Contents
What is Bowen’s disease
Bowen’s disease is a very early form of skin cancer that hasn’t spread beyond the top layer of skin. It is also called squamous cell carcinoma in situ or intraepidermal squamous cell carcinoma. Bowen’s disease (intraepidermal squamous cell carcinoma) is derived from squamous cells, the flat epidermal cells that make keratin—the horny protein that makes up skin, hair and nails. ‘Intraepidermal’ and ‘in situ’ mean the malignant cells are confined to cell of origin, that is, the epidermis. It is not usually serious and there are good treatments available, but don’t ignore it since there’s a small chance it can spread and become a more serious form of skin cancer.
Types of Bowen’s disease
Bowen’s disease develops in the epidermis, the outermost layer of skin. It can develop anywhere on the body, but it’s most common on the trunk, arms or legs. It can also appear on the lips, inside the mouth, or around the genitals or anus.
Bowen’s disease is more common in people who have had a lot of sun exposure, who are infected with the Human Papilloma Virus (HPV), people who have problems with their immune system, or those who have been exposed to arsenic or radiation. People with Bowen’s disease often also have other forms of skin cancer such as basal cell carcinoma.
If you notice a new or changing mole, freckle or spot, you should see your doctor. They will examine you and, if necessary, they will refer you to a dermatologist (a skin specialist).
Bowen’s disease can be diagnosed by investigating how the patch of skin looks and behaves, but you will often need a biopsy to confirm it. This is when a small sample of tissue is removed to be examined in a laboratory.
Figure 1. Skin structure
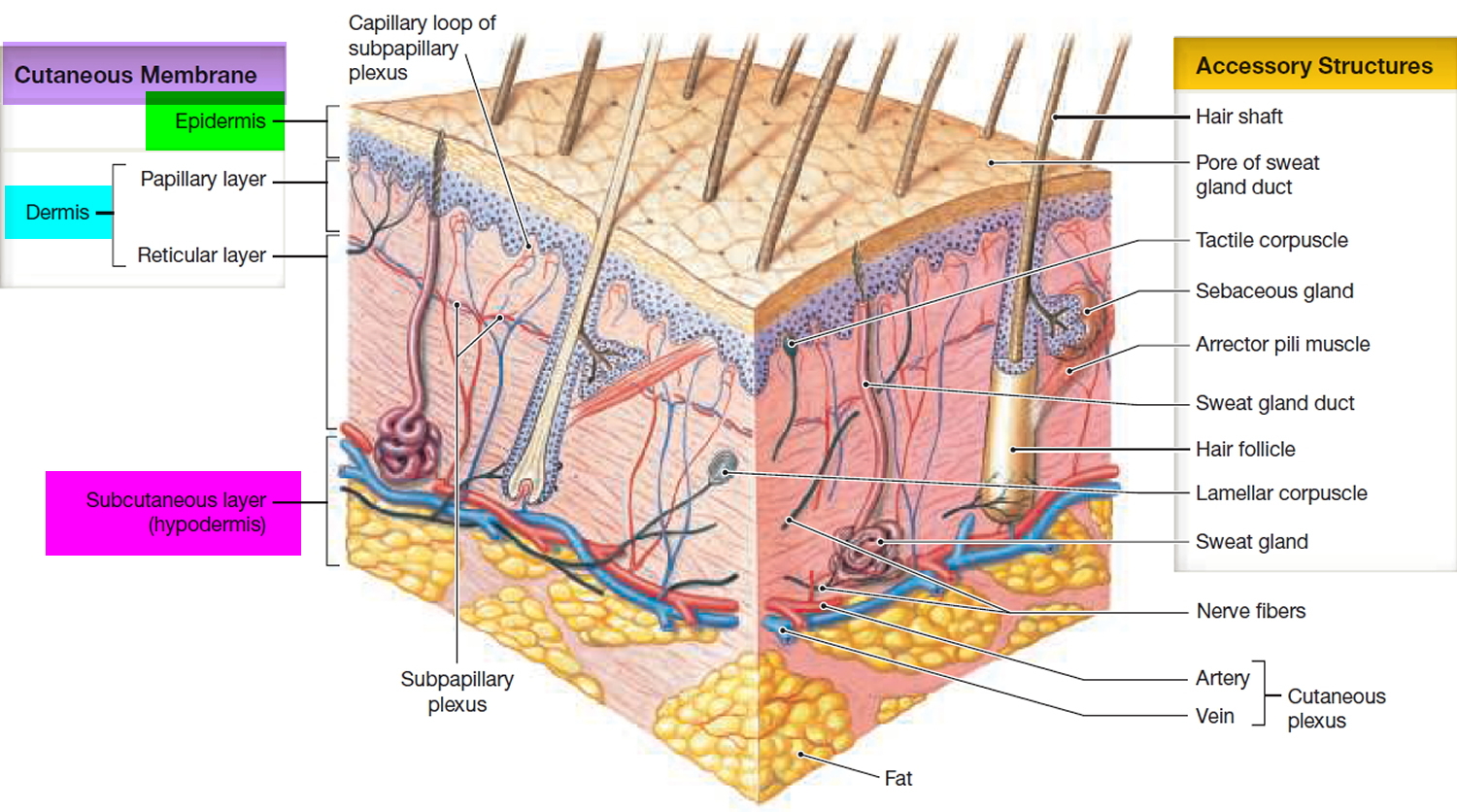
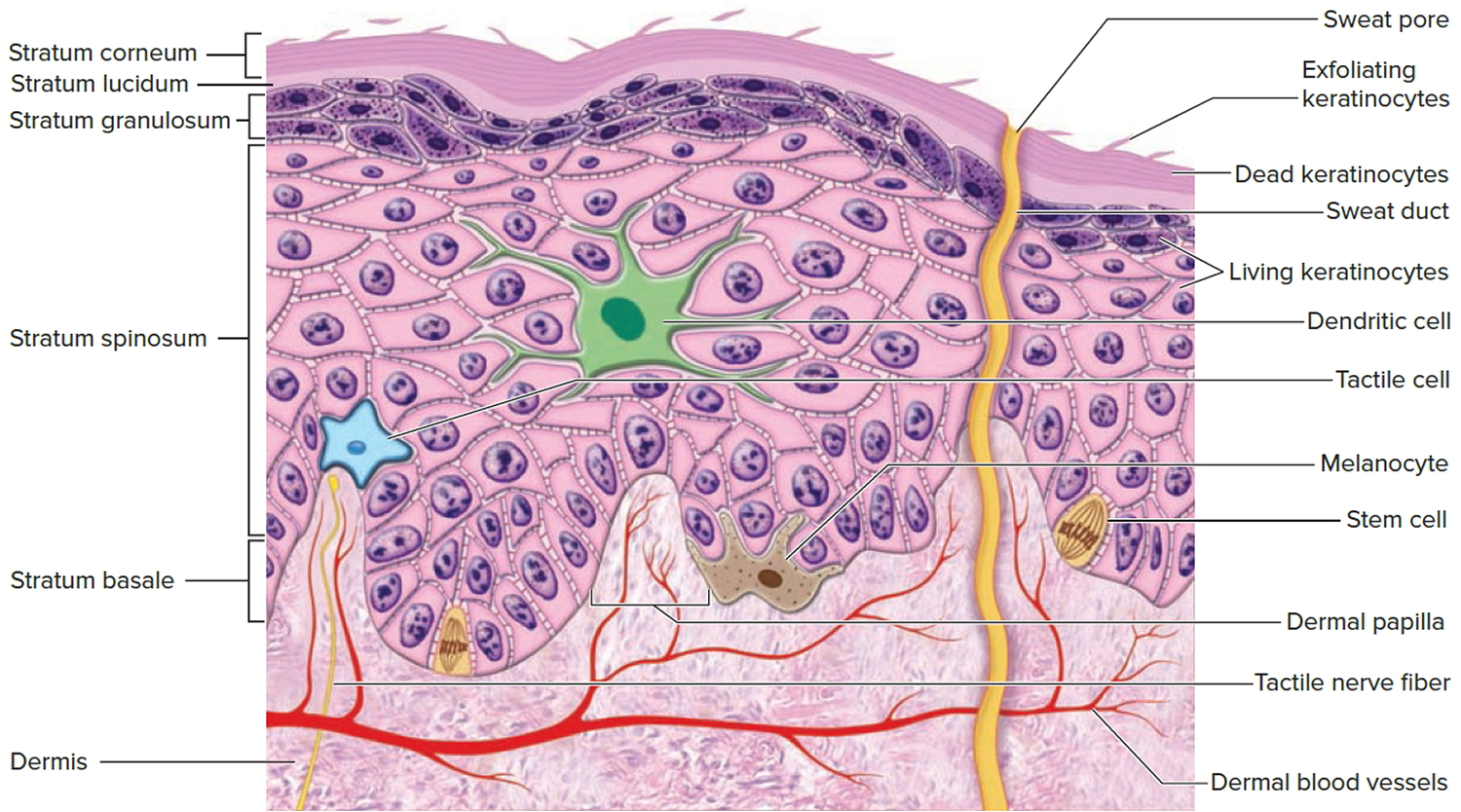
Figure 2. Structure and skin cells of the Epidermis
See your doctor if you have a persistent red, scaly patch of skin and don’t know the cause.
It’s important to get a proper diagnosis, as Bowen’s disease can look like other conditions, such as psoriasis or eczema.
If necessary, your doctor will refer you to a skin specialist (dermatologist) to determine what the problem is.
If they’re not sure about the cause, they may need to remove a small sample of skin so it can be looked at more closely (a biopsy).
Is Bowen’s disease contagious?
No. Bowen’s disease is a very early form of skin cancer called intraepidermal squamous cell carcinoma. This skin cancer tends to develop on skin that has been exposed to the sun for years. It is most frequently seen on sun-exposed areas, such as the head, neck, and back of the hands. People who use tanning beds have a much higher risk of getting squamous cell carcinoma. They also tend to get squamous cell carcinoma earlier in life.
Bowen’s disease doesn’t run in families and you can’t pass it on to others.
Is Bowen’s disease fatal?
Bowen’s disease (intraepidermal squamous cell carcinoma) is not usually serious and there are good treatments available, but don’t ignore it since there’s a small chance it can spread and become a more serious form of skin cancer.
Is Bowen’s disease serious?
Bowen’s disease itself isn’t usually serious. It tends to grow very slowly over months or years, and there are several very effective treatments for it.
The concern is that Bowen’s disease can eventually develop into a different type of skin cancer called squamous cell skin cancer if it’s left undiagnosed or neglected.
It’s estimated this happens in up to 1 in 20 to 1 in 30 people with untreated Bowen’s disease.
Squamous cell skin cancer is often treatable, but it can spread deeper into the body and is sometimes very serious.
Who gets Bowen’s disease?
Bowen’s disease usually affects older people in their 60s and 70s.
Risk factors for Bowen’s disease include:
- Sun exposure: intraepidermal squamous cell carcinoma is most often found in sun damaged individuals.
- Arsenic ingestion: intraepidermal squamous cell carcinoma is common in populations exposed to arsenic.
- Ionizing radiation: intraepidermal squamous cell carcinoma was common on unprotected hands of radiologists early in the 20th century.
- Human papillomavirus (HPV) infection: this is implicated in intraepidermal squamous cell carcinoma on fingers and fingernails.
- Immune suppression due to disease (e.g., chronic lymphocytic leukaemia) or medicines (eg azathioprine, ciclosporin).
Up to 50% of patients with intraepidermal squamous cell carcinoma have other keratinocytic skin cancers, mainly basal cell carcinoma.
What causes Bowen’s disease?
The exact cause of Bowen’s disease is unclear, but it has been closely linked with:
- long-term exposure to the sun or use of sunbeds – especially in people with fair skin
- having a weak immune system – for example, it’s more common in people taking medication to suppress their immune system after an organ transplant, or those with AIDS
- previously having radiotherapy treatment
- the human papillomavirus (HPV) – a common virus that often affects the genital area and can cause genital warts
Ultraviolet radiation (UV) is the main cause of Bowen’s disease. It damages the skin cell nucleic acids (DNA), resulting in a mutant clone of the gene p53. This sets off uncontrolled growth of the skin cells. UV also suppresses the immune response, preventing recovery from damage.
Human papillomavirus (HPV) is another major cause of Bowen’s disease. Oncogenic strains of HPV are the main cause of squamous intraepithelial lesions (SIL), that is, Bowen’s disease in mucosal tissue.
Bowen’s disease prevention
Very careful sun protection at any time of life can reduce the number of intraepidermal squamous cell carcinomas. This is particularly important for ageing, sun-damaged white skin; and in patients that are immune suppressed by disease, for example with human immunodeficiency virus (HIV) infection, or by medications.
- Stay indoors or under the shade in the middle of the day.
- Wear covering clothing.
- Apply high protection SPF50+, broad-spectrum sunscreens generously to exposed skin if outdoors.
- Avoid indoor tanning (sun beds and solaria).
Bowen’s disease prognosis
Bowen’s disease (intraepidermal squamous cell carcinoma) may recur months or years after treatment. The same treatment can be repeated or another method used.
Patients that have been treated for Bowen’s disease (intraepidermal squamous cell carcinoma) are at risk of developing new lesions of intraepidermal squamous cell carcinoma. They are also at increased risk of other skin cancers, especially squamous cell carcinoma, basal cell carcinoma and melanoma.
Bowen’s disease symptoms
Bowen’s disease usually looks like a patch of red, scaly skin that grows slowly over time. Sometimes the patch may be raised and look sore, or it can look like a wart or a dark brown patch in the genital area. The patch is often itchy.
There aren’t usually any other symptoms. Bowen’s disease is often mistaken for psoriasis, eczema or a fungal infection.
Bowen’s disease clinical features
Bowen’s disease usually appears as a patch on the skin with irregular scaly plaques of up to several centimeters in diameter that has clear edges and doesn’t heal. Some people have more than one patch. They are most often red but may also be pigmented.
The patch may be:
- red or pink
- scaly or crusty
- flat or raised
- up to a few centimetres across
- itchy – but isn’t always
Although Bowen’s disease may arise on any area of skin, it is most often diagnosed on sun-exposed sites of the ears, face, hands and lower legs. Sometimes they can affect the groin area and, in men, the penis. When there are multiple plaques, distribution is not symmetrical (unlike psoriasis).
Bowen’s disease may also start to grow under a nail, when it results in a red streak (erythronychia) that later may destroy the nail plate.
If the patch bleeds, starts to turn into an open sore (ulcer) or develops a lump, it could be a sign it has turned into squamous cell skin cancer.
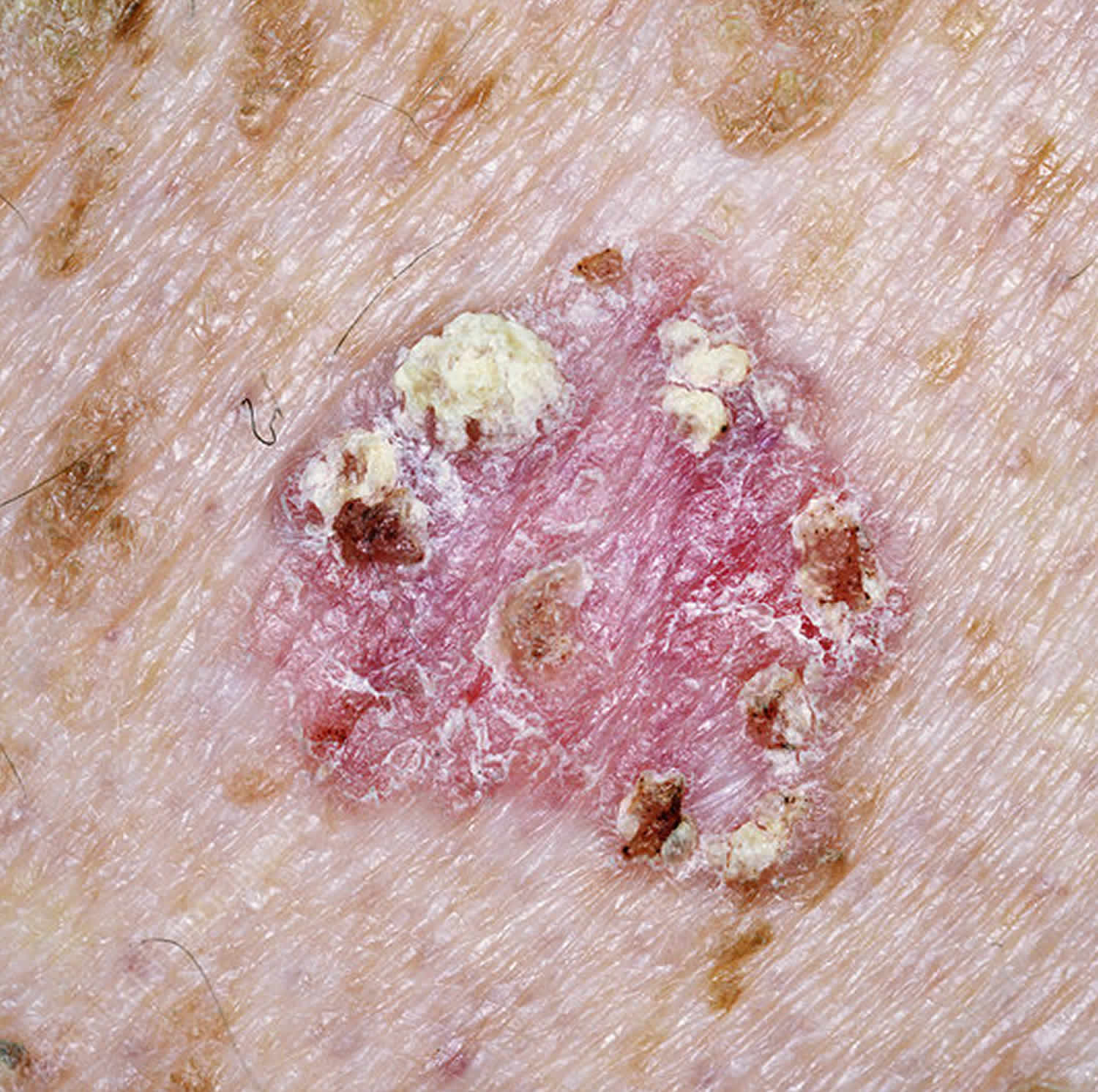
Figure 3. Bowen’s disease
Bowen’s disease treatment
As Bowen’s disease (intraepidermal squamous cell carcinoma) is confined to the surface of the skin, there are various ways to remove it. Because it is such an early cancer, it can very likely be cured. However, recurrence rates are high, whatever method is used, particularly in immune suppressed patients.
The best type of treatment for you will depend on the size and thickness of the Bowen’s disease, where it is on your body, your age and health, and your preference. Treatments include:
- Freezing it off (cryotherapy): Liquid nitrogen is sprayed onto the patch of skin to freeze it. It will scab over and fall off after a few days. The procedure can be a little uncomfortable. Cryotherapy leaves a permanent white mark at the site of treatment.
- Chemotherapy cream: A medicine such as 5-fluorouracil or imiquimod is put on the patch regularly for a few weeks. The skin often gets red and inflamed before it gets better.
- Curettage and cautery: You are given a local anaesthetic before the patch of skin is scraped away and then heat or electricity are used to stop any bleeding. Dressings are applied to the open wound to encourage moist wound healing over the next few weeks.
- Photodynamic therapy (PDT): A cream that reacts to light is spread on the patch of skin and then a laser is shone on the area a few hours later to kill the cancer cells. This may need to be repeated. The treated area develops an inflammatory reaction and then heals over a couple of weeks or so. The best studied, methyl levulinate cream photodynamic therapy used off licence, provides high cure rates for intraepidermal squamous cell carcinoma on the face or lower legs, with excellent cosmetic results. The main disadvantage is the pain experienced by many patients during treatment.
- Surgery: Solitary lesions can be cut out, and the defect repaired by stitching it up. Excision is often recommended if there is suspicion of invasive squamous cell carcinoma. The patch is cut out under local anaesthetic. You may need stitches afterwards.
Sometimes, Bowen’s disease comes back after treatment, so it’s important to go to follow-up appointments with your doctor or dermatologist.
As the risk of invasive squamous cell carcinoma is low, it may not be necessary to remove all lesions particularly in elderly patients. Keratolytic emollients, e.g., containing urea or salicylic acid, may be sufficient to improve symptoms.
Other treatments
Other treatments occasionally used in the treatment of Bowen’s disease include:
- Combination treatments
- Diclofenac gel
- Topical retinoid (tazarotene, tretinoin)
- Chemical peel
- Radiotherapy
- Electron beam therapy
- Carbon dioxide laser ablation
- Erbium:YAG laser ablation
- Oral retinoid (acitretin, isotretinoin).
Looking after your skin after treatment
After your Bowen’s disease treatment, you may need follow-up appointments with your dermatologist or doctor to see if you need any further treatment.
If you had surgery, you may need to have any stitches removed at your doctor surgery a week or two later.
After treatment:
- see your doctor if an existing patch starts to bleed, change in appearance or develops a lump – don’t wait for your follow-up appointment
- see your doctor if you notice any worrying new patches on your skin
- make sure you protect your skin from the sun – wear protective clothing and use a sunscreen with a high sun protection factor (SPF) of at least 30