Contents
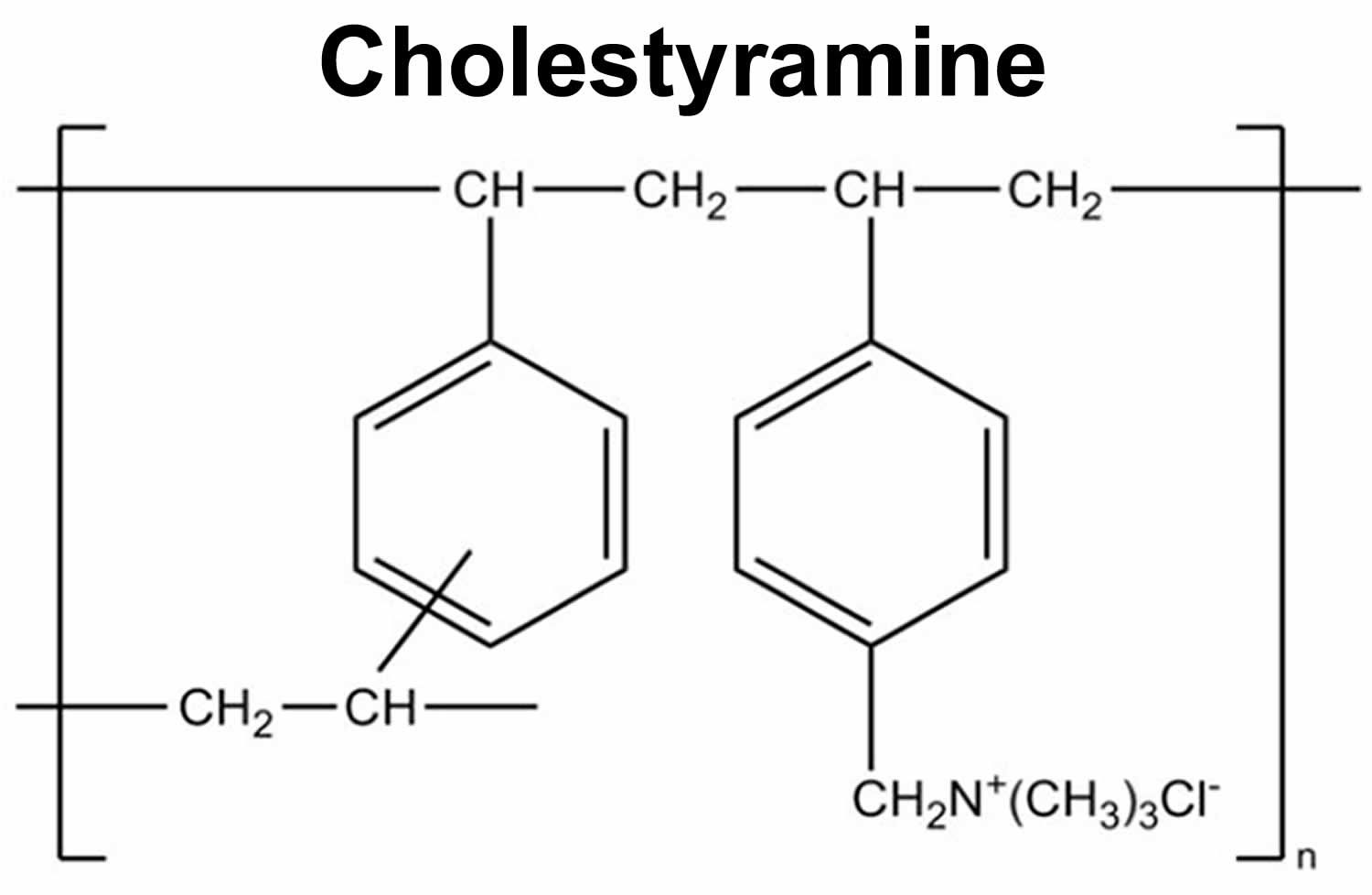
What is cholestyramine
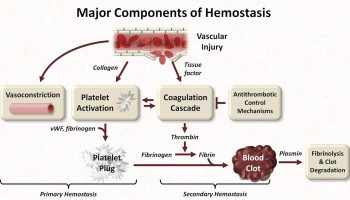
Cholestyramine is an anion exchange resin with cholesterol lowering activity. Cholestyramine works by blocking bile acid in your stomach from being absorbed into your blood. Your liver then needs the cholesterol from your blood to make more bile acid. This reduces your cholesterol level. Lowering your blood level of cholesterol and fats may help to prevent heart disease, angina (chest pain), strokes, and heart attacks. Cholestyramine is a nonabsorbed bile acid sequestrant that is used to treat high cholesterol (hyperlipidemia or hypercholesterolemia) and for the pruritus of chronic liver disease and biliary obstruction. Cholestyramine resin adsorbs and combines with bile acids in your intestine to form an insoluble complex, which is then excreted in the feces, resulting in an increased oxidation of cholesterol to bile acids, that help lower your LDL (bad) cholesterol and decrease your blood cholesterol levels.
Cholestyramine also may help people with type 2 diabetes manage their blood sugar.
Cholestyramine has been associated with mild and transient serum enzyme elevations during therapy, but has not been linked to cases of clinically apparent liver injury with jaundice.
High cholesterol is associated with an increased risk of heart disease and atherosclerosis (clogged arteries).
Improving your cholesterol levels can help protect you from:
- Heart disease
- Heart attack
- Stroke
Your health care provider will work with you to lower your cholesterol by improving your diet. If this is not successful, medicines to lower the cholesterol may be the next step.
Statins are thought to be the best drugs to use for people who need medicines to lower their cholesterol.
Some people may be prescribed these medicines in combination with other drugs. They may also need to take them if other medicines are not tolerated due to allergies or side effects.
Both adults and teenagers can use cholestyramine when needed.
Cholestyramine is available only with your doctor’s prescription.
Cholestyramine is available in the following dosage forms:
- Powder for oral suspension
- You will need to mix powder forms with water or other fluids.
- The powder may also be mixed with soups or blended fruit.
- Tablet
- Pill forms should be taken with plenty of water.
- DO NOT chew or crush the tablet.
- Chewable bar
Do not take the cholestyramine powder alone. To take the powder, follow these steps:
- Stir the powder into a glass of water, milk, heavy or pulpy fruit juices such as orange juice, or other beverage. If you use a carbonated beverage, mix the powder slowly in a large glass to avoid excessive foaming.
- Drink the mixture slowly.
- Rinse the drinking glass with more of the beverage and drink it to be sure that you get all of the powder.
The powder also may be mixed with applesauce, crushed pineapple, pureed fruit, and soup. Although the powder may be mixed in hot foods, do not heat the powder. To improve the taste and for convenience, you can prepare doses for an entire day on the previous evening and refrigerate them.
To take the chewable bars, chew each bite thoroughly before swallowing.
Drink plenty of liquids while you are taking cholestyramine. You should take cholestyramine with food, unless otherwise directed. Cholestyramine usually is taken two to four times a day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take cholestyramine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Take cholestyramine before a meal and/or at bedtime, and try to take any other medications at least 1 hour before or 4 hours after you take cholestyramine because cholestyramine can interfere with their absorption.
Continue to take cholestyramine even if you feel well. Do not stop taking cholestyramine without talking to your doctor. This precaution is especially important if you also take other drugs; changing your cholestyramine dose may change their effects.
You should follow a healthy diet while taking cholestyramine. This includes eating less fat in your diet. Other ways you can help your heart include:
- Getting regular exercise
- Managing stress
- Quitting smoking
Before you start taking cholestyramine, tell your provider if you:
- Have bleeding problems or stomach ulcers
- Are pregnant, plan to become pregnant, or are breastfeeding
- Have allergies
- Are taking other medicines
- Plan to have surgery or dental work
If you have certain conditions, you may need to avoid cholestyramine. These include:
- Liver or gallbladder problems
- High triglycerides
- Heart, kidney, or thyroid conditions
Tell your provider about all of your medicines, supplements, vitamins, and herbs. Certain medicines may interact with cholestyramine. Be sure to tell your doctor before taking any new medicines.
Taking cholestyramine may also affect how vitamins and other medications are absorbed in the body. Ask your healthcare provider if you should take a multivitamin supplement.
Regular blood tests will tell you and your provider how well the medicine is working.
What special precautions should I follow?
Before taking cholestyramine:
- tell your doctor and pharmacist if you are allergic to cholestyramine or any other drugs.
- tell your doctor and pharmacist what prescription and nonprescription medications you are taking, especially amiodarone (Cordarone), antibiotics, anticoagulants (‘blood thinners’) such as warfarin (Coumadin), digitoxin, digoxin (Lanoxin), diuretics (‘water pills’), iron, loperamide (Imodium), mycophenolate (Cellcept), oral diabetes medications, phenobarbital, phenylbutazone, propranolol (Inderal), thyroid medications, and vitamins.
- tell your doctor if you have or have ever had heart disease, especially angina (heart pain); stomach, intestinal, or gallbladder disease; or phenylketonuria.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking cholestyramine, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking cholestyramine.
Pregnancy (All Trimesters)
Pregnancy Category C: Animal studies have shown an adverse effect and there are no adequate studies in pregnant women OR no animal studies have been conducted and there are no adequate studies in pregnant women.
Breastfeeding
Studies suggest that this medication may alter milk production or composition. If an alternative to this medication is not prescribed, you should monitor the infant for side effects and adequate milk intake.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking cholestyramine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using cholestyramine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Bezafibrate
- Deferasirox
- Digoxin
- Mycophenolate Mofetil
- Mycophenolic Acid
Using cholestyramine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Aceclofenac
- Amiodarone
- Anisindione
- Cephalexin
- Cerivastatin
- Diclofenac
- Dicumarol
- Digitoxin
- Ezetimibe
- Furosemide
- Hydrochlorothiazide
- Levothyroxine
- Meloxicam
- Metronidazole
- Phenprocoumon
- Propranolol
- Valproic Acid
- Warfarin
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your cholestyramine with alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of cholestyramine. Make sure you tell your doctor if you have any other medical problems, especially:
- Bleeding problems or
- Constipation or
- Gallstones or
- Heart or blood vessel disease or
- Hemorrhoids or
- Stomach ulcer or other stomach problems or
- Underactive thyroid—Cholestyramine may make these conditions worse
- Kidney disease—There is an increased risk of developing electrolyte problems (problems in the blood)
- Phenylketonuria (PKU) —Phenylalanine in aspartame is included in the sugar-free brand of cholestyramine and should be avoided. Aspartame can cause problems in people with phenylketonuria. Therefore, it is best if you avoid using the sugar-free product.
Cholestyramine uses
- Cholestyramine is used to lower high cholesterol levels in the blood. This may help prevent medical problems caused by cholesterol clogging the blood vessels.
- Cholestyramine is also used to remove substances called bile acids from your body. With some liver problems, there is too much bile acid in your body and this can cause severe itching.
Cholestyramine works by attaching to certain substances in the intestine. Since cholestyramine is not absorbed into the body, these substances also pass out of the body without being absorbed.
Cholestyramine may also be used for other conditions as determined by your doctor.
For patients taking cholestyramine for high cholesterol:
- Importance of diet—Before prescribing medicine for your condition, your doctor will probably try to control your condition by prescribing a personal diet for you. Such a diet may be low in fats, sugars, and/or cholesterol. Many people are able to control their condition by carefully following their doctor’s orders for proper diet and exercise. Medicine is prescribed only when additional help is needed. Follow carefully the special diet your doctor gave you, since the medicine is effective only when a schedule of diet and exercise is properly followed.
- Also, cholestyramine is less effective if you are greatly overweight. It may be very important for you to go on a reducing diet. However, check with your doctor before going on any diet.
- Remember that cholestyramine will not cure your cholesterol problem but it will help control it. Therefore, you must continue to take it as directed if you expect to lower your cholesterol level.
Cholestyramine dosage
Patients with preexisting constipation: Initiate with 4 g (1 packet or 1 level scoop) orally once a day for 5 to 7 days; increasing to twice a day with monitoring of constipation and of serum lipoproteins, at least twice, 4 to 6 weeks apart. If the initial dose is well tolerated, the dose may be increased as needed by one dose/day (at monthly intervals) with periodic monitoring of serum lipoproteins.
It is very important that your doctor check your progress at regular visits. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it.
Cholestyramine Powder for Suspension
Your doctor will tell you how much medicine to use. Do not use more than directed.
Take cholestyramine just before eating or with meals.
You should not use the cholestyramine powder in dry form, since it could cause you to choke.
Instead, always mix cholestyramine powder as follows:
- Place cholestyramine powder in 2 ounces of any beverage and mix thoroughly. Then add an additional 2 to 4 ounces of beverage and again mix thoroughly (it will not dissolve) before drinking. After drinking all the liquid containing the medicine, rinse the glass with a little more liquid and drink that also, to make sure you get all the medicine.
- You may also mix cholestyramine powder with milk in hot or regular breakfast cereals, or in thin soups such as tomato or chicken noodle soup. Or you may add it to some pulpy fruits such as crushed pineapple, pears, peaches, or fruit cocktail.
Mix in 4 to 6 ounces of water, fruit juice, or milk until completely dissolved. Drink this mixture right away. Rinse the glass with more liquid and drink that too, so you get all of the medicine.
You may also mix the cholestyramine powder in thin soup, with soft fruits such as fruit cocktail or crushed pineapple, or with milk in breakfast cereal.
Drink several glasses of liquids each day while using cholestyramine.
If a dose is missed:
Take the missed dose as soon as possible.
Skip the missed dose if it is almost time for your next regular dose.
You should not use two doses at the same time.
Adult Dose for Hyperlipoproteinemia
- Initial dose: 4 g (1 packet or level scoop) orally once or twice a day
- Maintenance dose: 8 to 16 g (2 to 4 packets or level scoops orally in 2 divided doses
- Maximum dose: 24 g (6 packets or level scoops) per day. This is divided into two to six doses.
Comments:
- Increases in dose should be gradual with periodic assessment of lipid/lipoprotein levels at intervals of not less than 4 weeks.
- Although the recommended dosing schedule is up to twice a day, this drug may be administered in 1 to 6 doses per day.
Uses:
- As adjunctive therapy to diet for the reduction of elevated serum cholesterol in patients with primary hypercholesterolemia (elevated low density lipoprotein [LDL] cholesterol) who do not respond adequately to diet; may be useful to lower LDL cholesterol in patients who also have hypertriglyceridemia, but it is not indicated where hypertriglyceridemia is the abnormality of most concern; this drug has also been shown to delay the progression and increase the rate of regression of coronary atherosclerosis
- For the relief of pruritus associated with partial biliary obstruction
Adult Dose for Hyperlipoproteinemia Type IIa (Elevated LDL)
- Initial dose: 4 g (1 packet or level scoop) orally once or twice a day
- Maintenance dose: 8 to 16 g (2 to 4 packets or level scoops orally in 2 divided doses
- Maximum dose: 24 g (6 packets or level scoops) per day. This is divided into two to six doses.
Comments:
- Increases in dose should be gradual with periodic assessment of lipid/lipoprotein levels at intervals of not less than 4 weeks.
- Although the recommended dosing schedule is up to twice a day, this drug may be administered in 1 to 6 doses per day.
Uses:
- As adjunctive therapy to diet for the reduction of elevated serum cholesterol in patients with primary hypercholesterolemia (elevated low density lipoprotein [LDL] cholesterol) who do not respond adequately to diet; may be useful to lower LDL cholesterol in patients who also have hypertriglyceridemia, but it is not indicated where hypertriglyceridemia is the abnormality of most concern; this drug has also been shown to delay the progression and increase the rate of regression of coronary atherosclerosis
- For the relief of pruritus associated with partial biliary obstruction
Adult Dose for Pruritus of Partial Biliary Obstruction
- Initial dose: 4 g (1 packet or level scoop) orally once or twice a day
- Maintenance dose: 8 to 16 g (2 to 4 packets or level scoops orally in 2 divided doses
- Maximum dose: 24 g (6 packets or level scoops) per day. This is divided into two to six doses.
Comments:
- Increases in dose should be gradual with periodic assessment of lipid/lipoprotein levels at intervals of not less than 4 weeks.
- Although the recommended dosing schedule is up to twice a day, this drug may be administered in 1 to 6 doses per day.
Uses:
- As adjunctive therapy to diet for the reduction of elevated serum cholesterol in patients with primary hypercholesterolemia (elevated low density lipoprotein [LDL] cholesterol) who do not respond adequately to diet; may be useful to lower LDL cholesterol in patients who also have hypertriglyceridemia, but it is not indicated where hypertriglyceridemia is the abnormality of most concern; this drug has also been shown to delay the progression and increase the rate of regression of coronary atherosclerosis
- For the relief of pruritus associated with partial biliary obstruction
Pediatric Dose for Hyperlipoproteinemia
- 240 mg/kg/day orally in 2 to 3 divided doses. Then, your doctor may increase your dose to 8 to 24 grams a day. This is divided into two or more doses.
Comments:
- It is very important that your doctor check your progress at regular visits. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it.
- An optimal dosage schedule has not been established in pediatric patients.
- Dosage expressed in terms of anhydrous resin.
- The effects of long-term administration as well as this drug’s effect in maintaining lowered cholesterol levels in pediatric patients are unknown.
Use:
- As adjunctive therapy to diet for the reduction of elevated serum cholesterol in patients with primary hypercholesterolemia (elevated low density lipoprotein [LDL] cholesterol) who do not respond adequately to diet; may be useful to lower LDL cholesterol in patients who also have hypertriglyceridemia, but it is not indicated where hypertriglyceridemia is the abnormality of most concern
Renal Dose Adjustments
- Data not available
Liver Dose Adjustments
- Data not available
Cholestyramine side effects
The most frequently reported side effect is constipation.
Cholestyramine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- constipation
- bloating
- stomach pain
- gas
- upset stomach
- vomiting
- diarrhea
- loss of appetite
- heartburn
- indigestion
- belching
- dizziness
- headache
If you experience the following symptom, call your doctor immediately:
- unusual bleeding (such as bleeding from the gums or rectum)
Rare side effects
- Black, tarry stools
- Stomach pain (severe) with nausea and vomiting
- Loss of weight (sudden)
Gastrointestinal
Intestinal obstruction occurred rarely and 2 deaths in pediatric patients were reported.
- Very common (10% or more): Constipation
- Uncommon (0.1% to 1%): Tongue irritation, irritation of perianal area, abdominal discomfort/pain/distention, flatulence, nausea, vomiting, diarrhea, heartburn, dyspepsia, steatorrhea
- Rare (less than 0.1%): Intestinal obstruction
- Frequency not reported: Rectal bleeding, black stools, hemorrhoidal bleeding, bleeding from known duodenal ulcer, dysphagia, hiccoughs, ulcer attack, sour taste, pancreatitis, rectal pain, diverticulitis, eructation, dental bleeding, dental caries, calcification of gallbladder, tooth discoloration, erosion of tooth enamel
Cardiovascular
- Frequency not reported: Claudication, angina, arteritis, thrombophlebitis, myocardial infarction, myocardial ischemia, postprandial angina increased
Musculoskeletal
- Common (1% to 10%): Osteoporosis
- Frequency not reported: Backache, arthritis, muscle/joint pain
Hematologic
- Uncommon (0.1% to 1%): Bleeding
- Frequency not reported: Prothrombin time increased, prothrombin time decreased, anemia, hypoprothrombinemia
Metabolic
- Uncommon (0.1% to 1%): Anorexia, hyperchloremic acidosis, Vitamin A deficiency, Vitamin K deficiency
Dermatologic
- Uncommon (0.1% to 1%): Rash, skin irritation
- Frequency not reported: Ecchymosis, xanthoma of hands/fingers, urticaria
Hepatic
- Frequency not reported: Liver function test abnormal
Nervous system
- Frequency not reported: Headache, paresthesia, syncope, dizziness, drowsiness, femoral nerve pain
Other
- Frequency not reported: Vertigo, weight loss, weight gain, glands swollen, edema, chest pain, tinnitus
Ocular
- Frequency not reported: Arcus juvenilis, uveitis, night blindness
Genitourinary
- Frequency not reported: Hematuria, dysuria, burnt odor to urine, diuresis
Respiratory
- Frequency not reported: Asthma, wheezing, shortness of breath
Psychiatric
- Frequency not reported: Libido increased