Contents
What is eosinophils
Eosinophils are granulocytic leukocytes (white blood cell) with granules that are stained by the dye, eosin. Eosinophils, normally account for less than 7% of the circulating white blood cells (100 to 500 eosinophils per microliter of blood). Eosinophils are believed to function in allergic responses, asthma, infection with parasites and in resisting some infections. Eosinophils have a role in the protective immunity against certain parasites and respond to infections caused by parasites. Eosinophils also contribute to the inflammation that occurs in allergic disorders (hypersensitivities), and control the extent of immune responses and inflammation.
Eosinophils normal range
- Normal eosinophil count is less than 500 cells per microliter (cells/mcL).
- Normal value ranges may vary slightly among different laboratories. Talk to your provider about the meaning of your specific test results. Some laboratories use different measurements or may test different specimens.
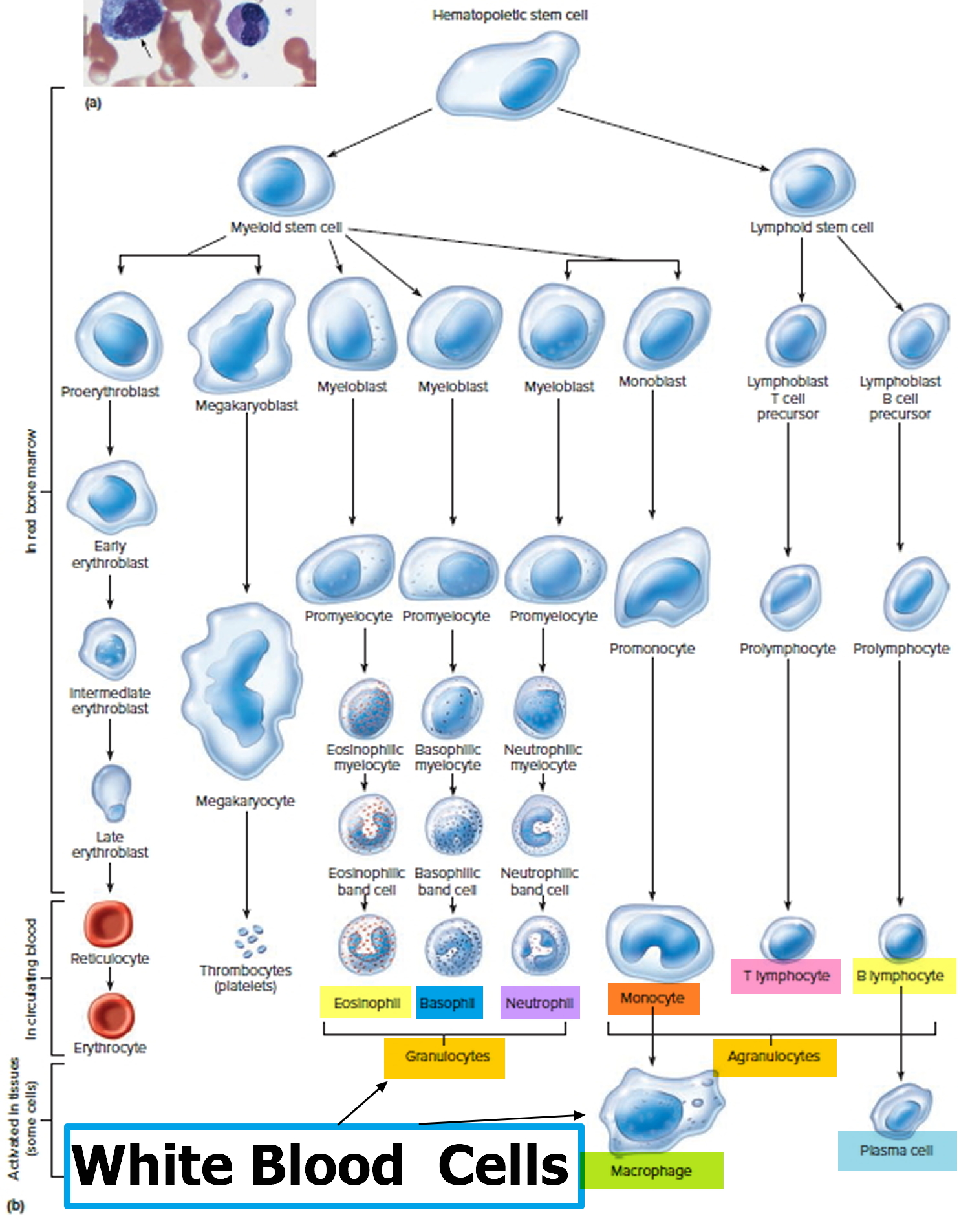
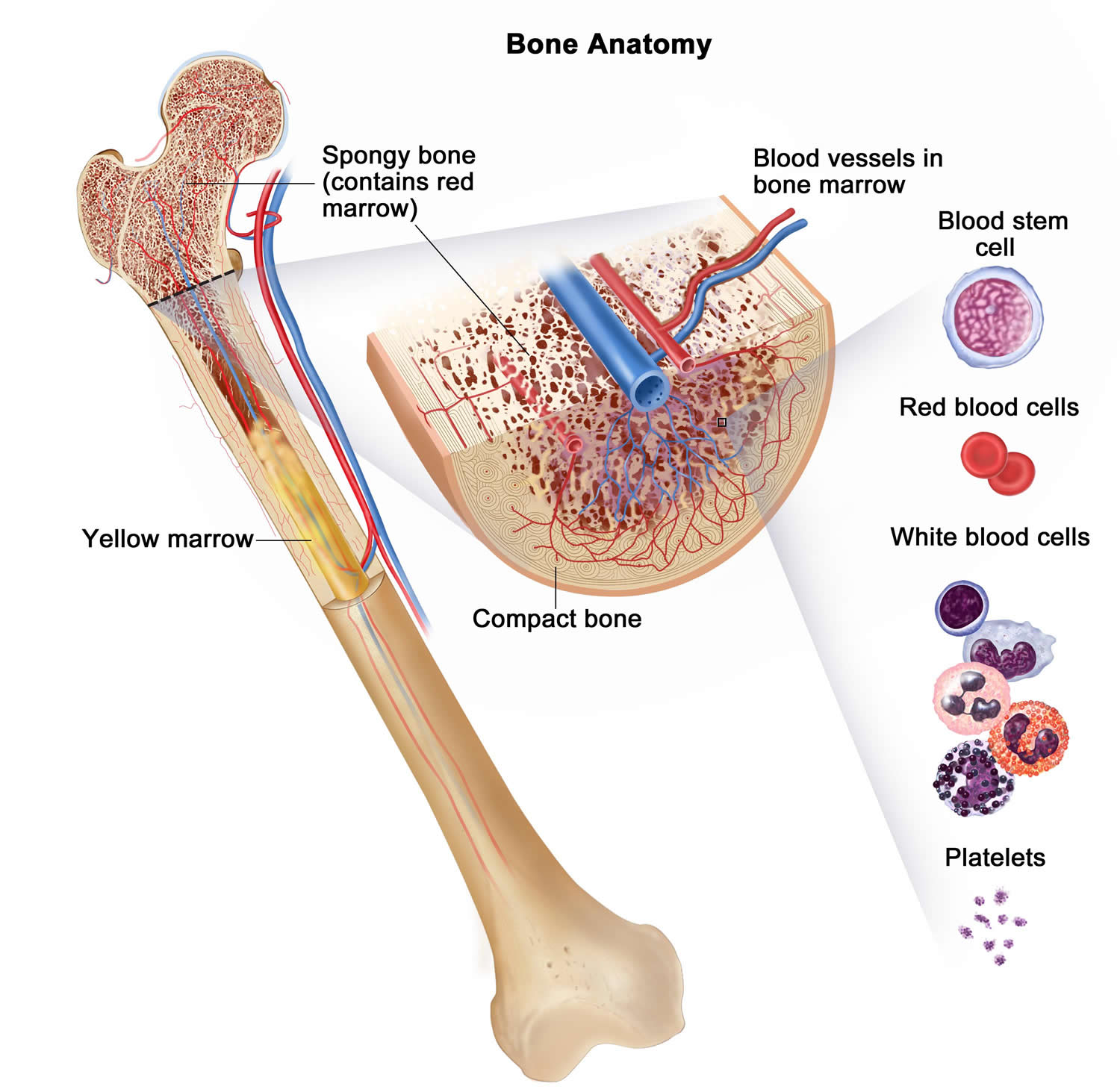
Eosinophils are granulocytes that develop in the bone marrow in response to IL-5 (interlukin-5), with a minor role for IL-3, granulocyte-macrophage colony-stimulating factor (GM-CSF), and IL-33 1. IL-5 (interlukin-5) also mediates the release of mature eosinophils into the bloodstream from where they migrate into tissues 2. In healthy individuals, eosinophils are found in the bone marrow, blood, spleen, thymus, gastrointestinal tract, and uterus 3. Under pathological conditions, eosinophils can infiltrate other tissues as well. Eosinophils are usually measured in the blood because tissue eosinophils are hard to measure 4. Eosinophil counts over 450–500 cells/microliter blood are considered mild eosinophilia and counts over 1,500 cells/microliter are characterized as hypereosinophilia 5.
The main chemotaxins for eosinophils are eotaxins, which homeostatically recruit eosinophils to the gastrointestinal tract, thymus, and uterus 6 and to other organs in disease states 7. Humans express three functional eotaxins (CCL11, CCL24, and CCL26 or CC-chemokine ligand) 8. The eotaxin receptor, CCR3, is highly expressed on eosinophils and to a low level on human basophils, mast cells, and Th2 cells 9. Other eosinophil chemoattractants include CCL5 and lipid mediators such as leukotriene B4 and prostaglandin D2, although these factors are not specific for eosinophils 10.
Figure 1. White blood cells development
Figure 2. Bone marrow anatomy
Eosinophils are implicated in numerous aspects of immunity and disease, however, the precise functions of eosinophils, remain enigmatic 11.
Sometimes, eosinophils cause inflammation in certain organs and result in symptoms.
Your body may produce more eosinophils in response to:
- Allergic disorders
- Skin conditions
- Parasitic and fungal infections
- Autoimmune diseases
- Some cancers
- Bone marrow disorders
You can have high levels of eosinophils (>500 cells per microliter or > 500 cells/mcL) in your blood (blood eosinophilia) or in tissues at the site of an infection or inflammation (tissue eosinophilia).
- Tissue eosinophilia may be found in samples taken during an exploratory procedure or in samples of certain fluids, such as mucus released from nasal tissues. If you have tissue eosinophilia, the level of eosinophils in your bloodstream is likely normal.
- Blood eosinophilia may be detected with a blood test, usually as part of a complete blood count. A count of more than 500 eosinophils per microliter of blood is generally considered eosinophilia in adults. A count of more than 1,500 eosinophils per microliter of blood that lasts for several months is called hypereosinophilia.
In some conditions, the eosinophils can move outside the bloodstream and build up in organs and tissues. This can happen in many different parts of the body, including the esophagus, heart, lungs, blood, and intestines. Treatment of eosinophilic disorders can vary, depending on the cause and which part of the body is affected. Steroids are often part of the treatment.
Elevated eosinophils (eosinophilia) occurs when a large number of eosinophils are recruited to a specific site in your body or when the bone marrow produces too many eosinophils.
High eosinophils count can be caused by a variety of factors, including:
- Parasitic and fungal diseases
- Allergies including allergies to medications or food
- Adrenal conditions
- Skin disorders
- Toxins
- Autoimmune disorders
- Endocrine disorders
- Tumors
Specific diseases and conditions that can result in blood or tissue eosinophilia include:
- Acute myelogenous leukemia (AML)
- Ascariasis (a roundworm infection)
- Asthma
- Atopic dermatitis (eczema)
- Cancer
- Churg-Strauss syndrome
- Crohn’s disease
- Drug allergy
- Eosinophilic esophagitis
- Eosinophilic leukemia
- Hay fever (allergic rhinitis)
- Hodgkin’s lymphoma (Hodgkin’s disease)
- Hypereosinophilic syndrome
- Idiopathic hypereosinophilic syndrome (HES), an extremely high eosinophil count of unknown origin
- Lymphatic filariasis (a parasitic infection)
- Ovarian cancer
- Parasitic infection
- Primary immunodeficiency
- Trichinosis (a roundworm infection)
- Ulcerative colitis (a type of inflammatory bowel disease)
Parasitic diseases and allergic reactions to medication are among the more common causes of eosinophilia. Hypereosinophila that causes organ damage is called hypereosinophilic syndrome. This syndrome tends to have an unknown cause or results from certain types of cancer, such as bone marrow or lymph node cancer.
Eosinophilia is usually found when your doctor has ordered blood tests to help diagnose a condition you’re already experiencing. It’s usually not an unexpected finding, but it’s possible that it may be discovered simply by chance.
Talk to your doctor about what these results mean. Evidence of blood or tissue eosinophilia and results from other tests may indicate the cause of your illness. Your doctor may suggest other tests to check your condition.
It’s important to determine what other conditions or disorders you may have. If you get an accurate diagnosis and can receive treatment for any relevant conditions or disorders, the eosinophilia will likely resolve.
If you have hypereosinophilic syndrome, your doctor may prescribe medications, such as corticosteroids. And he or she will want to monitor your health, as this condition may cause significant complications over time.
Eosinophils function
Eosinophils are multifunctional granulocytes that contribute to initiation and modulation of inflammation. Their role in asthma and parasitic infections has long been recognized. Growing evidence now reveals a role for eosinophils in autoimmune diseases. Eosinophils are extremely versatile effector cells that damage tissues or modulate the activity of other immune and stromal cells.
Possible eosinophil effector functions in autoimmune diseases:
- Damage of tissues by cytotoxic granule proteins
- Antibody-dependent cellular cytotoxicity
- Activation of tissue remodeling and fibrosis
- Antigen presentation
- Modulation of the adaptive immune response
- Promotion of B cell responses
- Induction of tissue repair processes.
Eosinophils play two roles in your immune system:
- Destroying foreign substances. Eosinophils can consume foreign substances. For example, they fight substances related to parasitic infection that have been flagged for destruction by your immune system.
- Regulating inflammation. Eosinophils help promote inflammation, which plays a beneficial role in isolating and controlling a disease site. But sometimes inflammation may be greater than is necessary, which can lead to troublesome symptoms or even tissue damage. For example, eosinophils play a key role in the symptoms of asthma and allergies, such as hay fever. Other immune system disorders also can contribute to ongoing (chronic) inflammation.
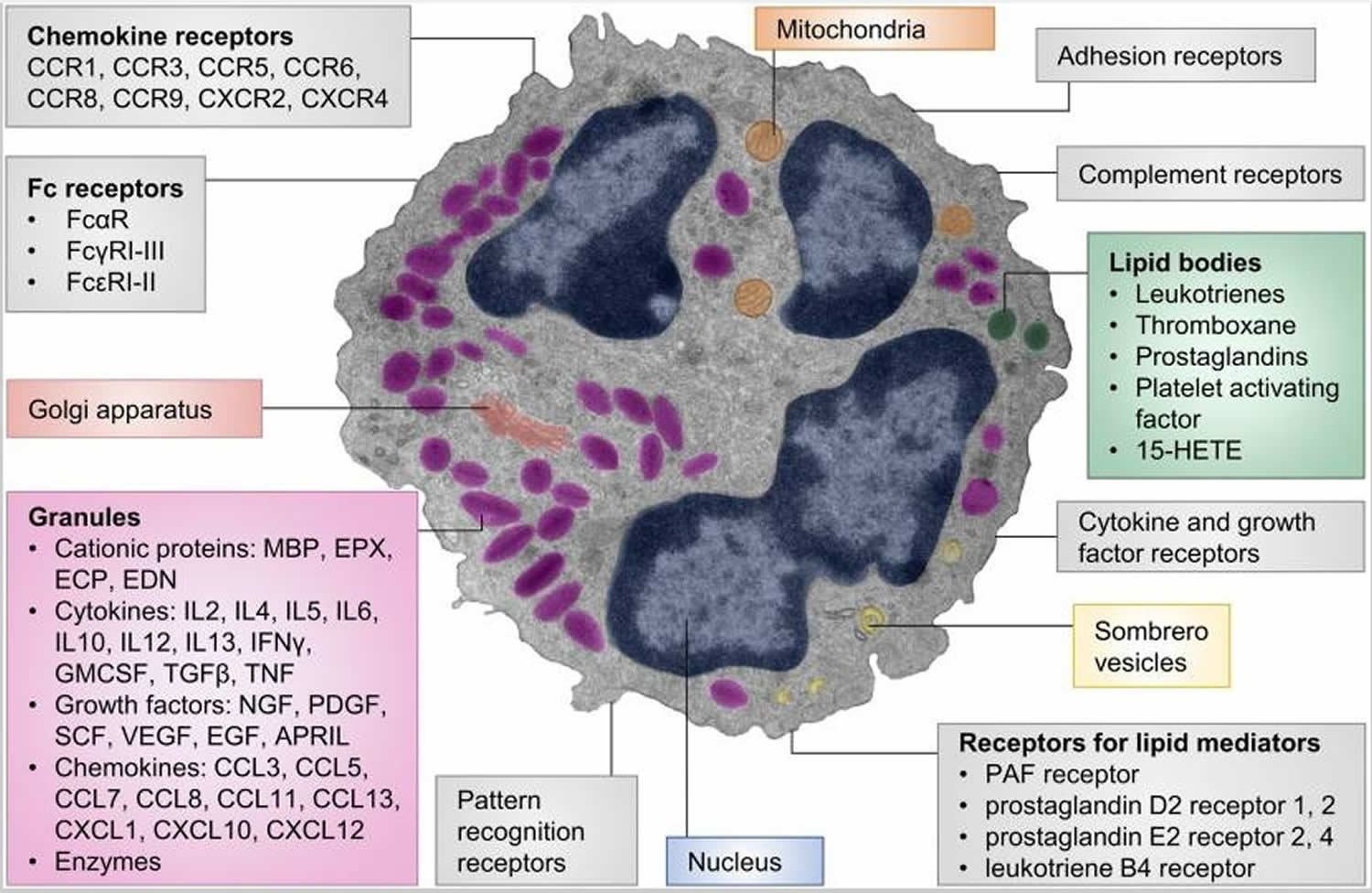
A unique characteristic of eosinophils are their specific (also termed secondary or secretory) granules. These are secretory vesicles with an electron-dense core and an electron-lucent matrix. Eosinophil granules contain four major granule proteins and numerous cytokines, chemokines, and growth factors 12 (Figure 3). Cytotoxic effects to host tissues and pathogens have been demonstrated for all major granule proteins: eosinophil cationic protein (ECP), eosinophil-derived neurotoxin (EDN), eosinophil peroxidase (EPX), and major basic protein (MBP) 13. MBP can disrupt the cell membrane and is therefore highly cytotoxic to mammalian cells, helminths, and bacteria 14. Other effects of major basic protein include altering smooth muscle contraction, inducing mast cell and basophil degranulation, provoking acetylcholine release from peripheral nerves, and promoting nerve cell survival 15. The granule proteins ECP and EDN are ribonucleases 16 with neurotoxic and strong antiviral activities 17 and immune modulatory functions 18. Eosinophil peroxidase (EPX) generates reactive oxygen species that are directed extracellularly 19. These products have cytotoxic, prothrombotic, and pro-inflammatory effects 20. Granule contents are generally preformed in eosinophils and released upon stimulation. Piecemeal degranulation is the most common process by which eosinophils release their granule contents 21. Specific granule factors, rather than the entire granule, are released in response to an activating signal. This leaves the eosinophil intact and able to respond to subsequent stimulation.
Figure 3. Eosinophils function
Footnotes: Cellular structure, receptors, and mediators of eosinophils. The pseudocolored composite electron micrograph of an eosinophil highlights cellular structures. Characteristic features of eosinophils include the multilobed nucleus, specific eosinophil granules, lipid bodies, and sombrero vesicles. Eosinophil granules contain cationic proteins, cytokines, growth factors, chemokines, and enzymes. The granule contents can be released upon stimulation. Lipid bodies are the place of synthesis for numerous lipid mediators. Granule contents can be released through sombrero vesicles. Eosinophils carry numerous cell surface receptors including chemokine receptors, Fc receptors, pattern recognition receptors, receptors for lipid mediators, cytokine receptors, complement receptors, and adhesion receptors.
Abbreviations: 15-HETE = 15-hydroxyeicosatetraenoic acid; APRIL = a proliferation-inducing ligand; CCL = CC-chemokine ligand; CCR= CC-chemokine receptor; CXCL = CXC-chemokine ligand; CXCR = CXC-chemokine receptor; ECP = eosinophil cationic protein; EDN = eosinophil-derived neurotoxin; EGF = epidermal growth factor; EPX = eosinophil peroxidase; GMCSF = granulocyte-macrophage colony-stimulating factor; IFN = interferon; MBP = major basic protein; NGF = nerve growth factor; PDGF = platelet-derived growth factor; PAF = platelet-activating factor; SCF = stem cell factor; TGF = transforming growth factor; TNF = tumor necrosis factor; VEGF = vascular endothelial growth factor.
[Source 22]The ability of eosinophils to bind antibodies and consequently degranulate and kill cells links the adaptive autoimmune response to eosinophil effector functions. Eosinophils express complement receptors 23 and Fc receptors (FcαR, FcγRI–III, and FcεRI–II) either constitutively or under inflammatory conditions 24. As a result, they are capable of antibody-dependent cellular cytotoxicity (ADCC) to parasites and mammalian targets 25. In autoimmune diseases, eosinophils may kill host cells bound by autoantibodies.
Eosinophils also interact with stromal cells. Actively degranulating eosinophils are frequently found in areas of fibrogenesis, suggesting a potential profibrotic role 26. Granule proteins and eosinophil-derived transforming growth factor (TGF)β1 were demonstrated to affect tissue remodeling and fibrosis. Eosinophils can promote fibroblast proliferation 27, proteoglycan accumulation 28, matrix metalloproteinase and TGFβ expression, and extracellular matrix protein synthesis 29. These profibrotic functions of eosinophils may add to tissue dysfunction in autoimmune diseases. In chronic inflammatory conditions, eosinophils preferentially locate to nerves 30. This interaction results in activation of eosinophils 31, nerve damage 32, altered nerve growth 33, and neuropeptide release 34. Contact between eosinophils and nerves has functional consequences. For example, it is one of the causes of airway hypersensitivity in asthma 35.
Eosinophils can form extracellular DNA traps by quickly releasing mitochondrial DNA and granule proteins 36. These structures bind and kill pathogens and contribute to tissue injury in inflammatory conditions 37. DNA extracellular traps have been described in allergic asthma 38, drug hypersensitivity reactions, and allergic contact dermatitis 39. Eosinophils may initiate or perpetuate inflammation by releasing cytokines and chemokines and by interacting with other innate immune cells. For example, eosinophils release MBP, IL-9, stem cell factor, or nerve growth factor, which affect mast cell maturation, survival, and histamine release 40.
Eosinophils can also influence the adaptive immune response. They are capable antigen-presenting cells that upregulate MHCII and costimulatory molecules in the context of parasitic infection or allergic asthma 41. Moreover, eosinophils migrate to draining lymph nodes 42, and in vitro experiments have demonstrated their ability to present antigen to and activate T cells 43. Eosinophils may contribute to the initiation of autoimmune responses by presenting antigen to and activating T cells.
Eosinophil granules contain numerous cytokines such as IL-4, IL-13, IL-25, TGFβ, IL-10, or IDO 12, which suggests an ability to affect T cell differentiation. Eosinophils were shown to suppress Th1/Th17 differentiation 44 or activate Th2 responses in draining lymph nodes 45. In addition, they modulate dendritic cell activity, thereby indirectly affecting polarization of naïve T cells into Th2 cells 46. Eosinophils also shape the humoral immune response. In the bone marrow, eosinophils stimulate plasma cell survival by producing IL-6 and a proliferation-inducing ligand 47, and in the intestine, they promote class-switching to IgA 48. These properties enable eosinophils to shape the adaptive immune response in autoimmune diseases.
Eosinophils may also fulfill immune regulatory and protective functions. Eosinophil-derived mediators like TGFβ and TGFα 49, platelet-derived growth factor 50, vascular endothelial growth factor 51, and fibroblast growth factor 52 can all contribute to tissue repair and angiogenesis. IL-4 released from eosinophils was shown to play a role in liver 53 and muscle 54 regeneration. Whether eosinophils contribute to tissue repair or tissue damage is likely context and disease dependent.
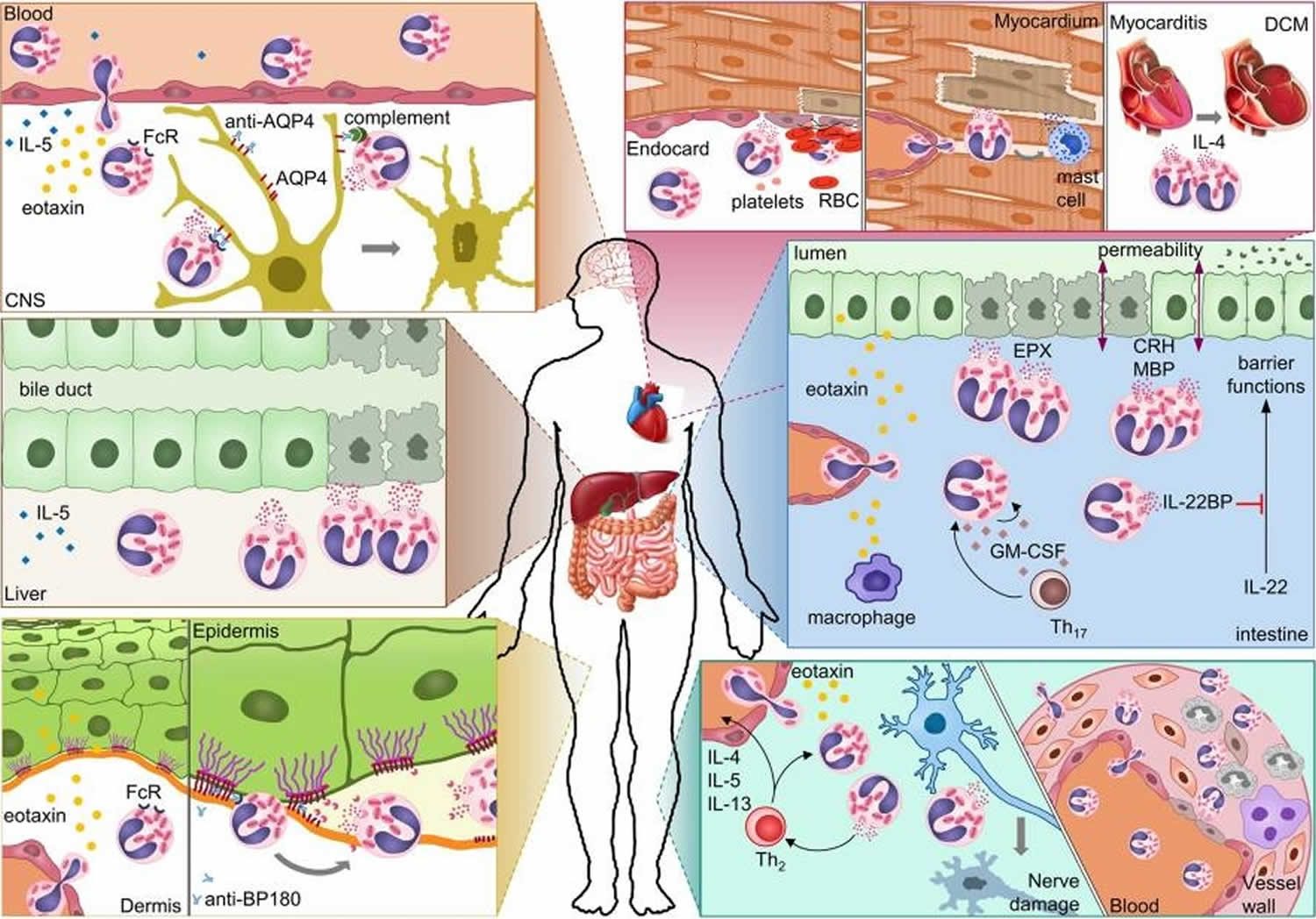
Figure 4. Eosinophil-mediated damage in autoimmune diseases
Footnotes: Possible mechanisms of eosinophil-mediated damage in different autoimmune diseases. In neuromyelitis optica, eosinophils damage astrocytes through antibody-dependent and complement-dependent cell-mediated cytotoxicity. Eosinophil degranulation in damaged bile ducts was shown for primary biliary cirrhosis. In bullous pemphigoid, eosinophils release proteases that degrade the dermal–epidermal anchoring complex. Eosinophil infiltration in the heart results in damage to the endocardium and myocardium either directly or indirectly through mast cells. Eosinophil-derived IL-4 can drive progression from autoimmune myocarditis to DCM. In inflammatory bowel diseases, eosinophils can damage the mucosa through multiple mechanisms. Eosinophil granule proteins damage epithelial cells and increase epithelial barrier permeability. Eosinophil-derived IL-22BP blocks the protective effects of IL-22 on epithelial cells. GM-CSF may prolong survival and activation of eosinophils in the intestine. In eosinophilic granulomatosis with polyangiitis, eosinophils damage nerves and blood vessels.
Abbreviations: CNS = central nervous system; AQP4 = aquaporin 4; FcR = Fc receptor; BP180 = bullous pemphigoid 180; RBC = red blood cell; DCM = dilated cardiomyopathy; EPX = eosinophil peroxidase; CRH = corticotropin-releasing hormone; MBP = major basic protein; IL-22BP = IL-22-binding protein; GM-CSF = granulocyte-macrophage colony-stimulating factor; Th17 = T-helper 17 cell; Th2 = T-helper 2 cell.
[Source 22]Following activation, eosinophils effector functions include production of:
- cationic granule proteins and their release by degranulation 55.
- reactive oxygen species such as hypobromite, superoxide, and peroxide (hypobromous acid, which is preferentially produced by eosinophil peroxidase) 56.
- lipid mediators like the eicosanoids from the leukotriene (e.g., LTC4, LTD4, LTE4) and prostaglandin (e.g., PGE2) families 57.
- enzymes, such as elastase.
- growth factors such as TGF beta, VEGF, and PDGF 58.
- cytokines such as IL-1, IL-2, IL-4, IL-5, IL-6, IL-8, IL-13, and TNF alpha 59.
There are also eosinophils that play a role in fighting viral infections, which is evident from the abundance of RNases they contain within their granules, and in fibrin removal during inflammation. Eosinophils, along with basophils and mast cells, are important mediators of allergic responses and asthma pathogenesis and are associated with disease severity. They also fight helminth (worm) colonization and may be slightly elevated in the presence of certain parasites.
Eosinophils are also involved in many other biological processes, including postpubertal mammary gland development, oestrus cycling, allograft rejection and neoplasia 60. Eosinophils have also been implicated in antigen presentation to T cells 61.
Eosinophils are responsible for tissue damage and inflammation in many diseases, including asthma 62. High levels of interleukin-5 has been observed to up regulate the expression of adhesion molecules, which then facilitate the adhesion of eosinophils to endothelial cells, thereby causing inflammation and tissue damage 63.
An accumulation of eosinophils in the nasal mucosa is considered a major diagnostic criterion for allergic rhinitis (nasal allergies).
Eosinophils high
Eosinophilia is a higher than normal level of eosinophils (>500 cells per microliter or > 500 cells/mcL). Eosinophils are a type of disease-fighting white blood cell. Elevated eosinophils condition most often indicates a parasitic infection, an allergic reaction or cancer.
The most common causes of a high number of eosinophils (called eosinophilia or hypereosinophilia) are:
- Allergic disorders
- Infections by parasites
- Certain cancers
Allergic disorders, including asthma, allergic rhinitis, and atopic dermatitis, often increase the number of eosinophils. Many parasites, particularly ones that invade tissue, cause eosinophilia. Cancers that cause eosinophilia include Hodgkin lymphoma, leukemia, and certain myeloproliferative disorders.
If the number of eosinophils is only slightly elevated, people usually do not have symptoms, and the high number of eosinophils in the blood is only discovered when a complete blood count is done for other reasons. However, sometimes, particularly when the number of eosinophils is very high, the increased number of eosinophils inflame tissues and cause organ damage. The heart, lungs, skin, and nervous system are most often affected, but any organ can be damaged.
Symptoms are related to the organ affected. For example, people may have a rash when the skin is affected, wheezing and shortness of breath when the lungs are affected, shortness of breath and fatigue (symptoms of heart failure) when the heart is affected, or throat and stomach pain when the esophagus or stomach is affected. Accordingly, eosinophilic disorders are diagnosed according to the location where the levels of eosinophils are elevated:
- Eosinophilic pneumonia (lungs)
- Eosinophilic cardiomyopathy (heart)
- Eosinophilic esophagitis (esophagus)
- Eosinophilic gastritis (stomach)
- Eosinophilic enteritis (small intestine)
- Eosinophilic colitis (large intestine)
Often, people are first tested and treated for more common causes of their symptoms. For example, they might undergo testing for infection and even receive antibiotics even though no infection is found. Because people still have symptoms after treatment, doctors often take a sample of tissue for examination (biopsy), which will show eosinophils within the organ that is affected.
Treatment of these conditions frequently includes oral corticosteroids.
Hypereosinophilic syndrome
Hypereosinophilic Syndromes are a group of rare disorders in which high numbers of eosinophils are found in the blood (more than 1,500 cells per microliter of blood) and tissue, for prolonged period of time (6 months or more) for which a cause cannot be found. While most people have blood eosinophil levels of less than 500/ml, those with hypereosinophilic syndromes typically have blood levels of more than 1,500/ml.
Continuous presence of high number of eosinophils in blood can eventually cause multiple organ tissue damage as these eosinophils infiltrate different tissues and cause inflammation. Hypereosinophilic syndromes can affect any organ in the body, including the stomach and intestines, the heart, lungs, skin and other organs. Some people have a rare chromosome disorder.
People of any age can develop hypereosinophilic syndrome, but it is more common in men older than 50. The increased number of eosinophils can damage the heart, lungs, liver, skin, and nervous system. For example, the heart can become inflamed in a condition called Löffler endocarditis, leading to formation of blood clots, heart failure, heart attacks, or malfunctioning heart valves.
Symptoms may include weight loss, fevers, night sweats, fatigue, cough, chest pain, swelling, stomachache, rash, pain, weakness, confusion, and coma. Additional symptoms of this syndrome depend on which organs are damaged.
The syndrome is suspected when repeated blood tests reveal that the number of eosinophils is persistently increased in people who have these symptoms. The diagnosis is confirmed when doctors determine that the eosinophilia is not caused by a parasitic infection, an allergic reaction, or another diagnosable disorder and when biopsies show eosinophils within organs.
Without treatment, generally more than 80% of the people who have this syndrome die within 2 years, but with treatment, more than 80% survive. Heart damage is the principal cause of death. Some people need no treatment other than close observation for 3 to 6 months, but most need drug treatment with prednisone, hydroxyurea, or chemotherapy drugs.
Some people with hypereosinophilic syndrome have an acquired abnormality of a gene that regulates cell growth. This type of hypereosinophilia can respond to treatment with imatinib, a drug used to treat cancer. If treatment with these drugs is not successful, various other drugs may be used, and they can be combined with a procedure to remove eosinophils from the blood (leukapheresis—plateletpheresis [platelet donation]).
Hypereosinophilic syndrome causes
The cause of Hypereosinophilic syndromes is not known.
While both men and women may be affected by Hypereosinophilic syndromes, the disease is more commonly seen in males ages 20-50. While it is more commonly diagnosed in adulthood, it has also been diagnosed in children.
Hypereosinophilic syndrome symptoms
The symptoms of Hypereosinophilic syndromes may vary widely, depending on the part of the body that is affected. Symptoms may include cough, fever, fatigue, shortness of breath and wheezing. The symptoms of Hypereosinophilic syndromes are also common in many other medical problems, including autoimmune diseases, allergic disease, cancer, and drug reactions, making Hypereosinophilic syndromes more difficult to diagnose.
Hypereosinophilic syndrome prognosis
The prognosis in Hypereosinophilic syndromes depends on the organ systems involved, disease severity and response to therapy. Outcomes can vary greatly from one person to the next. There is no cure. If Hypereosinophilic syndromes is left untreated, the disease may be fatal. Your doctor can best answers questions about your specific prognosis in Hypereosinophilic syndromes.
Bone marrow biopsy in Hypereosinophilic Syndrome, exhibiting a markedly increased number of eosinophils. This may happen with a number of disorders, including parasitic infection.
Hypereosinophilic syndrome diagnosis
Since many different problems can cause high numbers of eosinophils in the blood, higher than normal blood eosinophil number alone does not mean an individual has, or will develop, hypereosinophilic syndromes.
Criteria has been developed that must be fulfilled for an individual to be diagnosed with hypereosinophilic syndromes.
- Peripheral blood eosinophilia (high numbers of eosinophils in the blood) more than 1500 eosinophils, for at least six months’ duration.
- End-organ (heart, lungs, GI tract, brain, skin, etc) involvement with eosinophil tissue infiltration (invasion) and injury.
- Exclusion of known other causes for the eosinophilia such as parasitic infections and certain bone marrow/blood diseases.
Tests are needed to diagnose hypereosinophilic syndromes and include a complete blood cell count, including eosinophil count, blood samples for liver and kidney function, and blood tests for Vitamin B12 and tryptase.
Depending on symptoms and test results, other studies may be performed. For instance, ultrasound (echocardiography) is used to look at the function of the heart. A chest x-ray may be done to examine the lungs. A bone marrow biopsy is recommended in patients suspected of having hypereosinophilic syndromes. It commonly reveals high number of eosinophils and some other abnormalities, suggestive of an innate bone marrow/blood disease of eosinophils. Therefore, hypereosinophilic syndromes is classified as hematologic neoplasm (disease of the blood and bone marrow) and is part of the larger group of myeloproliferative neoplasms.
Closely related disease to hypereosinophilic syndromes is chronic eosinophilic leukemia. Major difference, in simple terms, is that in chronic eosinophilic leukemia all eosinophils found in the bone marrow and blood are proven to be identical (also called “clonal”, meaning that all originate from the same, one, abnormal eosinophil).
The disease may be diagnosed and monitored by a team of specialists, such as allergist/immunologist, hematologist, and/or cardiologist.
Hypereosinophilic syndrome treatment
Treatment goals include decreasing blood eosinophil numbers, preventing organ damage, and slowing disease progression. Treatments vary based on organs involved and disease verity, as well as on the presence of other medical problems a patient may have. Therapy for hypereosinophilic syndrome requires careful discussion with your health care providers regarding the risks and benefits of the treatment for your specific hypereosinophilic syndromes- related organ involvement.
Hypereosinophilic syndromes treatment may include glucocorticosteroids (i.e., prednisone) and chemotherapy medicines such as chlorambucil, hydroxyurea, and vincristine. Frequent injections of interferon-alpha may also be prescribed.
Improved treatment options for hypereosinophilic syndromes are an area of ongoing research, including the use of tyrosine kinase inhibitors (i.e., Gleevec, Dasatinib, and Nilotinib) and anti-interleukin-5 (IL-5) monoclonal antibodies (mepolizumab and reslizumab).
Systemic steroids are often needed to treat Hypereosinophilic syndromes with organ involvement or with systemic symptoms, like a severe rash, fluid retention, and similar. Steroids are medications that fight (suppress) many types of inflammation. They are not specific for suppressing eosinophils, although eosinophils are particularly sensitive to them. Systemic steroids, those that are absorbed into the bloodstream (oral or IV), are very effective for treating a number of eosinophilic disorders. Steroids are very effective for controlling eosinophil numbers in blood and most Hypereosinophilic syndromes patients can be maintained on oral steroid medication (called prednisone) for a long period of time with good control of the disease. However, the blood eosinophils and disease symptoms generally return once steroids have been stopped. Long-term steroid use (especially when used in high doses) has, unfortunately, been associated with certain side-effects. Serious side effects can include osteoporosis (brittle bones from bone loss), infections, adrenal insufficiency (body becomes unable to properly respond to illness or stress), avascular necrosis (collapse of the bones in a joint, usually the hip), and stunted growth. Common side effects may include fluid retention (swelling), increased appetite, “moon-face”, and irritability.
Interferon alpha (IFNa) is used for a variety of diseases including infections (like hepatitis) and malignancies (like certain types of leukemia). IFNa has been shown to be effective in Hypereosinophilic syndromes by suppressing the symptoms related to the disease. Toxicity, however, is a major obstacle to the use of this therapy. IFNa is commonly injected into the fatty tissue under the skin 3-5 times a week. Upon the initiation of therapy most patients experience influenza-like symptoms such as fever, chills, muscle aches, headaches, and joint pain. Other side effects of IFNa are low blood counts and elevated liver enzymes that require careful monitoring. These side effects usually lessen over time, but other toxicities can manifest themselves in various forms after long-term therapy. Overall experience with IFNa in myeloproliferative neoplasms is that about 25-30% of patients require discontinuation of therapy due to side effects. New long-acting forms of IFNa (pegylated interferons) have been developed over the last few years and are now approved as a therapy for hepatitis. These medications are administered only once a week and may, therefore, be better tolerated.
Cyclosporine is a potent medication that suppresses the immune system and it is used primarily to prevent organ rejection in people who have had organ transplants. In some patients with hypereosinophilic syndromes there might be evidence that the immune cells have a role in supporting the diseases existence (so-called T cells) and cyclosporine may have a role as therapy in such cases.
Anti-neoplastic agents (chemotherapy) provide an alternative approach to therapy of advanced cases of hypereosinophilic syndromes. These are chemotherapeutic agents that may control the disease. They are used to treat many malignancies and are not specific for eosinophilic disorders. They are potent medications that kill cells that grow the fastest (eosinophils in Hypereosinophilic syndromes) but may potentially have harmful side effects and are reserved only for more severe cases. Careful monitoring while taking these medications is essential. Chemotherapeutic agents that have been used in hypereosinophilic syndromes include: Hydroxyurea, Methotrexate, Etoposide, Cyclophosphamide, Vincristine, and Cladribine.
Gleevec (Imatinib Mesylate) is a tyrosine kinase inhibitor. As a result of cell growth research, scientists have been able to develop a group of therapeutic agents known as tyrosine kinase inhibitors. Tyrosine kinases are enzymes in the cells with a variety of functions. By blocking the ability of tyrosine kinases to function, tyrosine kinase inhibitor provides a valuable tool for controlling malignant cell growth. Several years ago a discovery was made in some patients with hypereosinophilic syndromes of a genetic abnormality involving tyrosine kinase called PDGFRα. In these cases, it seems that PDGFRα abnormality is responsible for disease existence. Gleevec is tyrosine kinase inhibitor that inhibits PDGFRα and may eliminate the disease in Hypereosinophilic syndromes patients with PDGFRα abnormality. Genetic testing for PDGFRα abnormality is usually part of the bone marrow evaluation and can help determine if Gleevec is best first therapy. Not all patients with Hypereosinophilic syndromes will respond to Gleevec as about 10-20% of patients may have PDGFRα. In Hypereosinophilic syndromes patients without PDGFRα abnormality, Gleevec can be tried as therapy but it is unlikely to eliminate the disease; it may help control the disease signs and symptoms for a period of time.
New Therapies for Hypereosinophilic syndromes
For patients who are refractory to conventional therapies, use of monoclonal antibody therapy (medications that selectively bind to specific proteins) should be considered. Two drugs are currently available: mepolizumab that targets interleukin-5, a cytokine in blood that is recognized as a very important protein that governs eosinophil growth, and alemtuzumab that targets the CD52 protein expressed on the surface of eosinophils (its function not yet known). Mepolizumab, therefore, by blocking interleukin-5 eliminates a cytokine from blood that provides signal for eosinophil growth. Alemtuzumab, on the other hand, by binding to CD52 kills the eosinophil. Mepolizumab is not approved therapy yet and is currently available in a compassionate-use program sponsored by GlaxoSmithKline, for patients with life-threatening hypereosinophilic syndromes that is not responding to usual therapy. Alemtuzumab is currently approved by the Food and Drug Administration for use in B-cell chronic lymphocytic leukemia.
Low eosinophils
A low number of eosinophils in the blood (eosinopenia) can occur with Cushing syndrome, bloodstream infections (sepsis), and treatment with corticosteroids. However, a low number of eosinophils does not usually cause problems because other parts of the immune system compensate adequately.
A low number of eosinophils is usually detected by chance when a complete blood count is done for other reasons.
Treatment of the cause restores the normal number of eosinophils.
What is absolute eosinophils
An absolute eosinophil count is a blood test that measures the number of white blood cells called eosinophils. Eosinophils become active when you have certain allergic diseases, infections, and other medical conditions.
You will have this test to see if you have abnormal results from a blood differential test. This test may also be done if the provider thinks you may have a specific disease.
Absolute eosinophil count test may help diagnose:
- Acute hypereosinophilic syndrome (a rare, but sometimes fatal leukemia-like condition)
- An allergic reaction (can also reveal how severe the reaction is)
- Early stages of Cushing disease
- Infection by a parasite
The absolute eosinophil count is used to help confirm a diagnosis. Absolute eosinophil count test cannot tell if the higher number of eosinophils is caused by allergy or parasite infection.
How the absolute eosinophils test performed
Most of the time blood is drawn from a vein on the inside of the elbow or the back of the hand. The site is cleaned with an antiseptic. The health care provider wraps an elastic band around your upper arm to make the vein swell with blood.
Next, the provider gently inserts a needle into the vein. The blood collects into an airtight tube attached to the needle. The elastic band is removed from your arm. The needle is then removed and the site is covered to stop bleeding.
In infants or young children, a sharp tool called a lancet may be used to prick the skin. The blood collects in a small glass tube, or onto a slide or test strip. A bandage is put on the spot to stop bleeding.
In the lab, the blood is placed on a microscope slide. A stain is added to the sample. This causes eosinophils to show up as orange-red granules. The technician then counts how many eosinophils are present per 100 cells. The percentage of eosinophils is multiplied by the white blood cell count to give the absolute eosinophil count.
Most of the time, adults do not need to take special steps before this test. Tell your provider the medicines you are taking, including the ones without a prescription. Some drugs may change the test results.
Medicines that may cause you to have an increase in eosinophils include:
- Amphetamines (appetite suppressants)
- Certain laxatives containing psyllium
- Certain antibiotics
- Interferon
- Tranquilizers
A high number of absolute eosinophils (eosinophilia) are often linked to a variety of disorders. A high eosinophil count may be due to:
- Allergic disease
- Parasite infection, such as worms
- Certain fungus infections
- Asthma
- Autoimmune diseases
- Eczema
- Hay fever
- Leukemia and other blood disorders
- Hypereosinophilic syndrome
A lower-than-normal absolute eosinophils count may be due to:
- Alcohol intoxication
- Overproduction of certain steroids in the body (such as cortisol)
- Johnston LK, Hsu C-L, Krier-Burris RA, Chhiba KD, Chien KB, McKenzie A, et al. IL-33 precedes IL-5 in regulating eosinophil commitment and is required for eosinophil homeostasis. J Immunol (2016) 197(9):3445–53.10.4049/jimmunol.1600611[↩]
- Collins PD, Marleau S, Griffiths-Johnson DA, Jose PJ, Williams TJ. Cooperation between interleukin-5 and the chemokine eotaxin to induce eosinophil accumulation in vivo. J Exp Med (1995) 182:1169–74.10.1084/jem.182.4.1169[↩]
- Rothenberg ME, Hogan SP. The eosinophil. Annu Rev Immunol (2006) 24:147–74.10.1146/annurev.immunol.24.021605.090720[↩]
- Diny NL, Rose NR, Čiháková D. Eosinophils in Autoimmune Diseases. Frontiers in Immunology. 2017;8:484. doi:10.3389/fimmu.2017.00484 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5406413/[↩]
- Kovalszki A, Weller PF. Eosinophilia. Prim Care (2016) 43(4):607–17.10.1016/j.pop.2016.07.010[↩]
- Gouon-Evans V, Pollard JW. Eotaxin is required for eosinophil homing into the stroma of the pubertal and cycling uterus. Endocrinology (2001) 142:4515–21.10.1210/endo.142.10.8459[↩]
- Diny NL, Hou X, Barin JG, Chen G, Talor MV, Schaub J, et al. Macrophages and cardiac fibroblasts are the main producers of eotaxins and regulate eosinophil trafficking to the heart. Eur J Immunol (2016) 46:2749–60.10.1002/eji.201646557[↩]
- Lee JJ, Jacobsen EA, Ochkur SI, McGarry MP, Condjella RM, Doyle AD, et al. Human versus mouse eosinophils: “that which we call an eosinophil, by any other name would stain as red”. J Allergy Clin Immunol (2012) 130:572–84.10.1016/j.jaci.2012.07.025[↩]
- Bochner BS. Novel therapies for eosinophilic disorders. Immunol Allergy Clin North Am (2015) 35:577–98.10.1016/j.iac.2015.05.007[↩]
- Rosenberg HF, Dyer KD, Foster PS. Eosinophils: changing perspectives in health and disease. Nat Rev Immunol (2013) 13:9–22.10.1038/nri3341 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4357492/[↩]
- Eosinophils in the zebrafish: prospective isolation, characterization, and eosinophilia induction by helminth determinants. Blood 2010 116:3944-3954 https://doi.org/10.1182/blood-2010-03-267419[↩]
- Rosenberg HF, Dyer KD, Foster PS. Eosinophils: changing perspectives in health and disease. Nat Rev Immunol (2013) 13:9–22.10.1038/nri3341[↩][↩]
- Acharya KR, Ackerman SJ. Eosinophil granule proteins: form and function. J Biol Chem (2014) 289:17406–15.10.1074/jbc.R113.546218[↩]
- Frigas E, Loegering DA, Gleich GJ. Cytotoxic effects of the guinea pig eosinophil major basic protein on tracheal epithelium. Lab Invest (1980) 42:35–43[↩]
- Morgan RK, Costello RW, Durcan N, Kingham PJ, Gleich GJ, McLean WG, et al. Diverse effects of eosinophil cationic granule proteins on IMR-32 nerve cell signaling and survival. Am J Respir Cell Mol Biol (2005) 33:169–77.10.1165/rcmb.2005-0056OC[↩]
- Rosenberg HF, Ackerman SJ, Tenen DG. Human eosinophil cationic protein. Molecular cloning of a cytotoxin and helminthotoxin with ribonuclease activity. J Exp Med (1989) 170:163–76.10.1084/jem.170.1.163[↩]
- Domachowske JB, Dyer KD, Bonville CA, Rosenberg HF. Recombinant human eosinophil-derived neurotoxin/RNase 2 functions as an effective antiviral agent against respiratory syncytial virus. J Infect Dis (1998) 177:1458–64.10.1086/515322[↩]
- Yang D, Chen Q, Rosenberg HF, Rybak SM, Newton DL, Wang ZY, et al. Human ribonuclease A superfamily members, eosinophil-derived neurotoxin and pancreatic ribonuclease, induce dendritic cell maturation and activation. J Immunol (2004) 173:6134–42.10.4049/jimmunol.173.10.6134[↩]
- Lacy P, Latif DA, Steward M, Musat-Marcu S, Man SFP, Moqbel R. Divergence of mechanisms regulating respiratory burst in blood and sputum eosinophils and neutrophils from atopic subjects. J Immunol (2003) 170:2670–9.10.4049/jimmunol.170.5.2670[↩]
- Wang J-G, Mahmud SA, Thompson JA, Geng J-G, Key NS, Slungaard A. The principal eosinophil peroxidase product, HOSCN, is a uniquely potent phagocyte oxidant inducer of endothelial cell tissue factor activity: a potential mechanism for thrombosis in eosinophilic inflammatory states. Blood (2006) 107:558–65.10.1182/blood-2005-05-2152[↩]
- Spencer LA, Melo RCN, Perez SAC, Bafford SP, Dvorak AM, Weller PF. Cytokine receptor-mediated trafficking of preformed IL-4 in eosinophils identifies an innate immune mechanism of cytokine secretion. Proc Natl Acad Sci U S A (2006) 103:3333–8.10.1073/pnas.0508946103[↩]
- Diny NL, Rose NR, Čiháková D. Eosinophils in Autoimmune Diseases. Frontiers in Immunology. 2017;8:484. doi:10.3389/fimmu.2017.00484. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5406413/[↩][↩]
- ischer E, Capron M, Prin L, Kusnierz JP, Kazatchkine MD. Human eosinophils express CR1 and CR3 complement receptors for cleavage fragments of C3. Cell Immunol (1986) 97(2):297–306.10.1016/0008-8749(86)90400-4[↩]
- Decot V, Woerly G, Loyens M, Loiseau S, Quatannens B, Capron M, et al. Heterogeneity of expression of IgA receptors by human, mouse, and rat eosinophils. J Immunol (2005) 174(2):628–35.10.4049/jimmunol.174.2.628[↩]
- Hallam C, Pritchard DI, Trigg S, Eady RP. Rat eosinophil-mediated antibody-dependent cellular cytotoxicity: investigations of the mechanisms of target cell lysis and inhibition by glucocorticoids. Clin Exp Immunol (1982) 48(3):641–8[↩]
- Birring SS, Parker D, McKenna S, Hargadon B, Brightling CE, Pavord ID, et al. Sputum eosinophilia in idiopathic pulmonary fibrosis. Inflamm Res (2005) 54:51–6.10.1007/s00011-004-1321-x[↩]
- Kay AB, Phipps S, Robinson DS. A role for eosinophils in airway remodelling in asthma. Trends Immunol (2004) 25:477–82.10.1016/j.it.2004.07.006[↩]
- Hernnäs J, Särnstrand B, Lindroth P, Peterson CG, Venge P, Malmström A. Eosinophil cationic protein alters proteoglycan metabolism in human lung fibroblast cultures. Eur J Cell Biol (1992) 59:352–63[↩]
- Pégorier S, Wagner LA, Gleich GJ, Pretolani M. Eosinophil-derived cationic proteins activate the synthesis of remodeling factors by airway epithelial cells. J Immunol (2006) 177:4861–9.10.4049/jimmunol.177.7.4861[↩]
- Smyth CM, Akasheh N, Woods S, Kay E, Morgan RK, Thornton MA, et al. Activated eosinophils in association with enteric nerves in inflammatory bowel disease. PLoS One (2013) 8:e64216.10.1371/journal.pone.0064216[↩]
- Sawatzky DA, Kingham PJ, Court E, Kumaravel B, Fryer AD, Jacoby DB, et al. Eosinophil adhesion to cholinergic nerves via ICAM-1 and VCAM-1 and associated eosinophil degranulation. Am J Physiol Lung Cell Mol Physiol (2002) 282(6):L1279–88.10.1152/ajplung.00279.2001[↩]
- Hogan SP, Mishra A, Brandt EB, Royalty MP, Pope SM, Zimmermann N, et al. A pathological function for eotaxin and eosinophils in eosinophilic gastrointestinal inflammation. Nat Immunol (2001) 2(4):353–60.10.1038/86365[↩]
- Kingham PJ, McLean WG, Walsh M-T, Fryer AD, Gleich GJ, Costello RW. Effects of eosinophils on nerve cell morphology and development: the role of reactive oxygen species and p38 MAP kinase. Am J Physiol Lung Cell Mol Physiol (2003) 285(4):L915–24.10.1152/ajplung.00094.2003[↩]
- Garland A, Necheles J, White SR, Neeley SP, Leff AR, Carson SS, et al. Activated eosinophils elicit substance P release from cultured dorsal root ganglion neurons. Am J Physiol (1997) 273(5 Pt 1):L1096–102[↩]
- Elbon CL, Jacoby DB, Fryer AD. Pretreatment with an antibody to interleukin-5 prevents loss of pulmonary M2 muscarinic receptor function in antigen-challenged guinea pigs. Am J Respir Cell Mol Biol (1995) 12(3):320–8.10.1165/ajrcmb.12.3.7873198[↩]
- Yousefi S, Gold JA, Andina N, Lee JJ, Kelly AM, Kozlowski E, et al. Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat Med (2008) 14:949–53.10.1038/nm.1855[↩]
- Simon D, Simon HU, Yousefi S. Extracellular DNA traps in allergic, infectious, and autoimmune diseases. Allergy (2013) 68:409–16.10.1111/all.12111[↩]
- Dworski R, Simon H-U, Hoskins A, Yousefi S. Eosinophil and neutrophil extracellular DNA traps in human allergic asthmatic airways. J Allergy Clin Immunol (2011) 127(5):1260–6.10.1016/j.jaci.2010.12.1103[↩]
- Simon D, Hoesli S, Roth N, Staedler S, Yousefi S, Simon H-U. Eosinophil extracellular DNA traps in skin diseases. J Allergy Clin Immunol (2011) 127(1):194–9.10.1016/j.jaci.2010.11.002[↩]
- Otani IM, Anilkumar AA, Newbury RO, Bhagat M, Beppu LY, Dohil R, et al. Anti-IL-5 therapy reduces mast cell and IL-9 cell numbers in pediatric patients with eosinophilic esophagitis. J Allergy Clin Immunol (2013) 131:1576–82.10.1016/j.jaci.2013.02.042[↩]
- Wang H-B, Ghiran I, Matthaei K, Weller PF. Airway eosinophils: allergic inflammation recruited professional antigen-presenting cells. J Immunol (2007) 179(11):7585–92.10.4049/jimmunol.179.11.7585[↩]
- Shi HZ, Humbles A, Gerard C, Jin Z, Weller PF. Lymph node trafficking and antigen presentation by endobronchial eosinophils. J Clin Invest (2000) 105(7):945–53.10.1172/JCI8945[↩]
- Garro AP, Chiapello LS, Baronetti JL, Masih DT. Rat eosinophils stimulate the expansion of Cryptococcus neoformans-specific CD4(+) and CD8(+) T cells with a T-helper 1 profile. Immunology (2011) 132(2):174–87.10.1111/j.1365-2567.2010.03351.x[↩]
- Jacobsen EA, Zellner KR, Colbert D, Lee NA, Lee JJ. Eosinophils regulate dendritic cells and Th2 pulmonary immune responses following allergen provocation. J Immunol (2011) 187:6059–68.10.4049/jimmunol.1102299[↩]
- Jacobsen EA, Doyle AD, Colbert DC, Zellner KR, Protheroe CA, LeSuer WE, et al. Differential activation of airway eosinophils induces IL-13 mediated allergic Th2 pulmonary responses in mice. Allergy (2015) 70(9):1148–59.10.1111/all.12655[↩]
- Chu DK, Jimenez-Saiz R, Verschoor CP, Walker TD, Goncharova S, Llop-Guevara A, et al. Indigenous enteric eosinophils control DCs to initiate a primary Th2 immune response in vivo. J Exp Med (2014) 211:1657–72.10.1084/jem.20131800[↩]
- Chu VT, Fröhlich A, Steinhauser G, Scheel T, Roch T, Fillatreau S, et al. Eosinophils are required for the maintenance of plasma cells in the bone marrow. Nat Immunol (2011) 12:151–9.10.1038/ni.1981[↩]
- Jung Y, Wen T, Mingler MK, Caldwell JM, Wang YH, Chaplin DD, et al. IL-1β in eosinophil-mediated small intestinal homeostasis and IgA production. Mucosal Immunol (2015) 8(4):930–42.10.1038/mi.2014.123[↩]
- Todd R, Donoff BR, Chiang T, Chou MY, Elovic A, Gallagher GT, et al. The eosinophil as a cellular source of transforming growth factor alpha in healing cutaneous wounds. Am J Pathol (1991) 138:1307.[↩]
- Ohno I, Nitta Y, Yamauchi K, Hoshi H, Honma M, Woolley K, et al. Eosinophils as a potential source of platelet-derived growth factor B-chain (PDGF-B) in nasal polyposis and bronchial asthma. Am J Respir Cell Mol Biol (1995) 13:639–47.10.1165/ajrcmb.13.6.7576701[↩]
- Horiuchi T, Weller PF. Expression of vascular endothelial growth factor by human eosinophils: upregulation by granulocyte macrophage colony-stimulating factor and interleukin-5. Am J Respir Cell Mol Biol (1997) 17:70–7.10.1165/ajrcmb.17.1.2796[↩]
- Stenfeldt A-L, Wennerås C. Danger signals derived from stressed and necrotic epithelial cells activate human eosinophils. Immunology (2004) 112:605–14.10.1111/j.1365-2567.2004.01906.x[↩]
- Goh YPS, Henderson NC, Heredia JE, Red Eagle A, Odegaard JI, Lehwald N, et al. Eosinophils secrete IL-4 to facilitate liver regeneration. Proc Natl Acad Sci U S A (2013) 110:9914–9.10.1073/pnas.1304046110[↩]
- Heredia JE, Mukundan L, Chen FM, Mueller AA, Deo RC, Locksley RM, et al. Type 2 innate signals stimulate fibro/adipogenic progenitors to facilitate muscle regeneration. Cell (2013) 153:376–88.10.1016/j.cell.2013.02.053[↩]
- The functional heterogeneity of eosinophil cationic protein is determined by a gene polymorphism and post-translational modifications. Clin Exp Allergy. 2007 Feb;37(2):208-18. https://www.ncbi.nlm.nih.gov/pubmed/17250693[↩]
- Leukotriene D4 and eosinophil transendothelial migration, superoxide generation, and degranulation via beta2 integrin. Ann Allergy Asthma Immunol. 2004 Dec;93(6):594-600. https://www.ncbi.nlm.nih.gov/pubmed/15609771[↩]
- The cellular biology of eosinophil eicosanoid formation and function. J Allergy Clin Immunol. 2002 Mar;109(3):393-400. https://www.ncbi.nlm.nih.gov/pubmed/11897981[↩]
- Leukotriene D4 induces production of transforming growth factor-beta1 by eosinophils. Int Arch Allergy Immunol. 2005;137 Suppl 1:17-20. Epub 2005 Jun 2. https://www.ncbi.nlm.nih.gov/pubmed/15947480[↩]
- Eosinophils: biological properties and role in health and disease. Clin Exp Allergy. 2008 May;38(5):709-50. doi: 10.1111/j.1365-2222.2008.02958.x. Epub 2008 Apr 1. https://www.ncbi.nlm.nih.gov/pubmed/18384431[↩]
- The eosinophil. Annu Rev Immunol. 2006;24:147-74. https://www.ncbi.nlm.nih.gov/pubmed/16551246[↩]
- Eosinophils function as antigen-presenting cells. J Leukoc Biol. 2004 Sep;76(3):520-7. Epub 2004 Jun 24. https://www.ncbi.nlm.nih.gov/pubmed/15218055[↩]
- The immunology of asthma. Nat Immunol. 2015 Jan;16(1):45-56. doi: 10.1038/ni.3049. https://www.ncbi.nlm.nih.gov/pubmed/25521684[↩]
- Sanderson, Colin (1992). “Interleukin-5, Eosinophils, and Disease”. Blood. 79 (12): 3101–3109.[↩]