Contents
- Chronic kidney disease
- Kidneys
- CKD stages
- Chronic kidney disease causes
- Chronic kidney disease prevention
- Chronic kidney disease signs and symptoms
- Chronic kidney disease complications
- Chronic kidney disease diagnosis
- Chronic kidney disease treatment
- Treating the cause of your kidney disease
- Lifestyle changes for people with chronic kidney disease
- Treating complications
- Monitoring your kidney health
- Treatment for end-stage kidney disease
- How does Hemodialysis work?
- How does Peritoneal Dialysis work?
- How Kidney Transplantation Works
- Medical, Psychological, and Social Evaluation at a Transplant Center
- Who is on your transplant team?
- Placement on the Waiting List
- Waiting Period
- Kidney Transplant Surgery
- Recovery from Kidney Transplant Surgery
- Pros and Cons of Kidney Transplantation
- What do you need to know about care after your kidney transplant?
- What are signs that your body is rejecting your new kidney?
- How do you know your new kidney is working properly?
- What are the side effects of immunosuppressants?
- What financial help is available to pay for a kidney transplant?
- What help is available to pay for kidney transplant medicines?
- Eating, Diet, and Nutrition for Kidney Transplant Patients
- What is conservative management for kidney failure?
- Kidney failure diet
- Living with chronic kidney disease
- Chronic kidney disease prognosis
Chronic kidney disease
Chronic kidney disease also known as CKD or chronic kidney failure, is a long-term condition (chronic or more than 3 months) where your kidneys are damaged and lose their ability to filter waste and fluid out of your blood. Chronic kidney disease is called “chronic” because the damage to your kidneys happens slowly over a long period of time. Advanced chronic kidney disease can cause dangerous levels of fluid, electrolytes, toxins and wastes to build up in your body and harm your health. A person is said to have chronic kidney disease (CKD) if they have abnormalities of kidney function or structure present for more than 3 months. If the kidney damage is severe, your kidneys may stop working. This is called kidney failure and it means you will need dialysis or a kidney transplant. The medical definition of CKD includes all individuals with markers of kidney damage or those with an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73m² on at least 2 occasions 90 days apart (with or without markers of kidney damage) 1. A normal eGFR is above 90mL/min/1.73m². Markers of kidney disease may include: albuminuria (albumin:creatinine ratio [ACR] > 3 mg/mmol), presence of blood in urine (hematuria) (or presumed or confirmed renal origin), electrolyte abnormalities due to tubular disorders, renal histological abnormalities, structural abnormalities detected by imaging (e.g. polycystic kidneys, reflux nephropathy) or a history of kidney transplantation 1.
Chronic kidney disease is a common condition often associated with getting older. Chronic kidney disease can affect anyone, but it’s more common in people who are black or of south Asian origin.
CKD can get worse over time and eventually the kidneys may stop working altogether or end-stage renal disease (ESRD) is when your kidneys have stopped working well enough for you to survive without dialysis or a kidney transplant, but this is uncommon. Many people with CKD are able to live long lives with the condition. In the U.S., 37 million people have CKD 2. That is more than 1 in 7 adults. In the United States, diabetes and high blood pressure are the leading causes of kidney failure, accounting for 3 out of 4 new cases.
Many people with chronic kidney disease (CKD) will not have symptoms because it does not usually cause problems until it reaches an advanced stage. CKD may only be diagnosed if you have a blood or urine test for another reason and the results show a possible problem with your kidneys.
The diagnosis of CKD requires the following:
- Decline of kidney function for 3 months or more AND
- Evidence of kidney damage (e.g. albuminuria or abnormal biopsy) OR
- GFR <60 mL/min/1.73 m²
At a more advanced kidney disease stage, symptoms can include:
- tiredness
- swollen ankles, feet or hands
- shortness of breath
- feeling sick
- blood in your pee (urine)
Damage to your kidneys cannot be reversed. But if doctors find CKD early, there are ways you can keep the damage from getting worse, such as following a kidney-friendly eating plan, being active and taking certain medicines. If you have a medical condition that increases your risk of kidney disease, your doctor may monitor your blood pressure and kidney function with urine and blood tests during office visits.
Treatment for chronic kidney disease focuses on slowing the progression of kidney damage, usually by controlling the cause. But, even controlling the cause might not keep kidney damage from progressing. Chronic kidney disease can progress to end-stage kidney failure, which is fatal without artificial filtering (dialysis) or a kidney transplant.
Who is more likely to get CKD?
Anyone can get CKD, but some people have a higher chance, such as people who:
- Have diabetes, high blood pressure or heart disease
- Diabetes. Diabetes is the leading cause of CKD. High blood glucose, also called blood sugar, from diabetes can damage the blood vessels in your kidneys. Almost 1 in 3 people with diabetes has CKD 2
- High blood pressure. High blood pressure is the second leading cause of CKD. Like high blood glucose, high blood pressure also can damage the blood vessels in your kidneys. Almost 1 in 5 adults with high blood pressure has CKD 2
- Heart disease. Research shows a link between kidney disease and heart disease. People with heart disease are at higher risk for kidney disease, and people with kidney disease are at higher risk for heart disease. Researchers are working to better understand the relationship between kidney disease and heart disease
- Have a close family member with kidney disease. If your mother, father, sister, or brother has kidney failure, you are at risk for CKD. Kidney disease tends to run in families. If you have kidney disease, encourage family members to get tested.
- Are over age 60
- Are African American, Hispanic, Native American or Asian American 3. The greater risk is due mostly to higher rates of diabetes and high blood pressure among these groups. Scientists are studying other possible reasons for this increased risk 4.
Talk to your doctor about getting tested if you have any of these risk factors for CKD.
What is glomerular filtration rate (GFR)?
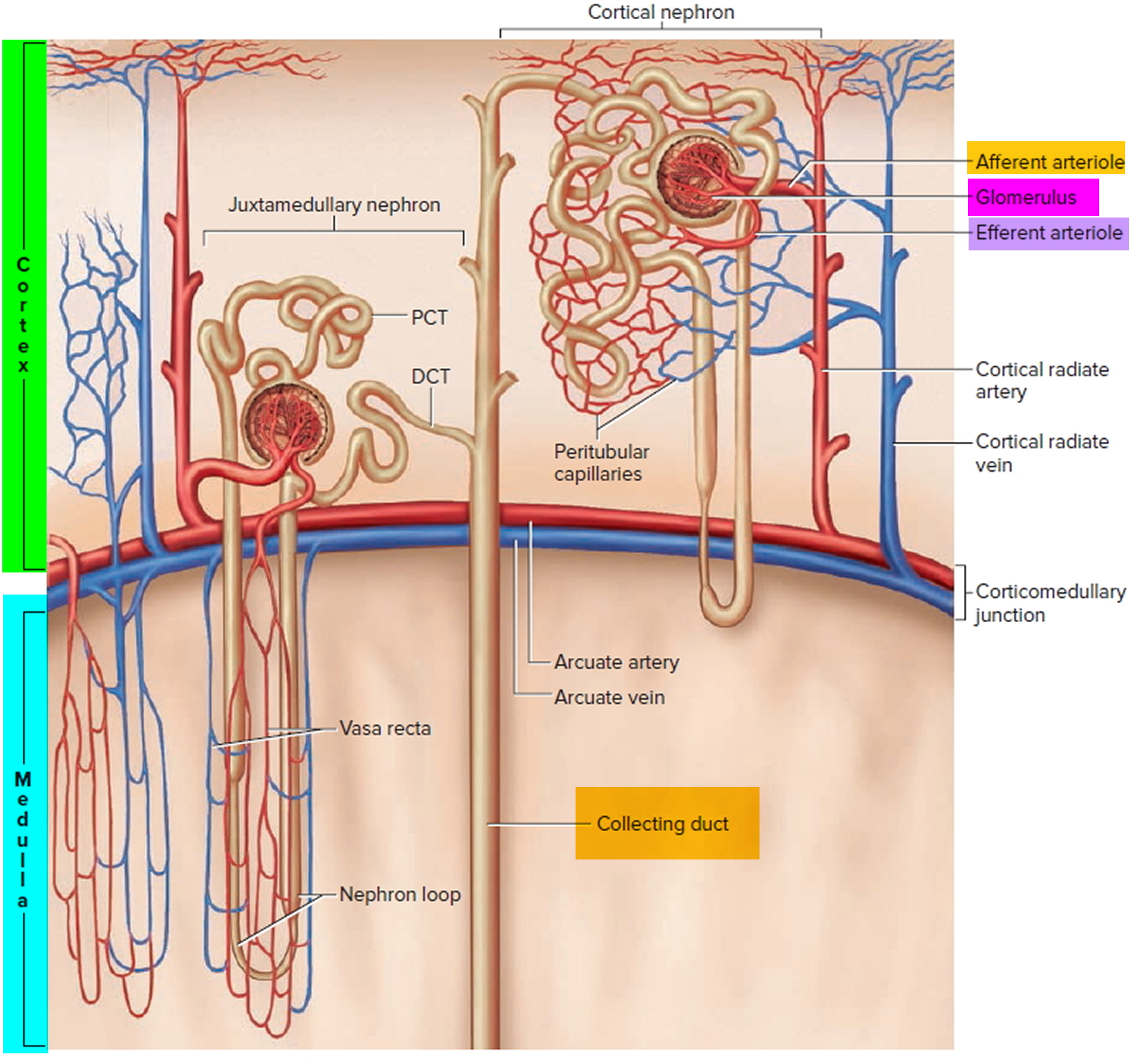
Each kidney has about one million tiny “tiny network of blood vessels that are the cleaning units of your kidney” called renal corpuscles or glomeruli. The glomerular filtration rate (GFR) shows how much blood is filtered per minute. In healthy people, this is between 85 and 135 milliliters per minute – based on a body surface area of 1.73 m² that is used for calculating the GFR.
However, it would be very difficult to measure the GFR directly. That’s why it’s usually estimated glomerular filtration rate (eGFR)– for instance, using the level of creatinine in the blood. Creatinine is a breakdown product of the muscles. The most commonly used formula for estimating the GFR uses serum creatinine, the person’s age, sex and race.
- eGFR (mL/min/1.73 m2) = 175 x (serum creatinine)–1.154 x (Age)–0.203 x (0.742 if female) x (1.212 if African American)
- End Stage Kidney failure (stage 5) is an eGFR < 15 ml/minute.
- eGFR is not reliable for patients with rapidly changing creatinine levels, extremes in muscle mass and body size, or altered diet patterns.
- For a free Glomerular Filtration Rate (GFR) Calculators please go here: https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/kidney-disease/laboratory-evaluation/glomerular-filtration-rate-calculators/recommended
What is kidney failure?
Kidney failure means your kidneys no longer work well enough to do their job 5. Healthy kidneys clean your blood by removing excess fluid, minerals, and wastes. They also make hormones that keep your bones strong and your blood healthy.
Glomerular filtration rate (GFR) is the best measure of overall kidney function in health and disease 6. The normal level of glomerular filtration rate (GFR) varies according to age, sex, and body size. Normal glomerular filtration rate (GFR) in young adults is approximately 120 to 130 mL/min per 1.73 m² and declines with age 7. A glomerular filtration rate (GFR) level less than 60 mL/min per 1.73 m² represents loss of half or more of the adult level of normal kidney function. Below this level, the prevalence of complications of chronic kidney disease increases. Although the age-related decline in GFR has been considered part of normal aging, decreased GFR in the elderly is an independent predictor of adverse outcomes, such as death and cardiovascular disease 8. In addition, decreased GFR in the elderly requires adjustment in drug dosages, as in other patients with chronic kidney disease 9. Therefore, the definition of chronic kidney disease is the same, regardless of age. Because GFR declines with age, the prevalence of chronic kidney disease increases with age; approximately 17% of persons older than 60 years of age have an estimated GFR less than 60 mL/min per 1.73 m² 10.
The National Kidney Foundation Practice Guidelines define kidney failure as either:
- GFR less than 15 mL/min per 1.73 m² (GFR <15 mL/min/1.73 m²), which is accompanied in most cases by signs and symptoms of uremia, or
- A need to start kidney replacement therapy (dialysis or transplantation).
Having kidney failure means that:
- 85-90% of your kidney function is gone
- your kidneys don’t work well enough to keep you alive
There is no cure for kidney failure, but with treatment it is possible to live a long life.
- Approximately 98% of patients with kidney failure in the United States begin dialysis when their GFR is less than 15 mL/min per 1.73 m² 11. Kidney failure is not synonymous with end-stage renal disease (ESRD). End-stage renal disease is an administrative term in the United States. It indicates that a patient is treated with dialysis or transplantation, which is the condition for payment for health care by the Medicare end-stage renal disease Program. The classification of end-stage renal disease does not include patients with kidney failure who are not treated with dialysis and transplantation. Thus, although the term end-stage renal disease provides a simple operational classification of patients according to treatment, it does not precisely define a specific level of kidney function.
- The level of kidney function, regardless of diagnosis, determines the stage of chronic kidney disease according to the Kidney Disease Outcomes Quality Initiative chronic kidney disease classification.
Every day, your kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. Kidney failure means your kidneys are not filtering as well as they should. When your kidneys fail, harmful wastes and extra salt and fluid buildup in your body. You then need treatment to replace the work your damaged kidneys have stopped doing.
Your kidneys filter wastes and extra fluid from your blood to keep you healthy. The wastes and extra fluid become urine that is stored in your bladder until you urinate. When your kidneys fail, dialysis can take over a small part of the work your damaged kidneys can no longer do.
Will my chronic kidney disease get better?
Kidney disease is often “progressive”, which means it gets worse over time. The damage to your kidneys causes scars and is permanent.
You can take steps to protect your kidneys, such as managing your blood pressure and your blood glucose, if you have diabetes.
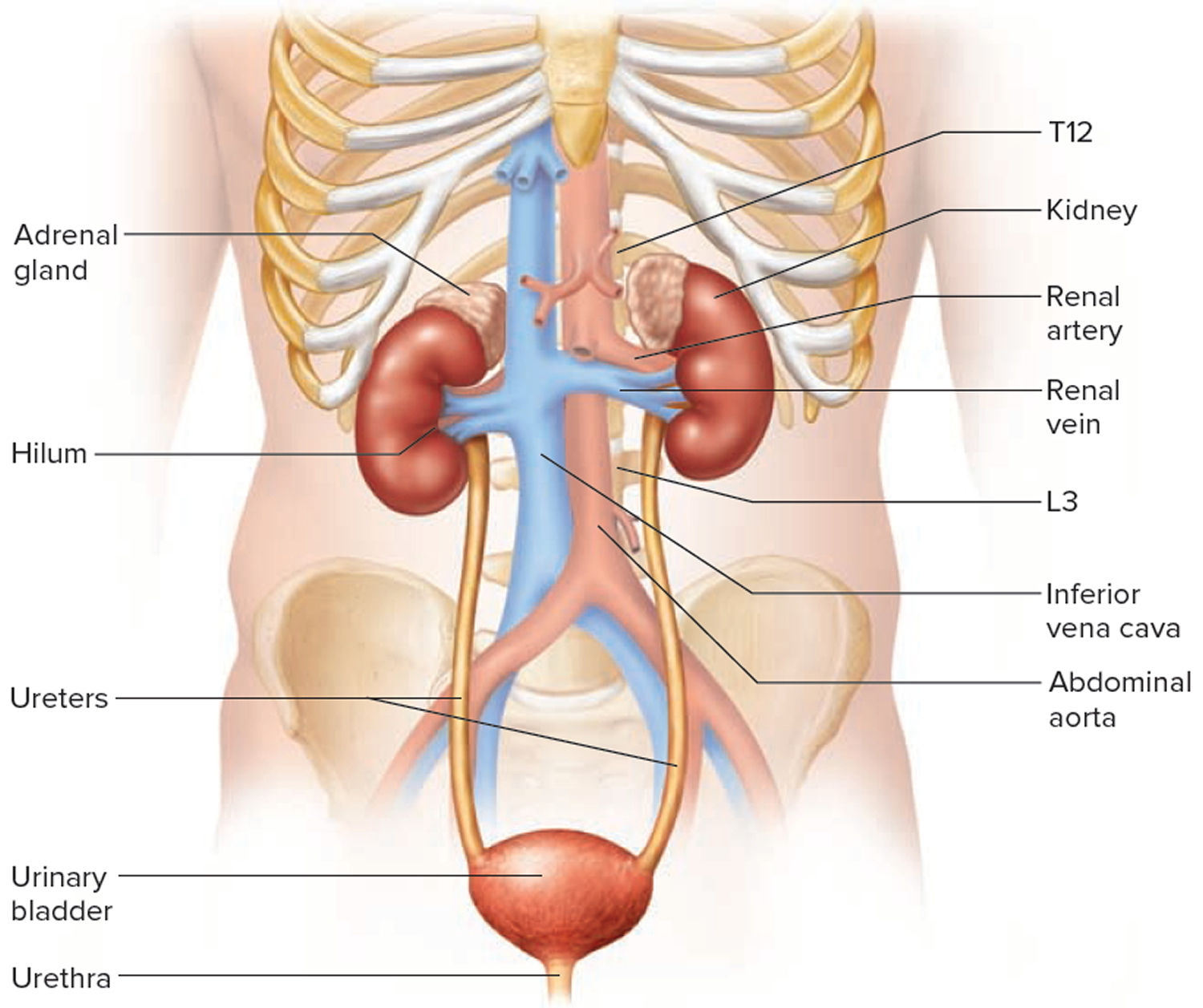
Kidneys
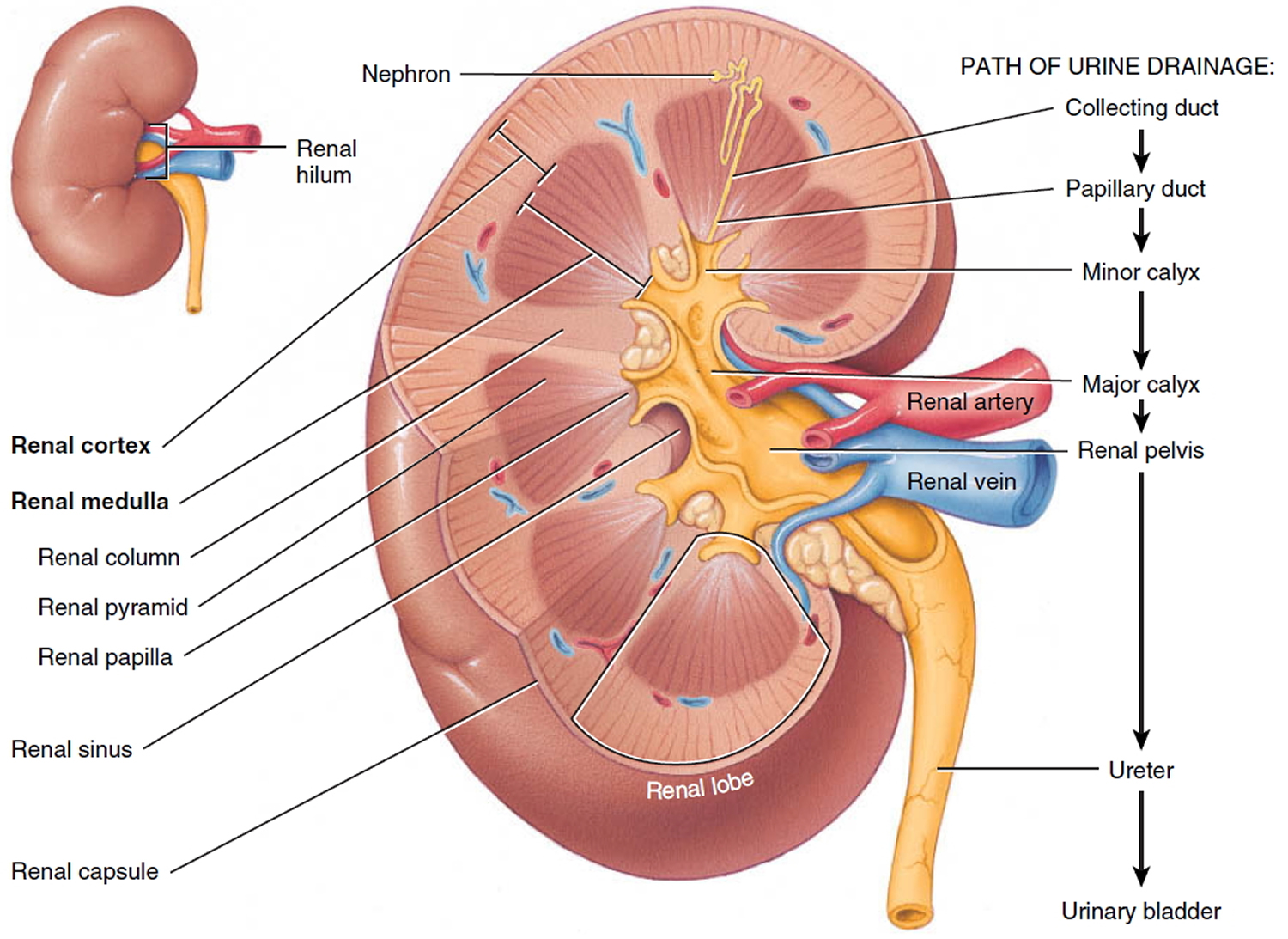
Your paired kidneys are reddish, kidney bean–shaped organs located just above the waist between the peritoneum and the posterior wall of the abdomen. Because their position is posterior to the peritoneum of the abdominal cavity, the organs are said to be retroperitoneal (Figure 1). The kidneys are located between the levels of the last thoracic vertebrae T12 and third lumbar (L3) vertebrae, a position where they are partially protected by ribs 11 and 12. If these lower ribs are fractured, they can puncture the kidneys and cause significant, even life-threatening damage. The right kidney is slightly lower than the left (see Figure 1) because the liver occupies considerable space on the right side superior to the kidney.
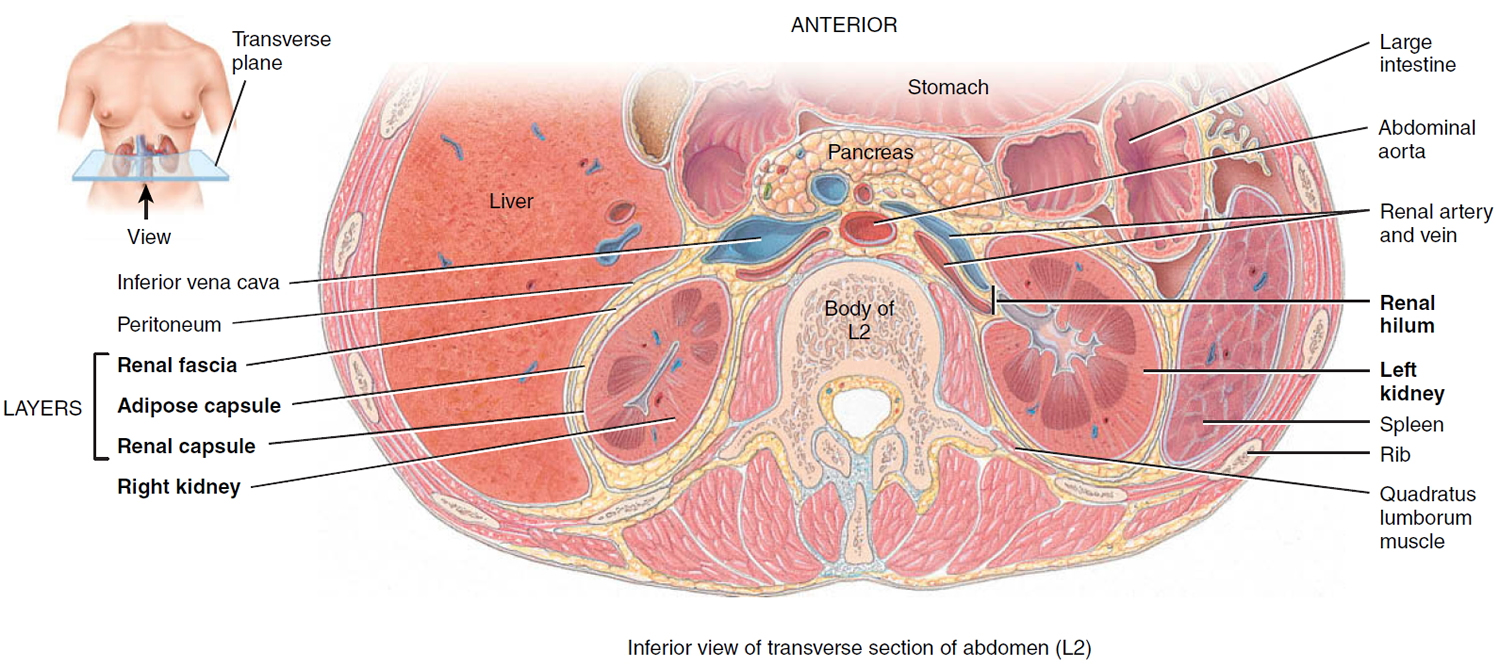
A typical adult kidney is 10–12 cm (4–5 in.) long, 5–7 cm (2–3 in.) wide, and 3 cm (1 in.) thick—about the size of a bar of bath soap—and weighs about 135–150 g (4.5–5 oz). The concave medial border of each kidney faces the vertebral column (see Figure 2). Near the center of the concave border is an indentation called the renal hilum, through which the ureter emerges from the kidney along with blood vessels, lymphatic vessels, and nerves.
Three layers of tissue surround each kidney. The deep layer, the renal capsule, is a smooth, transparent sheet of dense irregular connective tissue that is continuous with the outer coat of the ureter. It serves as a barrier against trauma and helps maintain the shape of the kidney. The middle layer, the adipose capsule, is a mass of fatty tissue surrounding the renal capsule. It also protects the kidney from trauma and holds it firmly in place within the abdominal cavity. The superficial layer, the renal fascia, is another thin layer of dense irregular connective tissue that anchors the kidney to the surrounding structures and to the abdominal wall. On the anterior surface of the kidneys, the renal fascia is deep to the peritoneum.
Figure 1. Kidney location
Figure 2. Kidney location (transverse section)
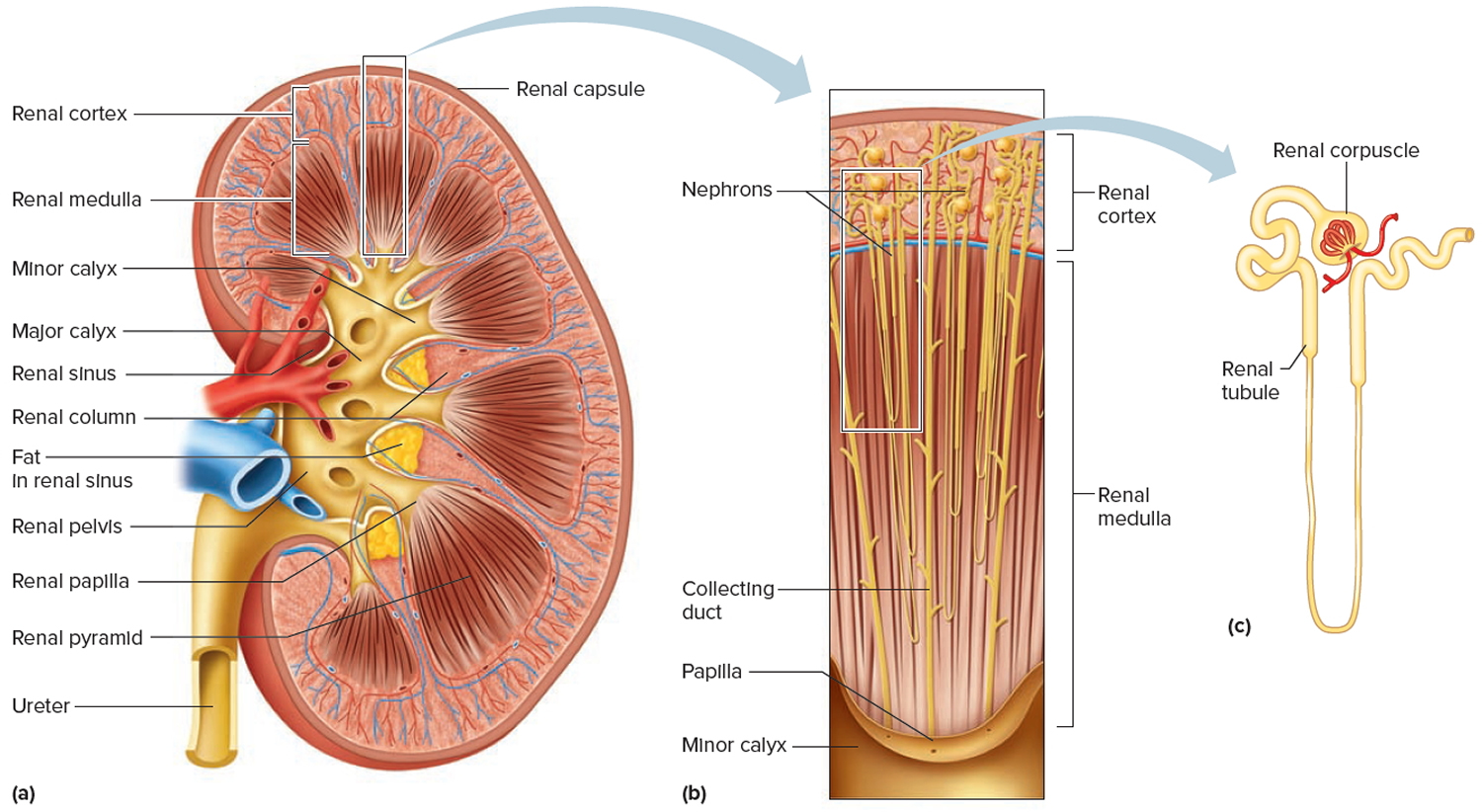
Kidney anatomy
A frontal section through the kidney reveals two distinct regions: a superficial, light red region called the renal cortex and a deep, darker reddish-brown inner region called the renal medulla (medulla = inner portion) (Figure 3). The renal medulla consists of several cone-shaped renal pyramids. The base (wider end) of each pyramid faces the renal cortex, and its apex (narrower end), called a renal papilla, points toward the renal hilum. The renal cortex is the smooth-textured area extending from the renal capsule to the bases of the renal pyramids and into the spaces between them. It is divided into an outer cortical zone and an inner juxtamedullary zone. Those portions of the renal cortex that extend between renal pyramids are called renal columns.
Together, the renal cortex and renal pyramids of the renal medulla constitute the parenchyma or functional portion of the kidney. Within the parenchyma are the functional units of the kidney—about 1 million microscopic structures called nephrons. Filtrate (filtered fluid) formed by the nephrons drains into large papillary ducts, which extend through the renal papillae of the pyramids. The papillary ducts drain into cuplike structures called minor and major calyces. Each kidney has 8 to 18 minor calyces and 2 or 3 major calyces. A minor calyx receives filtrate from the papillary ducts of one renal papilla and delivers it to a major calyx. Once the filtrate enters the calyces it becomes urine because no further reabsorption can occur. The reason for this is that the simple epithelium of the nephron and ducts becomes transitional epithelium in the calyces. From the major calyces, urine drains into a single large cavity called the renal pelvis and then out through the ureter to the urinary bladder.
The hilum expands into a cavity within the kidney called the renal sinus, which contains part of the renal pelvis, the calyces, and branches of the renal blood vessels and nerves. Adipose tissue helps stabilize the position of these structures in the renal sinus.
Figure 3. Kidney anatomy
Figure 4. Kidney structure
Figure 5. Microcirculation of the kidney
Note: DCT = distal convoluted tubule; PCT = proximal convoluted tubule
Kidney function
The primary function of the kidneys is to help maintain homeostasis by regulating the composition (including pH) and the volume of the extracellular fluid. The kidneys accomplish this by removing metabolic wastes from the blood and combining the wastes with excess water and electrolytes to form urine, which they then excrete.
Kidneys maintain homeostasis
- Regulatory function
- Control composition and volume of blood
- Maintain stable concentrations of inorganic anions such as sodium (Na), potassium (K), and calcium (Ca)
- Maintain acid-base balance
- Excretory function
- Produce urine
- Remove metabolic wastes including nitrogenous waste
Kidneys blood filtration and urine production
- Filtration: Glomeruli generate ultrafiltrate of the plasma.
- Reabsorption: Tubules selectively reabsorb substances from the ultrafiltrate.
- Secretion: Tubules secrete substances into the urine.
Examples:
- Potassium is reabsorbed from and secreted into the urine by the tubules.
- Sodium is generally reabsorbed by the tubules.
- Organic acids are secreted into the urine.
- Albumin is generally reabsorbed within the tubules.
Damaged kidneys allow albumin to cross the filtration barrier into the urine
- Increased glomerular permeability allows albumin (and other proteins) to cross the glomerulus into the urine.
- Higher levels of protein within the tubule may exacerbate kidney damage by exceeding tubules’ ability to reabsorb the proteins.
- An elevated urine albumin-to-creatinine ratio (UACR) is used to identify damaged kidneys. Urine albumin-to-creatinine ratio (UACR) results are used for screening, diagnosing, and treating chronic kidney disease. Forty percent of people are identified with chronic kidney disease on the basis of urine albumin alone.
The kidneys have several other important functions:
- Produce Erythropoietin which stimulates marrow production of red blood cells.
- Playing a role in the activation of vitamin D [activate 25(OH)D to 1,25 (OH)2D (active vitamin D)].
- Helping to maintain blood volume and blood pressure by secreting the enzyme Renin.
- Metabolize drugs and endogenous substances (e.g., insulin).
In patients with kidney failure:
- Kidneys cannot maintain homeostasis.
- Kidney failure is associated with fluid, electrolyte, and hormonal imbalances and metabolic abnormalities.
- End stage kidney failure means the patient is on dialysis or has a kidney transplant.
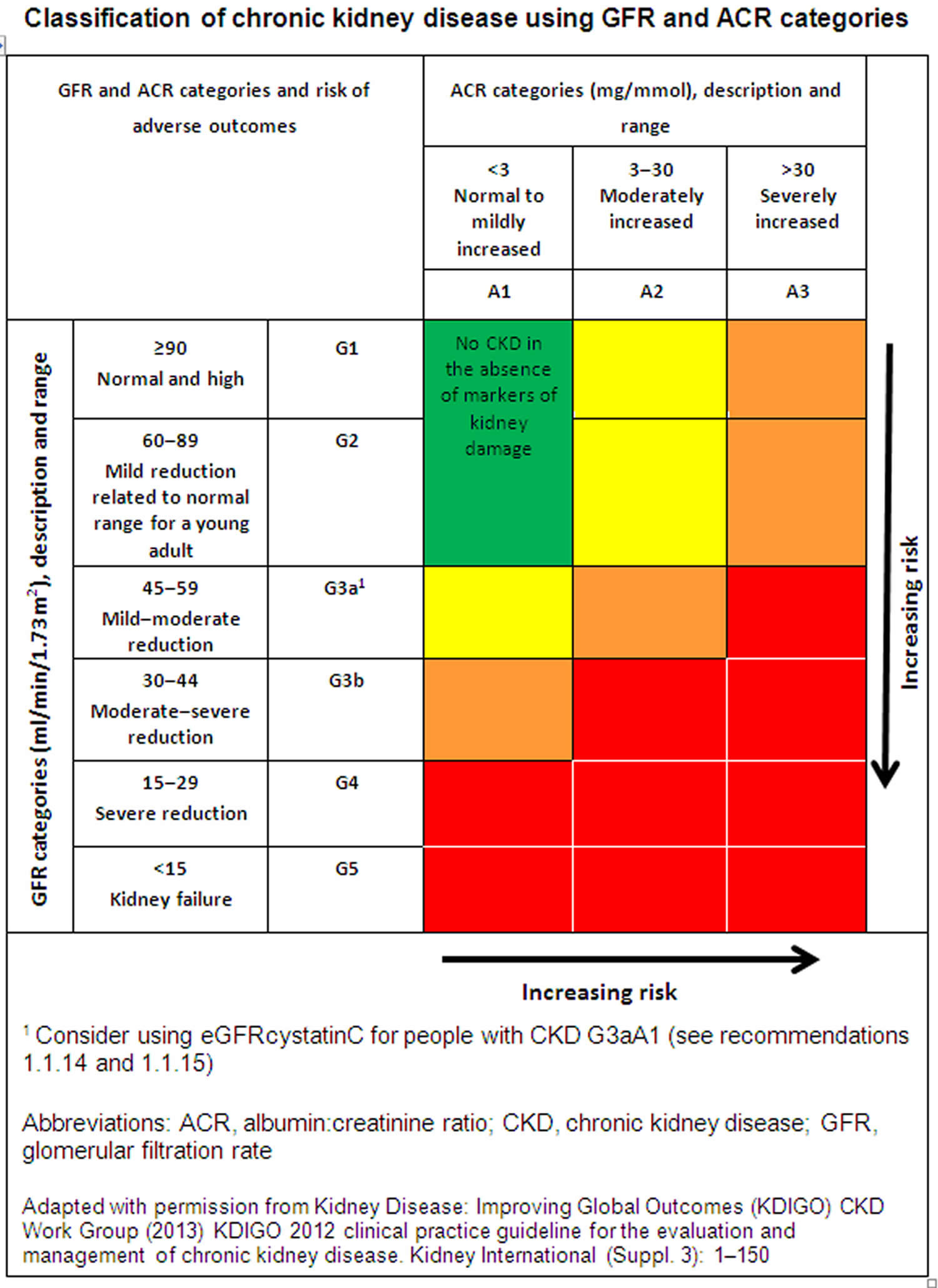
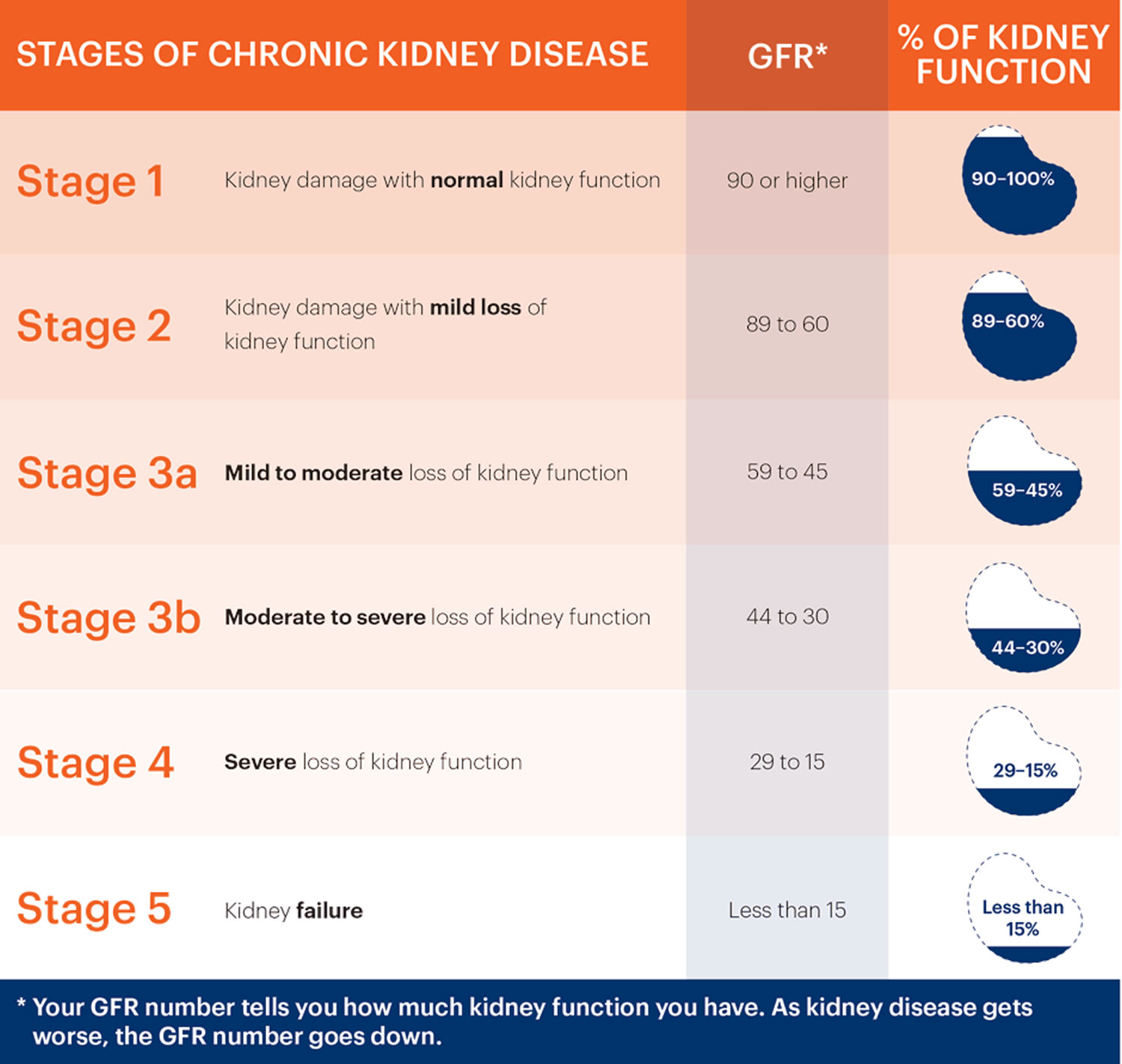
CKD stages
Each chronic kidney disease patient is classified into one of the following 5 stages of CKD based on their estimated glomerular filtration rate (eGFR) and the level of proteinuria, because management and prognosis varies according to the progression of damage.
- CKD Stage 1: Kidney damage with normal or increased eGFR (above 90 mL/min/1.73 m²), but other tests have detected signs of kidney damage
- CKD Stage 2: Mild reduction in eGFR (60-89 mL/min/1.73 m²), with other signs of kidney damage
- CKD Stage 3: Moderate reduction in eGFR (30-59 mL/min/1.73 m²)
- Stage 3a (G3a) – an eGFR of 45 to 59ml/min/1.73 m²
- Stage 3b (G3b) – an eGFR of 30 to 44ml/min/1.73 m²
- CKD Stage 4: Severe reduction in eGFR (15-29 mL/min/1.73 m²)
- CKD Stage 5 (End Stage Kidney Disease or ESRD): Kidney failure (eGFR less than 15 mL/min/1.73 m²), meaning the kidneys have lost almost all of their function and require dialysis
Alongside your eGFR, your urine albumin:creatinine ratio (ACR) can help give a more accurate picture of how well your kidneys are working.
Your albumin:creatinine ratio (ACR) result is given as a stage from 1 to 3:
- A1 – an ACR of less than 3mg/mmol
- A2 – an ACR of 3 to 30mg/mmol
- A3 – an ACR of more than 30mg/mmol
For both eGFR and ACR, a higher stage indicates more severe kidney disease.
Figure 6. CKD stages
Stage 1 CKD
Stage 1 CKD means you have a normal estimated glomerular filtration rate (eGFR) of 90 ml/min per 1.73m² or greater and mild damage to your kidneys. Your kidneys are still working well, so you may not have any symptoms, but you may have signs of kidney damage or physical damage to your kidneys. You may have other signs of kidney damage, such as protein in your urine (proteinuria) or blood in your urine (hematuria). The presence of protein alone means you are in Stage 1 CKD.
At stage 1 CKD, there is a lot you can do to help keep your kidneys working well for as long as possible. Here are some healthy life changes you can make:
- Eat a kidney-friendly diet. A dietitian is a nutrition expert who can look at results from your lab tests and help you plan healthy meals and snacks you’ll want to eat — your “kidney diet.”
- Be active for at least 30 minutes on most days of the week. This can be anything from walking or riding a bike to swimming or dancing.
- Keep a healthy weight. Talk with your doctor about what a healthy weight is for you.
- Quit smoking or using tobacco.
What are the symptoms of stage 1 CKD?
Most people with stage 1 CKD do not have any symptoms that affect their health, which is why many people do not know they have it. However, there are some signs of Stage 1 CKD people may notice themselves, or that doctors may notice when testing for kidney damage or other health conditions.
Signs and symptoms of stage 1 CKD include:
- High blood pressure
- Swelling in your hands or feet
- Urinary tract infections
- Protein in your urine
- Blood in your urine (also called hematuria)
- Kidney damage that shows up in an ultrasound, CT scan, MRI, or kidney biopsy
Stage 1 CKD treatment
At stage 1 CKD, doctors mostly focus on slowing down kidney damage and keeping your kidneys working well for as long as possible.
Doctors will work with you to:
- Control your blood sugar if you have diabetes.
- Keep your blood pressure in a healthy range (less than 120/80 mmHG, is best).
- Decide if you should start or stop any medicines to help protect your kidneys.
If you do not have a nephrologist (kidney doctor), talk to your regular doctor about finding one. You and your nephrologist can work together to make a treatment plan just for you.
Stage 2 CKD
Stage 2 CKD means your eGFR has gone down to between 60 and 89 ml/min/1.73m², and you have mild damage to your kidneys. Most of the time, your kidneys are still working well, so you may not have any symptoms. You may have other signs of kidney damage, such as protein in your urine or physical damage.
Many people with Stage 2 CKD do not have any symptoms. However, if you have a family history of kidney disease, or a health condition that can damage your kidneys, such as diabetes or high blood pressure, your doctor may test the health of your kidneys.
To find out what stage of CKD you are in and what caused your CKD, your doctor will do tests, such as:
- eGFR blood tests (a blood test)
- Blood pressure checks
- Urine tests
- Imaging tests to take detailed pictures of the inside of your body, such as ultrasound, CT scan or MRI
- Kidney biopsy (taking out part of your kidney tissue to look at it under a microscope)
- Genetic testing (if doctors suspect a rare disease or one that runs in your family)
In Stage 2 CKD, making healthy choices to slow down the damage to your kidneys is important.
Here are some tips you can use:
- Eat a kidney-friendly diet. A dietitian is a nutrition expert who can look at results from your lab tests and help you plan healthy meals and snacks you’ll want to eat: your “kidney diet.”
- Be active for at least 30 minutes on most days of the week. This can be anything from walking or riding a bike to swimming or dancing.
- Keep a healthy weight. Talk with your doctor about what a healthy weight is for you.
- Quit smoking or using tobacco.
What are the symptoms of stage 2 CKD?
Often, symptoms of kidney disease do not start until stage 3 CKD, which is why many people with stage 2 CKD might not know they have it. However, there are some signs of stage 2 CKD people may notice, or that doctors may notice when testing for kidney damage or other health conditions.
Signs and symptoms of stage 2 CKD include:
- Protein in your urine
- High blood pressure
- Swelling in your hands or feet
- Urinary tract infections
- Blood in your urine (hematuria)
- Kidney damage that shows up in an ultrasound, CT scan, MRI or kidney biopsy
Stage 2 CKD treatment
Your doctor will work with you to slow down kidney damage and to keep your kidneys working well for as long as possible.
Your doctor can help you:
- Control your blood sugar if you have diabetes.
- Keep your blood pressure in a healthy range (less than 120/80 mmHG, is best).
- Decide if you start or stop any medicines to help protect your kidneys.
If you do not have a nephrologist (kidney doctor), talk to your regular doctor about finding one. You and your nephrologist can work together to make a treatment plan just for you.
Stage 3 CKD
Stage 3 CKD means you have an eGFR between 30 and 59 ml/min/1.73m² and you have mild to moderate damage to your kidneys. Your kidneys do not work as well as they should to filter waste and extra fluid out of your blood. This waste can build up in your body and begin to cause other health problems, such as high blood pressure and bone disease. You may begin to have symptoms, such as feeling weak and tired or swelling in your hands or feet, but you do not need a dialysis or a kidney transplant..
Stage 3 CKD is split into two substages based on your eGFR:
- Stage 3a means you have an eFGR between 45 and 59 ml/min/1.73m²
- Stage 3b means you have an eGFR between 30 and 44 ml/min/1.73m²
With treatment and healthy life changes, many people in Stage 3 do not move to Stage 4 or Stage 5.
To find out what stage of CKD you are in and find out what caused your CKD, your doctor will do tests, such as:
- eGFR blood tests
- Urine tests
- Blood pressure checks
- Imaging tests to take detailed pictures of the inside of your body, such as ultrasound, CT scan or MRI
- Kidney biopsy (a procedure where doctors take a small piece of tissue from your kidneys to look at it under a microscope)
- Genetic testing (if doctors suspect a rare disease or one that runs in your family)
What are the symptoms of stage 3 CKD?
Some people with stage 3 CKD do not have any symptoms. But for many people with stage 3 CKD is when their kidney disease begins to affect their health, and they start to notice symptoms.
Symptoms of stage 3 CKD may include:
- Feeling weak and tired
- Swelling in your hands or feet
- Skin that feels dry or itchy
- Pain in your lower back
- Muscle cramps
- Trouble sleeping
- Restless leg syndrome (an uncomfortable feeling in your legs that makes it hard to sit still or fall asleep)
- Urinating more or less often than normal
- Urine that is foamy or darker in color than usual
Stage 3 CKD treatment
Doctors treat Stage 3 CKD with medicines that help with your symptoms and with other health problems kidney disease can cause, such as diabetes and high blood pressure.
These medicines include:
- Blood pressure medicines like ACE inhibitors and angiotensin receptor blockers (angiotensin 2 receptor antagonists) (even if you do not have high blood pressure, these medicines can help slow the damage to your kidneys to keep them working well as long as possible)
- Diabetes medicines to keep your blood sugar at a healthy level (even if you do not have diabetes)
- Calcium and vitamin D supplements to keep your bones strong
- Diuretics to help with swelling (these are medicines that help your kidneys get rid of salt and water and make you urinate more)
- Iron supplements to help with anemia (not enough red blood cells in your body)
You may also need to stop taking certain medicines that can worsen the damage to your kidneys, such as pain medicines called NSAIDs (nonsteroidal anti-inflammatory drugs) and some arthritis medicines. Tell your doctor about all the medicines you take even ones they did not prescribe.
How can I slow down the damage to my kidneys?
Healthy life changes can make a big difference in how you feel and can help keep your kidneys working well for as long as possible. Eating kidney-friendly foods in the right amounts is one of the best ways to slow the damage to your kidneys from CKD and to feel your best. A dietitian is a nutrition expert who can look at results from your lab tests and help you plan healthy meals and snacks you’ll want to eat: your “kidney diet.”
Here are other healthy changes that will help slow the damage to your kidneys:
- Be active for at least 30 minutes on most days of the week. This can be anything from walking or riding a bike to swimming or dancing.
- If you have diabetes, follow your treatment plan to keep your blood sugar within your target range.
- Quit smoking or using tobacco.
Stage 4 of CKD
Stage 4 CKD means you have an eGFR between 15 and 29 ml/min/1.73m² and moderate to severe damage to your kidneys. Your kidneys do not work as well as they should to filter waste out of your blood. This waste can build up in your body and cause other health problems, such as high blood pressure, bone disease and heart disease. You will likely have symptoms such as swelling of your hands and feet and pain in your lower back.
Stage 4 CKD means that your kidneys are moderately or severely damaged and are not working as well as they should to filter waste from your blood. Waste products may build up in your blood and cause other health problems, such as:
- High blood pressure
- Anemia (not enough red blood cells in your body)
- Bone disease
- Heart disease
- High potassium
- High phosphorus
- Metabolic acidosis (a buildup of acid in your body)
Stage 4 CKD is the last stage before kidney failure. It is important to have regular visits with a nephrologist (kidney doctor) to take steps to slow kidney damage and plan ahead for possible treatments for kidney failure.
To find out what stage of CKD you are in and what caused your CKD, your doctor will do tests, such as:
- eGFR blood tests
- Urine tests
- Blood pressure checks
- Imaging tests to take detailed pictures of the inside of your body, such as ultrasound, CT scan or MRI
- Kidney biopsy (a procedure where doctors take a small piece of tissue from your kidneys to look at it under a microscope)
- Genetic testing (if doctors suspect a rare disease or one that runs in your family)
What are the symptoms of stage 4 CKD?
Symptoms of Stage 4 CKD may include:
- Feeling weak and tired
- Swelling in your arms or legs
- Urinating more or less often than normal
- Pain in your lower back
- Muscle cramps
- Feeling sick to your stomach or throwing up
- Feeling less hungry than normal
Stage 4 CKD treatment
You will need to see a nephrologist (kidney doctor). Your nephrologist will treat Stage 4 CKD with medicines that help with your symptoms and other health problems that kidney disease can cause, such as diabetes and high blood pressure.
These medicines include:
- Blood pressure medicines like ACE inhibitors and angiotensin receptor blockers (angiotensin 2 receptor antagonists) (even if you do not have high blood pressure, these medicines can help slow the damage to your kidneys to keep them working well as long as possible)
- Diabetes medicines to keep your blood sugar at a healthy level (even if you do not have diabetes)
- Calcium and vitamin D supplements to keep your bones strong
- Diuretics to help with swelling (these are medicines that help your kidneys get rid of salt and water and make you urinate more)
- Erythropoiesis-stimulating agents or iron supplements to help with anemia (not enough red blood cells in your body)
Your doctor may tell you to stop taking medicines that can damage your kidneys, such as pain medicines called NSAIDs (nonsteroidal anti-inflammatory medicines).
Your nephrologist will decide if your kidneys are close to failure and if you need to start treatment. If you need treatment, they will talk with you about your choices, which include:
- Dialysis, which is a treatment to clean your blood when your kidneys are not able to. Learn more about the 2 types of dialysis.
- A kidney transplant, which is surgery to give you a kidney from someone else’s body. Learn more about kidney transplants.
How can I slow down the damage to my kidneys?
There is usually no cure for CKD, and you usually cannot reverse the kidney damage you already have by the time you get to stage 4 CKD. However, you can take steps to slow down the damage to your kidneys and help you feel your best.
To slow down the damage to your kidneys, your doctor will recommend that you:
- Have visits with a nephrologist about every three months.
- Meet with a dietitian to help you create and follow a kidney-friendly eating plan.
- Keep your blood pressure at a healthy level. Your doctor may prescribe blood pressure medicines like ACE inhibitors and angiotensin receptor blockers (angiotensin 2 receptor antagonists).
- Keep your blood sugar at a healthy level if you have diabetes.
- Be active for at least 30 minutes on most days of the week. This can be anything from walking or riding a bike to swimming or dancing.
- Quit smoking or using tobacco.
How long can I live with Stage 4 CKD?
How long you may live (your life expectancy) depends on many things, such as:
- Your age when diagnosed with CKD
- How well you follow your treatment plan
- Other health problems you have
Stage 5 of CKD
Stage 5 CKD also known as End Stage Kidney Disease or ESRD, which means you have an eGFR less than 15 ml/min/1.73m² and severe damage to your kidneys. Your kidneys are getting very close to failure or have already failed (stopped working). Because your kidneys have stopped working to filter waste out of your blood, waste products build up in your body, which can make you very sick and cause other health problems. When your kidneys fail, treatment options to survive include dialysis or a kidney transplant.
Stage 5 CKD means that your kidneys are severely damaged and have stopped doing their job to filter waste from your blood. Waste products may build up in your blood and cause other health problems, such as:
- High blood pressure
- Anemia (not enough red blood cells in your body)
- Bone disease
- Heart disease
- High potassium
- High phosphorus
- Metabolic acidosis (a buildup of acid in your body)
To find out what stage of CKD you are in and find out what caused your CKD, your doctor may do other tests, including:
- eGFR blood tests
- Urine tests
- Blood pressure checks
- Imaging tests to take detailed pictures of the inside of your body, such as ultrasound, CT scan or MRI
- Kidney biopsy (a procedure where doctors take a small piece of tissue from your kidneys to look at it under a microscope)
- Genetic testing (if doctors suspect a rare disease or one that runs in your family)
What are the symptoms of stage 5 CKD?
You may have these symptoms in stage 5 CKD if your kidneys begin to fail:
- Feeling weak and tired
- Swelling in your arms, hands, legs or feet
- Making little or no urine
- Headaches
- Pain in your lower back
- Muscle cramps
- Feeling sick to your stomach or throwing up
- Feeling less hungry than normal
- Trouble breathing
- Changes in your skin color
Stage 5 CKD treatment
You will need to see a nephrologist (kidney doctor). Your nephrologist will discuss your treatment options, which include:
- Dialysis, which is a treatment to clean your blood when your kidneys are not able to. Learn more about the two types of dialysis.
- A kidney transplant, which is surgery to give you a kidney from someone else’s body. Learn more about kidney transplants.
Your doctor will help you decide which treatment is best for you and create a plan to manage your kidney disease. As part of the plan, your doctor may give you medicines to help with your symptoms and other health problems kidney disease can cause, such as diabetes and high blood pressure.
Your medicines may include:
- Blood pressure medicines like ACE inhibitors and angiotensin receptor blockers (angiotensin 2 receptor antagonists) (even if you do not have high blood pressure, these medicines can help slow the damage to your kidneys to keep them working well as long as possible)
- Diabetes medicines to keep your blood sugar at a healthy level (even if you do not have diabetes)
- Calcium and vitamin D supplements to keep your bones strong
- Diuretics to help with swelling (these are medicines that help your kidneys get rid of salt and water and make you urinate more)
- Phosphorus binders, which prevent your body from absorbing phosphorus from foods you eat
- Erythropoiesis-stimulating agents or to help with anemia (i.e., not enough red blood cells in your body)
Your doctor may tell you to stop taking medicines that can damage your kidneys, such as pain medicines called NSAIDs (nonsteroidal anti-inflammatory medicines).
What steps can I take to manage Stage 5 CKD?
At Stage 5 CKD, there is usually no cure and you cannot reverse the damage to kidney function. There are treatment options for kidney failure that can help you live life.
Your doctor will recommend that you:
- Have visits with a nephrologist to check your blood levels and overall health.
- Meet with a dietitian to help you create and follow a kidney-friendly eating plan. Your eating plan may involve limiting certain things to prevent them from building up in your body, such as fluids, potassium, salt (sodium) or phosphorus. Learn more about a kidney-friendly diet for CKD.
- Keep your blood pressure at a healthy level. They may prescribe blood pressure medicines like ACE inhibitor and ARBs.
- Keep your blood sugar at a healthy level if you have diabetes.
- Be active for at least 30 minutes on most days of the week. This can be anything from walking or riding a bike to swimming or dancing.
- Quit smoking or using tobacco.
How long can I live with Stage 5 CKD?
How long you may live (your life expectancy) depends on many things, such as:
- Your age when diagnosed with CKD
- How well you follow your treatment plan
- Your overall health
- Your wishes
Chronic kidney disease causes
Chronic kidney disease is usually caused by other disease or condition that impairs kidney function, causing kidney damage to worsen over several months or years such as a disease like diabetes or high blood pressure. Diabetes means that your blood sugar is too high and diabetes is the most common cause of kidney failure. High blood pressure is the second most common cause of kidney failure. Chronic kidney disease is often the result of a combination of different problems.
CKD can be caused by:
- High blood pressure (hypertension) – over time, this can put strain on the small blood vessels in the kidneys and stop the kidneys working properly
- Diabetes (type 1 diabetes or type 2 diabetes) – too much glucose in your blood can damage the tiny filters in the kidneys
- High cholesterol – this can cause a build-up of fatty deposits in the blood vessels supplying your kidneys, which can make it harder for them to work properly
- Kidney infections also called pyelonephritis
- Glomerulonephritis – an inflammation of the kidney’s filtering units (glomeruli)
- Interstitial nephritis, an inflammation of the kidney’s tubules and surrounding structures
- Polycystic kidney disease (PKD) – an inherited condition where growths called cysts develop in the kidneys
- Other inherited kidney diseases
- Hemolytic uremic syndrome in children
- IgA vasculitis
- Renal artery stenosis
- Lupus nephritis is the medical name for kidney disease caused by lupus
- Kidney cancer
- Vesicoureteral reflux (VUR), a condition that causes urine to back up into your kidneys
- Disorders in which the body’s immune system attacks its own cells and organs, such as anti-GBM disease (Goodpasture’s disease)
- Prolonged obstruction of the urinary tract – for example, from kidney stones that keep coming back, or an enlarged prostate
- Long-term, regular use of certain medicines – such as lithium and non-steroidal anti-inflammatory drugs (NSAIDs) that are toxic to the kidneys
- Plasma cell dyscrasias or neoplasm
- Heavy metal poisoning, such as lead poisoning
- Sickle Cell Nephropathy which accounts for less than 1% of end-stage renal disease (ESRD) patients in the United States 12
- Rare genetic conditions, such as Alport syndrome
You can help prevent CKD by making healthy lifestyle changes and ensuring any underlying conditions you have are well controlled.
Risk factors for developing CKD
Risk factors are things that give you a higher chance of having a condition, such as kidney disease. Having one of these risk factors does not mean that you will get kidney disease. But if you do, and you find and treat kidney disease early, you may be able to prevent it from getting worse.
Risk factors that can increase your risk of chronic kidney disease include:
- Diabetes. Diabetes is the leading risk factor for kidney disease and the most common cause of kidney failure. High blood sugar from diabetes damages your kidneys and lowers their ability to filter waste and fluid from your blood. Over time, this causes kidney disease. If you have diabetes, healthy eating, being active and taking medicine can help slow or avoid damage to your kidneys.
- High blood pressure. High blood pressure is a leading risk factor for kidney disease and the second most common cause of kidney failure, after diabetes. When you have high blood pressure, the force of your blood flowing through the tiny blood vessels in your kidneys can cause damage. High blood pressure can also be a symptom of kidney disease. Keeping your blood pressure under control can help prevent kidney disease or keep it from getting worse.
- Heart (cardiovascular) disease
- Smoking
- Obesity
- Being Black, Native American or Asian American
- Family history of kidney disease
- Abnormal kidney structure
- Older age
- Frequent use of medications that can damage the kidneys.
Chronic kidney disease prevention
To reduce your risk of developing kidney disease:
- Follow instructions on over-the-counter medications. When using nonprescription pain relievers, such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others), follow the instructions on the package. Taking too many pain relievers for a long time could lead to kidney damage.
- Maintain a healthy weight. If you’re at a healthy weight, maintain it by being physically active most days of the week. If you need to lose weight, talk with your doctor about strategies for healthy weight loss.
- Don’t smoke. Cigarette smoking can damage your kidneys and make existing kidney damage worse. If you’re a smoker, talk to your doctor about strategies for quitting. Support groups, counseling and medications can all help you to stop.
- Manage your medical conditions with your doctor’s help. If you have diseases or conditions that increase your risk of kidney disease, work with your doctor to control them. Ask your doctor about tests to look for signs of kidney damage.
Chronic kidney disease signs and symptoms
Signs and symptoms of chronic kidney disease develop over time if kidney damage progresses slowly. In the early stages of chronic kidney disease, you might have few signs or symptoms. You might not realize that you have kidney disease until the condition is advanced. This is because your kidneys have a greater capacity to do their job than is needed to keep you healthy. For example, you can donate one kidney and remain healthy. You can also have kidney damage without any symptoms because, despite the damage, your kidneys are still doing enough work to keep you feeling well. For many people, the only way to know if you have kidney disease is to get your kidneys checked with blood and urine tests.
Loss of kidney function can cause a buildup of fluid or body waste or electrolyte problems. Depending on how severe it is, loss of kidney function can cause:
- Nausea
- Vomiting
- Loss of appetite
- Fatigue and weakness
- Sleep problems
- Urinating more or less
- Decreased mental sharpness
- Muscle cramps
- Swelling of feet and ankles
- Dry, itchy skin
- High blood pressure (hypertension) that’s difficult to control
- Shortness of breath, if fluid builds up in the lungs
- Chest pain, if fluid builds up around the lining of the heart
Signs and symptoms of kidney disease are often nonspecific. This means they can also be caused by other illnesses. Because your kidneys are able to make up for lost function, you might not develop signs and symptoms until irreversible damage has occurred.
Make an appointment with your doctor if you have signs or symptoms of kidney disease. Early detection might help prevent kidney disease from progressing to kidney failure.
Early stages of CKD
Kidney disease does not tend to cause symptoms when it’s at an early stage. This is because the body is usually able to cope with a significant reduction in kidney function. Kidney disease is often only diagnosed at this stage if a routine test for another condition, such as a blood or urine test, detects a possible problem. If it’s found at an early stage, medicine and regular tests to monitor it may help stop it becoming more advanced.
Later stages of CKD
A number of symptoms can develop if kidney disease is not found early or it gets worse despite treatment.
Later stages of CKD symptoms can include:
- weight loss and poor appetite
- swollen ankles, feet or hands – as a result of water retention (edema)
- shortness of breath
- tiredness
- blood in your pee (urine)
- an increased need to pee – particularly at night
- difficulty sleeping (insomnia)
- itchy skin
- muscle cramps
- feeling sick
- headaches
- erectile dysfunction in men
People with late stage CKD can also develop anemia, bone disease, and malnutrition. This stage of CKD is known as kidney failure, end-stage renal disease or established renal failure. It may eventually require treatment with dialysis or a kidney transplant.
Chronic kidney disease complications
Chronic kidney disease can affect almost every part of your body. Potential complications include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart’s function and can be life-threatening
- Anemia
- Heart disease. If you have kidney disease, it increases your chances of having a stroke or heart attack.
- High blood pressure can be both a cause and a result of kidney disease. High blood pressure damages your kidneys, and damaged kidneys don’t work as well to help control your blood pressure.
- Weak bones and an increased risk of bone fractures
- Decreased sex drive, erectile dysfunction or reduced fertility
- Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures
- Decreased immune response, which makes you more vulnerable to infection
- Pericarditis, an inflammation of the saclike membrane that envelops your heart (pericardium)
- Pregnancy complications that carry risks for the mother and the developing fetus
- Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival
If you have CKD, you also have a higher chance of having a sudden change in kidney function caused by illness, injury, or certain medicines. This is called acute kidney injury (AKI).
Chronic kidney disease diagnosis
As a first step toward diagnosis of kidney disease, your doctor discusses your personal and family history with you. Among other things, your doctor might ask questions about whether you’ve been diagnosed with high blood pressure, if you’ve taken a medication that might affect kidney function, if you’ve noticed changes in your urinary habits and whether you have family members who have kidney disease.
Next, your doctor performs a physical exam, checking for signs of problems with your heart or blood vessels, and conducts a neurological exam.
For kidney disease diagnosis, you might also need certain tests and procedures to determine how severe your kidney disease is (stage).
Chronic kidney disease (CKD) can be diagnosed with blood and urine tests. In many cases, CKD is only found when a routine blood or urine test you have for another problem shows that your kidneys may not be working normally.
Blood test
The main test for kidney disease is a blood test. The test measures the levels of a waste product called creatinine and urea in your blood. Your doctor uses your blood test results, plus your age, size, gender and ethnic group to calculate how many milliliters (mL) of waste your kidneys should be able to filter in a minute. This calculation is known as your estimated glomerular filtration rate (eGFR). Healthy kidneys should be able to filter more than 90mL/min. You may have CKD if your rate is lower than this.
Your test results can be used to determine how damaged your kidneys are, known as the stage of CKD.
This can help your doctor decide the best treatment for you and how often you should have tests to monitor your condition.
The Glomerular filtration rate (GFR) provides an estimate of how much blood is filtered by the kidneys each minute.
- The formula used to estimate GFR uses serum creatinine, age, gender, and race. In normal kidneys GFR > 60 ml/minute. A GFR of less than 60 ml/minute/1.73m² may mean you have kidney disease
- eGFR (mL/min/1.73 m2) = 175 x (serum creatinine)–1.154 x (Age)–0.203 x (0.742 if female) x (1.212 if African American)
- End Stage Kidney failure (stage 5) is an eGFR < 15 ml/minute. Most people below this level need dialysis or a kidney transplant. Talk with your health care provider about your treatment options.
- eGFR is not reliable for patients with rapidly changing creatinine levels, extremes in muscle mass and body size, or altered diet patterns.
- For a free Glomerular Filtration Rate (GFR) Calculators please go here: https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/kidney-disease/laboratory-evaluation/glomerular-filtration-rate-calculators/recommended
Table 1. Reference Table for Population Mean eGFR from NHANES III
| Age (years) | Mean eGFR (mL/min/1.73 m²) |
|---|---|
| 20–29 | 116 |
| 30–39 | 107 |
| 40–49 | 99 |
| 50–59 | 93 |
| 60–69 | 85 |
| 70 | 75 |
Each chronic kidney disease patient is classified into one of the following 5 stages of CKD based on their estimated glomerular filtration rate (eGFR) and the level of proteinuria, because management and prognosis varies according to the progression of damage.
- CKD Stage 1: Kidney damage with normal or increased eGFR (above 90 mL/min/1.73 m²), but other tests have detected signs of kidney damage
- CKD Stage 2: Mild reduction in eGFR (60-89 mL/min/1.73 m²), with other signs of kidney damage
- CKD Stage 3: Moderate reduction in eGFR (30-59 mL/min/1.73 m²)
- Stage 3a (G3a) – an eGFR of 45 to 59ml/min/1.73 m²
- Stage 3b (G3b) – an eGFR of 30 to 44ml/min/1.73 m²
- CKD Stage 4: Severe reduction in eGFR (15-29 mL/min/1.73 m²)
- CKD Stage 5 (End Stage Kidney Disease or ESRD): Kidney failure (eGFR less than 15 mL/min/1.73 m²), meaning the kidneys have lost almost all of their function and require dialysis
Alongside your eGFR, your urine albumin:creatinine ratio (ACR) can help give a more accurate picture of how well your kidneys are working.
Urine test
A urine test is also done to:
- check the levels of substances called albumin and creatinine in your urine – known as the albumin:creatinine ratio (ACR) or urine albumin-to-creatinine ratio (UACR)
- Doctors use your urine albumin-to-creatinine ratio (UACR) to estimate how much albumin would pass into your urine over 24 hours. A urine albumin result of
- 30 mg/g or less is normal
- more than 30 mg/g may be a sign of kidney disease
- Albumin is a protein found in your blood. A healthy kidney doesn’t let albumin pass into the urine. A damaged kidney lets some albumin pass into the urine. The less albumin in your urine, the better. Having albumin in the urine is called albuminuria. The amount of protein in urine is taken as a sign of how bad the damage is.
- If you have kidney disease, measuring the albumin in your urine helps your doctor know which treatment is best for you. A urine albumin level that stays the same or goes down may mean that treatments are working.
- Doctors use your urine albumin-to-creatinine ratio (UACR) to estimate how much albumin would pass into your urine over 24 hours. A urine albumin result of
- check for blood in your urine. Healthy kidneys usually almost completely prevent certain substances in the blood from entering the urine. Kidney damage may become noticeable when blood is found in urine. Blood and protein are only found in significant amounts in urine if the kidneys are damaged.
If you have albumin in your urine, your doctor may want you to repeat the urine test one or two more times to confirm the results.
Alongside your eGFR, your urine albumin:creatinine ratio (ACR) can help give a more accurate picture of how well your kidneys are working.
You can tell that your treatments are working if your:
- GFR stays the same
- urine albumin stays the same or goes down
Your albumin:creatinine ratio (ACR) result is given as a stage from 1 to 3:
- A1 – an ACR of less than 3 mg/mmol
- A2 – an ACR of 3 to 30 mg/mmol
- A3 – an ACR of more than 30 mg/mmol
For both eGFR and ACR, a higher stage indicates more severe kidney disease.
Other tests
Sometimes other tests are also used to assess the level of damage to your kidneys.
These may include:
- an ultrasound scan, MRI scan or CT scan – to see what the kidneys look like and check whether there are any blockages
- a kidney biopsy – a small sample of kidney tissue is removed using a needle and the cells are examined under a microscope for signs of damage. Kidney biopsy is often done with local anesthesia using a long, thin needle that’s inserted through your skin and into your kidney. The biopsy sample is sent to a lab for testing to help determine what’s causing your kidney problem.
Chronic kidney disease treatment
There’s no cure for chronic kidney disease (CKD). Depending on the cause, some types of kidney disease can be treated. Your treatment will depend on the stage of your CKD. Treatment usually consists of measures to help control signs and symptoms, reduce complications, and slow progression of the kidney disease. If your kidneys become severely damaged, you might need treatment for end-stage kidney disease.
The main treatments for chronic renal failure are:
- Treating the cause of your kidney disease
- Lifestyle changes – to help you stay as healthy as possible
- Medicine – to control associated problems, such as high blood pressure and high cholesterol
- Dialysis – treatment to replicate some of the kidney’s functions, which may be necessary in advanced (stage 5) CKD
- Kidney transplant – this may also be necessary in advanced (stage 5) CKD
Treating the cause of your kidney disease
Your doctor will work to slow or control the cause of your kidney disease. Treatment options vary depending on the cause. But kidney damage can continue to worsen even when an underlying condition, such as diabetes mellitus or high blood pressure, has been controlled.
Controlling your blood pressure
The most important step you can take to treat kidney disease is to control your blood pressure. High blood pressure can damage your kidneys. You can protect your kidneys by keeping your blood pressure at or less than the goal set by your health care provider. For most people, the blood pressure goal is less than 140/90 mmHg.
Work with your health care provider to develop a plan to meet your blood pressure goals. Steps you can take to meet your blood pressure goals may include eating heart-healthy and low-sodium meals, quitting smoking, being active, getting enough sleep, and taking your medicines as prescribed.
Controlling your blood glucose if you have diabetes
To reach your blood glucose goal, check your blood glucose level regularly. Use the results to guide decisions about food, physical activity, and medicines. Ask your health care provider how often you should check your blood glucose level.
Your health care provider will also test your A1C. The A1C is a blood test that measures your average blood glucose level over the past 3 months. This test is different from the blood glucose checks you do regularly. The higher your A1C number, the higher your blood glucose levels have been during the past 3 months. Stay close to your daily blood glucose numbers to help you meet your A1C goal.
The A1C goal for many people with diabetes is below 7 percent. Ask your health care provider what your goal should be. Reaching your goal numbers will help you protect your kidneys.
Lifestyle changes for people with chronic kidney disease
The following lifestyle measures are usually recommended for people with kidney disease:
- stop smoking if you smoke
- eat a healthy, balanced diet
- restrict your salt intake to less than 6g a day – that’s around 1 teaspoon
- do regular exercise – aim to do at least 150 minutes a week
- manage your alcohol intake so you drink no more than the recommended limit of 14 units of alcohol a week
- lose weight if you’re overweight or obese
- avoid over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, except when advised to by a medical professional – these medicines can harm your kidneys if you have kidney disease
Treating complications
Kidney disease complications can be controlled to make you more comfortable. Treatments might include:
- High blood pressure medications. People with kidney disease can have worsening high blood pressure. Your doctor might recommend medications to lower your blood pressure — commonly angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers — and to preserve kidney function. High blood pressure medications can initially decrease kidney function and change electrolyte levels, so you might need frequent blood tests to monitor your condition. Your doctor may also recommend a water pill (diuretic) and a low-salt diet.
- Medications to relieve swelling. People with chronic kidney disease often retain fluids. This can lead to swelling in the legs as well as high blood pressure. Medications called diuretics can help maintain the balance of fluids in your body.
- Medications to treat anemia. Supplements of the hormone erythropoietin (EPO), sometimes with added iron, help produce more red blood cells. This might relieve fatigue and weakness associated with anemia.
- Medications to lower cholesterol levels. Your doctor might recommend medications called statins to lower your cholesterol. People with chronic kidney disease often have high levels of bad cholesterol, which can increase the risk of heart disease.
- Medications to protect your bones. Hyperphosphatemia is a frequent complication of CKD due to a decreased filtered load of phosphorous. This leads to increased secretion of a parathyroid hormone (PTH) and causes secondary hyperparathyroidism. Hyperparathyroidism results in the normalization of phosphorous and calcium but at the expense of bone. This results in renal osteodystrophy. Therefore, phosphorus binders along with dietary restriction of phosphorus are used to treat secondary hyperparathyroidism. Calcium and vitamin D supplements can help prevent weak bones and lower your risk of fracture. You might also take medication known as a phosphate binder to lower the amount of phosphate in your blood and protect your blood vessels from damage by calcium deposits (calcification).
- A lower protein diet to minimize waste products in your blood. As your body processes protein from foods, it creates waste products that your kidneys must filter from your blood. To reduce the amount of work your kidneys must do, your doctor might recommend eating less protein. A registered dietitian can suggest ways to lower your protein intake while still eating a healthy diet.
Your doctor might recommend regular follow-up testing to see whether your kidney disease remains stable or progresses.
Monitoring your kidney health
The tests that your doctors use to test for kidney disease can also be used to track changes to kidney function and damage. Kidney disease tends to get worse over time. Each time you get checked, ask your kidney specialist how the test results compare to the last results. Your goals will be to
- keep your GFR the same
- keep your urine albumin the same or lower
Your kidney specialist will also check your blood pressure and, if you have diabetes, your A1C level, to make sure you are meeting your blood pressure and blood glucose goals.
Treatment for end-stage kidney disease
If your kidneys can’t keep up with waste and fluid clearance on their own and you develop complete or near-complete kidney failure, you have end-stage kidney disease. At that point, you need dialysis or a kidney transplant.
- Dialysis. Dialysis artificially removes waste products and extra fluid from your blood when your kidneys can no longer do this. In hemodialysis, a machine filters waste and excess fluids from your blood. In peritoneal dialysis, a thin tube inserted into your abdomen fills your abdominal cavity with a dialysis solution that absorbs waste and excess fluids. After a time, the dialysis solution drains from your body, carrying the waste with it.
- Kidney transplant. A kidney transplant involves surgically placing a healthy kidney from a donor into your body. Transplanted kidneys can come from deceased or living donors. After a transplant, you’ll need to take medications for the rest of your life to keep your body from rejecting the new organ. You don’t need to be on dialysis to have a kidney transplant.
For some who choose not to have dialysis or a kidney transplant, a third option is to treat your kidney failure with conservative measures. Conservative measures likely will include symptom management, advance care planning and care to keep you comfortable (palliative care).
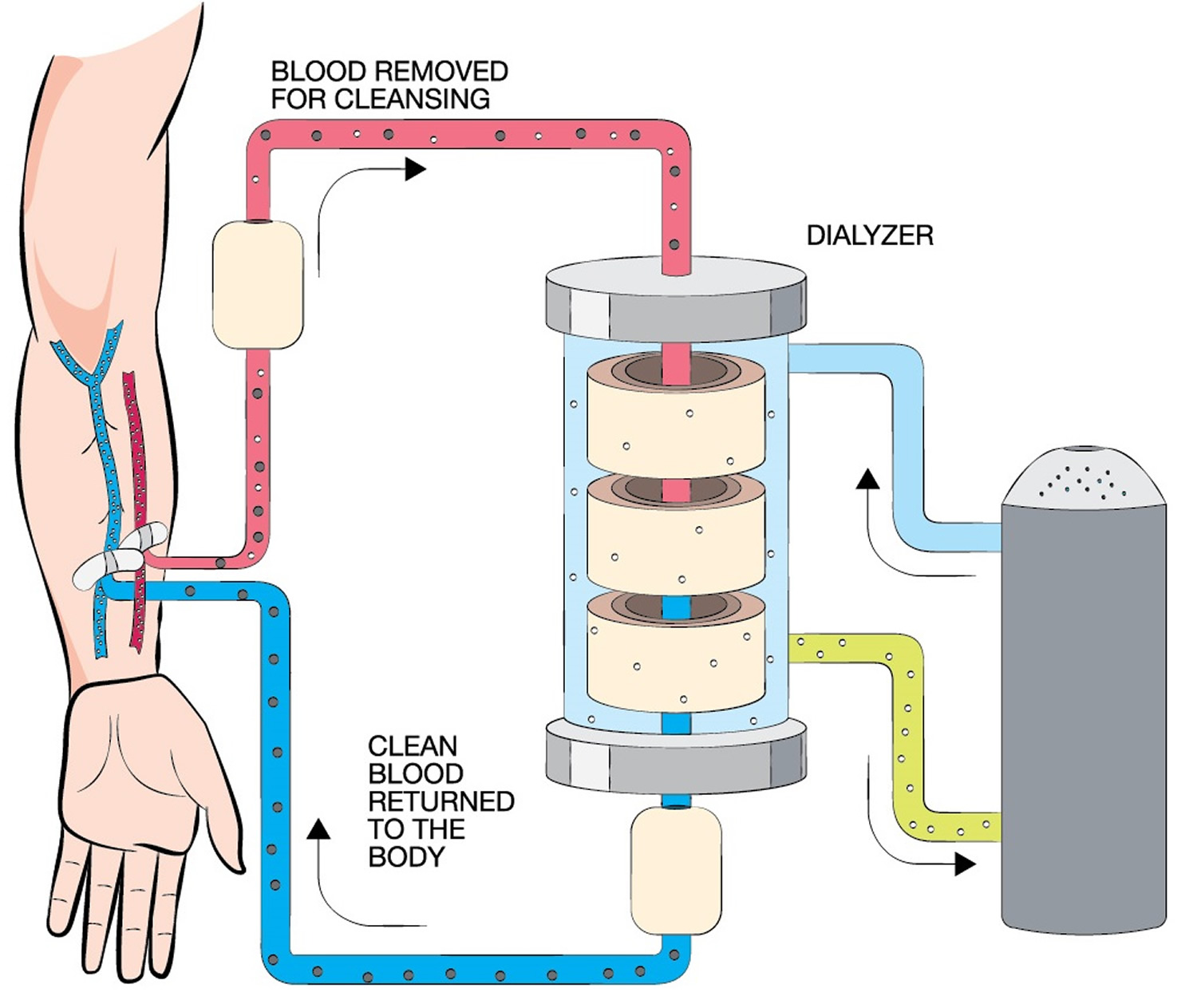
How does Hemodialysis work?
Purpose of Hemodialysis
The purpose of hemodialysis is to filter your blood. This type of dialysis uses a machine to remove harmful wastes and extra fluid, as your kidneys did when they were healthy. Hemodialysis helps control blood pressure and balance important minerals, such as potassium, sodium, calcium, and bicarbonate, in your blood. Hemodialysis is not a cure for kidney failure; however, it can help you feel better and live longer.
How Hemodialysis Works
Before you can begin dialysis, a surgeon will create a vascular access, usually in your arm. A vascular access lets high volumes of blood flow continuously during hemodialysis treatments to filter the largest possible amounts of blood per treatment.
Hemodialysis uses a machine to move your blood through a filter, called a dialyzer, outside your body. A pump on the hemodialysis machine draws your blood through a needle into a tube, a few ounces at a time. Your blood then travels through the tube, which takes it to the dialyzer. Inside the dialyzer, your blood flows through thin fibers that filter out wastes and extra fluid. After the dialyzer filters your blood, another tube carries your blood back to your body. You can do hemodialysis at a dialysis center or in your home.
Hemodialysis can replace part of your kidney function. You will also need dietary changes, medicines, and limits on water and other liquids you drink and get from food. Your dietary changes, the number of medicines you need, and limits on liquid will depend on where you receive your treatments—at a dialysis center or at home—and how often you receive treatments—three or more times a week.
Pros and Cons of Hemodialysis
The pros and cons of hemodialysis differ for each person. What may be bad for one person may be good for another. Following is a list of the general pros and cons of dialysis center and home hemodialysis.
Dialysis Center Hemodialysis
Pros
- Dialysis centers are widely available.
- Trained health care providers are with you at all times and help administer the treatment.
- You can get to know other people with kidney failure who also need hemodialysis.
- You don’t have to have a trained partner or keep equipment in your home.
Cons
- The center arranges everyone’s treatments and allows few exceptions to the schedule.
- You need to travel to the center for treatment.
- This treatment has the strictest diet and limits on liquids because the longer time between treatments means wastes and extra fluid can build up in your body.
- You may have more frequent ups and downs in how you feel from day to day because of the longer time between sessions.
- Feeling better after a treatment may take a few hours.
Home Hemodialysis
Pros
- You can do the treatment at the times you choose; however, you should follow your doctor’s orders about how many times a week you need treatment.
- You don’t have to travel to a dialysis center.
- You gain a sense of control over your treatment.
- You will have fewer ups and downs in how you feel from day to day because of more frequent sessions.
- You can do your treatments at times that will let you work outside the home.
- You will have a more manageable diet and fewer limits on liquids because the shorter time between sessions prevents the buildup of wastes and extra fluid.
- You can take along a hemodialysis machine when traveling.
- You can spend more time with your loved ones because you don’t have to go to the dialysis center three times a week.
Cons
- Not all dialysis centers offer home hemodialysis training and support.
- You and a family member or friend will have to set aside a week or more at the beginning for training.
- Helping with treatments may be stressful for your family or friend.
- You need space for storing the hemodialysis machine and supplies at home.
- You will need to learn to put dialysis needles into your vascular access.
- Medicare and private insurance companies may limit the number of treatments they will pay for when you use home hemodialysis. Few people can afford the costs for additional treatments.
Figure 3. Hemodialysis

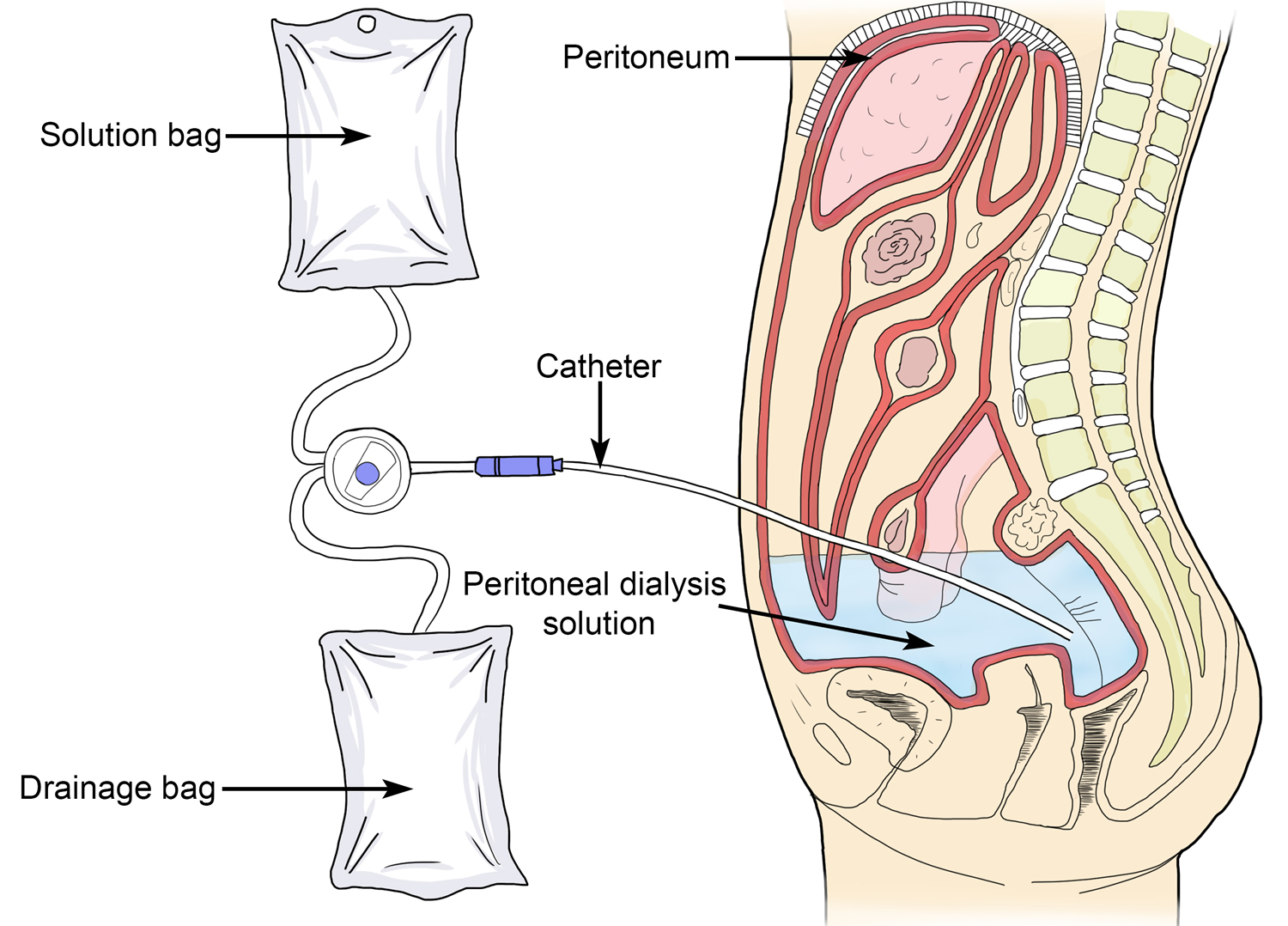
How does Peritoneal Dialysis work?
Purpose of Peritoneal Dialysis
The purpose of peritoneal dialysis is to filter wastes and extra fluid from your body. This type of dialysis uses the lining of your belly—the space in your body that holds your stomach, bowels, and liver—to filter your blood. This lining, called the peritoneum, acts to do the work of your kidneys.
How Peritoneal Dialysis Works
A doctor will place a soft tube, called a catheter, in your belly a few weeks before you start treatment. The catheter stays in your belly permanently. When you start peritoneal dialysis, you will empty a kind of salty water, called dialysis solution, from a plastic bag through the catheter into your belly. When the bag is empty, you can disconnect your catheter from the bag so you can move around and do your normal activities. While the dialysis solution is inside your belly, it soaks up wastes and extra fluid from your body. After a few hours, you drain the used dialysis solution through another tube into a drain bag. You can throw away the used dialysis solution, now filled with wastes and extra fluid, in a toilet or tub. Then you start over with a fresh bag of dialysis solution. The process of emptying the used dialysis solution and refilling your belly with fresh solution is called an exchange. The process goes on continuously, so you always have dialysis solution in your belly soaking up wastes and extra fluid from your body.
Figure 4. Peritoneal dialysis
Types of Peritoneal Dialysis
Two types of peritoneal dialysis are available. After you have learned about the types of peritoneal dialysis, you can choose the type that best fits your life. If one schedule or type of peritoneal dialysis does not suit you, talk with your doctor about trying the other type.
Continuous ambulatory peritoneal dialysis does not require a machine and you can do it in any clean, well-lit place. The time period that the dialysis solution is in your belly is the dwell time. With continuous ambulatory peritoneal dialysis, the dialysis solution stays in your belly for a dwell time of 4 to 6 hours, or more. The process of draining the used dialysis solution and replacing it with fresh solution takes about 30 to 40 minutes. Most people change the dialysis solution at least four times a day and sleep with solution in their belly at night. With continuous ambulatory peritoneal dialysis, you do not have to wake up and perform dialysis tasks during the night.
Continuous cycler-assisted peritoneal dialysis uses a machine called a cycler to fill and empty your belly three to five times during the night while you sleep. In the morning, you begin one exchange with a dwell time that lasts the entire day. You may do an additional exchange in the middle of the afternoon without the cycler to increase the amount of waste removed and to reduce the amount of fluid left behind in your body.
You may need a combination of continuous ambulatory peritoneal dialysis and continuous cycler-assisted peritoneal dialysis if you weigh more than 175 pounds or if your peritoneum filters wastes slowly. For example, some people use a cycler at night and perform one exchange during the day. Others do four exchanges during the day and use a minicycler to perform one or more exchanges during the night. You’ll work with your health care team to find the best schedule for you.
Pros and Cons of Peritoneal Dialysis
Each type of peritoneal dialysis has pros and cons.
Continuous Ambulatory Peritoneal Dialysis
Pros
- You can do continuous ambulatory peritoneal dialysis alone.
- You can do continuous ambulatory peritoneal dialysis at the times you choose, as long as you perform the required number of exchanges each day.
- You can do continuous ambulatory peritoneal dialysis in many locations.
- You can travel as long as you bring dialysis bags with you or have them delivered to your destination.
- You don’t need a machine for continuous ambulatory peritoneal dialysis.
- You gain a sense of control over your treatment.
Cons
- Continuous ambulatory peritoneal dialysis can disrupt your daily schedule.
- Continuous ambulatory peritoneal dialysis is a continuous treatment, and you should do all exchanges 7 days a week.
- Boxes of dialysis solution will take up space in your home.
Continuous Cycler-assisted Peritoneal Dialysis
Pros
- You can do exchanges at night, while you sleep.
- You may not have to perform exchanges during the day.
Cons
- You need a machine.
- Your connection to the cycler limits your movement at night.
Is dialysis a cure for kidney failure?
No. Hemodialysis and peritoneal dialysis help you feel better and live longer; however, they do not cure kidney failure. Although people with kidney failure are now living longer than ever, over the years kidney disease can cause other problems, such as heart disease, bone disease, arthritis, nerve damage, infertility, and malnutrition. These problems won’t go away with dialysis; however, doctors now have new and better ways to prevent or treat them. You should discuss these problems and their treatments with your doctor.
How Kidney Transplantation Works
The transplant process has many steps.
The first step is to talk with your health care provider about whether you are a candidate for a transplant. Transplantation is not for everyone. Your health care provider may tell you that you are not healthy enough for surgery or that you have a condition that would make transplantation unlikely to succeed. If you are a good candidate for a transplant, your health care provider will refer you to a transplant center.
Medical, Psychological, and Social Evaluation at a Transplant Center
The next step is a thorough physical, psychological, and social evaluation at the transplant center, where you will meet members of your transplant team. Your pretransplant evaluation may require several visits to the transplant center over the course of weeks or even months.
You will need to have blood tests as well as other tests to check your heart and other organs. Your blood type and other matching factors help determine whether your body will accept an available donor kidney.
Your transplant team will make sure you are healthy enough for surgery. Some medical conditions or illnesses could make transplantation less likely to succeed.
In addition, your team will make sure you can understand and follow the schedule for taking the medicines needed after surgery. Team members need to be sure that you are mentally prepared for the responsibilities of caring for a transplanted kidney.
If a family member or friend wants to donate a kidney, that person will need a health exam to test whether the kidney is a good match.
Who is on your transplant team?
Your transplant team has many members, including your
- surgeon—the doctor who places the kidney in your body.
- nephrologist—a doctor who specializes in kidney health. The nephrologist may work in partnership with a nurse practitioner or a physician’s assistant.
- transplant coordinator—a specially trained nurse who will be your point of contact, arrange your appointments, and educate you before and after the transplant.
- social worker—a person who is trained to help people solve problems in their daily lives, such as finding employment, affordable housing, or daycare.
- dietitian—a person who is an expert in food and nutrition. Dietitians teach people about the foods they should eat and how to plan healthy meals.
Placement on the Waiting List
If your medical evaluation shows you are a good candidate for a transplant, your transplant center will submit your name to be placed on the national waiting list for a kidney from a deceased donor. The Organ Procurement and Transplantation Network has a computer network that links all regional organ-gathering organizations—known as organ procurement organizations—and transplant centers. The United Network for Organ Sharing (UNOS), a private, nonprofit organization, runs the Organ Procurement and Transplantation Network under a contract with the Federal Government. When UNOS officially adds you to the waiting list, UNOS will notify you and your transplant team.
UNOS allows you to register with multiple transplant centers to increase your chances of receiving a kidney. Each transplant center usually requires a separate medical evaluation.
Waiting Period
UNOS gives preference to people who have been on the waiting list the longest. However, other factors—such as your age, where you live, and your blood type—may make your wait longer or shorter. Wait times can range from a few months to several years.
If you have a living donor, you do not need to be placed on the waiting list and can schedule the surgery when it is convenient for you and your donor.
While you are on the waiting list, notify the transplant center of changes in your health. Also, let the transplant center know if you move or change phone numbers. The center will need to find you immediately when a kidney becomes available.
While you wait for a kidney, you will have blood drawn once a month. The sample will be sent to the transplant center. The center must have a recent sample of your blood for comparison with any kidney that becomes available.
Organ procurement organizations identify potential organs for transplant and coordinate with the national network. When a deceased donor kidney becomes available, the organ procurement organization notifies UNOS and creates a computer-generated list of suitable recipients.
Whether you are receiving your kidney from a deceased donor or a living donor, the transplant team considers three factors in matching kidneys with potential recipients. These matching factors help predict whether your body’s immune system—which protects your body from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances—will accept or reject the new kidney.
- Blood type. Your blood type—A, B, AB, or O—must be compatible with the donor’s. Blood type is the most important matching factor. Some transplant centers have developed techniques for transplanting kidneys that are not matched by blood type.
- Human leukocyte antigens. These six antigens are proteins that help your immune system tell the difference between your own body’s tissues and foreign substances. You may still receive a kidney if the antigens do not completely match, as long as your blood type is compatible with the organ donor’s blood type and other tests show no problems with matching.
- Cross-matching antigens. The cross-match is the last test performed before a kidney transplant can take place. A lab technician mixes a small sample of your blood with a sample of the organ donor’s blood in a tube to see if the mixture causes a reaction. If no reaction occurs—called a negative cross-match—the transplant can proceed.
Kidney Transplant Surgery
If you are on a waiting list for a deceased donor kidney, you must go to the hospital as soon as you receive notification that a kidney is available. If a family member or friend is donating the kidney you will receive, you will schedule the operation in advance. Your transplant team will operate on you and your donor at the same time, usually in side-by-side rooms. One surgeon will perform the nephrectomy—the removal of the kidney from the donor—while another prepares you for placement of the donated kidney. In some centers, the same surgeon performs both operations. You will receive general anesthesia to make you sleep during the operation. The surgery usually takes 3 or 4 hours.
Surgeons—place most transplanted kidneys in the lower front part of your abdomen. The kidney is connected to an artery, which brings unfiltered blood into the kidney, and a vein, which takes filtered blood out of the kidney. The surgeon also transplants the ureter from the donor to let urine from the new kidney flow to your bladder. Unless your damaged kidneys cause problems such as infection, they can remain in their normal position. The transplanted kidney takes over the job of filtering your blood. Your body normally attacks anything it sees as foreign, so to keep your body from attacking the kidney you need to take medicines called immunosuppressants for as long as the transplanted kidney functions.
Recovery from Kidney Transplant Surgery
After surgery, you will probably feel sore and groggy when you wake up. However, many people who have a transplant report feeling much better immediately after surgery. Even if you wake up feeling great, you will typically need to stay in the hospital for several days to recover from surgery, and longer if you have any complications. You will have regular follow-up visits after leaving the hospital.
If you have a living donor, the donor will probably also stay in the hospital for several days. However, a new technique for removing a kidney for donation uses a smaller incision and may make it possible for the donor to leave the hospital in 2 to 3 days.
Pros and Cons of Kidney Transplantation
Following is a list of the pros and cons of kidney transplantation.
Kidney Transplantation
Pros
- A transplanted kidney works like a healthy kidney.
- If you have a living donor, you can choose the time of your operation.
- You may feel healthier and have an improved quality of life.
- You have fewer dietary restrictions.
- You won’t need dialysis.
- People who receive a donated kidney have a greater chance of living a longer life than those who stay on dialysis.
Cons
- Transplantation requires surgery.
- You will go through extensive medical testing at the transplant clinic.
- You may need to wait years for a deceased donor kidney.
- Your body may reject the new kidney, so one transplant may not last a lifetime.
- You’ll need to take immunosuppressants, which may cause other health problems, for as long as the transplanted kidney functions.
What do you need to know about care after your kidney transplant?
You need to know how to keep your body from rejecting your new kidney. Your immune system will sense that your new kidney is foreign. To keep your body from rejecting it, you will have to take medicines, called immunosuppressants, that turn off, or suppress, your immune system response. You may have to take two or more immunosuppressants, as well as medicines such as antibiotics to protect against infections. Your transplant team will teach you what each medicine is for and when to take each one. Be sure you understand the instructions for taking your medicines before you leave the hospital.
What are signs that your body is rejecting your new kidney?
Often, rejection begins before any signs appear. The signs of rejection include indications that your kidney is not working as well as it should—for example, high blood pressure or swelling because your kidney is not getting rid of extra salt and fluid in your body. Advances in immunosuppressants have made other signs of rejection—such as fever, soreness in the lower abdomen where the new kidney is, and a decrease in the amount of urine you make—rare. If you have any of these symptoms, tell your transplant team. You will receive stronger doses of your immunosuppressants and additional medicines to help keep your body from rejecting your new kidney.
Even if you do everything you should, your body may still reject the new kidney, and you may need to go on dialysis. Unless your transplant team determines that you are no longer a good candidate for transplantation, you can go back on the waiting list for another kidney.
How do you know your new kidney is working properly?
Blood tests help you know your new kidney is working. Before you leave the hospital, you will schedule an appointment with your transplant team at the transplant center. At that appointment, a health care provider will draw blood to be tested. The tests show how well your kidneys are removing wastes from your blood. At first, you may return to the transplant center every 2 weeks, then every month. Eventually, you will need to return to the transplant center only once every 6 months or once every year, after your transplant team has determined that your kidney is doing its job.
Your blood tests may show that your kidney is not removing wastes from your blood as well as it should. You may have other signs that your body is rejecting your new kidney. If these problems occur, your transplant surgeon or nephrologist may order a kidney biopsy. Biopsy is a procedure that involves taking a small piece of tissue for examination under a microscope. Your transplant surgeon or nephrologist performs the biopsy in the transplant center or a hospital. The health care provider will give you light sedation and local anesthetic; however, in some cases, a patient may require general anesthesia. A pathologist—a doctor who specializes in diagnosing diseases—examines the tissue in a lab. The test can show whether your body is rejecting your new kidney.
What are the side effects of immunosuppressants?
Some immunosuppressants may change your appearance. Your face may get fuller; you may gain weight or develop acne or facial hair. Not all people have these problems, and those who do can use diet, makeup, and hair removal to minimize changes in appearance.
Immunosuppressants weaken your immune system, which can lead to infections. In some people over long periods of time, a weakened immune system can increase their risk of developing cancer. Some immunosuppressants cause cataracts, diabetes, extra stomach acid, high blood pressure, and bone disease. When used over time, these medicines may also cause liver or kidney damage in some people. Your transplant team will order regular tests to monitor the levels of immunosuppressants in your blood and to measure your liver and kidney function.
What financial help is available to pay for a kidney transplant?
United States citizens who have kidney failure are eligible to receive Medicare, the Federal Government insurance program. Treatment for kidney failure costs a lot; however, Medicare pays much of the cost, usually up to 80 percent. Often, private insurance pays the rest. For people who are not eligible for Medicare or who still need help with the portion Medicare does not cover, states have Medicaid programs that provide funds for health care based on financial need. Your social worker can help you locate resources for financial help.
What help is available to pay for kidney transplant medicines?
Through patient-assistance programs, prescription drug companies give discounts to people who can show they cannot afford the cost of their prescribed medicines. Social workers can help patients complete applications to these programs.
The Partnership for Prescription Assistance has a website that directs patients, caregivers, and doctors to more than 275 public and private patient-assistance programs, including more than 150 programs offered by pharmaceutical companies. The website www.pparx.org features tools to help a person determine which programs might be available.
NeedyMeds is a nonprofit organization that helps people find appropriate patient-assistance programs. The NeedyMeds website—www.needymeds.org —provides a directory of patient-assistance programs that can be searched by a medicine’s brand or generic name or by a program or company name. Applications for these programs are usually available online.
Eating, Diet, and Nutrition for Kidney Transplant Patients
The diet for transplant patients has more choices than the diet for dialysis patients, although you may still have to cut back on some foods. Your diet will probably change as your medicines, test results, weight, and blood pressure change.
- You may need to count calories. Your medicines may give you a bigger appetite and cause you to gain weight.
- You may have to eat less sodium. Your medicines may cause your body to retain sodium, leading to high blood pressure.
Your transplant center’s dietitian can help you understand the reasons for dietary limits, recognize foods you should avoid, and plan healthy and tasty meals.
What is conservative management for kidney failure?
Conservative management for kidney failure is the choice to say no to or stop dialysis treatments. For many people, dialysis not only extends life, it also improves the quality of life. For others who have serious conditions in addition to kidney failure, dialysis may seem like a burden that only prolongs suffering. If you have serious conditions in addition to kidney failure, dialysis may not prolong your life or improve the quality of your life.
You have the right to say no to or stop dialysis. You may want to speak with your doctor, spouse, family, counselor, or renal social worker, who helps people with kidney disease, to help you make this decision.
If you stop dialysis treatments or say you do not want to begin them, you may live for a few weeks or for several months, depending on your health and your remaining kidney function. You may choose to receive care from a hospice—a facility or home program designed to meet the physical and emotional needs of the terminally ill—during this time. Hospice care focuses on relief of pain and other symptoms. Whether or not you choose to use a hospice, your doctor can give you medicines to make you more comfortable. Your doctor can also give you medicines to treat the problems of kidney failure, such as anemia or weak bones. You may restart dialysis treatment if you change your mind.
Advance Directives
An advance directive is a statement or document in which you give instructions either to withhold certain treatments, such as dialysis, or to provide them, depending on your wishes and the specific circumstances. Even if you are happy with your quality of life on dialysis, you should think about circumstances that might make you want to stop dialysis treatments. At some point in a medical crisis, you might lose the ability to tell your health care team and loved ones what you want. Advance directives may include
- a living will
- a durable power of attorney for health care decisions
- a do not resuscitate (DNR) order—a legal form that tells your health care team you do not want cardiopulmonary resuscitation (CPR) or other life-sustaining treatment if your heart were to stop or if you were to stop breathing.
A living will is a document that details the conditions under which you would want to refuse treatment. You may state that you want your health care team to use all available means to sustain your life, or you may direct that you be withdrawn from dialysis if you fall into a coma from which you most likely won’t wake up. In addition to dialysis, you may choose or refuse the following life-sustaining treatments:
- CPR
- feedings through a tube in your stomach
- mechanical or artificial means to help you breathe
- medicines to treat infections
- surgery
- receiving blood
Refusing to have CPR is the same as a do not resuscitate (DNR) order. If you choose to have a do not resuscitate (DNR) order, your doctor will place the order in your medical chart.
A durable power of attorney for health care decisions or a health care proxy is a document you use to assign a person to make health care decisions for you in the event you cannot make them for yourself. Make sure the person you name understands your values and will follow your instructions.
Each state has its own laws on advance directives. You can obtain a form for an advance medical directive that’s valid in your state from the National Hospice and Palliative Care Organization.
Kidney failure diet
Your dialysis center has a renal dietitian to help you plan your meals. A renal dietitian has special training in caring for the food and nutrition needs of people with kidney disease. Work with a registered dietitian to develop a meal plan that includes foods that you enjoy eating while maintaining your kidney health.
Depending on your situation, kidney function and overall health, dietary recommendations might include the following:
- Avoid products with added salt or sodium. Lower the amount of sodium you eat each day by avoiding products with added salt, including many convenience foods, such as frozen dinners, canned soups and fast foods. Other foods with added salt include salty snack foods, canned vegetables, and processed meats and cheeses.
- Choose lower potassium foods. High-potassium foods include bananas, oranges, potatoes, spinach and tomatoes. Examples of low-potassium foods include apples, cabbage, carrots, green beans, grapes and strawberries. Be aware that many salt substitutes contain potassium, so you generally should avoid them if you have kidney failure.
- Limit the amount of protein you eat. Your registered dietitian will estimate how many grams of protein you need each day and make recommendations based on that amount. High-protein foods include lean meats, eggs, milk, cheese and beans. Low-protein foods include vegetables, fruits, breads and cereals.
Step 1: Choose and prepare foods with less salt and sodium
Why? To help control your blood pressure. Your diet should contain less than 2,300 milligrams of sodium each day 14.
- Buy fresh food often. Sodium (a part of salt) is added to many prepared or packaged foods you buy at the supermarket or at restaurants.
- Cook foods from scratch instead of eating prepared foods, “fast” foods, frozen dinners, and canned foods that are higher in sodium. When you prepare your own food, you control what goes into it.
- Use spices, herbs, and sodium-free seasonings in place of salt.
- Check for sodium on the Nutrition Facts label of food packages. A Daily Value of 20 percent or more means the food is high in sodium.
- Try lower-sodium versions of frozen dinners and other convenience foods.
- Rinse canned vegetables, beans, meats, and fish with water before eating.
Look for food labels with words like sodium free or salt free; or low, reduced, or no salt or sodium; or unsalted or lightly salted.
Why is knowing about sodium important for someone with advanced chronic kidney disease?
Too much sodium in a person’s diet can be harmful because it causes blood to hold fluid. People with chronic kidney disease need to be careful not to let too much fluid build up in their bodies. The extra fluid raises blood pressure and puts a strain on the heart and kidneys. A dietitian can help people find ways to reduce the amount of sodium in their diet. Nutrition labels provide information about the sodium content in food. The U.S. Food and Drug Administration advises that healthy people should limit their daily sodium intake to no more than 2,300 milligrams (mg), the amount found in 1 teaspoon of table salt. People who are at risk for a heart attack or stroke because of a condition such as high blood pressure or kidney disease should limit their daily sodium intake to no more than 1,500 mg. Choosing sodium-free or low-sodium food products will help them reach that goal.
Sodium is found in ordinary table salt and many salty seasonings such as soy sauce and teriyaki sauce. Canned foods, some frozen foods, and most processed meats have large amounts of salt. Snack foods such as chips and crackers are also high in salt.
Alternative seasonings such as lemon juice, salt-free seasoning mixes, and hot pepper sauce can help people reduce their salt intake. People with advanced chronic kidney disease should avoid salt substitutes that use potassium, such as AlsoSalt or Nu-Salt, because chronic kidney disease limits the body’s ability to eliminate potassium from the blood. The table below provides some high-sodium foods and suggestions for low-sodium alternatives that are healthier for people with any level of chronic kidney disease who have high blood pressure.
| High-sodium Foods | Low-sodium Alternatives |
|---|---|
|
|
Why is knowing about potassium important for someone with advanced chronic kidney disease?
Keeping the proper level of potassium in the blood is essential. Potassium keeps the heart beating regularly and muscles working right. Problems can occur when blood potassium levels are either too low or too high. Damaged kidneys allow potassium to build up in the blood, causing serious heart problems. Potassium is found in many fruits and vegetables, such as bananas, potatoes, avocados, and melons. People with advanced chronic kidney disease may need to avoid some fruits and vegetables. Blood tests can indicate when potassium levels have climbed above normal range. A renal dietitian can help people with advanced chronic kidney disease find ways to limit the amount of potassium they eat. The potassium content of potatoes and other vegetables can be reduced by boiling them in water. The following table gives examples of some high-potassium foods and suggestions for low-potassium alternatives for people with advanced chronic kidney disease.
| High-potassium Foods | Low-potassium Alternatives |
|---|---|
|
|
Why is knowing about phosphorus important for someone with advanced chronic kidney disease?
Damaged kidneys allow phosphorus, a mineral found in many foods, to build up in the blood. Too much phosphorus in the blood pulls calcium from the bones, making the bones weak and likely to break. Too much phosphorus may also make skin itch. Foods such as milk and cheese, dried beans, peas, colas, canned iced teas and lemonade, nuts, and peanut butter are high in phosphorus. A renal dietitian can help people with advanced chronic kidney disease learn how to limit phosphorus in their diet.
As chronic kidney disease progresses, a person may need to take a phosphate binder such as sevelamer hydrochloride (Renagel), lanthanum carbonate (Fosrenol), calcium acetate (PhosLo), or calcium carbonate (Tums) to control the phosphorus in the blood. These medications act like sponges to soak up, or bind, phosphorus while it is in the stomach. Because it is bound, the phosphorus does not get into the blood. Instead, it is removed from the body in the stool.
The table below lists some high-phosphorus foods and suggestions for low-phosphorus alternatives that are healthier for people with advanced chronic kidney disease.
| High-phosphorus Foods | Low-phosphorus Alternatives |
|---|---|
|
|
Step 2: Eat the right amount and the right types of protein
Why? To help protect your kidneys. When your body uses protein, it produces waste. Your kidneys remove this waste. Eating more protein than you need may make your kidneys work harder.
- Eat small portions of protein foods.
- Protein is found in foods from plants and animals. Most people eat both types of protein. Talk to your dietitian about how to choose the right combination of protein foods for you.
When kidney function declines to the point where dialysis becomes necessary, patients should include more protein in their diet because dialysis removes large amounts of protein from the blood.
Animal-protein foods:
- Chicken
- Fish
- Meat
- Eggs
- Dairy
A cooked portion of chicken, fish, or meat is about 2 to 3 ounces or about the size of a deck of cards. A portion of dairy foods is ½ cup of milk or yogurt, or one slice of cheese.
Plant-protein foods:
- Beans
- Nuts
- Grains
A portion of cooked beans is about ½ cup, and a portion of nuts is ¼ cup. A portion of bread is a single slice, and a portion of cooked rice or cooked noodles is ½ cup.
Step 3: Choose foods that are healthy for your heart
Why? To help keep fat from building up in your blood vessels, heart, and kidneys. To help keep fat from building up in your blood vessels, heart, and kidneys.
- Grill, broil, bake, roast, or stir-fry foods, instead of deep frying.
- Cook with nonstick cooking spray or a small amount of olive oil instead of butter.
- Trim fat from meat and remove skin from poultry before eating.
- Try to limit saturated and trans fats. Read the food label.
Heart-healthy foods:
- Lean cuts of meat, such as loin or round
- Poultry without the skin
- Fish
- Beans
- Vegetables
- Fruits
- Low-fat or fat-free milk, yogurt, and cheese
Limit alcohol
Drink alcohol only in moderation: no more than one drink per day if you are a woman, and no more than two if you are a man. Drinking too much alcohol can damage the liver, heart, and brain and cause serious health problems. Ask your health care provider how much alcohol you can drink safely.
A renal dietitian can help people learn about the amount and sources of protein in their diet. Animal protein in egg whites, cheese, chicken, fish, and red meats contain more of the essential nutrients a body needs. With careful meal planning, a well-balanced vegetarian diet can also provide these nutrients. A renal dietitian can help people with advanced chronic kidney disease make small adjustments in their eating habits that can result in significant protein reduction. For example, people can lower their protein intake by making sandwiches using thinner slices of meat and adding lettuce, cucumber slices, apple slices, and other garnishes. The following table lists some higher-protein foods and suggestions for lower-protein alternatives that are better choices for people with chronic kidney disease trying to limit their protein intake.
Why is it important to keep track of how much liquid you eat or drink?
You may feel better if you keep track of and limit how much liquid you eat and drink. Excess fluid can build up in your body and may cause
- swelling and weight gain between dialysis sessions
- changes in your blood pressure
- your heart to work harder, which can lead to serious heart trouble
- a buildup of fluid in your lungs, making it hard for you to breathe
Hemodialysis removes extra fluid from your body. However, hemodialysis can remove only so much fluid at a time safely. If you come to your hemodialysis with too much fluid in your body, your treatment may make you feel ill. You may get muscle cramps or have a sudden drop in blood pressure that causes you to feel dizzy or sick to your stomach.
Your health care provider can help you figure out how much liquid is right for you.
One way to limit how much liquid you have is to limit the salt in the foods you eat. Salt makes you thirsty, so you drink more. Avoid salty foods such as chips and pretzels.
Your renal dietitian will give you other tips to help you limit how much liquid you consume while making sure you don’t feel too thirsty.
What foods count as liquid and why?
Foods that are liquid at room temperature, such as soup, contain water. Gelatin, pudding, ice cream, and other foods that include a lot of liquid in the recipe also count. Most fruits and vegetables contain water, such as melons, grapes, apples, oranges, tomatoes, lettuce, and celery. When you count up how much liquid you have in a day, be sure to count these foods.
What is your dry weight?
Your dry weight is your weight after a hemodialysis session has removed all extra fluid from your body. Controlling your liquid intake helps you stay at your proper dry weight. If you let too much fluid build up between sessions, it is harder to achieve your dry weight. Your health care provider can help you figure out what dry weight is right for you.
My dry weight goal: _____________.
Should you take vitamin and mineral supplements?
You may not get enough vitamins and minerals in your diet because you have to avoid so many foods. Hemodialysis also removes some vitamins from your body. Your health care provider may prescribe a vitamin and mineral supplement designed specifically for people with kidney failure.
Warning: Do not take nutritional supplements you can buy over the counter. These supplements may contain vitamins or minerals that are harmful to you. For safety reasons, talk with your health care provider before using probiotics, dietary supplements, or any other medicine together with or in place of the treatment your health care provider prescribes.
Living with chronic kidney disease
Many people with chronic kidney disease (CKD) are able to live long lives without being unduly affected by the condition. Although it’s not possible to repair damage that has already happened to your kidneys, CKD will not necessarily get worse. CKD only reaches an advanced stage in a small proportion of people. But even if your condition is mild, it’s important to take good care of yourself to help stop it getting worse and reduce your risk of other health problems, such as cardiovascular disease.
Take your medicine
It’s very important that you take any prescribed medicine, even if you do not feel unwell. Some medicines are designed to prevent serious problems from happening in the future.
It’s also useful to read the information leaflet that comes with the medicine about possible interactions with other medicines or supplements.
Check with your kidney healthcare team if you plan to take any painkillers or nutritional supplements. These can sometimes affect your kidneys or interfere with your medicine.
Also speak to your kidney healthcare team if you have any concerns about the medicine you are taking, or if you’re experiencing any side effects.
Have a healthy diet
A healthy, balanced diet can help improve your general health and reduce your risk of developing further problems.
A balanced diet should include:
- plenty of fruit and vegetables – aim for at least 5 portions a day
- meals that include starchy foods, such as potatoes, wholegrain bread, rice or pasta
- some dairy or dairy alternatives
- some beans or pulses, fish, eggs, or meat as a source of protein
- low levels of saturated fat, salt and sugar
You may also be given advice about dietary changes that can specifically help with kidney disease, such as limiting the amount of potassium or phosphate in your diet.
Exercise regularly
Regular physical activity can also help improve your general health. Do not be scared to exercise. Exercise is good for anyone with kidney disease, however severe. Not only will exercise boost your energy, help you sleep, strengthen your bones, ward off depression and keep you fit, it may also reduce your risk of problems such as heart disease.
If you have mild to moderate CKD, your ability to exercise should not be reduced. You should be able to exercise as often and as vigorously as someone the same age as you with healthy kidneys.
If your condition is more advanced or you’re already on dialysis, your ability to exercise is likely to be reduced and you may become breathless and tired more quickly. But exercise is still beneficial. Start slowly and build up gradually. Check with your doctor before beginning a new exercise program.
Stop smoking
If you smoke, stopping smoking can improve your overall health and reduce your risk of many other health problems.
Limit your alcohol consumption
You may still be able to drink alcohol if you have kidney disease, but it’s advisable not to exceed the recommended limits of more than 14 alcohol units a week.
Speak to your doctor if you find it difficult to cut down the amount of alcohol you drink.
Get vaccinated
Kidney disease can put a significant strain on your body and make you more vulnerable to infections. Everyone with kidney disease is encouraged to have the annual flu jab and the one-off pneumococcal vaccination.
Sex
Having CKD can affect a sexual relationship. Some couples become closer after a diagnosis of CKD, while others find their loved ones are affected by worries about how they’ll cope with the illness.
Both men and women may have issues about body image and self-esteem, and this can affect a relationship. Problems such as erectile dysfunction and reduced sex drive are also fairly common in people with CKD. Try to share your feelings with your partner. If you have problems with sex that do not get better with time, speak to your kidney care team. Treatment and support is available.
Pregnancy
If you have mild to moderate kidney disease, it’s unlikely your condition or its treatment will affect your chances of having children.
More advanced kidney disease may affect a woman’s periods and reduce a man’s sperm count, which can make it more difficult to get pregnant, although this does not mean you will not be able to have a child.
It’s important to use contraception if you do not want to get pregnant.
If you do want to try for a baby, it’s a good idea to speak to your healthcare team for advice first. There may be risks to mother and baby, and changes to your treatment or check-ups may be necessary.
Can you continue to work with kidney failure?
Yes, many people with kidney failure continue to work. Your employer may give you lighter physical jobs or schedule your work hours around your hemodialysis sessions. If you are on peritoneal dialysis, you will need space and time to change the dialysis solution in the middle of the work day. Most employers are happy to make these changes.
As a result of the Americans with Disabilities Act, an employer cannot fire you because you are on dialysis or had a kidney transplant. The law requires an employer to make reasonable adjustments to the workplace for a person with a disability. If your employer is not willing to meet your needs, your dialysis clinic’s renal social worker may be able to help find a way to satisfy both you and your employer. As a last resort, you may need to file a complaint with the Equal Employment Opportunity Commission. Your renal social worker may be able to help you with this complaint, or you may need the help of a lawyer. Many times, just the mention of legal action is enough to cause an employer to make reasonable changes in the workplace.
Can you be active with kidney failure?
Yes. Physical activity is an important part of staying healthy when you have kidney failure. Being active makes your muscles, bones, and heart stronger. Physical activity also makes your blood circulate faster so your body gets more oxygen. Your body needs oxygen to use the energy from food. If you are on dialysis, physical activity can help more wastes move into your blood for dialysis to remove them.
You will find that physical activity can also improve your mood and give you a sense of well-being.
Talk with your doctor before you start an exercise routine. Start slow, with easier activities such as walking at a normal pace or gardening. Work up to harder activities such as walking briskly or swimming. Aim for at least 30 minutes of exercise most days of the week.
Chronic kidney disease prognosis
Chronic kidney disease usually progresses slowly. Blood and urine tests can help doctors to decide whether the kidneys are still working well enough or whether dialysis will be needed soon, for example.
The health implications of chronic kidney disease will also depend on how healthy someone is otherwise. For that reason, doctors also look into conditions that may make chronic kidney disease get worse faster – including heart disease, poorly regulated high blood pressure or diabetes. This is important for individually adjusting treatment with medication or for planning further treatment steps far enough in advance. Someone who has a high risk of kidney failure in the foreseeable future can talk about what treatment would be best with their doctor before it’s too late. Furthermore frequent testing might also be needed.
Significant racial and ethnic differences exist in the incidence and prevalence rates of end-stage renal disease (ESRD) 15. The highest incidence is found in African Americans; followed by American Indians and Alaska Natives; followed by Asian Americans, Native Hawaiians, and other Pacific Islanders; followed by whites. Hispanics have higher incidence rates of ESRD than non-Hispanics 15.
Early-stage CKD and ESRD are associated with increased morbidity and health care utilization rates. A review of the USRDS 2009 annual data report suggests that the number of hospitalizations in ESRD patients is 1.9% per patient-year. In a study by Khan SS et al. 16, the prevalence of cardiovascular disease, cerebrovascular disease, and peripheral vascular disease in earlier stages of CKD was comparable to those in the US dialysis population. It was also found that patients with CKD had 3-fold higher rates of hospitalization and hospital days spent per patient-year compared to the general US population. CKD patients are at a higher risk of hospitalization and cardiovascular diseases and the risk increases with a decline in GFR.
Patients with CKD and particularly end-stage renal disease (ESRD) are at increased risk of mortality, particularly from cardiovascular disease 15. A review of USRDS 2009 data suggests that 5-year survival probability in a patient on dialysis is only around 34% 15.
- CKD Stages. https://ukkidney.org/health-professionals/information-resources/uk-eckd-guide/ckd-stages[↩][↩]
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2019. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2019.[↩][↩][↩]
- U.S. Renal Data System, USRDS 2016 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2016.[↩]
- Race, Ethnicity, & Kidney Disease. https://www.niddk.nih.gov/health-information/kidney-disease/race-ethnicity[↩]
- Kidney Failure. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure[↩]
- Smith HW The Kidney: Structure and Function in Health and DiseaseNew YorkOxford Univ Pr, 1951, pg. 520-74[↩]
- Lindeman RD, TobinJ, ShockNW. Longitudinal studies on the rate of decline in renal function with age, J Am Geriatr Soc, 1985, vol. 33, pg. 278-85[↩]
- ManjunathG, TighiouartH, CoreshJ, MacleodB, SalemDN, GriffithJL. Level of kidney function as a risk factor for cardiovascular outcomes in the elderly, Kidney Int, 2003, vol. 63, pg. 1121-1129[↩]
- Aronoff GR, Berns JS, BrierME, GolperTA, MorrisonG, SingerI. Drug Prescribing in Renal Failure: Dosing Guidelines for AdultsPhiladelphiaAmerican College of Physicians, 2002[↩]
- CoreshJ, AstorBC, GreeneT, EknoyanG, LeveyAS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey, Am J Kidney Dis, 2003, vol. 41, pg. 1-12[↩]
- ObradorGT, AroraPKauszAT, RuthazerR, PereiraBJ, LeveyAS. Level of renal function at the initiation of dialysis in the U.S. end-stage renal disease population, Kidney Int, 1999, vol. 56, pg. 2227-35[↩]
- Aeddula NR, Bardhan M, Baradhi KM. Sickle Cell Nephropathy. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526017[↩]
- http://nkdep.nih.gov/professionals/gfr_calculators/gfr_faq.htm[↩]
- Eating Right for Chronic Kidney Disease. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/eating-nutrition[↩]
- Vaidya SR, Aeddula NR. Chronic Renal Failure. [Updated 2022 Oct 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535404[↩][↩][↩][↩]
- Khan SS, Kazmi WH, Abichandani R, Tighiouart H, Pereira BJ, Kausz AT. Health care utilization among patients with chronic kidney disease. Kidney Int. 2002 Jul;62(1):229-36. doi: 10.1046/j.1523-1755.2002.00432.x[↩]