Contents
Carrion disease
Carrion’s disease also known as Peruvian wart, Oroya fever or Bartonellosis is an infectious disease caused by flagellated Gram-negative bacteria Bartonella bacilliformis that only occurs in the Andes Mountains at an altitude of 600 to 3200 m (≈1,968–10,498 ft) above sea level including Peru, Ecuador and Colombia 1, 2, 3. However, Carrion’s disease has recently been found to be spreading and emerging in some coastal areas of Guayas and Manabi in Ecuador and Amazonian locations 2, 3. Most Carrion disease cases are reported in Peru. In Peru, Carrion disease has been found in different regions along the Andes such as Piura, Amazonas, Cajamarca, La Libertad, Ancash, Lima, Huancavelica, Ayacucho, and Cusco 4, 5.
Carrion disease is transmitted to humans through the bite of blood sucking infected sand flies of the genus Lutzomyia, mainly the species Lutzomyia verrucarum (Figure 2) 6, 7.
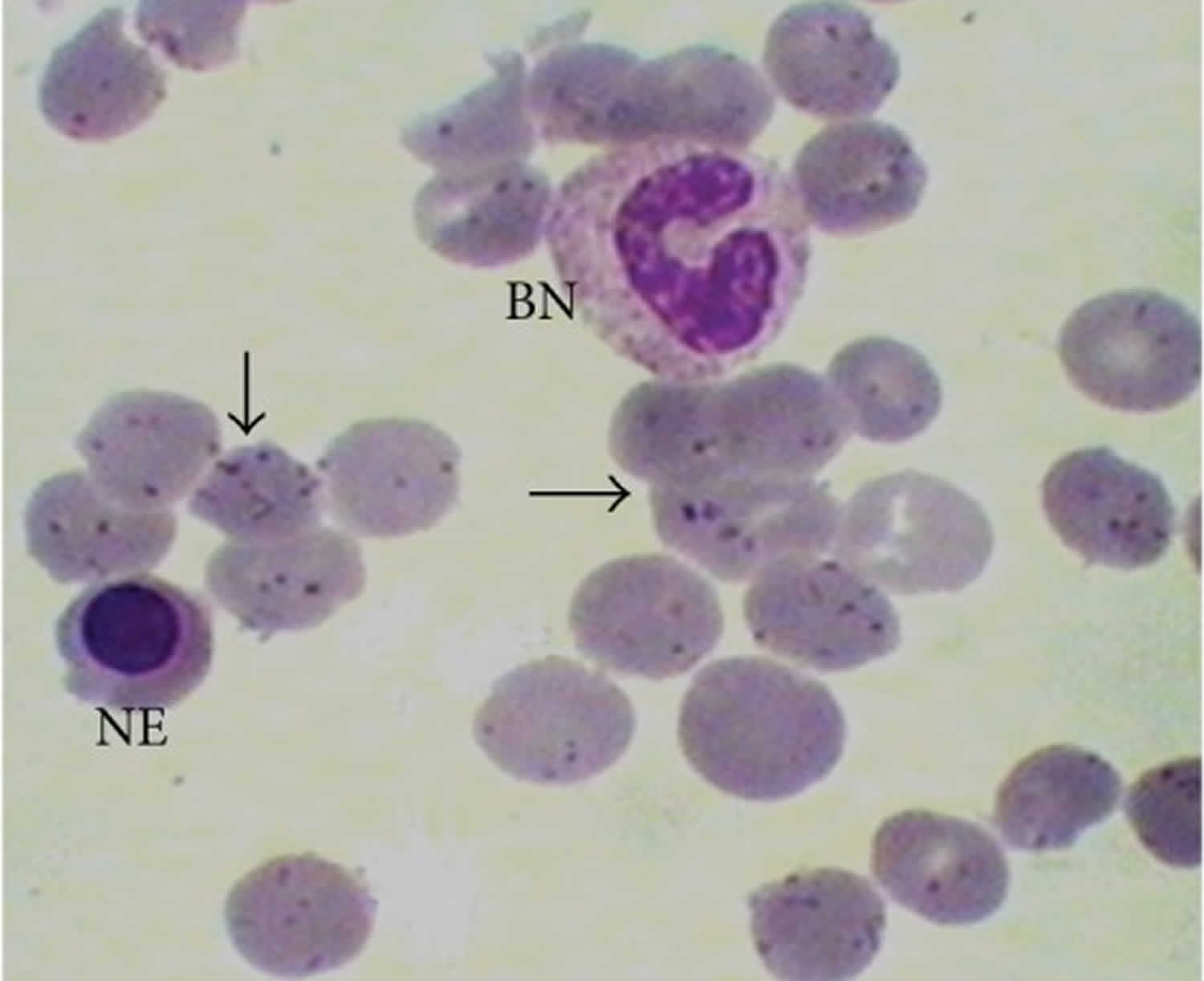
Bartonella bacilliformis bacteria are able to enter the bloodstream and parasitically invade red blood cells (erythrocytes) (Figure 1).
Carrion disease has been divided in to several clinical phases; two of the most remarkable phases are as follows 1:
- The hematic phase or acute phase also known as “Oroya fever” common symptoms of which are fever, hemolytic anemia, headache, pale appearance (pallor), muscle aches and pain, joint pain (arthralgia), and loss of consciousness. With an immune-compromised state Oroya fever facilitates secondary infections with Toxoplasma gondii myocarditis or bacteremia with Staphylococcus aureus or Salmonella enterica 8. Left untreated, Oroya fever is frequently referred to as having one of the highest death rates of all infectious diseases, being from 40 to 85% 9 and achieving 88% in a study by Gray and colleagues 10. Fortunately, effective antibiotic treatment is now available, and the mortality rates have decreased (10% case-fatality rates) 11. Partial immunity is developed after infection by Bartonella bacilliformis, resulting in high numbers of asymptomatic carriers 12.
- The chronic phase or eruptive phase or verrucous phase also known as “Peruvian wart” or “verruga peruana”, which appears after the recovery from the acute phase with the appearance of vascularized skin lesions (reddish verrucous eruptive lesions) of different sizes and shapes which is due secondary invasion of endothelial cells lining blood vessels and capillaries 5, 13. In some cases, patients without a history of the acute illness can display the verrucous phase. This phase has a very low mortality 12, 14.
These two phases typically occur sequentially but sometimes independently. A few cases of Oroya fever and Peruvian warts (verruga peruana) have been reported in American travelers who returned from the Andean highlands in South America, but the risk is low.
The persistence of Carrion’s disease in regions where it is endemic is associated mainly with poverty, warm weather, living conditions, low levels of education 15, 12. In endemic areas, the presence of asymptomatic carriers is important; research so far has indicated humans to be the only reservoir of Bartonella bacilliformis bacteria that cause Carrion disease. Evidence suggests that outbreaks of Carrion disease represent the emergence, in areas of nonendemicity, or the resurgence of Carrion disease, which appears to be an infectious emerging or reemerging pathology with a wide geographic range 5, 16.
Carrion’s disease usually affects men, with a slightly higher prevalence than for women 10, 17, 18, 19. Furthermore, Carrion’s disease has been considered an occupational disease in light of infected sand fly exposure of seasonal workers, mainly men, in most of the affected areas (e.g., coffee plantation workers living outside and traveling to areas of endemicity) 20. Moreover, the relationship between coffee plantations and the presence of Lutzomyia species sand flies has also been described 21.
Both children and pregnant women are especially affected. Fetal deaths, miscarriages, and premature births rank among the most serious Carrion’s disease complications affecting pregnant women 22. Children are the most affected by the acute phase of Carrion’s disease 18, 23. Additionally, high levels of malnutrition enhance the severity of Carrion disease 24.
Currently, the diagnosis of Carrion’s disease presents important limitations. The initial fever stage is often misdiagnosed because its symptom is similar to that of other illnesses 17, 25, 26, 27, 28. Although the warty phase is easier to diagnose, incorrect diagnosis can be made, especially in regions where the disease is not present and in cases imported from areas where it is endemic. One example was reported by Maguiña et al. 27, in which erroneous initial diagnoses were made in 19% of patients, including skin tumor in 7 patients, hemangioma in 5 patients, polyarthralgias in 2 patients, and systemic lupus erythematosis in 1 patient. Moreover, without the diagnosis of asymptomatic carriers, perpetuation of the disease will never end.
The treatment of Carrion’s disease differs depending on which phase of the disease is presented and includes blood transfusions and antibiotic agents 29.
Antibiotics typically used to treat Carrion disease in the systemic phase are:
- Adults: ciprofloxacin and chloramphenicol for 14 days
- Children: amoxicillin plus clavulanic acid for 14 days 12
The treatment of choice for Carrion disease in the cutaneous phase is:
- Azithromycin as a first-line treatment
- Erythromycin, ciprofloxacin, and rifampicin as second-line treatment 12
Figure 1. Carrion disease
Footnote: Blood smear of Carrion disease patient in acute phase. Parasitized red blood cells (erythrocytes) by bacillary and coccoid forms of Bartonella bacilliformis (arrows), a nucleated erythrocyte (NE), and a band neutrophil (BN) can be observed. Giemsa stain, 1000x.
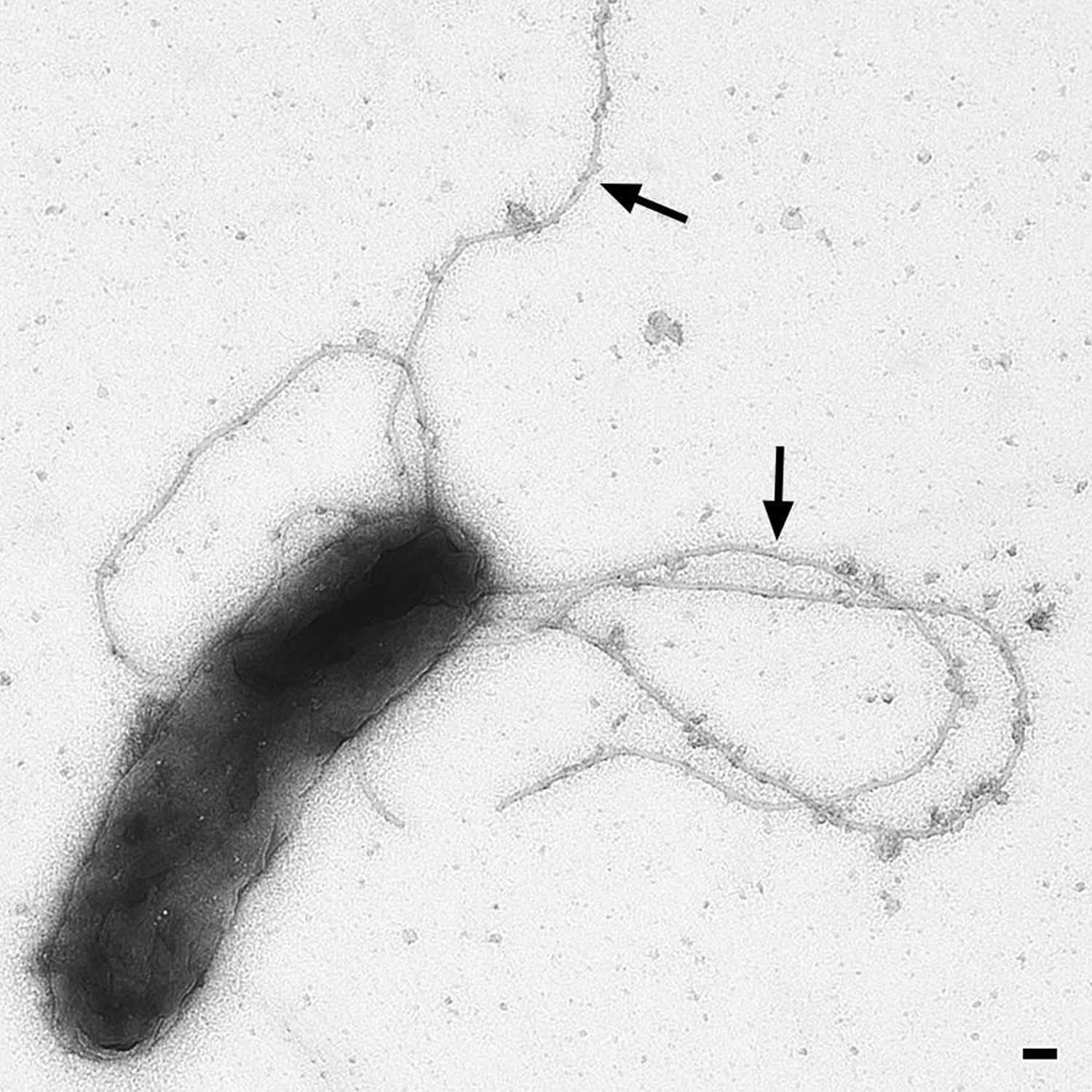
[Source 1 ]Figure 2. Bartonella bacilliformis
Footnotes: Electron microscopy of Bartonella bacilliformis ATCC 35686 (grown for four days at 28 °C in Bartonella liquid medium). Arrows indicate the presumptive BbadA expression on the bacterial surface. Scale-bar: 100 nm
[Source 1 ]Figure 3. Lutzomyia verrucarum sand flies
Footnotes: Adult Lutzomyia verrucarum sand flies. Left: male. Right: blood-fed female. Colony-bred adults. Length of each between 2 and 3 mm
[Source 30 ]Figure 4. Peruvian wart
Footnotes: Patients with Peruvian wart (Verruga peruana) caused by Bartonella bacilliformis. Left: 9-year-old girl with numerous bleeding verrugas on her legs. Right: 17-year-old girl (facing left) showing multiple verrugas close to her left elbow; a single verruga has broken the overlying epidermis, and may later bleed.
[Source 30 ]Who gets Carrion disease?
Most cases of Carrion disease occur in endemic regions of South America, due to the presence of Lutzomyia verrucarum sand flies that carry the Bartonella bacilliformis bacteria. Carrion disease is most prevalent in areas of Peru, Ecuador, and Colombia that are characterized by warm weather and containing populations with low socioeconomic status 12.
Age and the presence of family members with bartonellosis are the best predictors of the possible development of Bartonella bacilliformis infection 31. Bartonella bacilliformis is highly infectious and Bartonella bacilliformis infection are clustered in households. Eighteen percent of cohort households account for 70% of Carrion disease cases. This pattern of bartonellosis implies that 80% of cases take place in 20% of households (“20/80 rule”) 12. Therefore, people living with an individual infected by Bartonella bacilliformis have a risk to become infected that is 2.6 times greater that uninfected households 31. This finding has been related to the lack of intermediate hosts and person-to-sand fly to person transmission 32. It has also been shown that Carrion disease cases were more likely to report bites than controls in houses near or far away 25.
Children, pregnant women, and malnourished individuals tend to be more severely affected than healthy adults 29.
Carrion disease cause
Carrion disease is caused by flagellated Gram-negative bacteria Bartonella bacilliformis that only occurs in the Andes Mountains at an altitude of 600 to 3200 m (≈1,968–10,498 ft) above sea level including Peru, Ecuador and Colombia 1, 2, 3. However, Carrion’s disease has recently been found to be spreading and emerging in some coastal areas of Guayas and Manabi in Ecuador and Amazonian locations 2, 3. Most Carrion disease cases are reported in Peru. In Peru, Carrion disease has been found in different regions along the Andes such as Piura, Amazonas, Cajamarca, La Libertad, Ancash, Lima, Huancavelica, Ayacucho, and Cusco 4, 5.
Carrion disease is transmitted to humans through the bite of blood sucking infected sand flies of the genus Lutzomyia, mainly the species Lutzomyia verrucarum (Figure 2) 6, 7.
Other possible routes of transmission include direct contact with infected human blood, including blood transfusion, and vertical transmission from mother to child 33, 34, 35, 36, 29. Blood donors are usually apparently healthy people, and as such those who are infected are actually asymptomatic carriers who probably have a low bacterial load in blood, thereby hindering the detection of this microorganism 12. Moreover, there are no studies on how long a person can be an asymptomatic carrier, with as long as 3 years having been described in a specific case of an Ecuadorian expatriate 37. This, together with the ability of Bartonella bacilliformis bacteria to survive for long periods of up to 30 months in blood stored at 4°C, leads to a true risk when blood transfusions are made in areas of endemicity 38. In a PCR analysis of 42 samples from blood donors in an area of nonendemicity in the north of Peru, 2.4% of the samples were found to be positive for Bartonella bacilliformis 39. To avoid this risk, blood banks from Peruvian areas of endemicity include Carrion’s disease among infectious diseases to be considered, while no data about other countries are available 40, 41. Although not considered, Bartonella bacilliformis testing in blood banks outside countries where it is endemic would be extremely valuable due to the natural movement of people who may provide unexpected infected donations in far-away areas. It has been estimated that more than 2.5 million Peruvians live outside the country, with 22.1% of these individuals being from mountain areas 42.
Once transmitted to a human host, Bartonella bacilliformis invades the red blood cells (erythrocytes) and interior surface of the blood vessels (endothelial cells), resulting in a systemic and cutaneous phase respectively.
Carrion’s disease signs and symptoms
The clinical presentation of Carrion’s disease involves 2 syndromes that occur independently or sequentially 26:
- Acute phase called Oroya fever. Oroya fever signs and symptoms may include 29:
- Abdominal pain
- Anorexia
- Arthralgia
- Elevated Bilirubin
- Chills 43
- Diarrhea
- Dyspnea
- Fever (up to 99%) usually less than 100.4°F (<39°C) and intermittent
- Headache
- Reduced Hematocrit (up to >80%)
- Hemolytic Anemia with negative Coombs test (up to >90%)
- Enlarged liver (hepatomegaly)
- Hypothermia
- Jaundice
- Enlarged lymph node (lymphadenopathy)
- Malaise
- Muscle aches and pain (myalgia)
- Nausea and vomiting
- Pale appearance (pallor)
- Pollakiuria
- Elevated C reactive pretein (↑CRP)
- Splenomegaly
- Sweats
- Systolic murmur
- Tachycardia.
- Chronic phase called Peruvian warts or verruga peruana, which appears after the recovery from the acute phase with the appearance of vascularized skin lesions (reddish verrucous eruptive lesions) of different sizes and shapes which is due secondary invasion of endothelial cells lining blood vessels and capillaries 5, 13. However, the presence of Peruvian warts has also been described in the clinical care of acute or recovery phases of Oroya fever 44, 45. And in some cases, patients without a history of the acute illness can display the verrucous phase. Peruvian wart phase signs and symptoms may include 29:
- Arthralgia
- Bone pain
- Fever
- Headache
- Joint pain
- Lymphadenopathy
- Malaise
- Myalgia
- Skin lesions
Once a person is bitten by an infected sand fly, an asymptomatic infection or a mild to severe disease is presented. While the average incubation time of Carrion’s disease is 61 days (between 10 and 210 days) 46, the severity of Carrion disease is probably determined by individual predisposition and the specific virulence of the strain causing infection 12. According to Noguchi 47, strains isolated from people with very mild anemia or Peruvian warts are presumably less virulent. Similarly, Kosek et al. 48 proposed that a strain of Bartonella bacilliformis with diminished virulence had caused the infection when disease manifestations were milder than the typical manifestations of Oroya fever.
Oroya Fever (Acute Carrion disease)
Oroya fever also known as the hematic or systemic acute phase of Carrion disease, is characterized by severe hemolytic anaemia and transient immunosuppression. The major clinical consequences of infection with Bartonella bacilliformis result from invasion of the red blood cells (erythrocytes) by the bacteria in the acute phase of Carrion’s disease 12. Bartonella bacilliformis infects the red blood cells, which are subsequently destroyed in the spleen and liver, leading to severe hemolytic anemia and transient immunosuppression 12. Although not all the infected red blood cells are removed from the circulation, hemolytic anemia involves the destruction of the infected red blood cells by the reticuloendothelial system, with the red blood cells remaining within the circulation for a shorter time than normal, thereby leading to the development of anemia 49. Although increased production of erythrocytes in response to the great destruction of these cells may be up to five times greater than normal, in Oroya fever there is a substantial reduction in the number of erythrocytes with a compensatory increase in plasma, so that the total blood volume is not severely affected 49. On the other hand, a deregulation of the immune system causes a deterioration of cellular immunity leading to immunosuppression, predisposing the patients to opportunistic infections 50, 51. The amount of microorganisms in the blood is higher in patients with severe anemia than in patients with warts 47. In a study by Maguiña et al. 27, the mean percentage of infected red blood cells in this phase of the disease was 61% (range, 2 to 100%), and in 25% of patients, >90% of the erythrocytes were infected at the time of admission.
The symptoms of Oroya fever are indistinguishable from the initial symptoms of other infectious diseases such as malaria, typhoid fever, dengue, tuberculosis, or even viral hepatitis 12. The onset is usually gradual, with malaise, fever, headache, and mild chills, and can include pallor, hepatomegaly, abdominal pain, and other unspecific symptoms 19, 23, 46, 52. The acute phase seems to have a greater effect on children and teenagers up to the age of 15 years 53, 19, 31, 54, 48. Overall, patients in the acute phase are younger than those in the eruptive phase; in a study by Maguiña et al. 27, it was observed that patients in the acute phase have a mean age of 14.6 years while those in the eruptive phase has a mean age of 18.4 years, suggesting the development of acquired immunity following exposure 31. The mortality rate in the acute phase is 40 to 85% in untreated patients; however, in reference centers (where severe cases are treated) with appropriate and timely treatment, this rate can be reduced to values of around 10% 53, 55, 46, 27, 9, 56. Complications or secondary opportunistic infections can dramatically worsen the clinical outcome, and unfortunately, they are quite common 19, 23, 46, 56, 57. There are several reports on noninfectious hematological, cardiovascular, and neurological complications 19, 23, 52. In regard to opportunistic infections, the most common pathogens involved are Salmonella spp., which are responsible for 90% of the deaths in Oroya fever 58. Moreover, mortality is increased during outbreaks, mainly in new transmission areas because health personnel are unaware of the disease and laboratory staff members are not trained to diagnose the disease 53. For example, in the late 1990s in La Convencion, a district of the Cusco department, acute cases of Carrion’s disease were systematically reported as viral hepatitis, with mortality rates of 39% in some hospitals 17. As indicated above, the risk of mortality is high in pregnant women during acute bartonellosis, with the possible presentation of severe complications, including fetal death 22, 46, 9.
Peruvian Warts
The chronic phase of Carrion’s disease called Peruvian warts or Verruga peruana, the skin phase of Carrion disease, is characterized by the development of dermal eruptions (cutaneous nodules) and red-to-purple vascular lesions. Peruvian warts or Verruga peruana usually occurs weeks to months after the onset of the systemic phase of Carrion disease (Oroya fever) and can persist from 1 month to 1 year 58, 46. Nonetheless, the chronic phase may occur in the absence of previous reported acute illness 59. Lesions vary in size and number, mainly affecting the arms and legs, although other body areas can also be affected 59. The lesions are polymorphic and most commonly appear on the arms and legs. They are typically painless and prone to ulceration and bleeding. The microorganisms are observed within the warts, both intracellularly and within the extracellular matrix 59.
3 types of Carrion’s disease skin lesions are classified as follows 59, 9:
- Miliary lesions, i.e., small (diameter <3 mm), often numerous, reddish papules situated at the papillary and medial dermis, may be itchy;
- Mular (eruptive-phase) lesions, i.e., erythematous round nodules (diameter >5 mm) which tend to extend deeper into the hypodermis with the possible involvement of subcutaneous tissue and muscle. They are often eroded and bleed easily.
- Subdermal or nodular lesions, are diffuse subcutaneous nodules showing no changes in the overlying skin, larger and more prominent than the miliary and mular lesions 60, 60.
The eruptions are most often miliary 59, although different types of warts may commonly be found in the same patient 53. Miliary lesions are normally painless, while the mular lesions may be painful, and two-thirds of patients complain of bleeding warts.
The eruptive phase is a more common manifestation in inhabitants of regions of endemicity, and the risk of developing Peruvian warts increases with age (49). This phase tends to heal spontaneously, and the mortality rate is insignificant. These eruptions are frequently accompanied by mild systemic manifestations, including fever, malaise, osteoarticular pain, lymphadenopathy, and headache (78, 145). Notwithstanding, in more severe cases, complications, including bleeding, may be observed in 66% and secondary infection in 12% of the patients, occasionally leading to fatal outcomes in the absence of timely blood transfusions (6, 139). In fact, in the period from 2005 to 2016, only 1 death related to the chronic phase of Carrion’s disease was reported (146).
Around 50% of patients with Peruvian warts are bacteremic (35, 147), with bacteremia being significantly correlated with the onset of the lesions as well as low hemoglobin levels. On the other hand, the number and distribution of the lesions and the clinical symptoms are not associated with bacteremia (147).
Although scarcely described, some reports have also indicated the presence of internal granulomas, which may be present in different organs, including the lungs, brain, or spleen (62, 133). By far the most ancient description of the presence of these granulomas was in a Tiahuanaco mummy, being suggestive of Carrion’s disease (2). Although the relationship of these lesions with Bartonella bacilliformis has not been definitively established, confirmation of the extension and the clinical parameters of the disease should be described and their true clinical relevance evaluated.
In a recent study on a patient with Peruvian warts, the presence of a concomitant infection by B. ancashensis (detected by molecular tools) and Bartonella bacilliformis (detected by molecular and culture methods) was observed. After treatment with rifampin, a blood culture of B. ancashensis was obtained in one patient (100). This report highlighted the possible coinfection by different strains or closely related microorganisms, as well as the need for in-depth analysis of the real role of B. ancashensis in the development of chronic Carrion’s disease. Moreover, this study lead to the question as to whether the two microorganisms were transferred together from the same vector or whether the patient had two different infectious processes.
Asymptomatic Carriers
It has long been known that these microorganisms can persist in blood for many years after the infection (70). Indeed, one study described the isolation of Bartonella bacilliformis from an individual who had visited Ecuador 3 years previously (62). Moreover, asymptomatic carriers have also been described in areas of endemicity (35, 50, 148, 149). It is believed that these carriers perpetuate the disease and can introduce it into new areas, either within a stable setting with a vector in the area (as described in Colombia in the mid-1930s) or within an unstable setting in which no vector is present. Indeed, Chamberlin and coworkers analyzed the prevalence of asymptomatic Bartonella bacilliformis carriers in an area of endemicity by PCR and found that 0.5% were positive (35). More recently, a study including an area of endemicity (Huancabamba) and an postoutbreak area (Lalaquiz), both in the northern Peruvian department of Piura, showed that approximately half of the volunteers in the area of endemicity and about 40% of the individuals in the postoutbreak area had a positive result by quantitative real time-PCR (qPCR), demonstrating the high number of asymptomatic carriers in these zones (50). It is of concern that the positivity observed was near the qPCR detection limit, showing that the presence of bacteria in the blood may have been very low. This suggests that the real number of Bartonella bacilliformis carriers may be underestimated when less-sensitive techniques are used. Although reinfections cannot be ruled out, the presence of microbiological failures seems evident, as all volunteers from the postoutbreak area were treated with ciprofloxacin during the outbreak (50).
Carrion disease complications
Carrion disease acute phase complications may include 29:
- Immunosuppression. During the immunocompromised period, an individual with systemic Carrion disease may acquire various opportunistic infections. The most common pathogens are the Salmonella species 12.
- Co-infections (simultaneous infection of a host by multiple pathogen species)
- bloodstream Salmonella
- bloodstream Staphylococcus aureus
- Leptospirosis
- Latent infections (infection by an organism that remains inactive in the body)
- Histoplasmosis
- Toxoplasmosis
- Tuberculosis
- Cardiovascular complications
- Generalized accumulation of fluid or edema in the interstitial space (anasarca)
- Cardiovascular shock
- Congestive heart failure
- Myocarditis
- Pericardial effusion
- Pericardial tamponade
- Gastrointestinal complication
- Bleeding in the gastrointestinal tract
- Gyneco-obstetrics complications. If Carrion disease is acquired when a woman is pregnant, there is an increased risk of miscarriage and prematurity 29.
- Fetal death
- Miscarriages
- Pre-term births
- Liver complications
- Acute cholecystitis
- Hepatocellular necrosis
- Neurological complications
- Altered mental status
- Increased intracranial pressure
- Coma
- Convulsion
- Respiratory complication
- Acute pulmonary edema
- Other
- Purpura
- Kidney failure
Carrion disease verrucous phase complications may include 29:
- Bleeding
- Dermal infection
- Necrosis
Carrion disease diagnosis
Carrion disease diagnosis depends on whether the affected individual presents in the systemic acute phase or the chronic skin phase.
Systemic acute phase (Oroya fever)
The diagnosis of Carrion disease in the systemic acute phase cannot be made on clinical features alone due to the non-specific signs and symptoms. A septic screen should be performed, and further investigations should be considered in cases where there are risk factors for Carrion disease.
The diagnosis can often be made with a Giemsa-stained peripheral blood smear. This has a low sensitivity (as has blood culture) and may not identify mild and subclinical cases. Other possible investigations include polymerase chain reaction (PCR), immunoblot, immunoglobulin (Ig)M or IgG indirect immunofluorescence, and indirect hemagglutination 61.
In rural areas of endemicity, the diagnosis of Oroya fever is based mainly on clinical symptoms and Giemsa-stained peripheral blood smears, a low-cost and easy-to-use technique 12. However, this method is requires expertise, and despite the high specificity of 96%, a very low sensitivity (24 to 36%) has been reported, especially in mild cases of disease and in the subclinical and chronic phases of illness 25, 15, 62. Moreover, the unspecific initial symptoms of Carrion’s disease should be taken into account, since they are common to several pathologies present in these areas, such as different arboviral diseases, malaria, or tuberculosis, thereby making diagnosis based only on clinical symptoms difficult 55. Outbreaks of Carrion’s disease have been reported using microscopy tools and clinical diagnostic techniques although analysis by molecular tools revealed another etiological cause 63.
Chronic skin phase (Peruvian warts)
The chronic skin phase of Carrion disease has characteristic skin lesions and clinical diagnosis is made by the presence of cutaneous angiomatous skin lesions. Histopathological diagnosis of a skin biopsy is possible, albeit difficult, with staining of sections with Warthin-Starry silver or Giemsa stain demonstrating the presence of bacteria in the skin eruptions 26.
The tissue culture of Bartonella bacilliformis from the skin lesions is often unreliable due to both laboratory contamination and slow growth rate (1 to 6 weeks) 61. Moreover, it is cumbersome and time-consuming, and contaminations have been described in 7 to 20% of the cultures 55, 27. Additionally, the sensitivity of tissue culture is extremely low. In one study a considerable portion of Peruvian wart cases yielded negative blood cultures 64, and another study showed that only 13% of patients with Peruvian warts had a positive culture or blood film 27. Moreover, a study in which cultures from persons known to be infected with Bartonella bacilliformis were performed over a 6-month period supported the suggestion that the proportion of positive cultures is much higher in the first months of infection than later 64. Lastly, different researchers have evaluated the use of different insect-based liquid culture media to isolate and grow Bartonella spp., no study on the utility of these media in the isolation and growth of Bartonella bacilliformis has been developed 65, 66, 67.
Serological Techniques
Serological tests are useful diagnostic tools for Carrion’s disease, especially when combined with other techniques such as PCR and blood culture. However, immune diagnostic methods for this disease are relatively underdeveloped 26 and the most-studied approaches, such as indirect fluorescence antibody assay (IFA) or enzyme-linked immunosorbent assay (ELISA), have the disadvantage of limited technical resources in areas of endemicity. In this context, the characterization of the antigens expressed during Bartonella bacilliformis infection, which is essential in the elucidation of Carrion’s disease pathogenesis, may also lead toward the development of rapid diagnostic tools 15, 68. A rapid diagnostic test which does not need experienced personnel or high-technology machinery could be easily introduced in low-income areas after basic training. Moreover, results can be obtained quickly, thereby facilitating early initiation of antibiotic treatment.
Bartonella bacilliformis immunoblot sonication of whole organisms is remarkably sensitive to Bartonella bacilliformis antibodies from sera of patients with chronic disease (94%) and also yields reasonable results in acute disease (70%). However, some cross-reactions with sera with antigenically similar bacteria such as Brucella spp. and Chlamydia psittaci were reported in 34% and 5% of the cases, respectively 62. An intense cross-reactivity between Bartonella bacilliformis and Chlamydia psittaci due to common surface epitopes has also been reported previously 69.
Chamberlin et al. 70 described an indirect fluorescence antibody assay (IFA) with irradiated Bartonella bacilliformis whole-cell antigen preparation cocultivated with Vero cells in which the 81% of acute confirmed cases were positive. Interestingly, 74% of the volunteers having a positive IFA reported bartonellosis within the last year, which decreased to 39% when a more distant or nonbartonellosis episode was reported. Overall, 45% of the volunteers from an area where Carrion’s disease is endemic were seropositive for Bartonella bacilliformis by this technique 70.
Carrion disease differential diagnosis
Carrion disease is often misdiagnosed because the signs and symptoms are similar to other infectious diseases in the endemic areas.
Carrion disease acute systemic phase differential diagnoses may include:
- Typhoid fever
- Malaria
- Yellow fever
- Brucellosis
- Viral hepatitis
- Hemolytic anaemia due to another cause 61
Carrion disease skin phase differential diagnoses may include:
- Cherry angiomas
- Pyogenic granuloma
- Bacillary angiomatosis
- Kaposi sarcoma
- Molluscum contagiosum
- Herpes zoster 61
Carrion disease treatment
The treatment of Carrion’s disease differs depending on which phase of the disease is presented and includes blood transfusions and antibiotic agents 29.
Antibiotics typically used to treat Carrion disease in the systemic phase are:
- Adults: ciprofloxacin and chloramphenicol for 14 days
- Children: amoxicillin plus clavulanic acid for 14 days 12
The treatment of choice for Carrion disease in the cutaneous phase is:
- Azithromycin as a first-line treatment
- Erythromycin, ciprofloxacin, and rifampicin as second-line treatment 12
Oroya fever treatment
Since 2003 and according to the Ministry of Health of Peru recommendations and guidelines, ciprofloxacin is the drug of choice for adults in the acute phase of Carrion’s disease, while in severe cases, ceftriaxone should be added to the treatment 71. However, Bartonella bacilliformis is intrinsically resistant to nalidixic acid 72 and it has been suggested that ciprofloxacin is not adequate for treatment of the acute phase and should be removed from the current guidelines 15, 73. Nonetheless, the issue of the most adequate antimicrobial remains controversial. On one hand, successful treatment has been reported, as in the case of a patient with a massive erythrocyte infection (more than 95%) who received a 10-day course of ciprofloxacin and ceftriaxone with full recovery 74, while on the other hand, therapeutic failure and persistent bacteremia of up to 22.6% have been described in patients who have completed treatment schedules 75.
Prior to the inclusion of ciprofloxacin in the guidelines, some studies reported the use of chloramphenicol with good results 53, 27, 76, 77, 78. Although chloramphenicol had been extensively used since 1956 35, a medical consensus considered chloramphenicol to be the treatment of choice for bartonelosis in acute cases from 1998 to 2003. It was then replaced by ciprofloxacin and relegated to rescue therapy. The reason for the change was the lack of clinical response in some patients 79, 80, 81, which had been sporadically reported early in the 1950s 82. Moreover, similar to the case for chloramphenicol 55, 59, ciprofloxacin provided good coverage against Salmonella infections 83. In the study by Gray and colleagues 10, none of 10 patients treated with chloramphenicol died, compared with 88% mortality among nontreated patients. In another study, 19 patients received chloramphenicol for 5 days and similar results were obtained; the temperature returned to normal within 24 hour, and the erythrocyte count and size were reestablished. Relapse was infrequent, and when it occurred, further administration of chloramphenicol resulted in recovery 84. Moreover, in a retrospective report on 215 patients, clinical cure was obtained with chloramphenicol in 89% of the cases 80. A good response to therapy was also achieved in 23 patients with the use of chloramphenicol and another antibiotic 27.
The acute illness is often complicated by other infections, usually with Salmonella spp., which greatly intensifies the clinical condition of the patient 23, 85. The lack of improvement after 72 hours of treatment may allow suspicion of a coinfection. A treatment scheme based on chloramphenicol has the advantage that it is a low-cost, broad-spectrum antibiotic which also covers potential coinfections 26. However, despite the effectiveness of chloramphenicol in some patients, therapeutic failures and persistent bacteremia, leading to asymptomatic carrier status, have been reported in other patients receiving chloramphenicol 25, 27, 75. In a study by Maguiña et al. 27, 3 out of 42 patients did not respond well to chloramphenicol therapy, and it is notable that these 3 patients had an initial microorganism burden of >80%. Another study reported 50% persistent bacteremia after chloramphenicol treatment in 66 patients; 28.8% presented posterior Peruvian warts, and the remaining presented positive blood cultures or PCR results 75. Moreover, in Europe as well as other locations, the use of chloramphenicol in humans is restricted, and its use in livestock production is strictly forbidden because of its potential to produce side effects in the bone marrow 86.
Regarding Salmonella coinfections and ciprofloxacin, in the last years the percentage of clinical isolates of Salmonella spp. resistant to nalidixic acid has been on the rise worldwide 87, 88, and it is extremely high in Peru 89, 90. This may lead to therapeutic failure during ciprofloxacin treatment of bloodstream Salmonella infections (324), being an established risk for the development of ciprofloxacin resistance 91. Moreover, although has been postulated that the development of ciprofloxacin-resistant Salmonella is difficult because of the severe effects on bacterial fitness, with impaired growth and decreased virulence capacity 92, 93, reports on ciprofloxacin-resistant isolates and the emergence of successful ciprofloxacin-resistant Salmonella clones have been described worldwide in the last years 94, 95.
These findings, together with the relevant presence of extended-spectrum beta-lactamase (ESBL)-carrying Salmonella spp. in the area 90, indicate a scenario in which correct and early diagnosis and analysis of resistance levels of both Bartonella bacilliformis and concomitant opportunistic pathogens are needed.
Peruvian wart treatment
From 1969 to 1975 streptomycin was the drug of choice for the treatment of the chronic phase of Carrion’s disease, and in the mid-1970s rifampin was introduced and became the first-line drug, showing better results than streptomycin 27, 96. In a study of 260 chronic-phase patients receiving rifampin, clinical cure was observed in 93.1% 80. Nevertheless, treatment failure with rifampin for Peruvian wart has also been reported 77, 97, 98 and alternatives have been used in the treatment of chronic-phase patients. A good response was obtained in an eruptive case treated with chloramphenicol 99 and in another case, a 12-year-old child was treated with sultamicillin and deflazacort for 10 days and showed rapid improvement of the overall symptoms and complete remission of skin lesions at 21 days 100. More recently, after the successful use of azithromycin 77, the Ministry of Health of Peru proposed the use of azithromycin for the eruptive phase of the disease 71.
Carrion disease prognosis
The mortality rate in the systemic phase of Carrion disease ranges from 40% to 85% in untreated patients. Mortality can be reduced to 10% if the infection is treated appropriately. Mortality is usually secondary to opportunistic infections or malnutrition 12.
The chronic phase of cutaneous Carrion disease is usually self-limiting and rarely results in complications.
- Acosta O, Solano L, Escobar J, Fernandez M, Solano C, Fujita R. Frequencies of Blood Group Systems MNS, Diego, and Duffy and Clinical Phases of Carrion’s Disease in Amazonas, Peru. Interdiscip Perspect Infect Dis. 2014;2014:576107. doi: 10.1155/2014/576107[↩][↩][↩][↩][↩]
- Amano Y, Rumbea J, Knobloch J, Olson J, Kron M. Bartonellosis in Ecuador: serosurvey and current status of cutaneous verrucous disease. Am J Trop Med Hyg. 1997 Aug;57(2):174-9. doi: 10.4269/ajtmh.1997.57.174[↩][↩][↩][↩]
- Lydy SL, Lascano MS, Garcia-Perez JE, Williams-Newkirk AJ, Grijalva MJ. Seroprevalence and risk factors for infection with Bartonella bacilliformis in Loja province, Ecuador. Emerg Microbes Infect. 2018 Jun 25;7(1):115. doi: 10.1038/s41426-018-0110-5[↩][↩][↩][↩]
- Maguiña C. Bartonelosis o Enfermedad de Carrión: Nuevos aspectos de una vieja enfermedad. Lima, Peru: Editor Importadores; 1998.[↩][↩]
- OGE/INS. Epidemiología de la Bartonelosis en el Perú. Lima, Peru: Módulos Técnicos; 2000. (Serie Documentos Monográficos).[↩][↩][↩][↩][↩]
- Gray GC, Johnson AA, Thornton SA, Smith WA, Knobloch J, Kelley PW, Obregon Escudero L, Arones Huayda M, Wignall FS. An epidemic of Oroya fever in the Peruvian Andes. Am J Trop Med Hyg. 1990 Mar;42(3):215-21. https://doi.org/10.4269/ajtmh.1990.42.215[↩][↩]
- Solano L, Solano V. La Enfermedad de Carrión y la Biología de Bartonella bacilliformis . Revista Peruana de Medicina Tropical UNMSM. 1991;5:13–18.[↩][↩]
- Maguina C, Garcia PJ, Gotuzzo E, Cordero L, Spach DH. Bartonellosis (Carrionʼs disease) in the modern era. Clinical Infect Dis. 2001;33:772–9.[↩]
- Ihler GM. 1996. Bartonella bacilllformis: dangerous pathogen slowly emerging from deep background. FEMS Microbiol Lett 144:1–11. doi: 10.1111/j.1574-6968.1996.tb08501.x[↩][↩][↩][↩]
- Gray GC, Johnson AA, Thornton SA, Smith WA, Knobloch J, Kelley PW, Obregon Escudero L, Arones Huayda M, Wignall FS. 1990. An epidemic of Oroya fever in the Peruvian Andes. Am J Trop Med Hyg 42:215–221. doi: 10.4269/ajtmh.1990.42.215[↩][↩][↩]
- Gomes C, Pons MJ, Del Valle Mendoza J, Ruiz J. Carrion’s disease: an eradicable illness? Infect Dis Poverty. 2016 Dec 1;5(1):105. doi: 10.1186/s40249-016-0197-7[↩]
- Gomes C, Ruiz J. Carrion’s Disease: the Sound of Silence. Clin Microbiol Rev. 2017 Nov 29;31(1):e00056-17. doi: 10.1128/CMR.00056-17[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Kosek M, Lavarello R, Gilman RH, Delgado J, Maguiña C, Verástegui M, Lescano AG, Mallqui V, Kosek JC, Recavarren S, Cabrera L. Natural history of infection with Bartonella bacilliformis in a nonendemic population. J Infect Dis. 2000 Sep;182(3):865-72. doi: 10.1086/315797[↩][↩]
- Huarcaya E, Maguiña C, Torres R, Rupay J, Fuentes L. Bartonelosis (Carrion’s Disease) in the pediatric population of Peru: an overview and update. Braz J Infect Dis. 2004 Oct;8(5):331-9. doi: 10.1590/s1413-86702004000500001[↩]
- Sanchez Clemente N, Ugarte-Gil CA, Solórzano N, Maguiña C, Pachas P, Blazes D, Bailey R, Mabey D, Moore D. 2012. Bartonella bacilliformis: a systematic review of the literature to guide the research agenda for elimination. PLoS Negl Trop Dis 6:e1819. doi: 10.1371/journal.pntd.0001819[↩][↩][↩][↩]
- Solano L, Marocho L, Caceres A, et al. Estudio de reservorios de Bartonella bacilliformis . Revista Peruana de Medicina Tropical UNMSM. 2004;1:71–74.[↩]
- Núñez Sánchez G, Canales Santander JC, Cjuno Huanca R, Grajeda Ancca P, Gonzales Campana C. 1999. Brote de bartonelosis en la provincia de La Convención—Cusco, 1998. Rev Situa 7:20–24.[↩][↩][↩]
- Sanchez Clemente N, Ugarte-Gil C, Solorzano N, Maguiña C, Moore D. 2016. An outbreak of Bartonella bacilliformis in an endemic Andean community. PLoS One 11:e0150525. doi: 10.1371/journal.pone.0150525[↩][↩]
- Cruz-Vilchez J, Vargas-Cruz M. 2003. Bartonelosis aguda complicada. Presentación de 44 casos. Huancabamba, Piura. Rev Soc Per Med Inter 16:5–9.[↩][↩][↩][↩][↩]
- González C, Maguiña C, Heras F, Conde-Salazar L. 2007. Bartonelosis (fiebre de la Oroya o verruga Peruana) ¿Enfermedad ocupacional? Med Segur Trab 53:35–41.[↩]
- Contreras-Gutiérrez MA, Vélez ID, Porter C, Uribe SI. Lista actualizada de flebotomíneos (Diptera: Psychodidae: Phlebotominae) de la región cafetera colombiana [An updated checklist of Phlebotomine sand flies (Diptera: Psychodidae: Phlebotominae) from the Colombian Andean coffee-growing region]. Biomedica. 2014 Jul-Sep;34(3):483-98. Spanish. doi: 10.1590/S0120-41572014000300017[↩]
- López Guimaraes D, Giraldo Villafane M, Maguiña Vargas C. 2006. Complicaciones ginecoobstétricas en la bartonelosis aguda: 50 casos observados en Caraz, Ancash. Acta Med Per 23:148–151.[↩][↩]
- Breña-Chavez JP, Maguiña Vargas CP, Hernández Díaz HR, Castillo Díaz ME, Pozo Tovar WE. 2006. Bartonelosis aguda en niños: estudio de 32 casos en el Instituto Especializado de Salud del Niño y el Hospital Nacional Cayetano Heredia (período 1993-2003). Rev Med Hered 17:122–131.[↩][↩][↩][↩][↩]
- Tarazona A, Maguiña C, López de Guimaraes D, Montoya M, Pachas P. 2006. Terapia antibiótica para el manejo de la bartonelosis o enfermedad de Carrión en el Perú. Rev Peru Med Exp Salud Publica 23:188–200.[↩]
- Ellis B, Rotz LD, Leake JA, Samalvides F, Bernable J, Ventura G, Padilla C, Villaseca P, Beati L, Regnery R, Childs JE, Olson JG, Carrillo CP. 1999. An outbreak of acute bartonellosis (Oroya fever) in the Urubamba region of Peru, 1998. Am J Trop Med Hyg 61:344–349. doi: 10.4269/ajtmh.1999.61.344[↩][↩][↩][↩]
- Minnick MF, Anderson BE, Lima A, Battisti JM, Lawyer PG, Birtles RJ. 2014. Oroya fever and verruga peruana: bartonelloses unique to South America. PLoS Negl Trop Dis 8:e2919. doi: 10.1371/journal.pntd.0002919[↩][↩][↩][↩][↩]
- Maguiña C, Garcia PJ, Gotuzzo E, Cordero L, Spach DH. 2001. Bartonellosis (Carrión’s disease) in the modern era. Clin Infect Dis 33:772–779. doi: 10.1086/322614[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- del Valle Mendoza J, Silva W, Tinco C, Pons MJ, del Valle LJ, Champin Michelena D, Bazán Mayra J, Zavaleta Gavidea V, Vargas M, Ruiz J. 2014. Diagnosis of Carrion’s disease by direct blood PCR in thin blood smear negative samples. PLoS One 9:e92283. doi: 10.1371/journal.pone.0092283[↩]
- Pons MJ, Gomes C, Del Valle-Mendoza J, Ruiz J. Carrion’s Disease: More Than a Sand Fly-Vectored Illness. PLoS Pathog. 2016 Oct 13;12(10):e1005863. doi: 10.1371/journal.ppat.1005863[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Garcia-Quintanilla, M., Dichter, A.A., Guerra, H. et al. Carrion’s disease: more than a neglected disease. Parasites Vectors 12, 141 (2019). https://doi.org/10.1186/s13071-019-3390-2[↩][↩]
- Chamberlin J, Laughlin LW, Romero S, Solórzano N, Gordon S, Andre RG, Pachas P, Friedman H, Ponce C, Watts D. 2002. Epidemiology of endemic Bartonella bacilliformis: a prospective cohort study in a Peruvian mountain valley community. J Infect Dis 186:983–990. doi: 10.1086/344054[↩][↩][↩][↩]
- Masuoka P, Andre R, Montgomery BC, Rejmankova E, Roberts D, Carbajal F, Chamberlin J, Laughlin L, Ponce Garcia C, Watts D, Elinan E. 1998. Remote sensing and GIS investigations of bartonellosis in Peru. Proc Int Geosci Remote Sens Symp 2:816–818.[↩]
- Krumdieck CF. 1949. La enfermedad de Carrión o verruga peruana en el niño. An Fac Med 32:227–306. doi: 10.15381/anales.v32i4.9584[↩]
- Tarazona A, Solórzano N, Chiroque J, Rojas Y, Peralta J, Sacramento H, Broncazo F, Pachas P. 2003. Transmisión vertical de bartonelosis humana, reporte de un caso, abstr 23, p 28. Abstr 8th Congr Peruano Med Enfermedades Infecciosas Tropicales, Lima, Peru.[↩]
- Maguiña C. 1998. Bartonellosis o enfermedad de Carrión. Nuevos aspectos de una vieja enfermedad. A.F.A. Editores Importadores, Lima, Peru: https://sisbib.unmsm.edu.pe/bibvirtual/libros/medicina/bartonellosis/ficha.htm[↩][↩]
- Pons MJ, Lovato P, Silva J, Urteaga N, del Valle Mendoza J, Ruiz J. 2016. Carrion’s disease after blood transfusion. Blood Transfus 14:527–530. doi: 10.2450/2015.0036-15[↩]
- Lydy SL, Eremeeva ME, Asnis D, Paddock CD, Nicholson WL, Silverman DJ, Dasch GA. 2008. Isolation and characterization of Bartonella bacilliformis from an expatriate Ecuadorian. J Clin Microbiol 46:627–637. doi: 10.1128/JCM.01207-07[↩]
- Walker TS, Winkler HH. Bartonella bacilliformis: colonial types and erythrocyte adherence. Infect Immun. 1981 Jan;31(1):480-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC351807/pdf/iai00165-0500.pdf[↩]
- Pons MJ, Urteaga N, Alva-Urcia C, Lovato P, Silva Y, Ruiz J, del Valle J. 2016. Infectious agents, Leptospira spp. and Bartonella spp, in blood donors from Cajamarca, Peru. Blood Transfus 14:504–508. doi: 10.2450/2015.0081-15[↩]
- Ministerio de Salud. 1998. Doctrina, normas y procedimientos del programa nacional de hemoterapia y bancos de sangre. Ministerio de Salud, Lima, Peru.[↩]
- Ministerio de Salud Sistema de Gestión de la Calidad del Pronahebas. 2004. Manual de calidad. Ministerio de Salud, Lima, Peru.[↩]
- Instituto Nacional de Estadísticas e Informática. 2013. Perú: Estadísticas de la emigración internacional de peruanos e inmigración de extranjeros, 1990–2012. Organización Internacional para las Migraciones, Lima, Peru.[↩]
- [↩]
- Gonzales Olaechea M. 1890. Un caso de verruga infecciosa visceral. Cron Med 7:324–326.[↩]
- Howe C. 1943. Immune serum therapy for Oroya fever. Arch Int Med 72:429–438. doi: 10.1001/archinte.1943.00210100002001[↩]
- Maguiña C, Gotuzzo E. 2000. Bartonellosis new and old. Infect Dis Clin North Am 14:1–22. doi: 10.1016/S0891-5520(05)70215-4[↩][↩][↩][↩][↩][↩]
- Noguchi H. 1928. Etiology of Oroya fever. X. Comparative studies of different strains of Bartonella bacilliformis, with special reference to the relationship between the clinical types of Carrión’s disease and the virulence of the infecting organism. J Exp Med 31:219–234. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2131357/pdf/219.pdf[↩][↩]
- Kosek M, Lavarello R, Gilman RH, Delgado J, Maguiña C, Verástegui M, Lescano AG, Mallqui V, Kosek JC, Recavarren S, Cabrera L. 2000. Natural history of infection with Bartonella bacilliformis in a nonendemic population. J Infect Dis 182:865–872. doi: 10.1086/315797[↩][↩]
- Reynafarje C, Ramos J. 1961. The hemolytic anemia of human bartonellosis. Blood 17:562–578.[↩][↩]
- Weiss P. 1926. Hacia una concepción de la Verruga Peruana. An Fac Med 12:279–299. doi: 10.15381/anales.v12i0.10136[↩]
- Ticona E, Huaroto L, Garcia Y, Vargas L, Madariaga MG. 2010. The pathophysiology of the acute phase of human bartonellosis resembles AIDS. Med Hypotheses 74:45–49. doi: 10.1016/j.mehy.2009.06.054[↩]
- Maguiña C, Ugarte-Gil C, Breña P, Ordaya E, Ventosilla P, Huarcaya E, Henriquez C. 2008. Actualización de la enfermedad de Carrión. Rev Med Hered 19:36–41.[↩][↩]
- Pachas P. 2001. Enfermedad de Carrión (bartonelosis) en el Perú. Ministerio de la Salud, OGE, INS, Lima, Peru.[↩][↩][↩][↩][↩]
- Huarcaya E, Maguiña C, Torres R, Rupay J, Fuentes L. 2004. Bartonelosis (Carrion’s disease) in the pediatric population of Peru: an overview and update. Braz J Infect Dis 8:331–339. doi: 10.1590/S1413-86702004000500001[↩]
- Pachas P. 2000. Epidemiología de la bartonelosis en el Peru. Ministerio de Salud, Lima, Peru.[↩][↩][↩][↩]
- Pons MJ, Gomes C, del Valle-Mendoza J, Ruiz J. 2016. Carrion’s disease: more than a sand fly-vectored illness. PLoS Pathog 12:e1005863. doi: 10.1371/journal.ppat.1005863[↩][↩]
- Huerta A, Salas M, Yarinsueca J, Maguiña C. Enfermedad de Carrión grave complicada con leptospirosis aguda: reporte de un caso [Carrión’s disease complicated with severe acute leptospirosis: a case report]. Rev Peru Med Exp Salud Publica. 2014 Apr;31(2):380-4. Spanish.[↩]
- Schultz MG. 1968. A history of bartonellosis (Carrión’s disease). Am J Trop Med Hyg 17:503–515. doi: 10.4269/ajtmh.1968.17.503[↩][↩]
- Maguiña C, Guerra H, Ventosilla P. 2009. Bartonellosis. Clin Dermatol 27:271–280. doi: 10.1016/j.clindermatol.2008.10.006[↩][↩][↩][↩][↩][↩]
- Maguiña C, Guerra H, Ventosilla P. Bartonellosis. Clin Dermatol. 2009 May-Jun;27(3):271-80. doi: 10.1016/j.clindermatol.2008.10.006[↩][↩]
- Dehio C, Maguina C, Walker DH. Bartonelloses. In: Guerrant R, Walker D, Weller P (eds). Tropical infectious diseases: principles, pathogens and practice, 3rd edn. Philadelphia: Elsevier Saunders, 2011: 265–70.[↩][↩][↩][↩]
- Mallqui V, Speelmon EC, Verástegui M, Maguiña-Vargas C, Pinell-Salles P, Lavarello R, Delgado J, Kosek M, Romero S, Arana Y, Gilman RH. Sonicated diagnostic immunoblot for bartonellosis. Clin Diagn Lab Immunol. 2000 Jan;7(1):1-5. doi: 10.1128/CDLI.7.1.1-5.2000[↩][↩]
- Cornejo A, Gomes C, Suarez L, Martinez-Puchol S, Bustamante P, Pons MJ, Ruiz J, del Valle J. 2015. An unidentified cluster of infection in the Peruvian Amazon Department. J Infect Dev Countr 9:524–529. doi: 10.3855/jidc.6235[↩]
- Herrer A. 1953. Carrión’s disease. II. Presence of Bartonella bacilliformis in the peripheral blood of patients with the benign form. Am J Trop Med Hyg 2:645–649.[↩][↩]
- Maggi RG, Duncan AW, Breitschwerdt EB. 2005. Novel chemically modified liquid medium that will support the growth of seven Bartonella species. J Clin Microbiol 43:2651–2655. doi: 10.1128/JCM.43.6.2651-2655.2005[↩]
- Lynch T, Iverson J, Kosoy M. 2011. Combining culture techniques for Bartonella: the best of both worlds. J Clin Microbiol 49:1363–1368. doi: 10.1128/JCM.02403-10[↩]
- Riess T, Dietrich F, Schmidt KV, Kaiser PO, Schwarz H, Schäfer A, Kempf VA. 2008. Analysis of a novel insect cell culture medium-based growth medium for Bartonella species. Appl Environ Microbiol 74:5224–5227. doi: 10.1128/AEM.00621-08[↩]
- Padmalayam I, Kelly T, Baumstark B, Massung R. 2000. Molecular cloning, sequencing, expression, and characterization of an immunogenic 43-kilodalton lipoprotein of Bartonella bacilliformis that has homology to NlpD/LppB. Infect Immun 68:4972–4979. doi: 10.1128/IAI.68.9.4972-4979.2000[↩]
- Knobloch J, Bialek R, Müller G, Asmus P. 1988. Common surface epitopes of Bartonella bacilliformis and Chlamydia psittaci. Am J Trop Med Hyg 39:427–433. doi: 10.4269/ajtmh.1988.39.427[↩]
- Chamberlin J, Laughlin L, Gordon S, Romero S, Solórzano N, Regnery RL. Serodiagnosis of Bartonella bacilliformis infection by indirect fluorescence antibody assay: test development and application to a population in an area of bartonellosis endemicity. J Clin Microbiol. 2000 Nov;38(11):4269-71. doi: 10.1128/JCM.38.11.4269-4271.2000[↩][↩]
- Ministerio de Salud. 2006. Atención de la bartonelosis o enfermedad de Carrión en el Perú. Norma Técnica no. 048-MINSA/GPSP-V.01. Instituto Nacional de Salud, Lima, Peru.[↩][↩]
- del Valle LJ, Flores L, Vargas M, García-de la-Guarda R, Quispe RL, Ibañez ZB, Alvarado D, Ramírez P, Ruiz J. 2010. Bartonella bacilliformis, endemic pathogen of the Andean region, is intrinsically resistant to quinolones. Int J Infect Dis 14:506–510. doi: 10.1016/j.ijid.2009.07.025[↩]
- Angelakis E, Raoult D. 2014. Pathogenicity and treatment of Bartonella infections. Int J Antimicrob Agents 44:16–25. doi: 10.1016/j.ijantimicag.2014.04.006[↩]
- Seas C, Villaverde H, Maguiña C. 2012. A 60-year-old man from the highlands of Peru with fever and hemolysis. Am J Trop Med Hyg 86:381. doi: 10.4269/ajtmh.2012.11-0540[↩]
- Pachas P, Rojas Y, Solorzano N, Chiroque J, Chancafe JA, Canal E, Suarez-Ognio L, Maguiña M, Tarazona A, Salazar J, Mezarina J, Jones F. 2006. Persistence of bacteremia by Bartonella bacilliformis post treatment with cloranfenicol, Ancash, Peru, abstr 791, p 229. Abstr ASTMH Annu Meet, Atlanta, GA.[↩][↩][↩]
- Zegarra Araujo N. 1957. Tratamiento actual de la enfermedad de Carrión. An Fac Med 40:32–35. doi: 10.15381/anales.v40i1.10720[↩]
- Rolain JM, Brouqui P, Koehler JE, Maguina C, Dolan MJ, Raoult D. 2004. Recommendations for treatment of human infections caused by Bartonella species. Antimicrob Agents Chemother 48:1921–1933. doi: 10.1128/AAC.48.6.1921-1933.2004[↩][↩][↩]
- Payne EH, Urteaga O. 1951. Carrion’s disease treated with chloromycetin. Antibiot Chemother 1:92–99.[↩]
- Ministerio de Salud. 1998. Doctrina, normas y procedimentos para el control de la bartonelosis o enfermedad de Carrión en el Perú. Ministerio de Salud, Lima, Peru.[↩]
- Arroyo A. 2008. Esquemas de tratamiento para la enfermedad de Carrión no complicada en la ciudad de Caraz, Perú. An Fac Med 69:7–11. doi: 10.15381/anales.v69i1.1171[↩][↩][↩]
- Mendoza-Mujica G, Flores-León D. 2015. Resistencia antimicrobiana de cepas de Bartonella bacilliformis procedentes de regiones endémicas de la enfermedad de Carrión en el Perú. Rev Peru Med Exp Salud Publica 32:659–666. doi: 10.17843/rpmesp.2015.324.1755[↩]
- Cuadra M. 1957. Tratamiento con cloramfenicol de casos de Bartonellosis aguda (enfermedad de Carrión) en periodo de inicio. An Fac Med 3:747–772. Spanish.[↩]
- Hohmann EL. 2001. Nontyphoidal salmonellosis. Clin Infect Dis 32:263–269. doi: 10.1086/318457[↩]
- Urteaga O, Payne EH. 1955. Treatment of the acute febrile phase of Carrión’s disease with chloramphenicol. Am J Trop Med Hyg 4:507–511. doi: 10.4269/ajtmh.1955.4.507[↩]
- Alzamora y Castro VV. 1940. Enfermedad de Carrión—ensayo de etiopatogenia. An Fac Med 23:9–55. doi: 10.15381/anales.v23i1.9750[↩]
- Hanekamp JC, Bast A. 2015. Antibiotic exposure and health risks: chloramphenicol. Environ Toxicol Pharmacol 39:213–220. doi: 10.1016/j.etap.2014.11.016[↩]
- Cabrera R, Ruiz J, Marco F, Oliveira I, Arroyo M, Aladueña A, Usera MA, Jiménez de Anta MT, Gascón J, Vila J. 2004. Mechanism of resistance to several antimicrobial agents in Salmonella clinical isolates causing traveler’s diarrhea. Antimicrob Agents Chemother 48:3934–3939. doi: 10.1128/AAC.48.10.3934-3939.2004[↩]
- Mandomando I, Bassat Q, Sigaúque B, Massora S, Quintó L, Ácacio S, Nhampossa T, Vubil D, Garrine M, Macete E, Aide P, Sacoor C, Herrera-León S, Ruiz J, Tennant SM, Menéndez C, Alonso PL. 2015. Invasive Salmonella infections among children from rural Mozambique, 2001–2014. Clin Infect Dis 61(Suppl 4):S339–S345. doi: 10.1093/cid/civ712[↩]
- García C, Lejon V, Horna G, Astocondor L, Vanhoof R, Bertrand S, Jacobs J. 2014. Intermediate susceptibility to ciprofloxacin among Salmonella enterica serovar Typhi isolates in Lima, Peru. J Clin Microbiol 52:968–970. doi: 10.1128/JCM.02663-13[↩]
- Gonzales Escalante E. 2015. Incremento de aislamientos de Salmonella spp. productora de β-lactamasas de espectro extendido en pacientes pediátricos del Instituto Nacional de Salud del Niño. Rev Peru Med Exp Salud Publica 32:605–607. doi: 10.17843/rpmesp.2015.323.1701[↩][↩]
- Ruiz J, Gómez J, Navia MM, Ribera A, Sierra JM, Marco F, Mensa J, Vila J. 2002. High prevalence of nalidixic acid resistant, ciprofloxacin susceptible phenotype among clinical isolates of Escherichia coli and other Enterobacteriaceae. Diagn Microbiol Infect Dis 42:257–261. doi: 10.1016/S0732-8893(01)00357-1[↩]
- Ballesté-Delpierre C, Fàbrega A, Ferrer-Navarro M, Mathur R, Ghosh S, Vila J. 2016. Attenuation of in vitro host-pathogen interactions in quinolone-resistant Salmonella Typhi mutants. J Antimicrob Chemother 71:111–122. doi: 10.1093/jac/dkv299[↩]
- Fàbrega A, Soto SM, Ballesté-Delpierre C, Fernández-Orth D, Jiménez de Anta MT, Vila J. 2014. Impact of quinolone-resistance acquisition on biofilm production and fitness in Salmonella enterica. J Antimicrob Chemother 69:1815–1824. doi: 10.1093/jac/dku078[↩]
- Le Hello S, Bekhit A, Granier SA, Barua H, Beutlich J, Zając M, Münch S, Sintchenko V, Bouchrif B, Fashae K, Pinsard JL, Sontag L, Fabre L, Garnier M, Guibert V, Howard P, Hendriksen RS, Christensen JP, Biswas PK, Cloeckaert A, Rabsch W, Wasyl D, Doublet B, Weill FX. 2013. The global establishment of a highly-fluoroquinolone resistant Salmonella enterica serotype Kentucky ST198 strain. Front Microbiol 4:395. doi: 10.3389/fmicb.2013.00395[↩]
- Liang Z, Ke B, Deng X, Liang J, Ran L, Lu L, He D, Huang Q, Ke C, Li Z, Yu H, Klena JD, Wu S. 2015. Serotypes, seasonal trends, and antibiotic resistance of non-typhoidal Salmonella from human patients in Guangdong Province, China, 2009-2012. BMC Infect Dis 15:53. doi: 10.1186/s12879-015-0784-4[↩]
- Maguina C, Gotuzzo E. Treatment of Bartonellosis. J Travel Med. 1995 Dec 1;2(4):278. doi: 10.1111/j.1708-8305.1995.tb00681.x[↩]
- Biswas S, Raoult D, Rolain JM. 2007. Molecular mechanisms of resistance to antibiotics in Bartonella bacilliformis. J Antimicrob Chemother 59:1065–1070. doi: 10.1093/jac/dkm105[↩]
- Biswas S, Rolain JM. 2010. Bartonella infection: treatment and drug resistance. Future Microbiol 5:1719–1731. doi: 10.2217/fmb.10.133[↩]
- Matteelli A, Castelli F, Spinetti A, Bonetti F, Graifenberghi S, Carosi G. 1994. Short report: verruga peruana in an Italian traveller from Peru. Am J Trop Med Hyg 50:143–144. doi: 10.4269/ajtmh.1994.50.143[↩]
- Gutierrez Z, Luna S. 1998. Verruga Peruana tratada con sultamicilina y deflazacort. Dermatol Peru 8:43–46.[↩]