Contents
What is bronchiectasis
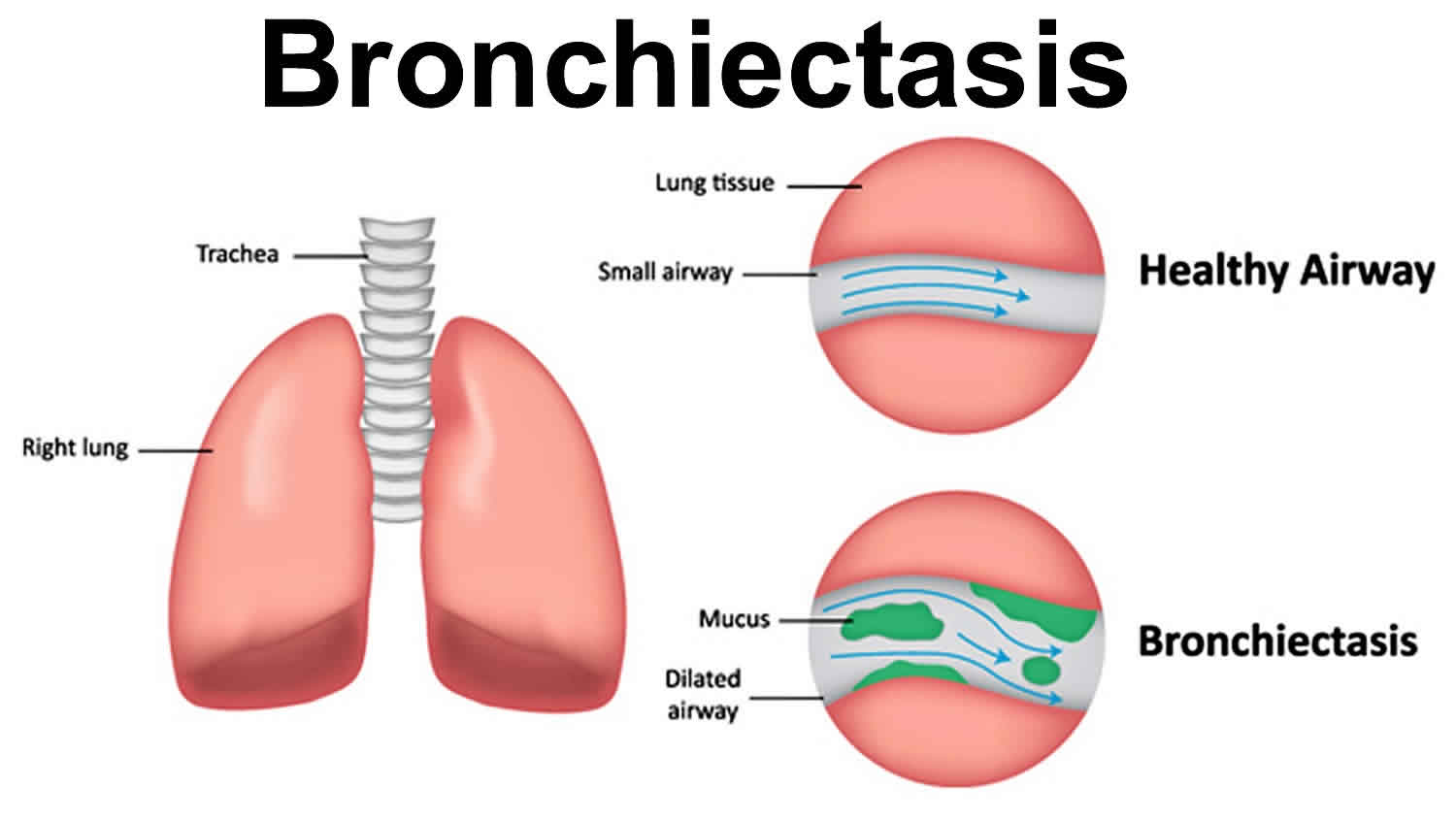
Bronchiectasis is a chronic condition where the walls of the bronchi (the main airways of the lungs) become abnormally widened and flabby and scarred due to inflammation and infection, leading to a build-up of excess mucus that can make the lungs more vulnerable to infection. Bronchiectasis usually is the result of an infection or other condition that injures the walls of your main airways or prevents the airways from clearing mucus. Mucus is a slimy substance that the airways produce to help remove inhaled dust, bacteria, and other small particles.
In bronchiectasis, your airways slowly lose their ability to clear out mucus. When mucus can’t be cleared, it builds up and creates an environment in which bacteria can grow. This leads to repeated, serious lung infections. Each infection causes more damage to your airways. Over time, the airways lose their ability to move air in and out. This can prevent enough oxygen from reaching your vital organs.
Bronchiectasis can lead to serious health problems, such as respiratory failure, atelectasis and heart failure.
People with bronchiectasis have periodic flare-ups of breathing difficulties, called exacerbations.
Bronchiectasis can affect just one section of one of your lungs or many sections of both lungs.
The initial lung damage that leads to bronchiectasis often begins in childhood. However, symptoms may not occur until months or even years after you start having repeated lung infections.
In the United States, common childhood infections—such as whooping cough and measles—used to cause many cases of bronchiectasis. However, these causes are now less common because of vaccines and antibiotics.
Now bronchiectasis usually is due to a medical condition that injures the airway walls or prevents the airways from clearing mucus. Examples of such conditions include cystic fibrosis and primary ciliary dyskinesia 1.
Bronchiectasis that affects only one part of the lung may be caused by a blockage rather than a medical condition.
Bronchiectasis can be congenital or acquired:
- Congenital bronchiectasis affects infants and children. It’s the result of a problem with how the lungs form in a fetus.
- Acquired bronchiectasis occurs as a result of another condition or factor. This type of bronchiectasis can affect adults and older children. Acquired bronchiectasis is more common than the congenital type.
The most common symptoms of bronchiectasis include:
- a persistent cough that usually brings up phlegm (sputum)
- breathlessness
The severity of symptoms can vary widely. Some people have only a few symptoms that don’t appear often, while others have wide-ranging daily symptoms.
The symptoms tend to get worse if you develop an infection in your lungs.
You should see your doctor if you develop a persistent cough. While this may not be caused by bronchiectasis, it requires further investigation.
If your doctor suspects you may have bronchiectasis, they’ll refer you to a specialist in treating lung conditions (a respiratory consultant) for further tests.
The damage caused to the lungs by bronchiectasis is permanent, but treatment can help relieve your symptoms and stop the damage getting worse.
The main treatments include:
- exercises and special devices to help you clear mucus out of your lungs
- medication to help improve airflow within the lungs
- antibiotics to treat any lung infections that develop
Surgery is usually only considered for bronchiectasis in rare cases where other treatments haven’t been effective, the damage to your bronchi is confined to a small area, and you’re in good general health.
Bronchiectasis key facts
- In people with bronchiectasis, the walls of the bronchi become thickened.
- Bacteria and other microbes often infect the lungs of people with bronchiectasis, and this leads to worsened breathing and other symptoms.
- People with bronchiectasis have periodic flare-ups of breathing difficulties, called exacerbations.
How the lungs are affected by bronchiectasis
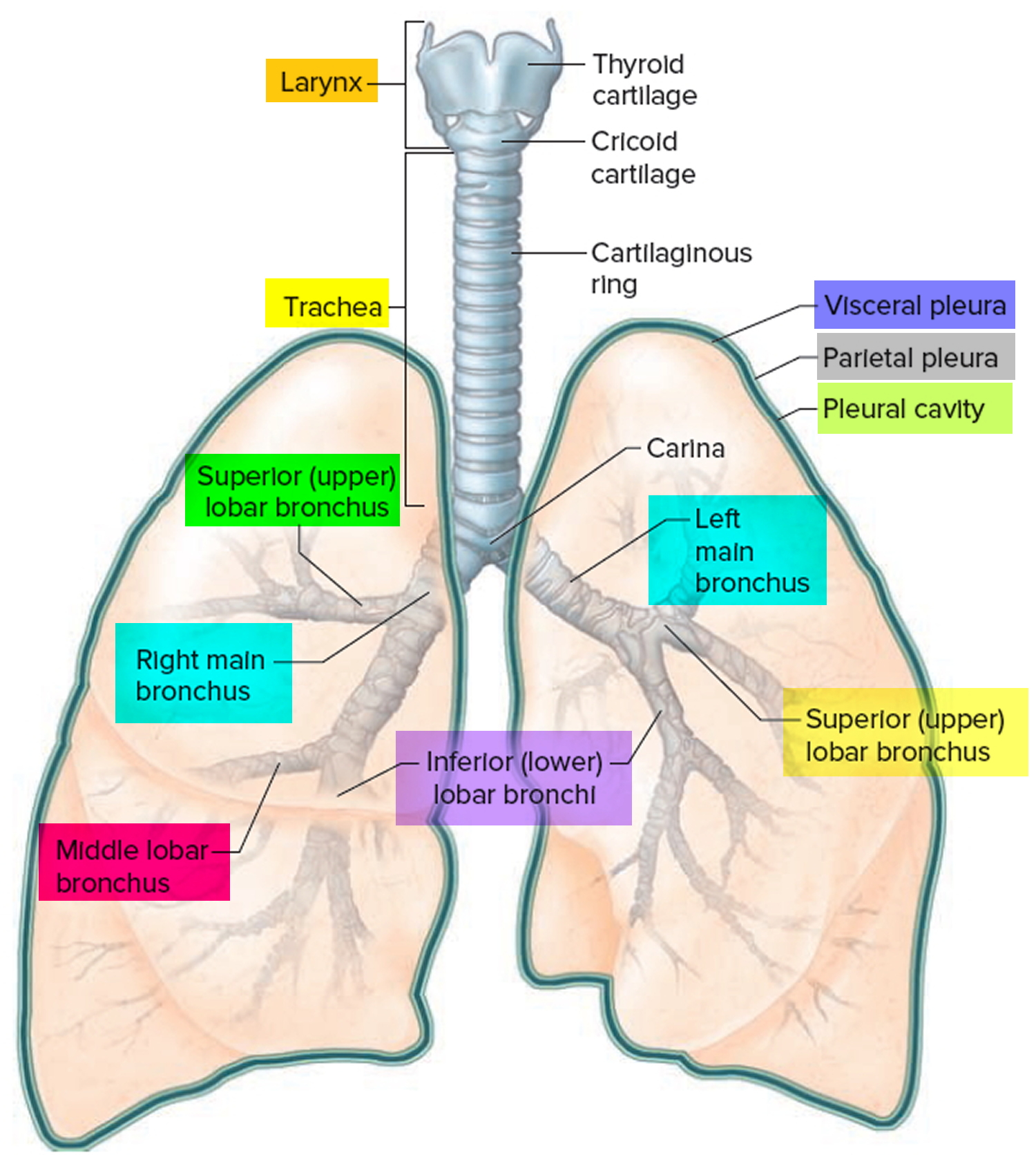
The lungs are full of tiny branching airways known as bronchi. Oxygen travels through these airways, ends up in tiny sacs called alveoli, and from there is absorbed into the bloodstream.
The inside walls of the bronchi are coated with sticky mucus, which protects against damage from particles moving down into the lungs.
In bronchiectasis, one or more of the bronchi are abnormally widened. This means more mucus than usual gathers there, which makes the bronchi more vulnerable to infection (see Figure 2 below).
If an infection does develop, the bronchi may be damaged again, so even more mucus gathers in them and the risk of infection increases further.
Over time, this cycle can cause gradually worsening damage to the lungs.
Why it happens
Bronchiectasis can develop if the tissue and muscles that surround the bronchi are damaged or destroyed.
There are many reasons why this may happen. The 3 most common causes are:
- Having had a lung infection in the past, such as pneumonia or whooping cough, that damages the bronchi
- Underlying problems with the immune system (the body’s defence against infection) that make the bronchi more vulnerable to damage from an infection
- Allergic bronchopulmonary aspergillosis – an allergy to a certain type of fungi that can cause the bronchi to become inflamed if spores from the fungi are inhaled
But in many cases, no obvious cause for the condition can be found. This is known as idiopathic bronchiectasis.
Figure 1. Bronchial tree of the lungs
Some people with bronchiectasis develop a severe lung infection that may need to be treated in hospital.
Signs and symptoms of a serious lung infection include:
- a blueish tinge to the skin and lips (cyanosis)
- confusion
- a high temperature of 100.4 °F (38 °C) or above
- rapid breathing (more than 25 breaths a minute)
- severe chest pain that makes it too painful to cough and clear your lungs
If you experience any of the above, phone the healthcare professional in charge of your care immediately.
This may be your doctor, a doctor who specializes in lung conditions (pulmonologist), or a specialist nurse.
When to seek medical advice
If you haven’t previously been diagnosed with bronchiectasis and you develop a persistent cough, visit your doctor for advice.
While persistent coughing may not necessarily be the result of bronchiectasis, it requires further investigation.
If you have been diagnosed with bronchiectasis previously and begin to experience symptoms that suggest you have a lung infection, contact your doctor.
You’ll usually need treatment with antibiotics.
Some people with bronchiectasis are given a stock of antibiotics as a precaution in case they suddenly develop a lung infection.
Is bronchiectasis contagious?
No. Bronchiectasis is a chronic condition where the walls of the bronchi (the main airways of the lungs) become abnormally widened and flabby and scarred due to inflammation and infection, leading to a build-up of excess mucus that can make the lungs more vulnerable to infection.
Bronchiectasis can develop if the tissue and muscles that surround the bronchi are damaged or destroyed.
There are many reasons why this may happen. The 3 most common causes are:
- Having had a lung infection in the past, such as pneumonia or whooping cough, that damages the bronchi
- Underlying problems with the immune system (the body’s defence against infection) that make the bronchi more vulnerable to damage from an infection
- Allergic bronchopulmonary aspergillosis – an allergy to a certain type of fungi that can cause the bronchi to become inflamed if spores from the fungi are inhaled
But in many cases, no obvious cause for the condition can be found. This is known as idiopathic bronchiectasis.
Bronchiectasis vs Bronchitis
Bronchitis is an inflammation of the bronchial tubes, the major airways that carry air into your lungs. Bronchitis causes a cough that often brings up mucus. Bronchitis can also cause shortness of breath, wheezing, a low fever, and chest tightness. There are two main types of bronchitis: acute and chronic bronchitis.
Acute bronchitis is the sudden development of inflammation in bronchial tubes. Acute bronchitis usually happens because of a virus or breathing in things that irritate the lungs such as tobacco smoke, fumes, dust and air pollution. Bacteria sometimes cause acute bronchitis.
Acute bronchitis is temporary and usually does not cause any permanent breathing difficulties. Most cases of acute bronchitis get better within several days. But your cough can last for several weeks after the infection is gone.
It is possible for people with weakened immune systems or other major health problems to develop severe problems such as pneumonia or respiratory failure. In general, those who develop major problems from acute bronchitis are:
- The elderly
- Young children
- People with other major health conditions including cancer or diabetes
- People who have not been immunized for the flu, pneumonia and whooping cough.
The same viruses that cause colds and the flu often cause acute bronchitis. These viruses spread through the air when people cough, or though physical contact (for example, on unwashed hands). Being exposed to tobacco smoke, air pollution, dusts, vapors, and fumes can also cause acute bronchitis. Less often, bacteria can also cause acute bronchitis.
To diagnose acute bronchitis, your health care provider will ask about your symptoms and listen to your breathing. You may also have other tests.
Treatments include rest, fluids, and aspirin (for adults) or acetaminophen to treat fever. A humidifier or steam can also help. You may need inhaled medicine to open your airways if you are wheezing. Antibiotics won’t help if the cause is viral. You may get antibiotics if the cause is bacterial.
Bronchiectasis causes
Bronchiectasis is caused by the airways of the lungs becoming damaged and widened. This can be the result of an infection or another condition, but sometimes the cause isn’t known. Your lungs are continually exposed to germs, so your body has sophisticated defence mechanisms designed to keep the lungs free of infection.
If a foreign substance (such as bacteria or a virus) gets past these defences, your immune system will attempt to stop the spread of any infection by sending white blood cells to the location of the infection.
These cells release chemicals to fight the infection, which can cause the surrounding tissue to become inflamed.
For most people, this inflammation will pass without causing any further problems.
But bronchiectasis can occur if the inflammation permanently destroys the elastic-like tissue and muscles surrounding the bronchi (airways), causing them to widen.
The abnormal bronchi then become filled with excess mucus, which can trigger persistent coughing and make the lungs more vulnerable to infection.
If the lungs become infected again, this can result in further inflammation and further widening of the bronchi.
As this cycle is repeated, the damage to the lungs gets progressively worse.
How quickly bronchiectasis progresses can vary significantly. For some people, the condition will get worse quickly, but for many the progression is slow.
Bronchiectasis common causes
In around half of all cases of bronchiectasis, no obvious cause can be found. This is known as idiopathic bronchiectasis.
Some of the more common triggers that have been identified are described below.
Childhood infections
Around a third of cases of bronchiectasis in adults are associated with a severe lung infection in childhood, such as:
- Severe pneumonia
- Whooping cough
- Tuberculosis (TB)
- Measles (uncommon in the United States due to vaccination)
But as there are now vaccinations available for these infections, it’s expected that childhood infections will become a less common cause of bronchiectasis in the future.
Immunodeficiency
Some cases of bronchiectasis occur because a person has a weakened immune system, which makes their lungs more vulnerable to tissue damage.
The medical term for having a weakened immune system is immunodeficiency.
Some people are born with an immunodeficiency because of problems with the genes they inherit from their parents, such as common variable immunodeficiency.
It’s also possible to acquire an immunodeficiency after an infection such as HIV and AIDS.
Allergic bronchopulmonary aspergillosis
Some people with bronchiectasis develop the condition as a complication of an allergic condition known as allergic bronchopulmonary aspergillosis (ABPA) or allergic bronchopulmonary aspergillosis.
People with allergic bronchopulmonary aspergillosis (ABPA) have an allergy to a type of fungi known as aspergillus, which is found in a wide range of different environments across the world.
If a person with allergic bronchopulmonary aspergillosis (ABPA) breathes in fungal spores, it can trigger an allergic reaction and persistent inflammation, which in turn can progress to bronchiectasis.
Aspiration
Aspiration is the medical term for stomach contents accidentally passing into your lungs, rather than down into your gastrointestinal tract.
The lungs are very sensitive to the presence of foreign objects, such as small samples of food or even stomach acids, so this can trigger inflammation leading to bronchiectasis.
Chronic (ongoing) pulmonary aspiration is a condition in which you inhale food, liquids, saliva, or vomited stomach contents into your lungs. Aspiration can inflame the airways, which can lead to bronchiectasis.
Cystic fibrosis
Cystic fibrosis leads to almost half of the cases of bronchiectasis in the United States. Cystic fibrosis is a relatively common genetic disorder, where the lungs become clogged up with mucus.
The mucus then provides an ideal environment for a bacterial infection to take place, leading to the symptoms of bronchiectasis.
Cilia abnormalities
Cilia are the tiny hair-like structures that line your airways in the lungs. They’re designed to protect the airways and help move away any excess mucus (a slimy substance) out of your airways.
Bronchiectasis can develop if there’s a problem with the cilia that means they’re unable to effectively clear mucus from the airways.
Conditions that can cause problems with the cilia include:
- Young’s disease – a rare condition only affecting males thought to be caused by exposure to mercury in childhood
- Primary ciliary dyskinesia – a rare condition caused by inheriting faulty genes
But as the regulations regarding the use of mercury are now much stricter than they were in the past, it’s expected that Young’s syndrome will become a much less common cause of bronchiectasis in the future.
Connective tissue diseases
Certain conditions that cause inflammation in other areas of the body are sometimes associated with bronchiectasis.
These include:
- Rheumatoid arthritis
- Sjögren’s syndrome
- Crohn’s disease
- Ulcerative colitis
These conditions are usually thought to be caused by a problem with the immune system, where it mistakenly attacks healthy tissue.
Other conditions
Other conditions, such as an airway blockage, also can lead to bronchiectasis. Many things can cause a blockage, such as a growth or a noncancerous tumor. An inhaled object, such as a piece of a toy or a peanut that you inhaled as a child, also can cause an airway blockage.
A problem with how the lungs form in a fetus may cause congenital bronchiectasis. This condition affects infants and children.
Risk factors for bronchiectasis
People who have conditions that damage the lungs or increase the risk of lung infections are at risk for bronchiectasis. Such conditions include:
- Cystic fibrosis. This disease leads to almost half of the cases of bronchiectasis in the United States.
- Immunodeficiency disorders, such as common variable immunodeficiency and, less often, HIV and AIDS.
- Allergic bronchopulmonary aspergillosis. This is an allergic reaction to a fungus called aspergillus. The reaction causes swelling in the airways.
- Disorders that affect cilia function, such as primary ciliary dyskinesia. Cilia are small, hair-like structures that line your airways. They help clear mucus (a slimy substance) out of your airways.
Bronchiectasis can develop at any age. Overall, two-thirds of people who have the condition are women. However, in children, the condition is more common in boys than in girls.
Bronchiectasis prevention
To prevent bronchiectasis, it’s important to prevent the lung infections and lung damage that can cause it.
Childhood vaccines for measles and whooping cough prevent infections related to these illnesses. These vaccines also reduce complications from these infections, such as bronchiectasis.
Avoiding toxic fumes, gases, smoke, and other harmful substances also can help protect your lungs.
Proper treatment of lung infections in children also may help preserve lung function and prevent lung damage that can lead to bronchiectasis.
Stay alert to keep children (and adults) from inhaling small objects (such as pieces of toys and food that might stick in a small airway). If you think you, your child, or someone else has inhaled a small object, seek prompt medical care.
In some cases, treating the underlying cause of bronchiectasis can slow or prevent its progression.
Bronchiectasis signs and symptoms
The initial airway damage that leads to bronchiectasis often begins in childhood. However, signs and symptoms may not appear until months or even years after you start having repeated lung infections.
The most common symptom of bronchiectasis is a persistent cough that occurs over months or years, that brings up a large amount of phlegm (sputum) on a daily basis. The phlegm (sputum) can be clear, pale yellow or yellow-greenish in color. Other people may only occasionally cough up small amounts of phlegm, or none at all.
Other symptoms may include:
- Shortness of breath
- Wheezing
- Coughing up blood or bloodstained phlegm
- Chest pain
- Joint pain
- Clubbing of the fingertips – the tissue beneath the nail thickens and the fingertips become rounded and bulbous
If your doctor listens to your lungs with a stethoscope, he or she may hear abnormal lung sounds.
Over time, you may have more serious symptoms. You may cough up blood or bloody mucus and feel very tired. Children may lose weight or not grow at a normal rate.
Signs of a lung infection:
If you develop a lung infection, your symptoms usually get worse within a few days. This is known as an infective exacerbation.
It can cause:
- coughing up even more phlegm, which may be more green than usual or smell unpleasant
- worsening shortness of breath
You may also:
- feel very tired
- cough up blood, if you haven’t already done so
- experience a sharp chest pain that’s made worse when breathing (pleurisy)
- feel generally unwell
Bronchiectasis complications
Complications of bronchiectasis are rare, but they can be serious.
Complications of bronchiectasis may include:
- Cor pulmonale
- Coughing up blood
- Low oxygen levels (in severe cases)
- Recurrent pneumonia
- Depression
Severe bronchiectasis can lead to other serious health conditions, such as respiratory failure and atelectasis.
Respiratory failure is a condition in which not enough oxygen passes from your lungs into your blood. The condition also can occur if your lungs can’t properly remove carbon dioxide (a waste gas) from your blood.
Respiratory failure can cause shortness of breath, rapid breathing, and air hunger (feeling like you can’t breathe in enough air). In severe cases, signs and symptoms may include a bluish color on your skin, lips, and fingernails; confusion; and sleepiness.
Atelectasis is a condition in which one or more areas of your lungs collapse or don’t inflate properly. As a result, you may feel short of breath. Your heart rate and breathing rate may increase, and your skin and lips may turn blue.
If bronchiectasis is so advanced that it affects all parts of your airways, it may cause heart failure. Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs.
The most common signs and symptoms of heart failure are shortness of breath or trouble breathing, tiredness, and swelling in the ankles, feet, legs, abdomen, and veins in the neck.
Other serious complications of bronchiectasis is coughing up large amounts of blood, caused by one of the blood vessels in the lungs splitting. This can be life threatening and may require emergency surgery to treat it.
Coughing up large amounts of blood
A rare, but serious, complication of bronchiectasis is coughing up large amounts of blood (the medical term for this is massive hemoptysis).
This can occur when a section of one of the blood vessels supplying the lungs suddenly splits open.
Symptoms that may indicate massive hemoptysis include:
- coughing up more than 100ml of blood in a 24-hour period – 100ml is roughly equivalent to a third of a can of drink
- breathing difficulties – caused by blood obstructing your airways
- feeling lightheaded and dizzy, and having cold, clammy skin – caused by rapid blood loss
Massive hemoptysis is a medical emergency. If you think someone is experiencing massive hemoptysis, call your local emergency services number for an ambulance.
A person with massive hemoptysis needs to be admitted to hospital. A tube may need to be placed into their throat to assist them with their breathing.
A procedure called a bronchial artery embolization will be required to stop the bleeding.
During a bronchial artery embolization, a special dye is injected into your arteries so they show up clearly on X-rays.
Then, using X-ray scans as a guide, the source of the bleeding is located and injected with tiny particles, around the size of a grain of sand, that will help clog the vessel up and stop the bleeding.
Bronchiectasis prognosis
Currently, bronchiectasis has no cure. The prognosis for people with bronchiectasis is highly variable and often depends on the underlying cause. With treatment, most people live without major disability.
For people with very severe symptoms, however, bronchiectasis can be fatal if the lungs stop working properly. However, with proper care, most people who have it can enjoy a good quality of life.
Early diagnosis and treatment of bronchiectasis are important. The sooner your doctor starts treating bronchiectasis and any underlying conditions, the better your chances of preventing further lung damage.
Bronchiectasis life expectancy
Living with bronchiectasis can be stressful and frustrating, but most people with the condition have a normal life expectancy.
Bronchiectasis diagnosis
Your doctor may suspect bronchiectasis if you have a daily cough that produces large amounts of sputum (spit).
To find out whether you have bronchiectasis, your doctor may recommend tests to:
- Identify any underlying causes that require treatment
- Rule out other causes of your symptoms
- Find out how much your airways are damaged
Diagnostic Tests and Procedures
Chest CT Scan
A chest computed tomography scan, or chest CT scan, is the most common test for diagnosing bronchiectasis. Currently, the most effective test available to diagnose bronchiectasis is called a high-resolution CT (HRCT) scan. A high-resolution CT (HRCT) scan involves taking several X-rays of your chest at slightly different angles. A computer is then used to put all the images together.
This produces a very detailed picture of the inside of your body, and the airways inside your lungs (the bronchi) should show up very clearly.
In a healthy pair of lungs, the bronchi should become narrower the further they spread into your lungs, in the same way a tree branch separates into narrower branches and twigs.
If the high-resolution CT (HRCT) scan shows that a section of airways is actually getting wider, this usually confirms bronchiectasis.
Chest X Ray
This painless test creates pictures of the structures in your chest, such as your heart and lungs. A chest x ray can show areas of abnormal lung and thickened, irregular airway walls.
Other Tests
Your doctor may recommend other tests, such as:
- Blood tests. These tests can show whether you have an underlying condition that can lead to bronchiectasis. Blood tests also can show whether you have an infection or low levels of certain infection-fighting blood cells.
- A sputum culture. Lab tests can show whether a sample of your sputum contains bacteria (such as the bacteria that cause tuberculosis) or fungi.
- Lung function tests. A small, handheld device (a spirometer) that you blow into is used to measure how hard and how quickly you can expel air from your lungs; this can assess how well your lungs are working. Lung function tests help show how much lung damage you have.
- A sweat test or other tests for cystic fibrosis.
Bronchoscopy
If your bronchiectasis doesn’t respond to treatment, your doctor may recommend bronchoscopy (bron-KOS-ko-pee). Doctors use this procedure to look inside the airways.
During bronchoscopy, a flexible tube with a light on the end is inserted through your nose or mouth into your airways. The tube is called a bronchoscope. It provides a video image of your airways. You’ll be given medicine to numb your upper airway and help you relax during the procedure.
Bronchoscopy can show whether you have a blockage in your airways. The procedure also can show the source of any bleeding in your airways.
Bronchiectasis treatment
The damage to the lungs associated with bronchiectasis is permanent, but treatment can help prevent the condition getting worse.
In most cases, treatment involves a combination of medication, hydration, and chest physical therapy (CPT), exercises you can learn, and devices to help clear your airways. Surgery for bronchiectasis is rare. Your doctor may recommend surgery if the bronchiectasis is isolated to a section of lung or you have a lot of bleeding.
There are a number of things you can do to help relieve the symptoms of bronchiectasis and stop the condition getting worse.
These include:
- stopping smoking (if you smoke)
- having the flu vaccine every year
- making sure you have had the pneumococcal vaccine to protect against pneumonia
- exercising regularly
- keeping yourself well hydrated
- eating a balanced diet
If the bronchiectasis is widespread and causing respiratory failure, your doctor may recommend oxygen therapy.
The goals of treatment are to:
- Treat any underlying conditions and lung infections.
- Remove mucus (a slimy substance) from your lungs. Maintaining good hydration helps with mucus removal.
- Prevent complications.
Early diagnosis and treatment of the underlying cause of bronchiectasis may help prevent further lung damage.
In addition, any disease associated with the bronchiectasis, such as cystic fibrosis or immunodeficiency, also should be treated.
Medicines
Your doctor may prescribe antibiotics, bronchodilators, inhaled corticosteroids, expectorants, or mucus-thinning medicines to treat bronchiectasis.
Expectorants and Mucus-Thinning Medicines
Your doctor may prescribe expectorants and mucus thinners to help you cough up mucus.
Expectorants help loosen the mucus in your lungs. They often are combined with decongestants, which may provide extra relief. Mucus thinners, such as acetylcysteine, loosen the mucus to make it easier to cough up.
Mucus thinning medications are often given through a nebulizer, where it is mixed with hypertonic saline solution, turned into a mist, and inhaled deep into the lungs. The medication given through the nebulizer helps to dissolve mucus in the bronchi so that it can be coughed up more easily.
Sometimes another inhaled mucus thinning medication called dornase alfa (Pulmozyme®) is given to patients with bronchiectasis who have non-cystic fibrosis bronchiectasis.
For some of these treatments, little information is available to show how well they work.
Bronchodilators
Bronchodilators relax the muscles around your airways. This helps open your airways and makes breathing easier. Most bronchodilators are inhaled medicines. You will use an inhaler or a nebulizer to breathe in a fine mist of medicine. Nebulizers are devices consisting of a face mask or mouthpiece, a chamber to convert the medication into a fine mist, and a compressor to pump the medication into your lungs. Examples of this type of medication include beta 2-adrenergic agonist, anticholinergics and theophylline.
Inhaled bronchodilators work quickly because the medicine goes straight to your lungs. Your doctor may recommend that you use a bronchodilator right before you do chest physical therapy (CPT).
Inhaled Corticosteroids
If you also have wheezing or asthma with your bronchiectasis, your doctor may prescribe inhaled corticosteroids (used to treat inflammation in the airways).
Antibiotics
Antibiotics are the main treatment for the repeated lung infections that bronchiectasis causes. Oral antibiotics often are used to treat these infections.
For hard-to-treat infections, your doctor may prescribe intravenous (IV) antibiotics. These medicines are given through an IV line inserted into your arm. Your doctor may help you arrange for a home care provider to give you IV antibiotics at home.
Some antibiotics can be inhaled using a nebulizer machine. Macrolides are a type of antibiotic that not only kill certain types of bacteria but also reduce inflammation in the bronchi. Examples of macrolides include azithromycin, erythromycin, and clarithromycin. Sometimes macrolides are given for long-term use over several months. This may be beneficial for some people but also may come with serious side effects, like diarrhea, nausea, hearing loss, dizziness, and the development of resistant bacteria in the lungs. You should discuss with your healthcare provider whether the use of a macrolide is appropriate for you.
Preventative treatment
If you have 3 or more infective exacerbations in any one year or your symptoms during an infective exacerbation were particularly severe, it may be recommended that you take antibiotics on a long-term basis.
This can help prevent further infections and give your lungs the chance to recover.
This could involve taking low-dose antibiotic tablets to minimise the risk of side effects, or using an antibiotic nebulizer.
Using antibiotics in this way increases the risk that one or more types of bacteria will develop a resistance to the antibiotic. You may be asked to give regular phlegm samples to check for any resistance.
If bacteria do show signs of developing a resistance, your antibiotic may need to be changed.
Hydration
Drinking plenty of fluid, especially water, helps prevent airway mucus from becoming thick and sticky. Good hydration helps keep airway mucus moist and slippery, which makes it easier to cough up.
Chest Physical Therapy
Chest physical therapy (CPT) also is called physiotherapy or chest clapping or percussion. This technique is generally performed by a respiratory therapist but can be done by a trained member of the family. It involves the therapist pounding your chest and back over and over with his or her hands or a device. Doing this helps loosen the mucus from your lungs so you can cough it up.
You can sit with your head tilted down or lie on your stomach with your head down while you do chest physical therapy (CPT). Gravity and force help drain the mucus from your lungs.
Devices
Some people find chest physical therapy (CPT) hard or uncomfortable to do. There are also a number of handheld devices that can help remove mucus from your lungs.
Although these devices look different, most work in a similar way. Generally, they use a combination of vibrations and air pressure to make it easier to cough out any mucus.
Several devices can help with chest physical therapy, such as:
- An electric chest clapper, known as a mechanical percussor.
- An inflatable therapy vest that uses high-frequency air waves to force mucus toward your upper airways so you can cough it up.
- A small handheld device that you breathe out through. It causes vibrations that dislodge the mucus.
- A mask that creates vibrations to help break loose mucus from your airway walls.
Examples of these devices include the flutter, the RC cornet and the Acapella.
Some of these methods and devices are popular with patients and doctors, but little information is available on how well they actually work. Choice usually is based on convenience and cost.
Exercises
There are a range of exercises, known as airway clearance techniques, that can help remove mucus from your lungs. This can often help improve coughing and breathlessness in people with bronchiectasis.
You can be referred to a physiotherapist, who can teach you these techniques.
Several breathing techniques also are used to help move mucus to the upper airway so it can be coughed up. These techniques include forced expiration technique (FET) and active cycle breathing (ACB).
Forced expiration technique (FET) involves forcing out a couple of breaths and then doing relaxed breathing. Active cycle breathing (ACB) is forced expiration technique (FET) that involves deep breathing exercises.
Active cycle of breathing techniques
The most widely used technique in the US is called active cycle of breathing (ACB) techniques. Active cycle breathing (ACB) involves repeating a cycle made up of a number of different steps.
These include a period of normal breathing, followed by deep breaths to loosen the mucus and force it up, then coughing the mucus out. The cycle is then repeated for 20 to 30 minutes.
Don’t attempt active cycle of breathing (ACB) if you haven’t first been taught the steps by a suitably trained physiotherapist, as performing the techniques incorrectly could damage your lungs.
If you’re otherwise in good health, you’ll probably only need to perform active cycle of breathing (ACB) once or twice a day. If you develop a lung infection, you may need to perform active cycle of breathing (ACB) on a more frequent basis.
Postural drainage
Changing your position can also make it easier to remove mucus from your lungs. This is known as postural drainage.
Each technique can involve several complex steps, but most techniques involve leaning or lying down while the physiotherapist or a carer uses their hands to vibrate certain sections of your lungs as you go through a series of “huffing” and coughing.
Oxygen Therapy
Oxygen therapy can help raise low blood oxygen levels. For this treatment, you’ll receive oxygen through nasal prongs or a mask. Oxygen therapy can be done at home, in a hospital, or in another health facility.
Surgery
Your doctor may recommend surgery if no other treatments have helped and only one part of your airway is affected and you don’t have an underlying condition that could cause bronchiectasis to recur. If you have major bleeding in your airway, your doctor may recommend surgery to remove part of your airway or a procedure to control the bleeding.
The lungs are made up of sections known as lobes – the left lung has 2 lobes and the right lung has 3 lobes.
Surgery for focal bronchiectasis would usually involve removing the lobe affected by the bronchiectasis in a type of operation known as a lobectomy.
Surgery won’t be used if more than one lobe is affected, as it’s too dangerous to remove so much lung tissue.
In very rare instances of severe bronchiectasis, your doctor may recommend that you receive a lung transplant replacing your diseased lungs with a healthy set of lungs.
Living with bronchiectasis
Early diagnosis and treatment of bronchiectasis can prevent further damage to your lungs. People who have bronchiectasis should have ongoing care and try to follow a healthy lifestyle.
Ongoing Care
If you have bronchiectasis, work closely with your doctor to learn how to improve your quality of life. This involves learning as much as you can about bronchiectasis and any underlying conditions that you have.
Take steps to avoid lung infections. Ask your doctor about getting flu and pneumonia vaccines. Wash your hands often to lower your risk of getting viruses and bacterial infections.
Healthy Lifestyle
Following a healthy lifestyle is important for overall health and well-being. For example, if you smoke, try to quit. Smoking harms nearly every organ in your body, including your lungs.
Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
You also can protect your airways by avoiding toxic fumes, gases, and other harmful substances.
A healthy lifestyle also involves following a healthy diet. A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
Staying hydrated also is important. Drinking plenty of fluids, especially water, helps prevent airway mucus from becoming thick and sticky.
Try to be as physically active as you can. Physical activity, such as walking and swimming, can help loosen mucus. Ask your doctor what types and amounts of activity are safe for you.
- Bronchiectasis. https://www.nhlbi.nih.gov/health-topics/bronchiectasis[↩]