Contents
What is ciguatera
Ciguatera or ciguatera fish poisoning is caused by eating fish contaminated with the naturally occurring toxins, ciguatoxins, that are produced by microorganisms that live around coral reefs. Multiple ciguatoxins have been identified and ciguatoxins are derived from benthic dinoflagellates of the genus Gambierdiscus, growing predominantly in association with macroalgae in coral reefs in tropical and subtropical climates 1. Small fish eat the microorganisms, and large fish eat the small fish, which concentrates the ciguatoxins. The toxins accumulate in the flesh of reef dwelling fish, particularly predatory species, which are then harvested either commercially or by recreational fishermen. The highest concentrations of toxins are found in the liver, intestines, eggs, and head. The toxin is transferred through the food web as the toxic marine algae is consumed by herbivorous fish, which are consumed by carnivorous fish, which are in turn consumed by humans 2. Barracuda, black grouper, blackfin snapper, cubera snapper, dog snapper, greater amberjack, hogfish, horse-eye jack, king mackerel, and yellowfin grouper have been known to carry ciguatoxins 3. It is important to note that not all fish within a given reef or common catch area are equally toxic; toxin levels of fish caught side by side may vary greatly.
Ciguatoxins are commonly found in tropical or subtropical areas worldwide between 35° north latitude and 35° south latitude, which includes the South Atlantic Ocean bordering the Caribbean Sea, the Caribbean Sea, the South Pacific Ocean, the Indian Ocean and the Gulf of Mexico (including the Flower Garden Banks National Marine Sanctuary). Because ciguatoxic endemic areas are localized, primary seafood processors should recognize and avoid purchasing fish from established and emerging areas of concern 4.
Because fish can be shipped around the world, ciguatera can occur anywhere, including in the United States. However, the risk is highest in fish from the Caribbean Sea and the Pacific and Indian Oceans. As many as 3% of travelers to these areas get ciguatera. Ciguatera is most commonly caused by eating barracuda, grouper, moray eel, amberjack, sea bass, sturgeon, parrot fish, surgeonfish, and red snapper.
People who have ciguatera fish poisoning may experience gastrointestinal symptoms such as nausea, vomiting, diarrhea, and neurologic symptoms such as numbness and tingling of the lips and fingers or toes (paresthesias), itching of hands and feet (pruritis), joint pain (arthralgia), muscle pain (myalgia), headache, reversal of hot and cold sensation, acute and extreme sensitivity to temperature, dizziness, vertigo, and muscular weakness (myasthenia). Cardiovascular symptoms may occur and include irregular heartbeat (arrhythmia) including slow heartbeat (bradycardia) or rapid heartbeat (tachycardia), and low blood pressure. People also may find that cold things feel hot and hot things feel cold. Ciguatera has no cure. Symptoms usually go away in days or weeks but can last for years.
The onset of ciguatera fish poisoning usually occurs within 6 hours after consumption of toxic fish and generally subsides from several days to a few weeks. However, severe cases have been known to cause recurring neurological symptoms lasting for months to years.
People who have ciguatera can be treated for their symptoms.
What type of toxin is ciguatera toxin?
Ciguatera fish poisoning or ciguatera is an illness caused by eating fish that contain ciguatera toxins (ciguatoxins) produced by a marine microalgae called Gambierdiscus toxicus.
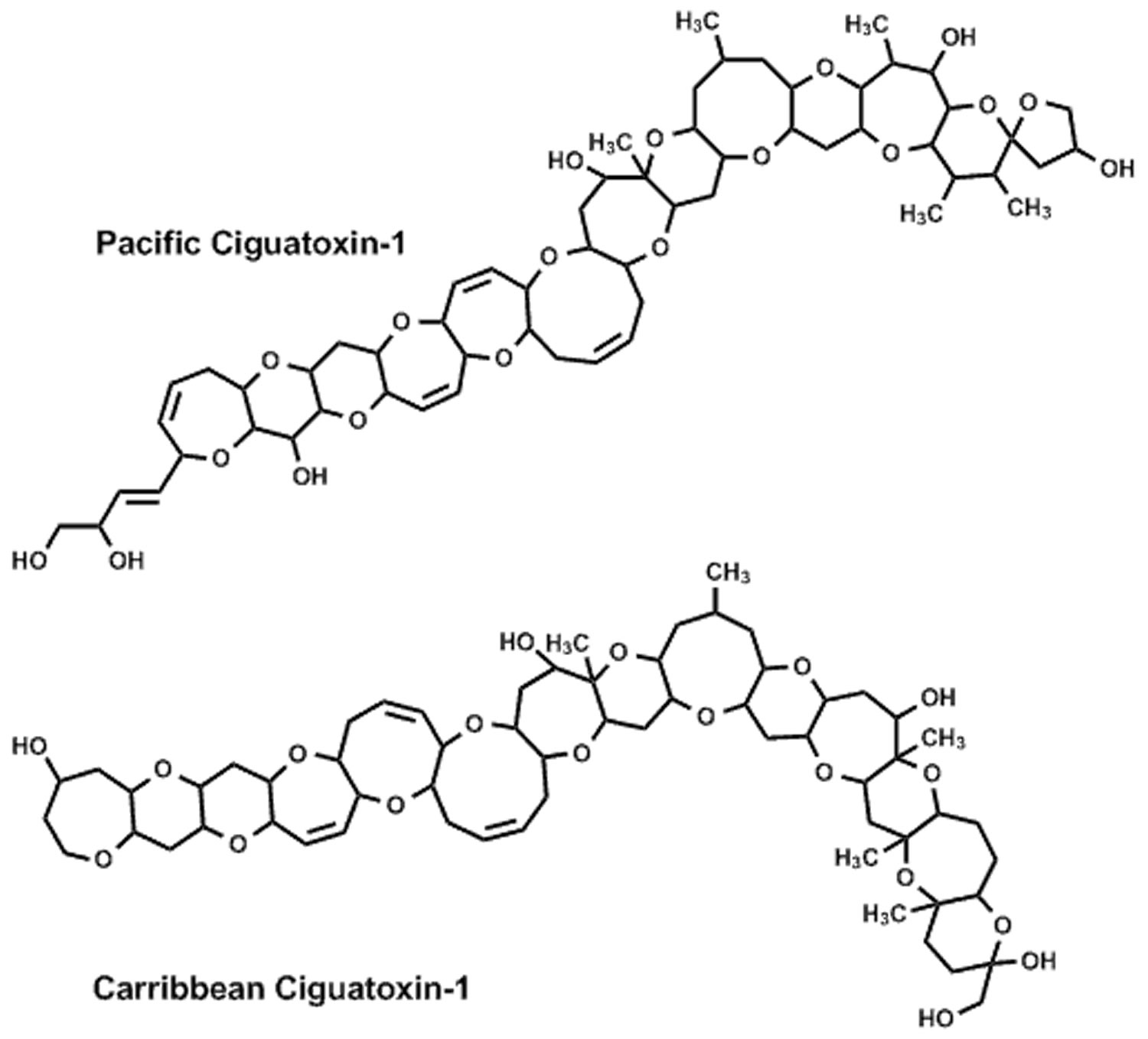
Figure 1. Ciguatera toxins
Ciguatera prevention
There is no treatment for ciguatera, so travelers should avoid eating the fish listed above, particularly barracuda and moray eel, and avoid eating the organs in which the concentration of toxins is highest. The toxins that cause ciguatera do not affect the appearance, taste, or smell of fish, so there is no way to tell if fish is contaminated. The toxins are not destroyed by heat, so even thoroughly cooked fish is a risk.
Prevention of ciguatera fish poisoning relies on the individual’s avoidance of fish that have a greater likelihood of ciguatoxicity 5. Local residents in endemic areas often report being aware of specific reefs and/or seasons to avoid when fishing. Local residents also report a variety of simple home tests to detect toxic fish, but none of these are scientifically validated.
Intoxication is associated with consumption of large reef fish, and greater illness severity is associated with eating the fish viscera and larger portions 6. Thus, people are advised to avoid eating the viscera of reef fish. It is also advisable to avoid consuming large predatory reef fish from areas known to be associated with ciguatera fish poisoning. With regard to fish size, avoidance of fish in excess of 3 kilograms (approximately 6.6 pounds) 7, or even more conservatively, avoidance of fish in excess of 1.35 kilograms (approximately 3 pounds) 8 has been recommended. It has also been proposed that eating small portions (i.e. <50 grams or < 0.11 pounds) of different fish is safer than eating larger portions of any individual fish that might be associated with ciguatera fish poisoning 6.
Some common ciguatoxic fish to avoid (although any large coral reef fish has the potential to be ciguatoxic) 5:
- Moray eel
- Barracuda
- Grouper
- Kingfish
- Jacks
- Snapper
- Surgeonfish
- Parrot fish
- Wrasses
- Hogfish
- Narrow barred Spanish mackerel
- Coral trout
- Flowery cod
- Red emperor
The following are also associated with ciguatera fish poisoning:
- Eating fish viscera or roe 9
- Large, predatory reef fish 10
- Reef fish from areas known to be associated with ciguatera fish poisoning occurrence 6
Note that eating small portions (i.e. <50 grams or <0.11 pounds) of different fish may be safer 11 than eating larger portions (i.e. >200 grams) of any one potentially ciguatoxic fish 6.
Ciguatera symptoms
Ciguatera poisoning symptoms usually develop 1–3 hours after eating contaminated fish and generally subsides from several days to a few weeks. Ciguatera poisoning symptoms can include nausea, vomiting, diarrhea, and stomach pain. Some people may have neurologic symptoms, such as a tingling sensation, tooth pain or feeling as if the teeth are loose, itching, a metallic taste in the mouth, and blurred vision.
People who have ciguatera fish poisoning may experience gastrointestinal symptoms such as nausea, vomiting, diarrhea, and neurologic symptoms such as numbness and tingling of the lips and fingers or toes (paresthesias), itching of hands and feet (pruritis), joint pain (arthralgia), muscle pain (myalgia), headache, reversal of hot and cold sensation, acute and extreme sensitivity to temperature, dizziness, vertigo, and muscular weakness (myasthenia). Cardiovascular symptoms may occur and include irregular heartbeat (arrhythmia) including slow heartbeat (bradycardia) or rapid heartbeat (tachycardia), and low blood pressure. People also may find that cold things feel hot and hot things feel cold. Ciguatera has no cure. Symptoms usually go away in days or weeks but can last for years. Severe cases have been known to cause recurring neurological symptoms lasting for months to years.
Symptom recurrence and sensitization
There are reports of sensitization to ciguatoxins in ciguatera fish poisoning patients; that is, individuals who previously suffered from ciguatera fish poisoning have been reported to experience recurrence of ciguatera fish poisoning symptoms after eating a potentially ciguateric fish that did not produce symptoms in other individuals 12. Also, anecdotal reports indicate that some patients experience recurrence of neurologic ciguatera fish poisoning symptoms upon consuming alcohol, any type of fish, and certain other foods (see below), even years after the initial exposure 13. When this occurs many years after exposure, however, alternative etiologies for symptoms should be ruled out, given that apparent ciguatera fish poisoning symptoms and signs may actually be indicators of other severe pathology 7. Such reports of recurrence have not been noted for cardiac or gastrointestinal symptoms.
Foods and behaviors associated with symptom recurrence:
- Alcohol
- Nuts
- Caffeine
- Pork
- Chicken
- Any kind of fish
- Physical activity/exertion
One theory to explain the recurrence of neurologic symptoms is that ingested ciguatera toxin may be stored in a person’s adipose tissue, and that any activity involving increased lipid metabolism may result in ciguatoxins re-entering the blood stream, with subsequent re-emergence of ciguatera fish poisoning symptoms 14. Alternatively, symptom recurrence may be related to immunologically mediated sensitization to ciguatera toxin after initial exposure 7.
Ciguatera diagnosis
There are currently no reliable biomarkers that can be used to confirm exposure to ciguatera toxin in humans, although studies using animals 15 indicate that detection of ciguatera toxin in human blood or serum may be possible in the near future.
At present, therefore, ciguatera fish poisoning diagnosis is based on the presenting symptoms and time course, the history of having eaten a reef fish (as opposed to shellfish as in Neurotoxic Shellfish Poisoning), and importantly, the exclusion of other diagnoses that could account for the symptoms. Ciguatera fish poisoning has symptoms in common with Paralytic and Neurotoxic Shellfish Poisonings, scombroid and pufferfish toxicity, botulism, enterovirus 71, and bacteremia 7, as well as organophosphate pesticide poisoning, eosinophilic meningitis, multiple sclerosis, and other neurologic conditions.
The current gold standard diagnosis of ciguatera fish poisoning would include confirmation of ciguatera toxin in the consumed fish by appropriate laboratory methods. Also, multiple individuals consuming the same fish, with all individuals experiencing signs, symptoms and time course consistent with ciguatera fish poisoning, strongly supports the ciguatera fish poisoning diagnosis 16.
Detection in fish
Although diagnostic methods for detecting ciguatera toxins in human specimens are still under development, methods for detecting the toxins in samples of the implicated fish have been developed, and the results have been used to support clinical diagnoses of ciguatera fish poisoning in the United States, Caribbean and South Pacific. Within the USA, laboratories of the Food and Drug Administration (FDA) perform ciguatera toxins analyses on fish to assist in the ciguatera fish poisoning diagnosis of patients. Remnants of consumed fish can be submitted to the FDA for analysis. However, because the results of such analyses are generally not immediately available to the physician at the time of the patient’s initial presentation and examination, initial care of the patient must proceed based on symptom progression, recent fish-eating history, and exclusion of alternative diagnoses or explanations.
The FDA fish testing procedure is a two-tiered protocol involving: 1) in vitro assay, i.e. a high-throughput screen for toxicity consistent with ciguatoxin’s mode of action; and 2) an analytical chemistry technique known as liquid chromatography-mass spectrometry (LC-MS).
In the first tier, suspect fish specimens are screened for the specific effects of ciguatera toxins. Specifically, fish specimens are screened for voltage-gated sodium channel–specific activating effects on cell membranes. The screening procedure used is the in vitro mouse neuroblastoma (N2a) cell assay (American Type Culture Collection CCL-131), using a ouabain-veratridine dependent method 17. Through appropriate experimental design, this screening method can detect effects of algal toxins on sodium channels in cell membranes, can discriminate between effects of toxins that activate (e.g. brevetoxins, ciguatoxins) versus block (e.g. tetrodotoxins, saxitoxins) voltage-gated sodium channels, and can discriminate between the effects of sodium channel specific toxins and toxins with other modes of action. However, this screening procedure does not identify specifically the sodium channel active agent present in the fish tissue. Therefore, in the second tier, fish samples that test positive for sodium channel specific toxicity are subjected to LC-MS, to confirm the molecular presence of ciguatera toxins in the fish tissue. Multiple Reaction Monitoring (MRM) is used to selectively detect product ions from ciguatoxin precursor ions. This method provides a high level of specificity for detecting ciguatera toxins in fish 18.
Of note, alternative methods for ciguatera toxins detection in fish tissues with equivalent or lesser sensitivity and specificity have been reported, and include receptor binding assay which is also sodium channel specific and is considered to be sensitive 19; liquid chromatography-mass spectrometry methods 20; and a host of other less frequently employed assay systems 21.
While the fish analysis procedures described here are performed generally in specially equipped laboratories by trained professionals, attempts have been made to develop simpler procedures that are cost-effective and can be used to detect ciguatera toxins on a routine basis by fishermen, fish vendors or consumers. However, developing such simplified techniques involves substantial challenges, including the low levels of ciguatera toxins present in ciguateric fish (<0.05 parts per billion for one common type of ciguatera toxins molecule), multiple structural toxin forms present within a single fish, and the small quantities of ciguatera compounds available for research 11. A membrane immunobead assay was developed in Hawaii 22 as a simplified ciguatoxin detection procedure, but available studies evaluating the immunobead procedure on samples from the Caribbean and from Hong Kong revealed false negative detection rates ranging from 50–82%, and false positive rates ranging from 33–44% 23. To date, there is no commercially available fish-testing product that has been demonstrated by independent investigation to provide ciguatoxin detection with adequate accuracy 23.
Access to ciguatera toxins for research purposes is a significant challenge. Purified ciguatera toxins from the Caribbean and Pacific are not widely available for laboratory experimentation due to the low amount of toxin present in fish, although a few specialized laboratories have purified sufficient quantities for research and outbreak investigations 24.
Ciguatera treatment
Over the years, a myriad of treatments, mostly responding to ciguatera fish poisoning symptoms, have been tried. However, there have been few well-designed randomized controlled trials investigating the effectiveness of specific treatments for ciguatera fish poisoning. Some of the research design challenges and problems include the relative infrequency and irregularity of ciguatera fish poisoning’s occurrence, lack of resources for conducting scientific treatment investigations in those places where it occurs with greater frequency, the inability to confirm the diagnosis of ciguatera fish poisoning using a human biological assay, small numbers of patients (which is particularly problematic when attempting to compare subgroups of participants), variability among study participants in time to treatment, and potential differences between Pacific, Indian Ocean, and Caribbean toxins and their effects. In addition, in the ciguatera fish poisoning literature, unless fish testing was available, it is generally unknown if the case reports and even clinical trials of ciguatera fish poisoning treatments were treating actual cases of ciguatera fish poisoning.
Symptomatic and supportive treatments
With acute ciguatera fish poisoning, support of any depressed vital functions is of utmost importance 6, and supportive therapies may be necessary for controlling fluid and electrolyte balance 11. As in any acute poisoning, IV fluid resuscitation with large volumes of isotonic fluids may be necessary for patients in shock, with the addition of an IV pressor infusion if needed after volume repletion. Symptomatic bradycardia may require IV atropine dosing as needed (0.5 mg every 5 minutes to maintain a heart rate goal of 60 beats per minute, with no maximum total dosage limit) and/or temporary cardiac pacing. Rarely, critically ill ciguatera fish poisoning patients may require endotracheal intubation and mechanical ventilation for either airway protection if comatose or for respiratory failure. The prognosis for full recovery of critically ill patients is excellent with intensive care treatment when needed. Also, patients seen within the first few hours after ingestion of toxic fish may benefit from treatment with oral activated charcoal to prevent further absorption of toxin from the gut, although ongoing severe vomiting and diarrhea may prevent this 25.
Various medical treatments for other ciguatera fish poisoning symptoms have been tried, but with variable success 26 and without randomized controlled trials to establish their effectiveness for this purpose. For instance, fluoxetine has been used for chronic fatigue 27; amitriptyline for paresthesias, pruritis and headaches 28; and paracetemol (acetaminophen) and nifedipine for headaches 27. Gabapentin has been used to treat pain 29 but caution is warranted in prescribing medications with addiction potential, given that there are no randomized controlled trials examining their safety and effectiveness for ciguatera fish poisoning, that patients’ complaints may last for months, and that chronic complaints may be confounded with psychiatric or other medical causes. It has been recommended that opiates and barbiturates be avoided since they may lead to hypotension, and because opiates may interact with maitotoxin, a natural marine toxin that may also be present in ciguatoxic fish 30.
There is also a variety of traditional herbal medicines and remedies that have been used to treat ciguatera. For instance, 64 different plant species have been reportedly used in the Western Pacific 31, and extracts of Argusia argentea leaves or Davalliea sp. have been reported in New Caledonia 32. However, there is no scientific evidence demonstrating that these remedies are safe or effective in treating ciguatera fish poisoning 14.
Mannitol
Intravenous (IV) mannitol infusion is the most studied therapy for ciguatera fish poisoning, and the only therapy evaluated by randomized blinded clinical trials 33. IV mannitol is administered at 0.5 to 1.0 g/kg body weight over a 30–45 minute period. It is suggested that it be given within 48–72 hours of ingestion of toxic fish 34, although beneficial effects have been observed even up to several weeks after intoxication 35. The effect of mannitol infusion is thought to be mediated by the osmotic reduction of neuronal edema 36. Also, mannitol may act as a scavenger of free radicals generated by the ciguatera toxins molecule, and may reduce the action of ciguatera toxins at sodium and/or potassium channels 37. Nicholson and Lewis note that hazards of mannitol’s clinical use include loss of further fluids in patients suffering from acute diarrhea and vomiting, and that patients experiencing bradycardia and hypotension are at higher risk of cardiac failure if infused with high doses of mannitol 14. Lewis and King 6 indicated that mannitol should not be administered until the patient is adequately rehydrated. Mannitol therapy has been recommended for two primary goals: reduction of acute symptoms (especially neurologic) and possible prevention of chronic neurologic symptoms.
Early descriptive reports on the use of IV mannitol suggested that it provided significant, rapid improvement and even resolution of acute ciguatera fish poisoning signs and symptoms. Also, based on the anecdotal reports that individuals treated with IV mannitol appeared to show reduced likelihood of returning for additional medical care, it was suggested that IV mannitol may even prevent the development of chronic ciguatera fish poisoning symptoms 35. Palafox et al. 38 described 24 cases, 17 of whom experienced complete resolution of ciguatera fish poisoning symptoms within 48 hours of infusion, including two cases of coma and one case of shock who improved within minutes of infusion. They suggested that treatment with IV mannitol was associated with shortened time of significant morbidity and shortened hospital stays, based on their clinical experience. Another early report 39 examined 12 ciguatera fish poisoning cases, and indicated that IV mannitol was generally effective at alleviating symptoms when administered within several days of fish ingestion. Notably, in this report, one case showed complete recovery by 24 hours after ingestion without any treatment.
Blythe et al. 40 provided a descriptive report on the experience of local South Florida practitioners using IV mannitol to treat patients with acute and chronic ciguatera fish poisoning symptoms. The report described 70 ciguatera fish poisoning cases treated with IV mannitol; the mean time from exposure to clinical presentation was 11.5 days. The study indicated that 29 of the 32 (91%) patients who received mannitol within 48 hours of presumed exposure experienced complete reversal of symptoms. In addition, IV mannitol was associated with moderate reduction, and in some patients complete resolution, of symptoms if given from 3–14 days after exposure; there was also a reported benefit when administered up to 70 days after exposure. Multiple treatments (e.g., up to four additional infusions) were necessary in five individuals. The authors reported that there were no adverse effects of mannitol treatment. Although 37 non-mannitol patients were included in the case series, analysis comparing symptom outcome between mannitol and non-mannitol treated patients was not reported, and there was no randomization or blinding employed as part of the study design, so it cannot be ruled out that patient or interviewer expectations, rather than the mannitol itself, accounted for all or part of the reported benefit in patients who received mannitol.
A study by Bagnis et al. 41 randomized 63 ciguatera fish poisoning patients in French Polynesia to one of two treatment groups: IV mannitol infusion (n=34), or “standard” treatment (n=29) which included intravenous infusion of glucose, Vitamin B and calcium gluconate. Results indicated a statistically significant, greater reduction in symptomatology in the mannitol group compared to the standard treatment group.
Schnorf et al. 33 conducted a double-blind, randomized study of mannitol treatment. Fifty patients were included in the study and were randomized to either mannitol treatment (n=25) or normal saline infusion (n=25). Results indicated that both treatments were associated with clinical improvement and to a similar degree, and mannitol was not superior to saline. However, 25% of the mannitol group received their mannitol between 69 hours and 672 hours (28 days) after symptom onset, which is generally beyond the 48–72 hour period recommended by other reports 40, and which may have obscured the identification of benefits in patients who received it early on. The authors then compared outcome of patients receiving mannitol within 24 hours to those receiving it after 24 hours, and found no difference. However this subpopulation analysis suffered from small sample size. In addition, by truncating the group at 24 hours post symptom onset rather than 48–72 hours (which has been associated with mannitol benefit), true difference in benefits may have been diluted in the comparison. Also, as is common in ciguatera fish poisoning treatment studies, the results may have been confounded by potential ciguatera fish poisoning misdiagnoses among study participants, since the diagnosis of ciguatera fish poisoning cannot be confirmed by any tests using human fluid or tissue samples, and since the study did not employ fish testing to confirm ciguatera toxins in remnants of fish consumed by patients.
Food and dehydration avoidance
Frequent anecdotal reports to physicians and investigators indicate that after experiencing ciguatera fish poisoning, ingesting alcohol 28 and any kind of fish 42 can cause an augmentation or relapse of symptoms. Ingesting caffeine 30, nuts 30, chicken 43 and pork 43, or experiencing physical over-exertion or dehydration 28 have also been associated with symptom recurrence or augmentation. Therefore, patients are advised to avoid behaviors or activities that cause dehydration, and to avoid such foods for 3–6 months after intoxication or until all ciguatera fish poisoning-related symptoms have resolved. However, controlled investigations of the incidence of symptom recurrence as well as the effectiveness of specific food and activity avoidance measures have not been conducted, and any beneficial impact may vary among individuals.
- Friedman MA, Fleming LE, Fernandez M, et al. Ciguatera fish poisoning: treatment, prevention and management. Mar Drugs. 2008;6(3):456-79. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2579736/[↩]
- Pearn J. Neurology of ciguatera. J Neurol Neurosurg & Psych. 2001;70:4–8[↩]
- Ciguatera. https://www.cdc.gov/nceh/ciguatera/[↩]
- Guidance for Industry: Purchasing Reef Fish Species Associated with the Hazard of Ciguatera Fish Poisoning. https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/ucm375214.htm[↩]
- Friedman MA, Fleming LE, Fernandez M, et al. Ciguatera fish poisoning: treatment, prevention and management. Mar Drugs. 2008;6(3):456-79. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2579736[↩][↩]
- Lewis R. In: Ciguatera (fish poisoning) Williamson JA, editor. University of New South Wales Press; Sydney: 1996.[↩][↩][↩][↩][↩][↩]
- Ting JY. Ciguatera poisoning: a global issue with common management problems. Europ J Emerg Med. 2001;8:295–300[↩][↩][↩][↩]
- Lange WR. Ciguatera toxicity. Am Fam Phys. 1987;35:177–182.[↩]
- Chateau-Degat ML. Prevalence of chronic symptoms of ciguatera disease in French Polynesian adults. Am J Trop Med Hyg. 2007;77:842–846.[↩]
- Ting JY. Ciguatera poisoning: a global issue with common management problems. Europ J Emerg Med. 2001;8:295–300.[↩]
- Lewis R. Ciguatera management. SPC Live Reef Fish Information Bulletin. 2000;7:11–13.[↩][↩][↩]
- Ruff RL. Clinical aspects of ciguatera: an overview. Memoirs of the Queensland Museum. 1994:609–619.[↩]
- Glaziou P. Study of factors that influence the clinical response to ciguatera fish poisoning. Bull Soc Pathol Exotique. 1992;85:419–420.[↩]
- Nicholson GM. Ciguatoxins: cyclic polyether modulators of voltage-gated ion channel function. Mar Drugs. 2006;4:88–118.[↩][↩][↩]
- Ryan JC. Transcriptional profiling of whole blood and serum protein analysis of mice exposed to the neurotoxin Pacific Ciguatoxin-1. NeuroToxicol. 2007;28:1099–1109.[↩]
- Stinn JF. GIS in public health, 3rd National Conference; San Diego, CA. 2000.[↩]
- Dickey R. Monitoring brevetoxins during a Gymnodinium breve red tide: comparison of sodium channel specific cytotoxicity assay and mouse bioassay for determination of neurotoxic shellfish toxins in shellfish extracts. Nat Toxins. 1999;7:157–165.[↩]
- Dickey R. In: Seafood and Freshwater Toxins: Pharmacology, Physiology, and Detection. 2. Botana LM, editor. Taylor and Francis (CRC Press); 2008. pp. 479–500.[↩]
- Darius HT. Ciguatera risk assessment in two toxic sites of French Polynesia using the receptor-binding assay. Toxicon. 2007;50:612–626.[↩]
- Pottier I. Identification of slow and fast-acting toxins in highly ciguatoxic barracuda (Sphyraene barracuda) by HPLC/MS and radiolabelled ligand binding. Toxicon. 2003;42:663–672.[↩]
- Lewis J. In: Manual on harmful marine microalgae. Hallegraeff GM, editor. UNESCO; Paris: 2004. pp. 1–22. IOC Manuals and Guides No. 33.[↩]
- Hokama Y. Simplified solid-phase membrane immunobead assay (MIA) with monoclonal anti-ciguatoxin antibody (MAb-CTX) for detection of ciguatoxin and related polyether toxins. J Nat Tox. 1998;7:1–21[↩]
- Wong CK. Study of an outbreak of ciguatera fish poisoning in Hong Kong. Toxicon. 2005;46:563–571.[↩][↩]
- Hamilton B. Isolation and characterisation of Indian Ocean ciguatoxin. Toxicon. 2002;40:685–693.[↩]
- Baden D. In: Marine toxins. deWolff FA, editor. Vol. 21 Elsevier Press; Amsterdam: 1995.[↩]
- Watters MR. In: Marine neurotoxins as a starting point to drugs. Botana LM, editor. Taylor and Francis (CRC Press); 2007.[↩]
- Berlin RM. Symptomatic improvement of chronic fatigue with fluoxetine in ciguatera fish poisoning. Med J Austr. 1992;157:567.[↩][↩]
- Lange WR. Travel and ciguatera fish poisoning. Arch Int Med. 1992;152:2049–2053.[↩][↩][↩]
- Perez CM. Treatment of ciguatera poisoning with gabapentin. New Engl J Med. 2001;344:692–693[↩]
- Fleming LE. ciguatera fish poisoning. Shoreman’s Travel Medicine Monthly. 1997;1:1–5.[↩][↩][↩]
- Bourdy G. Traditional remedies used in the western Pacific for the treatment of ciguatera poisoning. J Ethnopharmacol. 1992;36:163–74.[↩]
- Benoit E. Reversal of Pacific ciguatoxin-1B effects on myelinated axons by agents used in ciguatera treatment. Cybium. 2000;24:33–40.[↩]
- Schnorf H. Ciguatera fish poisoning: a double-blind randomized trial of mannitol therapy. Neurology. 2002;58:873–880.[↩][↩]
- Blythe DG. In: Foodborne Disease Handbook. Hui YH, editor. Marcel Dekker; New York, NY: 2001. pp. 311–320.[↩]
- Blythe DG. Clinical experience with i.v. Mannitol in the treatment of ciguatera. Bull Soc Pathol Exotique. 1992;85:425–426.[↩][↩]
- Pearn J. Neurology of ciguatera. J Neurol Neurosurg & Psych. 2001;70:4–8.[↩]
- Birinyi-Strachan LC. Neuroprotectant effects of iso-osmolar d-mannitol to prevent Pacific ciguatoxin-1 induced alterations in neuronal excitability: A comparison with other osmotic agents and free radical scavengers. Neuropharmacol. 2005;49:669–686.[↩]
- Palafox NA. Successful treatment of ciguatera fish poisoning with intravenous mannitol. J Am Med Assoc. 1988;259:2740–2742.[↩]
- Pearn JH. Ciguatera and mannitol: experience with a new treatment regimen. Medical Journal of Australia. 1989;151:77–80.[↩]
- Blythe DG. Mannitol Therapy for acute and chronic ciguatera fish poisoning. Memoirs of the Queensland Museum. 1994;34[↩][↩]
- Bagnis R. [Evaluation of the efficacy of mannitol in the treatment of ciguatera in French Polynesia] Med Tropicale. 1992;52:67–73.[↩]
- Gillespie NC. Ciguatera in Australia. Occurrence, clinical features, pathophysiology and management. Med J Austr. 1986;145:584–590.[↩]
- Lewis RJ. The changing face of ciguatera. Toxicon. 2001;39:97–106.[↩][↩]