Contents
Cerebral salt wasting syndrome
Cerebral salt wasting syndrome also called cerebral salt wasting, describe how cerebral (brain) disorders could impair your kidneys’ ability to conserve salt, resulting in salt depletion or low blood sodium level (hyponatremia, serum sodium level of less than 135 mmol/L) and extracellular fluid loss or low blood volume in the body (hypovolemia) that responds to fluid and salt replacement 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13. The term cerebral salt wasting syndrome was coined in 1950 by Peters and colleagues 1. Cerebral salt wasting syndrome is a rare but potential cause of hyponatremia (serum sodium level of less than 135 mmol/L). Cerebral salt wasting syndrome is characterized by hyponatremia, elevated urine sodium, and hypovolemia 3. Cerebral salt wasting syndrome can arise in the setting of multi-spectrum central nervous system (brain and spinal cord) pathologies, most notably due to aneurysmal subarachnoid bleeding 14. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) and cerebral salt-wasting syndrome (CSWS) are the most common causes of hyponatremia in patients with neurological problems 15, 16. However differentiating syndrome of inappropriate antidiuretic hormone secretion (SIADH) and cerebral salt-wasting syndrome (CSWS) remains difficult and the pathophysiological mechanisms underlying cerebral salt wasting are unclear 11, 13, 15, 16. In the current medical literature, scientists debate if cerebral salt-wasting syndrome (CSWS) is a distinct condition or a special form of the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) 3. The differentiation between the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) and cerebral salt-wasting syndrome (CSWS) has confused clinicians for more than 60 years as there is no consistent diagnostic criteria, no available diagnostic tests in this field, and the effective and reliable method to distinguish cerebral salt-wasting syndrome from SIADH (syndrome of inappropriate secretion of antidiuretic hormone) is limited 1, 2, 17.
In addition, SIADH and cerebral salt-wasting syndrome are two typical types of refractory hyponatremia, and the differential diagnosis between these two syndromes is difficult because of the overlapping signs, symptoms, and key laboratory data 13. Both SIADH and cerebral salt-wasting syndrome show hyponatremia, low serum osmolality, and increased urinary sodium and urine osmolality 1, 2. Besides the clinical signs and symptoms of the primary disease, the symptoms of SIADH and cerebral salt-wasting syndrome are very similar, ranging from no symptoms with mild hyponatremia to serious impairment, including muscle cramps, seizures, coma, and even death, with severe hyponatremia 18, 19.
Therefore, it is important to distinguish between cerebral salt-wasting syndrome and SIADH (syndrome of inappropriate secretion of antidiuretic hormone) as the 2 are treated with opposite treatment strategies 17, 20. For cerebral salt-wasting syndrome the patient is given fluids and sodium supplementation. For SIADH the patient is fluid restricted. Cerebral salt wasting tends to resolve within weeks to months after onset but can remain a chronic issue. Leading theories for the pathophysiology of cerebral salt wasting include the release of brain natriuretic peptide (BNP) or damage to the hypothalamus with subsequent disorder sympathetic system 11.
The cause of cerebral salt wasting is not completely understood 3. Cerebral salt wasting is most commonly seen after a central nervous system (brain and spinal cord) insult. The most commonly described precipitating insult is aneurysmal subarachnoid hemorrhage. Why cerebral salt wasting occurs more frequently after aneurysmal subarachnoid hemorrhage versus traumatic subarachnoid hemorrhage or other central nervous system (brain and spinal cord) insult is not well defined 3. Other conditions in which cerebral salt wasting has been reported include: after surgery for a pituitary tumor or acoustic neuroma or calvarial remodeling, glioma, infections including tuberculous meningitis and viral meningitis, metastatic carcinoma, and cranial trauma 3. Why cerebral salt wasting is uncommon after other injuries or diseases is also not well defined 3.
The proper diagnosis of SIADH requires the detection of urine and serum osmolality, urinary sodium, cortisol, and thyroid hormone 21. However, a recent registry analysis, including 1,524 adjudicated adult patients with SIADH from 225 sites in the United States and the European Union showed that proper and comprehensive laboratory tests are only performed in 21% of identified SIADH patients 22. Moreover, a recent study 23 supported by the Italian Endocrine Society found that less than half of clinicians surveyed were able to use validated biochemical parameters to diagnose SIADH.
The treatment of cerebral salt wasting and syndrome of inappropriate secretion of antidiuretic of hormone (SIADH) is very different, so it is critical to have the correct diagnosis prior to initiating treatment. Typically, cerebral salt wasting syndrome patient is started on isotonic saline with 0.9% sodium chloride for mild to moderate cases of hyponatremia of cerebral salt wasting 21, 3. The isotonic fluid provides the fluid for the hypovolemic patient as well as helps to restore the body’s sodium stores. For moderate to severe cases of hyponatremia, more aggressive sodium replenishment may be required with either hypertonic saline such as 3% hypertonic saline and/or salt tabs (1 to 2 grams up to three times daily) as well as limiting free water intake. Some have advocated for the use of fludrocortisone as well for the treatment of cerebral salt wasting 24.
When correcting the hyponatremia, the serum sodium should be monitored frequently. Overcorrection of the serum sodium can lead to hypernatremia (high blood sodium level) which can cause muscle twitching, lethargy, seizure, and death. Additionally, hyponatremia should not be corrected too quickly. There is the risk of central pontine myelinolysis if the hyponatremia is corrected too quickly, especially for long-standing hyponatremia. Most experts recommend correcting no more than 10 mmol/L/24 hours or 1 mmol/L every 2 hours.
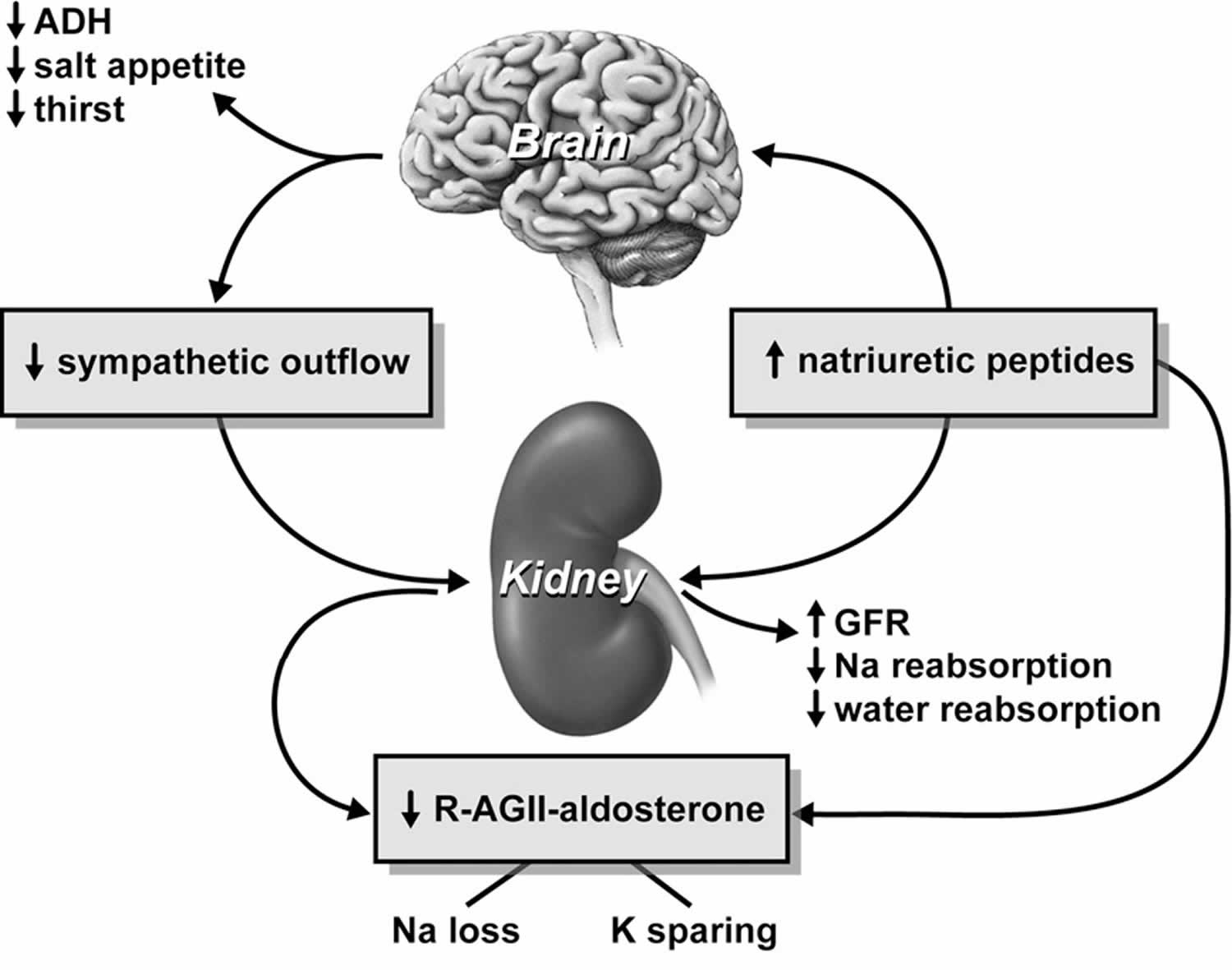
Figure 1. Cerebral salt wasting
Footnotes: Proposed mechanisms responsible for the production of cerebral salt wasting syndrome.
Abbreviations: ADH = antidiuretic hormone; GFR = glomerular filtration rate; K = potassium; Na = sodium; R-AG II = renin-angiotensin 2.
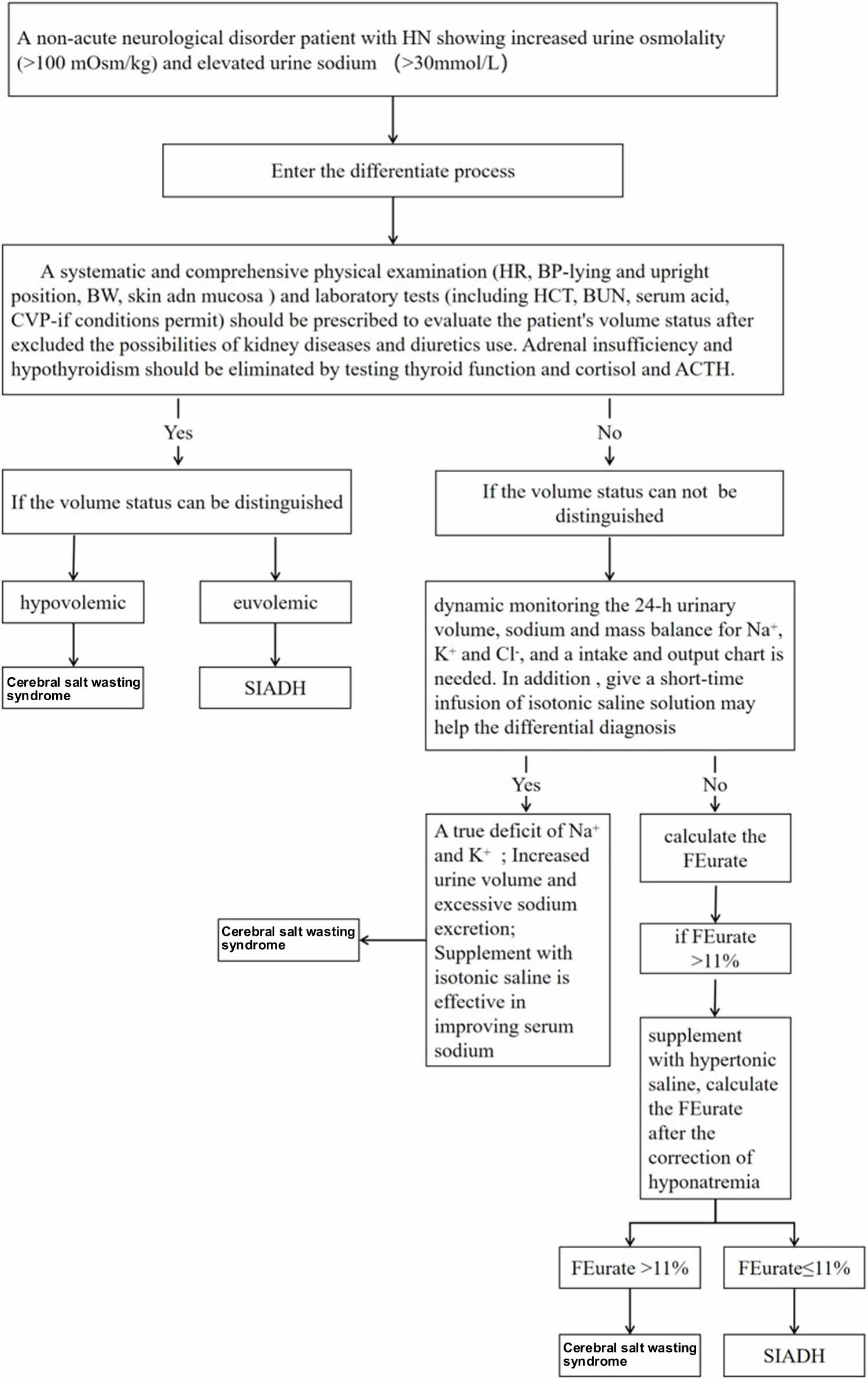
[Source 25 ]Figure 2. Cerebral salt wasting syndrome diagnosis
Footnote: The process to differentiate cerebral salt-wasting syndrome (CSWS) from syndrome of inappropriate antidiuretic hormone secretion (SIADH). The extracellular volume status of patients is a key factor to differentiate SIADH and cerebral salt wasting syndrome, despite it being difficult to evaluate in clinical practices. Instead of monitoring the urinary sodium excretion, more attention should be paid to the total mass balance, including sodium, potassium, chloride and extracellular fluid. Furthermore, the dynamic detection of fractional excretion urate (FEurate) before and after correction of hyponatremia and a short-term infusion of isotonic saline solution may be useful in identifying the cause of hyponatremia.
Abbreviations: FEurate = Fractional excretion urate
[Source 13 ]Cerebral salt wasting causes
The cause of cerebral salt wasting is not completely understood 3. Cerebral salt wasting is most commonly seen after a central nervous system (brain and spinal cord) insult. The most commonly described precipitating insult is aneurysmal subarachnoid hemorrhage. Why cerebral salt wasting occurs more frequently after aneurysmal subarachnoid hemorrhage versus traumatic subarachnoid hemorrhage or other central nervous system (brain and spinal cord) insult is not well defined 3. Other conditions in which cerebral salt wasting has been reported include: after surgery for a pituitary tumor or acoustic neuroma or calvarial remodeling, glioma, infections including tuberculous meningitis and viral meningitis, metastatic carcinoma, and cranial trauma 3. Why cerebral salt wasting is uncommon after other injuries or diseases is also not well defined 3.
Some have calculated that cerebral salt wasting accounts for up to one-quarter of severe hyponatremia after aneurysmal subarachnoid hemorrhage. The incidence of cerebral salt wasting for other central nervous system insults is mostly reported as case reports. The incidence and prevalence of cerebral salt wasting outside of patients with central nervous system insult are not reliably reported.
Cerebral salt wasting pathophysiology
The true cause of cerebral salt wasting syndrome remains an area of debate and research 3. As noted, some scientists argue cerebral salt wasting does not exist and is a form of SIADH.
There are two current theories for the cause of cerebral salt wasting syndrome: the effect of a circulating natriuretic factors such as atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) or sympathetic nervous system dysfunction 26, 27, 28, 29, 30, 31.
- Some research points to the brain releasing brain natriuretic peptide (BNP) after injury, which then enters systemic circulation through a disrupted blood-brain barrier 30. The brain natriuretic peptide (BNP) acts on the collecting ducts of the renal tubules to inhibit sodium reabsorption as well as decrease the release of renin.
- The second theory suggests that an injured sympathetic nervous system can no longer promote sodium reabsorption and stimulate renin and aldosterone release due to injury to the hypothalamus 31. The exact mechanism of cerebral salt wasting remains open to debate.
Cerebral salt wasting symptoms
The most common presenting symptom for cerebral salt wasting syndrome is hyponatremia after aneurysmal subarachnoid hemorrhage 9. Cerebral salt wasting has also been reported after surgery of the central nervous system including pituitary surgery, vestibular schwannoma resection, and calvarial remodeling. Additionally, cerebral salt wasting has been seen after a head injury, intracranial malignancy, and central nervous system (CNS) infections.
A subarachnoid hemorrhage is bleeding in the space between the brain and the surrounding membrane (subarachnoid space). The primary symptom is a sudden, severe headache often called thunderclap headache. It is often worse near the back of the head. Many people often describe it as the “worst headache ever” and unlike any other type of headache pain. The headache may start after a popping or snapping feeling in the head.
Along with having a headache, some people may experience:
- Nausea
- Vomiting
- Stiff neck
- Problems with vision
- Brief loss of consciousness
- Decreased consciousness and alertness
- Eye discomfort in bright light (photophobia)
- Mood and personality changes, including confusion and irritability
- Muscle aches (especially neck pain and shoulder pain)
- Nausea and vomiting
- Numbness in part of the body
- Seizure
- Stiff neck
- Vision problems, including double vision, blind spots, or temporary vision loss in one eye
- Eyelid drooping
- Pupil size difference
- Sudden stiffening of back and neck, with arching of the back (opisthotonos; not very common)
A few days after the aneurysmal subarachnoid hemorrhage the patient’s serum sodium begins to drop while the urine sodium increases. The patient’s fluid status also decreases, and the patient becomes hyponatremia and hypovolemic. With treatment, the cerebral salt wasting resolves within a few weeks to months, and long-term treatment is not commonly required.
Hyponatremia signs and symptoms may include:
- Nausea and vomiting
- Headache
- Problems with balance that may result in falls
- Mental changes, such as confusion, memory problems, strange behavior
- Loss of energy, drowsiness and fatigue
- Restlessness and irritability
- Muscle weakness, spasms or cramps
- Seizures or coma in severe cases.
The earliest signs and symptoms of acute hyponatremia include nausea and malaise, which may be seen when the serum sodium concentration falls below 125 to 130 mmol/L (normal 135 to 145 mmol/L) 32. Vomiting is an ominous sign for patients with acute hyponatremia. With a more severe and acute fall in sodium concentration, headache, lethargy, obtundation, and eventually, seizures can occur. Coma and respiratory arrest can occur if the serum sodium level falls below 115 to 120 mmol/L. Acute hyponatremia encephalopathy may be reversible, but permanent neurologic damage or death can occur, particularly in premenopausal women.
Chronic hyponatremia allows brain adaptation, and the patients remain asymptomatic despite a serum sodium concentration below 120 mmol/L. Nonspecific symptoms like nausea, vomiting, gait disturbances, memory, cognitive problems, fatigue, dizziness, confusion, and muscle cramps can occur with chronic hyponatremia. Sign and symptoms or mild and chronic hyponatremia are often subtle and missed during the history and physical examination. Nausea and vomiting affect approximately one-third of patients with chronic hyponatremia who have a serum sodium concentration of less than 120 mmol/L.
Cerebral salt wasting diagnosis
It is critically important to distinguish cerebral salt wasting syndrome from the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) as the treatments are opposite. Evaluation for cerebral salt wasting begins with a basic metabolic panel that includes blood sodium to identify the hyponatremia (serum sodium less than 135 mmol/L). Urine studies are commonly checked for urine sodium and osmolality. Urine sodium is typically elevated above 40 mmol/L. Urine osmolality is elevated above 100 mosmol/kg. The patient must also have signs or symptoms of hypovolemia such as hypotension, decreased central venous pressure, lack of skin turgor, or elevated hematocrit.
Lab tests that can confirm and help diagnose low sodium include:
- Comprehensive metabolic panel (includes blood sodium)
- Serum osmolality and serum sodium
- Urine sodium concentration and osmolality
- Urine potassium
- Toxicology screens for certain medicines
- Renal function tests: BUN and creatinine
- BSR (Blood sugar random)
- Thyroid profile
- Serum cortisol
- Serum K+, bicarbonate, chloride
- Fasting lipid profile
- Liver function tests
- Blood tests to check for bleeding disorders
Since cerebral salt wasting syndrome was not well-defined and the diagnostic criteria are complicated, Misra et al 33 presented a simplified bedside criteria and the cerebral salt wasting syndrome was considered in the presence of at least two out of four following features in a patient with hyponatremia:
- clinical findings of hypovolemia, such as hypotension, dry mucous membranes, tachycardia, or postural hypotension;
- laboratory evidence of dehydration, such as elevated hematocrit, hemoglobin, serum albumin, or blood urea nitrogen;
- negative fluid balance as determined by intake output chart and/or weight loss;
- central venous pressure (CVP) less than 6 cm of water.
The most important criterion is the extracellular volume status 34. The state of extracellular volume is one of the factors that may help in distinguishing the two situations, being normal or increased volemia in SIADH and hypovolemic in cerebral salt wasting syndrome 13.
Syndrome of inappropriate secretion of antidiuretic of hormone (SIADH) will have a similar laboratory picture as cerebral salt wasting with hyponatremia and increased urine sodium. However, with SIADH, the patient is euvolemic to hypervolemic from the retained free water as compared to the hypovolemic picture of cerebral salt wasting 35, 24.
Arieff et al. 36 also indicated that in patients with hyponatremia complicated with a cerebral lesion, the detection of urine volume and sodium excretion is critical. Therefore, intake-output chart may help in differentiating cerebral salt wasting syndrome from SIADH; in addition, polyuria and negative fluid balance from a chart is a feasible bedside measure. Patients with cerebral salt wasting syndrome manifested markedly elevated urine volume and sodium excretion when compared to SIADH. The elevated urine sodium excretion may reflect the balance of sodium in the body to some extent; nevertheless, to determine whether there is a true deficit of sodium, mass balances rather than excretion rates of sodium should be detected 37, and mass balance for sodium and potassium rather than just for sodium should be included since sodium may enter into cells in conjunction with potassium exit. Cerebral salt-wasting syndrome is a common exclusion of diagnosis; overall balances including sodium, potassium, chloride and extracellular fluid must be evaluated, and the diagnosis should not be made in a patient without a true deficit of sodium and potassium 13.
Previous studies found that serum uric acid levels are generally decreased and fractional excretion (FE) urate is increased in both SIADH and cerebral salt wasting syndrome; however, hypouricemia increased and still showed in cerebral salt wasting syndrome but not in SIADH after the correction of hyponatremia 2, 38. Researchers found that V1 receptor stimulation may play a central role in inducing hypouricemia in SIADH; however, the mechanism of increased fractional excretion (FE) urate in cerebral salt wasting syndrome remains unclear39.
Fractional excretion (FE) urate can be calculated with simultaneous blood and urine collection by the following standard formula 18:
- Fractional excretion (FE) urate = Uurate/Surate ÷ UCr/SCr × 100
Abbreviations: U = urine, S = serum, and Cr = creatinine
Normal value of FEurate is about 4–11%. It is suggested that FEurate can be used in the algorithm to differentiate SIADH from cerebral salt wasting syndrome 18, 40. In most cases, the level of FEurate is more than 11%, and in SIADH, correction of hyponatremia will normalize FEurate to 4–11%; in contrast, it will continue to rise to higher than 11% in cerebral salt wasting syndrome (see Table 2). Consequently, the dynamic detection of FEurate may be a feasible method to identify the etiology for patients with intractable hyponatremia.
Other potential causes of hyponatremia should also be sought including diarrhea, vomiting, sweating, polydipsia, kidney diseases, advanced liver disease, heart failure, hypothyroidism (low levels of thyroid hormone), heart failure, cancer, Addison’s disease, hormone deficiency, pseudohyponatremia, recreational drug ecstasy and use of diuretic medicines (water pills), which increase urine output and loss of sodium through the urine. Many times cerebral salt wasting becomes a diagnosis of exclusion after labs reveal serum hyponatremia with increased urine sodium levels.
To diagnose a subarachnoid hemorrhage, your doctor is likely to recommend:
- CT scan. This imaging test can detect bleeding in the brain. While a CT scan is a highly effective test when performed properly, the scan may not find the bleed if you have a low red blood cell count (anemia) and only a small amount of blood is lost during the bleed. Your doctor may inject a contrast dye to view your blood vessels in greater detail (CT angiogram).
- Magnetic resonance imaging (MRI). This imaging test also can detect bleeding in the brain. Your doctor might inject a dye into a blood vessel to view the arteries and veins in greater detail (MR angiogram) and to highlight blood flow. This may show signs of a subarachnoid hemorrhage in rare cases when the signs don’t show on a CT scan.
- Cerebral angiography. You doctor inserts a long, thin tube (catheter) into an artery and threads it to your brain. Dye is injected into the blood vessels of your brain to make them visible under X-ray imaging. Your provider might recommend cerebral angiography to get more-detailed images. They may also recommend the test if a subarachnoid hemorrhage is suspected, but the cause isn’t clear or doesn’t appear on other imaging. You might need a second cerebral angiogram if the first one did not show an aneurysm, but your doctor thinks an aneurysm is likely.
- Transcranial Doppler ultrasound, to look at blood flow in the arteries of the brain
In some cases of aneurysmal subarachnoid hemorrhages, the bleeding may not appear on initial imaging. If your first CT scan doesn’t show bleeding, your doctor might recommend lumbar puncture. A needle is inserted into the lower back to withdraw a small amount of the fluid that surrounds the brain and spinal cord (cerebrospinal fluid). The fluid is studied to look for blood, which may mean that you have a subarachnoid hemorrhage.
Table 1. Comparison of the clinical and laboratory indicators of cerebral salt wasting syndrome and SIADH
| SIADH (syndrome of inappropriate antidiuretic hormone secretion) | Cerebral salt-wasting syndrome | Affect factors and limitations of clinical utility | |
|---|---|---|---|
| Related to blood volume | |||
| Blood pressure | Normal/increased | Decreased/orthopedic hypotension | Stress state; measurement error |
| Heart rate | Normal | Increased | Nutrition state, history of liver disease |
| Body weight | Normal/increased | Decreased | Bed rest >1 week; caloric intake 41 |
| Blood urea nitrogen (BUN) | Normal/decreased | Increased | Caloric intake |
| Albumin | Normal | Increased | Nutrition state, history of liver disease |
| Hematocrit (Hct) | Normal | Increased | Anemia; history of chronic heart and lung disease |
| Wedge pressure | Normal/slightly | Decreased | History of heart disease; invasive method |
| Central venous pressure (CVP) | Normal/slightly increased | Decreased | Intrathoracic pressure, inotropic efficacy, and compliance of the venous system 42; invasive method |
| Serum uric acid concentration | Decrease | Decrease | Purines intake; renal function; history of hyperuricemia |
| Skin and mucosa | Normal | Dry | Subjective factor; age-related changes; status of nutrition |
| Related to sodium balance | |||
| Urine volume | Normal/decrease | High | The administration of diuretics or antihypertensives; age; change in volume status |
| Urine sodium concentration | >30 mmol/L | >>30 mmol/L | Supplement of sodium; the administration of diuretics |
| Brain natriuretic peptide (BNP) | Normal | Increased | History of heart and lung disease; age related; stress state |
Table 2. Changes of fractional excretion urate in SIADH and cerebral salt wasting syndrome after correction of hyponatremia
| Fractional excretion urate (normal value 4–11%) | Cerebral salt wasting syndrome | SIADH |
|---|---|---|
| Before correction of hyponatremia | >11% | >11% |
| After correction of hyponatremia | >11% | 4–11% |
Cerebral salt wasting differential diagnosis
It is critical to distinguish between cerebral salt wasting and the syndrome of inappropriate secretion of antidiuretic hormone (SIADH). Both conditions are characterized by hyponatremia with elevated urine sodium, concentrated urine, and no edema. The key distinguishing factor is that in cerebral salt wasting the patient is hypovolemic versus in SIADH the patient is euvolemic to hypervolemic 35, 13. Patients with cerebral salt wasting showed excessive water and sodium excretion by the kidney, whereas patients with SIADH showed increased water retention by the kidney. Hyponatremia secondary to SIADH is a result of water retention due to dysregulated release of antidiuretic hormone (ADH) 43 or gain-of-function mutations in the V2 vasopressin receptor in renal collecting tubules 2, 44. Cerebral salt wasting syndrome is characterized by hyponatremia and volume depletion 45.
The differential diagnosis of the cause of cerebral salt wasting syndrome is:
- Head injury
- Brain tumor
- Stroke
- Intracranial surgery
- Intracerebral hemorrhage
- Craniosynostosis repair
- Tuberculous meningitis
Cerebral salt wasting management
The treatment of cerebral salt wasting and syndrome of inappropriate secretion of antidiuretic of hormone (SIADH) is very different, so it is critical to have the correct diagnosis prior to initiating treatment.
Cerebral salt wasting syndrome typically occurs after aneurysmal subarachnoid hemorrhage, the first treatment strategies are targeted at treating the underlying subarachnoid hemorrhage and aneurysm or another central nervous system (CNS) insult. The treatment focuses on stabilizing your condition, treating an aneurysm if you have one, and preventing complications. Your doctor will check your breathing, blood pressure, and blood flow.
If your subarachnoid bleeding is caused by a ruptured brain aneurysm, your doctor might recommend:
- Surgery. The surgeon makes an incision in the scalp and locates the brain aneurysm. A metal clip is placed on the aneurysm to stop the blood flow to it.
- Endovascular embolization. The surgeon inserts a catheter into an artery and threads it to your brain. Detachable platinum coils are guided through the catheter and placed in the aneurysm. The coils fill the aneurysm, reducing blood flow into the aneurysm sac and causing the blood to clot. Different types of coils have been developed to treat various aneurysms.
- Other endovascular treatments. Certain aneurysms can be treated with endovascular embolization that uses newer technology such as stent-assisted or balloon-assisted coiling or devices that divert blood flow.
Preventing complications is important because you can bleed again, have poor blood flow to the brain, have low sodium in your blood (hyponatremia), develop too much fluid on the brain (hydrocephalus), or have high or low blood sugar. One medication, nimodipine (Nymalize) has been shown to decrease circulation problems to the brain after a subarachnoid hemorrhage.
A common complication after an aneurysmal subarachnoid hemorrhage is delayed spasm of the blood vessels in the brain. This can cause stroke if it reduces the blood flow below a certain level. When this complication occurs, strokes may be avoided by raising the blood pressure with intravenous medications or increasing the width of the blood vessels in the brain with medications.
Another common complication is hydrocephalus which is an accumulation of fluid in brain spaces. This problem can be treated with drains inserted in the head (ventriculostomy catheter) or in the lower back (lumbar drains).
Sometimes, procedures need to be repeated. You’ll have regular follow-up appointments with your doctor to watch for any changes. You may also need physical, occupational and speech therapy.
Secondly, your extracellular fluid loss or low blood volume in the body (hypovolemia) must be volume repleted while treating the hyponatremia. Typically, cerebral salt wasting syndrome patient is started on isotonic saline with 0.9% sodium chloride for mild to moderate cases of hyponatremia of cerebral salt wasting 21, 3. The isotonic fluid provides the fluid for the hypovolemic patient as well as helps to restore the body’s sodium stores. For moderate to severe cases of hyponatremia, more aggressive sodium replenishment may be required with either hypertonic saline such as 3% hypertonic saline and/or salt tabs (1 to 2 grams up to three times daily) as well as limiting free water intake. Some have advocated for the use of fludrocortisone as well for the treatment of cerebral salt wasting 24.
When correcting the hyponatremia, the serum sodium should be monitored frequently. Overcorrection of the serum sodium can lead to hypernatremia (high blood sodium level) which can cause muscle twitching, lethargy, seizure, and death. Additionally, hyponatremia should not be corrected too quickly. There is the risk of central pontine myelinolysis if the hyponatremia is corrected too quickly, especially for long-standing hyponatremia. Most experts recommend correcting no more than 10 mmol/L/24 hours or 1 mmol/L every 2 hours.
Fludrocortisone, as a type of mineralocorticoid hormone, has been reported to effectively control sodium excretion in the urine (natriuresis) 46. This hormone was first reported for the treatment of cerebral salt wasting syndrome in the 1980s in three elderly patients with head injury. As a result, all three patients responded well to fludrocortisone therapy 47. Single reports of its administration in cerebral salt wasting syndrome patients have appeared sporadically 48, 49, 50, 51. Following the treatment of fluid and salt replacement, mineralocorticoid supplement also seems to be a safe and effective treatment for cerebral salt wasting syndrome. Misra et al. 52 conducted a recent randomized clinical trial and provided class 2 evidence on the role of fludrocortisone in the treatment of hyponatremia related to cerebral salt wasting syndrome in tuberculous meningitis patients. The results suggested that fludrocortisone (at an oral dose of 0.1–0.4 mg per day and starts with a small dose) may lead to earlier normalization of serum sodium levels, without affecting outcomes at 6 months, and the results are consistent with those of a randomized clinical trial in subarachnoid hemorrhage patients with cerebral salt wasting syndrome 53.
The most important issue is to distinguish between cerebral salt wasting and syndrome of inappropriate secretion of antidiuretic of hormone (SIADH) as they are treated with opposite approaches. In cases of SIADH, the treatment is typically fluid restriction, hypertonic saline, demeclocycline, and/or furosemide. However, if fluid restriction may be insufficient or impractical. Tolvaptan, an oral vasopressin V2-receptor antagonist, might be an attractive option for correcting the hyponatremia due to SIADH 21. The SALT-1 and SALT-2 trials have shown that serum sodium can be safely improved at day 4 and 30 by the administration of tolvaptan in patients with SIADH 54. The role of tolvaptan in the treatment of SIADH is indisputable; however, the cost of therapy and the need for long-term safety data may limit its widespread use. Therefore, several precautions are needed for using tolvaptan: (1) Tolvaptan should be initiated at a small dose and should not be used in conjunction with fluid restriction. In addition, it is important to monitor the serum sodium closely (recommended every 4–6 hours after starting treatment) in case of an overly rapid correction 55, 56. It is recommended to test liver function before the administration of tolvaptan due to its potential liver toxicity with chronic use 57. Tolvaptan may serve as a double-sided sword because of its high risk of rapid correction of hyponatremia and the potential liver toxicity. However, giving a bolus of saline is beneficial before restriction of fluid or challenging with tolvaptan 55.
If the patient truly has cerebral salt wasting, they are hypovolemic, and the SIADH treatment modalities would be detrimental by exacerbating the hypovolemia 58, 59, 60.
Cerebral salt wasting prognosis
Cerebral salt wasting prognosis or outcomes for most patients not due to a subarachnoid hemorrhage are good. However, some patients may continue to have mild neurological deficits despite optimal treatment 61, 62.
- Peters J. P., Welt L. G., Sims E. A., Orloff J., Needham J. (1950). A salt-wasting syndrome associated with cerebral disease. Trans. Assoc. Am. Phys. 63, 57–64.[↩][↩][↩][↩]
- Schwartz W. B., Bennett W., Curelop S., Bartter F. C. (1957). A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am. J. Med. 23, 529–542. 10.1016/0002-9343(57)90224-3[↩][↩][↩][↩][↩]
- Tenny S, Thorell W. Cerebral Salt Wasting Syndrome. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534855[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Saha U, Hassan A, Zaman CF, Afroz S, Faruq R. Hiccup: The Striking Manifestation of Hyponatremia Due to Ischemic Stroke-Induced Cerebral Salt Wasting Syndrome (CSWS). Cureus. 2022 Sep 28;14(9):e29677. doi: 10.7759/cureus.29677[↩]
- Daghmouri MA, Ouesleti M, Touati MA, Faten O, Zakhama S, Rebai L. Cerebral Salt Wasting Syndrome Caused by Severe Traumatic Brain Injury in a Pediatric Patient and Review of the Literature. Case Rep Crit Care. 2021 Oct 22;2021:6679279. doi: 10.1155/2021/6679279[↩]
- Liangos O, Madias NE. Severe symptomatic hyponatremia due to cerebral salt wasting syndrome in a patient with traumatic head injury and Dandy-Walker malformation of the brain. Clin Nephrol Case Stud. 2021 Feb 19;9:4-10. doi: 10.5414/CNCS110146[↩]
- Costa MM, Esteves C, Castedo JL, Pereira J, Carvalho D. A challenging coexistence of central diabetes insipidus and cerebral salt wasting syndrome: a case report. J Med Case Rep. 2018 Jul 17;12(1):212. doi: 10.1186/s13256-018-1678-z[↩]
- Lin YL, Hung KL, Lo CW. Mycoplasma pneumoniae-associated encephalitis complicated by cerebral salt wasting syndrome. Clin Case Rep. 2017 Sep 26;5(11):1830-1833. doi: 10.1002/ccr3.1192[↩]
- Cerdà-Esteve M, Cuadrado-Godia E, Chillaron JJ, Pont-Sunyer C, Cucurella G, Fernández M, Goday A, Cano-Pérez JF, Rodríguez-Campello A, Roquer J. Cerebral salt wasting syndrome: review. Eur J Intern Med. 2008 Jun;19(4):249-54. doi: 10.1016/j.ejim.2007.06.019[↩][↩]
- Attout H, Guez S, Seriès C. Syndrome de perte de sel d’origine cérébrale avec hyponatrémie au cours d’une méningite bactérienne [Cerebral salt wasting syndrome in bacterial meningitis]. Ann Endocrinol (Paris). 2007 Oct;68(5):395-7. French. doi: 10.1016/j.ando.2007.06.025[↩]
- Leonard J, Garrett RE, Salottolo K, Slone DS, Mains CW, Carrick MM, Bar-Or D. Cerebral salt wasting after traumatic brain injury: a review of the literature. Scand J Trauma Resusc Emerg Med. 2015 Nov 11;23:98. doi: 10.1186/s13049-015-0180-5[↩][↩][↩]
- Harrigan MR. Cerebral salt wasting syndrome: a review. Neurosurgery. 1996 Jan;38(1):152-60. doi: 10.1097/00006123-199601000-00035[↩]
- Cui H, He G, Yang S, Lv Y, Jiang Z, Gang X, Wang G. Inappropriate Antidiuretic Hormone Secretion and Cerebral Salt-Wasting Syndromes in Neurological Patients. Front Neurosci. 2019 Nov 8;13:1170. doi: 10.3389/fnins.2019.01170[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Ramirez FC, Graham DY. Hiccups, compulsive water drinking, and hyponatremia. Ann Intern Med. 1993 Apr 15;118(8):649. doi: 10.7326/0003-4819-118-8-199304150-00020[↩]
- Kalita J., Singh R. K., Misra U. K. (2017). Cerebral salt wasting is the most common cause of hyponatremia in stroke. J. Stroke Cerebrovasc. Dis. 26, 1026–1032. 10.1016/j.jstrokecerebrovasdis.2016.12.011[↩][↩]
- Moritz M. L. (2019). Syndrome of inappropriate antidiuresis. Pediatr. Clin. North Am. 66, 209–226. 10.1016/j.pcl.2018.09.005[↩][↩]
- Cuesta M., Hannon M. J., Thompson C. J. (2016). Diagnosis and treatment of hyponatraemia in neurosurgical patients. Endocrinol. Nutr. 63, 230–238. 10.1016/j.endonu.2015.12.007[↩][↩]
- Maesaka J. K., Imbriano L., Mattana J., Gallagher D., Bade N., Sharif S. (2014). Differentiating SIADH from cerebral/renal salt wasting: failure of the volume approach and need for a new approach to hyponatremia. J. Clin. Med. 3, 1373–1385. 10.3390/jcm3041373[↩][↩][↩]
- Monig H., Arlt A. (2017). Hyponatremia: differential diagnosis and treatment. Dtsch. Med. Wochenschr. 142, 1231–1247. 10.1055/s-0043-108953[↩]
- Maesaka J. K., Imbriano L. J., Miyawaki N. (2018). High prevalence of renal salt wasting without cerebral disease as cause of hyponatremia in general medical wards. Am. J. Med. Sci. 356, 15–22. 10.1016/j.amjms.2018.03.020[↩]
- Spasovski G., Vanholder R., Allolio B., Annane D., Ball S., Bichet D., et al.. (2014). Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol. Dial. Transplant. 29 (Suppl. 2), i1–i39. 10.1093/ndt/gfu040[↩][↩][↩][↩]
- Greenberg A, Verbalis JG, Amin AN, Burst VR, Chiodo JA 3rd, Chiong JR, Dasta JF, Friend KE, Hauptman PJ, Peri A, Sigal SH. Current treatment practice and outcomes. Report of the hyponatremia registry. Kidney Int. 2015 Jul;88(1):167-77. doi: 10.1038/ki.2015.4[↩]
- Giuliani C, Cangioli M, Beck-Peccoz P, Faustini-Fustini M, Fiaccadori E, Peri A. Awareness and management of hyponatraemia: the Italian Hyponatraemia Survey. J Endocrinol Invest. 2013 Oct;36(9):693-8. doi: 10.3275/8925[↩]
- Yee AH, Burns JD, Wijdicks EF. Cerebral salt wasting: pathophysiology, diagnosis, and treatment. Neurosurg Clin N Am. 2010 Apr;21(2):339-52. doi: 10.1016/j.nec.2009.10.011[↩][↩][↩]
- Yee AH, Burns JD, Wijdicks EF. Cerebral salt wasting: pathophysiology, diagnosis, and treatment. Neurosurg Clin N Am. 2010 Apr;21(2):339-52. https://doi.org/10.1016/j.nec.2009.10.011[↩]
- Yee AH, Burns JD, Wijdicks EF. Cerebral salt wasting: pathophysiology, diagnosis, and treatment. Neurosurg Clin N Am (2010) 21(2):339–52. 10.1016/j.nec.2009.10.011[↩]
- Rabinstein AA, Wijdicks EF. Hyponatremia in critically ill neurological patients. Neurologist (2003) 9(6):290–300 10.1097/01.nrl.0000095258.07720.89[↩]
- Kim DK, Joo KW. Hyponatremia in patients with neurologic disorders. Electrolyte Blood Press (2009) 7(2):51–7. 10.5049/ebp.2009.7.2.51[↩]
- Steele MK, Gardner DG, Xie PL, Schultz HD. Interactions between ANP and ANG II in regulating blood pressure and sympathetic outflow. Am J Physiol. 1991 Jun;260(6 Pt 2):R1145-51. doi: 10.1152/ajpregu.1991.260.6.R1145[↩]
- Berendes E., Walter M., Cullen P., Prien T., Van Aken H., Horsthemke J., et al.. (1997). Secretion of brain natriuretic peptide in patients with aneurysmal subarachnoid haemorrhage. Lancet. 349, 245–249. 10.1016/S0140-6736(96)08093-2[↩][↩]
- Bitew S., Imbriano L., Miyawaki N., Fishbane S., Maesaka J. K. (2009). More on renal salt wasting without cerebral disease: response to saline infusion. Clin. J. Am. Soc. Nephrol. 4, 309–315. 10.2215/CJN.02740608[↩][↩]
- Yasir M, Mechanic OJ. Syndrome of Inappropriate Antidiuretic Hormone Secretion. [Updated 2023 Mar 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507777[↩]
- Misra U. K., Kalita J., Bhoi S. K., Singh R. K. (2016). A study of hyponatremia in tuberculous meningitis. J. Neurol. Sci. 367, 152–157. 10.1016/j.jns.2016.06.004[↩]
- Harrigan MR. Cerebral salt wasting syndrome. Crit Care Clin. 2001 Jan;17(1):125-38. doi: 10.1016/s0749-0704(05)70155-x[↩]
- Oh JY, Shin JI. Syndrome of inappropriate antidiuretic hormone secretion and cerebral/renal salt wasting syndrome: similarities and differences. Front Pediatr. 2015 Jan 22;2:146. doi: 10.3389/fped.2014.00146[↩][↩]
- Arieff A. I., Gabbai R., Goldfine I. D. (2017). Cerebral salt-wasting syndrome: diagnosis by urine sodium excretion. Am. J. Med. Sci. 354, 350–354. 10.1016/j.amjms.2017.05.007[↩]
- Carlotti A. P., Bohn D., Mallie J. P., Halperin M. L. (2001). Tonicity balance, and not electrolyte-free water calculations, more accurately guides therapy for acute changes in natremia. Intensive Care Med. 27, 921–924. 10.1007/s001340100911[↩]
- Maesaka J. K., Imbriano L. J., Ali N. M., Ilamathi E. (2009). Is it cerebral or renal salt wasting? Kidney Int. 76, 934–938. 10.1038/ki.2009.263[↩]
- Taniguchi K., Tamura Y., Kumagai T., Shibata S., Uchida S. (2016). Stimulation of V1a receptor increases renal uric acid clearance via urate transporters: insight into pathogenesis of hypouricemia in SIADH. Clin. Exp. Nephrol. 20, 845–852. 10.1007/s10157-016-1248-x[↩]
- Sonnenblick M, Rosin A. Increased uric acid clearance in the syndrome of inappropriate secretion of antidiuretic hormone. Isr J Med Sci. 1988 Jan;24(1):20-3.[↩]
- Greenleaf J. E., Bernauer E. M., Young H. L., Morse J. T., Staley R. W., Juhos L. T., et al.. (1977). Fluid and electrolyte shifts during bed rest with isometric and isotonic exercise. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 42, 59–66. 10.1152/jappl.1977.42.1.59[↩]
- Shippy C. R., Appel P. L., Shoemaker W. C. (1984). Reliability of clinical monitoring to assess blood volume in critically ill patients. Crit. Care Med. 12, 107–112. 10.1097/00003246-198402000-00005[↩]
- Zerbe R., Stropes L., Robertson G. (1980). Vasopressin function in the syndrome of inappropriate antidiuresis. Annu. Rev. Med. 31, 315–327. 10.1146/annurev.me.31.020180.001531[↩]
- Robertson G. L. (2006). Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am. J. Med. 119, S36–42. 10.1016/j.amjmed.2006.05.006[↩]
- Harrigan M. R. (2001). Cerebral salt wasting syndrome. Crit. Care Clin. 17, 125–138. 10.1016/S0749-0704(05)70155-X[↩]
- Sakarcan A., Bocchini J., Jr. (1998). The role of fludrocortisone in a child with cerebral salt wasting. Pediatr. Nephrol. 12, 769–771. 10.1007/s004670050543[↩]
- Ishikawa S. E., Saito T., Kaneko K., Okada K., Kuzuya T. (1987). Hyponatremia responsive to fludrocortisone acetate in elderly patients after head injury. Ann. Intern. Med. 106, 187–191. 10.7326/0003-4819-106-2-187[↩]
- Berendes E., Scherer R., Schuricht G., Rol R., Hengst K. (1992). Massive natriuresis and polyuria after triple craniocervical subarachnoid hemorrhage: cerebral salt wasting syndrome? Anasthesiol. Intensivmed. Notfallmed. Schmerzther. 27, 445–448. 10.1055/s-2007-1000333[↩]
- Kinik S. T., Kandemir N., Baykan A., Akalan N., Yordam N. (2001). Fludrocortisone treatment in a child with severe cerebral salt wasting. Pediatr. Neurosurg. 35, 216–219. 10.1159/000050424[↩]
- Lee P., Jones G. R., Center J. R. (2008). Successful treatment of adult cerebral salt wasting with fludrocortisone. Arch. Intern. Med. 168, 325–326. 10.1001/archinternmed.2007.126[↩]
- Gurnurkar S., Villacres S., Warner L., Chegondi M. (2018). Successful use of fludrocortisone in a child with refractory cerebral salt wasting syndrome: a case report and review of literature. Cureus 10:e3505. 10.7759/cureus.3505[↩]
- Misra U. K., Kalita J., Kumar M. (2018b). Safety and efficacy of fludrocortisone in the treatment of cerebral salt wasting in patients with tuberculous meningitis: a randomized clinical trial. JAMA Neurol. 75, 1383–1391. 10.1001/jamaneurol.2018.2178[↩]
- Hasan D., Lindsay K. W., Wijdicks E. F., Murray G. D., Brouwers P. J., Bakker W. H., et al.. (1989). Effect of fludrocortisone acetate in patients with subarachnoid hemorrhage. Stroke. 20, 1156–1161. 10.1161/01.STR.20.9.1156[↩]
- Schrier R. W., Gross P., Gheorghiade M., Berl T., Verbalis J. G., Czerwiec F. S., et al.. (2006). Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N. Engl. J. Med. 355, 2099–2112. 10.1056/NEJMoa065181[↩]
- Cuesta M., Thompson C. J. (2016). The syndrome of inappropriate antidiuresis (SIAD). Best Pract. Res. Clin. Endocrinol. Metab. 30, 175–187. 10.1016/j.beem.2016.02.009[↩][↩]
- Thajudeen B., Salahudeen A. K. (2016). Role of tolvaptan in the management of hyponatremia in patients with lung and other cancers: current data and future perspectives. Cancer Manag. Res. 8, 105–114. 10.2147/CMAR.S90169[↩]
- Peri A, Giuliani C. Management of euvolemic hyponatremia attributed to SIADH in the hospital setting. Minerva Endocrinol. 2014 Mar;39(1):33-41. https://www.minervamedica.it/en/journals/minerva-endocrinology/article.php?cod=R07Y2014N01A0033[↩]
- Jin S, Long Z, Wang W, Jiang B. Hyponatremia in neuromyelitis optica spectrum disorders: Literature review. Acta Neurol Scand. 2018 Jul;138(1):4-11. doi: 10.1111/ane.12938[↩]
- Moritz ML. Syndrome of Inappropriate Antidiuresis. Pediatr Clin North Am. 2019 Feb;66(1):209-226. doi: 10.1016/j.pcl.2018.09.005[↩]
- Maesaka JK, Imbriano LJ, Miyawaki N. High Prevalence of Renal Salt Wasting Without Cerebral Disease as Cause of Hyponatremia in General Medical Wards. Am J Med Sci. 2018 Jul;356(1):15-22. doi: 10.1016/j.amjms.2018.03.020[↩]
- John CA, Day MW. Central neurogenic diabetes insipidus, syndrome of inappropriate secretion of antidiuretic hormone, and cerebral salt-wasting syndrome in traumatic brain injury. Crit Care Nurse. 2012 Apr;32(2):e1-7; quiz e8. doi: 10.4037/ccn2012904[↩]
- Rahman M, Friedman WA. Hyponatremia in neurosurgical patients: clinical guidelines development. Neurosurgery. 2009 Nov;65(5):925-35; discussion 935-6. doi: 10.1227/01.NEU.0000358954.62182.B3[↩]