Contents
What is a bowel resection
Bowel resection is also called partial colectomy, is an operation that removes a diseased or damaged part of the colon (large intestine) or rectum. Bowel resection can be done for many diseases that affect the colon, such as colorectal cancer, diverticulitis, or Crohn’s disease.
- Removal of the entire colon and the rectum is called a proctocolectomy.
- Removal of all of the colon but not the rectum is called subtotal colectomy.
- Removal of part of the colon but not the rectum is called a partial colectomy.
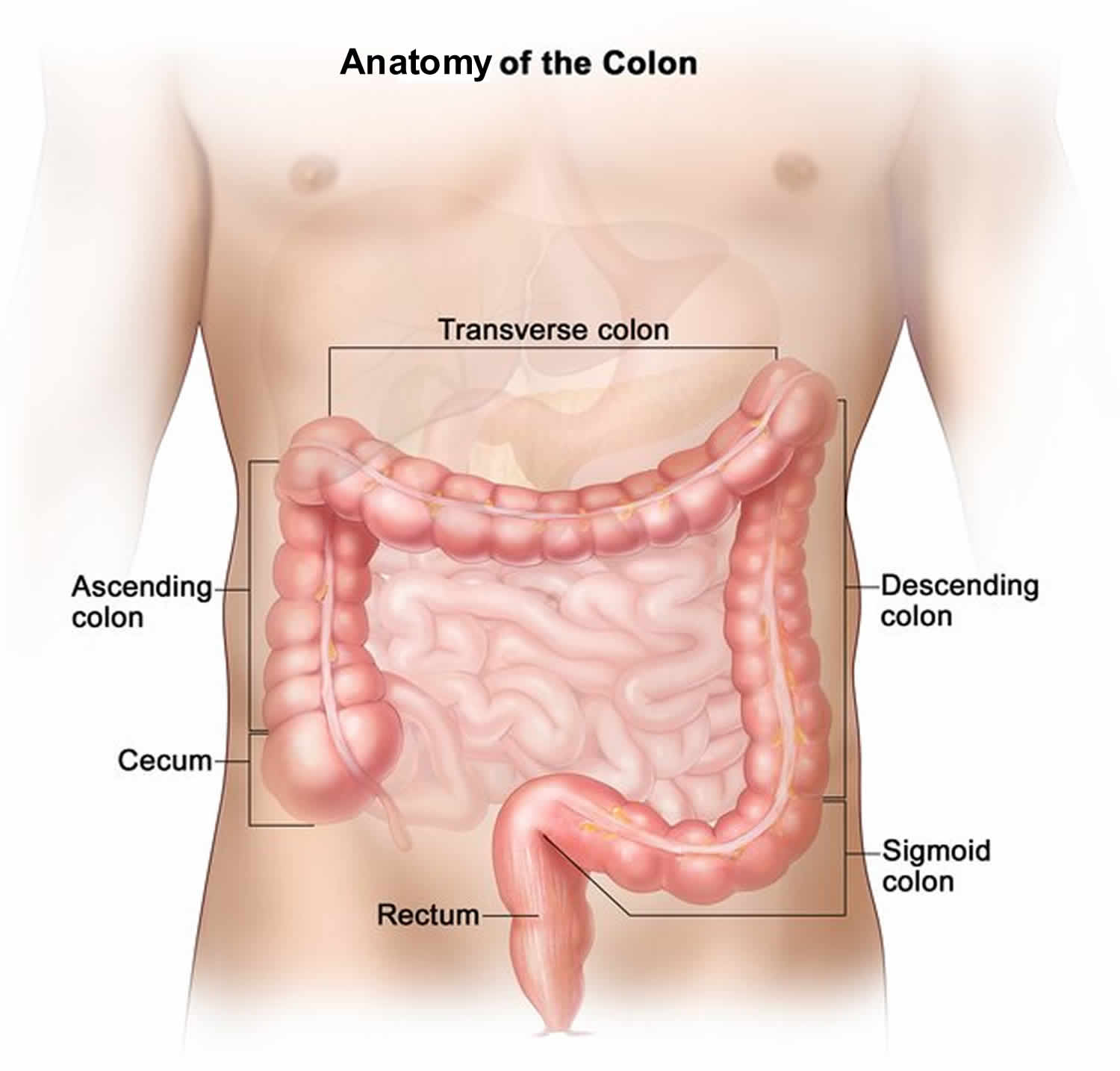
The large bowel connects the small intestine to the anus. Normally, stool passes through the large bowel before leaving the body through the anus (see Figure 1).
The goal of bowel resection is to take out the part of the colon or rectum where the problem is. If the doctor is removing cancer from the colon, nearby lymph nodes are taken out and tested for cancer. Then healthy parts of the colon or rectum are sewn back together. Bowel resection is done either by opening the abdomen (open resection) or by laparoscopy.
Laparoscopy for bowel resection usually involves 3 to 6 very small incisions instead of one large one. Recovery time is faster.
You and your doctor will think about several things in deciding whether you should have open bowel resection or a laparoscopic bowel resection. These include:
- The location and extent of the disease.
- Your general health.
- Whether you have scar tissue in the area from previous surgery.
- Your doctor’s expertise and experience.
Sometimes a laparoscopic surgery has to be changed to an open bowel resection during the surgery.
Figure 1. Large intestine anatomy
Why is bowel resection done?
Bowel resection may be done to remove cancer or when the colon cannot function normally because of damage or disease. You may need a bowel resection if you have:
- A bowel obstruction.
- Colon cancer.
- Crohn’s disease.
- Diverticulitis.
Bowel resection is the most successful treatment for invasive colorectal cancer. Up to 12 out of 100 people who have bowel resection surgery for diverticulitis develop diverticulitis again 1. But another surgery is usually not needed.
Some people who have two-stage bowel resection surgeries may not have the second part of the surgery to reattach the intestine and repair the colostomy. This is often because the intestine does not heal well enough to be rejoined 2.
Bowel resection surgery is not a cure for Crohn’s disease. When surgery for Crohn’s is needed, as little of the large intestine as possible is removed to keep the intestines working normally. Crohn’s disease tends to return to other areas of the intestines after surgery. In children, bowel resection surgery may improve well-being and quality of life and restore normal growth and sexual development.
Large bowel resection reasons
Large bowel resection is used to treat many conditions, including:
- A blockage in the intestine due to scar tissue
- Colon cancer
- Diverticular disease (disease of the large bowel)
Other reasons for bowel resection are:
- Familial polyposis (polyps are growths on the lining of the colon or rectum)
- Injuries that damage the large bowel
- Intussusception (when one part of the intestine pushes into another)
- Precancerous polyps
- Severe gastrointestinal bleeding
- Twisting of the bowel (volvulus)
- Ulcerative colitis
- Bleeding from the large intestine
- Lack of nerve function to the large intestine
Before the bowel resection procedure
Tell your surgeon or nurse what medicines you are taking, even drugs, supplements, or herbs you bought without a prescription.
Talk with your surgeon or nurse about how surgery will affect:
- Intimacy and sexuality
- Pregnancy
- Sports
- Work
During the 2 weeks before your surgery:
- You may be asked to stop taking blood thinner drugs. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and others.
- Ask the surgeon which drugs you should still take on the day of your surgery.
- If you smoke, try to stop. Smoking increases the risk for problems such as slow healing. Ask your doctor or nurse for help quitting.
- Tell the surgeon right away if you have a cold, flu, fever, herpes breakout, or other illness before your surgery.
- You may be asked to go through a bowel preparation to clean your intestines of all stool. This may involve staying on a liquid diet for a few days and using laxatives.
The day before your bowel resection surgery:
- You may be asked to drink only clear liquids such as broth, clear juice, and water.
- Follow instructions about when to stop eating and drinking.
On the day of your bowel resection surgery:
- Take the drugs your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
Large bowel resection surgery procedure
You’ll receive general anesthesia at the time of your surgery. This will keep you asleep and pain-free.
The surgery can be performed laparoscopically or with open surgery. Depending on which surgery you have, the surgeon will make one or more cuts (incisions) in your belly.
If you have laparoscopic bowel resection surgery:
- The surgeon makes 3 to 5 small cuts (incisions) in your belly. A medical device called a laparoscope is inserted through one of the cuts. The scope is a thin, lighted tube with a camera on the end. It lets the surgeon see inside your belly. Other medical instruments are inserted through the other cuts.
- A cut of about 2 to 3 inches (5 to 7.6 centimeters) may also be made if your surgeon needs to put his or her hand inside your belly to feel or remove the diseased bowel.
- Your belly is filled with a harmless gas to expand it. This makes the area easier to see and work in.
- The surgeon examines the organs in your belly to see if there are any problems.
- The diseased part of your large bowel is located and removed. Some lymph nodes may also be removed.
If you have open bowel resection surgery:
- The surgeon makes a cut of 6 to 8 inches (15.2 to 20.3 centimeters) in your lower belly.
- The organs in your belly are examined to see if there are any problems.
- The diseased part of your large bowel is located and removed. Some lymph nodes may also be removed.
In both kinds of surgery, the next steps are:
- If there is enough healthy large intestine left, the ends are stitched or stapled together. This is called an anastomosis. Most patients have this done.
- If there is not enough healthy large intestine to reconnect, the surgeon makes an opening called a stoma through the skin of your belly. The colon is attached to the outer wall of your belly. Stool will go through the stoma into a drainage bag outside your body. This is called a colostomy. The colostomy may be either short-term or permanent.
Large bowel resection surgery usually takes between 1 and 4 hours.
Bowel resection recovery
Bowel resection requires general anesthesia. You may stay in the hospital for 3 to 7 days or as long as 2 weeks after bowel resection surgery. You may have to stay longer if the colectomy was an emergency operation. You may also need to stay longer if a large amount of your large intestine was removed or you develop problems.
By the second or third day, you will probably be able to drink clear liquids. Thicker fluids and then soft foods will be added as your bowel begins to work again.
After you go home, follow instructions on how to take care of yourself as you heal.
Sometimes the two parts of the colon or rectum cannot be reattached, so the surgeon performs a colostomy. This creates an opening, called a stoma, on the outside of your body for the stool, or feces, to pass through into a colostomy bag. Usually the colostomy is temporary, until the colon or rectum heals. If the lower part of the rectum has been removed, the colostomy is permanent.
When the two-stage operation is done, the time between operations is usually 6 to 12 weeks.
Bowel resection recovery time
The recovery time after a one-stage bowel resection surgery or after the final operation of a two-stage bowel resection surgery is usually 6 to 8 weeks.
Bowel resection diet
If you have had part of your colon removed after a bowel cancer diagnosis, it is likely that your stools (poop) will be looser because one of the functions of the colon is to absorb water from the stools. This may mean that you experience repeated episodes of diarrhea or urgency – when you need to go, you need to go now.
You should inform your healthcare team if diarrhea becomes a problem because medication is available to help control symptoms.
You may find some foods upset your bowels, particularly during the first few months after your bowel resection surgery.
Different foods can upset different people, but food and drink that is commonly known to cause problems include:
- fruit and vegetables that are high in fiber, such as beans, cabbages, apples and bananas
- carbonated (soft) drinks and beer.
You may find it useful to keep a food diary to record the effects of different foods on your bowel.
If you find that you are having continual problems with your bowels as a result of your diet, or you are finding it difficult to maintain a healthy diet, you should contact your doctor. You may need to be referred to a dietitian for further advice.
YOU CAN EAT
- White bread and pasta
- Refined cereals – rice bubbles, cornflakes
- White rice
- Milk, smooth yogurt, ice cream
- Rice pudding, semolina, tapioca
- Soups and sauces (strained), clear soups and stock
- Cheese
- Tender, lean meat, poultry, fish
- Eggs
- Oil, margarine, butter and mayonnaise
- Fruit juices (except prune juice)
- Vegetable juices
- Smooth peanut butter – up to two tablespoons a day
- Fats, oils and dressings without seeds
- Desserts with no seeds or nuts
- Smooth jam, honey
LOW-FIBER VEGETABLES THAT CAN BE EATEN RAW:
- Avocado (1/4 – 1/2)
- Lettuce – soft
- Cucumber (no skin or seeds)
LOW FIBER VEGETABLES THAT CAN BE EATEN IF WELL COOKED (NO SKIN OR SEEDS):
- Carrots
- Tomatoes
- Potatoes
- Asparagus tips
- Pureed spinach
- Eggplant – peeled
- Green beans
YOU SHOULD AVOID:
- Wholegrain bread and pasta
- Brown or wild rice
- Wholegrain cereals – porridge, muesli, weetabix, branflakes
- Yogurt, pudding and ice cream with nuts or pieces of fruit
- Soups with pieces of vegetable
- Tough or coarse meats with gristle
- Fatty foods
- Chunky peanut butter
- Coconut
- Marmalade with shreds
- Dried fruits
- Dried beans or peas (pulses)
- Baked beans
- Seeds and nuts
- Popcorn
- Pickles
- Horseradish
VEGETABLES TO AVOID:
- Broccoli
- Cauliflower
- Brussels sprouts
- Cabbage
- Peas
- Squashes
- Pulses and legumes
- Sweetcorn
FRUITS TO AVOID:
- Pineapple
- Figs
- Berries of any kind
- Coconut
- Dried fruits
- Prunes
Colostomy diet
In the first few weeks after having a colostomy, you’ll probably be advised to have a low-fiber diet. When you are on a low-fiber diet, you will eat foods that do not have much fiber and are easy to digest.
This is because a high-fiber diet can increase the size of your stools, which can temporarily block your bowel. After around eight weeks, you’ll usually be able to go back to a normal diet.
As you recover, you can start to eat a healthy, balanced diet that includes plenty of fresh fruit and vegetables.
You should be able to return to the diet you previously enjoyed. If you previously had a restricted diet, you should be able to reintroduce the restricted foods.
Low fiber diet
A low-fiber diet can include foods you are used to eating, like cooked vegetables, fruits, white breads, and meats.
Choose foods that are lower in fat and added sugar when following a low-fiber diet.
Because a low-fiber diet does not have the variety of foods that your body normally needs to stay healthy, you may have to take supplements, such as a multi-vitamin. Check with your doctor or dietitian.
A low-fiber diet does NOT include foods that are higher in fiber or cause gas such as:
- Beans and legumes
- Whole grains
- Many raw vegetables and fruits or their juices
- Fruit and vegetable skins
- Nuts and seeds
- The connective tissues of meats
This diet can provide your body’s needed:
- Protein
- Fluid
- Salt
- Vitamins and minerals
Your doctor or dietitian will likely tell you not to eat more than a certain number of grams of fiber a day, such as 10 to 15 grams (g).
Below are some of the foods recommended for a low-fiber diet. It is still possible for some of these foods to upset your system. Talk to your doctor or dietitian if a food is making your problem worse.
Milk products:
- You may have yogurt, kefir, cottage cheese, milk, pudding, creamy soup, or 1.5 ounces (43 g) of hard cheese. If you are lactose intolerant, use lactose-free products.
- Avoid milk products with nuts, seeds, fruit, vegetables, or granola added to them.
Breads and grains:
- You may have refined white breads, dry cereals (such as puffed rice, corn flakes), farina, white pasta, and crackers. Make sure these foods have less than 2 grams of fiber per serving.
- DO NOT eat whole-grain breads, crackers, cereals, whole-wheat pasta, brown rice, barley, oats, or popcorn.
Vegetables: You may eat these vegetables raw:
- Lettuce (shredded, in small quantities at first)
- Cucumbers (without seeds or skin)
- Zucchini
You can eat these vegetables if they are well-cooked or canned (without seeds). You can also drink juices made from them if they do not contain seeds or pulp:
- Yellow squash (without seeds)
- Spinach
- Pumpkin
- Eggplant
- Potatoes, without skin
- Green beans
- Wax beans
- Asparagus
- Beets
- Carrots
DO NOT eat any vegetable that is not on the list above. DO NOT eat vegetables raw that are okay to eat cooked. DO NOT eat fried vegetables. Avoid vegetables and sauces with seeds.
Fruits:
- You may have fruit juices without pulp and many canned fruits or fruit sauces, such as applesauce. Avoid fruits canned in heavy syrup.
- Raw fruits you can have are very ripe apricots, bananas and cantaloupe, honeydew melon, watermelon, nectarines, papayas, peaches, and plums. Avoid all other raw fruit.
- Avoid canned and raw pineapple, fresh figs, berries, all dried fruits, fruit seeds, and prunes and prune juice.
Protein:
- You may eat cooked meat, fish, poultry, eggs, smooth peanut butter, and tofu. Make sure your meats are tender and soft, not chewy with gristle.
- Avoid deli meats, hot dogs, sausage, crunchy peanut butter, nuts, beans, tempeh, and peas.
Fats, oils, and sauces:
- You may eat butter, margarine, oils, mayonnaise, whipped cream, and smooth sauces and dressings.
- Smooth condiments are OK.
- Don’t eat very spicy or acidic foods and dressings.
- Avoid chunky relishes and pickles.
- Don’t eat deep-fried foods.
Other foods and drinks:
- Don’t eat desserts that have nuts, coconut, or fruits that are not OK to eat.
- Make sure you are drinking enough fluids, particularly if you are having diarrhea.
- Your doctor or dietitian will likely recommend that you also avoid caffeine and alcohol.
Bowel resection complications
All surgeries have some risks of infection, severe bleeding, or complications from general anesthesia.
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Blood clots, bleeding, infection
Possible complications after a bowel resection include:
- Bleeding inside your belly
- Bulging tissue through the surgical cut, called an incisional hernia
- Damage to nearby organs in the body or blood vessels
- Damage to the ureters or bladder
- Problems with the colostomy
- Scar tissue (adhesions) that forms in the belly and causes a blockage of the intestines
- A leak between the joined edges of your intestines that are sewn together come open (anastomotic leak), which may be life threatening
- Wound breaking open
- Wound infection
- Peritonitis
Bowel resection does not usually cause problems, even in older people. Age should not be a reason to avoid having a bowel resection.
People who have colostomies need instructions about caring for the collection bag and about dietary changes that can reduce odor and gas. They also need emotional support, because many people find having a colostomy embarrassing.
Bowel resection prognosis
Most people who have a large bowel resection recover fully. Even with a colostomy, most people are able to do the activities they were doing before their surgery. This includes most sports, travel, gardening, hiking, other outdoor activities, and most types of work.
If you have a long-term (chronic) condition, such as cancer, Crohn disease, or ulcerative colitis, you may need ongoing medical treatment.
Small bowel resection
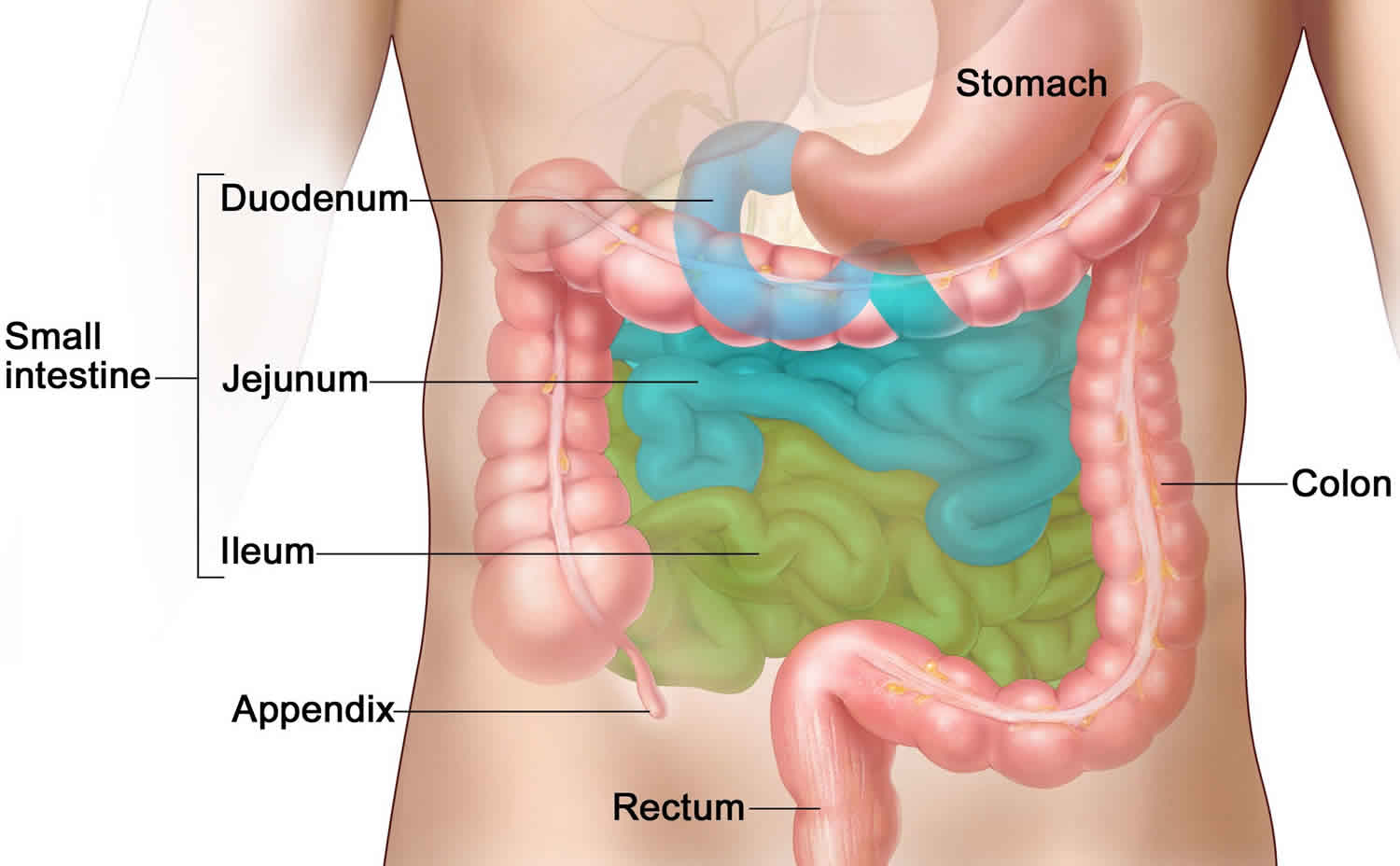
Small bowel resection is surgery to remove part or all of your small bowel (small intestines). Small bowel resection surgery is done when part of your small bowel is blocked or diseased.
The small bowel is also called the small intestine. Most digestion (breaking down and absorbing nutrients) of the food you eat takes place in the small intestine.
Figure 2. Small intestine anatomy
Why is small bowel resection done?
Small bowel resection is used to treat:
- A blockage in the intestine caused by scar tissue or congenital (from birth) deformities
- Bleeding, infection, or ulcers caused by inflammation of the small intestine from conditions such as Crohn disease
- Cancer
- Carcinoid tumor
- Injuries to the small intestine
- Meckel diverticulum (a pouch on the wall of the lower part of the intestine that is present at birth)
- Noncancerous (benign) tumors
- Precancerous polyps
Before the small bowel resection procedure
Tell your surgeon or nurse what medicines you are taking, even drugs, supplements, or herbs you bought without a prescription.
Talk with your surgeon or nurse about how surgery will affect:
- Intimacy and sexuality
- Pregnancy
- Sports
- Work
During the 2 weeks before your small bowel resection surgery:
- You may be asked to stop taking blood thinner drugs. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and others.
- Ask the surgeon which drugs you should still take on the day of your surgery.
- If you smoke, try to stop. Smoking increases the risk for problems such as slow healing. Ask your doctor or nurse for help quitting.
- Tell your surgeon right away if you have a cold, flu, fever, herpes breakout, or other illness before your surgery.
- You may be asked to go through a bowel preparation to clean your intestines of all stool. This may involve staying on a liquid diet for a few days and using laxatives.
The day before small bowel resection surgery:
- You may be asked to drink only clear liquids such as broth, clear juice, and water.
- Follow instructions about when to stop eating and drinking.
On the day of small bowel resection surgery:
- Take the drugs your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
Small bowel resection surgery procedure
You will receive general anesthesia at the time of your small bowel resection surgery. This will keep you asleep and pain-free.
Small bowel resection surgery can be performed laparoscopically or with open surgery.
If you have laparoscopic small bowel resection surgery:
- The surgeon makes 3 to 5 small cuts (incisions) in your lower belly. A medical device called a laparoscope is inserted through one of the cuts. The scope is a thin, lighted tube with a camera on the end. It lets the surgeon see inside your belly. Other medical instruments are inserted through the other cuts.
- A cut of about 2 to 3 inches (5 to 7.6 centimeters) may also be made if your surgeon needs to put his or her hand inside your belly to feel the intestine or remove the diseased segment.
- Your belly is filled with a harmless gas to expand it. This makes it easy for the surgeon to see and work.
- The diseased part of your small intestine is located and removed.
If you have open small bowel resection surgery:
- The surgeon makes a cut of 6 to 8 inches (15.2 to 20.3 centimeters) in your mid-belly.
- The diseased part of your small intestine is located and removed.
In both kinds of surgery, the next steps are:
- If there is enough healthy small intestine left, the ends are stitched or stapled together. This is called an anastomosis. Most patients have this done.
- If there is not enough healthy small intestine to reconnect, your surgeon makes an opening called a stoma through the skin of your belly. The small intestine is attached to the outer wall of your belly. Stool will go through the stoma into a drainage bag outside your body. This is called an ileostomy. The ileostomy may be either short-term or permanent.
Small bowel resection usually takes 1 to 4 hours.
Small bowel resection recovery time
You will be in the hospital for 3 to 7 days. You may have to stay longer if your surgery was an emergency operation.
You also may need to stay longer if a large amount of your small intestine was removed or you develop problems.
By the second or third day, you will most likely be able to drink clear liquids. Thicker fluids and then soft foods will be added as your bowel begins to work again.
If a large amount of your small intestine was removed, you may need to receive liquid nutrition through a vein (IV) for a period of time. A special IV will be placed in your neck or upper chest area to deliver nutrition.
After you go home, follow instructions on how to take care of yourself as you heal.
Small bowel resection complications
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Blood clots, bleeding, infection
Small bowel resection surgery complications may include:
- Bulging tissue through the incision, called an incisional hernia
- Damage to nearby organs in the body
- Diarrhea
- Problems with your ileostomy
- Scar tissue that forms in your belly and causes a blockage of your intestines
- Short bowel syndrome (when a large amount of the small intestine needs to be removed), which may lead to problems absorbing important nutrients and vitamins
- Chronic anemia
- The ends of your intestines that are sewn together come apart (anastomotic leak, which may be life threatening)
- Wound breaking open
- Wound infection
Small bowel resection prognosis
Most people who have a small bowel resection recover fully. Even with an ileostomy, most people are able to do the activities they were doing before their surgery. This include most sports, travel, gardening, hiking, and other outdoor activities, and most types of work.
If a large part of your small intestine was removed, you may have problems with loose stools and getting enough nutrients from the food you eat.
If you have a long-term (chronic) condition, such as cancer, Crohn disease or ulcerative colitis, you may need ongoing medical treatment.
- Davis BR, Matthews JB (2006). Diverticular disease of the colon. In M Wolfe et al., eds., Therapy of Digestive Disorders, 2nd ed., pp. 855–859. Philadelphia: Saunders Elsevier.[↩]
- Harford WV (2010). Diverticulosis, diverticulitis, and appendicitis. In EG Nabel, ed., ACP Medicine, section 4, chap. 12. Hamilton, ON: BC Decker.[↩]