Contents
What is encephalocele
Encephaloceles are rare neural tube birth defects associated with skull defects characterized by partial lacking of bone fusion leaving a gap through which a portion of the brain sticks out (protrudes). In some cases, cerebrospinal fluid or the membranes that cover the brain (meninges) may also protrude through this opening in the skull. The portion of the brain that sticks outside the skull is usually covered by skin or a thin membrane so that the defect resembles a small sac. Protruding tissue may be located on any part of the head, but most often affects the back of the skull (occipital encephalocele). Occurrence of occipital encephalocele is common in western hemisphere where as anterior encephaloceles are found more often in south East Asia 1. The Centers for Disease Control and Prevention (CDC) estimates that approximately 375 babies are born each year in the United States with an encephalocele. That would be approximately 1 in 10,000 babies each year. Females are more likely to have an encephalocele in the back (occipital area) of the skull, while males are more likely to have one in the front of the skull. In Western populations, encephaloceles are more common in the back of the skull. In Southeast Asia, they are more common in the front of the skull.
Incidence of encephalocele is not uncommon in developing countries. The incidence ranges from 1-3 per 1000 live births worldwide 2. Anterior encephalocele is a rare entity among encephalocele. Incidence of anterior encephalocele in the western countries varies from 1/35,000 to 1/40,000 live births, but in Asian countries its incidence increases to 1/5000 live births 3. Encephaloceles occurs commonly in the mid sagittal plane anywhere from frontonasal region to the occiput 4. Occurrence of encephalocele in occipital region (75%), followed by frontoethmoidal (13% to 15%), parietal (10% to 12%) or sphenoidal.
The functional problems that may arise depending on the location and the size of encephalocele. These are the following:
- Hydrocephalus (a condition in which excess cerebrospinal fluid in the skull causes pressure on the brain)
- Neurological problems
- Vision problems
- Growth problems
It may be emphasized, however, that many cases are not accompanied by functional problems and the mental development may be entirely normal.
Encephaloceles are classified as neural tube defects. The neural tube is a narrow channel in the developing fetus that allows the brain and spinal cord to develop. The neural tube folds and closes early during pregnancy (third or fourth week) to complete the formation of the brain and spinal cord. A neural tube defect occurs when the neural tube does not close completely, which can occur anywhere along the head, neck or spine. The lack of proper closing of the neural tube can lead to a herniation process which appears as a pedunculated (having a stalk-like base) or sessile (attached directly to its base without a stalk) cystic lesion protruding through a defect in the cranial vault referred as encephalocele. They may contain herniated meninges and brain tissue (encephalocele or meningoencephalocele) or only meninges (cranial meningocele). Encephaloceles containing tissue from the brain and spinal cord are called encephalomyeloceles.
Most encephaloceles are large and significant birth defects that are diagnosed before birth. However, in extremely rare cases, some encephaloceles may be small and go unnoticed. The exact cause of encephaloceles is unknown, but most likely the disorder results from the combination of several factors (multifactorial). There is a genetic component to the condition; it often occurs in families with a history of spina bifida and anencephaly in other family members 5.
Encephaloceles defects are caused by failure of the neural tube to close completely during fetal development. The result is a groove down the midline of the upper part of the skull, or the area between the forehead and nose, or the back of the skull. When located in the back of the skull, encephaloceles are often associated with neurological problems. Encephaloceles are usually dramatic deformities diagnosed immediately after birth; but occasionally a small encephalocele in the nasal and forehead region can go undetected.
Generally, surgery is performed during infancy to place the protruding tissues back into the skull, remove the sac, and correct the associated craniofacial abnormalities. Even large protrusions can often be removed without causing major functional disability. Hydrocephalus associated with encephaloceles may require surgical treatment with a shunt. Other treatment is symptomatic and supportive.
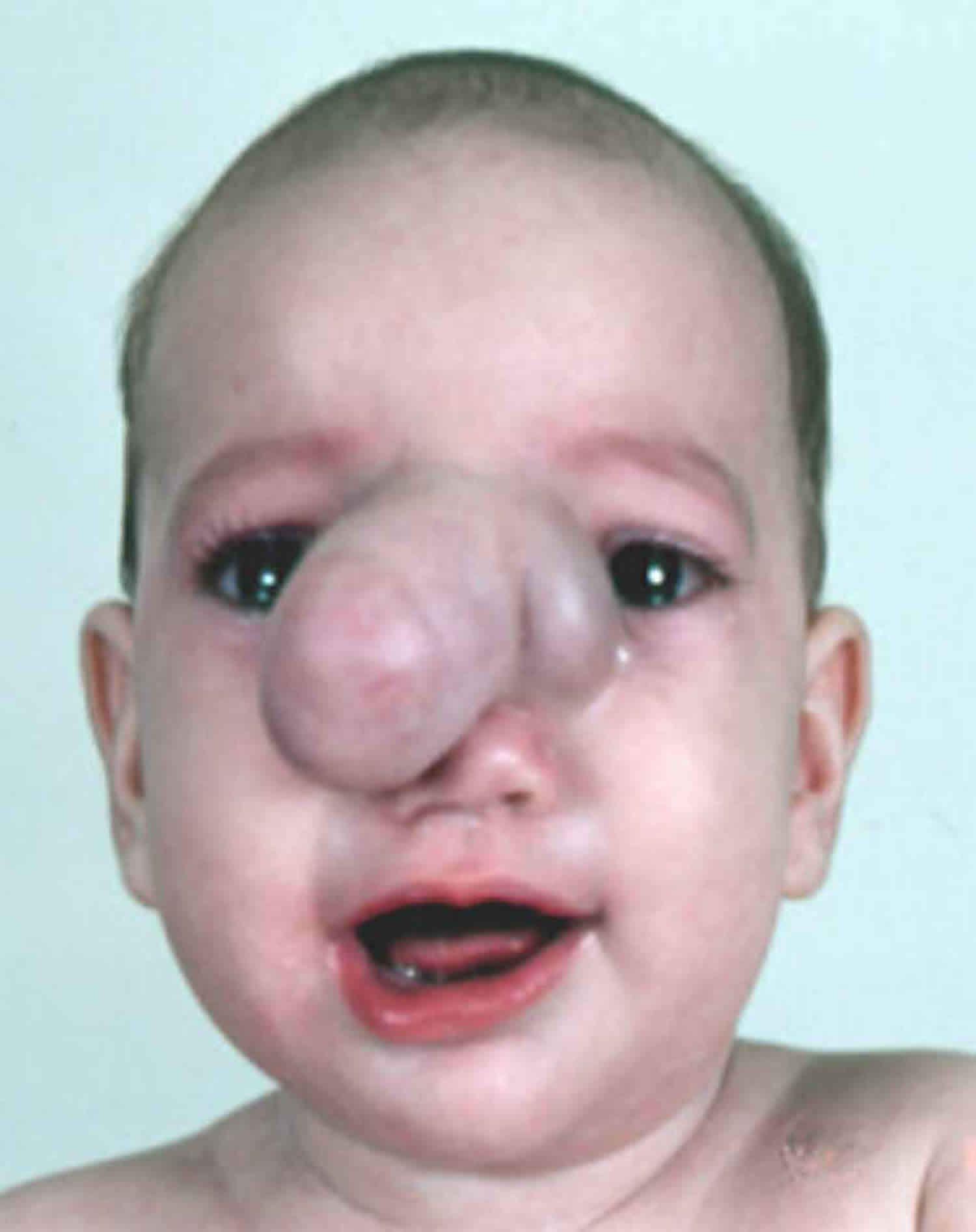
Figure 1. Frontal encephalocele
Figure 2. Occipital encephalocele (giant occipital encephalocele associated with microcephaly and micrognathia)
Footnote: 5-month-old male second child with a progressively increasing swelling at the back of head, since birth. He was delivered by caesarean section. Antenatal ultrasound picked a swelling at back of neck with no other abnormality. The child was taking feeds normally and moving all four limbs equally. Child had small jaw, receding chin with no breathing problem. Tongue was normal. His weight was 6 kg, and the head circumference was 30 cm with a bulging anterior fontanelle. There was a large occipital swelling which was tense, cystic measuring 22΄ 13 cm arising from posterior part of head. Lower part of swelling was extended up to mid-dorsal region. The child was taken up for surgery after obtaining informed consent. Before intubation, the encephalocele was aspirated slowly and about 150 ml of fluid was aspirated. The child was intubated in supine position with head supported from below by two people, over the edge of OT table. After intubation, the child was placed in prone position for surgery. To facilitate painting and draping, encephalocele was pulled with thick thread toward the roof. Excision of the encephalocele sac was done with the herniated glial tissue. Primary water tight closure of dura was done. The cranial defect was covered with spongistone (Gelfoam® ) for later cranioplasty. On third postoperative day, anterior fontanelle was tense. Non-contrast CT (NCCT) head revealed hydrocephalus, and a medium pressure ventriculo peritoneal shunt was done. Postoperative period was uneventful and the child was discharged on thirteen postoperative day. Cranioplasty for the bony defect was advised but parents refused due to personal reasons and took discharge for surgery at later date.
[Source 6 ]Encephalocele location and classification
Most of the encephaloceles are located at the posterior part of the skull (occipital encephalocele). Occipital encephaloceles have the worst prognosis and often fetus dies before pregnancy is completed.
The rest types of encephaloceles that constitute the smaller percentage have much better prognosis, they are located in the inferior part of the skull, and depending on their exact projection, they are characterized as:
- Nasofrontal when projecting between the frontal and nasal bones.
- Naso-Orbital when projecting in the orbit.
- Nasoethmoidal when projecting below the nasal bones (between nasal bones and nasal cartilages).
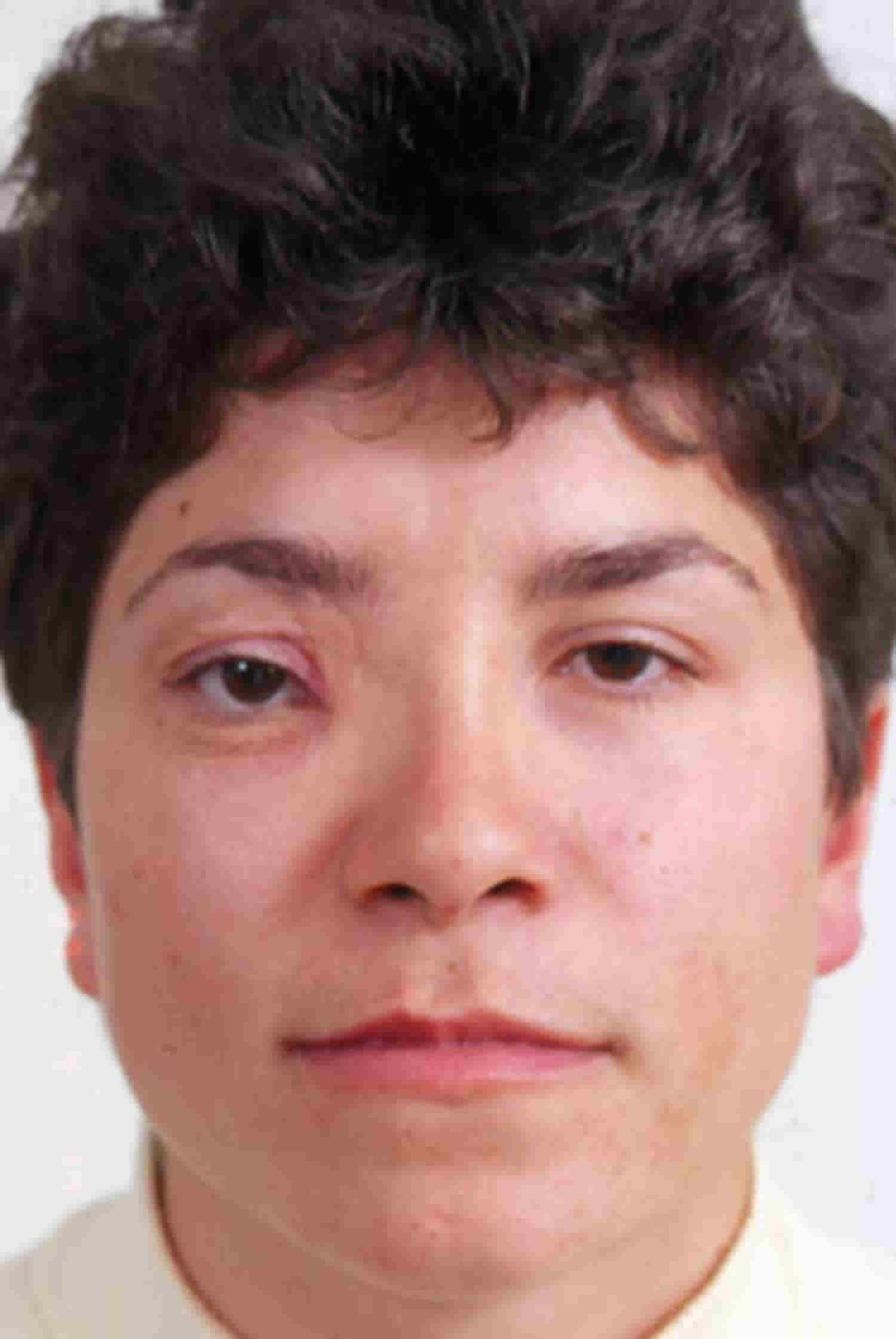
Figure 3. Nasofrontal encephalocele in adult
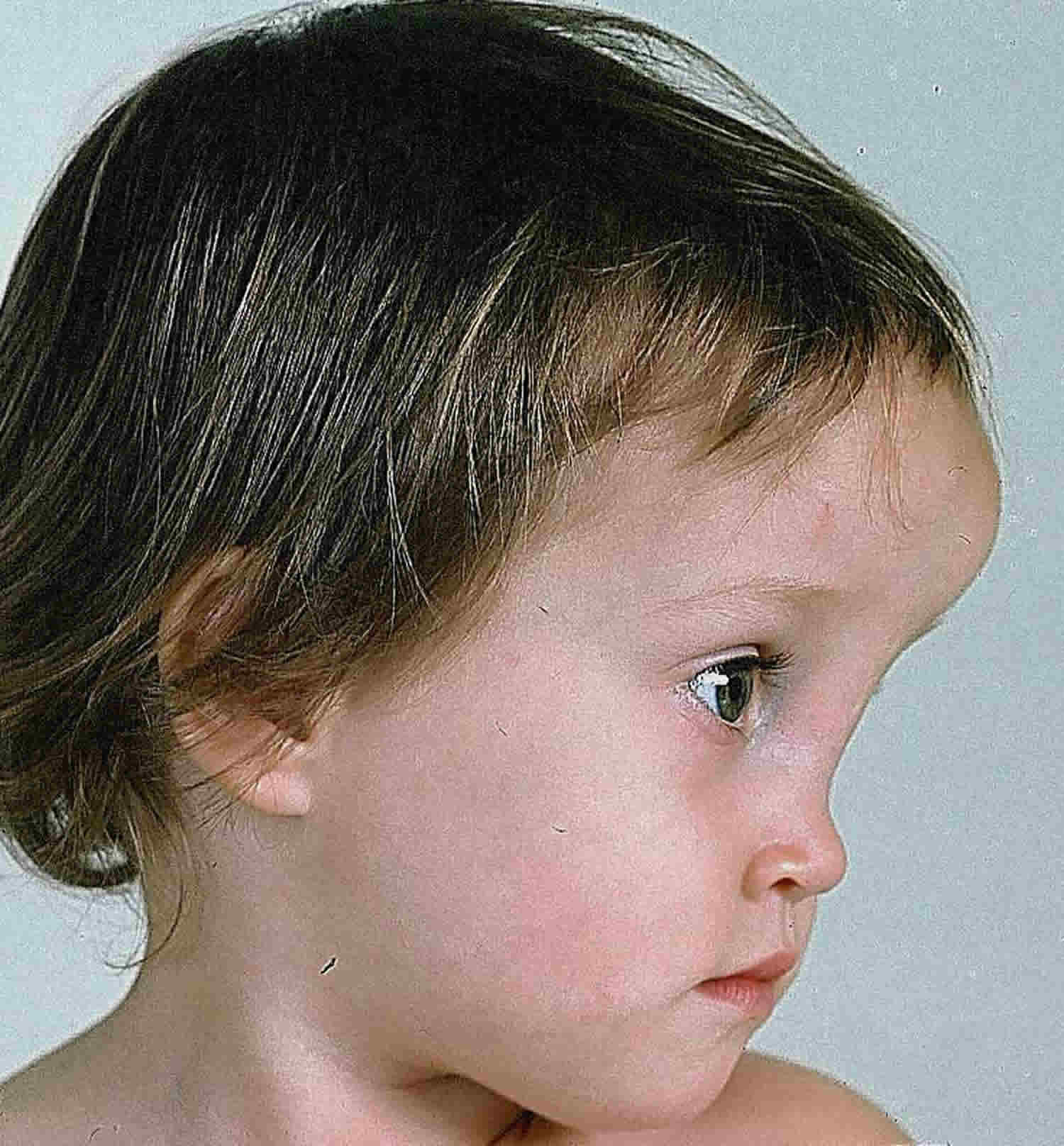
Figure 4. Naso-orbital encephalocele
Figure 5. Nasoethmoidal encephalocele
Encephalocele causes
The exact underlying cause of an encephalocele is unknown. Most cases occur sporadically. Most researchers believe that multiple factors are required for the development of an encephalocele including both genetic and environmental factors.
Encephaloceles are more common in individuals who have a family history of neural tube defects such as spina bifida or anencephaly. In such cases, individuals might have a genetic predisposition to developing a neural tube defect and may develop an encephalocele. A person who is genetically predisposed to certain disorders may carry a gene (or genes) for the disease, which may not necessarily be expressed unless it is triggered or “activated” under certain circumstances, such as the exposure to particular environmental factors.
No specific environmental factors have been confirmed as contributing to the development of an encephalocele. Researchers speculate that certain toxins or infections may be involved.
An encephalocele may occur as part of more than 30 different syndromes, including Meckel syndrome, Fraser syndrome, Roberts syndrome, and Walker-Warburg syndrome. Amniotic band syndrome can also be associated with an encephalocele.
Encephalocele symptoms
The symptoms of an encephalocele can vary from one individual to another depending upon many different factors including size, location and the amount and kind of brain tissue protruding from the skull. Encephaloceles are congenital malformations i.e. present at birth. The location of the encephaloceles is very important since there are distinct clinical implications for treatment and prognosis for anterior and posterior encephaloceles. Posterior encephaloceles are more often associated with neurological problems. Encephaloceles toward the front of the skull usually do not contain brain tissue and generally have a better prognosis.
Most registries and epidemiological studies classify encephaloceles using broad categories like frontal, parietal, occipital and sphenoidal.
The most common area of skull for the development of an encephalocele is the upper portion from the forehead to the lower back of the skull in the area of the occipital bone. Encephaloceles can also occur near the sinuses, forehead and nose or near the base of the skull.
Symptoms that can develop include delays in reaching developmental milestones, intellectual disability, learning disabilities, growth delays, seizures, vision impairment, uncoordinated voluntary movements (ataxia), and hydrocephalus, a condition in which excess cerebrospinal fluid in the skull causes pressure on the brain. Hydrocephalus can result in a variety of symptoms. Some affected individuals develop microcephaly, a condition that indicates that head circumference is smaller than would be expected for an infant’s age and sex. Also in some cases, affected individuals experience progressive weakness and loss of strength in the arms and legs due to increased muscle tone and stiffness (spastic paraplegia). However it is important to note that not all affected individuals may have the symptoms discussed above and some children may have normal intelligence, while others experience intellectual disability. Parents should talk to their child’s physician and medical team about their specific case, associated symptoms and overall prognosis.
In some cases, encephaloceles occur in association with other neurological conditions such as Dandy-Walker malformation or Chiari malformation. Dandy-Walker malformation is a brain malformation with partial or complete absence of the cerebellar vermis and enlargement of the fourth ventricle. Chiari malformation of the brain is characterized by a downward displacement of the cerebellar tonsils through the opening at the base of the skull (foramen magnum) which may result in the obstruction of cerebrospinal fluid (CSF) circulation leading sometime to a non-communicating hydrocephalus. (For more information on these disorders, choose the specific disorder name as your search term in the Rare Disease Database.)
Encephalocele prognosis
The prognosis for individuals with encephaloceles varies depending on the type of brain tissue involved, the location of the sacs, and the size of encephalocele as well as the brain malformations that may be coexist. In many cases, the brain tissue that projecting is not functional and therefore it can be removed without any problems.
According to data from the Metropolitan Atlanta Congenital Defects Program 7, the majority of deaths of children with encephalocele occurred during the first day of life and the estimated survival probability to 20 years of age was 67.3%, In addition, factors associated with increased mortality were low birth weight, presence of multiple defects instead of single defect, and Black or African American ancestry.
Encephalocele diagnosis
Most encephaloceles are diagnosed on a routine prenatal ultrasound or seen right away when a baby is born. In some cases, small encephaloceles may initially go unnoticed. These encephaloceles are usually located near the baby’s nose or forehead.
Clinical testing and work-up
An ultrasound exam is a routine examination in which reflected sound waves are used to create an image of the developing fetus. An encephalocele may appear as a cyst on an ultrasound examination. If an encephalocele is diagnosed prenatally, further tests may be recommended to detect whether additional anomalies are present. Such tests can include a prenatal magnetic resonance imaging (fetal MRI).
Encephalocele treatment
Surgical intervention is usually necessary for children with an encephalocele. The surgical intervention is usually performed during the neonatal or infancy period. Some factors such as if the encephalocele is covered by skin or not as well as the general condition of the newborn play a decisive role for the exact time of the surgery. Surgery is usually performed sometime between birth and 4 months of age depending upon the size, location and associated complications as well as whether a layer of skin covers the encephalocele. If a layer of skin is present and acts as a protective cover, surgery can be delayed for a few months. If no layer of skin protects an encephalocele, surgery might be recommended shortly after birth.
Surgery is done to put the protruding part of the brain that is outside the skull back into place and close the opening. The encephaloceles concerning the posterior part of the skull fall exclusively in the specialty of Neurosurgery, while the anterior encephaloceles require the combination of Neurosurgical and Craniofacial techniques.
Encephalocele repair
The basic principle of encephalocele repair is the excision of the area (part) that is projected and the definitive closure of the deficit, after a detailed assessment of the possible consequences of the excision. The repair of craniofacial deformity that accompanies each case, it may be performed during the initial surgery or if this is not possible, at a second time.
The neurosurgeon will cut and remove a portion of the skull (craniotomy), allowing access to the brain. Then, a neurosurgeon will cut through the dura mater, the tough outer covering of the brain.
Next, the neurosurgeon will relocate any herniated portion of the brain, meninges and fluid back into the skull and will remove the surrounding sac. Afterward, the dura mater is closed and the skull is repaired either by replacing the piece of the skull that was initially removed or using an artificial replacement. Surgical correction of an encephalocele can be achieved without causing any further functional disability, even in cases of large encephaloceles.
Additional treatment is based on the specific symptoms present in each individual case. Craniofacial abnormalities or additional abnormalities of the skull are treated surgically. Hydrocephalus may be treated by surgically implanting a shunt that allows excess cerebrospinal fluid to be drained.
Services that may be beneficial to the patient may include special remedial education, and other medical, social, and/or vocational services. Genetic counseling may be of benefit for affected individuals and their families. Other treatment is symptomatic and supportive.
Studies have shown that adding folic acid (a form of B vitamin) to the diet of women who might become pregnant can lower the risk of some neural tube defects. The CDC and other health agencies have advocated that women of childbearing age should have 400 micrograms of folic acid daily.
- Mahapatra AK, Aqrawal D. Anterior Encephaloceles: a series of 103 cases over 32 years. J Clin Neurosci. 2006;13:536–9.[↩]
- Rad IA, Farrokh-Islamlou HR, Khoshkalam M. Neural tube defects prevalence in a hospital-based study in Urmia. Iranian Journal of Child Neurology. 2008 Oct 18;2(3):19-23.[↩]
- Barrow N, Simpson DA. Cranium bifidum:Investigation, prognosis and management. AustPaediat J. 1966;2:20-26.[↩]
- Ramachandra CR, Phelps PD. Nasal encephalocoeles associated with unilateral absence of the cochlea. The Journal of Laryngology & Otology. 1977 Sep 1;91(09):813-7.[↩]
- Encephaloceles Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephaloceles-Information-Page[↩]
- Singh H, Singh D, Sharma D P, Tandon MS, Ganjoo P. Perioperative challenges in patients with giant occipital encephalocele with microcephaly and micrognathia. J Neurosci Rural Pract 2012;3:68-70 http://www.ruralneuropractice.com/text.asp?2012/3/1/68/91949[↩]
- Siffel C, Wong LY, Olney RS, Correa A. Survival of infants diagnosed with encephalocele in Atlanta, 1979-1998. Paediatr Perinat Epidemiol. 2003;17:40-48. http://www.ncbi.nlm.nih.gov/pubmed/12562471[↩]