What is the coccyx
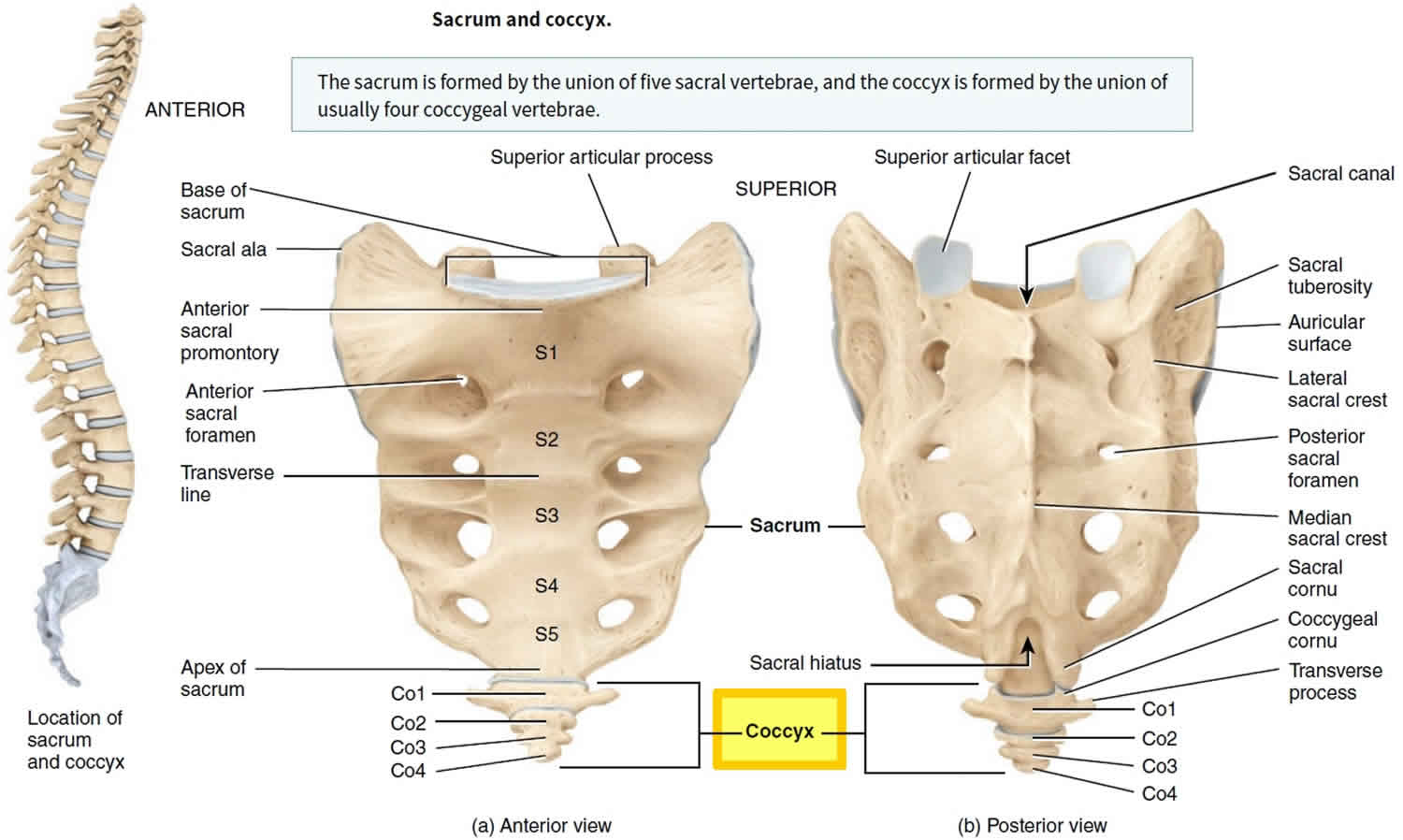
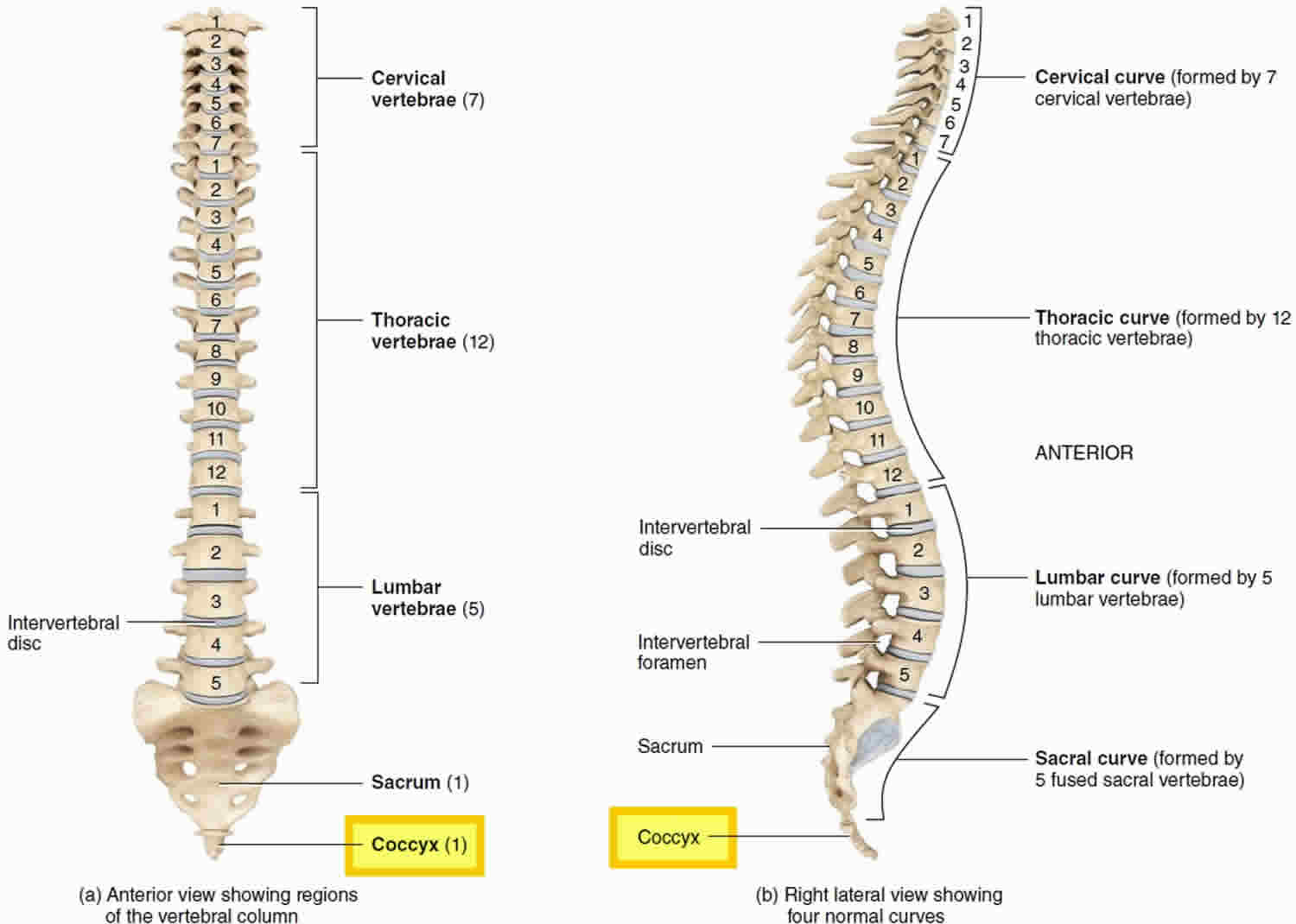
The coccyx also called the tailbone, is a small triangular bone and usually has four but sometimes five tiny vertebrae called the coccygeal vertebrae. Coccyx is a Greek word for “cuckoo”, because the shape resembles the bill of a cuckoo bird 1. The first segment is the largest, and the subsequent are smaller in size. Structure of the coccygeal vertebral junctions is variable and age-related, ranging from fully developed to rudimentary vertebral discs with varying degrees of cystic or fibrotic change, to fusion of the vertebrae in the later decades. Four (sometimes five) tiny coccygeal vertebrae (Co1 to Co4 or Co5) fuse and immovable by the age of 20 to 30 years to form the coccyx. Although the coccyx is the vestige of a tail, it is not entirely useless; the coccyx provides attachment for the muscles of the pelvic floor. The dorsal surface of the body of the first coccyx contains two long coccygeal cornua (horns) that are connected by ligaments to the sacral cornua that bind the coccyx to the sacrum. The coccygeal cornua are the pedicles and superior articular processes of the first coccygeal vertebra. They are on the lateral surfaces of the coccyx, formed by a series of transverse processes; the first pair are the largest. The coccyx articulates superiorly with the apex of the sacrum.
Despite its small size, the coccyx has several important functions. Along with being the insertion site for multiple muscles, ligaments, and tendons, it also serves as one leg of the tripod—along with the ischial tuberosities—that provides weight-bearing support to a person in the seated position. Leaning back while in a seated position leads to increased pressure on the coccyx. The coccyx also provides positional support to the anus.
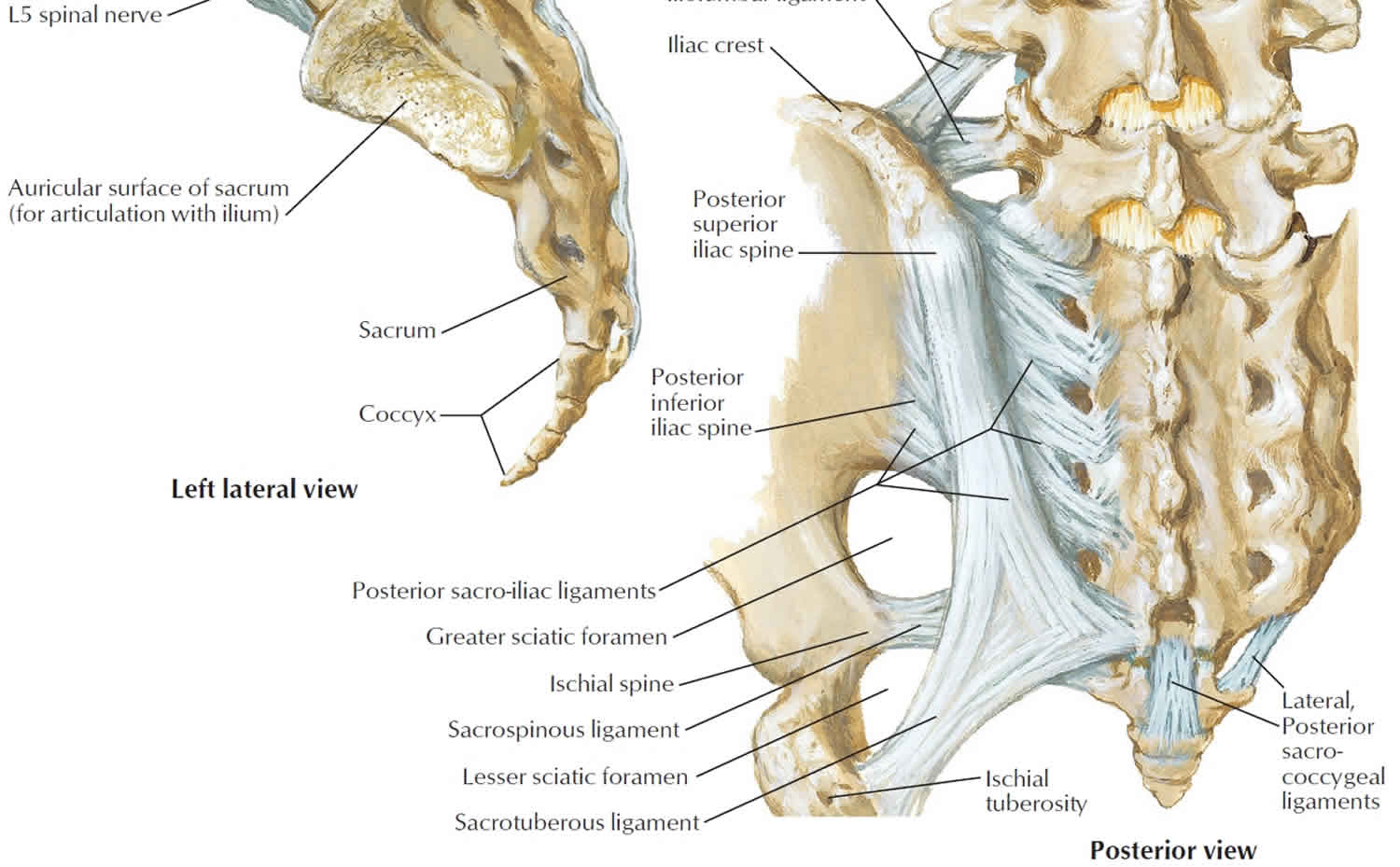
The coccyx is bordered anteriorly by the levator ani muscle and the sacrococcygeal ligament. Moving anteriorly to posteriorly, the lateral edges serve as insertion sites for the coccygeal muscles, the sacrospinous ligament, the sacrotuberous ligament, and fibers of the gluteus maximus muscle. Inferiorly, the iliococcygeus muscle tendon inserts onto the tip of the coccyx. These ligaments and muscles help support the pelvic floor and also contribute voluntary bowel control.
In a study of the gross anatomy of intercoccygeal joints, Maigne, Guedj, and Straus 2 describe the extensive variability in the structure of the joints: from intact discs resembling lumbar intervertebral discs to intermediate disc structures with cystic or fibrotic changes to synovial joints. In some cases, the joints are fused together. Certain types of coccygeal morphology also can lead to a predisposition to coccyx pain 3.
In females, the coccyx points inferiorly to allow the passage of a baby during birth; in males, it points anteriorly. The coccyx can be fractured by a difficult childbirth or a hard fall on the buttocks, which is extremely painful.
Coccyx anatomy
The coccyx consists of an anterior and posterior surface, two lateral surfaces, and apex and a base.
- anterior surface: concave, marked with three transverse grooves representing the fusions of the four separate vertebrae.
- posterior surface:
- convex, similarly marked with three transverse grooves.
- there is a vertical row of tubercles on either side, which are rudimentary articular processes of the coccygeal vertebrae.
- the superior pair are the largest and are called the coccygeal cornua and articulates with the sacral cornua.
- the coccygeal and sacral cornua combine to form the foramen for the transmission of the posterior division of the fifth sacral nerve.
- lateral surface:
- thin with several eminences that represent rudimentary transverse process of the coccygeal vertebra
- the most superior eminences join the lateral edges of the sacrum, forming the foramen for the transmission of the anterior division of the fifth sacral nerve
- it is the largest eminence and the inferior eminences subsequently decrease in size
- anteriorly to posteriorly, the lateral border serves as attachment for the coccygeus, sacrospinous ligament, sacrotuberous ligament, and fibers of the gluteus maximus
- base: proximal oval surface for the articulation with the sacrum
- apex: distal rounded prominence
Articulations
Sacrococcygeal symphysis: fibrocartilagenous joint that connects the apex of sacrum to coccyx. Movement is passive minor flexion and extension and the joint typically fuses with age.
Attachments
Ligamentous
Five ligaments support the sacrococcygeal symphysis.
- anterior sacrococcygeal ligament: continuation of the anterior longitudinal ligament – connects to the anterior aspect of 1st and sometimes 2nd vertebral bodies
- deep posterior sacrococcygeal ligament: connects from the 5th sacral body to the dorsal surface of the coccyx
- superficial posterior sacrococcygeal ligament: begins on the medial sacral crest and inserts on the dorsal surface of the coccyx
- lateral sacrococcygeal ligament: joins the transverse process of the first coccygeal vertebra to the inferolateral angle of the sacrum. This completes the foramen for the fifth sacral nerve anteriorly. Posteriorly the foramen is closed by the sacral and coccygeal cornua connected by the intercornual ligament.
- interarticular (intercornual) ligaments: connect the cornua of the sacrum to the cornua of the coccyx
- anococcygeal raphe: ligament that helps support the position of the anus
Musculotendinous
- gluteus maximus: attaches to the lateral coccyx
- levator ani: attaches to the anterior border and the apex of the coccyx
- sphincter ani externus: attaches to the apex of coccyx
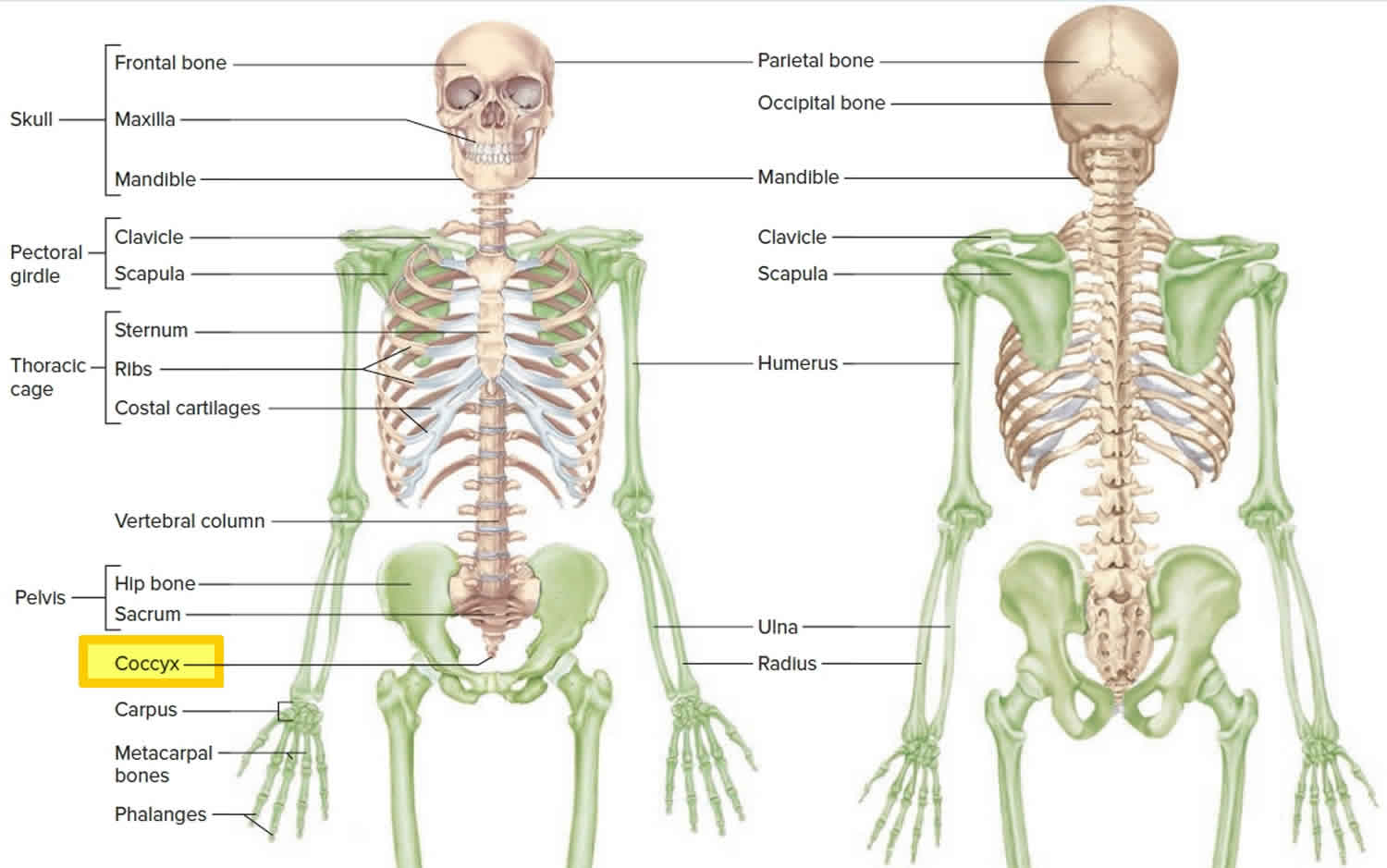
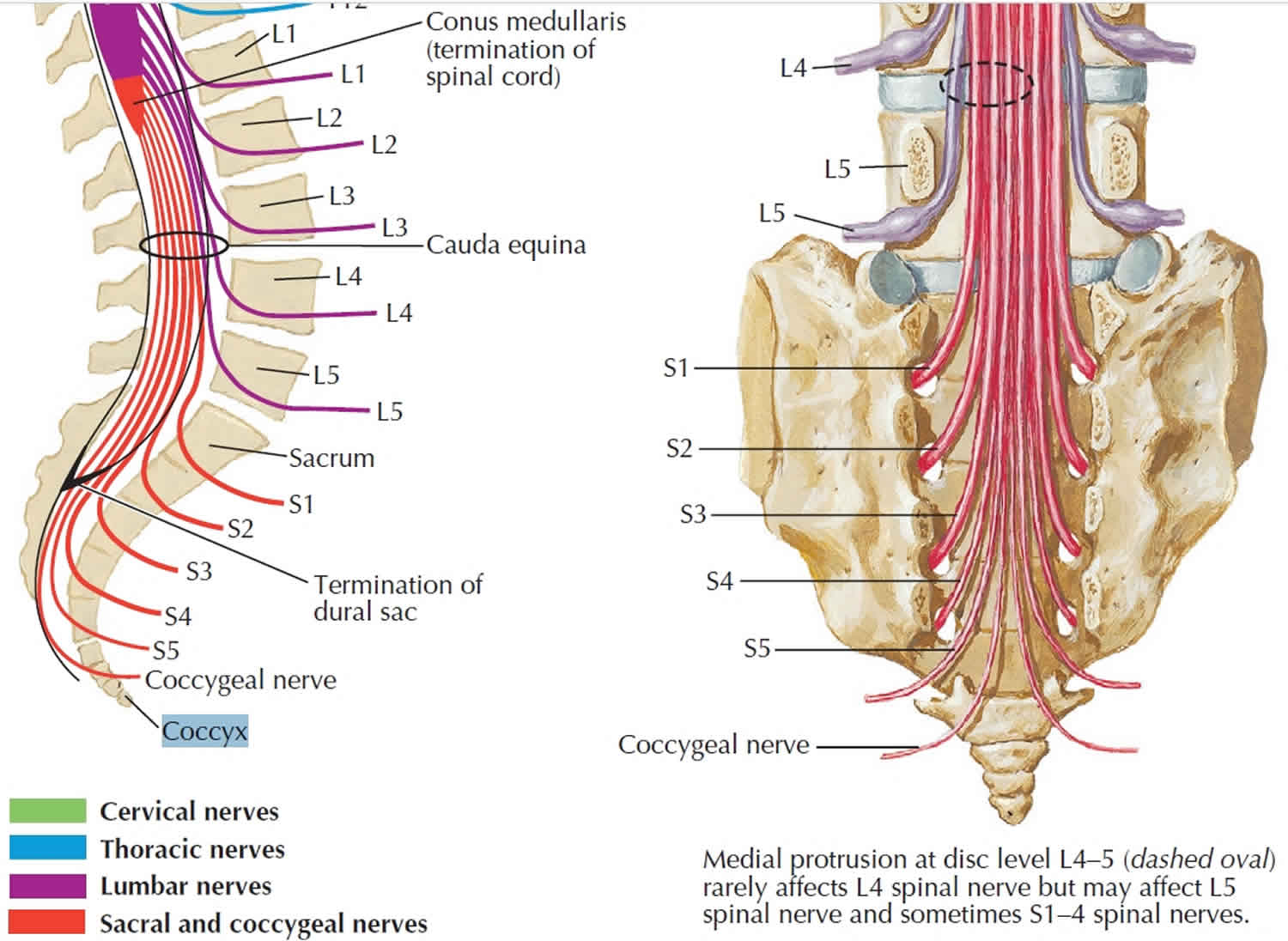
Figure 1. Coccyx bone location
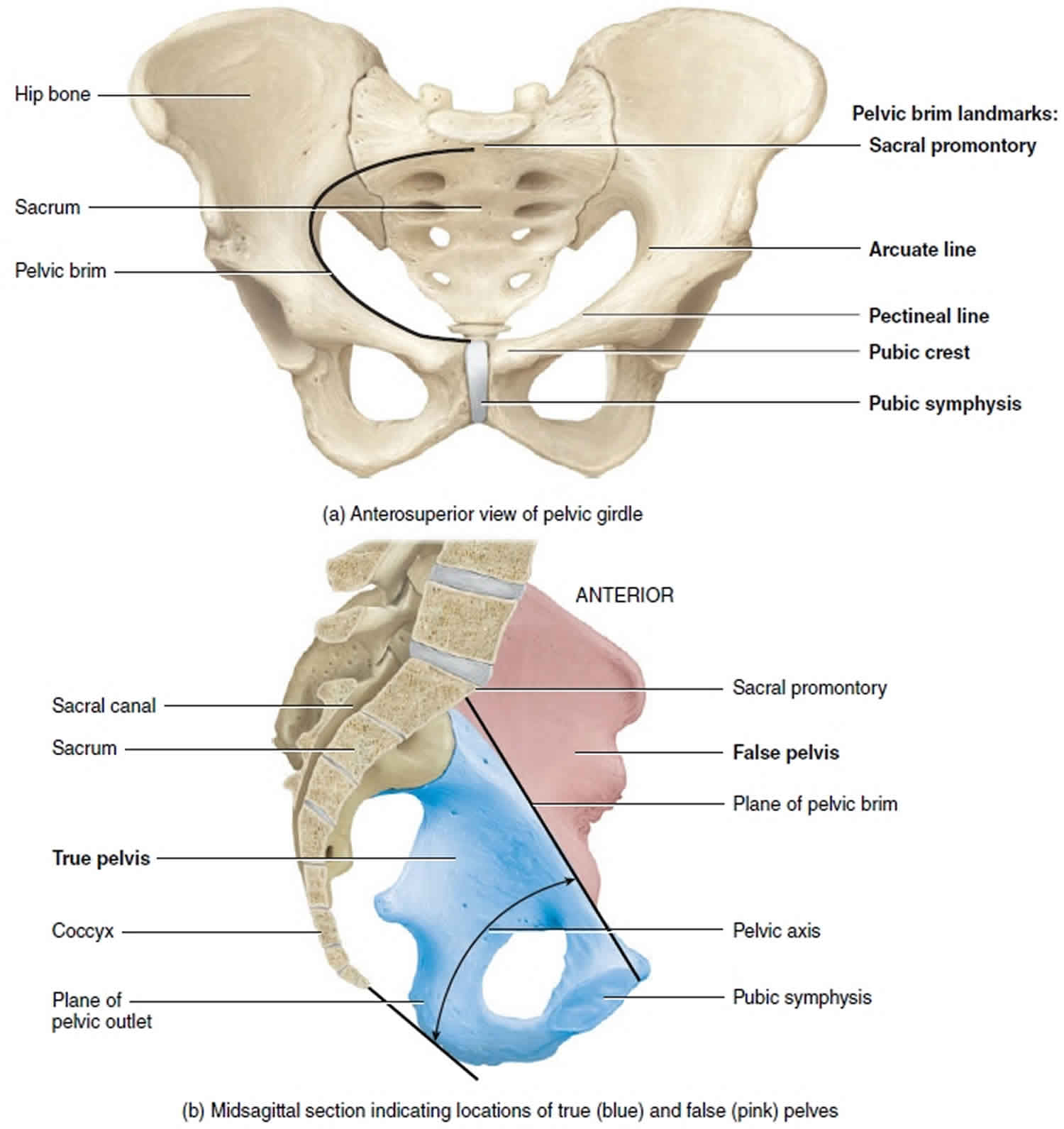
Figure 2. Coccyx bone
Figure 3. Coccyx nerves
Figure 4. Female pelvis anatomy
Tailbone pain
Tailbone pain also called coccydynia (coccyx pain) or coccygodynia 4, is a pain felt in your coccyx or tailbone. You can get it if you injure or strain your coccyx or the surrounding muscles and ligaments. Women are 5 times more likely to develop coccydynia than men 5. Adolescents and adults are more likely to present with coccydynia than children 6. The most common cause of tailbone pain is external or internal trauma. External trauma usually occurs due to a backwards fall, leading to a bruised, dislocated, or broken coccyx 7. The location of the coccyx makes it particularly susceptible to internal injury during childbirth, especially during a difficult or instrumented delivery. Minor trauma can also occur from repetitive or prolonged sitting on hard, narrow, or uncomfortable surfaces 8. Nontraumatic tailbone pain can result from a number of causes, including degenerative joint or disc disease, hypermobility or hypomobility of the sacrococcygeal joint, infectious, and variants of coccygeal morphology. Coccydynia can also be associated with nonorganic causes, such as somatization disorder and other psychological disorders 9. Less commonly, cancer have been associated with tailbone pain.
In most cases, tailbone pain will improve on its own over a few weeks or months, but occasionally it can last much longer and severely affect your ability to carry out every day activities.
Common causes of tailbone pain include:
- vaginal childbirth
- an injury or accident, such as a fall
- repeated or prolonged strain on the coccyx
- poor posture
- prolonged sitting on a hard or narrow surface
- being overweight or underweight
Less common causes can include a bony growth on the coccyx, the coccyx being too flexible or too rigid, and arthritis. Rare but serious causes include infection and cancer.
In many cases, no obvious cause can be found. Age-related “wear and tear” (degenerative joint changes) may play a part.
There are a number of treatments for tailbone pain.
Simple measures you can try at home are usually recommended first and other treatments may be used if these don’t help.
The main treatments are:
- avoiding prolonged sitting,
- lean forward while sitting down,
- using a specially-designed coccyx cushion (donut cushions) or wedge (V-shaped) cushion,
- applying hot or cold packs to your lower back and wearing loose clothing
- take over-the-counter pain relievers, such as acetaminophen (Tylenol, others) or non-steroidal anti-inflammatory (NSAID) painkillers such as ibuprofen (Advil, Motrin IB, others) or aspirin
Figure 4. Coccyx cushion
Persistent symptoms lasting longer than eight weeks may benefit from:
- physiotherapy exercises, massage and stretching
- injections of anti-inflammatories (corticosteroids) and painkillers into the coccyx or surrounding area
In a small number of cases where other treatments haven’t helped, surgery may be needed to manipulate the coccyx. Very rarely the coccyx may need to be removed (coccygectomy).
Tailbone pain (coccydynia) will often improve on its own after a few weeks and there are some simple treatments you can try at home.
If your tailbone pain doesn’t improve (chronic coccydynia), consult your doctor. He or she might do a rectal exam to rule out any other conditions. Your doctor might recommend using magnetic resonance imaging (MRI) to find out if you have a fracture, degenerative changes or, in rare cases, a tumor.
See your doctor if:
- the pain doesn’t start to improve within a few weeks
- simple home treatments don’t relieve the pain
- your pain is very severe
- you also have bleeding, a high temperature (fever) or pain away from your coccyx
Your doctor will carry out an examination to check for more serious causes of your pain, such as infection or a fracture.
Rectal examination allows the coccyx to be grasped between the forefinger and thumb. Manipulation will elicit pain and may reveal hypermobility or hypomobility of the sacrococcygeal joint. Normal range of motion should be approximately 13 degrees 10.
Possible treatments for chronic tailbone pain might include:
- Physical therapy. A physical therapist might show you how to do pelvic floor relaxation techniques, such as breathing deeply and completely relaxing your pelvic floor — as you would while urinating or defecating.
- Manipulation. Massaging the muscles attached to the tailbone might help ease pain. Manipulation is typically done through the rectum.
- Medication. An injection of a local anesthetic into the tailbone can relieve pain for a few weeks. Certain antidepressants or anti-epileptic medications might relieve tailbone pain as well.
- Surgery. During a procedure known as a coccygectomy, the coccyx is surgically removed. This option is typically only recommended when all other treatments fail.
Tailbone pain symptoms
The main symptom of coccyx pain is pain and tenderness in the area just above the buttocks.
The tailbone pain may:
- be dull and achy most of the time, with occasional sharp pains
- be worse when sitting down, moving from sitting to standing, standing for long periods, having sex and going for a poo
- make it very difficult to sleep and carry out everyday activities, such as driving or bending over
- for women, tailbone pain can make menstruation uncomfortable as well
Some people also have back pain, shooting leg pains (sciatica) and painful buttocks and hips.
Tailbone pain causes
You get tailbone pain when your coccyx, or the surrounding tissue, is damaged. This causes pain and discomfort at the base of your spine, particularly when sitting down.
The coccyx can be damaged in various ways, although in many cases it’s not possible to identify a cause.
The main causes of tailbone pain include:
Childbirth
Giving birth is one of the most common causes of tailbone pain.
The coccyx becomes more flexible towards the end of pregnancy. This allows your coccyx, and the part of your spine above it, to bend and give way when you give birth.
Sometimes childbirth can cause the muscles and ligaments (stretchy tissue that connects bones) around your coccyx to overstretch. This can result in tailbone pain.
Injuring your coccyx
You can injure your coccyx if you suffer a hard impact to the base of your spine. For example, from an accidental kick during contact sports.
Falling backwards is another common cause of injury to the coccyx.
In most cases where the coccyx is injured, it will only be badly bruised. But in more severe injuries, it may be dislocated (out of place) or fractured (broken).
Repetitive strain injury (RSI)
You may get tailbone pain if you regularly take part in sports such as cycling or rowing. This is due to continually leaning forward and stretching the base of your spine.
If this motion is repeated many times, the muscles and ligaments around your coccyx can become strained and stretched.
Straining your muscles and ligaments can permanently damage them. If this happens, your muscles will no longer be able to hold your coccyx in the correct position, causing pain and discomfort.
Poor posture
Sitting in an awkward position for a long period of time, such as at work or while driving, can put too much pressure on your coccyx. This causes pain and discomfort that will get worse the longer you stay in this position.
Being overweight or underweight
Being overweight or obese can place excess pressure on your coccyx when you’re sitting down. This can cause tailbone pain or make existing tailbone pain worse.
You may also develop tailbone pain if you are very slim. If this is the case, you may not have enough buttock fat to prevent your coccyx from rubbing against the tissues surrounding it.
Ageing
As you grow older the small discs of cartilage (a tough, flexible tissue) that help hold the coccyx in place can wear down. The bones that make up the coccyx can also become more tightly fused together. This can place more stress on the coccyx, leading to pain.
Infection
Rarely an infection can occur in the base of the spine or soft tissue and cause tailbone pain, such as a pilonidal abscess (a painful collection of pus that usually develops in the cleft of the buttocks).
Cancer
A less common cause of tailbone pain is cancer. This can be bone cancer or cancer that starts somewhere else in the body and then spreads into the bone (metastatic cancer).
Tailbone pain treatment
There are a number of treatments that can help reduce the tailbone pain. Simple measures you can try at home are usually recommended first.
Tailbone pain often improves over a few weeks or months. If it continues despite simple treatments, your doctor may refer you to a specialist to discuss other options.
Self-care measures
The following advice may help reduce pain and allow you to get on with your everyday activities.
- Use a specially-designed coccyx cushion – these can be bought online and from some shops; they help reduce the pressure on your tailbone while you’re sitting down.
- Avoid prolonged sitting whenever possible – try to stand up and walk around regularly; leaning forward while seated may also help.
- Wear loose-fitting clothes – avoid clothing such as tight jeans or trousers that may put pressure on your tailbone.
- Apply warm and cold packs to your tailbone – warm packs include hot water bottles and microwaveable heating pads; cold packs are available as freezable gel-filled pads from pharmacies, or you can use a bag of frozen peas wrapped in a towel.
- Try laxatives (medicines to treat constipation) if the pain is worse when you open your bowels – many laxatives are available to buy from pharmacies and supermarkets without a prescription.
- Take over-the-counter painkillers (see below).
Painkillers
Anti-inflammatory painkillers (NSAIDs)
If your pain and discomfort isn’t too severe, it may be relieved with over-the-counter painkillers.
A type of painkiller known as a non-steroidal anti-inflammatory drug (NSAID) is often recommended. Ibuprofen is a type of NSAID available over-the-counter without a prescription.
NSAIDs can help ease pain and reduce inflammation (swelling) around your coccyx.
However, some people can’t take non-steroidal anti-inflammatory drugs (NSAIDs) because they’re allergic to them or have an increased risk of developing stomach ulcers. If this is the case, try taking paracetamol instead. Ibuprofen gel that you rub into your skin may also be an option.
Ask a pharmacist or doctor for advice if you’re unsure what to take.
Other painkillers
If the pain is more severe, a stronger painkiller such as tramadol may be required. Tramadol can cause side effects, such as constipation, headaches and dizziness.
It’s usually prescribed for a short time as it can be addictive. If it’s prescribed for longer, the dose will have to be reduced gradually before being stopped to avoid withdrawal symptoms.
Physiotherapy
If your pain hasn’t started to improve after a few weeks, your doctor may be able to refer you to a physiotherapist.
A physiotherapist can:
- give you advice about posture and movement to help reduce your pain
- teach you some simple exercises to help relax the muscles around your tailbone
- try techniques such as massage and stretches
Injections
If your coccyx pain doesn’t respond to painkillers, your doctor may recommend injecting medication into your lower back.
Several different types of injections can be tried.
Steroid injections
Injections of corticosteroids into the area around the tailbone can reduce inflammation and pain. Sometimes, they’re combined with local anaesthetic (numbing medication) to make them even more effective.
The injections can help relieve the symptoms of coccyx pain, although the effects may only last for a few weeks.
They can’t cure your condition and too many injections can damage your tailbone and lower back, so you may only be able to have this type of treatment once or twice a year.
Nerve blocks
Injecting local anaesthetic into the nerves that supply the coccyx can help reduce the pain signals coming from them.
As with steroid injections, the effect may only last a few weeks or months.
But unlike steroid injections, it’s usually safe to have repeated injections of local anaesthetic.
Surgery
Surgery for tailbone pain is usually only recommended when all other treatments have failed.
It may involve removing some of your tailbone (partial coccygectomy) or occasionally all of it (total coccygectomy).
A coccygectomy is carried out under general anaesthetic (where you’re asleep).
After surgery, most people find their symptoms improve considerably, although it can take several months. Some people will continue to experience pain.
It takes a long time to recover from coccygectomy, anywhere from a few months to a year.
Tailbone injury
Most tailbone injuries lead to bruising of the bone or pulling of the ligaments and pain. Only in rare cases is there a fracture or broken bone.
Tailbone injuries are often caused by backward falls onto a hard surface, such as a slippery floor or ice.
A tailbone injury can be very painful and slow to heal. Healing time for an injured tailbone depends on the severity of the injury.
- If you have a tailbone fracture, healing can take between 8 to 12 weeks.
- If your tailbone injury is a bruise, healing takes about 4 weeks.
In rare cases, symptoms do not improve. Injection of a steroid medicine may be tried. Surgery to remove part of the tailbone may be discussed at some point, but not until 6 months or more after the tailbone injury.
If you suspect injury to the neck or spine, DO NOT attempt to move the person.
DO NOT
- DO NOT attempt to move the person if you think there may be injury to the spinal cord.
Get immediate medical help if:
- Spinal cord injury is suspected
- The person can’t move
- Pain is severe
- Sudden numbness, tingling or weakness in one or both legs
- Sudden increase in pain or swelling
- Injury does not seem to be healing as expected
- Prolonged constipation
- Problems controlling your bowel or bladder
Tailbone injury causes
Backward falls onto a hard surface, such as a slippery floor or ice, are the most common cause of this injury.
Tailbone injury prevention
Keys to preventing tailbone injury include:
- DO NOT run on slippery surfaces, such as around a swimming pool.
- Dress in shoes with good tread or slip-resistant soles, especially in snow or on ice.
Tailbone injury symptoms
Symptoms include:
- Bruising and swelling around the base of the spine
- Pain when sitting or putting pressure on the tailbone or the buttocks area
- Pain or tenderness in the lower back
- Pain or numbness with sitting
Tailbone injury treatment
For tailbone injury when no spinal cord injury is suspected:
- Ice your tailbone for about 20 minutes every hour while awake for the first 48 hours, then 2 to 3 times a day. DO NOT apply ice directly to the skin.
- Use an inflatable rubber ring or cushions or gel donut when sitting. The hole in the center will take pressure off your tailbone. You can buy the cushion at a drugstore.
- Avoid sitting a lot. When sleeping, lie on your belly to take pressure off the tailbone.
- Take acetaminophen for pain.
- Take a stool softener to avoid constipation.
For pain, you can use ibuprofen (Advil, Motrin, and others) or naproxen (Aleve, Naprosyn, and others). You can buy these medicines without a prescription.
- DO NOT use these medicines for the first 24 hours after your injury. They may increase the risk of bleeding.
- Talk with your health care provider before using these drugs if you have heart disease, high blood pressure, kidney disease, liver disease, or have had stomach ulcers or internal bleeding in the past.
- DO NOT take more than the amount recommended on the bottle or more than your provider advises you to take.
It may be painful to go to the bathroom. Eat plenty of fiber and drink plenty of fluids to avoid constipation. Use stool softener medicine if needed. You can buy stool softeners at the drugstore.
Activity
As your pain goes away, you can begin light physical activity. Slowly increase your activities, such as walking and sitting. You should:
- Continue to avoid sitting for long periods.
- Not sit on a hard surface.
- Keep using the cushion or gel donut when sitting.
- When sitting, alternate between each of your buttocks.
- Ice after activity if there is any discomfort.
Follow-up
Your doctor may not need to follow up if the injury is healing as expected. If the injury is more severe, you will likely need to see the doctor.
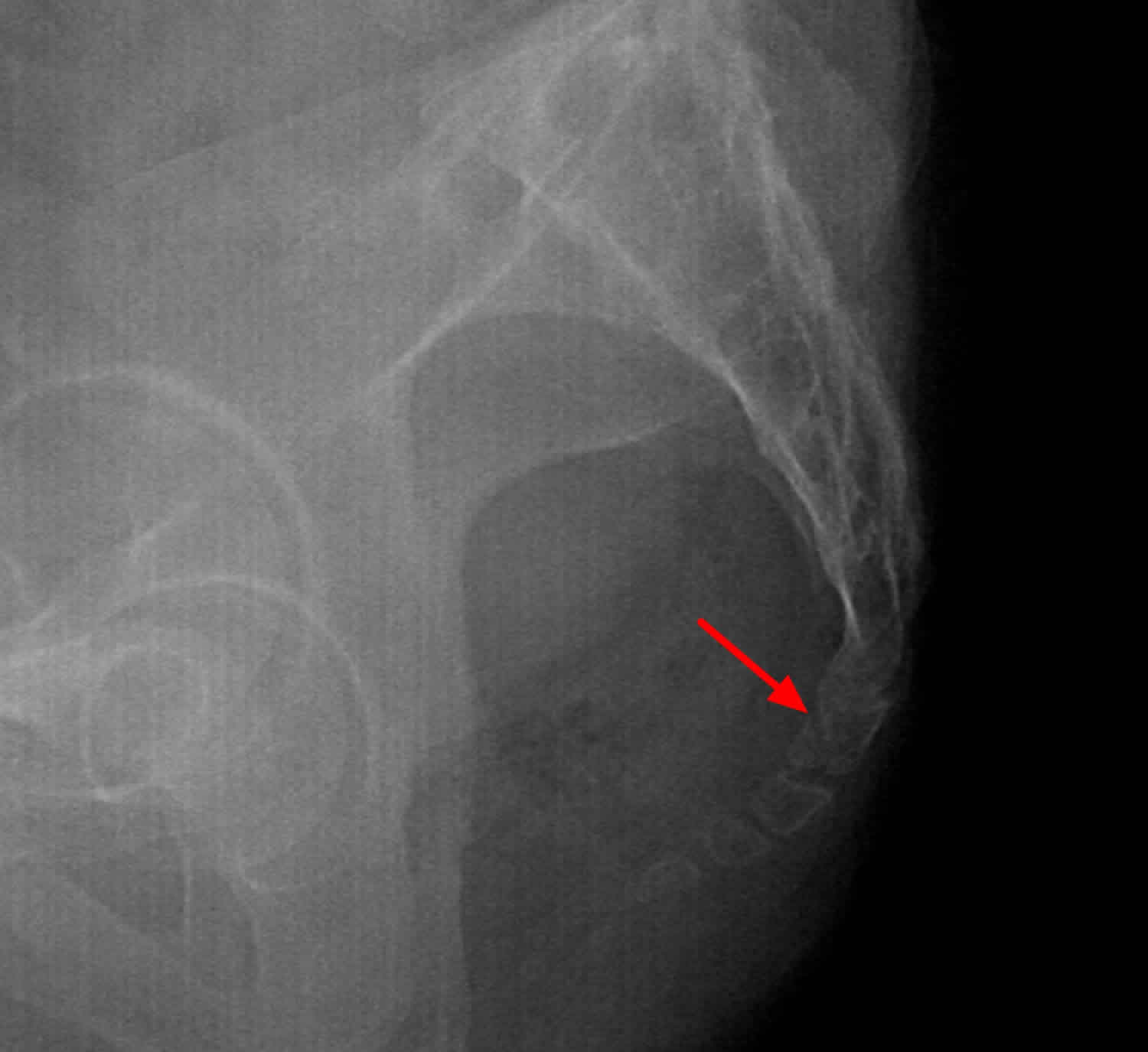
Coccyx fracture
Coccyx fractures are rarely diagnosed on pelvic x-rays and, when diagnosed, the treatment is usually conservative 11. Thus, the need of x-ray examination in suspected coccygeal fractures is questioned as it imparts additional radiation exposure to genitalia. Treatment for coccyx fractures is similar to tailbone pain (see above).
Patients who did not respond to conservative treatment after at least six months follow-up were offered coccygectomy. Overall, success rates have been reported in the relevant literature ~ 84% of patients who underwent coccygectomy benefited from surgery 12. One of the common complications of coccygectomy is wound infection. Doursounian et al. 13 showed an infection rate of 14.75%, with the most common organism being Staphylococcus aureus. Postacchini et al. 14 showed that partial skin necrosis and superficial wound infection were causes of delayed wound healing in more than 50% of patients.
Different investigators reported different experiences with postoperative infection and, therefore, suggested various strategies for antibiotic prophylaxis before surgery 15. Bayne et al. 16 reported an infection rate of 16.6%. They did not use any prophylactic antibiotics and recommended that from their experience they should be used. Cebesoy et al. 17 showed no infection with preoperative antibiotic prophylaxis which was continued for five days postoperatively. Pennekamp et al. 18 observed 19% postoperative complications (two superficial and one deep infection), which were all treated with surgical débridement and antibiotics. They recommended a perioperative prophylaxis with antibiotics, given either as a single shot or two to three days after surgery. None of these authors discussed the surgical technique nor did they give details about periosteal resection. Increased cost, side or adverse effects of antibiotic therapy and development of resistance of bacteria are among the factors why surgeons limit the use of prophylactic antibiotics.
In coccygectomy, the existing incision area is regarded as clean-contaminated tissue. Perineal contamination of the wound due to the difficulties of the patient visualising and caring for the wound and wound dehiscence due to the tension on the incision during sitting are proposed as the major reasons for wound complications 19. Furthermore, resection of the coccyx forms a surgical dead space that usually cannot be closed thoroughly. However, coccygectomy with subperiosteal dissection and preservation of the periosteum provides a means to close the surgical dead space. Moreover, during subperiosteal dissection coccygeal attachments with coccygeus and iliococcygeus muscles, and the anococcygeal ligament, are not released which may inhibit haematoma and/or seroma formation.
Figure 5. Coccyx fracture
- Coccyx. The bone named for a bird. Sugar O. Spine (Phila Pa 1976). 1995 Feb 1; 20(3):379-83.[↩]
- Idiopathic coccygodynia. Lateral roentgenograms in the sitting position and coccygeal discography. Maigne JY, Guedj S, Straus C. Spine (Phila Pa 1976). 1994 Apr 15; 19(8):930-4.[↩]
- Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. Postacchini F, Massobrio M. J Bone Joint Surg Am. 1983 Oct; 65(8):1116-24.[↩]
- Simpson J. Clinical lectures on the diseases of women. Lecture XVII: coccydynia and diseases and deformities of the coccyx. Medical Times Gazette. 1859;40:1–7.[↩]
- Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014;14(1):84-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963058/[↩]
- Maigne JY, Pigeau I, Aguer N, Doursounian L, Chatellier G. Chronic coccydynia in adolescents. A series of 53 patients. Eur J Phys Rehabil Med. 2011 Jun;47(2):245–251.[↩]
- Schapiro S. Low back and rectal pain from an orthopedic and proctologic viewpoint; with a review of 180 cases. Am J Surg. 1950 Jan;79(1):117–128.[↩]
- Pennekamp PH, Kraft CN, Stütz A, Wallny T, Schmitt O, Diedrich O. Coccygectomy for coccygodynia: does pathogenesis matter? J Trauma. 2005 Dec;59(6):1414–1419.[↩]
- Nathan ST, Fisher BE, Roberts CS. Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. J Bone Joint Surg Br. 2010 Dec;92(12):1622–1627.[↩]
- Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Maigne JY, Doursounian L, Chatellier G. Spine (Phila Pa 1976). 2000 Dec 1; 25(23):3072-9.[↩]
- Lirette LS, Chaiban G, Tolba R et-al. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014;14 (1): 84-7[↩]
- Bilgic S, Kurklu M, Yurttaş Y, Ozkan H, Oguz E, Sehirlioglu A. Coccygectomy with or without periosteal resection. Int Orthop. 2009;34(4):537-41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2903156/[↩]
- Doursounian L, Maigne JY, Faure F, et al. Coccygectomy for instability of the coccyx. Int Orthop. 2004;28:176–179. doi: 10.1007/s00264-004-0544-3[↩]
- Postacchini F, Massobrio M. Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. J Bone Joint Surg Am. 1983;65:1116–1124.[↩]
- Balain B, Eisenstein SM, Alo GO, et al. Coccygectomy for coccydynia: case series and review of literature. Spine. 2006;31(13):E414–E420. doi: 10.1097/01.brs.0000219867.07683.7a[↩]
- Bayne O, Bateman JE, Cameron HU. The influence of etiology on the results of coccygectomy. Clin Orthop. 1984;190:266–272[↩]
- Cebesoy O, Guclu B, Kose KC, Basarir K, Guner D, Us AK. Coccygectomy for coccygodynia: do we really have to wait? Injury. Injury. 2007;38:1183–1188. doi: 10.1016/j.injury.2007.01.022[↩]
- Pennekamp PH, Kraft CN, Stütz A, et al. Coccygectomy for coccygodynia: does pathogenesis matter? J Trauma. 2005;59(6):1414–1419. doi: 10.1097/01.ta.0000195878.50928.3c[↩]
- Wood KB, Mehbod AA. Operative treatment for coccygodynia. J Spinal Disord Tech. 2004;17(6):511–515. doi: 10.1097/01.bsd.0000128691.36652.16.[↩]