Contents
What is cyanosis
Cyanosis is a condition in which your lips, fingers, toes and mucous membrane appear blue, purple or grey caused by too little oxygen in your blood 1, 2. The word cyanosis is a derivative of the word cyan, a blue-green color 3, 2. Cyanosis happens when there’s not enough oxygen in your blood or you have poor blood circulation. Cyanosis is a clinical sign of many different conditions and not a disease by itself 3, 2. Underlying diseases that increase the deoxygenated hemoglobin to 5.0 g/dl or more leads to cyanosis 2. Since cyanosis is a clinical sign, a proper evaluation is important to determine the cause of cyanosis 4. Cyanosis happens in some people with congenital heart defects that cause the blood to circulate abnormally.
Red blood cells provide oxygen to body tissues. Most of the time, nearly all red blood cells in the arteries carry a full supply of oxygen. These blood cells are bright red and the skin is pinkish or red.
Blood that has lost its oxygen is dark bluish-red. People whose blood is low in oxygen tend to have a bluish color to their skin. This condition is called cyanosis. The majority of cyanosis is caused by heart or lung problems.
Cyanosis may be due to:
- A blood clot that blocks the blood supply to a leg, foot, hand, or arm
- Lung problems like asthma or pneumonia
- Airways problems like choking or croup
- Heart disease like heart failure or congenital heart disease
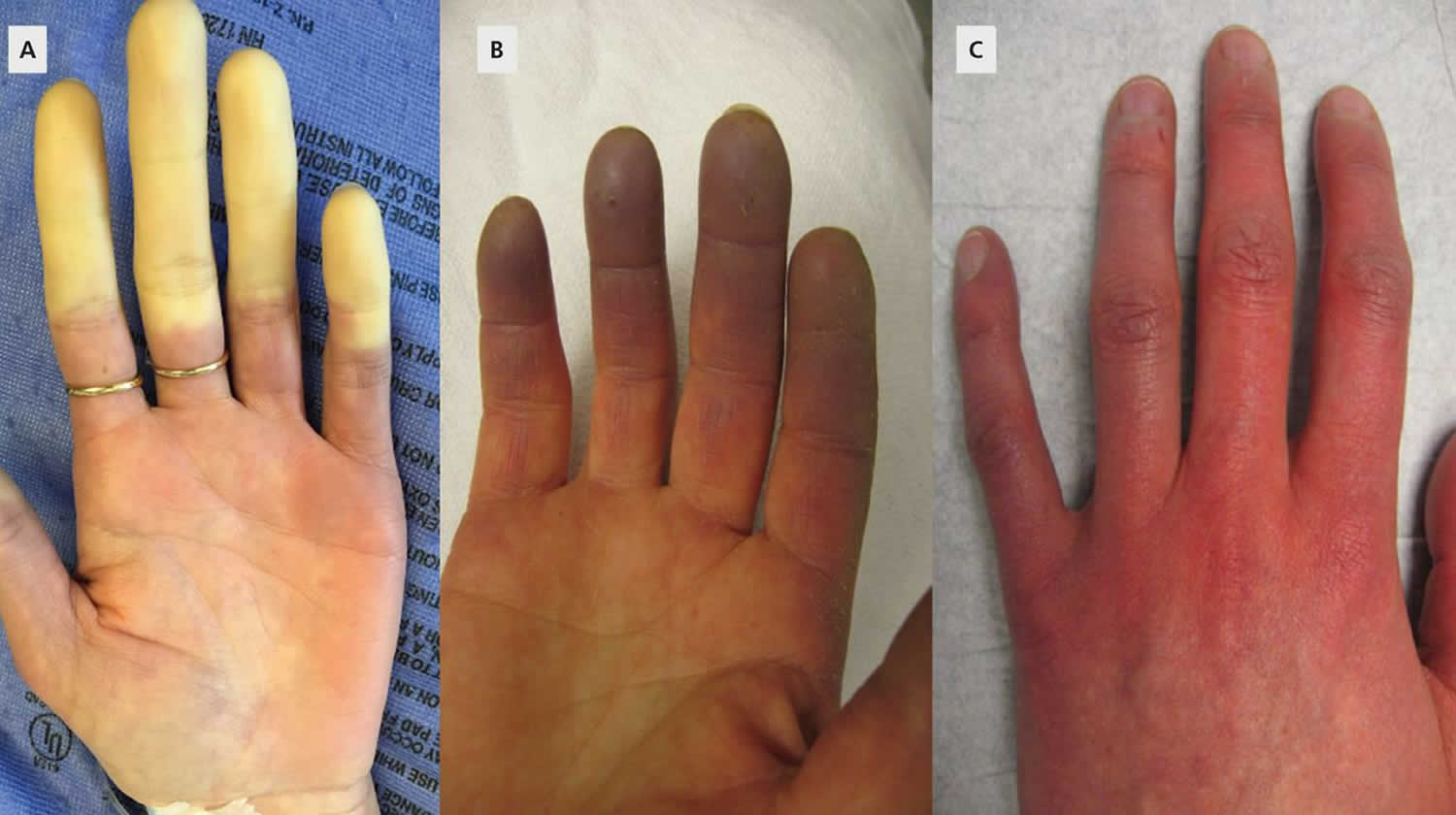
- Raynaud phenomenon is a condition in which cold temperatures or strong emotions cause blood vessel spasms, which block blood flow to the fingers, toes, ears, and nose, that results in cutaneous color changes and sensory symptoms of the digits (Figure 5). Raynaud phenomenon can occur in isolation as primary Raynaud phenomenon or secondary to another disease process. It is thought to be triggered by a heightened sympathetic vasoconstrictive response of small arteriovenous anastomoses in the fingers, toes, ears, and tip of the nose 5. These structures play a key role in maintaining a stable core body temperature by cutaneous thermoregulation 6. Secondary Raynaud phenomenon can be seen with a wide array of systemic conditions as well as environmental and drug exposures 5. Secondary Raynaud phenomenon is a frequent feature of autoimmune rheumatic conditions such as systemic sclerosis, mixed connective tissue disease, systemic lupus erythematosus, and dermatomyositis. Less commonly, cryoproteinemias, paraneoplastic syndromes, hypothyroidism, and carpal tunnel syndrome can be associated with or cause Raynaud phenomenon. Vibratory trauma (eg, from using a jackhammer) and drugs (eg, vasopressors, stimulants, ergots, chemotherapeutic agents) can also cause Raynaud phenomenon 6.
- Beta blockers medicine that is used to treat high blood pressure
- Being in cold air or water
- Wearing clothing or jewellery that’s too tight
Depending on the cause, cyanosis may develop suddenly, along with shortness of breath and other symptoms.
Cyanosis that is caused by long-term heart or lung problems may develop slowly. Symptoms may be present, but are often not severe.
When the oxygen level has dropped only a small amount, cyanosis may be hard to detect.
In dark-skinned people, cyanosis may be easier to see in the mucous membranes (lips, gums, around the eyes) and nails.
Cyanosis is further classified as central cyanosis, peripheral cyanosis and differential cyanosis 7:
- Central cyanosis is a generalized bluish discoloration of the body and at the lips, tongue, and sublingual tissues (visible mucous membranes), which occurs due to inadequate oxygenation secondary to conditions that lead to an increase in deoxygenated hemoglobin or presence of abnormal hemoglobin.
- Peripheral cyanosis is the bluish discoloration of the distal extremities (hands, fingertips, toes), and can sometimes involve circumoral and periorbital areas. Mucous membranes are generally not involved. Peripheral cyanosis when unaccompanied by hypoxemia (as determined by blood gas analysis), peripheral cyanosis is caused by peripheral vasoconstriction and is rarely a life-threatening medical emergency. However, it is essential to determine the underlying cause and its timely management to prevent potential complications.
- Differential cyanosis is the asymmetrical bluish discoloration between the upper and lower extremities. The typical clinical finding of differential cyanosis is usually cyanotic toes with normal fingers. Differential cyanosis is defined as a difference in oxygen saturation (SaO2) of at least 5% or a difference in partial pressure of oxygen (PaO2) of at least 20 mmHg between the arms and legs. This is seen in neonates with patent ductus arteriosus (PDA) and pulmonary arterial hypertension. The deoxygenated blood in the pulmonary artery goes through the patent ductus arteriosus (PDA), empties into the aorta, and flows to the lower half of the body. The upper half of the body continues to received oxygenated blood from the left ventricle 8. Reverse differential cyanosis (cyanotic fingers and normal toes) is seen in infants with transposition of the great arteries (TGA) with coarctation of the aorta or interrupted aortic arch and transposition of the great arteries (TGA) with suprasystemic pulmonary vascular resistance 9. In this setting, the descending aorta is filled with oxygenated blood from the pulmonary circulation, and the lower extremities have higher oxygen saturation than the upper extremities. Under guidelines from the American Academy of Pediatrics, American Heart Association, and the American College of Cardiology, asymptomatic neonates should be screened for congenital heart defects with pulse oximetry at two sites, including the right hand and foot, after 24 hours of life or before discharge. Overall, the percentage of severe congenital heart diseases diagnosed postnatally has increased from 58% with clinical examinations alone to 72% with pulse oximetry, making differential cyanosis rare in neonates 10. In adults, differential cyanosis is pathognomonic for a large untreated patent ductus arteriosus (PDA) associated with Eisenmenger syndrome (shunt reversal into a right-to-left shunt due to progressive pulmonary vascular disease) 8, 11, 12. In the setting of Eisenmenger syndrome (interrupted aortic arch with ventricular septal defect) in pregnancy, differential cyanosis is a rare condition in which cyanosis is evident in both the fingers and the toes, but the arterial oxygen saturation (SaO2) level (measured by pulse oximetry) is much lower in the toes 13.
The bluish discoloration despite adequate oxygenation is sometimes seen due to the ingestion of drugs, toxins, or metals. This is called ‘Pseudocyanosis’ 2
Before the era of rapid blood gas analysis, doctors often assessed a low level of oxygen in the blood (hypoxemia) on clinical grounds alone, primarily by looking for cyanosis in the perioral area and fingers 14, 15. Clinical assessment of hypoxemia (a low level of oxygen in the blood) is now known to be notoriously unreliable 16.
A host of factors, from natural skin pigment to room lighting, can affect detection of cyanosis 16. As with many other physical examination findings, significant interobserver variation occurs in detecting cyanosis 17. Clinicians may diagnose cyanosis as an indicator of hypoxemia when the patient has normal oxygen saturation; alternatively, physicians may miss cyanosis when it should be present (the patient has very low oxygen saturation with normal hemoglobin) 18.
Approximately 5 g/dL of deoxygenated hemoglobin in the capillaries generates the dark blue color appreciated clinically as cyanosis. For this reason, patients who are anemic may be hypoxemic without showing any cyanosis.
Ancillary signs and symptoms of hypoxemia (eg, tachycardia, tachypnea, mental status changes) are nonspecific and of no value in reliably detecting hypoxemia 16. For example, patients may be short of breath at rest for reasons other than hypoxemia (ie, they have normal partial pressure of oxygen [PaO2] and arterial oxygen saturation [SaO2]). Conversely, many patients who are chronically hypoxemic (low PaO2 and/or low SaO2) are perfectly lucid and without any obvious physical signs of their low oxygen state (at least while at rest).
If hypoxemia (low level of oxygen in the blood) is suspected for any reason, some measurement of the oxygen level is necessary (eg, arterial blood gas determination, pulse oximetry). No reliable alternative is available to measure of partial pressure of oxygen (PaO2) or arterial oxygen saturation (SaO2) when diagnosing hypoxemia or assessing the need for supplemental oxygen therapy 19. At the same time, one should not rely on the absence of cyanosis as reassurance that hypoxemia is not present 16.
Cyanosis treatment depends on the underlying cause.
Figure 1. Cyanosis
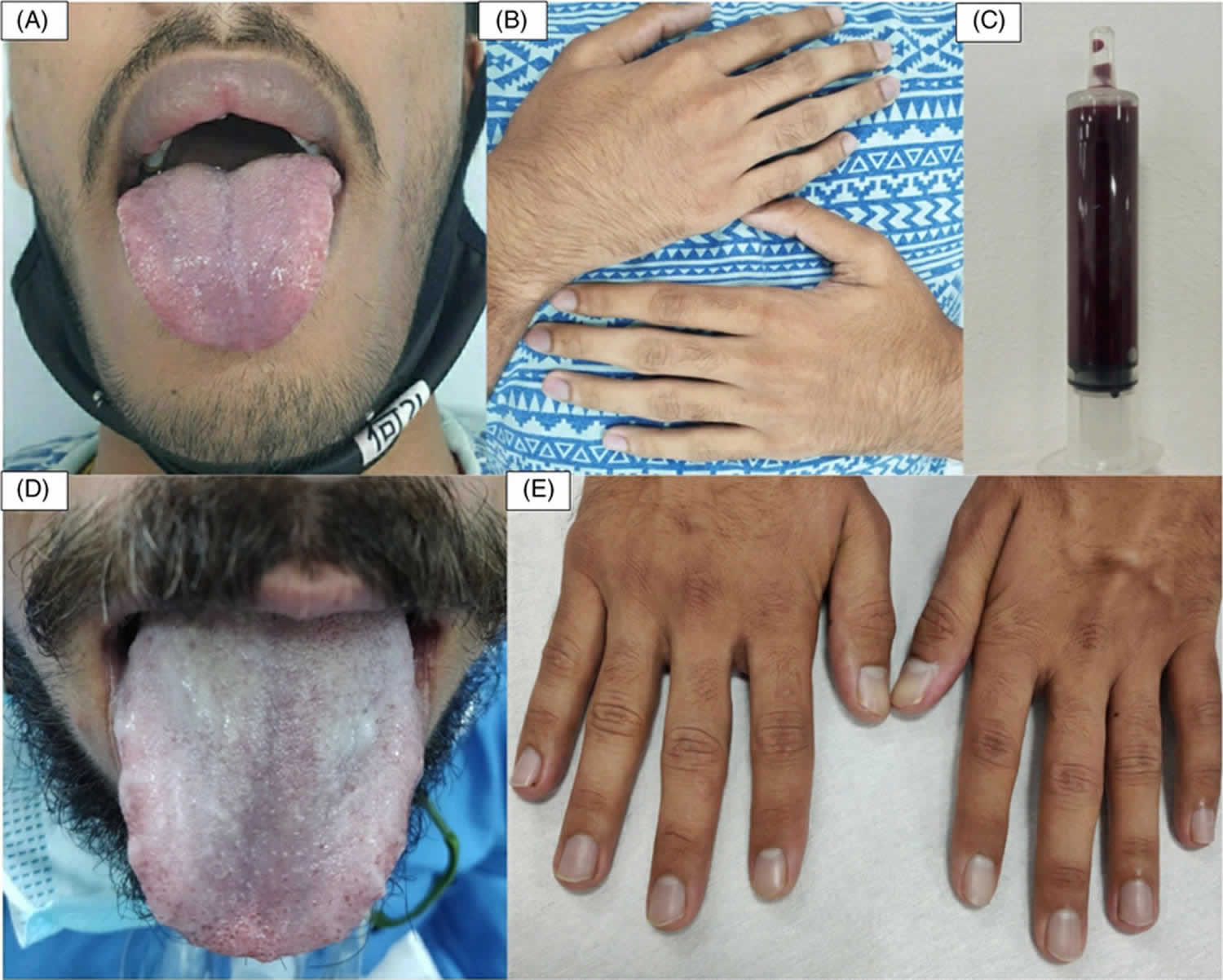
[Source 20 ]Figure 2. Peripheral cyanosis
Footnote: Peripheral cyanosis involving the fingertips. A 16-year-old female was admitted for a bluish discoloration of fingertips, toes, and tongue along with breathlessness, palpitation, and altered sensorium of two days’ duration. She had consumed 15 tablets of dapsone after a quarrel with her mother five days back. She had been taken to a local hospital after she complained of vomiting and abdominal pain. There she had been given a stomach wash and symptomatic treatment and discharged on the second day. On the fifth day after the incident, she was brought to our hospital with the above-mentioned symptoms. There was no history of fever or cough and no past history of any significant medical ailment.
[Source 21 ]Figure 3. Central cyanosis
[Source 22 ]Figure 4. Cyanosis due to methemoglobinemia
[Source 23 ]Figure 5. Raynaud’s phenomenon
Footnote: (A) White digits with intense vasoconstriction in Raynaud phenomenon; (B) blue digits with hypoxemic venous stasis; (C) red digits with hyperemic reperfusion.
[Source 5 ]Peripheral cyanosis
Peripheral cyanosis is a dusky or bluish tinge to the fingers and toes and may occur with or without central cyanosis (ie, with or without hypoxemia). When unaccompanied by hypoxemia, as determined by blood gas analysis, peripheral cyanosis is caused by peripheral vasoconstriction.
Peripheral cyanosis is characterized by the following:
- Localized cyanosis affecting only extremities
- Pink tongue as mucous membranes are almost never involved
- Cold extremities as compared to warm extremities in central cyanosis
- Clubbing is absent
- Pulse volume usually low
- Capillary refill time more than 2 seconds
- Disappears with massage and warming
- Shortness of breath (dyspnea) usually absent
Cyanosis can be a sign of many serious medical problems. Call or visit your health care provider.
For adults, call your doctor or your local emergency number if you have cyanosis and any of the following:
- You cannot get a deep breath or your breathing is getting harder, or faster
- Need to lean forward when sitting to breathe
- Are using muscles around the ribs to get enough air
- Have chest pain
- Are having headaches more often than usual
- Feel sleepy or confused
- Have a fever
- Are coughing up dark mucus
For children, call the doctor or your local emergency number if your child has cyanosis and any of the following:
- Hard time breathing
- Chest muscles moving in with each breath
- Breathing faster than 50 to 60 breaths per minute (when not crying)
- Making a grunting noise
- Sitting with shoulders hunched over
- Is very tired
- Is not moving around much
- Has a limp or floppy body
- Nostrils are flaring out when breathing
- Does not feel like eating
- Is irritable
- Has trouble sleeping
Cyanosis causes
Cyanosis, broadly speaking, is caused by disorders of deoxygenated hemoglobin and disorders of abnormal hemoglobin 3. Oxygen might not reach hemoglobin in an adequate or sufficient amount as a result of conditions affecting the respiratory system, cardiovascular system, and the central nervous system (CNS) 24.
Disorders of deoxygenated hemoglobin are further divided into two broad groups: central cyanosis and peripheral cyanosis. Central cyanosis occurs when the level of deoxygenated hemoglobin in the arteries is above 5 g/dL with oxygen saturation below 85% 3. The bluish hue is generally seen over the entire body surface and visible mucosa. In contrast, peripheral cyanosis is usually only seen in the upper and lower extremities where the blood flow is less rapid. In peripheral cyanosis, there is a significant difference in the saturation between the arterial and venous blood. This occurs as a result of increased oxygen extraction by the peripheral tissue in the capillary bed. Low cardiac output, venous stasis, and exposure to extreme cold causing vasoconstrictions are some of the conditions that can cause peripheral cyanosis.
Causes of central cyanosis include 25, 24:
- Hypoventilation due to conditions affecting the central nervous system, such as intracranial hemorrhage, tonic-clonic seizures, and heroin overdose.
- Pulmonary causes leading to ventilation-perfusion mismatch and impaired alveolar-arterial diffusion, for example, bronchospasm (asthma), pulmonary embolism, pneumonia, bronchiolitis, pulmonary hypertension, hypoventilation, and COPD 26, 27, 28
- Cardiovascular causes include heart failure, congenital heart diseases (right to left shunting), and valvular heart diseases.
- Hemoglobinopathies including methemoglobinemia, sulfhemoglobinemia
- Polycythemia
- High altitude
- Hypothermia
- Anatomic shunts
- Right to left shunt in congenital heart disease
- Intrapulmonary shunt
- Arteriovenous malformation
- Obstructive sleep apnea (OSA)
Peripheral cyanosis can be seen because of the following 2:
- Reduced cardiac output secondary to heart failure or shock
- Local vasoconstriction due to cold exposure, hypothermia, acrocyanosis, and Raynaud phenomenon
- Vasomotor instability
- Arterial obstruction causing regional ischemia secondary to peripheral vascular disease. Causes include atherosclerosis, Buerger disease, atheroembolism
- Venous stasis or obstruction, such as in deep vein thrombosis
- Hyperviscosity attributable to multiple myelomas, polycythemia, and macroglobulinemia
All causes of central cyanosis can also cause peripheral cyanosis. Cardiopulmonary causes and hemoglobin abnormalities are the common causes of central cyanosis.
Differential cyanosis can be seen in patent ductus arteriosus with pulmonary hypertension 29.
Furthermore, cyanosis can be caused by the presence of abnormal hemoglobin also known as hemoglobinopathies. Hemoglobin (Hb) is the major carrier of oxygen in the blood. It is made up of four subunits. Each of the four subunits is made of polypeptide chains, two alpha, and two beta. At the center is a heme group that contains iron. The presence of abnormal hemoglobin causes significant impairment in the oxygen-carrying capacity of the blood. This can cause tissue hypoxia which can manifest clinically as cyanosis.
Methemoglobinemia is a condition that can produce congenital or acquired cyanosis. Methemoglobinemia arises when the iron in hemoglobin (Hb) is converted from the ferrous (Fe2+) to the ferric (Fe3+) state and, for this reason, cannot bind to oxygen 23, 3. Approximately 2% of hemoglobin is present in methemoglobin (MetHb) form, the oxidized form of hemoglobin. The presence of methemoglobin (MetHb) can impart an intense bluish tinge to the skin; therefore, the cyanosis of methemoglobinemia is not related to reduced hemoglobin but to oxidized hemoglobin 30, 31. The methemoglobin (MetHb) shifts the oxygen-hemoglobin (Hb) dissociation curve to the left, hindering the release of oxygen in tissues. These two conditions compromise oxygen exchange and supply to tissues, causing a cyanosis that does not resolve with oxygen therapy, which is a clue to the diagnosis 32. Although excess methemoglobin (MetHb) reduces the measured arterial oxygen saturation (SaO2), partial pressure of oxygen (PaO2) is not affected, because methemoglobin (MetHb) does not affect transfer of oxygen from the atmosphere to the lungs. A low partial pressure of oxygen (PaO2) in a patient with excess methemoglobin (MetHb) suggests a concomitant pulmonary problem.
Methemoglobinemia can be triggered by exposure to some topical anesthetic agents (lidocaine-prilocaine cream), nitrite or nitrate-containing compounds (eg, nitroglycerin), or other strong oxidizing agents 33, 34, 35, 36. Dahshan and Donovan 37 reported a case of severe methemoglobinemia from topical benzocaine in a toddler. Dapsone, a drug used in human immunodeficiency virus (HIV) and non-HIV conditions, can also cause methemoglobinemia 35, 36, 38.
Methemoglobinemia can also be congenital (present at birth). Congenital methemoglobinemia type 1 and 2 is an autosomal recessive disorder due to deficiency of nicotinamide adenine dinucleotide (NADH)-cytochrome b5 reductase (cytb5r) 39. Congenital methemoglobinemia type 1 and 2 is extremely rare. The lack of enzymatic activity by cytochrome b5 reductase causes decreased reduction of methemoglobin 36.
A rare hereditary methemoglobinemia has also been described in a family with Hb M-Hyde Park (Hb M-Akita) (HBB:c.277C > T; p.His93Tyr) 40. Garcia Sanchez et al 41 reported the case of a cyanotic infant with methemoglobinemia from a cow’s milk protein allergy.
Methemoglobinemia resulting from toxic ingestion or inhalation in suicide attempts or completions is also found in the literature, including an unusual case in which a patient had concurrent methemoglobinemia and carboxyhemoglobinemia following pesticide ingestion 42, 43, 44.
The methemoglobin (MetHb) can be measured in a co-oximeter, which is incorporated into most hospital blood gas machines. The co-oximeter also measures carboxyhemoglobin, hemoglobin content, and arterial oxygen saturation (SaO2). Note that standard pulse oximeters, which measure arterial oxygen saturation (SaO2) using two wavelengths of light, do not measure methemoglobin (MetHb) or carboxyhemoglobin. However, pulse oximeters that use eight wavelengths of light do have the ability to measure carboxyhemoglobin and methemoglobin (MetHb) 45.
Sulfhemoglobinemia is another rare cause of cyanosis that arises from sulfur binding to hemoglobin so that oxygen cannot be bound 3. Sulfhemoglobinemia causes the uncoupling of oxygen from hemoglobin to be very difficult. The iron in the hemoglobin remains unchanged in its ferrous state in sulfhemoglobinemia 3. Sulfhemoglobin is similar to methemoglobin (MetHb) in causing low arterial oxygen saturation (SaO2) but not affecting partial pressure of oxygen (PaO2) and in imparting an intense bluish color to the skin. Although sulfhemoglobinemia is most often associated with the use of drugs such as phenacetin, metoclopramide, dapsone, phenzopyridine, and trimethoprim-sulfamethoxazole, hydrogen-sulfide-producing intestinal bacteria, such as Morganella morganii, have also been reported to be etiologic agents 46, 47.
Pseuodcyanosis is another uncommon condition that can mimic peripheral cyanosis and occurs as a result of contact with drugs such as amiodarone 3. Exposure to gold or silver salts also can cause pseudocyanosis. In pseudocyanosis there is no response to attempted “blanching” of the skin by applying pressure, and the presence of a bluish tinge to the skin and/or mucous membranes is not associated with either hypoxemia or peripheral vasoconstriction. For confirmation of the diagnosis, obtain pulse oximetry or arterial blood gas. Pseudocyanosis is generally due to drug exposure (eg, amiodarone) and, much more rarely, metal exposure (chrysiasis, argyria) 48. Baernstein et al 49 described blue-gray discoloration in a man who ingested colloidal silver for years for urinary tract infections due to a neurogenic bladder; his oxygen levels were normal. Zillich et al 50 described a girl with intensely blue skin from food coloring.
Lack of oxygen in your blood
Most cyanosis also called central cyanosis, occurs because of a lack of oxygen in your blood. This can be caused by the following problems.
Problems with your lungs:
- Blood clot in the arteries of the lungs (pulmonary embolism)
- Drowning or near-drowning
- High altitude
- Infection in the smallest air passages in the lungs of children, called bronchiolitis
- Long-term lung problems that become more severe, such as chronic obstructive pulmonary disease (COPD), asthma, and interstitial lung disease
- Pneumonia (severe)
Problems with your airways leading to your lungs:
- Breath-holding (although this is exceedingly difficult to do)
- Choking on something stuck in the airways
- Swelling around the vocal cords (croup)
- Inflammation of the tissue (epiglottis) that covers the windpipe (epiglottitis)
Problems with your heart:
- Heart defects that are present at birth (congenital)
- Heart failure
- Heart stops working (cardiac arrest)
Congenital heart defects that cause cyanosis include
- Tetralogy of Fallot
- Transposition of the great arteries
- Truncus arteriosus
- Tricuspid atresia
- Pulmonary atresia
- Total anomalous pulmonary venous connection
- Hypoplastic left heart syndrome
- Double Outlet Right Ventricle (DORV)
Other problems:
- Drug overdose (narcotics, benzodiazepines, sedatives)
- Exposure to cold air or water
- Seizure that lasts a long time
- Toxins such as cyanide
Cyanosis pathophysiology
Cyanosis is due to inadequate oxygenation of blood or the amount of oxygen bound to hemoglobin is very low 51, 52. Oxygen in the blood is carried in two physical states. About 98% of oxygen is normally bound to hemoglobin, with the remaining 2% dissolved in plasma 51, 52. Cyanosis results when the deoxyhemoglobin exceeds 5.0 g/dL. The bright red color of the blood is due to an adequate content of oxygen in the blood, which changes to a darker red with a reduced level of oxygen reflecting more blue light making the skin appear to have a blue tint. However, the blue tint is more apparent with high hemoglobin count 3.
The pathophysiology of cyanosis is as follows 51, 52:
- Hypoxic Hypoxia: Due to decreased oxygen tension and content in arterial and venous blood, the oxygen diffusion to the tissues is decreased 53.
- Inspired air is low in oxygen content: Sea level, high altitude
- Decreased ventilation: Emphysema, respiratory center depression
- Decreased diffusion through the alveolar-capillary membrane: fibrosis, interstitial edema
- Right to left shunting of blood in the heart: patent ductus arteriosus (PDA), interventricular or interatrial defects
- Stagnant Hypoxia: In this oxygen tension and content in the arterial blood is normal, but the hypoxia is due to reduced or uneven blood flow to the tissues. As a result of the increased extraction of the available oxygen at the tissue level, the oxygen tension, and content in the venous blood decrease.
- Generalized reduced blood flow: Congestive heart failure.
- Localized reduced blood flow: Peripheral vascular diseases such as Raynaud which can lead to peripheral vessel spasm (the lack of blood flow leads to the white coloration of fingers, followed by bluish discoloration when the veins dilate to keep the blood flow going, finally returning to red color on the restoration of blood flow)
- Asphyxia: In asphyxia, there is both hypoxia as well as increased levels of carbon dioxide (hypercapnia)
Peripheral cyanosis occurs due to the inability of the body to deliver oxygen-rich blood to the peripheral tissues 2. Congestive peripheral cyanosis can be caused due to the slowing of blood flow. Ischemic peripheral cyanosis occurs when vasoconstriction leads to diminished peripheral blood flow. In peripheral cyanosis, there is normal arterial oxygen saturation but increased oxygen extraction by the peripheral tissue in the capillary bed in the setting of peripheral vasoconstriction and decreased peripheral blood flow. This results in a significant difference in the saturation between the arterial and venous blood, with increased deoxygenated blood on the venous side of the capillary beds 54.
Reduced cardiac output in heart failure and shock can lead to peripheral cyanosis, if severe. Lack of pressure prevents an adequate supply of oxygen-rich blood to the extremities. Also, hypotension produces reflex cutaneous vasoconstriction to shunt blood from extremities to the internal organs. This redistribution of blood flow from extremities causes cyanosis of extremities.
Exposure to cold increases the transit time through capillary beds. This results in cyanosis due to increased unloading of oxygen from the blood to the tissues.
Benign vasomotor changes can cause acrocyanosis, a form of peripheral cyanosis. It can be a normal finding in babies which resolves within the first few days of life. Additionally, it can also be seen in infancy when babies cry, vomit, regurgitate, cough, hold their breath. It is not considered pathologic unless there is significantly low cardiac output leading to cutaneous vasoconstriction.
In the Raynaud phenomenon, abnormal vasospasm occurs with exposure to change in temperature and emotional events. The diminished blood flow causes a blue discoloration of the fingers and toes.
Cyanosis symptoms
Cyanosis is a condition in which your lips, fingers, toes and mucous membrane appear blue or grey caused by too little oxygen in your blood. Depending on the cause, cyanosis may develop suddenly, along with shortness of breath and other symptoms. In people with congenital heart defects, cyanosis can happen if the defect allows oxygen-poor blood from the right side of the heart to enter the left side of the heart directly, instead of traveling to the lungs for more oxygen. In the left side of the heart, the oxygen-poor blood mixes with oxygen-rich blood to be pumped through your body. Oxygen-poor blood is not as bright red as oxygen-rich blood. The low oxygen level in the blood is what makes the lips, fingers, and toes look blue.
Cyanosis in newborn
When a baby is first born, the skin is a dark red to purple color. As the baby begins to breathe air, the color changes to red. This redness normally begins to fade in the first day. A baby’s hands and feet may stay bluish in color for several days. This is a normal response to a newborn’s immature blood circulation.
Blue coloring of other parts of the body is not normal. Occasionally, a baby’s face or lips and mouth may turn purplish with very intense crying. However, this should turn back pink when the baby stops crying. If the baby’s color does not turn pink again, or there is an overall blue tinge to the baby, this may signal a problem. Cyanosis is often seen in babies with a heart defect, because the heart cannot pump the oxygenated blood to the rest of the body. Breathing difficulties may also cause cyanosis. Consult your baby’s pediatrician immediately if your baby has any blue coloring.
Cyanosis differential diagnosis
Abnormal bluish discoloration of different parts of the body could be attributable to different underlying pathologies. Some of them are mentioned below:
- Differential cyanosis where the lower limb is cyanosed and upper limb is pink. It can be seen in patent ductus arteriosus with reversed shunt due to pulmonary hypertension.
- Reversed differential cyanosis is seen more in upper limbs as compared to lower limbs. It is seen in the transposition of great arteries.
- Pigmentary birthmarks
- Large tattoos
- Drugs causing gray-blue skin discoloration side effects, such as amiodarone and silver
- Blue clothing dye
- Consumption of blue-dyed food such as popsicles
- Acrodermatitis enteropathica
- Anemia
- Asthma
- Heart failure
- Herb poisoning
- Hydrocarbon toxicity
- Metabolic acidosis
- Pediatric anaphylaxis
- Pulmonary embolism
- Rotavirus
Cyanosis diagnosis
Detailed history and physical examination are vital in determining the underlying cause of cyanosis. Your doctor will perform a physical examination. This will include listening to your breathing and heart sounds. In emergency situations (such as shock), you will be stabilized first.
Your doctor will ask about your symptoms. Questions may include:
- When did the bluish skin develop? Did it come on slowly or suddenly?
- Is your body blue all over? How about your lips or nailbeds?
- Have you been exposed to cold or gone to a high altitude?
- Do you have trouble breathing? Do you have a cough or chest pain?
- Do you have ankle, foot, or leg swelling?
In assessing cyanosis, the onset is an important clue to the underlying cause. If your cyanosis is present since birth, the cause is highly suggestive of a congenital cause. In congenital heart diseases, the conditions which present with cyanosis in the first week are tricuspid atresia, Ebstein anomaly, critical pulmonary stenosis, etc. The conditions which usually manifest with cyanosis after the first week are tetralogy of Fallot, transposition of great arteries (TGA), truncus arteriosus, etc. However, a more recent onset of cyanosis is highly suggestive of acquired cause of cyanosis. It is also essential to differentiate between central cyanosis, peripheral cyanosis, and differential cyanosis as each implies different causes. In children, the most common causes for life-threatening central cyanosis are congenital heart disorders and polycythemia. The common causes of peripheral cyanosis in this age group are cold exposure and acrocyanosis.
Fever may be seen if the cause of cyanosis is infectious such as croup, pneumonia, septic shock, etc. The presence of clubbing can most likely be seen in congenital heart conditions, right to left shunts, and pulmonary diseases. Respiratory symptoms are more commonly associated with central cyanosis.
Physical examination should be carried out in an adequate light for the correct assessment of cyanosis. Poor light exposure, the thickness of the skin, and pigmentation of the skin can affect the accuracy of physical assessment. Cheeks, nose, ears, and oral mucosa are the best areas to assess cyanosis as the skin in these areas is thin, and blood supply is good. This can help determine if the cyanosis is generalized, limited to extremities, or if there is a difference in the bluish discoloration in different extremities.
The prime sites of the bluish discoloration in central cyanosis are lips, tongue, hands, feet, and mucous membranes of the oral cavity. The depth of the color usually correlates with the amount of desaturated hemoglobin, and hence, the severity of cyanosis. Clubbing can be seen in some patients with long-standing central cyanosis. Methemoglobinemia or sulfhemoglobinemia should be high on differentials if central cyanosis does not get better with oxygen administration.
The inspection also includes looking for any thoracic cage deformity, accessory muscle use for respiration (nasal flaring, grunting, intrathoracic/supraclavicular retractions), asymmetry of chest expansion, discomfort in breathing, audible breath sounds, clubbing, posture, etc. These are helpful in narrowing down the underlying causes, especially if the cause is cardiac or pulmonary. It is helpful to carry out the palpation of brachial and femoral pulses, tactile and vocal fremitus, assessment of ventilation, and measurement of blood pressure in all four extremities.
Tests that may be ordered include:
- Arterial blood gas analysis
- Blood oxygen saturation by pulse oximetry
- Chest x-ray
- Chest CT scan
- Complete blood count (CBC)
- Electrocardiogram (ECG)
- Echocardiogram (ultrasound of the heart)
Oxygenation status can be assessed by determining the oxygen saturation of hemoglobin, partial pressure of oxygen, and total hemoglobin. Various types of devices can measure oxygen saturation, but the measured variables are different from each device. Co-oximetry and pulse oximetry are spectrophotometry methods to measure arterial blood oxygenation. Pulse oximetry is a non-invasive method as compared to co-oximetry, which requires a sample of arterial blood. The arterial blood gas shows the partial pressure of dissolved oxygen in the blood as well as the saturation of hemoglobin.
To begin with, pulse oximetry, a non-invasive and easily available test, should be done to rule out life-threatening hypoxemia as a cause. The pulse oximeter measures the absorption of light at only two wavelengths which correspond to that of oxyhemoglobin and deoxyhemoglobin. The drawback of measuring only two wavelengths is that it can create a misleading picture when evaluating a patient with cyanosis secondary to methemoglobinemia. This is because abnormal hemoglobin is not picked up by the pulse oximetry; therefore, in methemoglobinemia, the pulse oximetry reading is falsely elevated 55, 56, 57.
Co-oximetry provides a more accurate evaluation of oxygen saturation because it measures the absorption of light at four different wavelengths corresponding to oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin, and methemoglobin. Co-oximetry, in addition to measuring oxygen saturation, can be used for arterial blood gas analysis. For a patient presenting with cyanosis in which abnormal hemoglobin is suspected, co-oximetry is a useful diagnostic tool. Co-oximetry test also determines the value of hemoglobin derivatives such as oxygenated hemoglobin, deoxygenated hemoglobin, and dyshemoglobins (methemoglobin, carboxyhemoglobin, sulfhemoglobin, etc.). It, therefore, only indicates low oxygen levels in hypoxemia due to central cyanosis. In pseudocyanosis, both pulse oximetry and co-oximetry reveal normal oxygen levels 56, 58, 55.
Arterial blood gas analysis shows normal arterial oxygenation in peripheral cyanosis, i.e., 85-100%. Contrary to this, the arterial oxygen saturation is low in central cyanosis.
Another abnormal hemoglobin that can cause congenital cyanosis is hemoglobin M. This hemoglobin is formed as a result of mild structural changes in the alpha and beta chains that keep it in an oxidized ferric state, thereby reducing the oxygen-carrying capacity. Routine hemoglobin electrophoresis can best detect this 59.
Peripheral blood film, hemoglobin concentration, blood glucose, and sepsis workup should be considered depending on the clinical scenario to evaluate the causes of cyanosis.
Additionally, chest X-ray, ECG, and CT scan can be done to evaluate the cardiopulmonary cause. Echocardiogram and invasive cardiac evaluation may be necessary in some cases.
Cyanosis treatment
Cyanosis is a sign of a disease process and not a disease by itself. The treatment you receive depends on the underlying condition causing your cyanosis 60, 3, 2. For example, you may receive oxygen for shortness of breath. For cyanosis caused by exposure to cold or Raynaud phenomenon, dress warmly when going outside or stay in a well-heated room. For cyanosis caused by congenital heart diseases surgery for the correction congenital heart disease-causing cyanosis may be required. In infants and neonates with cyanotic congenital heart disease like tetralogy of Fallot, tricuspid atresia, truncus arteriosus, or total anomalous venous return, prompt referral for cardiology assessment and intervention is necessary. If the cardiac lesion is ductal dependent for pulmonary blood flow, prostaglandin E1 infusion might be necessary to keep the ductus arteriosus open. In the management of neonates with cyanosis, careful attention should be paid to the correction of metabolic derangements like hypoglycemia and hypocalcemia. Metabolic derangements can occur as a result of the inability to feed secondary to cyanotic heart diseases in children.
Impairment of oxygen diffusion and transfer and other conditions affecting the respiratory system that lead to hypoxia also can cause cyanosis. Oxygen support can be provided to resolve the hypoxia. The regular nasal cannula, high flow nasal cannula, and in some instances, assisted ventilation might be required to provide adequate respiratory support.
For methemoglobinemia-induced cyanosis, the standard treatment is methylene blue. Nicotinamide adenine dinucleotide phosphate helps in the conversion of methylene blue to leucomethylene blue. This end product helps reduce methemoglobin to normal hemoglobin 61, 57, 62.
Exposure to gold or silver salts also can produce cyanosis. The best therapy in this instance is to remove the offending agents.
In summary, treatment of cyanosis can be very challenging, and a multidisciplinary approach with different subspecialists might be needed in the management 3, 2.
- Hiremath G, Kamat D. Diagnostic considerations in infants and children with cyanosis. Pediatr Ann. 2015 Feb;44(2):76-80. doi: 10.3928/00904481-20150203-12[↩]
- Pahal P, Goyal A. Central and Peripheral Cyanosis. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559167[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Adeyinka A, Kondamudi NP. Cyanosis. [Updated 2023 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482247[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Kamp GA, Heymans HS, Breederveld C. Is ‘het maskertje’ teken van perifere of van centrale cyanose? [Is circumoral cyanosis a sign of peripheral or of central cyanosis?]. Ned Tijdschr Geneeskd. 1989 Jul 8;133(27):1360-4. Dutch.[↩]
- Shapiro SC, Wigley FM. Treating Raynaud phenomenon: Beyond staying warm. Cleve Clin J Med. 2017 Oct;84(10):797-804. https://doi.org/10.3949/ccjm.84a.17025[↩][↩][↩]
- Wigley FM, Flavahan NA. Raynaud’s Phenomenon. N Engl J Med. 2016 Aug 11;375(6):556-65. doi: 10.1056/NEJMra1507638[↩][↩]
- Chan HL. Cutaneous manifestations of cardiac diseases. Singapore Med J. 1990 Oct;31(5):480-5.[↩]
- Lin TW, Tseng CW, Huang CY, Wang KY, Liang KW. Familial clustering of congenital deafness, patent ductus arteriosus, Eisenmenger complex, and differential cyanosis: A case report. Medicine (Baltimore). 2017 Jun;96(24):e7105. doi: 10.1097/MD.0000000000007105[↩][↩]
- Al-Mukhaini KS, Mohamed AM. Transposition of the Great Arteries and Coarctation of the Aorta in an Infant Presenting with Bronchiolitis: An incidental finding. Sultan Qaboos Univ Med J. 2017 Aug;17(3):e348-e351. doi: 10.18295/squmj.2017.17.03.016[↩]
- Oster ME, Kochilas L. Screening for Critical Congenital Heart Disease. Clin Perinatol. 2016 Mar;43(1):73-80. doi: 10.1016/j.clp.2015.11.005[↩]
- Sabnis GR, Phadke MS, Lanjewar CP, Kerkar PG, Nabar AA. Differential cyanosis and clubbing sparing a single limb. J Am Coll Cardiol. 2014 Apr 15;63(14):e33. doi: 10.1016/j.jacc.2013.11.058[↩]
- Moccetti F, Kaufmann BA, Tobler D. Differential clubbing and cyanosis: a pathognomonic finding in cardiology. Eur Heart J. 2014 Jun 1;35(21):1410. doi: 10.1093/eurheartj/ehu020[↩]
- Chou WR, Kuo PH, Shih JC, Yang PC. A 31-year-old pregnant woman with progressive exertional dyspnea and differential cyanosis. Chest. 2004 Aug;126(2):638-41. doi: 10.1378/chest.126.2.638[↩]
- Lundsgaard C, Van Slyke DD. Cyanosis. Medicine. 1923 Feb 1. 2:1-76.[↩]
- Mizutani T, Hojo M. Severe hypoxaemia due to methaemoglobinaemia and aspiration pneumonia. Emerg Med J. 2012 Jan;29(1):74-6. doi: 10.1136/emj.03.2011.3937rep[↩]
- Cyanosis. https://emedicine.medscape.com/article/303533-overview#showall[↩][↩][↩][↩]
- Carpenter KD. A comprehensive review of cyanosis. Crit Care Nurse. 1993 Aug;13(4):66-72.[↩]
- COMROE JH Jr, BOTELHO S. The unreliability of cyanosis in the recognition of arterial anoxemia. Am J Med Sci. 1947 Jul;124(1):1-6. doi: 10.1097/00000441-194707000-00001[↩]
- Martin L. All You Really Need to Know to Interpret Arterial Blood Gases. 2nd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999.[↩]
- Peters, P.J., Delbressine, F., & Feijs, L.M. (2014). Designing preterm neonatal cyanosis simulation. International Work-Conference on Bioinformatics and Biomedical Engineering. [↩]
- Kamath SD, Sunny S, Upadhyay A. A Case Report of Cyanosis With Refractory Hypoxemia: Is It Methemoglobinemia? Cureus. 2022 Nov 30;14(11):e32053. doi: 10.7759/cureus.32053[↩]
- Pulmonary arteriovenous fistula mimicking as acyanotic heart disease with shunt reversal. January 2016 Medical Journal of Dr D Y Patil University 9(4):541. DOI:10.4103/0975-2870.186077[↩]
- Sapra, D., Singh, G.K., Bahuguna, A., Das, P. and Gupta, A. (2022), Three doses of dapsone causing methemoglobinemia in leprosy: A report of two cases. Dermatologic Therapy, 35: e15551. https://doi.org/10.1111/dth.15551[↩][↩]
- Lundsgaard C, Van Slyke D, Abbott ME. Cyanosis. Can Med Assoc J. 1923 Aug;13(8):601-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1707134/pdf/canmedaj00431-0081.pdf[↩][↩]
- Mutlu B, Yılmaz Keskin E, Oliveira AC, Relvas L, Bento C. A Rare Cause of Cyanosis Since Birth: Hb M-Iwate. Turk J Haematol. 2019 Nov 18;36(4):299-301. doi: 10.4274/tjh.galenos.2019.2019.0123[↩]
- Pahal P, Hashmi MF, Sharma S. Chronic Obstructive Pulmonary Disease Compensatory Measures. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525962[↩]
- Pahal P, Avula A, Sharma S. Emphysema. [Updated 2023 Jan 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482217[↩]
- Pahal P, Rajasurya V, Sharma S. Typical Bacterial Pneumonia. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534295[↩]
- Hobbelink EL, Salomons MA, Soetekouw R. Een vrouw met blauwe vingers [A woman with blue fingers]. Ned Tijdschr Geneeskd. 2018 Jul 20;162:D2449. Dutch.[↩]
- Bradberry SM. Occupational methaemoglobinaemia. Mechanisms of production, features, diagnosis and management including the use of methylene blue. Toxicol Rev. 2003;22(1):13-27. doi: 10.2165/00139709-200322010-00003[↩]
- Umbreit J. Methemoglobin–it’s not just blue: a concise review. Am J Hematol. 2007 Feb;82(2):134-44. doi: 10.1002/ajh.20738[↩]
- Carreira R, Palaré MJ, Prior AR, Garcia P, Abrantes M. An unusual cause of neonatal cyanosis…. BMJ Case Rep. 2015 Mar 9;2015:bcr2014208371. doi: 10.1136/bcr-2014-208371[↩]
- Yoon JC, Kim SE. Suicide attempt using sodium nitrite ordered on the internet: Two case reports. Medicine (Baltimore). 2022 Jul 15;101(28):e29355. doi: 10.1097/MD.0000000000029355[↩]
- Shamriz O, Cohen-Glickman I, Reif S, Shteyer E. Methemoglobinemia induced by lidocaine-prilocaine cream. Isr Med Assoc J. 2014 Apr;16(4):250-4. https://www.ima.org.il/FilesUploadPublic/IMAJ/0/77/38667.pdf[↩]
- Riaz S, Kudaravalli P, Saleem SA, Heisig D. Methemoglobinemia: A Life-threatening Complication of Topical Pharyngeal Anesthetics. Cureus. 2020 Apr 30;12(4):e7900. doi: 10.7759/cureus.7900[↩][↩]
- Taleb M, Ashraf Z, Valavoor S, Tinkel J. Evaluation and management of acquired methemoglobinemia associated with topical benzocaine use. Am J Cardiovasc Drugs. 2013 Oct;13(5):325-30. doi: 10.1007/s40256-013-0027-2[↩][↩][↩]
- Dahshan A, Donovan GK. Severe methemoglobinemia complicating topical benzocaine use during endoscopy in a toddler: a case report and review of the literature. Pediatrics. 2006 Apr;117(4):e806-9. doi: 10.1542/peds.2005-1952[↩]
- Shenouda M, Padilla M, Silva J, Castillo H, Austin A. Dapsone-Induced Methemoglobinemia: A Case Report. Cureus. 2022 Feb 21;14(2):e22466. doi: 10.7759/cureus.22466[↩]
- Aslan D, Türköz-Sucak G, Percy MJ. Recessive congenital methemoglobinemia in immediate generations. Turk J Pediatr. 2016;58(1):113-115. doi: 10.24953/turkjped.2016.01.019[↩]
- Schnedl WJ, Queissner R, Schenk M, Enko D, Mangge H. Hereditary methemoglobinemia caused by Hb M-Hyde Park (Hb M-Akita) (HBB:c.277C > T; p.His93Tyr). Wien Klin Wochenschr. 2019 Aug;131(15-16):381-384. doi: 10.1007/s00508-019-1525-2[↩]
- García Sánchez P, Santos Simarro G, Sampredro Martín M, Valladares Salado L, Escolano Taravillo L. A Cyanotic Infant: Infrequent Presentation of Cow’s Milk Protein Allergy. Cureus. 2022 Jan 28;14(1):e21678. doi: 10.7759/cureus.21678[↩]
- Arva K, Sharma A. A rare combination of methemoglobinemia and carboxyhemoglobinemia in pesticide poisoning. Am J Emerg Med. 2022 Dec;62:148.e5-148.e7. doi: 10.1016/j.ajem.2022.09.010[↩]
- Tazón-Varela MA, Padilla-Mielgo Á, Villaverde-Plazas R, Espinoza-Cuba F, Gallo-Salazar N, Muñoz-Cacho P. Methemoglobinemia Secondary to Inhalation of Automobile Emissions with Suicide Motivations. J Clin Med. 2023 Jan 17;12(3):734. doi: 10.3390/jcm12030734[↩]
- Majdanik S, Potocka-Banaś B, Glowinski S, Luzny S. Suicidal intoxication with mercury chloride. Forensic Toxicol. 2023 Jul;41(2):304-308. doi: 10.1007/s11419-022-00653-7[↩]
- Barker SJ, Curry J, Redford D, Morgan S. Measurement of carboxyhemoglobin and methemoglobin by pulse oximetry: a human volunteer study. Anesthesiology. 2006 Nov;105(5):892-7. doi: 10.1097/00000542-200611000-00008. Erratum in: Anesthesiology. 2007 Nov;107(5):863.[↩]
- George A, Goetz D. A case of sulfhemoglobinemia in a child with chronic constipation. Respir Med Case Rep. 2017 Mar 14;21:21-24. doi: 10.1016/j.rmcr.2017.03.009[↩]
- Murphy K, Ryan C, Dempsey EM, O’Toole PW, Ross RP, Stanton C, Ryan CA. Neonatal Sulfhemoglobinemia and Hemolytic Anemia Associated With Intestinal Morganella morganii. Pediatrics. 2015 Dec;136(6):e1641-5. doi: 10.1542/peds.2015-0996[↩]
- McMullen SM, Patrick W. Cyanosis. Am J Med. 2013 Mar;126(3):210-2. doi: 10.1016/j.amjmed.2012.11.004[↩]
- Baernstein A, Smith KM, Elmore JG. Singing the blues: is it really cyanosis? Respir Care. 2008 Aug;53(8):1081-4. https://rc.rcjournal.com/content/53/8/1081/tab-pdf[↩]
- Zillich AJ, Kuhn RJ, Petersen TJ. Skin discoloration with blue food coloring. Ann Pharmacother. 2000 Jul-Aug;34(7-8):868-70. doi: 10.1345/aph.19338[↩]
- Lundsgaard C. STUDIES ON CYANOSIS : II. SECONDARY CAUSES OF CYANOSIS. J Exp Med. 1919 Sep 1;30(3):271-93. doi: 10.1084/jem.30.3.271. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2126678/pdf/271.pdf[↩][↩][↩]
- Lundsgaard C. STUDIES ON CYANOSIS : I. PRIMARY CAUSES OF CYANOSIS. J Exp Med. 1919 Sep 1;30(3):259-69. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2126682/pdf/259.pdf[↩][↩][↩]
- Zemore Z, Sharma A, Carter K, Baghdassarian A. Delayed Presentation of Tetralogy of Fallot with Isolated Cyanosis. Case Rep Pediatr. 2018 Jun 20;2018:7412869. doi: 10.1155/2018/7412869[↩]
- Das S, Maiti A. Acrocyanosis: an overview. Indian J Dermatol. 2013 Nov;58(6):417-20. doi: 10.4103/0019-5154.119946[↩]
- Ralston AC, Webb RK, Runciman WB. Potential errors in pulse oximetry. III: Effects of interferences, dyes, dyshaemoglobins and other pigments. Anaesthesia. 1991 Apr;46(4):291-5. doi: 10.1111/j.1365-2044.1991.tb11501.x[↩][↩]
- Ralston AC, Webb RK, Runciman WB. Potential errors in pulse oximetry. I. Pulse oximeter evaluation. Anaesthesia. 1991 Mar;46(3):202-6. doi: 10.1111/j.1365-2044.1991.tb09410.x[↩][↩]
- Jubran A. Pulse oximetry. Crit Care. 2015 Jul 16;19(1):272. doi: 10.1186/s13054-015-0984-8[↩][↩]
- Webb RK, Ralston AC, Runciman WB. Potential errors in pulse oximetry. II. Effects of changes in saturation and signal quality. Anaesthesia. 1991 Mar;46(3):207-12. doi: 10.1111/j.1365-2044.1991.tb09411.x[↩]
- Da-Silva SS, Sajan IS, Underwood JP 3rd. Congenital methemoglobinemia: a rare cause of cyanosis in the newborn–a case report. Pediatrics. 2003 Aug;112(2):e158-61. doi: 10.1542/peds.112.2.e158[↩]
- Steinhorn RH. Evaluation and management of the cyanotic neonate. Clin Pediatr Emerg Med. 2008 Sep;9(3):169-175. doi: 10.1016/j.cpem.2008.06.006[↩]
- Wright RO, Lewander WJ, Woolf AD. Methemoglobinemia: etiology, pharmacology, and clinical management. Ann Emerg Med. 1999 Nov;34(5):646-56. doi: 10.1016/s0196-0644(99)70167-8[↩]
- Jubran A. Pulse oximetry. Intensive Care Med. 2004 Nov;30(11):2017-20. doi: 10.1007/s00134-004-2399-x[↩]