinary sphincter muscles)
- Pelvic osteotomy (closing the pelvic bones)
Closing the bladder early allows the bladder to cycle (fill and empty urine) which helps with bladder growth and development. Surgery is typically performed within 6-12 weeks after delivery. This gives parents an opportunity to bond with their newborn and allow the baby to grow healthy and strong.
Doctors prefer this approach because they believe that having the complete primary repair as soon as possible after birth allows for more normal bladder function to begin earlier, and gives your child the best chance for long-term continence that will last through adulthood.
Your child’s surgical team will include pediatric urologists and an orthopedic surgeon who work together to do the bladder exstrophy repair, collaborating on surgical techniques to optimize your child’s outcome.
After surgery, your child will be admitted to the hospital for approximately three weeks to allow him to heal. During this time your child will be in a hip spica cast that is split in half to allow access to the surgical incisions, skin and groin. Most children will be in the cast for about four weeks.
Bladder exstrophy surgery risks
Risks of anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots
- Infection
Risks with this procedure may include:
- Chronic urinary tract infections
- Sexual/erectile dysfunction
- Kidney problems
- Need for future surgeries
- Poor urinary control (incontinence)
Long-term outlook
The long-term goals for children with bladder exstrophy are to optimize daytime and nighttime urinary control, to preserve normal kidney function, and to optimize the appearance and function of the external genitalia. Your child may need additional surgery as she grows older to improve continence or to complete the genital reconstruction.
Surgical follow-up care for bladder exstrophy
After surgical repair of bladder exstrophy, your child will require lifelong follow-up care. After the initial surgery, your healthcare team will follow your family closely. Your child will be scheduled for regular follow-up visits and ultrasounds to ensure her bladder and kidneys continue to develop in a healthy and safe way.
In addition to the physical aspects of bladder exstrophy, there are emotional issues that arise for many children and their families throughout the course of the child’s development. For example, some children wonder how to explain their surgical scars to peers. Others struggle to manage issues related to their continence. Many parents experience very complicated feelings about having a child with a chronic medical condition. Dedicated psychologist can help your family and child deal with these challenges, and will remain available to you and your child throughout your care.
Expect children will have periods of time when things seem to be going well, and other times when the challenges of their medical condition seem to be a greater burden. Your healthcare team is available to your family as you manage these complex conditions over time.
Bladder exstrophy prognosis
Urinary control most often happens after the neck of the bladder is repaired. This surgery is not always successful. The child may need to repeat the surgery later on.
Even with repeat surgery, a few children will not have control of their urine. They may need catheterization.