Contents
What is cor pulmonale
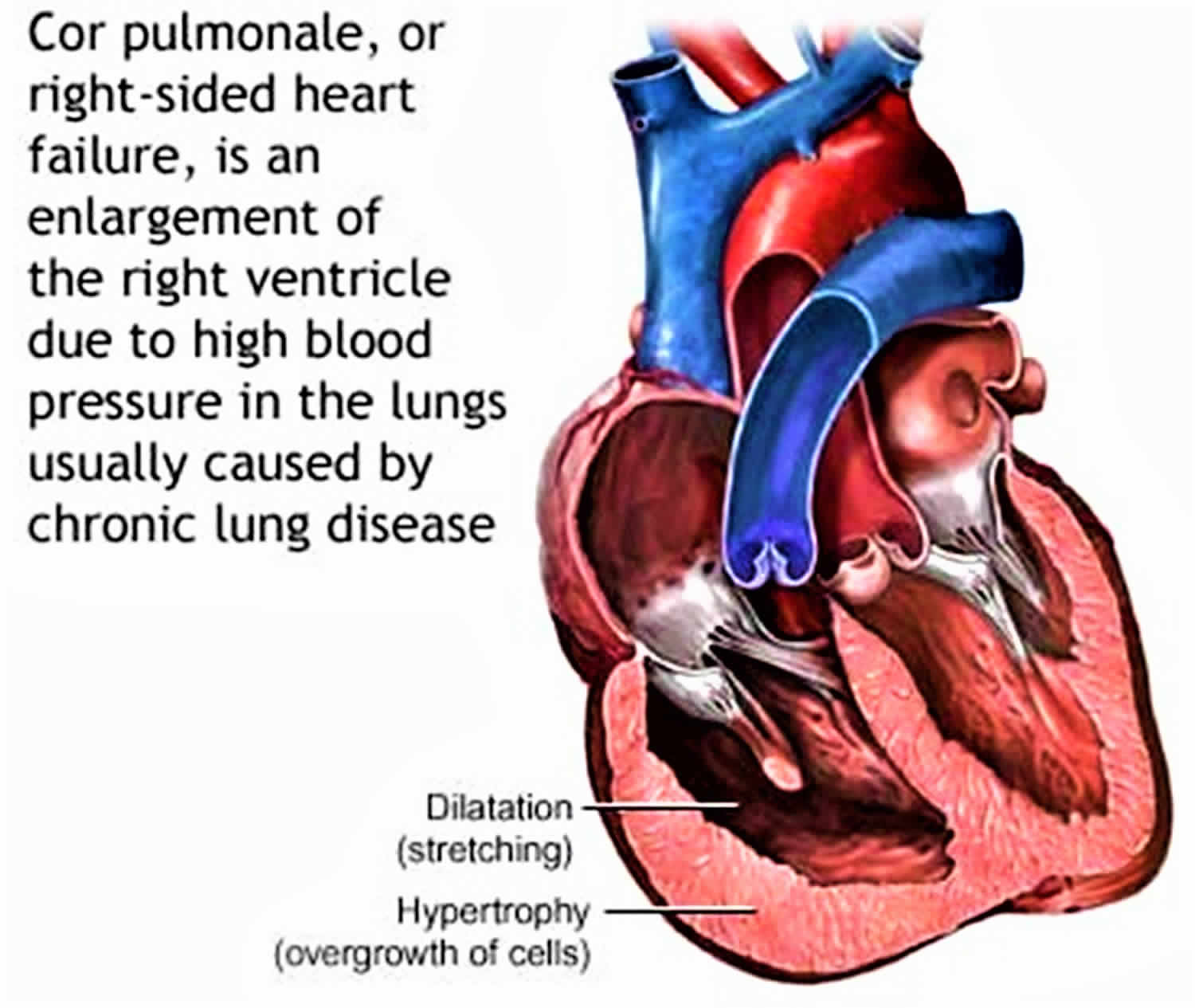
Cor pulmonale is a Latin word that means “pulmonary heart”, its definition varies, and presently, there is no consensual definition 1, 2. Cor pulmonale is a condition that causes the right side of the heart to fail from long-standing pulmonary artery high blood pressure (hypertension). Long-term high blood pressure in the arteries of the lung and right ventricle of the heart can lead to cor pulmonale. Cor pulmonale can be defined as an alteration in the structure (e.g., hypertrophy or dilatation) and function of the right ventricle (RV) of the heart caused by a primary disorder of the lungs (respiratory system) resulting in pulmonary hypertension 3.
The exact prevalence of cor pulmonale is difficult to determine, as physical examination and routine tests are relatively insensitive for the detection of pulmonary hypertension and right ventricle (RV) dysfunction. Cor pulmonale is estimated to account for 6% to 7% percent of all types of adult heart disease in the United States 1. Globally, the incidence of cor pulmonale varies widely among countries, depending on the prevalence of cigarette smoking, air pollution, and other risk factors for various lung diseases.
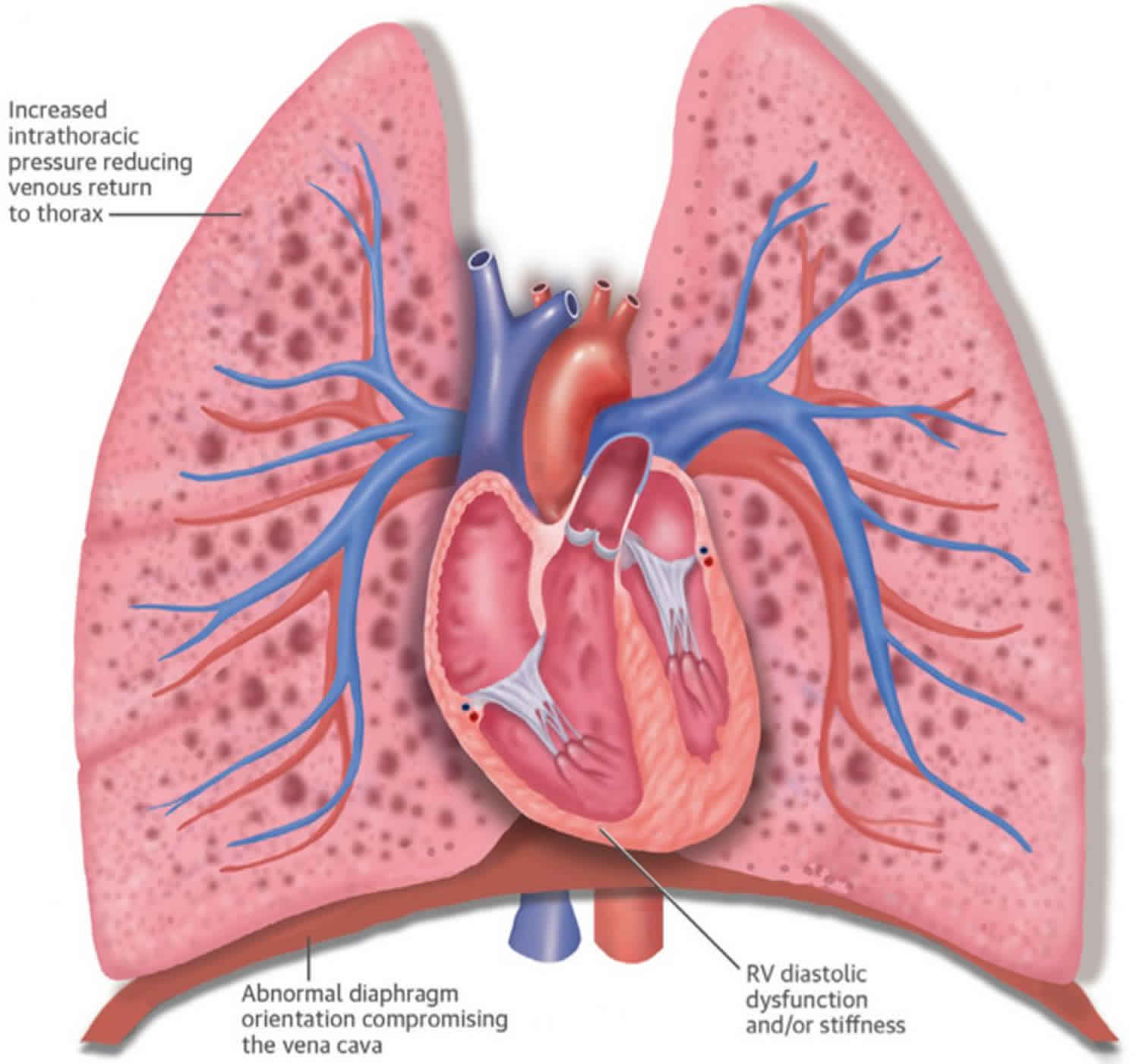
Unlike chronic cor pulmonale associated with long term high blood pressure in the arteries of the lung, acute cor pulmonale is a severe form of right ventricle failure caused by increased pulmonary vascular resistance or high pulmonary arterial pressure, signifying a poor prognosis for patients with acute respiratory distress syndrome (ARDS) 4. Acute respiratory distress syndrome (ARDS) is characterized by deleterious hypoxemia. Although high positive airway pressure is required to provide adequate gas exchange in patients with severe acute respiratory distress syndrome (ARDS) 5, it stresses pulmonary capillaries and increases pulmonary vascular resistance. It therefore creates right ventricular (RV) after load and can cause right ventricle failure 6. Reported incidence of acute cor pulmonale in patients with acute respiratory distress syndrome (ARDS) varies from 10% to 84%, despite being subjected to lung protective ventilation according to the current guidelines 7. Mechanical ventilation which is central to the management of ARDS also interferes with cardiac function by decreasing right ventricular (RV) preload and increasing after load 8. The deleterious effect of ARDS and mechanical ventilation on the right ventricle has been known for many years. ARDSNet protocol, which is in use for nearly one and half a decade, is primarily a lung protective ventilation strategy. Although lung protective ventilation improved mortality 9, it still affects right ventricle adversely. These effects range from pulmonary artery hypertension to development of acute cor pulmonale 10. Findings of this review 7 indicate the need of updating existing guidelines for ventilating ARDS patients to incorporate right ventricle protective strategy. This approach should include a stepwise ventilation strategy, keeping the pulmonary circulation and the right ventricle at the center of the decision-making process. It is based on the premise that “what is good for the right ventricle is also good for the lung and vice versa” 11. This strategy may consist of limiting plateau pressure below 27 cm H2O, driving pressure below 17 cm H2O and PCO2 below 60 mmHg 12. This strategy may also incorporate the early use of prone position ventilation or possibly extracorporeal membrane oxygenator if conventional ventilation does not meet the above criteria 13. Current studies do not show evidence in support of high-frequency oscillation ventilation 14.
Right-sided heart failure secondary to left-sided heart failure, or congenital heart disease is not considered cor pulmonale 1.
Cor pulmonale causes
High blood pressure in the arteries of the lungs is called pulmonary hypertension. It is the most common cause of cor pulmonale. Most cases of pulmonary hypertension are secondary to lung disease. Almost any chronic lung disease can cause cor pulmonale.
Pulmonary hypertension is associated with diseases of the lung (e.g., chronic obstructive pulmonary disease [COPD], interstitial lung disease), vasculature (e.g., idiopathic pulmonary arterial hypertension), upper airway (e.g., obstructive sleep apnea), or chest wall (e.g., kyphoscoliosis). Diseases that damage lungs are autoimmune (e.g., scleroderma), cystic fibrosis, and obesity hypoventilation syndrome are also lead to pulmonary hypertension.
In people who have pulmonary hypertension, changes in the small blood vessels inside the lungs can lead to increased blood pressure in the right side of the heart. This makes it harder for the heart to pump blood to the lungs. If this high pressure continues, it puts a strain on the right side of the heart. That strain can cause cor pulmonale.
Lung conditions that cause a low blood oxygen level in the blood over a long time can also lead to cor pulmonale. Some of these are:
- Autoimmune diseases that damage the lungs, such as scleroderma
- Chronic blood clots in the lungs
- Cystic fibrosis (CF)
- Scarring of the lung tissue (interstitial lung disease)
- Severe curving of the upper part of the spine (kyphoscoliosis)
- Obstructive sleep apnea, which causes stops in breathing because of airway inflammation
- Idiopathic (no specific cause) tightening (constriction) of the blood vessels of the lungs
- Pulmonary hypertension associated with disorders of the respiratory system and/or hypoxaemia
- Alveolar hypoventilation disorders
- Chronic exposure to high altitude
- Neonatal lung disease
- Alveolar capillary dysplasia
- Other
However in clinical practice, by far and away the predominant causes of cor pulmonale are:
- Chronic obstructive pulmonary disease (COPD) (e.g., emphysema, chronic bronchitis) in the chronic setting. Chronic obstructive pulmonary disease (COPD) is the most common cause of cor pulmonale. In most patients with COPD, cor pulmonale tends to be accompanied by mild pulmonary hypertension (i.e., mean pulmonary artery pressure 40 mmHg or less). The severity of cor pulmonale appears to correlate with the magnitude of hypoxemia, hypercapnia, and airflow obstruction.
- Pulmonary embolism in the acute setting. Massive pulmonary embolism is the most common cause of acute cor pulmonale. A massive pulmonary embolism can mimic a myocardial infarction with elevated troponins, ST changes, chest pain, and shortness of breath.
In cases of pulmonary embolism, one or many embolic clots (usually from the deep veins of the leg) occlude a part of the pulmonary arterial vasculature. In time, this results in increased pulmonary pressure, decreased cardiac output and a syndrome of right heart failure, usually with no cardiac compensation.
In the chronic setting (as in COPD) the pulmonary hypertension is due to changes to the lung tissues themselves. This is often associated with compensatory right heart changes, and eventually right heart failure.
Primary pulmonary hypertension, as the name suggests, has no known cause. Primary pulmonary hypertension is a rare disease. It is found in 0.1-0.2% of all patients at autopsy, but many are asymptomatic (showing no symptoms) until late in the process.
Table 1 lists the chronic respiratory diseases which may lead to cor pulmonale.
Table 1. Diseases of the respiratory system associated with pulmonary hypertension (except primary pulmonary hypertension, pulmonary thromboembolic disease, and diseases of the pulmonary vascular bed)
Obstructive lung diseases
- COPD* (chronic obstructive bronchitis, emphysema and their association)
- Asthma (with irreversible airway obstruction)
- Cystic fibrosis†
- Bronchiectasis
- Bronchiolitis obliterans
Restrictive lung diseases
- Neuromuscular diseases: amyotrophic lateral sclerosis, myopathy, bilateral diaphragmatic paralysis, etc
- Kyphoscoliosis†
- Thoracoplasty
- Sequelae of pulmonary tuberculosis
- Sarcoidosis
- Pneumoconiosis†
- Drug related lung diseases
- Extrinsic allergic alveolitis
- Connective tissue diseases
- Idiopathic interstitial pulmonary fibrosis†
- Interstitial pulmonary fibrosis of known origin
Respiratory insufficiency of “central” origin
- Central alveolar hypoventilation
- Obesity–hypoventilation syndrome† (formerly “Pickwickian syndrome”)
- Sleep apnoea syndrome†
Footnote:
*Very frequent cause of pulmonary hypertension.
†Relatively frequent cause of pulmonary hypertension.
Cor pulmonale pathophysiology
The pathophysiology of cor pulmonale is a result of increased right-sided filling pressures from pulmonary hypertension that is associated with diseases of the lung.
Under normal physiologic conditions, the right ventricle pumps against a low-resistance circuit.
Normal pulmonary vascular resistance is approximately one-tenth the resistance of the systemic arteries. Chronic hypoxemia leading to chronic vasoconstriction produces smooth muscle proliferation in small pulmonary arteries. Hypoxemia produces changes in vascular mediators such as Nitric Oxide, Endothelin1 (ET1) and platelet-derived growth factors (PDGf A and B). Nitric oxide is a vasodilator; hypoxemia reduces endothelial cell production of nitric oxide and results in impaired smooth ms relaxation.
The initial pathophysiologic event in the production of cor pulmonale is an elevation of the pulmonary vascular resistance. As the resistance increases, the pulmonary arterial pressure rises, and the right ventricular work increases leading to right ventricular enlargement (e.g., thickening, dilation, or both).
Cor pulmonale prevention
Do not smoke. Smoking causes lung disease, which can lead to cor pulmonale.
Cor pulmonale symptoms
Shortness of breath (dyspnea) on exertion or lightheadedness during activity is often the first symptom of cor pulmonale. You may also have a fast heartbeat and feel like your heart is pounding.
Over time, symptoms occur with lighter activity or even while you are at rest. Symptoms you may have are:
- Fainting spells during activity
- Chest discomfort, usually in the front of the chest
- Exertional chest pain
- Exertional syncope
- Swelling (edema) of the feet or ankles
- Symptoms of lung disorders, such as wheezing or coughing or phlegm production
- Bluish lips and fingers (cyanosis)
- Fatigue
- Lethargy
The clinical signs occur late, being observed at an advanced stage of the disease far after the development of pulmonary hypertension.
Signs of cor pulmonale may include:
- Jugular venous distension: Prominent jugular V wave, indicating the presence of tricuspid regurgitation
- Peripheral (ankle) edema: The best sign of RHF, but it is not specific and can arise from other causes
- Cardiovascular: Palpable left the parasternal lift, loud S2 (accentuation of the pulmonary component of the second heart sound) narrow splitting of S2, a holosystolic murmur of tricuspid regurgitation at the left lower sternal border, right-sided S4 heart sound
- Abdomen: Hepatomegaly and ascites (abdominal edema or distension).
Cor pulmonale possible complications
Cor pulmonale may lead to:
- Life-threatening shortness of breath
- Severe fluid buildup in your body
- Shock
- Death
Cor pulmonale diagnosis
Your health care provider will perform a physical exam and ask about your symptoms. The exam may find:
- Fluid buildup in your belly (ascites)
- Abnormal heart sounds
- Bluish skin
- Liver swelling (hepatomegaly)
- Swelling of the neck veins, which is a sign of high pressure in the right side of the heart
- Ankle swelling
These tests may help diagnose cor pulmonale as well as its cause:
- Chest x-ray: Enlargement of pulmonary artery may be seen, cardiomegaly is confined predominantly, if not exclusively, to the right ventricle and other features may be detected according to the cause
- CT scan of the chest, with or without an injection of a contrast fluid (dye): Chest CT angiography to rule out pulmonary thromboembolism as a cause. Main pulmonary artery diameter measurements greater than 29 mm have a sensitivity of 84% and specificity of 75% for the diagnosis of pulmonary hypertension.
- Echocardiogram: The non-invasive diagnosis of pulmonary hypertension is presently based on echocardiography. Continuous-wave Doppler echocardiography allows the calculation of the transtricuspid pressure gradient from the peak velocity of the tricuspid regurgitant jet
- ECG: Shows features of right ventricular hypertrophy/enlargement.
- Ventilation and perfusion scan of the lungs (V/Q scan): Ventilation/perfusion (V/Q) scanning can be particularly useful in evaluating patients with cor pulmonale, especially if pulmonary hypertension is due to chronic thromboembolic pulmonary hypertension.
- Pulmonary (lung) function tests: Pulmonary (lung) function tests and 6-minute walk test for assessment of severity of lung disease and exercise capacity respectively.
- Right heart catheterization: A right heart cath is a gold standard for diagnosis, assessment of Pulmonary hypertension severity. Right heart catheterization reveals evidence of right ventricular (RV) dysfunction (mean pulmonary artery pressure (PAP) above 25 mmHg) without left ventricular (LV) dysfunction. Differentiating left-sided from the right-sided disease includes measuring the pulmonary capillary wedge pressure (PCWP), which is an estimation of left atrial pressure. Thus, right ventricular (RV) dysfunction is also defined as having a pulmonary capillary wedge pressure below 15 mmHg.
- Measurement of blood oxygen by checking arterial blood gas (ABG)
- Tests for autoimmune lung disease
- Blood antibody tests
- Blood test to check for a substance called brain natriuretic peptide (BNP)
- Lung biopsy (rarely done)
Cor pulmonale treatment
The goal of treatment is to control symptoms — the aim is improving oxygenation and right ventricular (RV) function by increasing right ventricular contractility and decreasing pulmonary vasoconstriction. It is important to treat medical problems that cause pulmonary hypertension, because they can lead to cor pulmonale.
Many treatment options are available. In general, the cause of your cor pulmonale will determine which treatment you receive.
If your provider prescribes medicines, you may take them by mouth (oral), receive them through a vein (intravenous or IV), or breathe them in (inhaled). You will be closely monitored during treatment to watch for side effects and to see how well the medicine works for you. Never stop taking your medicines without first talking to your doctor.
Other treatments may include:
- Blood thinners to reduce the risk of blood clots
- Medicines to manage heart failure symptoms.
- Diuretics are used to decrease the elevated right ventricular (RV) filling volume in patients with chronic cor pulmonale.
- Vasodilators such as the calcium channel blockers may be particularly useful in reducing the pressure of the pulmonary circulation.
- The use of cardiac glycosides, such as digitalis in patients with cor pulmonale has been controversial, and the beneficial effect of these drugs is not as obvious as in the setting of left heart failure. Nevertheless, studies have confirmed a modest effect of digitalis on the failing right ventricle in patients with chronic cor pulmonale.
- Oxygen therapy at home. Oxygen therapy relieves hypoxemic pulmonary vasoconstriction, which then improves cardiac output, lessens sympathetic vasoconstriction, alleviates tissue hypoxemia, and improves renal perfusion.
- A lung or heart-lung transplant, if medicine does not work
Important tips to follow:
- Avoid strenuous activities and heavy lifting.
- Avoid traveling to high altitudes.
- Get a yearly flu vaccine, as well as other vaccines, such as the pneumonia vaccine.
- If you smoke, stop.
- Use oxygen if your doctor prescribes it.
- Women should not get pregnant.
Cor pulmonale prognosis
How well you do depends on the cause of your cor pulmonale. However, disease serious enough to cause significant right heart failure (usually massive pulmonary embolism or end stage COPD) are associated with poor prognoses.
Mild to moderate pulmonary emboli have the best outlook. Primary pulmonary hypertension has a poor prognosis with a porgressive course – heart and lung transplantation is an option in younger patients.
Development of cor pulmonale as a result of a primary pulmonary disease usually heralds a poorer prognosis.
As your illness gets worse, you will need to make changes to your home so that you can manage as well as possible. You will also need help around your house.
- Garrison DM, Memon J. Cor Pulmonale. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430739[↩][↩][↩]
- Weitzenblum E. Chronic cor pulmonale. Heart. 2003;89(2):225-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767533/[↩]
- Anon. Chronic cor pulmonale. Report of an expert committee. Circulation 1963;27:594–15.[↩]
- Repesse X, Charron C, Vieillard-Baron A. Acute cor pulmonale in ARDS: rationale for protecting the right ventricle. Chest. 2015;147(1):259–265. doi: 10.1378/chest.14-0877.[↩]
- Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Thompson BT, Ranieri VM. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38(10):1573–1582. doi: 10.1007/s00134-012-2682-1.[↩]
- Kotani T, Tanabe H, Yusa H, Saito S, Yamazaki K, Ozaki M. Electrical impedance tomography-guided prone positioning in a patient with acute cor pulmonale associated with severe acute respiratory distress syndrome. J Anesth. 2015;30(1):161-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4744250/[↩]
- Das SK, Choupoo NS, Saikia P, Lahkar A. Incidence Proportion of Acute Cor Pulmonale in Patients with Acute Respiratory Distress Syndrome Subjected to Lung Protective Ventilation: A Systematic Review and Meta-analysis. Indian J Crit Care Med. 2017;21(6):364-375. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5492739/[↩][↩]
- Acute cor pulmonale in ARDS: rationale for protecting the right ventricle. Repessé X, Charron C, Vieillard-Baron A. Chest. 2015 Jan; 147(1):259-265.[↩]
- Lung protective ventilation strategy for the acute respiratory distress syndrome. Petrucci N, De Feo C. Cochrane Database Syst Rev. 2013 Feb 28; (2):CD003844.[↩]
- Prevalence and prognosis of cor pulmonale during protective ventilation for acute respiratory distress syndrome. Boissier F, Katsahian S, Razazi K, Thille AW, Roche-Campo F, Leon R, Vivier E, Brochard L, Vieillard-Baron A, Brun-Buisson C, Mekontso Dessap A. Intensive Care Med. 2013 Oct; 39(10):1725-33.[↩]
- Right ventricular failure in acute lung injury and acute respiratory distress syndrome. Repessé X, Charron C, Vieillard-Baron A. Minerva Anestesiol. 2012 Aug; 78(8):941-8.[↩]
- Driving pressure and survival in the acute respiratory distress syndrome. Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG. N Engl J Med. 2015 Feb 19; 372(8):747-55.[↩]
- Right ventricle dilation as a prognostic factor in refractory acute respiratory distress syndrome requiring veno-venous extracorporeal membrane oxygenation. Lazzeri C, Cianchi G, Bonizzoli M, Batacchi S, Terenzi P, Bernardo P, Valente S, Gensini GF, Peris A. Minerva Anestesiol. 2016 Oct; 82(10):1043-1049.[↩]
- High-frequency oscillation in early acute respiratory distress syndrome. Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P, Zhou Q, Matte A, Walter SD, Lamontagne F, Granton JT, Arabi YM, Arroliga AC, Stewart TE, Slutsky AS, Meade MO, OSCILLATE Trial Investigators., Canadian Critical Care Trials Group. N Engl J Med. 2013 Feb 28; 368(9):795-805.[↩]