Contents
- What are catecholamines
- Catecholamines function
- Catecholamine synthesis
- Catecholamine release
- Catecholamine metabolism
- Catecholamine normal levels
- Catecholamines test
- 24 hour urine catecholamine
- Plasma free metanephrines
- When is plasma free metanephrines test ordered?
- What does high metanephrine and normetanephrine blood levels mean?
- Does the amount of plasma free metanephrines detected correspond to the size of the tumor?
- Is it really necessary to follow the dietary restrictions?
- Is it really necessary to lie down before testing?
- 24 hour urine metanephrines
- When is 24 hour urine metanephrines test ordered?
- What does high metanephrine and normetanephrine urine levels mean?
- Is it really necessary to collect urine for 24 hours?
- Does the amount of urine metanephrines detected correspond to the size of the tumor?
- Is it really necessary to follow the dietary restrictions?
- Can I have more than one pheochromocytoma at once?
What are catecholamines
Catecholamines are a group of similar hormones released into the bloodstream in response to physical or emotional stress. The primary catecholamines are dopamine, epinephrine (adrenaline), and norepinephrine (noradrenaline). Catecholamines are produced in the adrenal medulla, the interior portion of the adrenal glands, and released into the blood. The adrenal glands are small, triangular organs located on top of each kidney. Catecholamines are also produced by cells of the sympathetic nervous system. With the majority of dopamine production occurs in the brain, and the dopaminergic pathways it follows has vast implications on cortical neurophysiology.
Neuroendocrine chromaffin cells, responsible for the biosynthesis of catecholamines, are located throughout the brain and in the adrenal glands. The highest density of chromaffin cells is located within the adrenal medulla, the most functionally significant area of catecholamine production. The kidneys are responsible for excreting the byproducts of catecholamine degradation. Adrenergic receptors activated by catecholamines are located in multisystem smooth muscle and adipose tissue.
Catecholamines act both as neurotransmitters and hormones vital to the maintenance of homeostasis through the autonomic nervous system.
Catecholamines help transmit nerve impulses in the brain, increase glucose and fatty acid release for energy, dilate bronchioles, and dilate the pupils. Norepinephrine (noradrenaline) also constricts blood vessels, causing increased blood pressure, and epinephrine (adrenaline) increases heart rate and metabolism.
After completing their actions, catecholamines are metabolized to inactive compounds. Dopamine becomes homovanillic acid (HVA), norepinephrine (noradrenaline) breaks down into normetanephrine and vanillylmandelic acid (VMA), and epinephrine (adrenaline) becomes metanephrine and vanillylmandelic acid (VMA). Both catecholamines hormones and their metabolites are eliminated from the body in the urine.
Normally, catecholamines and their metabolites are present in the body in small, fluctuating amounts that only increase appreciably during and shortly after a stressful situation. However, rare tumors called pheochromocytomas and paragangliomas can produce large amounts of catecholamine hormones, resulting in increased concentrations in both the blood and urine. This can cause persistent or sudden bursts of hypertension, which may lead to severe headaches. Other symptoms include heart palpitations, sweating, nausea, anxiety, and tingling in the hands and feet.
Pheochromocytomas and paragangliomas are rare. While a few are cancerous, most are benign and do not spread beyond their original location. Left untreated, however, pheochromocytomas and paragangliomas tumors may continue to grow and symptoms may worsen. Over time, the hypertension caused by the excess hormones may lead to kidney damage, heart disease, and raise the risk for stroke or heart attack.
The Endocrine Society recommends that a test for plasma free metanephrine or urine metanephrine be used to help detect the presence of pheochromocytomas and paragangliomas (catecholamine-secreting tumors). Urine and/or blood tests for catecholamines may be used to help confirm or rule out the presence of these tumors. However, blood tests are not as reliable as urine testing because the stress from having blood drawn can elevate catecholamines.
It is important to diagnose and treat these tumors because they cause a potentially curable form of hypertension. In most cases, the tumors can be surgically removed and/or treated to significantly reduce the amount of catecholamines being produced and to reduce or eliminate their associated symptoms and complications.
Catecholamines function
All 3 catecholamines (dopamine, epinephrine, and norepinephrine) are important neurotransmitters in the central nervous system and also play a crucial role in the autonomic regulation of many homeostatic functions, namely, vascular tone, intestinal and bronchial smooth muscle tone, cardiac rate and contractility, and glucose metabolism. Their actions are mediated via alpha and beta adrenergic receptors and dopamine receptors, all existing in several subforms. The 3 catecholamines (dopamine, epinephrine, and norepinephrine) overlap, but also differ in their receptor activation profile and consequent biological actions.
Catecholamines cause general physiological changes that prepare the body for physical activity (fight-or-flight response). Some typical effects are increases in heart rate, blood pressure, blood glucose levels, and a general reaction of the sympathetic nervous system.
Norepinephrine and dopamine, act as neuromodulators in the central nervous system and as hormones in the blood circulation. The catecholamine norepinephrine is a neuromodulator of the peripheral sympathetic nervous system but is also present in the blood (mostly through “spillover” from the synapses of the sympathetic system).
High catecholamine levels in blood are associated with stress, which can be induced from psychological reactions or environmental stressors such as elevated sound levels, intense light, or low blood sugar levels.
Extremely high levels of catecholamines (also known as catecholamine toxicity) can occur in central nervous system trauma due to stimulation and/or damage of nuclei in the brainstem, in particular those nuclei affecting the sympathetic nervous system. In emergency medicine, this occurrence is widely known as catecholamine dump.
Extremely high levels of catecholamine can also be caused by neuroendocrine tumors in the adrenal medulla, a treatable condition known as pheochromocytoma.
Is serotonin a catecholamine?
No. Serotonin also known as 5-hydroxytryptamine or 5-HT, is a monoamine neurotransmitter that is synthesized from the essential amino acid L-Tryptophan that nerve cells in the brain use to communicate. Serotonin actual biological function is complex and multifaceted, modulating cognition, reward, learning, memory, and numerous physiological processes 1.. In the pineal gland, serotonin is converted enzymatically to melatonin.
Catecholamine synthesis
Catecholamines are produced mainly by the chromaffin cells of the adrenal medulla and the postganglionic fibers of the sympathetic nervous system. The systemically circulating fraction of the catecholamines is derived almost exclusively from the adrenal medulla, with small contributions from sympathetic ganglia.
Dopamine, which acts as a neurotransmitter in the central nervous system, is largely produced in neuronal cell bodies in two areas of the brainstem: the ventral tegmental area and the substantia nigra, the latter of which contains neuromelanin-pigmented neurons. The similarly neuromelanin-pigmented cell bodies of the locus ceruleus produce norepinephrine. Epinephrine is produced in small groups of neurons in the human brain which express its synthesizing enzyme, phenylethanolamine N-methyltransferase 2; these neurons project from a nucleus that is adjacent (ventrolateral) to the area postrema and from a nucleus in the dorsal region of the solitary tract 2.
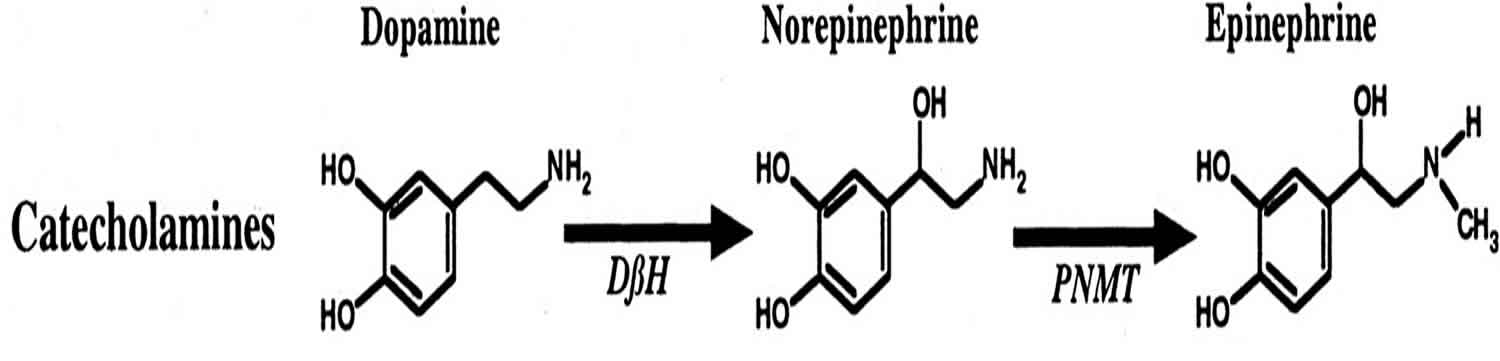
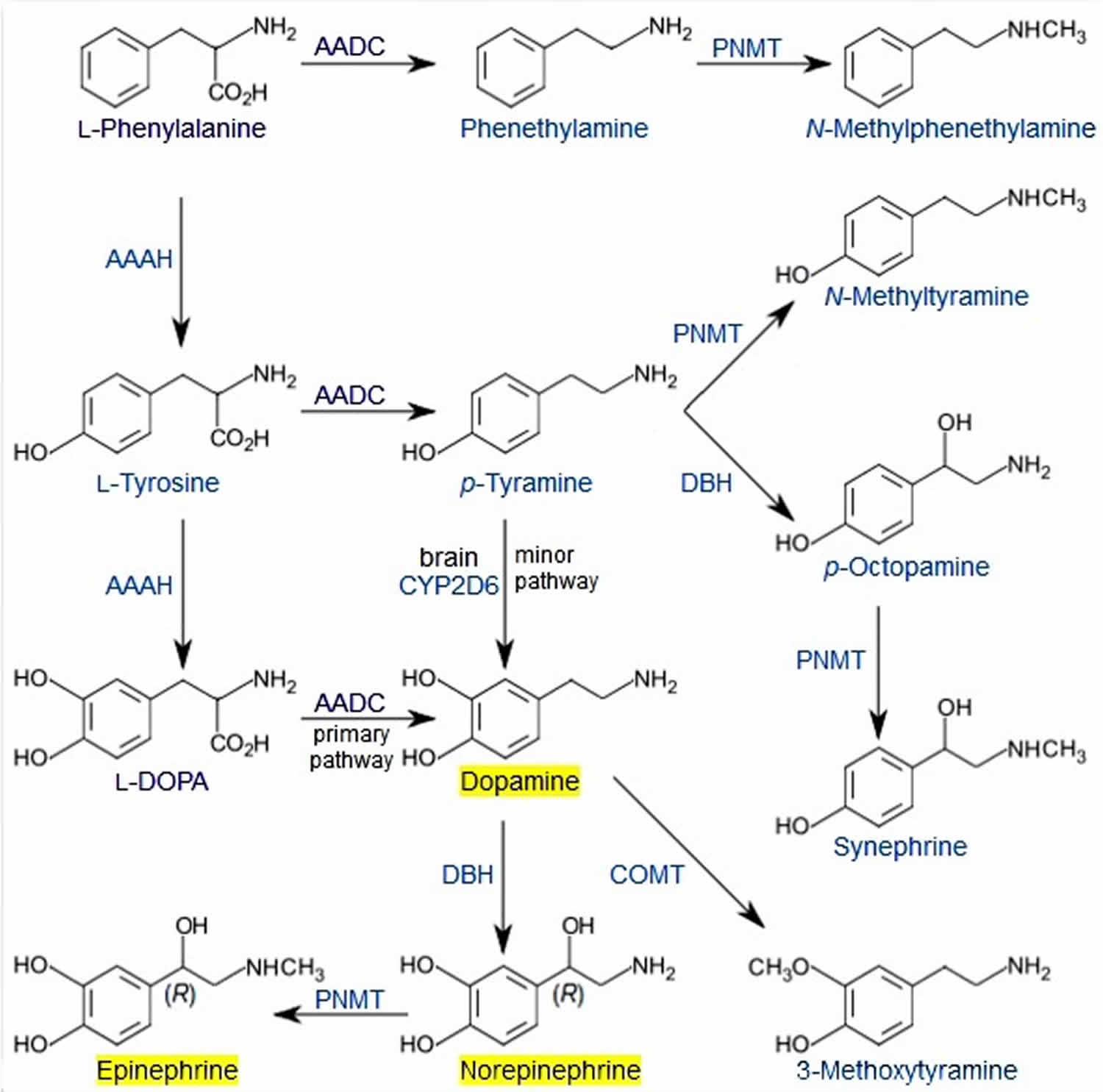
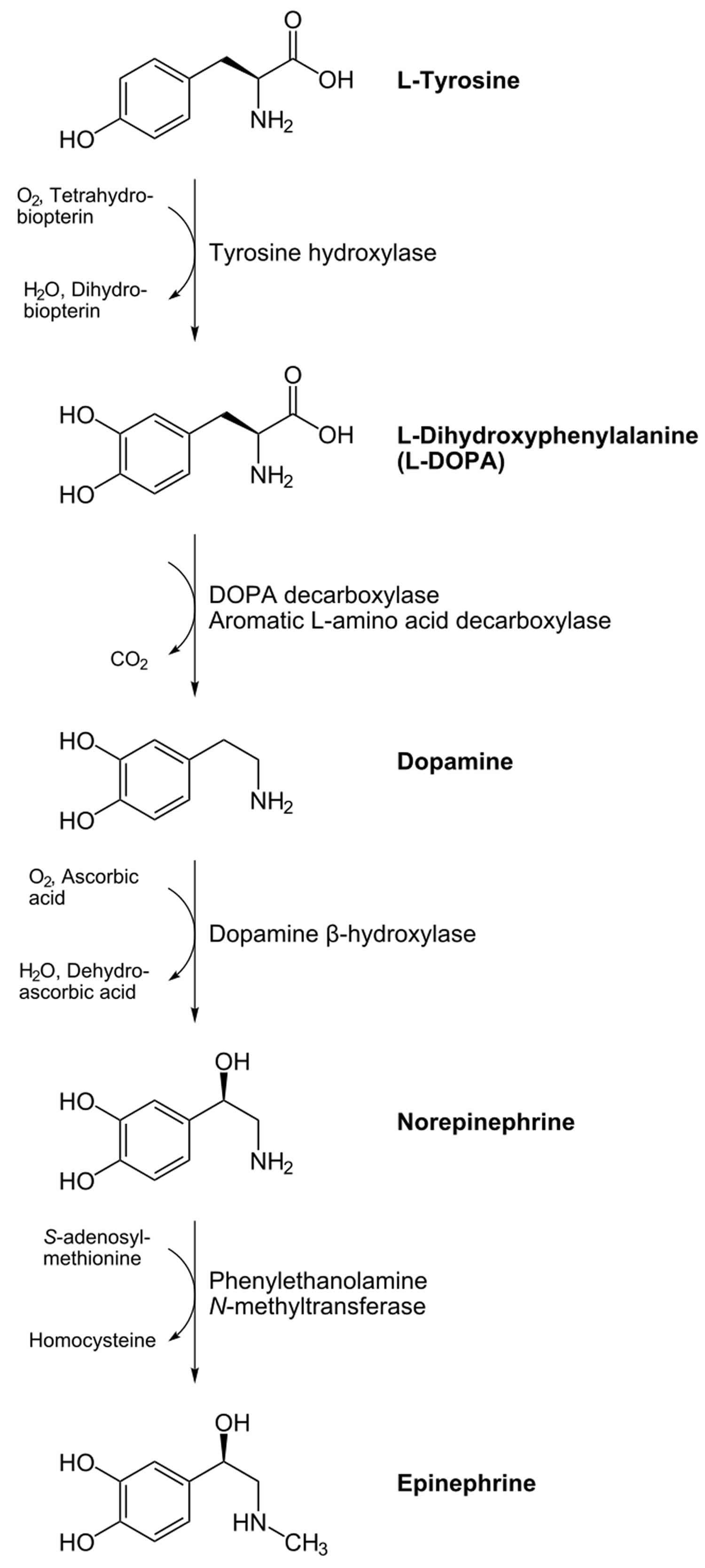
Catecholamine synthesis within the adrenal medulla is controlled by serum concentration of the amino acid tyrosine. Tyrosine undergoes hydroxylation via tyrosine hydroxylase to form L-DOPA (levodopa), which then undergoes decarboxylation to dopamine. Dopamine may be secreted into the bloodstream or undergo further hydroxylation to norepinephrine (noradrenaline). Norepinephrine can be secreted into the bloodstream or further modified by a methyltransferase to epinephrine (adrenaline) and then secreted. Glucocorticoids notably upregulate methyltransferase activity to increase epinephrine production. The enzyme dopamine hydroxylase requires copper as a cofactor (not shown in the diagram) and DOPA decarboxylase requires pyridoxal phosphate (pyridoxal 5′-phosphate) (not shown in the diagram). The rate limiting step in catecholamine biosynthesis through the predominant metabolic pathway is the hydroxylation of L-tyrosine to L-DOPA.
Catecholamine synthesis is inhibited by alpha-methyl-p-tyrosine (AMPT), which inhibits tyrosine hydroxylase.
The amino acids phenylalanine and tyrosine are precursors for catecholamines. Both amino acids are found in high concentrations in the plasma and brain. In mammals, tyrosine can be formed from dietary phenylalanine by the enzyme phenylalanine hydroxylase, found in large amounts in the liver. Insufficient amounts of phenylalanine hydroxylase result in phenylketonuria, a metabolic disorder that leads to intellectual deficits unless treated by dietary manipulation. Catecholamine synthesis usually is considered to begin with tyrosine. The enzyme tyrosine hydroxylase (TH) converts the amino acid l-tyrosine into 3,4- dihydroxyphenylalanine (L-DOPA). The hydroxylation of l-tyrosine by tyrosine hydroxylase (TH) results in the formation of the dopamine precursor L-DOPA, which is metabolized by l-aromatic amino acid decarboxylase (AADC) to the transmitter dopamine. This step occurs so rapidly that it is difficult to measure l-DOPA in the brain without first inhibiting l-aromatic amino acid decarboxylase [AADC]. In neurons that use DA as the transmitter, the decarboxylation of L-DOPA to dopamine is the final step in transmitter, However, in those neurons using norepinephrine (noradrenaline) or epinephrine (adrenaline) as transmitters, the enzyme dopamine b-hydroxylase (DBH), which converts dopamine to yield norepinephrine, is also present. In still other neurons in which epinephrine is the transmitter, a third enzyme phenylethanolamine N-methyltransferase, phenylethanolamine N-methyltransferase [PNMT]) converts norepinephrine into epinephrine. Thus, a cell that uses epinephrine as its transmitter contains four enzymes (tyrosine hydroxylase, AADC, dopamine b-hydroxylase, and phenylethanolamine N-methyltransferase [PNMT]), whereas norepinephrine neurons contain only three enzymes (lacking phenylethanolamine N-methyltransferase [PNMT]) and dopamine cells only two (tyrosine hydroxylase (TH) and l-aromatic amino acid decarboxylase [AADC]).
Figure 1. Catecholamine synthesis
Footnote: In humans, catecholamines (shown in yellow) are derived from the amino acid L-phenylalanine. L-Phenylalanine is converted into L-tyrosine by an aromatic amino acid hydroxylase (AAAH) enzyme (phenylalanine 4-hydroxylase), with molecular oxygen (O2) and tetrahydrobiopterin as cofactors. L-Tyrosine is converted into L-DOPA by another aromatic amino acid hydroxylase enzyme (tyrosine 3-hydroxylase) with tetrahydrobiopterin, O2, and ferrous iron (Fe2+) as cofactors. L-DOPA is converted into dopamine by the enzyme aromatic L-amino acid decarboxylase (AADC), with pyridoxal phosphate as the cofactor. Dopamine itself is also used as precursor in the synthesis of the neurotransmitters norepinephrine and epinephrine. Dopamine is converted into norepinephrine by the enzyme dopamine β-hydroxylase (DBH), with O2 and L-ascorbic acid as cofactors. Norepinephrine is converted into epinephrine by the enzyme phenylethanolamine N-methyltransferase (PNMT) with S-adenosyl-L-methionine as the cofactor.
Figure 2. Dopamine synthesis
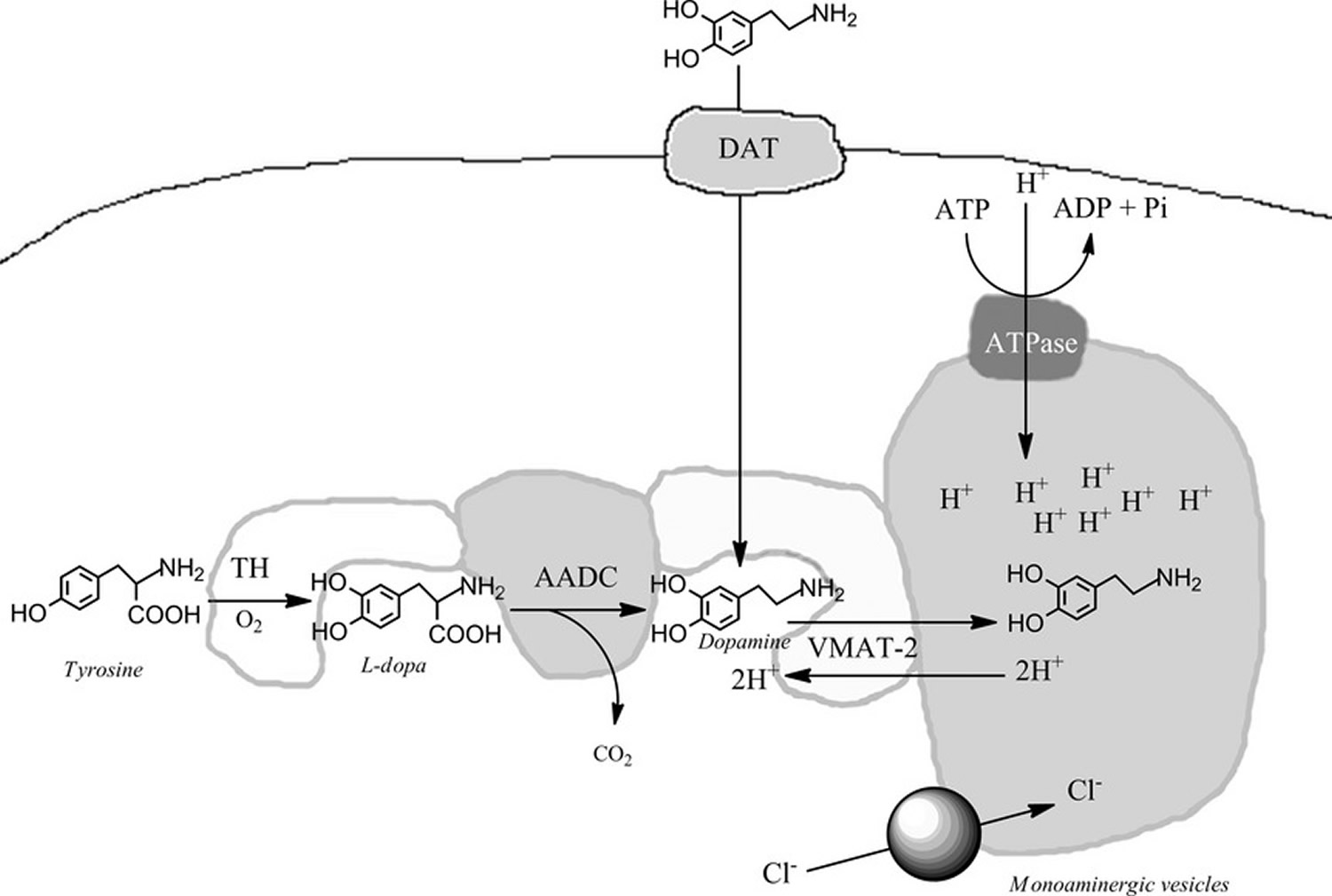 Footnotes: In the presence of oxygen tyrosine hydroxylase (TH) catalyzes the conversion of the amino acid tyrosine to l‐dopa that it is substrate for aromatic amino acid decarboxylase (AADC) that catalyzes the formation of dopamine and CO2. TH and AADC enzymes form a kind of complex with the vesicular monoaminergic transporter‐2 (VMAT‐2) that is localized in the membrane of monoaminergic vesicles. The complex of TH‐AADC‐VMAT‐2 prevents the release of dopamine into the cytosol since the formed dopamine is directly transported into monoaminergic vesicles. The monoaminergic vesicles have an ATPase that pump up protons into the vesicles using ATP, generating a pH decrease and proton gradient that is coupled to dopamine uptake mediated by VMAT‐2 because for one dopamine molecule uptake into the vesicles one proton is released to the cytosol. The low pH inside the monoaminergic vesicles is essential to store high concentration of protonated dopamine hydroxyl groups. [Source 3 ]
Footnotes: In the presence of oxygen tyrosine hydroxylase (TH) catalyzes the conversion of the amino acid tyrosine to l‐dopa that it is substrate for aromatic amino acid decarboxylase (AADC) that catalyzes the formation of dopamine and CO2. TH and AADC enzymes form a kind of complex with the vesicular monoaminergic transporter‐2 (VMAT‐2) that is localized in the membrane of monoaminergic vesicles. The complex of TH‐AADC‐VMAT‐2 prevents the release of dopamine into the cytosol since the formed dopamine is directly transported into monoaminergic vesicles. The monoaminergic vesicles have an ATPase that pump up protons into the vesicles using ATP, generating a pH decrease and proton gradient that is coupled to dopamine uptake mediated by VMAT‐2 because for one dopamine molecule uptake into the vesicles one proton is released to the cytosol. The low pH inside the monoaminergic vesicles is essential to store high concentration of protonated dopamine hydroxyl groups. [Source 3 ]Figure 3. Epinephrine synthesis
Catecholamine release
The catecholamines are normally present in the plasma in minute amounts, but levels can increase dramatically and rapidly in response to change in posture, environmental temperature, physical and emotional stress, hypovolemia, blood loss, hypotension, hypoglycemia, and exercise.
The “fight or flight” response of the sympathetic nervous system is a direct result of the multisystem action of catecholamines. After an external stimulus triggers the body’s stress response, the pituitary-adrenal axis and sympathetic division of the autonomic nervous system is activated. Glucocorticoids production increases in the adrenal cortex, and acetylcholine (Ach) is released from sympathetic splanchnic nerves. Acetylcholine (Ach) binds to nicotinic receptors located on the membrane of chromaffin cells in the adrenal medulla. These receptors promote exocytosis of catecholamine-filled vesicles for transport in the bloodstream. In the blood, catecholamines target alpha and beta-adrenergic receptors, a family of G-protein coupled receptors (GPCRs). These alpha and beta receptors can be further subdivided and subtyped with alphanumeric designation based on their cellular localization. The adrenergic receptors utilize either cyclic adenosine monophosphate (cAMP) or phosphoinositol second messenger systems to activate ion channels that ultimately mediate the body’s sympathetic response.
Secretion from the adrenal medulla proceeding the activation of the sympathetic nervous system functions to regulate blood pressure by contracting the smooth muscle in the vasculature (via alpha-1 receptors). The adrenergic receptors linked to blood vessels have an especially high affinity for norepinephrine relative to the other amines. Further musculoskeletal actions of catecholamines include enhanced contractility of cardiac muscle (via beta-1 receptors), contraction of the pupillary dilator (via alpha-1 receptors), piloerection (via alpha-1 receptors), and relaxation of smooth muscle in the gastrointestinal tract, urinary tract, and bronchioles (via beta-2 receptors). Both epinephrine and norepinephrine modulate metabolism to increase blood glucose levels by stimulating glycogenolysis in the liver (via beta-2 receptors), increased glucagon secretion (via beta-2 receptors) and decreased insulin secretion (via alpha-2 receptors) from the pancreas, and lipolysis in adipose tissue (via beta-3 receptors). Epinephrine also inhibits release of mediators from mast cells and basophils in type I hypersensitivity reactions.
In patients with pheochromocytoma (a potentially curable tumor of catecholamine-producing cells of the adrenal medulla), or less commonly of sympathetic ganglia (paraganglioma), plasma catecholamine levels may be continuously or episodically elevated. This results in episodic or sustained hypertension and in intermittent attacks of palpitations, cardiac arrhythmias, headache, sweating, pallor, anxiety, tremor, and nausea. Intermittent or continuous elevations of the plasma levels of 1 or several of the catecholamines may also be observed in patients with neuroblastoma and related tumors (ganglioneuroblastomas and ganglioneuromas) and, very occasionally, in other neuroectodermal tumors.
At the other end of the spectrum, inherited and acquired syndromes of autonomic dysfunction or failure and autonomic neuropathies are characterized by either inadequate production of 1 or several of the catecholamines or by insufficient release of catecholamines upon appropriate physiological stimuli (e.g.,, change in posture from supine to standing, cold exposure, exercise, stress).
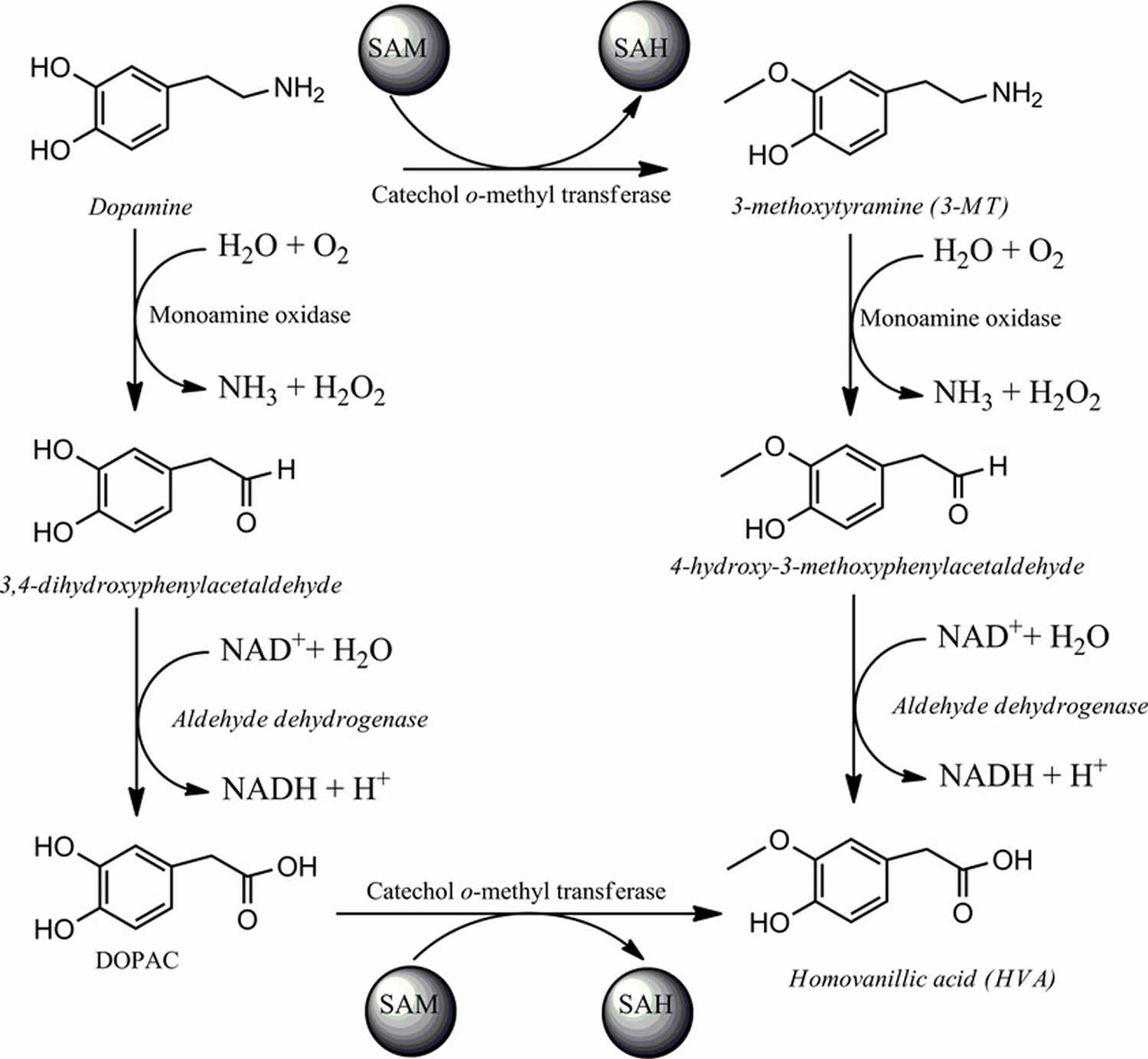
Catecholamine metabolism
Catecholamines have a half-life of a few minutes when circulating in the blood. Degradation of catecholamines to their metabolites occurs either by monoamine oxidase (MAO) located in the outer mitochondrial membrane of the cell and/or by catechol-o-methyltransferase (COMT) found within the cytosol of the cell. Monoamine oxidase (MAO) and catechol-o-methyltransferase (COMT) catabolize norepinephrine and epinephrine to vanillylmandelic acid (VMA), and dopamine to homovanillic acid (HVA). VMA (vanillylmandelic acid) and HVA (homovanillic acid) are excreted in urine.
Both enzymes require cofactors: COMT (catechol-o-methyltransferase) uses Mg2+ (magnesium) as a cofactor while MAO (monoamine oxidase) uses flavin adenine dinucleotide (FAD). The first step of the catabolic process is mediated by either MAO or COMT which depends on the tissue and location of catecholamines (for example degradation of catecholamines in the cleft is mediated by COMT because MAO is a mitochondrial enzyme). The next catabolic steps in the pathway involve alcohol dehydrogenase, aldehyde dehydrogenase and aldehyde reductase. The end product of epinephrine and norepinephrine is VMA (vanillylmandelic acid) which is excreted in the urine. Dopamine catabolism leads to the production of HVA (homovanillic acid) 4.
Figure 4. Dopamine degradation catalyzed by monoamine oxidase (MAO) and catechol methyl ortho‐transferase (COMT)
Catecholamine normal levels
Catecholamine testing measures the amounts of catecholamine hormones in the urine and/or blood. Urine testing is recommended over blood testing. Just the stress of having blood drawn can increase catecholamine blood levels, so results from blood tests are not as reliable as results from urine tests.
Norepinephrine
- Age <1 year: <11 mcg/24 hours
- Age 1 year: 1-17 mcg/24 hours
- Age 2-3 years: 4-29 mcg/24 hours
- Age 4-6 years: 8-45 mcg/24 hours
- Age 7-9 years: 13-65 mcg/24 hours
- Age> 10 years: 15-80 mcg/24 hours
Epinephrine
- Age <1 year: <2.6 mcg/24 hours
- Age 1 year: <3.6 mcg/24 hours
- Age 2-3 years: <6.1 mcg/24 hours
- Age 4-9 years: 0.2-10.0 mcg/24 hours
- Age 10-15 years: 0.5-20.0 mcg/24 hours
- Age > 16 years: <21 mcg/24 hours
Dopamine
- Age <1 year: <86 mcg/24 hours
- Age 1 year: 10-140 mcg/24 hours
- Age 2-3 years: 40-260 mcg/24 hours
- Age > 4 years: 65-400 mcg/24 hours
Catecholamines test
Tests used for determining the presence of catecholamine-secreting tumors (pheochromocytomas and paragangliomas) include plasma catecholamines, urine catecholamines, plasma free metanephrines and urine metanephrines. These tests measure either the catecholamines or their metabolites (metanephrines) and have varying sensitivity and specificity. Current guidelines recommend plasma free metanephrines or urinary fractionated metanephrines for initial biochemical testing. The healthcare provider may, however, select any one (or more than one) depending on the person’s presentation, family history, and/or genetic profile.
24 hour urine catecholamine
24 hour urine catecholamines testing measures the total amount of catecholamines released into the urine in 24 hours. Since the catecholamine hormones levels may fluctuate significantly during this period, the urine test may detect excess episodic production that is missed with the blood test.
The test for 24 hour urine catecholamines is very sensitive and false positives do occur. The 24 hour urine catecholamines test is affected by stress, drugs, smoking, and various foods such as caffeine-containing drinks and alcohol. If a person has only moderately elevated levels, then the healthcare provider may re-evaluate the person’s medications, diet, and stress level to look for interfering substances or conditions. Once these are resolved, the person may then be tested again to determine whether the levels are still elevated and take appropriate action.
24 hour urine catecholamines testing may be ordered when tests for plasma free metanephrines and/or urine metanephrines are inconclusive and a health practitioner needs more information about a possible catecholamine-secreting tumor. 24 hour urine catecholamines may be ordered when a person, especially a relatively young person (younger than age 40) has sudden bursts (paroxysms) of signs and symptoms such as:
- High blood pressure (hypertension), especially when a person has hypertension that is not responding to treatment, as people with pheochromocytomas and paragangliomas are frequently resistant to conventional therapies
- Severe headaches
- Sweating
- Flushing
- Rapid heart rate (palpitations)
- Tremor
The 24 hour urine catecholamine tests may also be ordered for an asymptomatic person if an adrenal or neuroendocrine tumor is detected during a scan conducted for another purpose or if the person has a strong personal or family history of pheochromocytoma.
It may also be ordered at intervals when a person has been previously treated for one of these tumors.
What does high level of catecholamines or catecholamine excess mean?
A high level of catecholamines in the blood and/or urine in a person with signs and symptoms strongly suggests the presence of a catecholamine-secreting tumor. A high level of catecholamines indicates that further investigation is needed. It is recommended that imaging studies be performed to locate the catecholamine-secreting tumor once there is clear biochemical evidence of such a tumor.
While plasma and urine catecholamines tests can help detect and diagnose catecholamine-secreting tumors, they cannot tell the location of the tumor, whether there is more than one, or whether or not the tumor is benign (although most are). The total amount of catecholamines produced will tend to increase as the tumor increases in size or number.
Although pheochromocytomas and extra-adrenal paragangliomas are rare, 25% occur in the setting of a hereditary syndrome associated with alterations in specific genes. These genetic syndromes have thus been identified as carrying an increased tumor risk. Examples include MEN-1 and MEN-2 (Multiple Endocrine Neoplasia, types 1 and 2) syndromes.
It has been proposed that all patients diagnosed with a pheochromocytoma or extra-adrenal paraganglioma should consider genetic counseling and testing. Early identification of a hereditary syndrome allows for early screening for other associated tumors. In addition, some patients with a hereditary syndrome are more likely to develop malignant or recurrent disease. Knowledge of the specific genetic mutation permits increased vigilance during preoperative localization or postoperative surveillance of such patients.
It is also recommended that if a mutation is identified, predictive genetic testing should be offered to asymptomatic at-risk family members.
A variety of medications can interfere with catecholamines testing. However, it is important to talk to your healthcare provider before discontinuing any prescribed medications. Your healthcare provider will work with you to identify potentially interfering substances and drug treatments and to determine which of them can be safely interrupted and which must be continued for your well-being.
If catecholamine levels are elevated in a person who has been treated for a catecholamine-secreting tumor, then it is likely that either treatment was not fully effective or that the tumor is recurring and appropriate follow up is needed.
If the level of catecholamines is normal, then it is unlikely that a person has a catecholamine-secreting tumor. However, pheochromocytomas do not necessarily produce catecholamines at a constant rate. Therefore, if the person has not had a recent episode of hypertension, their blood and urine concentrations of catecholamines could be at normal or near normal levels even when a pheochromocytoma is present. If suspicion remains high, testing may be repeated.
High levels of catecholamines can also be caused by monoamine oxidase A (MAO-A) deficiency. As MAO-A is one of the enzymes responsible for degradation of these neurotransmitters, its deficiency increases the bioavailability of these neurotransmitters considerably. It occurs in the absence of pheochromocytoma, neuroendocrine tumors, and carcinoid syndrome, but it looks similar to carcinoid syndrome such as facial flushing and aggression 5.
The acute porphyria’s can cause elevated catecholamines 6.
Can my state of mind really affect my test results?
Yes, because catecholamines are released from the adrenal glands in response to stress. If you are anxious or afraid, your catecholamines concentrations may be increased.
Can I have more than one pheochromocytoma at once?
Yes. Usually a single adrenal tumor will arise in one gland or the other, but multiple tumors can form. This is more likely in people with a strong family history of pheochromocytomas. A person may have a tumor in each adrenal gland or occasionally in other locations.
Plasma free metanephrines
The metanephrines – metanephrine and normetanephrine – are breakdown products (metabolites) of epinephrine (adrenaline) and norepinephrine. The plasma free metanephrines test measures the amount of metanephrine and normetanephrine in the blood.
The Endocrine Society recommends that a test for plasma free metanephrine or urine metanephrine be used as the primary test to help detect the presence of pheochromocytomas and paragangliomas. Although they are rare, it is important to diagnose these tumors because they cause a potentially curable form of hypertension. In most cases, the tumors can be surgically removed and/or treated to eliminate or significantly reduce the amount of catecholamine being produced and to eliminate their associated symptoms and complications.
The blood test may be most useful when the person has persistent hypertension or is currently experiencing a sudden burst (paroxysm) of hypertension. This is because the hormones do not stay long in the blood; they are used by the body and rapidly broken down (metabolized) and/or then eliminated. Urine testing measures the total amount of metanephrines released into the urine in 24 hours. Since the hormone levels may fluctuate significantly during this period, the urine test may detect excess production that is missed with the blood test.
The test for metanephrines is very sensitive and false positives do occur. The test is affected by stress, drugs, smoking and various foods such as caffeine-containing drinks and alcohol. If a person has only moderately elevated metanephrines, then the healthcare provider may re-evaluate the person’s medications, diet, and stress level to look for interfering substances or conditions. Once these are resolved, the person may be tested again to determine whether the metanephrines are still elevated and take appropriate action. Sometimes the plasma free metanephrines test will done in conjunction with 24-hour urine metanephrines testing and/or followed by catecholamines testing to help decide if a catecholamine-secreting tumor is present.
When is plasma free metanephrines test ordered?
The plasma free metanephrines test is primarily ordered when a health practitioner either suspects that someone has a catecholamine-secreting tumor or wants to rule out the possibility. It may be ordered when a person (especially a person younger than age 40) has sudden bursts (paroxysms) of signs and symptoms, such as:
- High blood pressure (hypertension), especially when a person has hypertension that is not responding to treatment since people with catecholamine-secreting tumors are frequently resistant to conventional therapies
- Severe headaches
- Sweating
- Flushing
- Rapid heart rate (palpitations)
- Tremor
Testing may also be ordered when a catecholamine-secreting tumor has been treated or removed to monitor for recurrence.
Occasionally, the test may be ordered when an adrenal tumor is detected incidentally, such as during a scan conducted for another purpose, or when someone has a strong personal or family history of catecholamine-secreting tumors. It may also be ordered for an asymptomatic person with a known genetic risk of these tumors.
What does high metanephrine and normetanephrine blood levels mean?
High levels of metanephrine and normetanephrine in a person with signs and symptoms suggest the presence of a catecholamine-secreting tumor. It is recommended that patients with a positive result should receive appropriate follow-up according to the test values noted and the clinical presentation. Imaging scans, such as MRI, should be done to locate the tumor.
If levels are elevated in someone who has been treated for a catecholamine-secreting tumor, it may be an indication that the treatment was not fully effective or that the tumor is recurring and appropriate follow-up is needed.
Normal metanephrine and normetanephrine blood levels mean it is unlikely that the person tested has a catecholamine-secreting tumor. The plasma free metanephrines test is very sensitive and these tumors are rare, so the negative predictive value of the test is very good.
Does the amount of plasma free metanephrines detected correspond to the size of the tumor?
No, it has more to do with the characteristics of the tumor. Even a very small tumor can produce large amounts of catecholamines.
Is it really necessary to follow the dietary restrictions?
The level of catecholamines (and their metabolites) in blood is affected by diet. For test accuracy, interfering substances need to be avoided. Various foods, including caffeine-containing foods such as coffee and energy drinks, and chocolate, as well as cigarette and cigar smoking may interfere with the test and should be avoided prior to testing. It is important to follow the instructions given by your healthcare provider and the specimen collecting site.
Is it really necessary to lie down before testing?
The patient may be seated for the blood sample collection. However, recent guidelines suggest that it is preferable for the patient to be lying down. The healthcare provider or the collection site will instruct the patient as to their specific requirements.
24 hour urine metanephrines
The metanephrines – metanephrine and normetanephrine – are breakdown products (metabolites) of epinephrine (adrenaline) and norepinephrine. 24 hour urine metanephrines test measures the amounts of metanephrine and normetanephrine that are released into the urine over a 24-hour period.
The Endocrine Society recommends that a test for plasma free metanephrine or urine metanephrine be used as the primary test to help detect the presence of pheochromocytomas and paragangliomas. Although they are rare, it is important to diagnose these tumors because they cause a potentially curable form of hypertension. In most cases, the tumors can be surgically removed and/or treated to eliminate or significantly reduce the amount of catecholamine being produced and to eliminate their associated symptoms and complications.
24 hour urine testing measures the total amount of metanephrines released into the urine in 24 hours. Since the hormone levels may fluctuate significantly during this period, the urine test may detect excess production that is missed with the blood test.
The test for metanephrines is very sensitive and false positives do occur. The test is affected by stress, drugs, smoking and various foods such as caffeine-containing drinks and alcohol. If a person has only moderately elevated metanephrines, then the healthcare provider may re-evaluate the person’s medications, diet, and stress level to look for interfering substances or conditions. Once these are resolved, the person may be tested again to determine whether the metanephrines are still elevated and take appropriate action. Sometimes the 24-hour urine metanephrines test will be done in conjunction with plasma free metanephrines testing and/or followed by catecholamines testing to help decide if a catecholamine-secreting tumor is present.
When is 24 hour urine metanephrines test ordered?
Urine metanephrines are ordered when a healthcare provider either suspects that someone has a catecholamine-secreting tumor or wants to rule out the possibility. 24 hour urine metanephrines test may be ordered when a person (especially a person younger than age 40) has sudden bursts (paroxysms) of signs and symptoms such as:
- High blood pressure (hypertension), especially when a person has hypertension that is not responding to treatment since people with catecholamine-secreting tumors are frequently resistant to standard therapies
- Severe headaches
- Sweating
- Flushing
- Rapid heart rate (palpitations)
- Tremor
24 hour urine metanephrines test may also be ordered when a catecholamine-secreting tumor has been treated or removed to monitor for recurrence.
Occasionally, 24 hour urine metanephrines test test may be ordered when an adrenal tumor is detected incidentally, such as during a scan conducted for another purpose, or when someone has a family history of pheochromocytomas. It may also be ordered on an asymptomatic person with a known genetic risk of these tumors.
What does high metanephrine and normetanephrine urine levels mean?
High levels of metanephrine and normetanephrine in a person with signs and symptoms suggest the presence of a catecholamine-secreting tumor. It is recommended that patients with a positive result should receive appropriate follow-up according to the test values noted and the clinical presentation. Imaging scans, such as MRI, should be done to locate the probable tumor.
If levels are elevated in someone who has been treated for a catecholamine-secreting tumor, it may be an indication that the treatment was not fully effective or that the tumor is recurring and appropriate follow-up is needed.
Normal urine levels of metanephrine and normetanephrine mean it is unlikely that the person tested has a catecholamine-secreting tumor. This test is very sensitive and these tumors are rare, so the negative predictive value of the test is very good.
Is it really necessary to collect urine for 24 hours?
Yes, for accurate test results, it is essential that all of the urine be collected. Because the catecholamines are released at varying times, one sample might not be sufficient to detect the average concentration of metanephrines.
Does the amount of urine metanephrines detected correspond to the size of the tumor?
No, it has more to do with the characteristics of the tumor. Even a very small tumor can produce large amounts of catecholamines.
Is it really necessary to follow the dietary restrictions?
The level of catecholamines (and their metabolites) in blood is affected by diet. For test accuracy, interfering substances need to be avoided. Various foods, including caffeine-containing foods such as coffee and energy drinks, and chocolate, as well as cigarette and cigar smoking may interfere with the test and should be avoided prior to testing. It is important to follow the instructions given by your healthcare provider and the specimen collection site.
Can I have more than one pheochromocytoma at once?
Yes. Usually a single adrenal tumor will arise in one gland or the other, but multiple tumors can form. This is more likely in people with a strong family history of pheochromocytomas. A person may have a tumor in each adrenal gland or occasionally in other locations.
- Young SN. How to increase serotonin in the human brain without drugs. J Psychiatry Neurosci. 2007;32(6):394-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2077351/[↩]
- Adrenergic neurons in human brain demonstrated by immunohistochemistry with antibodies to phenylethanolamine-N-methyltransferase (PNMT): discovery of a new group in the nucleus tractus solitarius. Neurosci Lett. 1985 Feb 4;53(3):303-8. https://www.ncbi.nlm.nih.gov/pubmed/3885079[↩][↩]
- Protective and toxic roles of dopamine in Parkinson’s disease. Journal of Neurochemistry 18 Feb 2014. https://onlinelibrary.wiley.com/doi/full/10.1111/jnc.12686[↩][↩]
- Eisenhofer, G.; Kopin, IJ; Goldstein, DS (2004). “Catecholamine metabolism: a contemporary view with implications for physiology and medicine”. Pharmacol. Rev. 3 (56): 331–49. https://www.ncbi.nlm.nih.gov/pubmed/15317907[↩]
- Family-based and association studies of monoamine oxidase A and attention deficit hyperactivity disorder (ADHD): preferential transmission of the long promoter-region repeat and its association with impaired performance on a continuous performance test (TOVA). Molecular Psychiatry volume 7, pages 626–632 (2002). https://www.nature.com/articles/4001037.pdf[↩]
- Stewart MF, Croft J, Reed P, New JP. Acute intermittent porphyria and phaeochromocytoma: shared features. J Clin Pathol. 2007;60(8):935-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1994495/[↩]