Contents
- Disseminated intravascular coagulation
Disseminated intravascular coagulation
Disseminated intravascular coagulation also known as DIC, is a serious, sometimes life-threatening condition in which the proteins in your blood involved in blood clotting become overactive. Blood clots form in small blood vessels throughout your body. This can disrupt normal blood flow to organs such as the kidneys and liver and can lead to organ failure. Because the clotting uses up coagulation proteins and platelets, excessive bleeding can occur. This abnormal activation of blood clotting mechanisms can develop as the result of a variety of diseases and conditions.
Typically, when a person has an injury to a blood vessel and bleeding occurs, the body stops the bleeding by initiating a process called hemostasis. First, platelets adhere to the injury site and clump together, forming a loose plug. Then coagulation factors are sequentially activated (see coagulation cascade) to produce a net of fibrin threads that weave through the platelet plug and form a stable clot. The clot stays in place until the injury is healed, then other factors break the clot down (fibrinolysis) and remove it. This clotting process is tightly regulated. Feedback mechanisms accelerate the clotting process, then slow it down, and control the volume of clot produced.
Normally, the body initiates hemostasis and forms a blood clot only when needed, i.e., when there is an injury and bleeding. The body detects a pro-coagulant, a substance such as tissue factor that is released from cells when they are damaged. Based on the extent of the injury, the body responds by stimulating sufficient clotting to stop the bleeding and confining it locally, that is, only at the site of injury.
With conditions that trigger DIC, the response is exaggerated, clotting is activated throughout the body, and control mechanisms are inhibited. The result is the formation of a multitude of tiny clots that can block small blood vessels and prevent blood and oxygen from getting to tissues and organs, leading to multi-organ failure. Widespread clotting can use up platelets and coagulation factors at a rapid rate. This can overwhelm the system to the point that the body begins to bleed excessively because platelets and clotting factors have been depleted. Simultaneous clotting and bleeding can occur. DIC can develop very quickly, becoming serious or even life-threatening in a short time.
DIC signs and symptoms may include bleeding, bruising, low blood pressure, shortness of breath, or confusion. Complications can be life-threatening and include bleeding or multiple organ failure.
Signs and symptoms of DIC may include:
- Bruising, which may appear easily, and often in various areas as small dots or larger patches
- Bleeding at the site of wounds from surgical cuts or from placement of a needle
- Bleeding from the nose, gums, or mouth, including when you brush your teeth
- Blood in the stools from bleeding in the intestines or stomach. Stools may appear dark red or like tar.
- Blood in the urine
- Chest pain, trouble breathing, and shortness of breath
- Confusion, speech changes or trouble speaking, dizziness, or seizures
- Headaches
- Low blood pressure
- Pain, redness, warmth, and swelling in the lower leg
- Unusually heavy periods
Disseminated intravascular coagulation may occur with conditions such as:
- Infections, especially with severe or systemic infections (and sometimes resulting sepsis), primarily bacterial but also sometimes seen with fungal, viral, or parasitic infections
- Trauma, such as due to an accident or significant burns
- Major surgery, such as cardiopulmonary bypass surgery
- Pregnancy and childbirth, especially when a woman has retained placental material, or a fetus that has died (stillbirth)
- Cancers, such as acute promyelocytic leukemia or tumors that develop within glands (adenocarcinoma); cancer cells may release a pro-coagulant.
- Organ failure, such as liver, pancreas, or kidney failure
- Other less common causes, such as snake bite venom, toxic drug reaction, blood transfusion reaction, organ transplant, or frostbite
DIC may develop quickly over hours or days, or more slowly. Most cases of DIC that are diagnosed develop rapidly and suddenly (acute), but there are cases in which it develops gradually, occurring over a longer period of time. This chronic form of DIC is difficult to recognize and is much less often diagnosed. Simultaneous clotting and bleeding can occur with chronic DIC, but in most cases this is a lower grade, persistent clotting activation process and the body has sufficient capacity to compensate. With chronic disseminated intravascular coagulation, the predominant feature is typically increased clotting, not bleeding. Cancer is one of the most common causes of low-grade DIC.
DIC that develops quickly usually requires emergency treatment in the hospital. In treating DIC, your doctor will treat the disease that is causing DIC. Your doctor may also give you medicines to prevent blood clots, or blood products such as platelets or clotting factors to stop bleeding.
The goals of treatment for disseminated intravascular coagulation are to address the underlying condition that is causing the clotting activation and to stabilize the affected person. In most cases, DIC will resolve when the disease or condition is treated. Acute DIC is typically treated in a hospital setting.
Supportive measures may need to be taken to address bleeding and clotting. People primarily presenting with severe bleeding may be given platelets or fresh frozen plasma or cryoprecipitate that contains clotting factors, especially when surgical procedures are required to address the underlying condition – such as with a retained placental material.
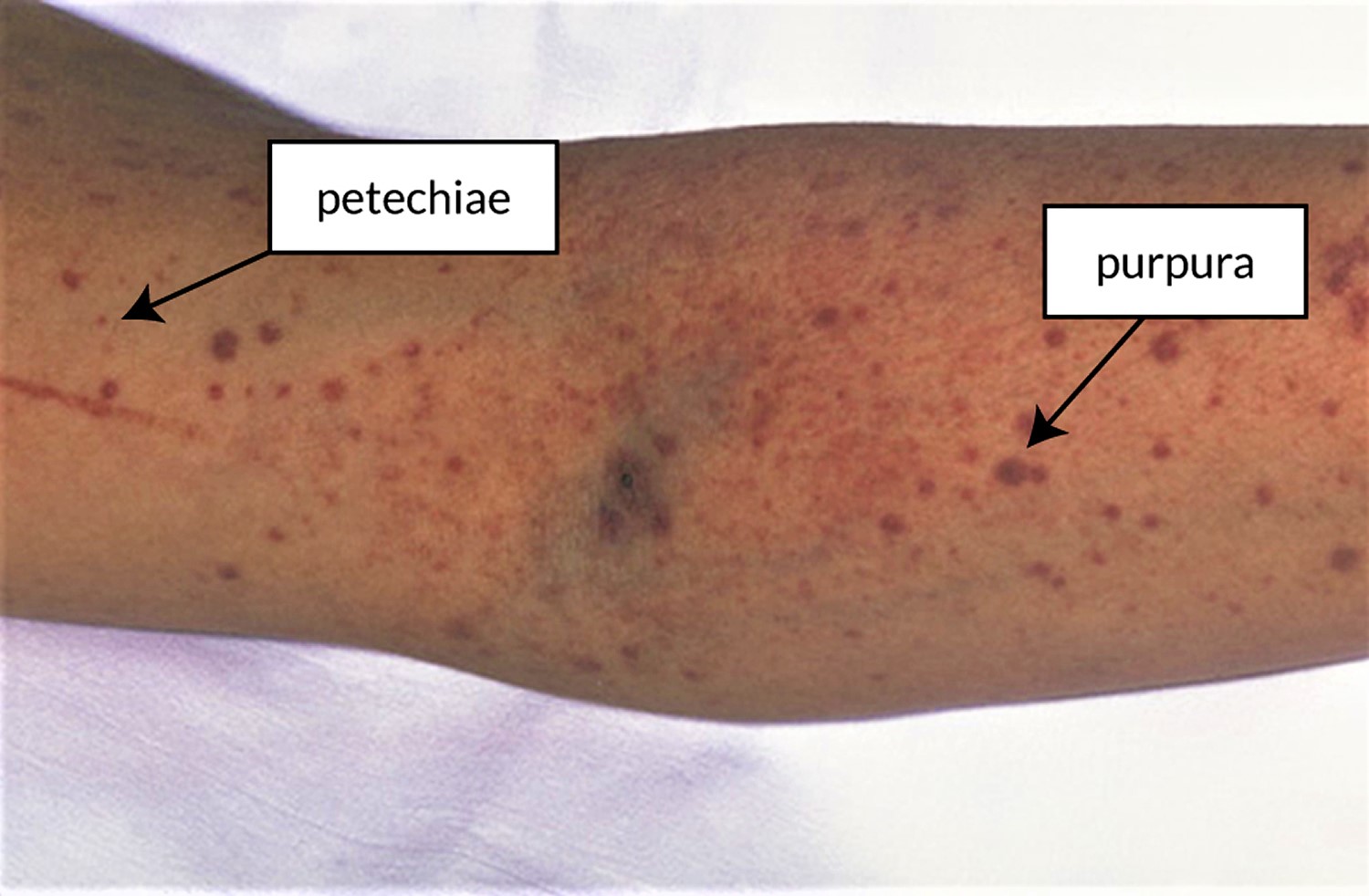
Figure 1. Purpura and petechiae that are often seen with DIC. The larger red, brown, and purple dots are purpura and the smaller red and purple dots are petechiae.
Disseminated intravascular coagulation causes
Disseminated intravascular coagulation is caused by another medical condition that makes the body’s normal blood clotting process become overactive. The condition progresses through two stages. In the early stages, overactive clotting leads to blood clots throughout the blood vessels. The clots can reduce or block blood flow, damaging organs.
As DIC progresses, the overactive clotting uses up platelets and clotting factors, which are proteins that help with normal blood clotting. Without these platelets and clotting factors, DIC can cause bleeding just beneath the skin, in the nose or mouth, or deep inside the body.
Causes of DIC include:
- Inflammation in response to infection, injury, or an illness
- Severe tissue damage, such as from burns or trauma
- Clotting factors caused by some cancers or pregnancy complications. Pregnancy complications that produce clotting factors include placental abruption, in which the placenta separates from the uterus, and amniotic fluid embolism, in which amniotic fluid that surrounds the unborn baby enters the mother’s bloodstream.
To understand DIC, it helps to understand the body’s normal blood clotting process. When you are injured, proteins in the blood that form blood clots travel to the injury site to help stop bleeding. Blood clots form naturally at sites of injury to prevent or control bleeding. When small cuts or breaks occur on the walls of the blood vessels, your body turns on clotting factors. The clotting factor thrombin forms long fibrin protein strands that clump together with platelets to create blood clots that then seal the cuts or breaks. Once bleeding stops, the body begins breaking down the clots as part of the blood vessel healing process. If these proteins become abnormally active throughout the body, you could develop DIC. The underlying cause is usually due to inflammation, infection, or cancer.
In some cases of DIC, small blood clots form in the blood vessels. Some of these clots can clog the vessels and cut off the normal blood supply to organs such as the liver, brain, or kidneys. Lack of blood flow can damage and cause major injury to the organs.
In other cases of DIC, the clotting proteins in your blood are consumed. When this happens, you may have a high risk of serious bleeding, even from a minor injury or without injury. You may also have bleeding that starts spontaneously (on its own). The disease can also cause your healthy red blood cells to fragment and break up when they travel through the small vessels that are filled with clots.
Risk factors for DIC
Risk factors for DIC include:
- Blood transfusion reaction
- Cancer including cancers affecting the pancreas, stomach, colon and especially certain types of leukemia
- Inflammation of the pancreas (pancreatitis)
- Infection in the blood or sepsis, a body-wide response to infection that causes inflammation, is the most common risk factor for DIC. The infection may be caused by parasites, bacteria, fungi, or viruses.
- Liver disease
- Pregnancy complications, such as when the placenta separates from the uterus before delivery, when amniotic fluid enters the bloodstream, or when there is serious bleeding during or after delivery (such as placenta that is left behind after delivery)
- Recent surgery or anesthesia
- Severe tissue injury (as in burns and head injury)
- Use of illegal drugs, such as cocaine and ecstasy, may increase the risk of DIC.
- Blood vessel abnormalities, including aortic aneurysms and large hemangiomas (blood vessels that are not formed properly), which are growths of tangled blood vessels
- Heat stroke
- Severe immune reactions, which may occur with an incompatible blood transfusion, rejection of an organ transplant, or a toxin such as snake venom
Disseminated intravascular coagulation signs and symptoms
Signs and symptoms of DIC depend upon the underlying condition, such as infection, trauma or malignancy, and on the severity and the extent of DIC. Signs and symptoms of DIC also depend on whether the condition is acute or chronic. Acute DIC is more severe and develops quickly over hours or days. The first sign may be bleeding. Chronic DIC, such as from cancer, happens more slowly and sometimes has no signs or symptoms. In addition to signs and symptoms of the underlying condition, those of disseminated intravascular coagulation are associated with bleeding and/or inappropriate clotting.
Bleeding
Significant bleeding usually occurs from at least three different sites:
- Blood in the stool or urine from internal bleeding
- Headaches and other symptoms associated with bleeding in the brain
- Bruising and the formation of small red dots on the skin (petechiae)
- Bleeding at the site of wounds, surgical sites, intravenous (IV) needle or catheter sites
- Mucosal bleeding – from the nose, gums, mouth, etc.
Blood clotting
Symptoms depend on the location of blood clots and may include:
- Symptoms associated with organ dysfunction caused by blood clots blocking blood flow and oxygen to organs such as the liver and kidney, leading to liver and kidney failure
- Blackening of the skin caused by blockage from blood clots and poor blood flow to the skin
- Chest pain, coughing up blood, and/or difficulty breathing caused by blood clots in the lungs
- Chest pain and/or a heart attack caused by clotting in the heart
- Headaches and other symptoms associated with a stroke, caused by clotting in the brain
Disseminated intravascular coagulation complications
Complications from DIC can occur from both the clotting that happens in the early stages of the condition and from bleeding in the later stages. Serious complications include organ damage and hemorrhage.
DIC can lead to complications resulting from overactive clotting or from the bleeding that follows. These complications can be life-threatening and may include:
- Acute respiratory distress syndrome (ARDS)
- Bleeding from the gastrointestinal tract (GI tract) or elsewhere in the body if you have acute DIC. This is not common in chronic DIC, since clotting develops more slowly, and your body can make enough platelets and clotting factors.
- Heart attack, if a blood clot blocks or limits blood flow to your heart
- Multiple organ failure, if blood clots prevent oxygen from reaching your organs. These organs can include the lungs and kidneys, followed by the brain, heart, liver, spleen, adrenal glands, pancreas, and the gastrointestinal tract.
- Shock
- Stroke, if a blood clot blocks or limits blood flow to your brain, or if there is bleeding in the brain
- Venous thromboembolism, which can include blood clots in the lungs, called pulmonary embolism, or in the deep veins of the legs, called deep vein thrombosis
Disseminated intravascular coagulation diagnosis
Your doctor will diagnose DIC based on your medical history, a physical exam, and tests. Your doctor will also look for the cause of DIC, because it does not occur on its own.
To help diagnose DIC, your doctor will ask about any medical conditions or recent events, such as illness or an injury, that could cause or be a risk factor for DIC. Your doctor will do a physical exam to look for signs and symptoms of blood clots, bleeding, or a condition that could cause DIC or a complication of DIC.
If your doctor suspects DIC, the following blood tests may help diagnose it. The goals of testing are to identify DIC, evaluate its severity, and to monitor its effects over time. There is not a single test that can be used to definitely diagnose DIC. A healthcare practitioner will consider many factors when assessing a person who may have this condition, such as signs and symptoms, presence of an underlying condition, physical examination, and medical history.
The severity and extent of DIC can change over time so laboratory testing is often performed at several intervals to monitor a person’s status. Some routine tests that may be performed include:
- CBC (complete blood count) – includes a platelet count; in DIC, platelets are often low.
- Blood smears from individuals with DIC often show decreased number of platelets and presence of large platelets and fragmented red cells (schistocytes).
- PT (prothrombin time) – often prolonged with DIC as coagulation factors are consumed
- PTT (partial thromboplastin time) – may be prolonged
- D-dimer – a test that detects a protein that results from clot break-down; it is often markedly elevated with DIC; if normal, then DIC is unlikely.
- Fibrinogen – one of the clotting factors; is low with DIC
A test scoring system developed by the International Society on Thrombosis and Haemostasis may be used to evaluate a group of test results to help determine if DIC is present. The score is based on the results of a platelet count, PT, D-dimer (or fibrin degradation products) and fibrinogen. The higher the score, the more likely it is that DIC is present.
As DIC can affect the health and function of several organs, more general testing, such as a comprehensive metabolic panel (CMP), may be ordered to evaluate, for example, the functional status of kidneys and liver. Additionally, several other tests may be ordered to help detect the underlying disease or condition that is causing a person to develop DIC.
Your doctor may suggest additional tests or procedures to find out whether another condition is causing your symptoms. These tests may include:
- ADAMTS13 testing to check blood levels and activity of this protein, which is low in thrombotic thrombocytopenic purpura (TTP), a type of platelet disorder
- Liver biopsy and liver function tests to check for cirrhosis or chronic liver disease, which may have signs and symptoms that are similar to DIC
Non-laboratory tests
An x-ray or other imaging scan is sometimes performed to help locate blood clots and evaluate organs.
Disseminated intravascular coagulation treatment
There is no specific treatment for DIC. The goal is to determine and treat the underlying cause of DIC. The main goals of treatment for DIC are to control clotting and bleeding and to treat the underlying cause. DIC may go away once the underlying cause is treated.
Supportive treatments may include:
- Plasma transfusions to replace blood clotting factors if a large amount of bleeding is occurring.
- Blood thinner medicine (heparin) to prevent blood clotting if a large amount of clotting is occurring.
Your doctor may use anticoagulants, also called blood thinners, to reduce blood clotting. You may be given them as a pill, as an injection, or through an IV. Possible side effects include bleeding, especially if you are taking other medicines that also thin your blood, such as aspirin.
Your doctor may recommend the following treatments:
- Clotting factor replacement such as fibrinogen. This is used to stop bleeding.
- Oxygen therapy to allow more oxygen to reach the lungs, the heart, and the rest of the body if blood clots are preventing oxygen from reaching your organs.
- Plasma transfusion, which provides clotting factors, to stop or prevent bleeding.
- Platelet transfusion to quickly raise platelet levels to stop or prevent bleeding.
Disseminated intravascular coagulation prognosis
Outcome depends on what is causing the disseminated intravascular coagulation. DIC can be life threatening.
Acute DIC and its underlying causes are serious life-threatening conditions, so your treatment management and recovery will likely be done in the hospital. If you have been diagnosed with DIC, it is important that you follow your treatment plan, get regular care, and learn the warning signs of complications.
You may need to take blood-thinning medicines to help prevent blood clots or to keep existing clots from getting larger. If you are taking blood thinners, talk to your doctor about how often you should schedule follow-up visits. Your doctor may recommend regular blood tests to check how well your blood is clotting.
Also, let everyone on your healthcare team know you are taking blood-thinning medicines. If you need surgery, your doctor may adjust the amount of medicine you take before, during, and after the surgery to prevent bleeding. This also may happen before dental work, but it is less common.
Talk with your doctor before using any over-the-counter medicines or products, including vitamins, supplements, or herbal remedies. Some of these products can affect blood clotting and bleeding. For example, aspirin and ibuprofen may thin your blood too much. This can increase your risk of bleeding. Vitamin K supplements can prevent certain blood thinners from working.
Learn the warning signs of serious complications and have a plan
DIC can lead to serious complications such as heart attack or stroke. Risks of treatment with blood thinners include severe bleeding in the brain.
If you think that you or someone else is having the following symptoms, call your local emergency services number immediately. Every minute matters.
Bleeding
If you take a dose of blood-thinning medicine that is too high, it may cause bleeding in the digestive system or in the brain. Signs and symptoms include severe pain in your head, sudden changes in your vision, sudden inability to move your legs or arms, memory loss or confusion, bright red vomit or vomit that looks like coffee grounds, blood in your urine or stool, or black, tarry stools.
A lot of bleeding after a fall or injury, or easy bruising or bleeding, may mean that your blood is too thin. Excessive bleeding is bleeding that will not stop after you apply pressure to a wound for 10 minutes. Call your doctor right away if you have any of these signs.
Heart attack
Heart attack symptoms include mild or severe chest pain or discomfort in the center of the chest or upper abdomen that lasts for more than a few minutes or goes away and comes back. This discomfort can feel like pressure, squeezing, fullness, heartburn, or indigestion. There also may be pain down the left arm. Although men and women can experience these symptoms, women are more likely to have other, less typical symptoms, such as shortness of breath, nausea, vomiting, unusual tiredness, and pain in the back, shoulders, or jaw. Read more about the signs and symptoms of a heart attack.
Stroke
If you think someone may be having a stroke, act F.A.S.T. and perform the following simple test.
- F—Face: Ask the person to smile. Does one side of the face droop?
- A—Arms: Ask the person to raise both arms. Does one arm drift downward?
- S—Speech: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- T—Time: If you observe any of these signs, call your local emergency services number immediately. Early treatment is essential.