What is ecthyma
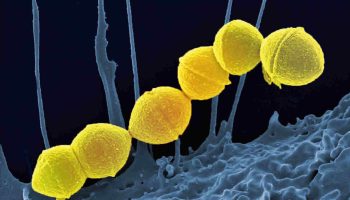
Ecthyma is a skin infection characterized by crusted sores beneath which ulcers form. Ecthyma is a deep form of impetigo, as the same bacteria causing the infection are involved. Ecthyma causes deeper erosions of the skin into the dermis. Streptococcus pyogenes and Staphylococcus aureus are the bacteria responsible for ecthyma.
Ecthyma is a condition in which the inflammation caused by a neglected pyogenic infection involves the entire epidermis. Lesions can evolve from within sites of pre-existing trauma or boils, and are most commonly found on the buttocks, legs and feet. The initial lesion is composed of one or more pustules or vesicles on an erythematous base. The lesion is soon covered by a crust, which can be thick and adherent. The margin can be indurated, raised and violaceous. Untreated lesions may enlarge slowly over weeks-months to a diameter of 2-3 cm. Lesions heal with scarring.
Patients are usually otherwise well.
People of all ages, sex and race can be affected, although children, older people and immunocompromised patients (e.g., diabetes, neutropenia, immunosuppressive medication, malignancy, HIV) tend to have a higher chance of ecthyma infection. Other factors that increase the risk of ecthyma include:
- Poor hygiene and crowded living conditions
- High temperature and humidity in tropical places
- Presence of minor injuries or other skin conditions such as scratches, insect bites or dermatitis
- Untreated impetigo, particularly in patients with poor hygiene.
Figure 1. Ecthyma
Ecthyma symptoms
Ecthyma most often affects buttocks, thighs, legs, ankle and feet. Occasionally, the local lymph nodes become swollen and painful.
Ecthyma lesion usually begins as a vesicle (small blister) or a pustule on an inflamed area of skin.
- A hard crust soon covers the blister.
- With difficulty, the crust can be removed to reveal an indurated ulcer that may be red, swollen and oozing with pus.
- Lesions may stay fixed in size and sometimes resolve spontaneously without treatment, or they may gradually enlarge to a sore of 0.5–3 cm in diameter.
- They resolve slowly leaving a scar.
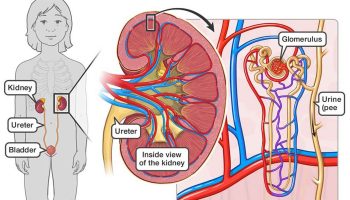
Ecthyma complications
Complications of ecthyma may include:
- More widespread infection: cellulitis, erysipelas, lymphangitis, gangrene, lymphadenitis, and bacteremia
- Permanent scarring
- Rarely, post-streptococcal glomerulonephritis.
Ecthyma treatment
Treatment depends on the extent and severity of infection. Any underlying disease or skin infection such as scabies or dermatitis should also be treated.
Soak crusted areas
- Soak a clean cloth in a mixture of half a cup of white vinegar in a litre of tepid water. Apply the compress to moist areas for about ten minutes several times a day. Gently wipe off the crusts.
Topical antiseptics or antibiotics
- A topical antibiotic ointment such as fusidic acid or >mupirocin is often prescribed for localised ecthyma. A topical antiseptic such as povidone iodine, superoxidised solution, antibacterial Manuka honey or hydrogen peroxide cream may be used instead. Apply it at least three times a day to the affected areas and surrounding skin. The treatment should be applied after removing crusts. Look carefully for new lesions to treat. Continue for several days after healing.
Oral antibiotics
- Oral antibiotics are recommended if the infection is extensive or proving slow to respond to topical antibiotics. The antibiotic of choice is a penicillin, usually dicloxacillin or flucloxacillin, which are active against both Streptococcus pyogenes and Staphylococcus aureus. The duration of treatment varies; several weeks of therapy may be necessary to completely resolve ecthyma.
Improve hygiene
Another critical factor to consider in the overall management of ecthyma is to improve hygiene. Measures to take include:
- Washing daily with antiseptic soap or cleanser
- Changing and laundering clothes and linen frequently
- Using separate towels and flannels to prevent spreading infection.
- Use nets and repellent sprays to prevent insect bites.
- Reduce scratching at insect bites, chickenpox blisters and scabies by applying calamine lotion, colloidal oatmeal or baking soda.
Ecthyma prognosis
Ecthyma can sometimes result in scarring.
Ecthyma gangrenosum
Ecthyma gangrenosum is an uncommon cutaneous infection most commonly associated with Pseudomonas aeruginosa bacteremia. Ecthyma gangrenosum usually occurs in critically ill and immunocompromised patients, especially when there is a prolonged spell of neutropenia. The characteristic lesions of ecthyma gangrenosum are hemorrhagic (bloody) pustules that evolve into necrotic (black) ulcers with a tender erythematous border.
Erythema gangrenosum is characterized by single or multiple cutaneous or mucous membrane ulcers that are most often associated with prolonged spells of neutropenia. Lesions resemble ecthyma. Erythema gangrenosum first present as a pustule or nodule, which quickly develops a central hemorrhagic area that subsequently breaks down to form a large necrotic ulcer with a tender erythematous border.
Patients are usually unwell
What does ecthyma gangrenosum look like?
The initial lesions of ecthyma gangrenosum appear as painless, round, red patches in the skin which rapidly become pustular with surrounding redness. A haemorrhagic focus appears in the centre, forming a blister. As the haemorrhagic blister spreads peripherally, it evolves into a gangrenous ulcer with a black/gray scab surrounded by a red halo. An early lesion may transform into a necrotic ulcer in as little as 12 hours.
Ecthyma gangrenosum may appear at any site but mainly affects the anogenital area and armpits. The arms and legs, trunk and face are less often involved.
Figure 2. Ecthyma gangrenosum
Figure 3. Ecthyma gangrenosum face
Footnote: 2-year-old boy with autoimmune lymphoproliferative syndrome presenting with solitary ecthyma gangrenosum on the forehead. Blood culture, as well as culture from the lesion both, showed growth of Pseudomonas aeruginosa. Pseudomonal sepsis responded well to piperacillin-tazobactam and amikacin therapy.
[Source 1 ]Ecthyma gangrenosum causes
Impaired immunity leads to increased susceptibility to infections with Pseudomonas or other pathogens. Breakdown of mechanical defensive barriers such as skin and mucosa allow entry of infectious organisms.
The lesions of ecthyma gangrenosum result from bacterial invasion of the walls of arteries and veins in the skin and subcutaneous tissue. The bacterial invasion may come from inside the vessel in the case of septicemia, or by direct inoculation of bacteria through the skin. Damage to the vessel walls causes interruption of the local blood supply with initially redness, edema, pustule formation and hemorrhage then necrosis of the skin with scab and ulcer formation.
Ecthyma gangrenosum is typically caused by Pseudomonas aeruginosa but ecthyma gangrenosum-like lesions have been observed in patients with other bacterial, fungal and viral infections including:
Gram-positive bacteria
- Staphylcoccus aureus
- Streptococcus pyogenes
Gram-negative bacteria
- Aeromonas hydrophila
- Chromobacterium violaceum
- and others
Fungi
- Aspergillus fumigatus
- Candida albicans
- Mucor and Rhizopus species (zygomycosis)
- and others
Viruses
- Herpes simplex
Ecthyma gangrenosum diagnosis
The following tests are performed to identify the exact cause of the infection.
Gram stain
- A Gram stain of fluid from the central hemorrhagic pustule or blister can rapidly indicate the diagnosis. If no fluid is present, the scab should be lifted and a swab taken from underneath.
Blood cultures
- Two specimens are normally taken prior to starting antibiotic therapy. The optimum time for collection is during a temperature spike. Sensitivity studies are done on any isolated organisms.
Skin biopsy
A skin biopsy is taken for routine histology and special stains may also be done to to rule out other organisms that may cause ecthyma gangrenosum-like lesions.
Histopathology of ecthyma gangrenosum lesions shows vascular necrosis with few inflammatory cells but many surrounding bacteria. In sections stained with Gram stain, gram-negative rods are numerous surrounding necrotic vessels. Hemorrhage, edema and necrosis are seen in and around the involved vessels.
Tissue cultures
A second skin biopsy is usually sent for tissue culture for bacteria, fungi, yeasts and mycobacteria. Sensitivity tests are done on any isolated organisms.
Ecthyma gangrenosum treatment
Ecthyma gangrenosum requires prompt diagnosis and treatment with appropriate antibiotics for the underlying cause. The presence of ecthyma gangrenosum should alert the physician to the likelihood of an accompanying Pseudomonas septicemia.
Antibiotics which may be used include
- Antipseudomonal penicillin such as piperacillin
- Aminoglycosides
- Fluoroquinolines
- Third-generation cephalosporins
- Aztreonam
While awaiting culture results, piperacillin is usually given in combination with an aminoglycoside. Antibiotic choice may require adjustment once antibiotic sensitivity results are known.
If a blood stream infection with fungi is suspected, systemic antifungal therapy should be considered to include cover against Aspergillus, Candida and Mucor species, with azoles such as itraconazole or fluconazole, and/or amphotericin B if appropriate.
Ecthyma gangrenosum prognosis
Development of ecthyma gangrenosum lesions in individuals with sepsis is associated with a poor prognosis and is fatal in 20% to 77% of patients 2. In individuals with non-bacteremic ecthyma gangrenosum, the mortality rate is significantly lower at 8% 2. The underlying immunosuppressive state (e.g., malignancy, renal failure, or other) is often the main determinant of clinical outcome 3. The presence of neutropenia at the time of diagnosis is the most important prognostic factor of mortality 4.
- Ecthyma Gangrenosum as the Presenting Clinical Feature of Autoimmune Lymphoproliferative Syndrome. Indian Journal of Paediatric Dermatology 2018, Volume: 19, Issue Number:1, Page: 62-64. http://www.ijpd.in/temp/IndianJPaediatrDermatol19162-4593106_011633.pdf[↩]
- Sarkar S, Patra AK, Mondal M. Ecthyma gangrenosum in the periorbital region in a previously healthy immunocompetent woman without bacteremia. Indian Dermatol Online J. 2016 Jan-Feb;7(1):36-9[↩][↩]
- Grisaru-Soen G, Lerner-Geva L, Keller N, Berger H, Passwell JH, Barzilai A. Pseudomonas aeruginosa bacteremia in children: analysis of trends in prevalence, antibiotic resistance and prognostic factors. Pediatr. Infect. Dis. J. 2000 Oct;19(10):959-63[↩]
- Martínez-Longoria CA, Rosales-Solis GM, Ocampo-Garza J, Guerrero-González GA, Ocampo-Candiani J. Ecthyma gangrenosum: a report of eight cases. An Bras Dermatol. 2017 Sep-Oct;92(5):698-700[↩]