Contents
- Broken femur
- Types of femoral shaft fractures
- Broken femur cause
- Broken femur symptoms
- Broken femur diagnosis
- Broken femur treatment
- Broken femur recovery time
- Long term effects of broken femur
- Broken femur in children
- Distal Femur Fractures
Broken femur
Femur or thighbone is the longest and strongest bone in your body. Because the femur is so strong, it usually takes a lot of force to break it. Motor vehicle collisions, for example, are the number one cause of femur fractures. Fractures of the distal femur occur most frequently either as high-energy injuries in young men or low-energy fractures in elderly women 1. In elderly patients, distal femur fractures are the second most frequent fragility fractures of the femur following those of the hip 2, and these patients are at elevated risk for complications, given the high prevalence of medical comorbidities 2.
The long, straight part of the femur is called the femoral shaft. When there is a break anywhere along this length of bone, it is called a femoral shaft fracture. This type of broken leg almost always requires surgery to heal.
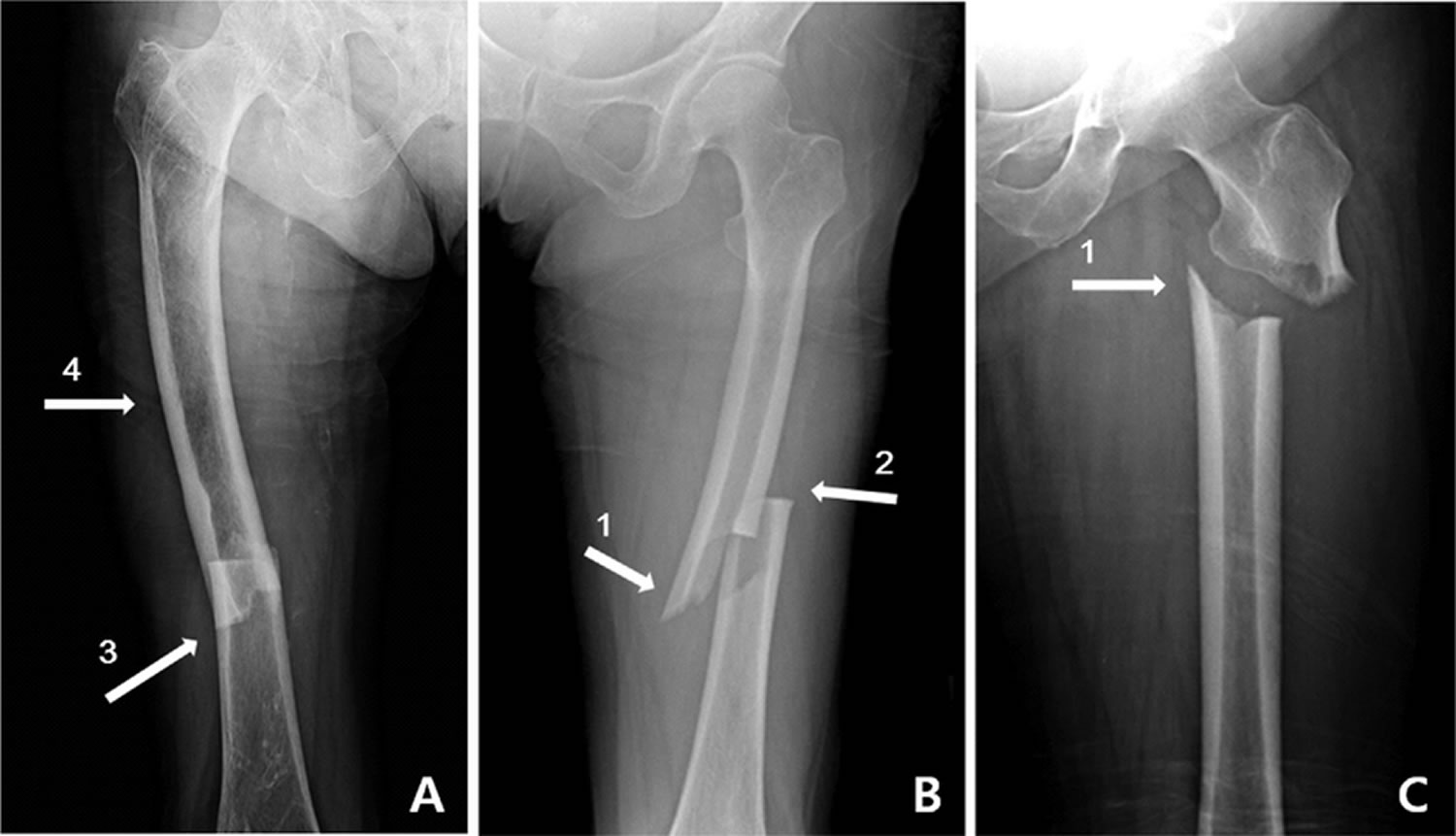
Figure 1. Broken femur
Footnote: Radiographs of the atypical femoral fracture. (A, B) shows atypical femoral fracture in femoral shaft region, and (C) in the subtrochanteric area. The radiographic features of atypical femoral fractures: (1) medial spike; (2) transverse fracture pattern (3) localized periosteal thickening of the lateral cortex; (4) generalized thickening of the femoral cortices.
Types of femoral shaft fractures
Broken femur vary greatly, depending on the force that causes the break. The pieces of bone may line up correctly (stable fracture) or be out of alignment (displaced fracture). The skin around the fracture may be intact (closed fracture) or the bone may puncture the skin (open fracture).
Doctors describe fractures to each other using classification systems. Femur fractures are classified depending on:
- The location of the fracture (the femoral shaft is divided into thirds: distal, middle, proximal)
- The pattern of the fracture (for example, the bone can break in different directions, such as crosswise, lengthwise, or in the middle)
- Whether the skin and muscle over the bone is torn by the injury
The most common types of femoral shaft fractures include:
- Transverse fracture. In this type of fracture, the break is a straight horizontal line going across the femoral shaft.
- Oblique fracture. This type of fracture has an angled line across the shaft.
- Spiral fracture. The fracture line encircles the shaft like the stripes on a candy cane. A twisting force to the thigh causes this type of fracture.
- Comminuted fracture. In this type of fracture, the bone has broken into three or more pieces. In most cases, the number of bone fragments corresponds with the amount of force needed to break the bone.
- Open fracture. If a bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the broken bone, the fracture is called an open or compound fracture. Open fractures often involve much more damage to the surrounding muscles, tendons, and ligaments. They have a higher risk for complications—especially infections—and take a longer time to heal.
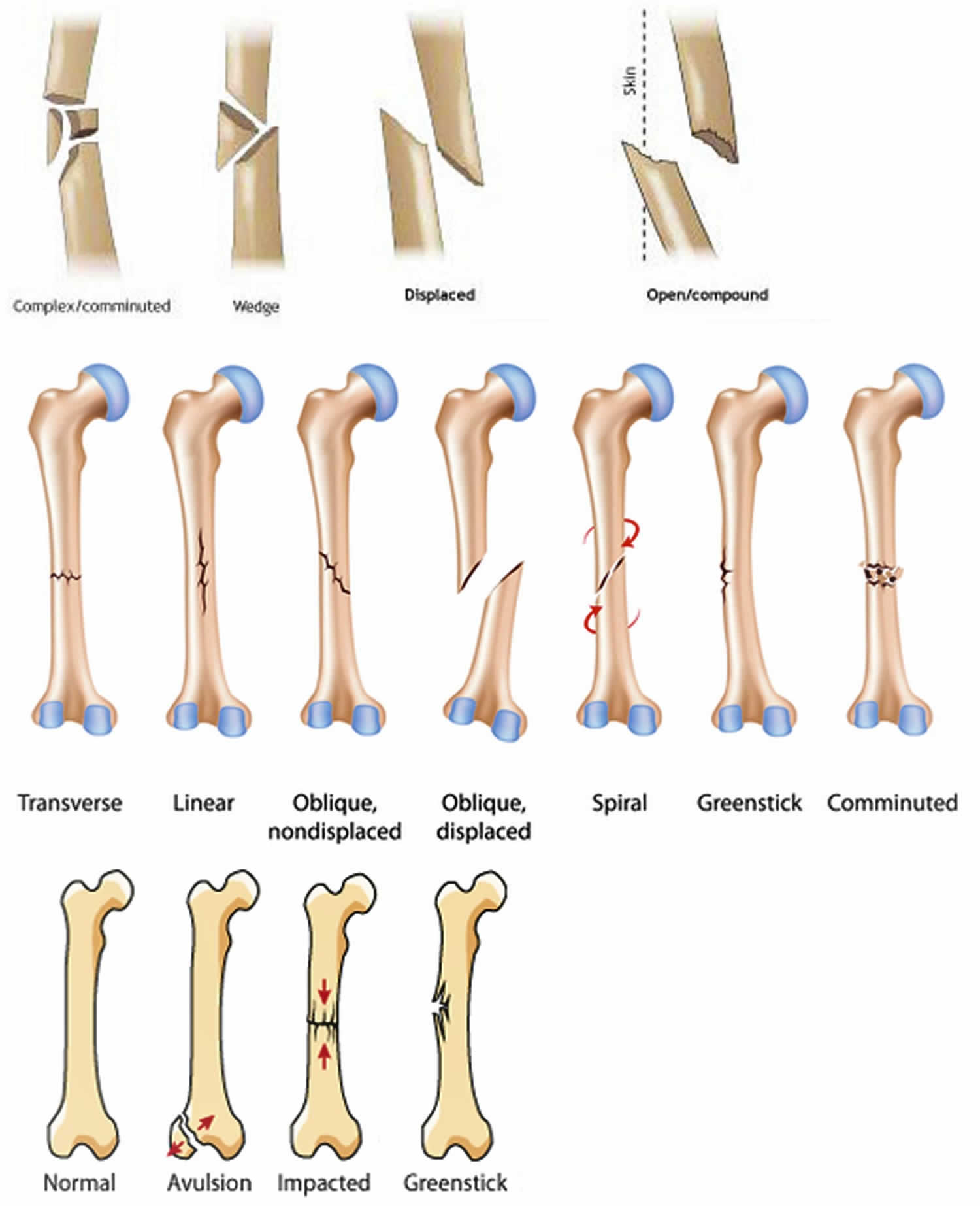
Figure 2. Broken femur types
Broken femur cause
Femoral shaft fractures in young people are frequently due to some type of high-energy collision. The most common cause of femoral shaft fracture is a motor vehicle or motorcycle crash. Being hit by a car while walking is another common cause, as are falls from heights and gunshot wounds.
A lower-force incident, such as a fall from standing, may cause a femoral shaft fracture in an older person who has weaker bones.
Broken femur symptoms
A femoral shaft fracture usually causes immediate, severe pain. You will not be able to put weight on the injured leg, and it may look deformed—shorter than the other leg and no longer straight.
Broken femur diagnosis
Medical history and physical examination
It is important that your doctor know the specifics of how you hurt your leg. For example, if you were in a car accident, it would help your doctor to know how fast you were going, whether you were the driver or a passenger, whether you were wearing your seat belt, and if the airbags went off. This information will help your doctor determine how you were hurt and whether you may be hurt somewhere else.
It is also important for your doctor to know if you have any other health conditions, such as high blood pressure, diabetes, asthma, or allergies. Your doctor will also ask you if you use tobacco products or are taking any medications.
After discussing your injury and medical history, your doctor will do a careful examination. Your doctor will assess your overall condition, and then focus on your leg. Your doctor will look for:
- An obvious deformity of the thigh/leg (an unusual angle, twisting, or shortening of the leg)
- Breaks in the skin
- Bruises
- Bony pieces that may be pushing on the skin
After the visual inspection, your doctor will feel along your thigh, leg, and foot looking for abnormalities and checking the tightness of the skin and muscles around your thigh. He or she will also feel for pulses. If you are awake, your doctor will test for sensation and movement in your leg and foot.
Imaging Tests
Imaging tests will provide your doctor with more information about your injury.
X-rays. The most common way to evaluate a fracture is with x-rays, which provide clear images of bone. X-rays can show whether a bone is intact or broken. They can also show the type of fracture and where it is located within the femur.
Computerized tomography (CT) scans. If your doctor still needs more information after reviewing your x-rays, he or she may order a CT scan. A CT scan shows a cross-sectional image of your limb. It can provide your doctor with valuable information about the severity of the fracture. For example, sometimes the fracture lines can be very thin and hard to see on an x-ray. A CT scan can help your doctor see the lines more clearly.
Broken femur treatment
Nonsurgical treatment
Most femoral shaft fractures require surgery to heal. It is unusual for femoral shaft fractures to be treated without surgery. Very young children are sometimes treated with a cast. For more information on that, see broken femur in children.
Broken femur surgery
Timing of surgery. Most femur fractures are fixed within 24 to 48 hours. On occasion, fixation will be delayed until other life-threatening injuries or unstable medical conditions are stabilized. To reduce the risk of infection, open fractures are treated with antibiotics as soon as you arrive at the hospital. The open wound, tissues, and bone will be cleaned during surgery.
For the time between initial emergency care and your surgery, your doctor may place your leg either in a long-leg splint or in traction. This is to keep your broken bones as aligned as possible and to maintain the length of your leg.
Skeletal traction is a pulley system of weights and counterweights that holds the broken pieces of bone together. It keeps your leg straight and often helps to relieve pain.
External fixation. In this type of operation, metal pins or screws are placed into the bone above and below the fracture site. The pins and screws are attached to a bar outside the skin. This device is a stabilizing frame that holds the bones in the proper position.
External fixation is usually a temporary treatment for femur fractures. Because they are easily applied, external fixators are often put on when a patient has multiple injuries and is not yet ready for a longer surgery to fix the fracture. An external fixator provides good, temporary stability until the patient is healthy enough for the final surgery. In some cases, an external fixator is left on until the femur is fully healed, but this is not common.
Figure 3. Broken femur external fixation
Intramedullary nailing. Currently, the method most surgeons use for treating femoral shaft fractures is intramedullary nailing. During this procedure, a specially designed metal rod is inserted into the canal of the femur. The rod passes across the fracture to keep it in position.
An intramedullary nail can be inserted into the canal either at the hip or the knee. Screws are placed above and below the fracture to hold the leg in correct alignment while the bone heals.
Intramedullary nails are usually made of titanium. They come in various lengths and diameters to fit most femur bones.
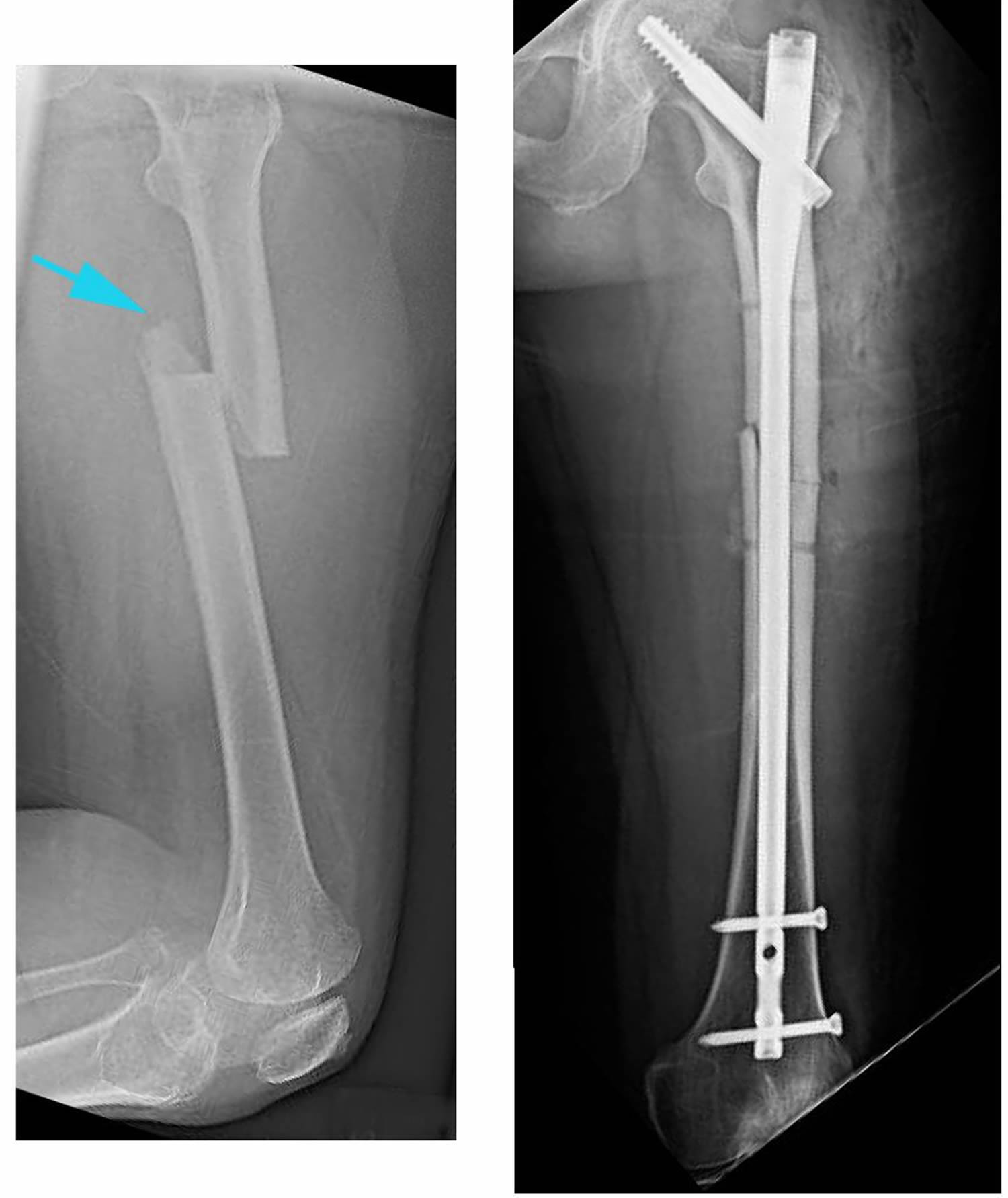
Figure 4. Broken femur intramedullary nailing
Footnote: (Left) This x-ray, taken from the side, shows a transverse fracture of the femur. (Right) In this front view x-ray, the fracture has been treated with intramedullary nailing.
Plates and screws. During this operation, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with screws and metal plates attached to the outer surface of the bone.
Plates and screws are often used when intramedullary nailing may not be possible, such as for fractures that extend into either the hip or knee joints.
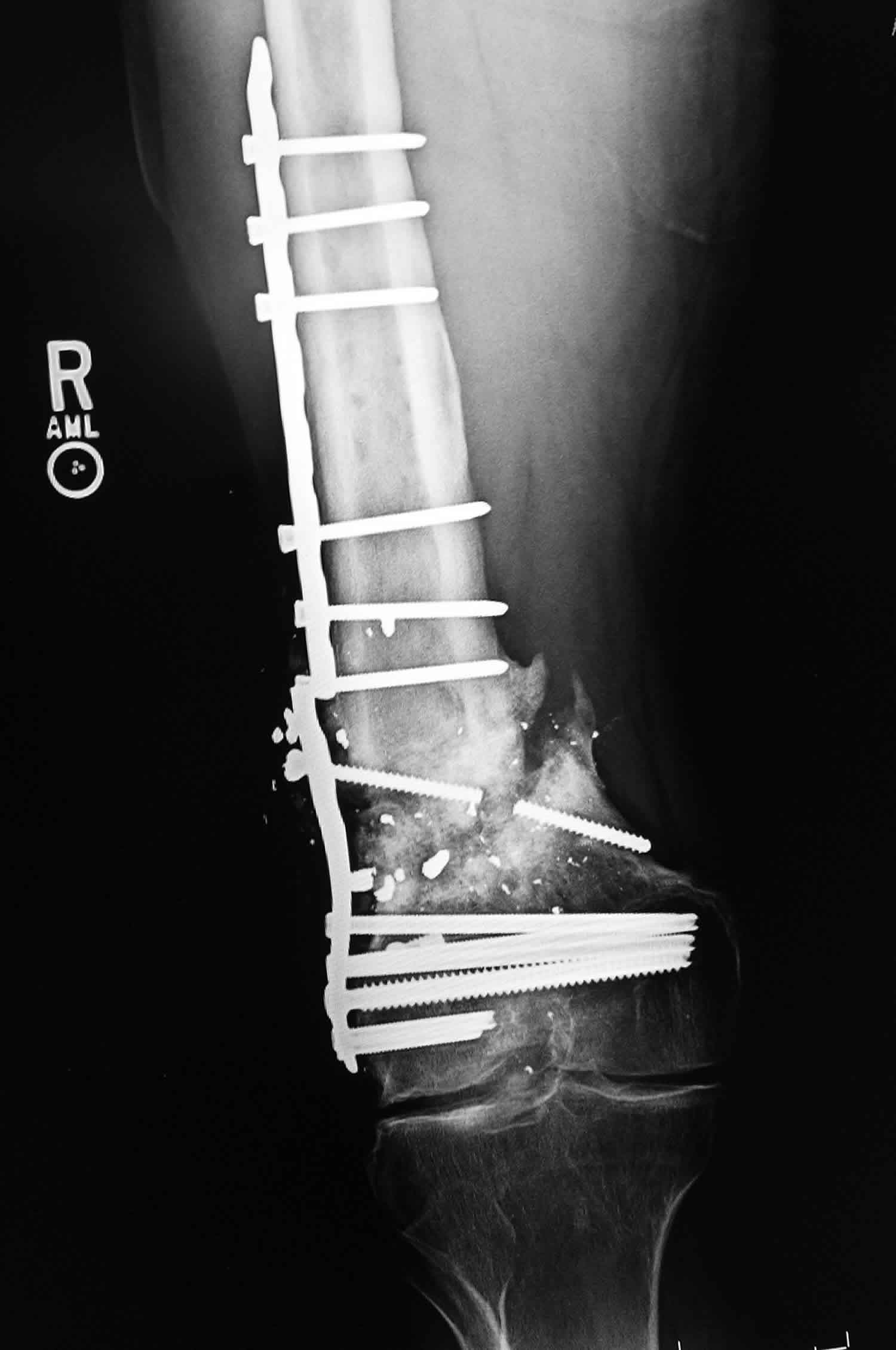
Figure 5. Broken femur plates and screws
Pain Management
Pain after an injury or surgery is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover faster.
Medications are often prescribed for short-term pain relief after surgery or an injury. Many types of medications are available to help manage pain. These include acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), gabapentinoids, muscle relaxants, opioids, and topical pain medications. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids. Some pain medications may have side effects that can impact your ability to drive and do other activities. Your doctor will talk to you about the side effects of your pain medications.
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your treatment.
Broken femur recovery time
Most femoral shaft fractures take 3 to 6 months to completely heal. Some take even longer, especially if the fracture was open or broken into several pieces or if the patient uses tobacco products.
Weightbearing
Many doctors encourage leg motion early on in the recovery period. It is very important to follow your doctor’s instructions for putting weight on your injured leg to avoid problems.
In some cases, doctors will allow patients to put as much weight as possible on the leg right after surgery. However, you may not be able to put full weight on your leg until the fracture has started to heal. Be sure to follow your doctor’s instructions carefully.
When you begin walking, you will probably need to use crutches or a walker for support.
Physical therapy
Because you will most likely lose muscle strength in the injured area, exercises during the healing process are important. Physical therapy will help to restore normal muscle strength, joint motion, and flexibility. It can also help you manage your pain after surgery.
A physical therapist will most likely begin teaching you specific exercises while you are still in the hospital. The therapist will also help you learn how to use crutches or a walker.
Long term effects of broken femur
Femoral shaft fractures can cause further injury and complications.
- The ends of broken bones are often sharp and can cut or tear surrounding blood vessels or nerves, though this is very rare.
- Acute compartment syndrome may develop. This is a painful condition that occurs when pressure within the muscles builds to dangerous levels. This pressure can decrease blood flow, which prevents nourishment and oxygen from reaching nerve and muscle cells. Unless the pressure is relieved quickly, permanent disability may result. This is a surgical emergency. During the procedure, your surgeon makes incisions in your skin and the muscle coverings to relieve the pressure.
- Open fractures expose the bone to the outside environment. Even with good surgical cleaning of the bone and muscle, the bone can become infected. Bone infection is difficult to treat and often requires multiple surgeries and long-term antibiotics.
- Occasionally, the ligaments around the knee can be injured during a femoral shaft fracture. If you have knee pain after surgery, tell your doctor.
Complications from surgery
In addition to the risks of surgery in general, such as blood loss or problems related to anesthesia, complications of surgery may include:
- Infection
- Injury to nerves and blood vessels
- Blood clots
- Fat embolism (bone marrow enters the blood stream and can travel to the lungs; this can also happen from the fracture itself without surgery)
- Malalignment or the inability to correctly position the broken bone fragments
- Delayed union or nonunion (when the fracture heals slower than usual or not at all)
- Hardware irritation (sometimes the end of the nail or the screw can irritate the overlying muscles and tendons).
Broken femur in children
The most common cause of thighbone fractures in infants under 1 year old is child abuse. Child abuse is also a leading cause of thighbone fracture in children between the ages of 1 and 4 years, but the incidence is much less in this age group.
In adolescents, motor vehicle accidents (either in cars, bicycles, or as a pedestrian) are responsible for the vast majority of femoral shaft fractures.
Risk factors for broken femur in children
Events with the highest risk for pediatric femur fractures include:
- Falling hard on the playground
- Taking a hit in contact sports
- Being in a motor vehicle accident
- Child abuse
Types of Femur Fractures (Classification)
Femur fractures vary greatly. The pieces of bone may be aligned correctly (straight) or out of alignment (displaced), and the fracture may be closed (skin intact) or open (bone piercing through the skin). An open fracture is rare.
Specifically, thighbone fractures are classified depending on:
- Location of fracture on the bone (proximal, middle, or distal third of the bone shaft)
- Shape of the fractured ends — bones can break all kinds of ways, such as straight across (transverse), angled (oblique), or spiraled (spiral)
- Position of the fractured edges (angulated or displaced)
- Number of fractured parts
- Two parts
- Several fractured parts (comminuted)
Broken femur in children symptoms
A thighbone fracture is a serious injury. It may be obvious that the thighbone is fractured because:
- Your child has severe pain
- The thigh is noticeably swollen or deformed
- Your child is unable to stand or walk, and/or
- There is a limited range of motion of the hip or knee allowed by the child because of pain.
Take your child to the emergency room right away if you think he or she has a broken thighbone.
Broken femur in children diagnosis
Doctor Examination
It is important that the doctor know exactly how the injury occurred. Tell the doctor if your child had any disease or other trauma before it happened.
The doctor will give your child pain relief medication and carefully examine the leg, including the hip and knee. A child with a thighbone fracture should always be evaluated for other serious injuries.
Imaging Tests
Your orthopaedic doctor will need x-rays to see what the broken bone looks like (refer to “Classification”). Your child’s healthy leg may also be x-rayed for comparison.
The orthopaedic doctor will also check the x-ray for any damage to the growth area (growth plate) near the end of the femur. This is the part that enables the child’s bone to grow. If needed, surgery may help to restore the growth plate’s function, and regular x-rays may be taken for many months to track the bone’s growth.
Broken femur in children treatment
To treat a child’s broken femur, the pieces of bone are realigned and held in place for healing. Treatment depends on many factors, such as your child’s age and weight, the type of fracture, how the injury happened, and whether the broken bone pierced the skin.
Nonsurgical treatment
In some thighbone fractures, the doctor may be able to manipulate the broken bones back into place without an operation (closed reduction). In a baby under 6 months old, a brace (called a Pavlik Harness) may be able to hold the broken bone still enough for successful healing.
Spica casting. In children between 7 months and 5 years old, a spica cast is often applied to keep the fractured pieces in correct position until the bone is healed.
There are different types of spica casts, but, in general, a spica cast begins at the chest and extends all the way down the fractured leg. The cast may also extend down the uninjured leg, or stop at the knee or hip. Your doctor will decide which type of spica cast is most effective for treating your child’s fracture.
Your doctor will sedate your child for the closed reduction, and apply a spica cast immediately (or within 24 hours of hospitalization) to keep the fractured pieces in correct position until healing occurs.
When a bone breaks and is displaced, the pieces often overlap and shorten the normal length of the bone. Because children’s bones grow quickly, your doctor may not need to manipulate the pieces back into perfect alignment. While in the cast, the bones will grow and heal back into a more normal shape.
In general, for the best results, the broken pieces should not overlap more than 2 cm when in the cast. The growth of the thighbone may be temporarily increased by the trauma. The mild shortening from the overlap will resolve.
Traction. If the shortening of the bones is too much (more than 3 cm) or if the bone is too crooked in the cast, it may be helpful to put the leg in a weight and counterweight system (traction) to make sure the bones are properly realigned.
Figure 6. Hip spica cast
Surgical treatment
Doctors generally agree that displaced femur fractures that have shortened more than 3 cm are not acceptable and require treatment to correct at least a portion of the shortening.
In some more complicated injuries, the doctor may need to surgically realign the bone and use an implant to stabilize the fracture.
Doctors are treating pediatric thighbone fractures more often with surgery than in previous years due to the benefits that have been recognized. These include earlier mobilization, faster rehabilitation, and shorter time spent in the hospital.
In children between 6 and 10 years old, flexible intramedullary (inside the bone) nails are often used to stabilize the fracture. Over the past decade, this treatment method has gained great acceptance.
Occasionally, the broken bone has too many pieces and cannot be treated successfully with flexible nails. Other options that can lead to successful outcomes in this situation include:
- A plate with screws that “bridges” the fractured segments
- An external fixator — this is often used if there has been a large open injury to the skin and muscles
- Prolonged traction with a pin temporarily placed into the thighbone
As the child nears the teenage years (11 years to skeletal maturity), the most common treatment choices include either flexible intramedullary nails or a rigid locked intramedullary nail. The rigid nail is particularly useful when the fracture is unstable. Both types of nails allow for the child to begin walking immediately.
Broken femur in children prognosis
Generally, children who sustain a thighbone fracture will heal well, regain normal function, and have legs that are equal in length. The intramedullary nails may need to be removed following healing if they cause irritation of the skin and tissues underneath.
Occasionally, children will require further treatment, either early on or in subsequent years, if they have a significant difference in the length of the legs, unacceptable angulation of the healed bone, abnormal rotation of the healed bone, infection, or (rarely) if a thighbone fracture persists (nonunion).
These problems can nearly always be resolved with further treatment.
Distal Femur Fractures
Broken femur that occur just above the knee joint are called distal femur fractures. The distal femur is where the bone flares out like an upside-down funnel.
Distal femur fractures most often occur either in older people whose bones are weak, or in younger people who have high energy injuries, such as from a car crash. In both the elderly and the young, the breaks may extend into the knee joint and may shatter the bone into many pieces.
Distal femur fractures vary. The bone can break straight across (transverse fracture) or into many pieces (comminuted fracture). Sometimes these fractures extend into the knee joint and separate the surface of the bone into a few (or many) parts. These types of fractures are called intra-articular. Because they damage the cartilage surface of the bone, intra-articular fractures can be more difficult to treat.
Distal femur fractures can be closed — meaning the skin is intact — or can be open. An open fracture is when a bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the broken bone. Open fractures often involve much more damage to the surrounding muscles, tendons, and ligaments. They have a higher risk for complications and take a longer time to heal.
When the distal femur breaks, both the hamstrings and quadriceps muscles tend to contract and shorten. When this happens the bone fragments change position and become difficult to line up with a cast.
Figure 7. Distal femur fracture
Footnote: 1, 2, 3, 4 the preoperative X-ray and CT three-dimensional reconstruction of femur.
Knee anatomy
The knee is the largest weightbearing joint in your body. The distal femur makes up the top part of your knee joint. The upper part of the shinbone (tibia) supports the bottom part of your knee joint.
The ends of the femur are covered in a smooth, slippery substance called articular cartilage. This cartilage protects and cushions the bone when you bend and straighten your knee.
Strong muscles in the front of your thigh (quadriceps) and back of your thigh (hamstrings) support your knee joint and allow you to bend and straighten your knee.
Distal femur fracture cause
Fractures of the distal femur most commonly occur in two patient types: younger people (under age 50) and the elderly.
- Distal femur fractures in younger patients are usually caused by high energy injuries, such as falls from significant heights or motor vehicle collisions. Because of the forceful nature of these fractures, many patients also have other injuries, often of the head, chest, abdomen, pelvis, spine, and other limbs.
- Elderly people with distal femur fractures typically have poor bone quality. As we age, our bones get thinner. Bones can become very weak and fragile. A lower-force event, such as a fall from standing, can cause a distal femur fracture in an older person who has weak bones. Although these patients do not often have other injuries, they may have concerning medical problems, such as conditions of the heart, lungs, and kidneys, and diabetes.
Distal femur fracture symptoms
The most common symptoms of distal femur fracture include:
- Pain with weightbearing
- Swelling and bruising
- Tenderness to touch
- Deformity — the knee may look “out of place” and the leg may appear shorter and crooked
In most cases, these symptoms occur around the knee, but you may also have symptoms in the thigh area.
Distal femur fracture complications
Infection
Newer techniques in treating these difficult fractures have cut the infection rate by more than a half: Currently less than 5% of patients have infections. If you have surgery, your doctor will give you antibiotics to help prevent infection.
Open fractures (those with tears in the skin) and high energy fractures (such as car accidents) are at higher risk for infection. If the infection is deep, it may involve the bone and the device used to fix the bone. A bone infection can require long-term, intravenous antibiotic treatment, as well as several surgeries to clean out the infection.
Stiffness
Some knee stiffness is expected after a distal femur fracture. Moving your knee soon after surgery is the best way to prevent stiffness. If you have lost significant knee motion and your fracture is healing, your doctor may suggest an additional operation to break up scar tissue around the kneecap.
Bone healing problems
In some cases, bone healing can be slow or not happen at all. If a follow-up x-ray shows rods, plates, and screws breaking or pulling out of the bone, it may be a sign that the bone is not healing. This can happen even if your fracture has been fixed well and you have followed your doctor’s guidelines.
Open fractures and high energy fractures are most at risk for not healing. These challenging fractures are also most at risk for infection, and infection can cause bone healing problems.
To help the fracture heal, your doctor may suggest applying a bone graft to the fracture, and changing or adding to how it was fixed (plates, screws, rods).
Knee arthritis
Distal femur fractures that enter the the knee joint may heal with a defect in the normally smooth surface of the joint. Because the knee is the largest weightbearing joint in the body, any defect can damage the protective articular cartilage and, over time, result in arthritis. In some cases, the joint surface may wear down to bare bone.
Arthritis caused by fracture or injury is called post-traumatic arthritis. It can be treated like other forms of osteoarthritis — with physical therapy, braces, medications, and lifestyle changes.
In cases of severe arthritis that limits activity, a total knee replacement may be the best option to relieve symptoms.
Distal femur fracture diagnosis
Medical History and Physical Examination
It is important that your doctor knows the circumstances of your injury. For example, if you fell from a tree, how far did you fall? It is just as important for your doctor to know if you sustained any other injuries and if you have any other medical problems, such as diabetes. Your doctor also needs to know if you take any medications.
After discussing your symptoms and medical history, your doctor will do a careful examination.
- Your doctor will assess your overall condition to make sure no other body parts have been injured (head, belly, chest, pelvis, spine, and other extremities)
- Your doctor will examine your skin around the fracture to make sure it is not an open fracture
- Your doctor will also check the blood and nerve supply to your leg
Tests
Other tests that will provide your doctor with more information about your injury include:
- X-rays. The most common way to evaluate a fracture is with x-rays, which provide clear images of bone. X-rays can show whether a bone is intact or broken. They can also show the type of fracture and where it is located within the femur. To make sure no other breaks are missed, your hip and ankle joints will also be x-rayed.
- Computed tomography (CT) scan. A CT scan shows a cross-sectional image of your limb. It can provide your doctor with valuable information about the severity of the fracture. This scan can show whether the fracture enters the joint surface and, if so, how many pieces of bone there are. A CT scan will help your doctor decide how to fix the break.
- Other tests. Your doctor may order other tests that do not involve the broken leg to make sure no other body parts are injured (head, chest, belly, pelvis, spine, arms, and other leg). Sometimes, other studies are done to check the blood supply to your leg.
Distal femur fracture treatment
Nonsurgical Treatment
Nonsurgical treatment options for distal femur fractures include:
- Skeletal traction. Skeletal traction is a pulley system of weights and counterweights that holds the broken pieces of bone together. A pin is placed in a bone to position the leg.
- Casting and bracing. Casts and braces hold the bones in place while they heal. In many cases of distal femur fracture, however, a cast or brace cannot correctly line up the bone pieces because shortened muscles pull the pieces out of place. Only fractures that are limited to two parts and are stable and well aligned can be treated with a brace. Casts and braces can also be uncomfortable.
Patients with distal femoral fractures of all ages do best when they can be up and moving soon after treatment (such as moving from a bed to a chair, and walking). Treatment that allows early motion of the knee lessens the risk of knee stiffness, and prevents problems caused by extended bed rest, such as bed sores and blood clots.
Because traction, casting, and bracing do not allow for early knee movement, they are used less often than surgical treatments. Your doctor will talk with you about the best treatment option for you and your injury.
Surgical treatment
Because of newer techniques and special materials, the results of surgical treatment are good, even in older patients who have poor bone quality.
Timing of surgery
Most distal femur fractures are not operated on right away — unless the skin around the fracture has been broken (open fracture). Open fractures expose the fracture site to the environment. They urgently need to be cleansed and require immediate surgery.
In most cases, surgery is delayed 1 to 3 days to develop a treatment plan and to prepare the patient for surgery. Depending on your age and medical history, your surgeon may recommend that you are evaluated by your primary doctor to make sure that you have no medical problems that need to be addressed before surgery.
External fixation
If the soft tissues (skin and muscle) around your fracture are badly damaged, or if it will take time before you can tolerate a longer surgery because of health reasons, your doctor may apply a temporary external fixator. In this type of operation, metal pins or screws are placed into the middle of the femur and tibia (shinbone). The pins and screws are attached to a bar outside the skin. This device is a stabilizing frame that holds the bones in the proper position until you are ready for surgery.
When you are ready, your surgeon will remove the external fixator and place internal fixation devices on or in the bone under the skin and muscles.
Internal fixation
The internal fixation methods most surgeons use for distal femur fractures include:
- Intramedullary nailing. During this procedure, a specially designed metal rod is inserted into the marrow canal of the femur. The rod passes across the fracture to keep it in position.
- Plates and screws. During this operation, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with special screws and metal plates attached to the outer surface of the bone.
Both of these methods can be done through one large incision or several smaller ones, depending on the type of fracture you have and the device your surgeon uses.
If the fracture is in many small pieces above your knee joint, your surgeon will not try to piece the bone back together like a puzzle. Instead, your surgeon will fix a plate or rod at both ends of the fracture without touching the many small pieces. This will keep the overall shape and length of the bone correct while it heals. The individual pieces will then fill in with new bone, called a callous.
In cases where a fracture may be slow to heal, such as when a patient is elderly with poor bone quality, a bone graft may be used to help the callous develop. Bone grafts may be obtained from the patient (most often taken from the pelvis) or from a tissue bank (cadaver bone). Other options include the use of artificial bone fillers.
In extreme cases, a fracture may be too complicated and the bone quality too poor to fix. These types of fractures are often treated by removing the fragments and replacing the bone with a knee replacement implant.
Fractures and knee replacements
As the population ages and the number of knee replacements rises, an increasing problem has emerged: More distal femur fractures are being seen in seniors who have knee replacements.
Those fractures are typically treated with rods or plates, just like other distal femur fractures. In rare cases, the artificial implant must be removed and replaced with a larger implant. This procedure is called a revision and may be necessary if the implant is loose or not supported by surrounding good bone.
Surgical complications
To prevent infection, you will be given intravenous antibiotics before your procedure. Because blood clots in your leg veins may develop after surgery, your doctor may also give you blood thinners.
There will be blood loss during your surgery. How much blood is lost will depend upon the severity of your fracture and the procedure used to treat it. Your doctor will assess your blood level during the operation and, if low, will determine whether it is in your best interest to have a blood transfusion.
Pain management
Pain after an injury or surgery is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover faster.
Medications are often prescribed for short-term pain relief after surgery or an injury. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your treatment.
Distal femur fracture recovery time
A distal femur fracture is a severe injury. Depending on several factors — such as your age, general health, and the type of fracture you have — it may take a year or more of rehabilitation before you are able to return to all everyday activities.
It typically takes a year or more for a distal femur fracture to completely heal. Factors that may significantly affect healing and your long-term satisfaction include:
- How severe your injury is. Higher energy fractures may be in more pieces and slower to heal, especially if they are open with more damage to soft tissues.
- Your bone quality. Better quality bone (younger patients) may keep the plates, screws, and rods better in place. Older patients and those with osteoporosis are at high risk for the implants loosening and pulling out of the bone. Newer techniques and implants may help prevent this risk, but cannot eliminate it entirely.
- Your commitment to your recovery. Although recovery is a slow process, your commitment to physical therapy and following your doctor’s guidelines are an essential part to returning to the activities you enjoy.
Your doctor will regularly check how your recovery is progressing. He or she will assess your pain level (if any), strength, and knee motion, and also how well you are able to perform daily activities.
Your satisfaction with doing normal everyday activities, as well as work and sports activities, is the final assessment of your recovery.
Early motion
Your doctor will decide when it is best to begin moving your knee in order to prevent stiffness. This depends on how well the soft tissues (skin and muscle) are recovering and how secure the fracture is after having been fixed.
Early motion sometimes starts with passive exercise: a physical therapist will gently move your knee for you, or your knee may be placed in a continuous passive motion machine that cradles and moves your leg.
If your bone was fractured in many pieces or your bone is weak, it may take longer to heal, and it may be a longer time before your doctor recommends motion activities.
Weightbearing
To avoid problems, it is very important to follow your doctor’s instructions for putting weight on your injured leg.
Whether your fracture is treated with surgery or not, your doctor will most likely discourage weightbearing until some healing has occurred. This may require as much as 3 months or more of healing before weightbearing can be done safely. During this time, you will need crutches or a walker to move around. You may also wear a knee brace for additional support.
Your doctor will regularly schedule x-rays to monitor how well your fracture is healing. If treated with a brace or cast, these regular x-rays show your doctor whether the fracture is lined up. Once your doctor determines that your fracture is stable enough, you can begin weightbearing activities. Even though you can put weight on your leg, you may still need crutches or a walker at times.
Rehabilitation
When you are allowed to put weight on your leg, it is very normal to feel weak, unsteady, and stiff. Even though this is expected, be sure to share your concerns with your doctor and physical therapist. A rehabilitation plan will be designed to help restore normal muscle strength, joint motion, and flexibility.
Your physical therapist is like a coach guiding you through your rehabilitation. Your commitment to physical therapy and making healthy choices can make a big difference in how well you recover. For example, if you are a smoker, your doctor or therapist may recommend that you quit. Some doctors believe that smoking may prevent bone from healing. Your doctor or therapist may be able to recommend professional services to help you quit smoking.
To help you gauge how well your rehabilitation is going, as you recover ask yourself:
- Is my ability to walk and care for myself improving?
- Are my normal activities of daily living improving?
- Is my pain gone or less, and are my knee motion, stability and strength improving?
The goals of rehabilitation are to get you and your knee back to as normal function as possible. This may take up to a year or more.
- Martinet O, Cordey J, Harder Y, Maier A, Buhler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury. 2000;31(suppl 3):C62–C63. doi: 10.1016/S0020-1383(00)80034-0[↩]
- Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, Cosman F. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int. 2010;21:399–408. doi: 10.1007/s00198-009-0962-6.[↩][↩]