Contents
What is blastomycosis
Blastomycosis is a fungal infection caused by a fungus called Blastomyces dermatitidis. Recent phylogenetic analysis suggests that Blastomyces dermatitidis may comprise two species, Blastomyces dermatitidis and Blastomyces gilchristii 1. The fungus lives in the environment, particularly in moist soil and in decomposing organic matter such as wood and leaves. Blastomyces mainly lives in areas of the United States and Canada 2 surrounding the Ohio and Mississippi River valleys, the Great Lakes and the Saint Lawrence River 3. A few blastomycosis cases have been reported from Africa 4 and India 5. People can get blastomycosis after breathing in the microscopic fungal spores (airborne conidia) from the air, often after participating in activities that disturb the soil. Although most people who breathe in the spores don’t get sick, some of those who do may have flu-like symptoms, and the infection can sometimes become serious if it is not treated. In some people, such as those who have weakened immune systems, the infection can become severe, especially if it spreads from the lungs to other organs.
Acute pulmonary blastomycosis can progress to acute respiratory distress syndrome (ARDS). Approximately 25 to 40% of symptomatic cases will develop extrapulmonary infection, which typically manifests as cutaneous, osteoarticular, genitourinary, or central nervous system disease 6.
Primary blastomycosis skin infection is uncommon but can result from traumatic inoculation 7.
Figure 1. Blastomycosis skin infection
Footnote: A 64-year-old man from New Brunswick, the eastern part of Canada, was referred to the dermatology department for a painless verrucous plaque (3.5 × 1.5 cm) on the helix of his left ear that evolved over the previous 5 months. Squamous cell carcinoma (SCC) was suggested by initial biopsy findings, which showed pseudoepitheliomatous hyperplasia. On analysis of specimens from a second biopsy, multiple broad-based budding yeasts compatible with Blastomyces dermatitidis were disclosed under special staining. The diagnosis of cutaneous blastomycosis was further confirmed by positive fungal cultures.
[Source 8 ]Is blastomycosis contagious?
No. Blastomycosis can’t spread between people or between people and animals.
Where does Blastomyces live?
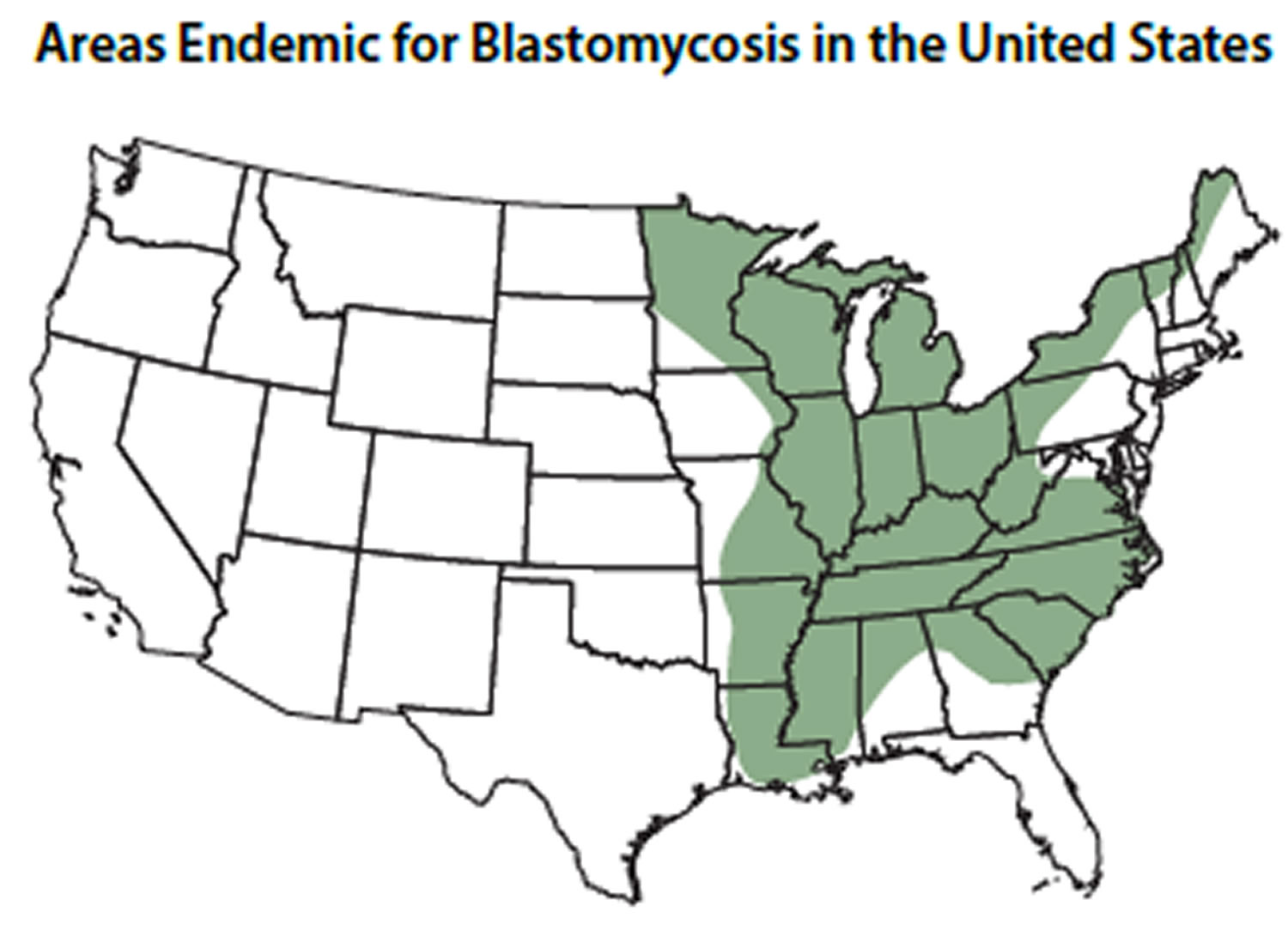
Blastomyces lives in the environment, particularly in moist soil and in decomposing organic matter such as wood and leaves. In the United States, the fungus mainly lives in the midwestern, south-central, and southeastern states, particularly in areas surrounding the Ohio and Mississippi River valleys, the Great Lakes, and the Saint Lawrence River 3. The fungus also lives in Canada 2 and a small number of blastomycosis cases have been reported from Africa 4 and India 5.
This map shows the approximate areas (called “endemic areas”) where Blastomyces is suspected to live in the United States. Cases of blastomycosis have also been reported from areas that are not shaded on the map.
Figure 2. Areas where Blastomyces is endemic
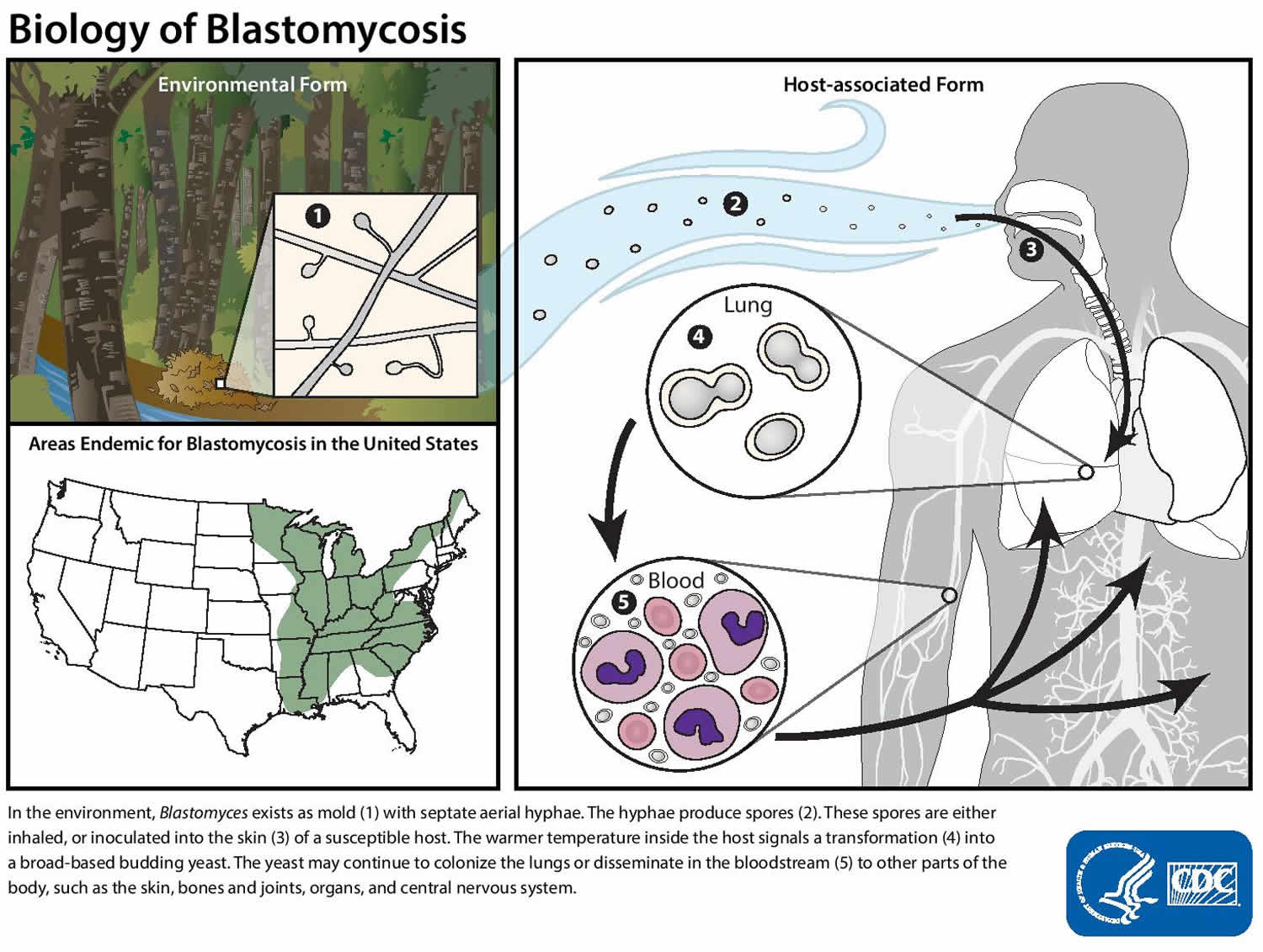
Blastomyces life cycle
Blastomyces lives in the environment as a mold that produces fungal spores. The spores are too small to see without a microscope. When people or animals breathe in the spores, they are at risk for developing blastomycosis. After the spores enter the lungs, the body temperature allows the spores to transform into yeast. The yeast can stay in the lungs or spread through the bloodstream to other parts of the body, such as the skin, bones and joints, organs, and central nervous system (brain and spinal cord).
Figure 3. Blastomyces life cycle
I’m worried that Blastomyces is in the soil near my home. Can someone test the environment to find out if the fungus is there?
No, in this situation, testing the environment for Blastomyces isn’t likely to be useful. When a soil sample tests positive for Blastomyces, it isn’t necessarily a source of infection, and when a sample tests negative, that doesn’t necessarily mean that the fungus isn’t in the soil. Also, there are no commercially-available tests to detect Blastomyces in the environment. Testing environmental samples for Blastomyces is currently only done for scientific research.
Who gets blastomycosis?
Anyone can get blastomycosis if they’ve been in an area where Blastomyces lives in the environment. People who participate in outdoor activities that expose them to wooded areas (such as forestry work, hunting, and camping) in these areas may be at higher risk for getting blastomycosis 9. People who have weakened immune systems may be more likely to develop severe blastomycosis than people who are otherwise healthy 10.
Blastomycosis in immunocompromised patients
Blastomyces dermatitidis appears no more likely to cause disease in a person with compromised cellular immunity than to cause disease in a normal host. The presence of natural defenses against inhaled conidia in the lung may explain this observation. When blastomycosis does occur in immunocompromised patients, the disease is more aggressive than in immunocompetent hosts 11. In one series, 30% of patients died of blastomycosis, and disseminated disease and involvement of the CNS (central nervous system) were relatively common 11. Among patients with AIDS, blastomycosis tends to be a severe illness with widespread dissemination, often including the CNS (central nervous system), and is associated with a high rate of early mortality 12. Miliary disease has occurred in the setting of HIV infection 13.
Can my pets get blastomycosis?
Yes. Pets, particularly dogs, can get blastomycosis, but it is not contagious between animals and people 14. The symptoms of blastomycosis in animals are similar to the symptoms in humans. If you are concerned about your pet’s risk of getting blastomycosis or if you think that your pet has blastomycosis, please talk to a veterinarian.
How can I prevent blastomycosis?
There is no vaccine to prevent blastomycosis, and it may not be possible to completely avoid being exposed to the fungus that causes blastomycosis in areas where it is common in the environment. People who have weakened immune systems may want to consider avoiding activities that involve disrupting soil in these areas.
Blastomycosis symptoms
Approximately half of people who are infected with the fungus Blastomyces will show symptoms 15. Symptoms of blastomycosis usually appear between 3 weeks and 3 months after a person breathes in the fungal spores 16.
The symptoms of blastomycosis are often similar to the symptoms of flu or other lung infections, and can include 9:
- Fever
- Cough
- Night sweats
- Muscle aches or joint pain
- Weight loss
- Chest pain
- Fatigue (extreme tiredness)
In some people (25%–40% of cases), particularly those who have weakened immune systems, blastomycosis can spread from the lungs to other parts of the body, such as the skin, bones and joints, and the central nervous system (the brain and spinal cord) 6. Disseminated blastomycosis occurs more frequently in immunosuppressed individuals, such as organ transplant recipients and those infected with HIV 17.
In the immunocompetent host, acute pulmonary blastomycosis can be mild and self-limited and may not require treatment 17. However, consideration should be given to treating all infected individuals to prevent extrapulmonary dissemination. All persons with moderate to severe pneumonia, disseminated infection, or immunocompromise require antifungal therapy.
Pulmonary Blastomycosis
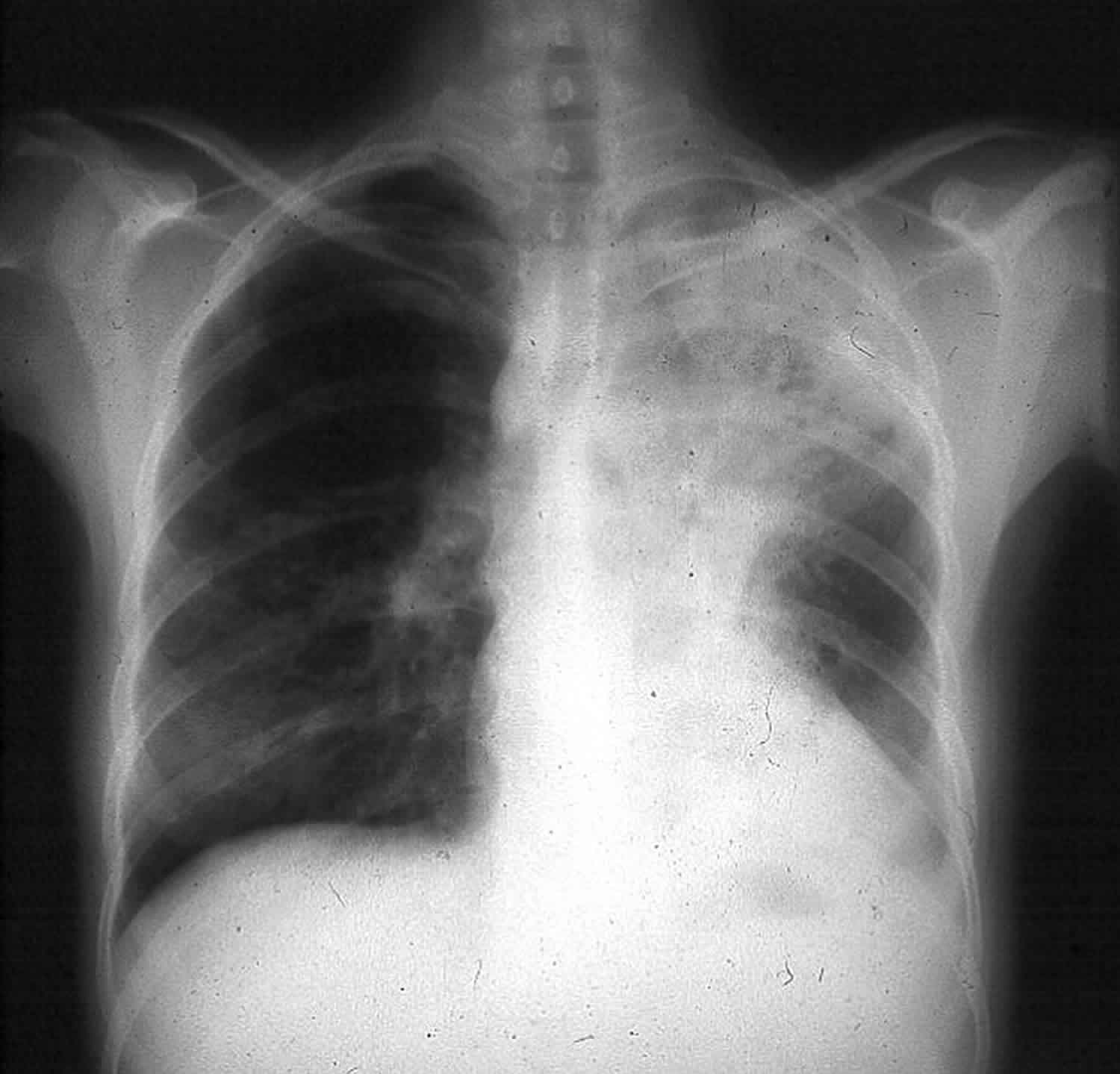
The majority of patients with blastomycosis, whether symptomatic or not, have an alveolar or mass-like infiltrate on chest radiography (Figure 4) 18. The specific location of the infiltrate is not particularly helpful diagnostically, although the upper lobes may be involved most often 19. Mass lesions mimic malignancy, so physicians in areas of endemicity must include blastomycosis in the initial differential diagnosis for a patient with presumed lung cancer. Reticulonodular and miliary radiographic patterns and solitary nodules are seen less often than alveolar and mass-like infiltrates. Cavitation of the lung parenchyma is uncommon relative to that seen with tuberculosis, histoplasmosis, and coccidioidomycosis. Although small pleural effusions may be present, massive effusions are uncommon 18.
Pulmonary blastomycosis presents clinically as acute pneumonia, chronic pneumonia, or an asymptomatic radiographic abnormality. Fever, chills, and productive cough, with or without hemoptysis, characterize acute pneumonia. This syndrome is indistinguishable from acute bacterial community-acquired pneumonia, and many patients receive antibacterial medications before the diagnosis of blastomycosis is considered 20. Among the subset of patients with acute pulmonary blastomycosis whose disease is self-limited, clinical improvement and resolution of pneumonia may be attributed mistakenly to effective antibacterial therapy.
A 2- to 6-month illness with weight loss, fever, night sweats, cough with sputum, and chest pain typifies chronic pneumonia 20. Mass-like pulmonary infiltrates may be more common in patients with chronic pneumonia 19. This illness may be misdiagnosed as pulmonary tuberculosis, chronic pulmonary histoplasmosis, or malignancy.
Miliary blastomycosis or endobronchial spread of infection can cause the adult respiratory distress syndrome (ARDS) with diffuse bilateral pulmonary infiltrates and noncardiogenic pulmonary edema 21. ARDS (adult respiratory distress syndrome) caused by pulmonary blastomycosis is associated with high mortality 22. In a series from Mississippi, 9 (∼8%) of 107 patients with pulmonary blastomycosis had ARDS (adult respiratory distress syndrome), and 7 (78%) of this number died of respiratory failure over a median course of about a week 23.
Figure 4. Pulmonary blastomycosis
Footnote: A chest radiograph from a patient with pulmonary blastomycosis showing opacification in the left upper lobe.
[Source 24 ]Extrapulmonary Blastomycosis
Blastomycosis skin infection
Skin involvement has been reported in 40% to 80% of cases 25. The skin manifestations of blastomycosis come in two forms, verrucous and ulcerative. Verrucous skin lesions, which lie above subcutaneous abscesses, are raised and crusted with an irregular shape and sharp borders (Figure 5). The gross appearance of these lesions can mimic basal cell cancer, squamous cell cancer, and giant keratoacanthoma 26. Histologically, there is papillomatosis with downward proliferation of the epidermis and formation of microabscesses 27. The presence of pseudoepitheliomatous hyperplasia and acanthosis (hyperplasia and diffuse thickening of the stratum spinosum of the epidermis) can be misleading, so it is important to look for yeast forms in biopsy specimens with a special stain, such as Grocott-Gomori methenamine silver nitrate 20. A cutaneous ulcer occurs when a subcutaneous abscess drains out through the skin. These ulcers have heaped-up borders with or without an exudative base. Microabscesses are present, even in lesions without overt clinical evidence of inflammation. Although less common than with disseminated histoplasmosis, mucosal lesions of the nose, mouth, or larynx can occur 28. Verrucous lesions of the pharynx may be confused with squamous cell cancer.
Figure 5. Verrucous cutaneous blastomycosis
Footnote: A chest radiograph from a patient with pulmonary blastomycosis showing opacification in the left upper lobe.
[Source 24 ]Blastomycosis bone infection
After the lungs and skin, bone is the third most common site of disease. Among patients with blastomycosis described in case series, the prevalence of bone disease ranges from approximately 6% to 48% 29. On average, osteomyelitis is present in approximately 25% of cases with extrapulmonary manifestations 20. About 75% of patients with osseous blastomycosis have pulmonary disease at the time of presentation 30. Although essentially any bone can be involved, the vertebrae, ribs, skull, and long bones are affected most commonly 31. Radiographically, osteomyelitis can appear as a clearly demarcated osteolytic lesion without periosteal involvement or as a diffuse, destructive process with periosteal new bone formation. Infection can spread into an adjacent joint, causing purulent arthritis 32. Extension into the soft tissues causes a painful subcutaneous abscess with draining sinuses.
Vertebral osteomyelitis due to blastomycosis most often affects the lower thoracic and lumbar regions of the spine although cervical, upper thoracic, and sacral involvement has been reported 33. Extension of infection from the spine, causing paravertebral or psoas abscess, is a frequent complication 34. All 8 patients with vertebral blastomycosis in one report had evidence of contiguous abscesses 33. As these abscesses track through soft tissues, subcutaneous masses can appear at any spinal level, in the flank, or in the thigh when a psoas abscess extends beneath the inguinal ligament. These purulent subcutaneous collections often drain through the skin, causing a chronic, discharging sinus or ulcer.
Blastomycosis genitourinary infection
Involvement of the genitourinary system is recognized in 10% to 30% of cases 29. Because men are more likely than women to have extrapulmonary blastomycosis, the most common genitourinary sites of disease are the prostate, the testicle, and the epididymis 35. Epididymo-orchitis causes swelling and pain, and prostatitis is associated with dysuria and symptoms of obstruction. Prostatic massage prior to collection of urine may enhance the yield of urine culture 36. Reported cases of female genitourinary blastomycosis include endometrial infection that occurred via transmission from a man with cutaneous blastomycosis of the penis 37 and tubo-ovarian abscess that occurred in the setting of reactivation disease 38. Peritoneal seeding with ascites may accompany tubo-ovarian abscess 39.
Blastomycosis central nervous system infection
Central nervous system (CNS) infection, in the form of meningitis or mass lesions, is apparent in 5% to 10% of cases of disseminated blastomycosis 40. Central diabetes insipidus has occurred in patients with blastomycosis 41. Pituitary involvement in conjunction with chronic meningitis, chronic pneumonia, and genitourinary infection resembles tuberculosis 42. The cerebrospinal fluid white cell differential may show neutrophilic predominance in patients with meningitis 43. Making the diagnosis of CNS blastomycosis is challenging; for example, in one series of patients with meningitis, culture of cerebrospinal fluid obtained via lumbar puncture yielded the diagnosis for only 2 of 22 patients 40. More-invasive procedures, such as brain biopsy and ventricular tap, are more likely to provide sufficient material for diagnosis 40. It is important to look for more-accessible sites of disease, such as the skin or lung, from which to obtain specimens for microscopic examination and culture.
Blastomycosis other sites of disease
Blastomyces dermatitidis can disseminate to virtually any organ system. As already mentioned, subcutaneous abscesses present as masses growing from deeper foci. Involvement of the reticuloendothelial system with lymphadenopathy or abscesses in the liver or spleen is well documented 44. Other uncommonly affected sites include the eye 45, the middle ear 46, the paranasal sinuses 47, breast tissue 48, the myocardium, the pericardium, and the gastrointestinal tract, as well as the thyroid and adrenal glands 26.
Blastomycosis diagnosis
Healthcare providers use your medical and travel history, symptoms, physical examinations, and laboratory tests to diagnose blastomycosis. A doctor will likely test for blastomycosis by taking a blood sample or a urine sample and sending it to a laboratory.
Healthcare providers may do imaging tests such as chest x-rays or CT scans of your lungs. No clinical or radiographic abnormalities are absolutely diagnostic of blastomycosis. The spectrum of disease that Blastomyces dermatitidis causes overlaps with those of other fungal pathogens and malignancy, and the clinical picture may be indistinguishable from tuberculosis 24. Therefore, visualization of characteristic yeast forms or growth of the fungus in culture is necessary to diagnose blastomycosis definitively.
Healthcare providersy may also collect a sample of fluid from your respiratory tract or perform a tissue biopsy, in which a small sample of affected tissue is taken from the body and examined under a microscope. Laboratories may also see if Blastomyces will grow from body fluids or tissues (this is called a culture).
Laboratory tests
- Antigen detection: Enzyme immunoassay (EIA) is typically performed on urine or serum, but can also be used on bronchoalveolar lavage fluid. Cross-reactions can occur with histoplasmosis and other fungal diseases.
- Antibody tests: antibody tests such as immunodiffusion (ID) and complement fixation (CF) are available, but have low sensitivity and specificity.
- Culture: the gold standard for diagnosing blastomycosis. A commercially available DNA probe (AccuProbe, GenProbe Inc.) can be used to confirm.
- Microscopy: important for detection of yeast in tissue or respiratory secretions.
- Polymerase chain reaction (PCR): Blastomyces PCR can be used to confirm culture or histopathologic identification and on blood to detect disseminated disease.
Where can I get tested for blastomycosis?
Most healthcare providers can order a test for blastomycosis.
How long will it take to get my test results?
It depends on the type of test. Results from a blood test or a urine test are usually available in a few days. If your healthcare provider sends a sample to a laboratory to be cultured, the results could take a couple of weeks.
Blastomycosis treatment
Most people with blastomycosis will need treatment with prescription antifungal medication. Itraconazole is a type of antifungal medication that is typically used to treat mild to moderate blastomycosis. Amphotericin B is usually recommended for severe blastomycosis in the lungs or infections that have spread to other parts of the body such as the central nervous system disease and in immunosuppressed patients or pregnant patients. Depending on the severity of the infection and the person’s immune status, the course of treatment can range from six months to one year 17.
Pulmonary Blastomycosis
- For moderately severe to severe disease, initial treatment with a lipid formulation of amphotericin B at a dosage of 3–5 mg/kg per day or amphotericin B deoxycholate at a dosage of 0.7–1 mg/kg per day for 1–2 weeks or until improvement is noted, followed by oral itraconazole, 200 mg 3 times per day for 3 days and then 200 mg twice per day, for a total of 6–12 months, is recommended 17.
- For mild to moderate disease, oral itraconazole, 200 mg 3 times per day for 3 days and then once or twice per day for 6–12 months, is recommended 17.
- Serum levels of itraconazole should be determined after the patient has received this agent for at least 2 weeks, to ensure adequate drug exposure 17.
Disseminated Extrapulmonary Blastomycosis
- For moderately severe to severe disease, lipid formulation amphotericin B, 3–5 mg/kg per day, or amphotericin B deoxycholate, 0.7–1 mg/kg per day, for 1–2 weeks or until improvement is noted, followed by oral itraconazole, 200 mg 3 times per day for 3 days and then 200 mg twice per day for a total of at least 12 months, is recommended 17.
- For mild to moderate disease, oral itraconazole, 200 mg 3 times per day for 3 days and then once or twice per day for 6–12 months, is recommended 17.
- Patients with osteoarticular blastomycosis should receive a total of at least 12 months of antifungal therapy 17.
- Serum levels of itraconazole should be determined after the patient has received this agent for at least 2 weeks, to ensure adequate drug exposure 17.
CNS Blastomycosis
- Amphotericin B, given as a lipid formulation at a dosage of 5 mg/kg per day over 4–6 weeks followed by an oral azole, is recommended. Possible options for azole therapy include fluconazole, 800 mg per day, itraconazole, 200 mg 2 or 3 times per day, or voriconazole, 200–400 mg twice per day, for at least 12 months and until resolution of CSF abnormalities 17.
Treatment for Immunosuppressed Patients with Blastomycosis
- Amphotericin B, given as a lipid formulation, 3–5 mg/kg per day, or amphotericin B deoxycholate, 0.7–1 mg/kg per day, for 1–2 weeks or until improvement is noted, is recommended as initial therapy for patients who are immunosuppressed, including those with AIDS 17.
- Itraconazole, 200 mg 3 times per day for 3 days and then twice per day, is recommended as step-down therapy after the patient has responded to initial treatment with amphotericin B and should be given to complete a total of at least 12 months of therapy 17.
- Serum levels of itraconazole should be determined after the patient has received this agent for at least 2 weeks, to ensure adequate drug exposure 17.
- Lifelong suppressive therapy with oral itraconazole, 200 mg per day, may be required for immunosuppressed patients if immunosuppression cannot be reversed and in patients who experience relapse despite appropriate therapy 17.
Treatment for Blastomycosis in Pregnant Women and in Children
- During pregnancy, lipid formulation amphotericin B, 3–5 mg/kg per day, is recommended 17. Azoles should be avoided because of possible teratogenicity 17.
- If the newborn shows evidence of infection, treatment is recommended with amphotericin B deoxycholate, 1.0 mg/kg per day 17.
- For children with severe blastomycosis, amphotericin B deoxycholate, 0.7–1.0 mg/kg per day, or lipid formulation amphotericin B, at a dosage of 3–5 mg/kg per day, is recommended for initial therapy, followed by oral itraconazole, 10 mg/kg per day (up to 400 mg per day) as step-down therapy, for a total of 12 months 17.
- For children with mild to moderate infection, oral itraconazole, at a dosage of 10 mg/kg per day (to a maximum of 400 mg orally per day) for 6–12 months, is recommended 17.
- Serum levels of itraconazole should be determined after the patient has received this agent for at least 2 weeks, to ensure adequate drug exposure 17.
- Brown EM, McTaggart LR, Zhang SX, Low DE, Stevens DA, Richardson SE. Phylogenetic analysis reveals a cryptic species Blastomyces gilchristii, sp. nov. within the human pathogenic fungus Blastomyces dermatitidis. PLoS One. 2013;8(3):e59237.[↩]
- Litvinov IV, St-Germain G, Pelletier R, Paradis M, Sheppard DC. Endemic human blastomycosis in Quebec, Canada, 1988-2011. Epidemiol Infect. 2013 Jun;141(6):1143-7.[↩][↩]
- Bradsher RW, Chapman SW, Pappas PG. Blastomycosis. Infect Dis Clin North Am. 2003;17(1) 21-40, vii.[↩][↩]
- Cheikh Rouhou S, Racil H, Ismail O, Trabelsi S, Zarrouk M, Chaouch N, et al. Pulmonary blastomycosis: a case from Africa. ScientificWorldJournal. 2008 Nov 2;8:1098-103.[↩][↩]
- Chakrabarti A, Slavin MA. Endemic fungal infections in the Asia-Pacific region. Med Mycol. 2011 May;49(4):337-44.[↩][↩]
- Chapman SW, Dismukes WE, Proia LA, Bradsher RW, Pappas PG, Threlkeld MG, et al. Clinical practice guidelines for the management of blastomycosis: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2008 Jun 15;46(12):1801-12.[↩][↩]
- Gray NA, Baddour LM. Cutaneous inoculation blastomycosis. Clin Infect Dis. 2002 May 15;34(10):E44-9.[↩]
- Auger I, Gagné É, Alain J, Pelletier R. Cutaneous Blastomycosis: A Clue for Reassessing the Recent Diagnosis of Pulmonary Sarcoidosis. Arch Dermatol. 2006;142(6):781–798. doi:10.1001/archderm.142.6.795[↩]
- Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010 Apr;23(2):367-81.[↩][↩]
- Pappas PG, Threlkeld MG, Bedsole GD, Cleveland KO, Gelfand MS, Dismukes WE. Blastomycosis in immunocompromised patients. Medicine. 1993;72(5):311–25.[↩]
- Pappas, P. G., M. G. Threlkeld, G. D. Bedsole, K. O. Cleveland, M. S. Gelfand, and W. E. Dismukes. 1993. Blastomycosis in immunocompromised patients. Medicine (Baltimore) 72:311-325.[↩][↩]
- Pappas, P. G., J. C. Pottage, W. G. Powderly, V. J. Fraser, C. W. Stratton, S. McKenzie, M. L. Tapper, H. Chmel, F. C. Bonebrake, R. Blum, R. W. Shafer, C. King, and W. E. Dismukes. 1992. Blastomycosis in patients with the acquired immunodeficiency syndrome. Ann. Intern. Med. 116:847-853.[↩]
- Herd, A. M., S. B. Greenfield, G. W. S. Thompson, and R. C. Brunham. 1990. Miliary blastomycosis and HIV infection. Can. Med. Assoc. J. 143:1329-1330.[↩]
- Brömel C, Sykes JE. Epidemiology, diagnosis, and treatment of blastomycosis in dogs and cats. Clin Tech Small Anim Pract. 2005 Nov;20(4):233-9.[↩]
- Klein BS, Vergeront JM, Weeks RJ, Kumar UN, Mathai G, Varkey B, et al. Isolation of Blastomyces dermatitidis in soil associated with a large outbreak of blastomycosis in Wisconsin. N Engl J Med. 1986 Feb 27;314(9):529-34.[↩]
- Klein BS, Vergeront JM, Davis JP. Epidemiologic aspects of blastomycosis, the enigmatic systemic mycosis. Semin Respir Infect. 1986 Mar;1(1):29-39.[↩]
- Stanley W. Chapman, William E. Dismukes, Laurie A. Proia, Robert W. Bradsher, Peter G. Pappas, Michael G. Threlkeld, Carol A. Kauffman; Clinical Practice Guidelines for the Management of Blastomycosis: 2008 Update by the Infectious Diseases Society of America, Clinical Infectious Diseases, Volume 46, Issue 12, 15 June 2008, Pages 1801–1812, https://doi.org/10.1086/588300[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bradsher, R. W., D. C. Rice, and R. S. Abernathy. 1985. Ketoconazole therapy for endemic blastomycosis. Ann. Intern. Med. 103:872-879.[↩][↩]
- Patel, R. G., B. Patel, M. F. Petrini, R. R. Carter, and J. Griffith. 1999. Clinical presentation, radiographic findings, and diagnostic methods of pulmonary blastomycosis: a review of 100 consecutive cases. South. Med. J. 92:289-295.[↩][↩]
- Bradsher, R. W. 1988. Blastomycosis. Infect. Dis. Clin. North Am. 2:877-898.[↩][↩][↩][↩]
- Amini, M., W. E. Shams, T. Barklow, and F. A. Sarubbi. 2007. A 45-year-old man with fever and adult respiratory distress syndrome. Clin. Infect. Dis. 44:566-567, 615-616.[↩]
- Meyer, K. C., E. J. McManus, and D. G. Maki. 1993. Overwhelming pulmonary blastomycosis associated with the adult respiratory distress syndrome. N. Engl. J. Med. 329:1231-1236.[↩]
- Lemos, L. B., M. Baliga, and M. Guo. 2001. Acute respiratory distress syndrome and blastomycosis: presentation of nine cases and review of the literature. Ann. Diagn. Pathol. 5:1-9.[↩]
- Clinical and Laboratory Update on Blastomycosis. Michael Saccente, Gail L. Woods. Clinical Microbiology Reviews Apr 2010, 23 (2) 367-381; DOI: 10.1128/CMR.00056-09 https://cmr.asm.org/content/23/2/367[↩][↩][↩]
- Witorsch, P., and J. P. Utz. 1968. North American blastomycosis: a study of 40 patients. Medicine 47:169-200.[↩]
- Bradsher, R. W., M. R. Martin, T. D. Wilkes, C. Waltman, and K. Bolyard. 1990. Unusual presentations of blastomycosis: ten case summaries. Infect. Med. 7:10-19.[↩][↩]
- Schwarz, J., and K. Salfelder. 1977. Blastomycosis: a review of 152 cases. Curr. Top. Pathol. 65:165-200.[↩]
- Suen, J. Y., S. J. Wetmore, and W. J. Wetzel. 1980. Blastomycosis of the larynx. Ann. Otol. 89:563-566.[↩]
- Busey, J. F. 1972. Blastomycosis: a comparative study of 2-hydroxystilbamidine and amphotericin B therapy. Am. Rev. Respir. Dis. 105:812-818.[↩][↩]
- Gehweiler, J. A., M. P. Capp, and E. W. Chick. 1970. Observations on the roentgen patterns in blastomycosis of bone. Am. J. Roentgenol. 108:497-510.[↩]
- Bassett, F. H., and J. P. Tindall. 1972. Blastomycosis of bone. South. Med. J. 65:547-555.[↩]
- Sanders, L. L. 1967. Blastomycosis arthritis. Arthritis Rheum. 10:91-98.[↩]
- Saccente, M., R. S. Abernathy, P. G. Pappas, H. R. Shah, and R. W. Bradsher. 1998. Vertebral blastomycosis with paravertebral abscess: report of eight cases and review of the literature. Clin. Infect. Dis. 26:413-418.[↩][↩]
- Nokes, S. R., J. Adametz, G. Gardner, and J. N. Beaton. 1995. Radiology case of the month: blastomycosis osteomyelitis with epidural and retropharyngeal abscess. J. Ark. Med. Soc. 92:253-254.[↩]
- Sarosi, G. A., and S. F. Davies. 1979. Blastomycosis: state of the art. Am. Rev. Respir. Dis. 120:911-938.[↩]
- Inoshita, T., G. A. Youngberg, L. J. Boelen, and J. Langston. 1983. Blastomycosis presenting with prostatic involvement: report of 2 cases and review of the literature. J. Urol. 130:160-162.[↩]
- Farber, E. R., M. S. Leahy, and T. R. Meadows. 1968. Endometrial blastomycosis acquired by sexual contact. Obstet. Gynecol. 32:195-199.[↩]
- Murray, J. J., C. A. Clark, R. H. Lands, C. R. Heim, and L. S. Burnett. 1984. Reactivation blastomycosis presenting as a tuboovarian abscess. Obstet. Gynecol. 64:828-830.[↩]
- Mouzin, E. L., and M. A. Beilke. 1996. Female genitourinary blastomycosis: case report and review. Clin. Infect. Dis. 22:718-719.[↩]
- Kravitz, G. R., S. F. Davies, M. R. Eckman, and G. A. Sarosi. 1981. Chronic blastomycosis meningitis. Am. J. Med. 71:501-505.[↩][↩][↩]
- Kelly, P. M. 1982. Systemic blastomycosis with associated diabetes insipidus. Ann. Intern. Med. 96:66-67.[↩]
- Morse, H. G., W. P. Nichol, D. M. Cook, N. K. Blank, and T. T. Ward. 1983. Central nervous system and genitourinary blastomycosis: confusion with tuberculosis. West. J. Med. 139:99-103.[↩]
- Harley, W. B., M. Lomis, and D. W. Haas. 1994. Marked polymorphonuclear pleocytosis due to blastomycotic meningitis: case report and review. Clin. Infect. Dis. 18:816-818.[↩]
- Blastomycosis Cooperative Study of the Veterans Administration. 1964. Blastomycosis: a review of 198 collected cases in Veterans Administration hospitals. Am. Rev. Respir. Dis. 89:659-672.[↩]
- Lopez, R., J. O. Mason, J. S. Parker, and P. G. Pappas. 1994. Intraocular blastomycosis: case report and review. Clin. Infect. Dis. 18:805-807.[↩]
- Istorico, L. J., M. Sanders, R. F. Jacobs, S. Gilleon, C. Glasier, and R. W. Bradsher. 1992. Otitis media due to blastomycosis: report of two cases. Clin. Infect. Dis. 14:355-358.[↩]
- Witzig, R. S., E. M. Quimosing, W. L. Campbell, D. L. Greer, and R. A. Clark. 1994. Blastomyces dermatitidis infection of the paranasal sinuses. Clin. Infect. Dis. 18:267-268.[↩]
- Farmer, C., M. W. Stanley, R. H. Bardales, S. Korourian, H. Shah, R. Bradsher, and V. S. Klimberg. 1995. Mycoses of the breast: diagnosis by fine-needle aspiration. Diagn. Cytopathol. 12:51-55.[↩]