Contents
What is cerebral edema
Cerebral edema simply means swelling of the brain. Cerebral edema is a relatively common phenomenon with numerous causes. Cerebral edema can be asymptomatic, merely seen on imaging, or it can cause life-threatening complications 1. Cerebral edema is categorized into either vasogenic, cellular, osmotic, and interstitial causes 2. Cerebral edema can arise from a variety of causes, including head trauma, vascular ischemia 3, intracranial lesions, or obstructive hydrocephalus resulting in interstitial edema. The consequences of cerebral edema can be devastating, even fatal, if untreated.
The explanation of the mechanism of injury arising from cerebral edema comes via the Monroe-Kellie doctrine. The Monroe-Kellie doctrine states that space of the cranial cavity is fixed in volume and contains fixed proportions of brain matter (approximately 1400 ml), blood (approximately 150 ml) and cerebrospinal fluid (approximately 150 ml) 4. The Monroe-Kellie Doctrine states that intracranial volume is constant and an increase in the volume of one component will cause a decrease in the volume of one or both of the others. Because of this fixed space, an increase in the volume of one of these components must, therefore, result in the loss of another component in equal amounts 5. In cerebral edema, the relative volume of brain tissue increases as the brain tissues swells with edema. Within a rigid skull structure, this change can have significant effects, such as decreases perfusion (blood) to the brain or herniation of brain tissue and the pressure can cause further damage to both the edematous and non-edematous brain. When brain herniation occurs, the location of the herniation affects the presenting symptoms and the clinical outcomes.
Brain herniation can occur:
- Between areas inside the skull, such as those separated by a rigid membrane like the tentorium cerebelli or falx cerebri
- Through a natural opening at the base of the skull called the foramen magnum
- Through openings created during brain surgery
Clinical presentation of cerebral edema is variable, ranging from asymptomatic to severe autonomic dysregulation, coma, and death. Symptoms appear as the intracranial pressure (ICP) rises above 20 cm H2O in most patients. Treatment for cerebral edema targets the underlying cause and any life-threatening complications. Treatments include hyperventilation, osmotherapy, diuretics, corticosteroids, and surgical decompression.
What causes brain swelling
Cerebral edema can result from a variety of causes. The major types include vasogenic, cellular, osmotic, and interstitial.
Through these mechanisms, brain swelling occurs from tumor, trauma, hypoxia, infection, metabolic derangements, or acute hypertension. Causes are widespread and divide into neurological and non-neurological categories. Other non-neurologic causes include hepatitis, Reye syndrome, carbon monoxide poisoning, lead poisoning, and high altitude cerebral edema.
Vasogenic cerebral edema
Vasogenic cerebral edema, the most common form, results from the disruption of the blood-brain-barrier. With the disrupted blood-brain-barrier ions and proteins flow more freely into the extravascular space which causes osmotic draw of fluid into the brain interstitium. For example, vascular endothelial growth factor (VEGF), glutamate, and leukotrienes produced locally increase the permeability of vessels around tumors 6. These factors and a lack of tight endothelial cell junctions in the vessels around the tumors cause this increased permeability, which allows for an influx of proteinaceous solute and fluid into the brain parenchyma, particularly in the white matter 7. Peritumor edema, for example, leads to 65% of patients developing cognitive impairment resulting from displacement and damage to white matter tracts 8.
Cellular or cytotoxic cerebral edema
Traumatic brain injury and stroke cause this form of brain swelling. Cellular or cytotoxic brain swelling often results within minutes of the insult/injury and affects glial, neuronal, and endothelial cells within the brain. In cytotoxic brain swelling, the cells lack hemostatic mechanisms, and primarily sodium enters the cell freely, with the failure of the export mechanism. Anions then follow, attempting to return neutrality to the cell, resulting in intracellular edema as the cells swell with increased water following the ions into the intracellular compartment 9.
Interstitial cerebral edema
Interstitial cerebral edema results from the outflow of cerebrospinal fluid from the intraventricular space to the interstitial areas of the brain. Patients with hydrocephalus or meningitis are examples of those affected by this etiology. The increased pressure, against the cerebrospinal fluid (CSF) and brain, drives fluid into the brain parenchyma. The fluid accumulates in the extracellular space of mostly the white matter causing the cerebral edema.
Osmotic cerebral edema
Osmotic brain swelling generally stems from derangements affecting osmolarity, such as hyponatremia, diabetic ketoacidosis (DKA), or similar metabolic pathologies. The cells of the brain pull water from the plasma in these instances, resulting in widespread edema.
Cerebral edema signs and symptoms
Cerebral edema can be asymptomatic, merely seen on imaging, or it can cause life-threatening complications. The history can help provide insights as to the etiology of the cerebral edema. Patients may have a history of trauma, a hypoxic event, cancer, metabolic diseases or other factors which can help identify the possible etiology of the cerebral edema.
The physical exam findings of cerebral edema can vary widely depending on the location and extent of the cerebral edema. Localized cerebral edema can cause dysfunction of the edematous brain and include weakness, visual disturbances, seizures, sensory changes, diplopia, and other neurologic disturbances. For diffuse cerebral edema, the patient may have headaches, nausea, vomiting, lethargy, altered mental status, confusion, coma, seizure or other manifestations. With diffuse or focal cerebral edema the patient can develop increased intracranial pressure (ICP) which typically presents with headaches, nausea, vomiting, lethargy, cranial neuropathy, altered mental status to coma and death.
Cerebral edema complications
Complications of cerebral edema range from mild cognitive impairment to death. Untreated, severe cerebral edema is fatal due to brain and brainstem compression and herniation. The presence of significant cerebral edema can cause diffuse brain injury, precipitate seizures in some cases, or create large areas of ischemic brain tissue. Cerebral edema, particularly when widespread, can increase ICP (intracranial pressure), and this is the most life-threatening complication of brain swelling due to the potential for herniation and brainstem injury. Permanent brain injury can occur in more severe cases. Many of the complications are related to the underlying cause(s) of the edema.
Cerebral edema diagnosis
It is extremely important to identify severe cerebral edema as early as possible to prevent herniation and death. For example malignant middle cerebral artery stroke presenting with severe cerebral edema. Malignant middle cerebral artery stroke is seen more commonly in the younger population. Usually, these patients are admitted to the ICU setting. Following the Neurological exam closely is very important. Usually, there is an altered mental status and development of fixed and dilated pupil. Patients presenting with findings suggestive of cerebral insult should undergo computed tomography (CT) scan of the brain; this can show the edema, which is visible as areas of low density and loss of gray/white matter differentiation, on an unenhanced image. There can also be the obliteration of the cisterns and sulcal spaces. A CT scan can also reveal the cause in some cases. If flattened gyri or narrowed sulci, or compression of the ventricles, is seen, this suggests increased ICP. Serial CT scans are used to show the progression or improvement of the edema.
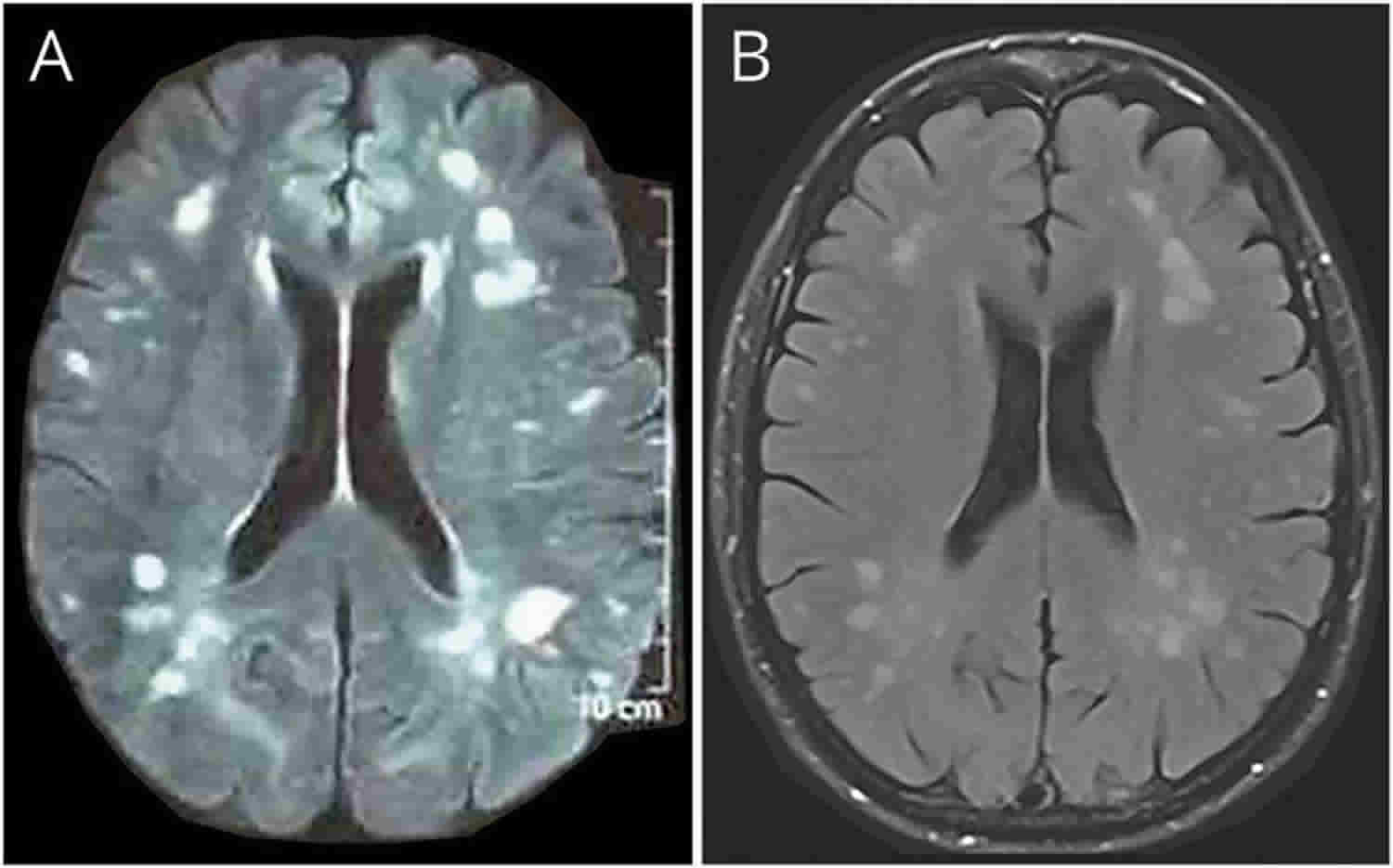
Magnetic resonance imaging (MRI) can show increased T2 and FLAIR signal changes (hyperintensity) within the brain.
If increased ICP is a concern from the cerebral edema, then an ICP monitor or ventriculostomy may be needed to monitor ICP and can provide better outcomes by helping to tailor therapy 10.
Cerebral edema treatment
Treatment of cerebral edema is two-fold: prevent further injury from the cerebral edema and remediate the original insult causing the cerebral edema if able 1.
Treating the underlying and ongoing insult can include correcting metabolic derangements, controlling hypertension, removing intracranial lesion(s) or shunting hydrocephalus depending on the cause of the cerebral edema.
Brain swelling should be controlled to prevent further injury, and complications such as increased ICP (intracranial pressure) should be mitigated. Glucocorticoids have shown potential benefit in cerebral edema secondary to vasogenic edema but have limited utility in other forms of edema and should be avoided altogether in the face of trauma 11. Avoidance of hypotonic fluids is a strong recommendation in instances of cerebral edema as they can worsen cerebral edema and cause elevations in ICP. If the cerebral edema is causing elevated ICP, various methods are available to help control ICP including positioning, hyperosmolar therapy, antipyretics, sedatives 12, paralytics, modulation of PCO2 13, and surgical intervention 14.
In the management of malignant middle cerebral artery stroke presenting with severe cerebral edema, osmotic agents can be used to create an osmotic gradient across blood thereby drawing fluid intravascularly and decreasing cerebral edema. Mannitol was the primary agent used at doses of 0.25 to 1 g/kg body weight and is thought to exert its greatest benefit by decreasing blood viscosity and to a lesser extent by decreasing blood volume. Side effects of mannitol use are eventual osmotic diuresis and dehydration as well as renal injury if serum osmolality exceeds 320 mOsm. Three percent hypertonic saline is also commonly used to decrease cerebral edema and can be administered as a 5 ml/kg bolus or a continuous infusion, monitoring serum sodium levels closely. It is considered relatively safe while serum sodium is < than 160mEq/dl or serum osmolality is less than 340 mOsm. A decompressive craniectomy is a neurosurgical procedure wherein a part of the skull is removed, and dura lifted, allowing the brain to sell without causing compression. It is usually considered as a last resort when all other ICP lowering measures have failed. When considered it is a good idea to do this procedure sooner rather than later 15.
High altitude cerebral edema
High altitude sickness, also known as acute mountain sickness, is caused by the low oxygen levels in the air at altitudes above about 8,000 feet (2,438 meters). High altitude sickness is caused by reduced air pressure and lower oxygen levels at high altitudes. High altitude sickness occurs when your body has not had time to adjust to less oxygen. Altitude sickness can be fatal if not treated.
High altitude sickness can affect anybody – being young or physically fit does not decrease the risk. Whether or not you get altitude sickness could depend on:
- your height above sea level
- the time you took to make the ascent
- whether or not you have any problems affecting you heart and lungs
The faster you climb to a high altitude, the more likely you will get acute mountain sickness.
If you have high altitude sickness, you are likely to feel dizzy and weak, you might also have a headache and feel nauseous. It can feel like a hangover.
High altitude sickness can affect your lungs, in which case it is sometimes known as high altitude pulmonary edema or HAPE. People with high altitude pulmonary edema (HAPE) can feel short of breath and have a cough and a racing heart. In extreme cases, their lips turn blue.
High altitude sickness can also cause your brain to swell with fluid, which is sometimes known as high altitude cerebral edema or HACE. People with high altitude cerebral edema (HACE) can feel confused and irritable and behave in an erratic way.
Altitude sickness can be worse at night and can last for days, even if you stay at the same altitude.
You are at higher risk for high altitude sickness if:
- You live at or near sea level and travel to a high altitude.
- You have had the illness before.
- You ascend quickly.
- You have not acclimatized to the altitude.
- Alcohol or other substances have interfered with acclimatization.
- You have medical problems involving the heart, nervous system, or lungs.
If you have high altitude sickness, you should stay at the same altitude or go lower until the symptoms disappear. Rest, fluids and pain killers are likely to improve the symptoms. Do not continue to climb higher.
It is best not to drink alcohol or take sedatives or sleeping pills because they interfere with the body’s adaptation to high altitude.
If you have signs of altitude sickness affecting your lungs or your brain, this is a medical emergency. You need help to descend as soon as possible. Breathing oxygen from a tank can help.
A medicine called acetazolamide (Diamox) may be given to help you breathe better. It can help reduce symptoms. This medicine can make you urinate more often. Make sure you drink plenty of fluids and avoid alcohol when taking this drug. This medicine works best when taken before reaching a high altitude.
Dexamethasone (Decadron) may help reduce acute mountain sickness symptoms and swelling in the brain (cerebral edema).
High altitude sickness complications may include:
- Coma (unresponsiveness)
- Fluid in the lungs (pulmonary edema)
- Swelling of the brain (cerebral edema), which can lead to seizures, mental changes, or permanent damage to the nervous system
- Death
How is high altitude sickness prevented?
If you’re planning to travel to a high altitude, consider talking to your doctor about drugs that can help with acclimatization, particularly if you have had altitude sickness before.
You can reduce the chance of getting altitude sickness by:
- avoiding a rapid ascent from sea level – don’t go above about 8,000 feet (2,438 meters) for the first night’s sleep
- once you get above 9,842 feet (3,000 meters), ascending by no more than 1,642 feet (500 meters) per day
- spending the night below the day’s highest altitude
- avoiding strenuous exercise before your body has had time to adjust to the lower oxygen levels
- avoiding alcohol at high altitude
If you have a medical problem that affects your lungs, heart or circulation, you are at increased risk of getting high altitude sickness.
High altitude sickness symptoms
Your symptoms will also depend on the speed of your climb and how hard you push (exert) yourself. Symptoms range from mild to life-threatening. They can affect the nervous system, lungs, muscles, and heart.
In most cases, symptoms are mild. Symptoms of mild to moderate acute mountain sickness may include:
- Difficulty sleeping
- Dizziness or light-headedness
- Fatigue
- Headache
- Loss of appetite
- Nausea or vomiting
- Rapid pulse (heart rate)
- Shortness of breath with exertion
Symptoms that may occur with more severe acute mountain sickness include:
- Blue color to the skin (cyanosis)
- Chest tightness or congestion
- Confusion
- Cough
- Coughing up blood
- Decreased consciousness or withdrawal from social interaction
- Gray or pale complexion
- Cannot walk in a straight line, or walk at all
- Shortness of breath at rest
High altitude sickness diagnosis
Your health care provider will examine you and listen to your chest with a stethoscope. This may reveal sounds called crackles (rales) in the lung. Rales may be a sign of fluid in the lungs.
Tests that may be done include:
- Blood tests
- Brain CT scan
- Chest x-ray
- Electrocardiogram (ECG)
High altitude sickness treatment
Early diagnosis is important. Acute mountain sickness is easier to treat in the early stages.
The main treatment for all forms of mountain sickness is to climb down (descend) to a lower altitude as rapidly and safely as possible. You should not continue climbing if you develop symptoms.
Extra oxygen should be given, if available.
People with severe mountain sickness may need to be admitted to a hospital.
A medicine called acetazolamide (Diamox) may be given to help you breathe better. It can help reduce symptoms. This medicine can make you urinate more often. Make sure you drink plenty of fluids and avoid alcohol when taking this drug. This medicine works best when taken before reaching a high altitude.
If you have fluid in your lungs (pulmonary edema), treatment may include:
- Oxygen
- A high blood pressure medicine called nifedipine
- Beta agonist inhalers to open the airways
- Breathing machine in severe cases
- Medicine to increase blood flow to the lungs called phosphodiesterase inhibitor (such as sildenafil)
Dexamethasone (Decadron) may help reduce acute mountain sickness symptoms and swelling in the brain (cerebral edema).
Portable hyperbaric chambers allow hikers to simulate conditions at lower altitudes without actually moving from their location on the mountain. These devices are very helpful if bad weather or other factors make climbing down the mountain impossible.
High altitude sickness prognosis
Most high altitude sickness cases are mild. Symptoms improve quickly when you climb down the mountain to a lower altitude.
Severe cases may result in death due to lung problems or brain swelling.
In remote locations, emergency evacuation may not be possible, or treatment may be delayed. This can have a negative effect on the outcome.
The outlook depends on the rate of descent once symptoms begin. Some people are more prone to developing altitude-related sickness and may not respond as well.
- Nehring SM, Tadi P, Tenny S. Cerebral Edema. [Updated 2019 Mar 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537272[↩][↩]
- Lawrence SE, Cummings EA, Gaboury I, Daneman D. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. J. Pediatr. 2005 May;146(5):688-92[↩]
- Yang Y, Rosenberg GA. Blood-brain barrier breakdown in acute and chronic cerebrovascular disease. Stroke. 2011 Nov;42(11):3323-8.[↩]
- Kostecki K, Pearson-Shaver AL. Subfalcine Herniation. [Updated 2018 Dec 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536946[↩]
- Jha SK. Cerebral Edema and its Management. Med J Armed Forces India. 2003 Oct;59(4):326-31[↩]
- Senger DR, Van de Water L, Brown LF, Nagy JA, Yeo KT, Yeo TK, Berse B, Jackman RW, Dvorak AM, Dvorak HF. Vascular permeability factor (VPF, VEGF) in tumor biology. Cancer Metastasis Rev. 1993 Sep;12(3-4):303-24[↩]
- Sorby-Adams AJ, Marcoionni AM, Dempsey ER, Woenig JA, Turner RJ. The Role of Neurogenic Inflammation in Blood-Brain Barrier Disruption and Development of Cerebral Oedema Following Acute Central Nervous System (CNS) Injury. Int J Mol Sci. 2017 Aug 17;18, 8[↩]
- Eichler AF, Chung E, Kodack DP, Loeffler JS, Fukumura D, Jain RK. The biology of brain metastases-translation to new therapies. Nat Rev Clin Oncol. 2011 Jun;8(6):344-56.[↩]
- Liang D, Bhatta S, Gerzanich V, Simard JM. Cytotoxic edema: mechanisms of pathological cell swelling. Neurosurg Focus. 2007 May 15;22(5):E2[↩]
- Lane PL, Skoretz TG, Doig G, Girotti MJ. Intracranial pressure monitoring and outcomes after traumatic brain injury. Can J Surg. 2000 Dec;43(6):442-8[↩]
- Lassen NA, Christensen MS. Physiology of cerebral blood flow. Br J Anaesth. 1976 Aug;48(8):719-34.[↩]
- Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J. Neurosurg. 1991 Nov;75(5):731-9.[↩]
- Burkert W, Paver HD. [Decompressive trepanation in therapy refractory brain edema]. Zentralbl. Neurochir. 1988;49(4):318-23.[↩]
- Strandgaard S, Paulson OB. Cerebral blood flow and its pathophysiology in hypertension. Am. J. Hypertens. 1989 Jun;2(6 Pt 1):486-92[↩]
- Pinto VL, Adeyinka A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 20, 2019. Increased Intracranial Pressure[↩]