Contents
- What are gallstones
- The gallbladder
- What is choledocholithiasis?
- Gallstone types
- What causes gallstones?
- Who’s at risk of gallstones?
- Gallstones prevention
- Gallstones signs and symptoms
- Gallstones complications
- Gallstones diagnosis
- Gallstones treatment
- Gallstones prognosis
What are gallstones
Cholelithiasis is a medical term for gallstones, which are hardened pebble-like pieces of digestive fluid, usually made of cholesterol or bilirubin, that can form in your gallbladder 1. Gallstones can range in size from a grain of sand to as large as a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time. Your gallbladder is a small pear-shaped organ located just beneath your liver, on the right side of your abdomen. The gallbladder holds a digestive fluid known as bile that is released into your small intestine. The gallbladder can make one large gallstone, hundreds of tiny stones, or both small and large stones.
There are 2 main types of gallstones that can form in your gallbladder:
- Cholesterol gallstones. The most common type of gallstone (80%-98% of gallstones), called a cholesterol gallstone, often appears yellow in color. These gallstones are composed mainly of undissolved cholesterol, but may contain other components. Cholesterol gallstones are not related to cholesterol level in the blood. Cholesterol gallstones are formed mainly due to over secretion of cholesterol by liver cells and hypomotility or impaired emptying of the gallbladder. In most cases, they are not visible on CT scans but are visible on a sonogram (ultrasound) of the abdomen.
- Pigment gallstones (2%-20% of gallstones). Approximately 2% to 20% of gallstones of all gallstones are black and brown pigment stones. These dark brown or black stones form when your bile contains too much bilirubin. Pigment stones occur when red blood cells are destroyed and too much bilirubin is in the bile. These can be found in individuals with high hemoglobin turnover. The pigment consists of mostly bilirubin. Patients with cirrhosis, ileal diseases, sickle cell anemia, and cystic fibrosis are at risk of developing black pigment stones. Brown pigments are mainly found in Southeast Asian population and are not common in the United States. Risk factors for brown pigment stones are intraductal stasis and chronic colonization of bile with bacteria.
In the United States, 6% of men and 9% of women have gallstones, most of which are asymptomatic 1. The highest prevalence of gallstones arises in Native American populations. Gallstones are not as common in Africa or Asia. The epidemic of obesity has likely magnified the rise of gallstones.
Despite how prevalent gallstones may be, more than 80% of people remain asymptomatic 1. In patients with asymptomatic gallstones discovered incidentally, the likelihood of developing symptoms or complications is 1% to 2% per year. Those who started to develop symptoms may continue to have major complications (cholecystitis, choledocholithiasis, gallstone pancreatitis, cholangitis) occur at a rate of 0.1% to 0.3% yearly. Asymptomatic gallbladder stones found in a normal gallbladder and normal biliary tree do not need treatment unless they develop symptoms. However, approximately 20% of these asymptomatic gallstones will develop symptoms over 15 years of follow-up. These gallstones may go on further to develop complications such as cholecystitis, cholangitis, choledocholithiasis, gallstone pancreatitis, and rarely cholangiocarcinoma 1.
Gallstones are more common if you:
- are female, particularly if you have had children, are taking the combined pill, or are undergoing high-dose estrogen therapy
- are overweight or obese
- are aged 40 years or older (the older you are, the more likely you are to develop gallstones)
- have a condition that affects the flow of bile (such as cirrhosis, primary sclerosing cholangitis, or obstetric cholestasis)
- have Crohn’s disease or irritable bowel syndrome (IBS). Patients with Crohn disease and those with ileum disease (or resection) are not able to reabsorb bile salts and this increases the risk of gallstones.
- have a close family member who’s also had gallstones
- have recently lost weight (from either dieting or weight loss surgery)
- are taking an antibiotic called ceftriaxone
Many people with gallstones do not have any symptoms. Gallstones that do not cause symptoms are called silent gallstones. Silent gallstones don’t stop your gallbladder, liver, or pancreas from working, so they do not need treatment. Gallstones are often found during a routine X-ray, abdominal surgery, or other medical procedure. However, if a gallstone lodges in a duct or tube that drains your gallbladder and causes a blockage, bile could build up in your gallbladder causing a gallbladder attack and you may have a cramping pain in the middle to right upper abdomen. This is known as biliary colic. The pain goes away if the stone passes into the first part of the small intestine.
Gallstone pain may last several minutes to a few hours. Gallbladder attacks often follow heavy meals and usually occur in the evening or during the night. If you’ve had one gallbladder attack, more attacks will likely follow.
Gallbladder attacks usually stop when gallstones move and no longer block the bile ducts. However, if any of your bile ducts stay blocked for more than a few hours, you may develop gallstone complications. Gallstones that do not block your bile ducts do not cause symptoms.
People who experience symptoms from their gallstones usually require gallbladder removal surgery. Gallstones that don’t cause any signs and symptoms typically don’t need treatment.
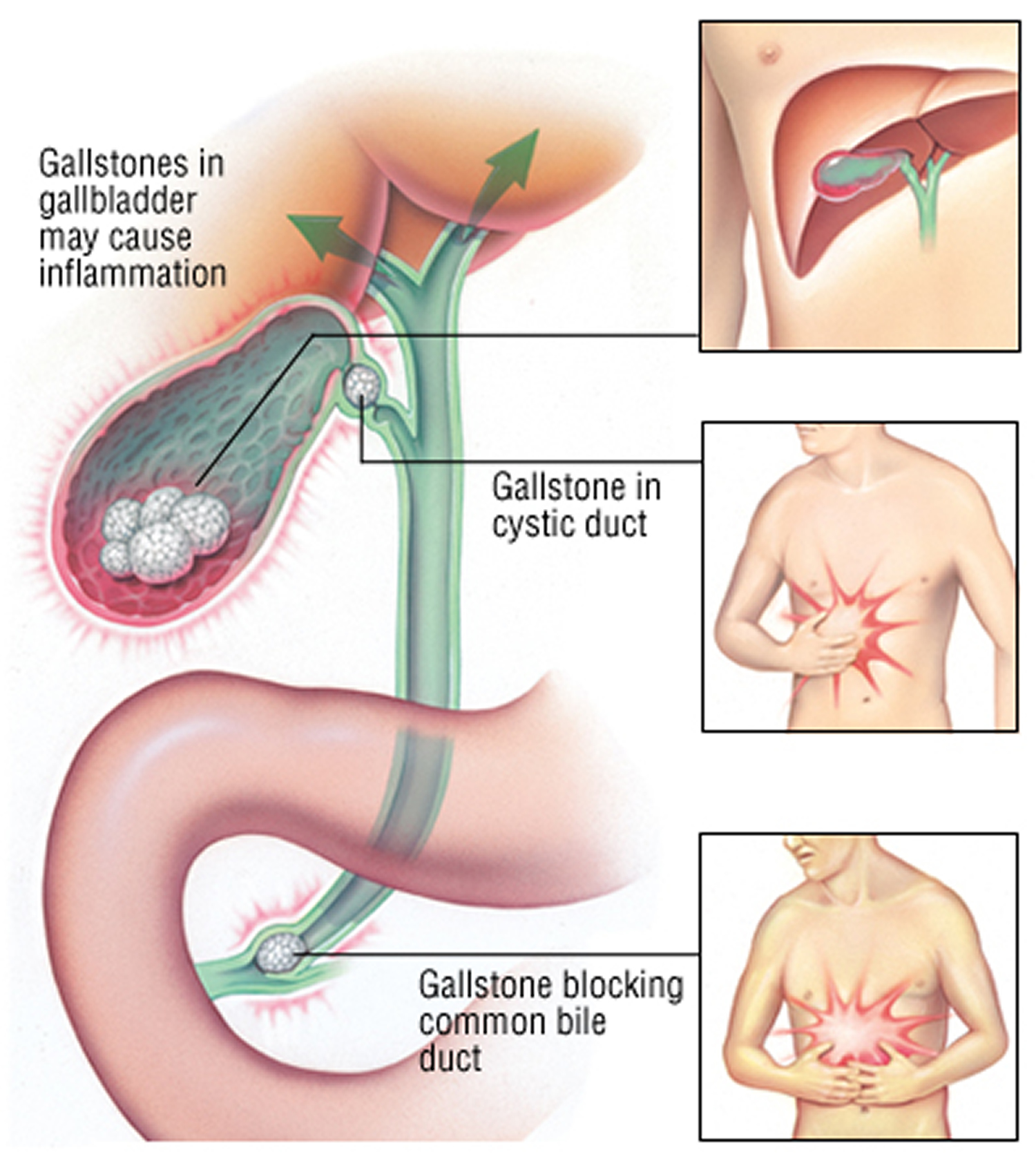
Symptoms and complications of gallstones result when stones obstruct the cystic duct, bile ducts or both. Temporary obstruction of the cystic duct (as when a stone lodges in cystic duct before the duct dilates and the stone returns to gallbladder) results in intense abdominal pain commonly known as biliary colic, but is usually short-lived, usually lasts 1 to 5 hours, although it can sometimes last just a few minutes. When gallstones cause symptoms or complications, it’s known as gallstone disease or cholelithiasis.
More persistent obstruction of cystic duct (as when a large gallstone gets permanently lodged in the neck of the gallbladder) can lead to acute cholecystitis (inflammation of the gallbladder). Acute cholecystitis can cause persistent pain, jaundice and a fever.
Sometimes a gallstone may get pass through the cystic duct and get lodged and impacted the common bile duct, and causes obstruction and jaundice. This complication is known as choledocholithiasis.
If gallstones pass through the cystic duct, common bile duct and get dislodged at the ampulla of the distal portion of the bile duct, acute gallstone pancreatitis may result from backing up of fluid and increase pressure in pancreatic ducts and in situ activation of pancreatic enzymes. Occasionally, large gallstones do perforate the gallbladder wall and create a fistula between the gallbladder and small or large bowel, producing bowel obstruction or ileus.
Make an appointment with your doctor if you have any signs or symptoms that worry you.
Seek immediate care if you develop signs and symptoms of a serious gallstone complication, such as:
- You develop abdominal pain, with or without fever, and there is no known cause.
- Your abdominal pain is so intense that you can’t sit still or find a comfortable position
- You develop jaundice (yellowing of your skin and the whites of your eyes).
- Fever—even a low-grade fever—or chills
- You have other symptoms of choledocholithiasis (gallstone in a common bile duct)
- Loss of appetite
- Nausea and vomiting
- Tea-colored urine and light-colored stools
These symptoms may be signs of a serious infection or inflammation of the gallbladder, liver, or pancreas. Gallstone symptoms may be similar to symptoms of other conditions, such as appendicitis, ulcers, pancreatitis, and gastroesophageal reflux disease (GERD), all of which should be treated by a doctor as soon as possible.
Gallstone complications can occur if your bile ducts stay blocked. Left untreated, blockages of the bile ducts or pancreatic duct can be fatal.
What is biliary colic?
Biliary colic is intermittent pain from gallstones that obstruct your biliary system intermittently (off and on). This is more common with gallbladder stones, but can happen with choledocholithiasis if a gallstone obstructs your common bile duct off and on — for example, if it moves in and out of your duct.
Who is more likely to develop gallstones?
Certain groups of people have a higher risk of developing gallstones than others 2:
- Women are more likely to develop gallstones than men. Women who have extra estrogen in their body due to pregnancy, hormone replacement therapy, or birth control pills may be more likely to produce gallstones.
- Older people are more likely to develop gallstones. As you age, the chance that you’ll develop gallstones becomes higher.
- People with a family history of gallstones have a higher risk.
- American Indians have genes that raise the amount of cholesterol in their bile, and have the highest rate of gallstones in the United States.
- Mexican Americans are also at higher risk of developing gallstones.
You are more likely to develop gallstones if you have one of the following health conditions:
- Cirrhosis. Cirrhosis is severe scarring of the liver, a condition in which your liver slowly breaks down and stops working due to chronic, or long-lasting, injury
- Cholangitis or infections in the bile ducts, which can also be a complication of gallstones
- Hemolytic anemias, conditions in which red blood cells are continuously broken down, such as sickle cell anemia
- Some intestinal diseases that affect normal absorption of nutrients, such as Crohn’s disease
- High triglyceride levels (hypertriglyceridemia)
- Low HDL cholesterol
- Metabolic syndrome, which can also raise the risk of gallstone complications
- Diabetes and insulin resistance
- Bone marrow or solid organ transplant
- Failure of the gallbladder to empty bile properly (this is more likely to happen during pregnancy)
You are more likely to develop gallstones if you:
- have obesity, especially if you are a woman
- have had rapid weight loss from eating a very low-calorie diet, or after weight loss surgery, also called metabolic and bariatric surgery
- have been on a diet high in calories and refined carbohydrates and low in fiber
- are receiving nutrition through a vein for a long period of time (intravenous feedings)
- are taking birth control pills.
How does weight affect gallstones?
Being overweight or having obesity may make you more likely to develop gallstones, especially if you are a woman. Researchers have found that people who have obesity may have higher levels of cholesterol in their bile, which can cause gallstones. People who have obesity may also have large gallbladders that do not work well. Some studies have shown that people who carry large amounts of fat around their waist may be more likely to develop gallstones than those who carry fat around their hips and thighs.
Losing weight very quickly may raise your chances of forming gallstones, however. Talk with your health care professional about how to lose weight safely.
How does my fast weight loss affect gallstones?
When you don’t eat for a long period of time or you lose weight quickly, your liver releases extra cholesterol into the bile. Fast weight loss can also prevent the gallbladder from emptying properly. Weight-loss surgery may lead to fast weight loss and higher risk of gallstones.
Your chances of developing gallstones may depend on the type of weight-loss treatment you choose. Diets or surgeries that cause fast weight loss may be more likely to lead to gallstone problems than diets or surgeries that lead to slower weight loss. If you have silent gallstones, you may also be more likely to develop gallstone symptoms.
Several factors may raise your chances of having problems with gallstones after weight-loss surgery or a very low-calorie diet. These factors include:
- gallstones that you had before your weight-loss surgery or before you went on a very low-calorie diet, especially if the stones caused symptoms
- a large amount of extra weight before you have weight-loss surgery or go on a very low-calorie diet
- very quick weight loss after the surgery or a very low-calorie diet
If you are starting a very low-calorie diet or having weight-loss surgery, talk with your doctor about how to lower your chances of developing gallstones. The medicine ursodiol can help prevent gallstones in people who lose weight rapidly through very low-calorie diets or weight-loss surgery.
Is weight cycling a problem?
Weight cycling, or losing and regaining weight repeatedly, may also lead to gallstones. The more weight you lose and regain during a cycle, the greater your chances of developing gallstones.
Stay away from “crash diets” that promise to help you drop the pounds quickly. Aim for losing weight at a slower pace and keeping it off over time.
How can I safely lose weight to lower my chances of getting gallstones?
Losing weight at a slow pace may make it less likely that you will develop gallstones. For people who are overweight or have obesity, experts recommend beginning with a weight loss of 5 to 10 percent of your starting weight over a period of 6 months 3. In addition, weight loss may bring you other benefits such as better mood, more energy, and positive self-image.
When making healthy food choices to help you lose weight, you can choose food that may also lower your chances of developing gallstones.
Regular physical activity, which will improve your overall health, may also lower your chances of developing gallstones. To improve health or prevent weight gain, aim for at least 150 minutes a week of moderate-intensity physical activity, like brisk walking or fast dancing. Adults also need muscle-strengthening activity, like lifting weights or doing push-ups, at least 2 days a week 4.
Talk with your doctor before you start an eating and physical activity plan to improve your health or maintain your weight loss.
What is choledocholithiasis vs. cholelithiasis?
You may have also heard the term “cholelithiasis,” which is similar. Cholelithiasis is the condition of having gallstones in your gallbladder. Gallstones may develop in your gallbladder or bile ducts, or both. A gallstone that develops in your gallbladder may also travel to your common bile duct.
The gallbladder
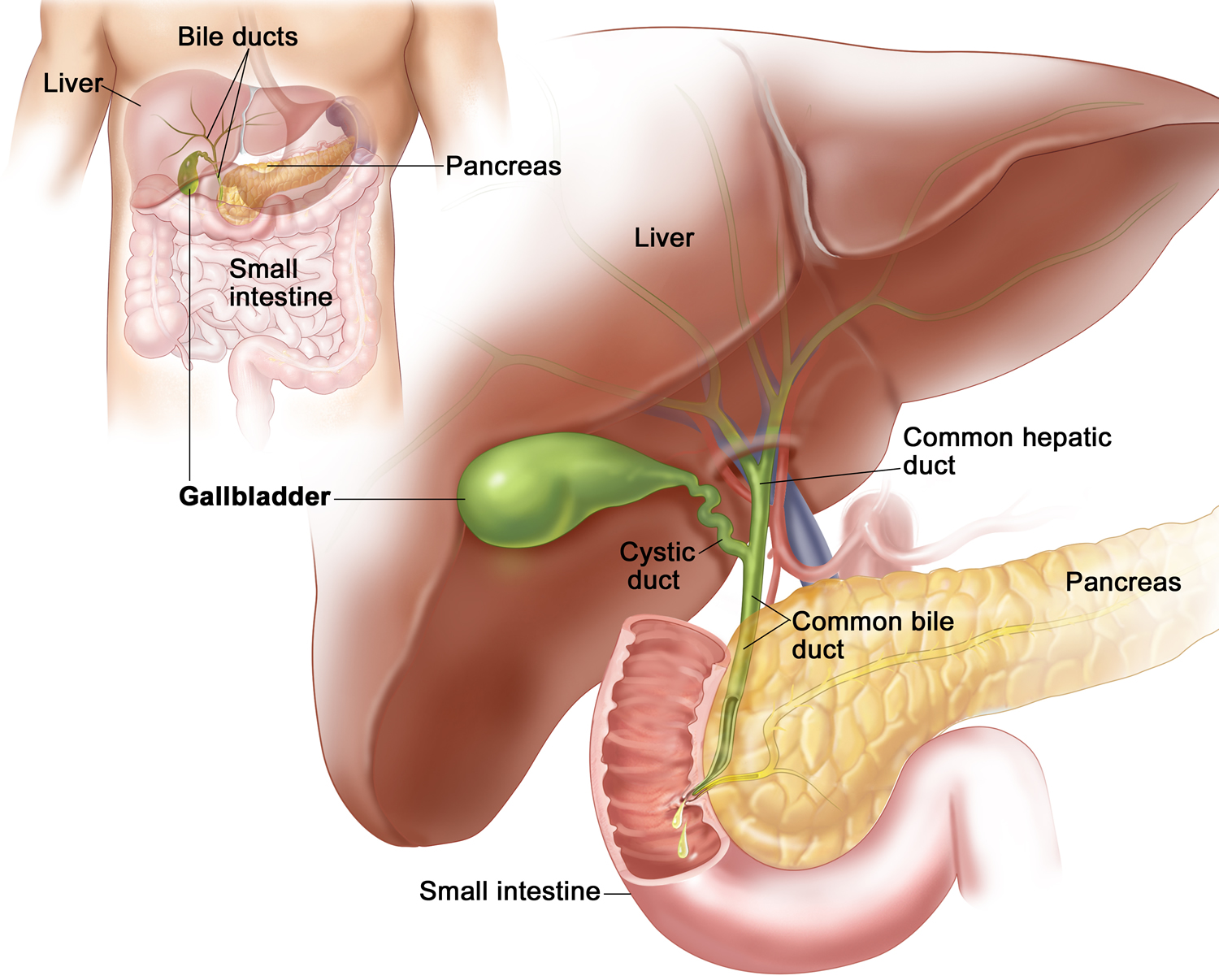
The gallbladder is a small, pouch-like organ found underneath the liver. Its main purpose is to store and concentrate bile.
Bile is a liquid produced by the liver to help digest fats. It’s passed from the liver into the gallbladder through a series of channels known as bile ducts.
The bile is stored in the gallbladder and, over time, becomes more concentrated, which makes it better at digesting fats.
The gallbladder releases bile into the digestive system when it’s needed.
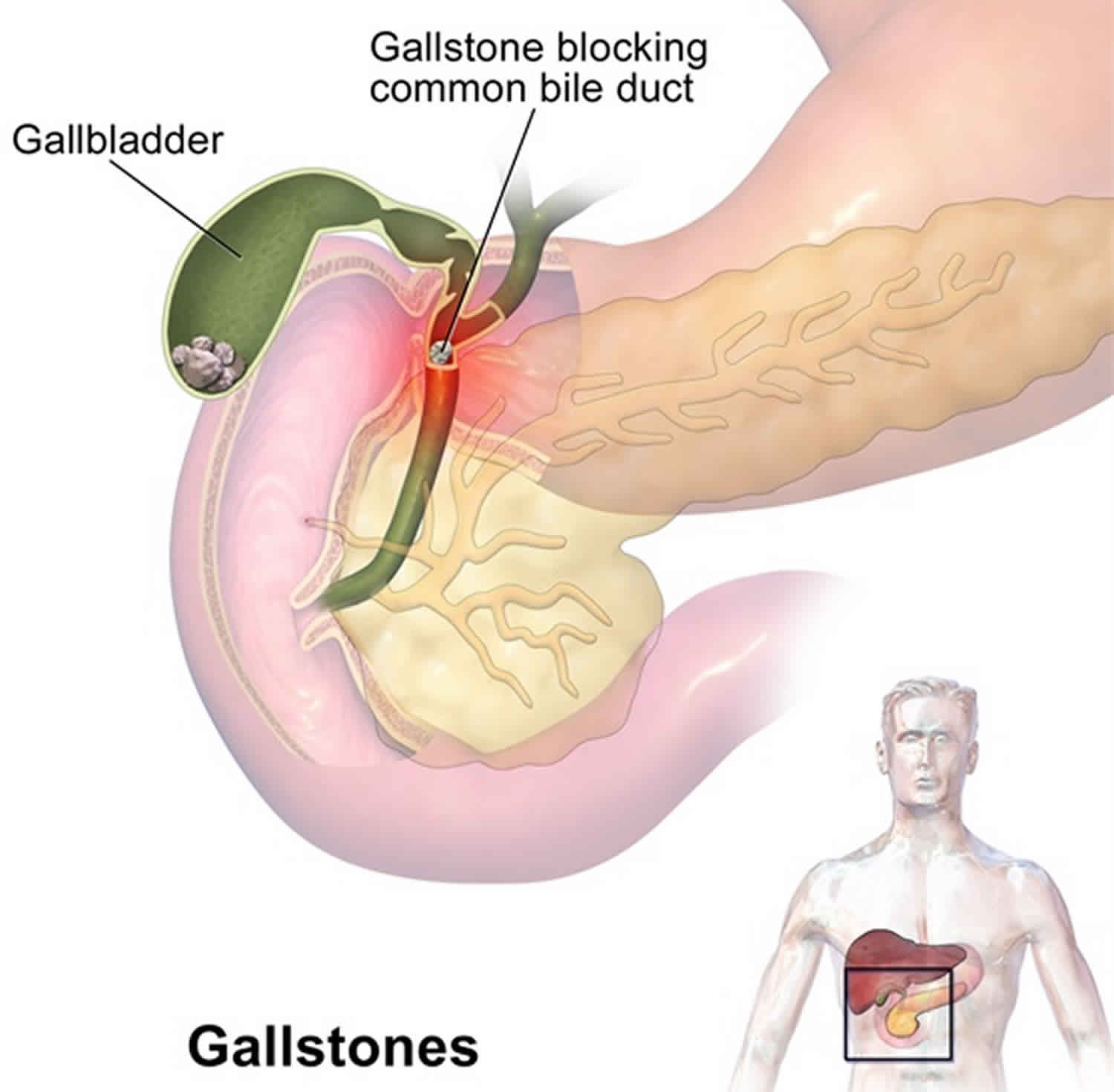
Figure 1. Gallbladder location
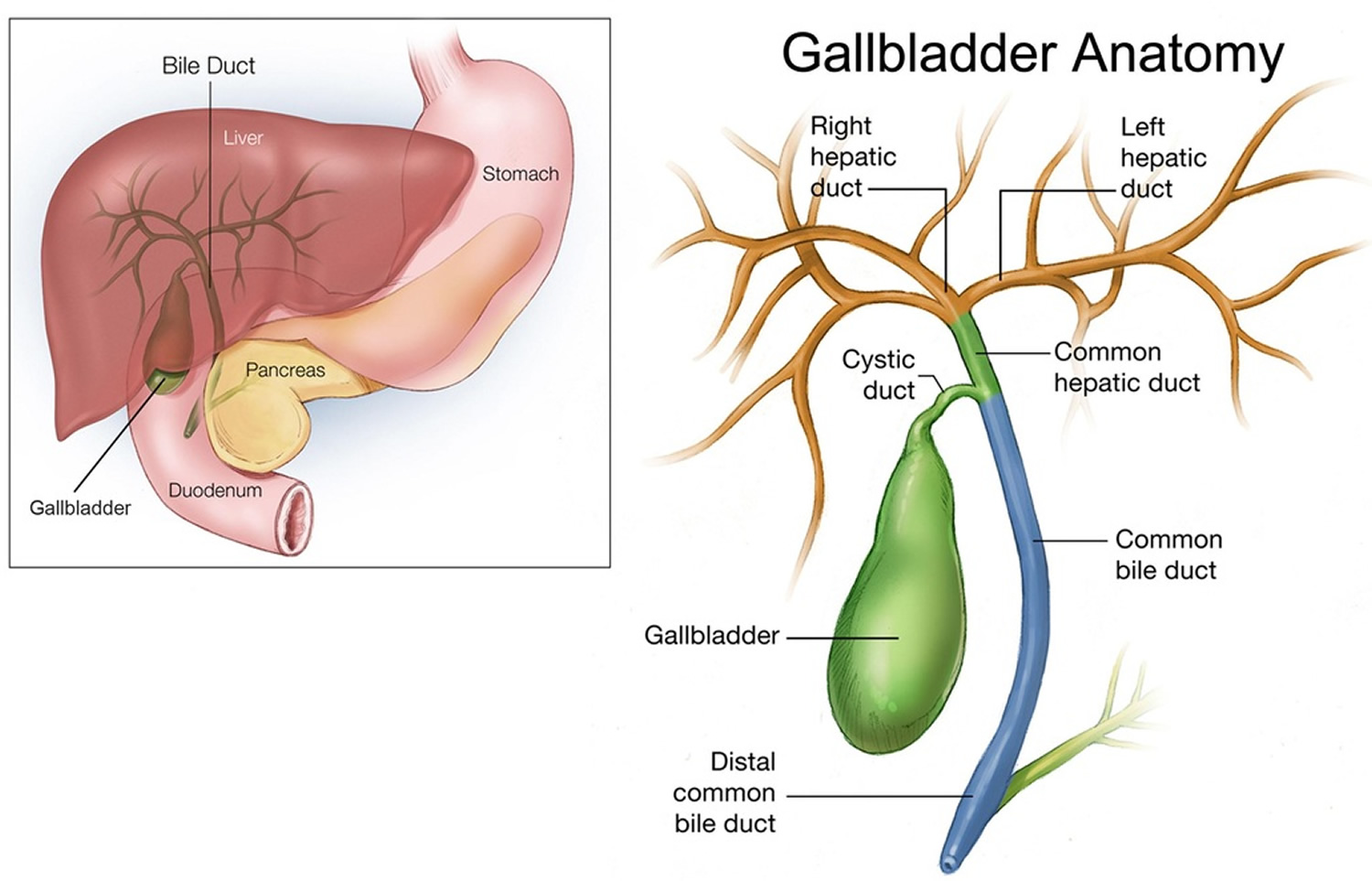
Figure 2. Gallbladder anatomy
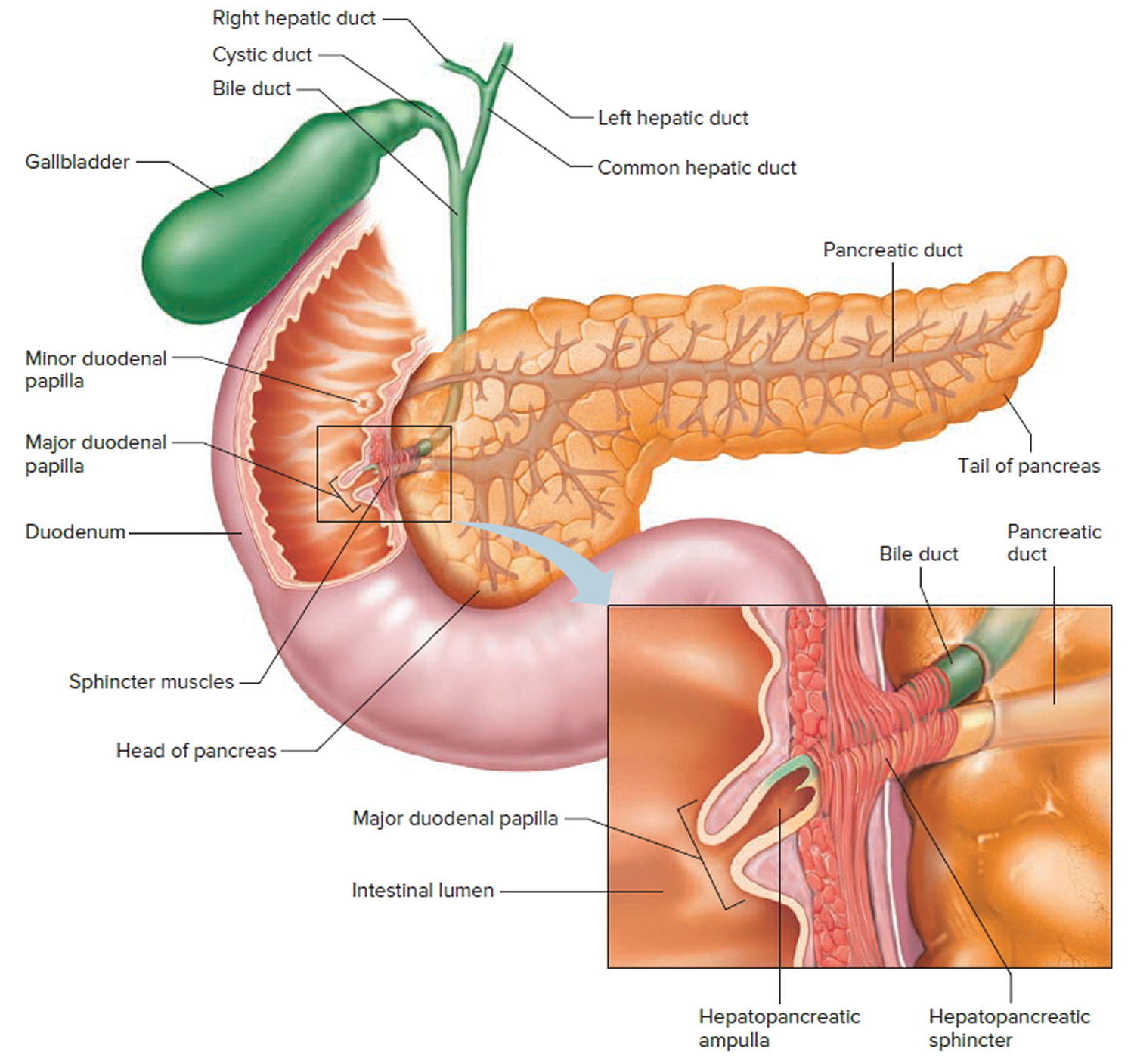
Figure 3. The common bile duct is closely associated with the pancreatic duct and the duodenum
Gallbladder function
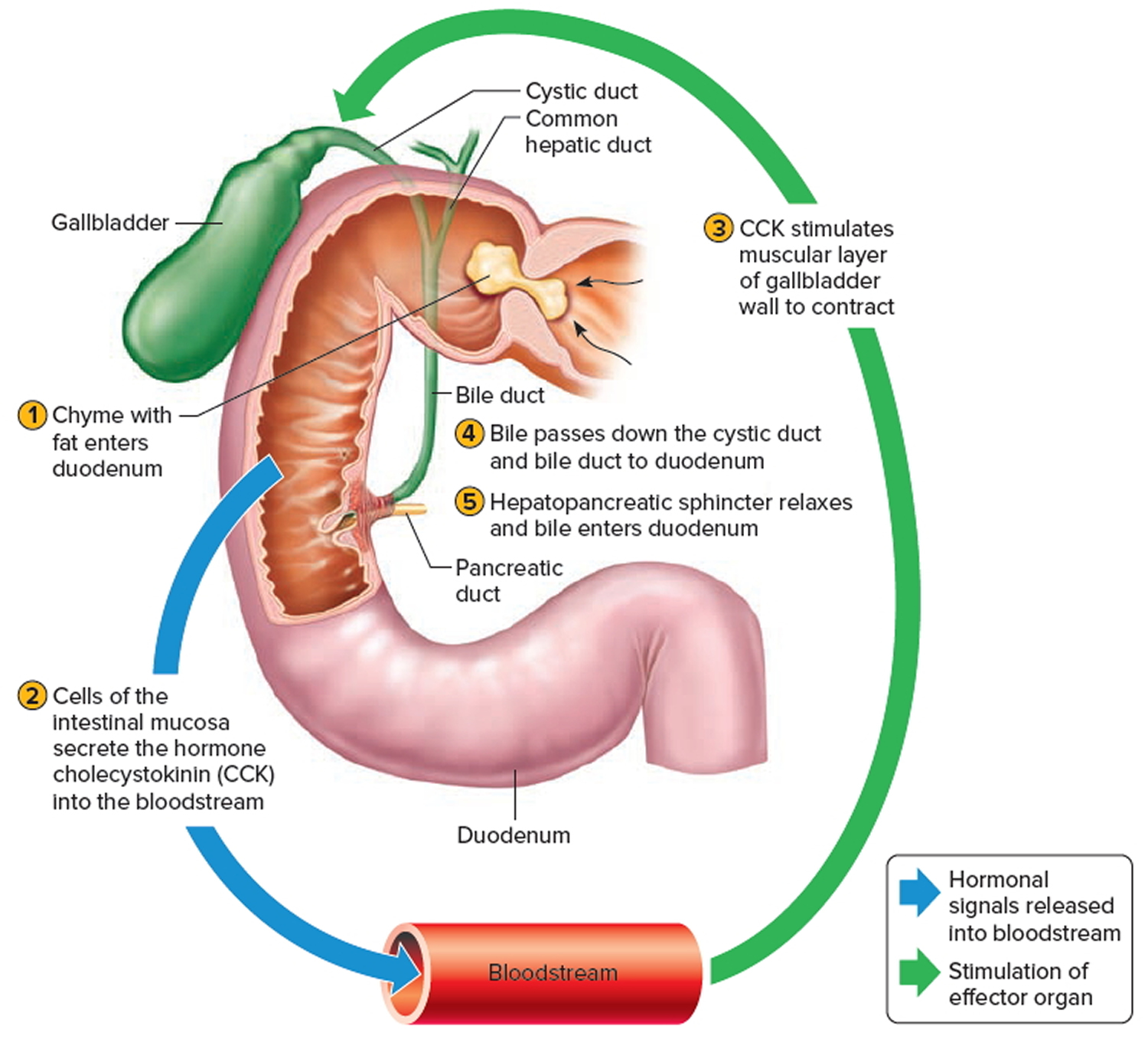
Following a meal, the mixing movements of the stomach wall aid in producing a semifluid paste of food particles and gastric juice called chyme.
As chyme enters the duodenum (the proximal portion of the small intestine), accessory organs—the pancreas, liver, and gallbladder—add their secretions.
Bile is a yellowish-green liquid continuously secreted from hepatic (liver) cells. In addition to water, bile contains bile salts, bile pigments (bilirubin and biliverdin), cholesterol, and electrolytes. Of these, bile salts are the most abundant and are the only bile components that have a digestive function.
Bile pigments are breakdown products of hemoglobin from red blood cells and are normally secreted in the bile.
Normally bile does not enter the duodenum until cholecystokinin stimulates the gallbladder to contract. Proteins and fats in chyme in the duodenum stimulate
the intestinal wall to release cholecystokinin. Cholecystokinin travels via the bloodstream to the pancreas also, where it stimulate the pancreas to release its pancreatic juice that has a high concentration of digestive enzymes.
The hepatopancreatic sphincter usually remains contracted until a peristaltic wave in the duodenal wall approaches it. Then the sphincter relaxes, and bile is squirted into the duodenum (see Figure 4).
Note: Cholecystokinin produced by the intestinal wall cells, in response to proteins and fats in the small intestine, decreases secretory activity of gastric glands and inhibits gastric motility; stimulates pancreas to secrete fluid with a high digestive enzyme concentration and stimulates gallbladder to contract and release bile.
Figure 4. Fatty chyme entering the duodenum stimulates the gallbladder to release bile
Figure 5. Gallstones
What is choledocholithiasis?
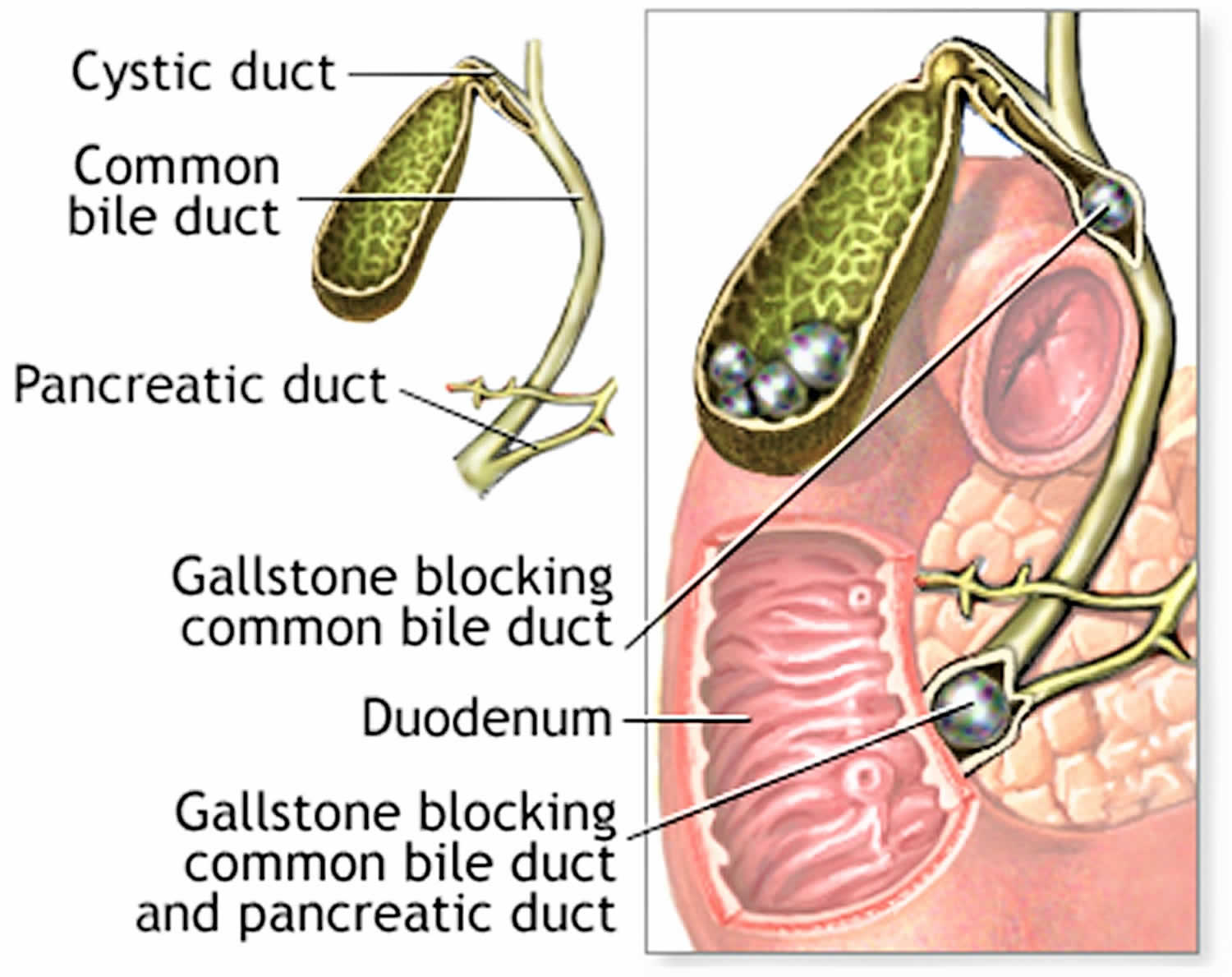
Choledocholithiasis is the presence of gallstone or gallstones within the common bile duct (CBD) 5, 6, 7, 8. “Choledocho” is the Latin term for the common bile duct and “lithiasis” means stones. Gallstone (cholelithiasis) may be made up of bile pigments or calcium and cholesterol salts. The common bile duct is a small tube that carries bile from the gallbladder to the duodenum (first segment of the small intestine). Bile is made in your liver and flows through the common hepatic duct and the cystic duct to the gallbladder, where it is stored. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder holds a digestive fluid called bile that’s released into your small intestine. When food is being digested, bile is released from the gallbladder and flows through the common bile duct (CBD), pancreas, and ampulla of Vater into the small intestine. Gallstones in the common bile duct pose a risk of obstructing the flow of bile. An obstruction can cause pain, inflammation and serious complications. Obstruction of the common bile duct may also lead to obstruction of the pancreatic duct because these ducts are usually connected. If the pancreatic duct is also obstructed, pancreatitis will likely develop.
If you have choledocholithiasis, you have at least one gallstone in your common bile duct (CBD). If a gallstone is very small, it may not cause you any problems and may even pass into your intestines. But if a gallstone becomes large enough or blocks your common bile duct, it’ll cause symptoms of severe constant pain and jaundice. A blockage in your common bile duct can cause inflammation, infection and life-threatening complications. Bile flow that is obstructed by stones within the common bile duct can lead to obstructive jaundice and possibly hepatitis. The stagnant bile can also lead to bactibilia (the presence of bacteria in gallbladder bile) and acute cholangitis. Acute cholangitis, also known as ascending cholangitis, is a life-threatening condition that is caused by an ascending bacterial infection of the biliary tree 9, 10. Delay in diagnosis and treatment can lead to septic shock. Cholangitis and sepsis are more common in patients with choledocholithiasis than other sources of bile duct obstruction because a bacterial biofilm typically covers common bile duct stones. The pancreatic duct joins the common bile duct near the duodenum, and therefore, the pancreas may also become inflamed by the obstruction of pancreatic enzymes. This is termed gallstone pancreatitis 11.
The incidence of choledocholithiasis in patients with gallstones (cholelithiasis) increases with age. Gallstones are hardened deposits of digestive fluid. Gallstones can vary in size and number. Gallstones (cholelithiasis) is more common in female patients, pregnant patients, older patients, and those with high serum lipid levels 12, 13. Gallstones are differentiated by their composition. Cholesterol stones are composed mainly of cholesterol, while black pigment stones are mainly made of pigment, and brown pigment stones are composed of a mix of pigment and bile lipids 14, 15. Cholesterol stones are typically found in obese patients with low physical activity or patients that have recently intentionally lost weight. Black pigment stones are found in patients with cirrhosis, patients receiving total parental nutrition, and in those who have undergone an ileal resection. Cholesterol stones make up approximately 75% of the secondary common bile duct stones in the United States, while black pigment stones comprise the remainder 5.
Choledocholithiasis is classified as primary or secondary according to stone origin 16:
- Primary choledocholithiasis refers to stones formed directly within the biliary tree,
- Secondary choledocholithiasis refers to stones ejected from the gallbladder.
Primary choledocholithiasis or primary common bile duct stones are usually brown pigment stones and is rare in Western populations 5. Secondary choledocholithiasis stone composition parallels that of cholelithiasis, with cholesterol as the most common type 16.
Your doctor will determine if treatment for choledocholithiasis is indicated based on your symptoms and the results of diagnostic testing. The goal of treatment is to relieve the blockage. The treatment for choledocholithiasis is the removal of the obstructing stones via endoscopic means.
Choledocholithiasis treatment may involve 17, 18, 19:
- Endoscopic retrograde cholangiopancreatography (ERCP) and a procedure called a sphincterotomy, which makes a surgical cut into the muscle in the common bile duct to allow stones to pass or be removed. Usually after removing gallstones from your bile ducts, doctors often recommend surgery to remove your gallbladder (cholecystectomy). This is to prevent more gallstones from exiting your gallbladder and causing choledocholithiasis again.
- Surgery to remove the gallbladder (cholecystectomy) and stones. Your doctor may recommend surgery to remove your gallbladder, since gallstones frequently recur. Once your gallbladder is removed, bile flows directly from your liver into your small intestine, rather than being stored in your gallbladder. You don’t need your gallbladder to live, and gallbladder removal doesn’t affect your ability to digest food, but it can cause diarrhea, which is usually temporary. A small number of people have softer and more frequent stools after gallbladder removal, because bile now flows into your duodenum more often. Changes in bowel habits are usually temporary; however, discuss them with your doctor.
- Cholecystectomy in patients with choledocholithiasis remains controversial, but most experts recommend it. Arguments can be made against cholecystectomy in patients who cannot tolerate surgery well (eg, due to age, medical problems), as long as the patient is asymptomatic.
- Medications to dissolve gallstones. Oral dissolution therapy such as Ursodiol (Actigall) and chenodiol (Chenix) are medicines that contain bile acids that can break up gallstones. These medicines work best to break up small cholesterol stones. But it may take months or years of treatment to dissolve your gallstones in this way, and gallstones will likely form again if treatment is stopped. Sometimes medications don’t work. Medications for gallstones aren’t commonly used and are reserved for people who can’t undergo surgery.
- Shock wave lithotripsy. A doctor can use shock wave lithotripsy to blast gallstones into small pieces. Doctors use this procedure only rarely, and sometimes along with Ursodiol (Actigall).
Depending on your condition, you may need treatment before your gallstones can be removed, such as:
- Antibiotics to treat infection.
- Biliary drainage to remove backed-up bile.
Figure 5. Choledocholithiasis
Make an appointment with your doctor if you have any signs or symptoms that worry you.
Seek immediate care if you develop signs and symptoms of a serious gallstone complication, such as:
- Abdominal pain so intense that you can’t sit still or find a comfortable position
- Yellowing of your skin and the whites of your eyes (jaundice)
- High fever with chills
How common is choledocholithiasis?
About 10% of people have gallstones, but most of them form in their gallbladder. About 1 in 7 people with gallstones will develop stones in the common bile duct. About 4.6% to 18.8% of people undergoing cholecystectomy have gallstones in their common bile duct. Gallstones will never bother most people. Only 20% of people with gallstones will have complications that require treatment.
What is choledocholithiasis vs. cholelithiasis?
You may have also heard the term “cholelithiasis,” which is similar. Cholelithiasis is the condition of having gallstones in your gallbladder. Gallstones may develop in your gallbladder or bile ducts, or both. A gallstone that develops in your gallbladder may also travel to your common bile duct.
Is choledocholithiasis an emergency?
A gallstone, or several, in your common bile duct isn’t necessarily an emergency, but it’s a risk. Smaller gallstones may pass safely through your common bile duct to your intestines and out of your body. The risk is that they’ll become stuck there and grow large enough over time to cause a blockage.
Because of this risk, healthcare providers prefer to treat common bile duct stones immediately when they find them. They’ll recommend an endoscopic procedure to examine and, most likely, remove the stones. That means a gastroenterologist will access your bile ducts via a catheter passed down your throat.
Choledocholithiasis causes
It’s not clear what causes gallstones to form. Doctors think gallstones may result when there’s too much of one of these — usually cholesterol, but sometimes bilirubin — and the excess materials turn into a kind of sediment. The sediment collects at the bottom of your gallbladder or your common bile duct and eventually hardens. The stones gradually grow as sediment continues to wash over them. This takes many years. Most gallstones form in your gallbladder and travel with the flow of bile into your common bile duct.
Probable causes gallstones to form 20:
- Your bile contains too much cholesterol. Normally, your bile contains enough chemicals to dissolve the cholesterol excreted by your liver. But if your liver excretes more cholesterol than your bile can dissolve, the excess cholesterol may form into crystals and eventually into stones.
- Your bile contains too much bilirubin. Bilirubin is a chemical that’s produced when your body breaks down red blood cells. Certain conditions cause your liver to make too much bilirubin, including liver cirrhosis, biliary tract infections and certain blood disorders. The excess bilirubin contributes to gallstone formation.
- Your gallbladder doesn’t empty correctly. If your gallbladder doesn’t empty completely or often enough, bile may become very concentrated, contributing to the formation of gallstones.
Choledocholithiasis occurs as a result of either the formation of stones in the common bile duct or the passage of gallstones that are formed in the gallbladder into the common bile duct. Bile stasis, the presence of bacteria in gall bladder bile (bactibilia), chemical imbalances, increased bilirubin excretion, pH imbalances, and the formation of sludge are some of the factors which lead to the formation of gallstones 5. Less commonly, stones are formed in the intrahepatic biliary tree, termed primary hepatolithiasis, and may lead to choledocholithiasis. Stones that are too large to pass through the ampulla of Vater remain in the distal common bile duct, causing obstructive jaundice that may lead to pancreatitis, hepatitis, or cholangitis.
Risk factors are associated with choledocholithiasis
Factors that may increase your risk of gallstones include:
- Being female
- Being age 40 or older
- Being a Native American
- Being a Hispanic of Mexican origin
- Being overweight or obese
- Being sedentary
- Being pregnant
- Eating a high-fat diet
- Eating a high-cholesterol diet
- Eating a low-fiber diet
- Having a family history of gallstones
- Having diabetes
- Having certain blood disorders, such as sickle cell anemia or leukemia
- Losing weight very quickly
- Taking medications that contain estrogen, such as oral contraceptives or hormone therapy drugs
- Having liver disease
You may be more likely to get a gallstone in your common bile duct if you:
- Have chronic cholangitis. Choledocholithiasis is a major cause of cholangitis, but it can also work the other way around. If you have inflammation in your bile ducts from another cause, it may cause bile to slow and stall in your bile ducts, leading to sedimentation and gallstones.
- Have had gallstones before. Most people with gallstones don’t have complications, but people who’ve had them before are more likely to have them again. Even if you’ve had your gallbladder removed to treat gallstones, rarely, you may still develop new stones in your bile ducts.
Choledocholithiasis can occur in people who have had their gallbladder removed.
You may be more likely to have gallstones in general if you:
- Have high cholesterol. Most (75% of) gallstones are formed from excess cholesterol in your blood. Other bile ingredients (bile salts and lecithin) are supposed to help emulsify the cholesterol, but if there’s an imbalance between them, this doesn’t work.
- Have female hormones. Estrogen increases cholesterol, and progesterone slows gallbladder contractions, which increases sedimentation. Both hormones are higher during certain periods in female reproductive life, and hormone replacement therapy can also elevate them.
Choledocholithiasis pathophysiology
Bile made in the liver and stored in the gallbladder can lead to gallstone formation. In some patients with gallstones, the stones will pass from the gallbladder into the cystic duct and then into the common bile duct (CBD). Most of the choledocholithiasis cases are secondary to the gallstones passage from the gallbladder into the CBD 5. Primary choledocholithiasis which is the formation of stones within the common bile duct (CBD) is seen less commonly. Primary choledocholithiasis occurs in the setting of bile stasis, which results in intraductal stone formation. The size of the bile duct increases with age. Older adults with dilated bile ducts and biliary diverticula are at risk for the formation of primary bile duct stones. Less common sources of choledocholithiasis include complicated Mirizzi syndrome or hepatolithiasis.
Choledocholithiasis prevention
As cholesterol gallstones are the most common type, you may be able to reduce your risk by reducing cholesterol in your blood through dietary and lifestyle changes. Doctors also recommend that you avoid “yo-yo” dieting and lose weight gradually. Losing too quickly can encourage gallstones.
You can reduce your risk of gallstones if you:
- Don’t skip meals. Try to stick to your usual mealtimes each day. Skipping meals or fasting can increase the risk of gallstones.
- Lose weight slowly. If you need to lose weight, go slow. Rapid weight loss can increase the risk of gallstones. Aim to lose 1 or 2 pounds (about 0.5 to 1 kilogram) a week.
- Eat more high-fiber foods. Include more fiber-rich foods in your diet, such as fruits, vegetables and whole grains.
- Maintain a healthy weight. Obesity and being overweight increase the risk of gallstones. Losing weight safely if you are overweight or have obesity. Work to achieve a healthy weight by reducing the number of calories you eat and increasing the amount of physical activity you get. Once you achieve a healthy weight, work to maintain that weight by continuing your healthy diet and continuing to exercise.
Choledocholithiasis signs and symptoms
Choledocholithiasis may cause no signs or symptoms. Unless your gallstones cause a blockage, you may never even know they’re there. If you do have symptoms, it means that a gallstone is blocking your common bile duct. The first sign of a blockage will be the symptoms of biliary colic. These can include 21, 22:
- Abdominal pain. Biliary pain occurs in episodes lasting from one to several hours, usually after a meal. It grows for the first 20 minutes and gradually declines after that. Most people feel it in their upper right abdomen, but it may also radiate to your right side or shoulder blade.
- Nausea and vomiting. Biliary colic is often accompanied by nausea and vomiting. You’ll notice that vomiting doesn’t relieve the pain, as it does with some other types, like migraines. If biliary colic isn’t as intense, you may only notice a general lack of appetite.
- Jaundice. Jaundice is the yellow discoloration of your skin, the whites of your eyes and body fluids. When bile backs up and leaks into your bloodstream, it may show up as a yellow tint to your skin or the whites of your eyes. It may also turn your pee a darker color. Jaundice can come and go, like biliary colic. But it’ll keep coming back until the blockage is cleared.
- Fever. Severe inflammation in your biliary system may cause a fever. Fever may also be a sign of an infection. When your bile ducts are blocked, bacteria aren’t flushed out as usual.
Choledocholithiasis complications
A gallstone that blocks your common bile duct (CBD) will cause bile to back up behind the blockage. This can affect all of the ducts and organs connected to it, including your gallbladder, pancreas and liver. It causes inflammation, breeds infection and can lead to long-term tissue damage.
Choledocholithiasis possible complications include:
- Blockage of the common bile duct. Gallstones can block the ducts through which bile flows from your gallbladder or liver to your small intestine. Severe pain, jaundice and bile duct infection can result.
- Infection. A blocked bile duct is an easy breeding ground for bacterial infections. An infection in your biliary system is very dangerous. It can spread to your liver and your bloodstream. An infection in your bloodstream (septicemia) can lead to life-threatening complications (sepsis).
- Cholangitis. Choledocholithiasis is the most common cause of cholangitis, inflammation and infection of your common bile duct. Backed-up bile causes your bile duct to swell, which further slows the flow of bile. Inflammation and infection can spread from your common bile duct to its branches, including those that run through your liver. It can cause your liver to swell.
- Cholecystitis. Cholecystitis is inflammation in your gallbladder. Bile backing up into your gallbladder will cause it to swell. This is painful and can stop it from functioning well and eventually damages the organ. This is the most common cause of gallbladder disease.
- Gallstone pancreatitis. Your bile ducts share the same exit channel into your intestines as your pancreas. Gallstones that block this common channel can also block secretions from your pancreas. These secretions, which contain very potent enzymes, will back up into your pancreas and cause severe inflammation and organ damage called pancreatitis. Pancreatitis causes intense, constant abdominal pain and usually requires hospitalization. Gallstones obstructing your bile ducts is the most common cause of non-alcohol-related pancreatitis.
- Gallbladder cancer. People with a history of gallstones have an increased risk of gallbladder cancer. But gallbladder cancer is very rare, so even though the risk of cancer is elevated, the likelihood of gallbladder cancer is still very small.
Choledocholithiasis diagnosis
Gallstones in your bile duct usually aren’t discovered unless they cause symptoms. If you have symptoms of biliary colic or jaundice, your doctor will investigate with blood tests and imaging tests. Blood tests will show the buildup of bile, and imaging will find the blockage.
Tests and procedures used to diagnose gallstones and complications of gallstones include:
- Abdominal ultrasound. This test is the one most commonly used to look for signs of gallstones. Abdominal ultrasound involves moving a device (transducer) back and forth across your stomach area. The transducer sends signals to a computer, which creates images that show the structures in your abdomen.
- Endoscopic ultrasound (EUS). Endoscopic ultrasound (EUS) test combines ultrasound technology with an upper endoscopy exam for a clearer picture of your bile ducts. It involves passing a tiny lighted camera on a tube (endoscope) down your throat and into your upper gastrointestinal tract. An ultrasound probe on the end of the endoscope sends out sound waves to produce images of your biliary system. This procedure can help identify smaller stones that may be missed on an abdominal ultrasound.
- Other imaging tests. Additional tests may include:
- Oral cholecystography,
- Hepatobiliary iminodiacetic acid (HIDA) scan,
- Abdominal CT scan,
- Magnetic resonance cholangiopancreatography (MRCP). Magnetic resonance cholangiopancreatography (MRCP) is a type of magnetic resonance imaging (MRI) that specifically visualizes the bile ducts. It’s noninvasive and creates very clear images of your biliary system, including the common bile duct. Your doctor might use this test first to find a suspected gallstone there. But if they’re already pretty sure it’s there, they might go straight to an endoscopic retrograde cholangiopancreatography (ERCP).
- Endoscopic retrograde cholangiopancreatography (ERCP). ERCP (endoscopic retrograde cholangiopancreatography) test is a little more invasive, but it’s a useful one for finding gallstones because it can also be used to remove them. It combines X-rays and endoscopy. When the endoscope reaches the top of your small intestine, your doctor slides another, smaller tube into the first one to reach farther down into your bile ducts. They inject a special dye through the tube and then take video X-rays (fluoroscopy) as the dye travels through your ducts. When they find stones, they can be removed during the ERCP procedure. Doctors can attach special tools to the endoscope to break up and remove the stones when they find them. Sometimes, they make a surgical cut into the muscle of the duct to open it up and allow stones to pass. This is called a sphincterotomy. After removing gallstones from your bile ducts, doctors often recommend surgery to remove your gallbladder (cholecystectomy). This is to prevent more gallstones from exiting your gallbladder and causing choledocholithiasis again.
- Percutaneous transhepatic cholangiogram (PTCA). A percutaneous transhepatic cholangiogram (PTCA) is an x-ray of the bile ducts. This test can help diagnose the cause of a bile duct blockage. Most of the time, percutaneous transhepatic cholangiogram (PTCA) is done after an endoscopic retrograde cholangiopancreatography (ERCP) test has been tried first. The PTCA may be done if an ERCP test cannot be performed or has failed to clear the blockage.
- Blood tests. Blood tests may reveal infection, jaundice, pancreatitis or other complications caused by gallstones. Blood tests may include:
- Complete blood count (CBC).
- Bilirubin test.
- Pancreas enzymes (amylase or lipase).
- Liver function tests.
Choledocholithiasis treatment
Your doctor will determine if treatment for choledocholithiasis is indicated based on your symptoms and the results of diagnostic testing. The goal of treatment is to relieve the blockage. The treatment for choledocholithiasis is the removal of the obstructing stones via endoscopic means.
Choledocholithiasis treatment may involve 17, 18, 19:
- Endoscopic retrograde cholangiopancreatography (ERCP) and a procedure called a sphincterotomy, which makes a surgical cut into the muscle in the common bile duct to allow stones to pass or be removed. Usually after removing gallstones from your bile ducts, doctors often recommend surgery to remove your gallbladder (cholecystectomy). This is to prevent more gallstones from exiting your gallbladder and causing choledocholithiasis again.
- Surgery to remove the gallbladder (cholecystectomy) and stones. Your doctor may recommend surgery to remove your gallbladder, since gallstones frequently recur. Once your gallbladder is removed, bile flows directly from your liver into your small intestine, rather than being stored in your gallbladder. You don’t need your gallbladder to live, and gallbladder removal doesn’t affect your ability to digest food, but it can cause diarrhea, which is usually temporary. A small number of people have softer and more frequent stools after gallbladder removal, because bile now flows into your duodenum more often. Changes in bowel habits are usually temporary; however, discuss them with your doctor.
- Cholecystectomy in patients with choledocholithiasis remains controversial, but most experts recommend it. Arguments can be made against cholecystectomy in patients who cannot tolerate surgery well (eg, due to age, medical problems), as long as the patient is asymptomatic.
- Medications to dissolve gallstones. Oral dissolution therapy such as Ursodiol (Actigall) and chenodiol (Chenix) are medicines that contain bile acids that can break up gallstones. These medicines work best to break up small cholesterol stones. But it may take months or years of treatment to dissolve your gallstones in this way, and gallstones will likely form again if treatment is stopped. Sometimes medications don’t work. Medications for gallstones aren’t commonly used and are reserved for people who can’t undergo surgery.
- Shock wave lithotripsy. A doctor can use shock wave lithotripsy to blast gallstones into small pieces. Doctors use this procedure only rarely, and sometimes along with Ursodiol (Actigall).
Depending on your condition, you may need treatment before your gallstones can be removed, such as:
- Antibiotics to treat infection.
- Biliary drainage to remove backed-up bile.
There are no medications that will cure choledocholithiasis. However, a one-time dose of 50 mg to 100 mg rectal indomethacin can be used to prevent post-procedure pancreatitis if the pancreatic duct was manipulated during an ERCP 5. Antibiotics are typically not needed for choledocholithiasis unless the patient also has associated cholecystitis or cholangitis 5.
Choledocholithiasis prognosis
The prognosis of choledocholithiasis depends on the presence of complications and their severity 5. Approximately 45% of patients with choledocholithiasis remain asymptomatic. Of all patients who refuse surgery or are unfit to undergo surgery, only 55% experience varying degrees of complications 5. Less than 20% of patients experience recurrence of symptoms even after undergoing therapeutic procedures. If treatment is initiated at the right time, the prognosis is deemed favorable under general circumstances 5.
Gallstone types
There are 2 main types of gallstones that can form in your gallbladder:
- Cholesterol gallstones. The most common type of gallstone (80%-98% of gallstones), called a cholesterol gallstone, often appears yellow in color. These gallstones are composed mainly of undissolved cholesterol, but may contain other components. Cholesterol gallstones are not related to cholesterol level in the blood. In most cases, they are not visible on CT scans but are visible on a sonogram (ultrasound) of the abdomen.
- Pigment gallstones (2%-20% of gallstones). These dark brown or black stones form when your bile contains too much bilirubin. Pigment stones occur when red blood cells are destroyed and too much bilirubin is in the bile.
Each stone has a unique set of risk factors. Some risk factors for the development of cholesterol gallstones are obesity, age, female gender, pregnancy, genetics, total parenteral nutrition, rapid weight loss, and certain medications (oral contraceptives, clofibrate, and somatostatin analogs).
Pigment gallstones (black and brown pigment stones) can be found in individuals with high hemoglobin turnover. The pigment consists of mostly bilirubin. Patients with cirrhosis, ileal diseases, sickle cell anemia, and cystic fibrosis are at risk of developing black pigment stones. Brown pigments are mainly found in the Southeast Asian population and are not common in the United States. Risk factors for brown pigment stones are intraductal stasis and chronic colonization of bile with bacteria 23, 24, 25, 26.
What causes gallstones?
Experts don’t know what causes gallstones to form. Doctors think gallstones may result when:
- Your bile contains too much cholesterol. Normally, your bile contains enough chemicals to dissolve the cholesterol excreted by your liver. But if your liver excretes more cholesterol than your bile can dissolve, the excess cholesterol may form into crystals and eventually into stones.
- Your bile contains too much bilirubin. Bilirubin is a chemical that’s produced when your body breaks down red blood cells. Certain conditions cause your liver to make too much bilirubin, including liver cirrhosis, biliary tract infections and certain blood disorders. The excess bilirubin contributes to gallstone formation.
- Your gallbladder doesn’t empty correctly. If your gallbladder doesn’t empty completely or often enough, bile may become very concentrated, contributing to the formation of gallstones.
How do you get gallstones
There are three main pathways in the formation of gallstones 1:
- Cholesterol supersaturation: Normally, bile can dissolve the amount of cholesterol excreted by the liver. But if the liver produces more cholesterol than bile can dissolve, the excess cholesterol may precipitate as crystals. Crystals are trapped in gallbladder mucus, producing gallbladder sludge. With time, the crystals may grow to form stones and occlude the ducts which ultimately produce the gallstone disease.
- Excess bilirubin: Bilirubin, a yellow pigment derived from the breakdown of red blood cells, is secreted into bile by liver cells. Certain hematologic conditions cause the liver to make too much bilirubin through the processing of breakdown of hemoglobin. This excess bilirubin may also cause gallstone formation.
- Gallbladder hypomotility or impaired contractility: If the gallbladder does not empty effectively, bile may become concentrated and form gallstones.
Depending on the cause, gallstones have different compositions. The three most common types are cholesterol gallstones, black pigment gallstones, and brown pigment gallstones. Ninety percent of gallstones are cholesterol gallstones.
Risk factors for developing gallstones
Factors that may increase your risk of gallstones include 20:
- Being female
- Being age 40 or older
- Being a Native American
- Being a Mexican-American
- Being overweight or obese
- Being sedentary
- Being pregnant
- Eating a high-fat diet
- Eating a high-cholesterol diet
- Eating a low-fiber diet
- Having a family history of gallstones
- Having diabetes
- Losing weight very quickly
- Taking medications that contain estrogen, such as oral contraceptives or hormone therapy drugs
- Having liver disease
Who’s at risk of gallstones?
Gallstones are more common if you:
- are female, particularly if you have had children, are taking the combined pill, or are undergoing high-dose oestrogen therapy
- are overweight or obese
- are aged 40 years or older (the older you are, the more likely you are to develop gallstones)
- have a condition that affects the flow of bile (such as cirrhosis, primary sclerosing cholangitis, or obstetric cholestasis)
- have Crohn’s disease or irritable bowel syndrome (IBS)
- have a close family member who’s also had gallstones
- have recently lost weight (from either dieting or weight loss surgery)
- are taking an antibiotic called ceftriaxone
Gallstones prevention
You can reduce your risk of gallstones if you:
- Don’t skip meals. Try to stick to your usual mealtimes each day. Skipping meals or fasting can increase the risk of gallstones.
- Lose weight slowly. If you need to lose weight, go slow. Rapid weight loss can increase the risk of gallstones. Aim to lose 1 or 2 pounds (about 0.5 to 1 kilogram) a week.
- Maintain a healthy weight. Obesity and being overweight increase the risk of gallstones. Work to achieve a healthy weight by reducing the number of calories you eat and increasing the amount of physical activity you get. Once you achieve a healthy weight, work to maintain that weight by continuing your healthy diet and continuing to exercise.
Diet for gallstones
From the limited evidence available, changes to your diet and losing weight (if you’re overweight) may help prevent gallstones. Because cholesterol appears to play a role in the formation of gallstones, it’s advisable to avoid eating too many foods with a high saturated fat content.
Foods high in saturated fat include:
- meat pies
- sausages and fatty cuts of meat
- butter, ghee and lard
- cream
- hard cheeses
- cakes and biscuits
- food containing coconut or palm oil
A healthy, balanced diet is recommended. This includes plenty of fresh fruit and vegetables (at least 5 portions a day) and wholegrains.
There’s also evidence that regularly eating nuts, such as peanuts or cashews, can help reduce your risk of developing gallstones.
Losing weight
Being overweight, particularly being obese, increases the amount of cholesterol in your bile, which increases your risk of developing gallstones.
You should control your weight by eating a healthy diet and taking plenty of regular exercise. But you should avoid low-calorie, rapid weight loss diets. There’s evidence they can disrupt your bile chemistry and increase your risk of developing gallstones.
A more gradual weight loss plan is recommended.
Once you achieve a healthy weight, work to maintain that weight by continuing your healthy diet and continuing to exercise.
Gallstones signs and symptoms
Many people with gallstones do not have any symptoms. Gallstones that do not cause symptoms are called silent gallstones. Silent gallstones don’t stop your gallbladder, liver, or pancreas from working, so they do not need treatment. Gallstones are often found during a routine X-ray, abdominal surgery, or other medical procedure. However, if a gallstone lodges in a duct or tube that drains your gallbladder and causes a blockage, bile could build up in your gallbladder causing a gallbladder attack and you may have a cramping pain in the middle to right upper abdomen. This is known as biliary colic. The pain goes away if the stone passes into the first part of the small intestine.
- Sudden and rapidly intensifying pain in the upper right portion of your abdomen called biliary colic, which is intermittent episodes of constant, sharp, right upper quadrant abdominal pain often associated with nausea and vomiting.
- Sudden and rapidly intensifying pain in the center of your abdomen, just below your breastbone
- Back pain between your shoulder blades
- Pain in your right shoulder
- Sweating, nausea or vomiting may accompany biliary colic (gallstones pain)
Gallstone pain may last several minutes to a few hours. Gallbladder attacks often follow heavy meals and usually occur in the evening or during the night. If you’ve had one gallbladder attack, more attacks will likely follow.
Gallbladder attacks usually stop when gallstones move and no longer block the bile ducts. However, if any of your bile ducts stay blocked for more than a few hours, you may develop gallstone complications. Gallstones that do not block your bile ducts do not cause symptoms.
Gallstones pain
Gallstones can cause sudden, severe abdominal pain that usually lasts 1 to 5 hours, although it can sometimes last just a few minutes. Biliary colic (gallstones pain) is usually caused by the gallbladder contracting in response to some form of stimulation, forcing a stone through the gallbladder into the cystic duct opening, leading to increased gallbladder wall tension and pressure which often result in pain known as biliary colic. As the gallbladder relaxes, the stones often fall back into the gallbladder, and the pain subsides within 30 to 90 minutes.
Gallstones pain can be felt:
- in the center of your abdomen (tummy)
- just under the ribs on your right-hand side – it may spread from here to your side or shoulder blade
The pain is constant and isn’t relieved by going to the toilet, passing wind or being sick.
It’s sometimes triggered by eating fatty foods, but may occur at any time of day and may wake you up during the night.
Biliary colic doesn’t happen often. After an episode of pain, it may be several weeks or months before you have another episode.
Some people also have periods where they sweat excessively and feel sick or vomit.
When gallstones cause episodes of biliary colic, it’s known as uncomplicated gallstone disease.
- Fatty meals are a common trigger for gallbladder contraction. The pain usually starts within an hour after a fatty meal and is often described as intense and dull, and may last from 1 to 5 hours. However, an association with meals is not universal, and in a significant proportion of patients, the pain is nocturnal. The frequency of recurrent episodes is variable, though most patients do not have symptoms on a daily basis.
- A thorough physical exam is useful to distinguish biliary pain due to acute cholecystitis (inflammation of the gallbladder), uncomplicated cholelithiasis or other complications.
- In an uncomplicated biliary colic, the patient is afebrile and has an essentially benign abdominal examination without rebound or guarding.
Acute cholecystitis occurs when persistent gallstone dislodged from the cystic duct causes the gallbladder to become distended and inflamed. The patient may also present with fever, pain in the right upper quadrant and tenderness over the gallbladder (this is known as Murphy’s sign).
When fever, persistent tachycardia (increased or fast heart beat), hypotension (low blood pressure), or jaundice are present, it requires a search for complications of gallstones, including cholecystitis (inflammation of the gallbladder), cholangitis (inflammation of the bile duct and/or liver), pancreatitis (inflammation of the pancreas), or other systemic causes.
Choledocholithiasis is a complication of gallstones when stones obstruct the common bile duct it impedes the flow of bile from the liver to the intestine. Pressure rises resulting in elevation of liver enzymes and jaundice.
Cholangitis is triggered by colonization of bacteria and overgrowth in static bile above an obstructing common duct stone. This produces purulent inflammation of the liver and biliary tree. Charcot’s triad consists of severe right upper quadrant tenderness with fever and jaundice and is classic for cholangitis. Surgical removal of gallstone obstruction with intravenous antibiotics is required to treat this condition.
Other symptoms
Occasionally, gallstones can cause more serious problems if they obstruct the flow of bile for longer periods or move into other organs, such as the pancreas or small bowel.
If this happens, you may develop:
- a high temperature of 100.4 °F (38 °C) or above
- more persistent pain
- a rapid heartbeat
- yellowing of the skin and whites of the eyes (jaundice)
- itchy skin
- diarrhea
- chills or shivering attacks
- confusion
- a loss of appetite
Doctors refer to this more severe condition as complicated gallstone disease.
Gallstones complications
A small number of people with gallstones may develop serious problems if the gallstones cause a severe blockage or move into another part of the digestive system.
Complications of gallstones may include:
Inflammation of the gallbladder (cholecystitis)
A gallstone that becomes lodged in the neck of the gallbladder can cause inflammation of the gallbladder (cholecystitis). If a bile duct becomes permanently blocked, it can lead to a build-up of bile inside the gallbladder. This can cause the gallbladder to become infected and inflamed. The medical term for inflammation of the gallbladder is acute cholecystitis. Acute cholecystitis can cause severe pain and fever.
Acute cholecystitis symptoms include:
- pain in your upper abdomen that travels towards your shoulder blade (unlike biliary colic, the pain usually lasts longer than 5 hours)
- a high temperature (fever) of 100.4 °F (38 °C) or above
- a rapid heartbeat
An estimated 1 in 7 people with acute cholecystitis also experience jaundice.
Acute cholecystitis is usually first treated with antibiotics to settle the infection and then keyhole surgery to remove the gallbladder.
The operation can be more difficult when performed as an emergency, and there’s a higher risk of it being converted to open surgery.
Sometimes a severe infection can lead to a gallbladder abscess (empyema of the gallbladder). Antibiotics alone don’t always treat these and they may need to be drained.
Occasionally, a severely inflamed gallbladder can tear, leading to inflammation of the inside lining of the abdomen (peritonitis).
If this happens, you may need antibiotics given directly into a vein (intravenous antibiotics), and surgery may be required to remove a section of the lining if part of it becomes severely damaged.
Jaundice
You can get jaundice if a gallstone passes out of the gallbladder into the bile duct and blocks the flow of bile.
Symptoms of jaundice include:
- yellowing of the skin and eyes
- dark brown urine
- pale stools
- itching
Sometimes the stone passes from the bile duct on its own. If it doesn’t, the stone needs to be removed.
Blockage of the common bile duct (choledocholithiasis)
Gallstones can block the tubes (ducts) through which bile flows from your gallbladder or liver to your small intestine. Jaundice and bile duct infection can result.
Infection of the bile ducts (acute cholangitis)
If the bile ducts become blocked, they’re vulnerable to infection by bacteria. The medical term for a bile duct infection is acute cholangitis.
Symptoms of acute cholangitis include:
- pain in your upper abdomen that travels towards your shoulder blade
- a high temperature
- jaundice
- chills
- confusion
- itchy skin
- generally feeling unwell
Antibiotics will help treat the infection, but it’s also important to help the bile from the liver to drain with an endoscopic retrograde cholangio-pancreatography (ERCP).
Acute pancreatitis
Acute pancreatitis may develop when a gallstone moves out of the gallbladder and blocks the pancreatic duct (the duct of the pancreas) (see Figure 3 above), causing the pancreas to become inflamed. The pancreatic duct is a tube that runs from the pancreas to the common bile duct. Pancreatic juices, which aid in digestion, flow through the pancreatic duct. A gallstone can cause a blockage in the pancreatic duct, which can lead to inflammation of the pancreas (pancreatitis). Pancreatitis causes intense, constant abdominal pain and usually requires hospitalization.
The most common symptom of acute pancreatitis is a sudden severe dull pain in the center of your upper abdomen, around the top of your stomach.
The pain of acute pancreatitis often gets steadily worse until it reaches a constant ache.
The ache may travel from your abdomen and along your back, and may feel worse after eating.
Leaning forward or curling into a ball may help relieve the pain.
Other symptoms of acute pancreatitis can include:
- feeling sick
- being sick
- diarrhea
- loss of appetite
- a high temperature
- tenderness of the abdomen
- less commonly, jaundice
There’s currently no cure for acute pancreatitis, so treatment focuses on supporting the body’s functions until the inflammation has passed.
This usually involves admission to hospital so you can be given:
- fluids into a vein (intravenous fluids)
- pain relief
- nutritional support
- oxygen through tubes into your nose
With treatment, most people with acute pancreatitis improve within a week and are well enough to leave hospital after 5 to 10 days.
Gallbladder cancer
People with a history of gallstones have an increased risk of gallbladder cancer. But gallbladder cancer is very rare, so even though the risk of cancer is elevated, the likelihood of gallbladder cancer is still very small.
Having a history of gallstones increases your risk of developing gallbladder cancer. About 4 out of 5 people who have cancer of the gallbladder also have a history of gallstones. But people with a history of gallstones have a less than 1 in 10,000 chance of developing gallbladder cancer.
If you have additional risk factors, such as a family history of gallbladder cancer or high levels of calcium inside your gallbladder, it may be recommended that your gallbladder be removed as a precaution, even if your gallstones aren’t causing any symptoms.
The symptoms of gallbladder cancer are similar to those of complicated gallstone disease, including:
- abdominal pain
- a high temperature
- jaundice
Gallbladder cancer can be treated with a combination of surgery, chemotherapy and radiotherapy.
Gallstone ileus
Gallstone ileus is another rare but serious complication of gallstones. It’s where the bowel becomes obstructed by a gallstone.
Gallstone ileus can occur when an abnormal channel, known as a fistula, opens up near the gallbladder. Gallstones are able to travel through the fistula and can block the bowel.
Symptoms of gallstone ileus include:
- abdominal pain
- being sick
- swelling of the abdomen
- constipation
A bowel obstruction requires immediate medical treatment. If it’s not treated, there’s a risk that the bowel could split open (rupture). This could cause internal bleeding and widespread infection.
Contact your doctor as soon as possible if you think you have an obstructed bowel.
Surgery is usually needed to remove the gallstone and unblock the bowel. The type of surgery you have will depend on where the obstruction in the bowel is.
Gallstones diagnosis
Doctors use your medical history, a physical exam, and lab and imaging tests to diagnose gallstones. Your doctor will ask you about your symptoms. He or she will ask if you have a history of health conditions or health concerns that make you more likely to get gallstones. Your doctor also may ask if you have a family history of gallstones and what you typically eat. During a physical exam, your doctor examines your body and checks for pain in your abdomen.
Tests and procedures used to diagnose gallstones and complications of gallstones include:
- Tests to create pictures of your gallbladder. Your doctor may recommend an abdominal ultrasound and a computerized tomography (CT) or magnetic resonance cholangiopancreatography (MRCP) scan to create pictures of your gallbladder. These images can be analyzed to look for signs of gallstones.
- Abdominal ultrasound is the primary modality for diagnosing gallstones. Point-of-care ultrasound has been shown in the hands of trained operators to be as accurate as radiology ultrasound in the detection of gallstones. Abdominal ultrasound involves moving a device (transducer) back and forth across your stomach area. The transducer sends signals to a computer, which creates images that show the structures in your abdomen.
- Endoscopic ultrasound (EUS) is a procedure that can help identify smaller stones that may be missed on an abdominal ultrasound. During endoscopic ultrasound (EUS) your doctor passes a thin, flexible tube (endoscope) through your mouth and through your digestive tract. A small ultrasound device (transducer) in the tube produces sound waves that create a precise image of surrounding tissue.
- Computed tomography (CT) scan. CT scans use a combination of x-rays and computer technology to create images of your pancreas, gallbladder, and bile ducts. CT scans can show gallstones, or complications such as infection and blockage of the gallbladder or bile ducts. However, CT scans also can miss gallstones that you may have.
- Magnetic resonance imaging (MRI). MRI machines use radio waves and magnets to produce detailed images of your organs and soft tissues without x-rays. MRIs can show gallstones in the ducts of the biliary tract.
- Tests to check your bile ducts for gallstones. A test that uses a special dye to highlight your bile ducts on images may help your doctor determine whether a gallstone is causing a blockage. Tests may include a hepatobiliary iminodiacetic acid (HIDA) scan, oral cholecystography or endoscopic retrograde cholangiopancreatography (ERCP).
- Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that combines upper gastrointestinal (GI) endoscopy and x-rays to find and treat problems of the bile and pancreatic ducts. To prepare for ERCP, you will need to talk with your doctor, arrange for a ride home, and avoid eating or drinking before the procedure. Gallstones discovered using endoscopic retrograde cholangiopancreatography (ERCP) can be removed during the procedure.
- Hydroxyl iminodiacetic acid scan (HIDA scan) also called cholescintigraphy or hepatobiliary scan—uses a safe radioactive material to produce pictures of your biliary tract. You’ll lie on a table while a health care professional injects a small amount of the radioactive material into a vein in your arm. The health care professional may also inject a substance that causes your gallbladder to squeeze. A special camera takes pictures of the radioactive material as it moves through your biliary tract. Doctors use cholescintigraphy to diagnose abnormal contractions of your gallbladder or a blockage in the bile ducts.
- Blood tests to look for complications. Blood tests may reveal an infection, jaundice, pancreatitis or other complications caused by gallstones.
Gallstones treatment
Management of gallstones can be divided into two categories: asymptomatic gallstones and symptomatic gallstones.
Asymptomatic gallstones: Most people with gallstones that don’t cause symptoms will never need treatment. Your doctor will determine if treatment for gallstones is indicated based on your symptoms and the results of diagnostic testing. Your doctor may recommend you be alert for symptoms of gallstone complications, such as intensifying pain in your upper right abdomen. If gallstone signs and symptoms occur in the future, you can have treatment.
As a general rule, the longer you go without symptoms, the less likely it is that your condition will get worse.
You may need treatment if you have a condition that increases your risk of developing complications, such as:
- scarring of the liver (cirrhosis)
- high blood pressure inside the liver (this is known as portal hypertension and is often a complication of alcohol-related liver disease)
- diabetes
Treatment may also be recommended if a scan shows high levels of calcium inside your gallbladder, as this can lead to gallbladder cancer in later life.
Gallstones without complications can be treated acutely with oral or parenteral analgesia in emergency department or urgent care center once the diagnosis has been established and alternative diagnoses excluded. Patients should also be offered dietary advice to reduce the chance of recurrent episodes and referred to a general surgeon for elective laparoscopic cholecystectomy. Patients with symptoms and workup consistent with acute cholecystitis will require admission to hospital, surgical consult and intravenous antibiotics. Patients with choledocholithiasis or gallstone pancreatitis will also require admission to hospital, gastrointestinal (GI) consultation and endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). Patients with acute ascending cholangitis are usually ill-appearing and septic. They often also require aggressive resuscitation and ICU-level care in addition to surgical intervention to drain an infection in the biliary tract.
Treatment options for gallstones include:
- Surgery to remove the gallbladder (cholecystectomy). Your doctor may recommend surgery to remove your gallbladder, since gallstones frequently recur. Once your gallbladder is removed, bile flows directly from your liver into your small intestine, rather than being stored in your gallbladder. You don’t need your gallbladder to live, and gallbladder removal doesn’t affect your ability to digest food, but it can cause diarrhea, which is usually temporary.
- Medications to dissolve gallstones. Medications you take by mouth may help dissolve gallstones. But it may take months or years of treatment to dissolve your gallstones in this way and gallstones will likely form again if treatment is stopped. Sometimes medications don’t work. Medications for gallstones aren’t commonly used and are reserved for people who can’t undergo surgery.
How to get rid of gallstones
Medication to dissolve gallstones
If your gallstones are small and don’t contain calcium, it may be possible to take ursodeoxycholic acid tablets to dissolve them.
But these aren’t prescribed very often because:
- they’re rarely very effective
- they need to be taken for a long time (up to 2 years)
- gallstones can recur once treatment is stopped
Side effects of ursodeoxycholic acid are uncommon and are usually mild. The most commonly reported side effects are feeling sick, being sick and itchy skin.
Ursodeoxycholic acid isn’t usually recommended for pregnant or breastfeeding women.
Sexually active women should either use a barrier method of contraception, such as a condom, or a low-dose oestrogen contraceptive pill while taking ursodeoxycholic acid, as it may affect other types of oral contraceptive pills.
Ursodeoxycholic acid tablets may occasionally be used to prevent gallstones if it’s thought you’re at risk of developing them.
For example, ursodeoxycholic acid may be prescribed if you have recently had weight loss surgery, as rapid weight loss can cause gallstones to grow.
Gallstones diet
In the past, people with gallstones who weren’t suitable for surgery were sometimes advised to adopt a very low-fat diet to stop the gallstones growing. But recent evidence suggests this isn’t helpful because rapid weight loss resulting from a very low-fat diet can actually cause gallstones to grow. This means that if surgery isn’t recommended or you want to avoid having an operation, it’s advisable to adopt a healthy, balanced diet. This involves eating a variety of foods, including moderate amounts of fat, and having regular meals.
A healthy diet won’t cure gallstones or completely eliminate your symptoms, but it can improve your general health and help control pain caused by gallstones.
Gallstones natural treatment
A gallbladder cleanse — also called a gallbladder flush or a liver flush — is an alternative remedy for ridding the body of gallstones. However, no scientific evidence suggests that a gallbladder cleanse helps prevent or treat gallstones or any other disease.
In most cases, a gallbladder cleanse involves eating or drinking a combination of olive oil, herbs and some type of fruit juice over the course of two or more days — during which you may be advised to eat nothing else. There’s no standard formula for gallbladder cleansing regimens and products. Different practitioners follow their own recipes.
Proponents of gallbladder cleansing claim that the treatment helps break up gallstones and stimulates the gallbladder to release them in stool. The large, repeated doses of olive oil in gallbladder cleanse preparations do have a laxative effect. And people who have taken a gallbladder cleanse report finding lumps that look like gallstones in their stool just after the procedure. When analyzed, though, these lumps turn out to be composed of oil, juice and other materials.
Gallbladder cleansing is not without risk. Some people have nausea, vomiting, diarrhea and abdominal pain during the flushing or cleansing period. Individual components of the herbal mixtures used in a gallbladder cleanse may present their own health hazards.
Gallstones that cause no symptoms typically require no treatment. If you have gallstones that require treatment, discuss proven treatment options with your doctor, such as surgical removal, bile salt tablets or sound wave therapy.
Is there a diet after gallbladder removal?
After having their gallbladder removed (cholecystectomy), some people develop frequent loose, watery stools. In most cases, the diarrhea lasts no more than a few weeks to a few months. There isn’t a specific gallbladder removal diet that you should follow if you have this problem, but there are a few things you might consider.
First, it helps to understand why you’re having diarrhea. Diarrhea after gallbladder removal seems to be related to the release of bile directly into the intestines. Normally, the gallbladder collects and concentrates bile, releasing it when you eat to aid the digestion of fat. When the gallbladder is removed, bile is less concentrated and drains more continuously into the intestines, where it can have a laxative effect.
The amount of fat you eat at one time also plays a role. Smaller amounts of fat are easier to digest, while larger amounts can remain undigested and cause gas, bloating and diarrhea.
Although there isn’t a set gallbladder removal diet, the following tips may help minimize problems with diarrhea after you’ve had your gallbladder out:
- Go easy on the fat. Avoid high-fat foods, fried and greasy foods, and fatty sauces and gravies for at least a week after surgery. Instead, choose fat-free or low-fat foods. Low-fat foods are those with no more than 3 grams of fat a serving. Check labels and follow the serving size listed.
- Increase the fiber in your diet. This can help normalize bowel movements. Add soluble fiber, such as oats and barley, to your diet. But be sure to increase the amount of fiber slowly, such as over several weeks, because too much fiber at first can make gas and cramping worse.
- Eat smaller, more-frequent meals. This may ensure a better mix with available bile. A healthy meal should include small amounts of lean protein, such as poultry, fish or fat-free dairy, along with vegetables, fruits and whole grains.
You may also try limiting foods that tend to worsen diarrhea, including:
- Caffeine
- Dairy products
- Very sweet foods
Talk with your doctor if your diarrhea doesn’t gradually go away or becomes more severe, or if you lose weight and become weak. Your doctor may recommend medicines, such as loperamide (Imodium A-D), which slows down intestinal movement, or medications that decrease the laxative effect of bile, such as cholestyramine (Prevalite). Your doctor may also suggest that you take a multivitamin to compensate for malabsorption of fat-soluble vitamins.
Gallstones treatment without surgery
Doctors use gallstones treatment without surgery only in special situations, like if you have cholesterol stones and you have a serious medical condition that prevents surgery. Even with treatment, gallstones can return. Therefore, you may have to be regularly treated for gallstones for a very long time, or even for the rest of your life.
A doctor may use the following types of nonsurgical treatments to remove or break up cholesterol gallstones:
- Endoscopic retrograde cholangiopancreatography (ERCP). Sometimes doctors use ERCP to remove a gallstone that is stuck in the common bile duct.
- Oral dissolution therapy. Ursodiol (Actigall) and chenodiol (Chenix) are medicines that contain bile acids that can break up gallstones. These medicines work best to break up small cholesterol stones. You may need months or years of treatment to break up all stones.
- Shock wave lithotripsy. A doctor can use shock wave lithotripsy to blast gallstones into small pieces. Doctors use this procedure only rarely, and sometimes along with ursodiol.
Diet for gallbladder stones
You can lower your risk of gallstones by following a healthy eating plan and getting regular physical activity to help you reach and maintain a healthy weight.
Experts recommend the following to help prevent gallstones:
- Eat more foods that are high in fiber, such as
- fruits, vegetables, beans, and peas.
- whole grains, including brown rice, oats, and whole wheat bread.
- Eat fewer refined carbohydrates and less sugar.
- Eat healthy fats, like fish oil and olive oil, to help your gallbladder contract and empty on a regular basis.
- Avoid unhealthy fats, like those often found in desserts and fried foods.
Talk with your family doctor before you make any changes to your eating plan. Losing weight too quickly may cause health problems. Very low-calorie diets and weight-loss surgery, also called metabolic and bariatric surgery, can lead to rapid weight loss and raise your risk of gallstones.
Gallstones surgery
Surgery to remove the gallbladder, called cholecystectomy, is one of the most common operations performed on adults in the United States. The gallbladder is not an essential organ, which means you can live normally without a gallbladder. A doctor will usually give you general anesthesia for surgery. Once the surgeon removes your gallbladder, bile flows out of your liver through the hepatic duct and common bile duct and directly into the duodenum, instead of being stored in the gallbladder.
Surgeons perform 2 types of cholecystectomy:
- Laparoscopic cholecystectomy. Almost all surgeons perform cholecystectomies with laparoscopy. Surgeons perform many laparoscopic cholecystectomies on an outpatient basis, meaning you may be able to go home the same day. You will probably be able to return to normal physical activity in about a week.
- Open cholecystectomy. A surgeon performs an open cholecystectomy when your gallbladder is severely inflamed, infected, or scarred from other operations. Your doctor may perform a cholecystectomy if problems occur during a laparoscopic cholecystectomy. After the surgery, you may need to stay in the hospital for up to a week. You will probably be able to return to normal physical activity after about a month.
What happens after gallbladder removal (cholecystectomy)?
A small number of people have softer and more frequent stools after gallbladder removal (cholecystectomy), because bile now flows into your duodenum more often. Changes in bowel habits are usually temporary; however, discuss them with your doctor.
All surgeries come with a possible risk of complications; however, gallbladder surgery complications are very rare. The most common complication is injury to the bile ducts, which can cause infection. You may need one or more additional operations to repair the bile ducts.
Gallstones prognosis
Data suggest that only 50% of patients with gallstones develop symptoms 1. The death rate following elective laparoscopic cholecystectomy is less than 1% 1. However, emergency cholecystectomy (surgery to remove the gallbladder) is associated with high mortality rates. Other problems include stones in the bile duct after surgery, incisional hernia, and injury to the bile duct. A few percentages of patients develop post-cholecystectomy pain.
- Tanaja J, Lopez RA, Meer JM. Cholelithiasis. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470440[↩][↩][↩][↩][↩][↩][↩]
- Portincasa P, Wang DQ-H. Gallstones. In: Podolsky, DK, Camilleri M, Fitz JG, Kalloo, AN, Shanahan F, Wang, TC, eds. Yamada’s Textbook of Gastroenterology. Volume 2. 6th edition. Hoboken, NJ: Wiley-Blackwell; 2015:1808–1834.[↩]
- Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014 Jun 24;129(25 Suppl 2):S102-38. doi: 10.1161/01.cir.0000437739.71477.ee. Epub 2013 Nov 12. Erratum in: Circulation. 2014 Jun 24;129(25 Suppl 2):S139-40.[↩]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: U.S. Department of Health and Human Services; 2019. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf[↩]
- McNicoll CF, Pastorino A, Farooq U, et al. Choledocholithiasis. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441961[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Molvar C, Glaenzer B. Choledocholithiasis: Evaluation, Treatment, and Outcomes. Semin Intervent Radiol. 2016 Dec;33(4):268-276. doi: 10.1055/s-0036-1592329[↩]
- Aleknaite A, Simutis G, Stanaitis J, Valantinas J, Strupas K. Risk assessment of choledocholithiasis prior to laparoscopic cholecystectomy and its management options. United European Gastroenterol J. 2018 Apr;6(3):428-438. doi: 10.1177/2050640617731262[↩]
- Choledocholithiasis. https://medlineplus.gov/ency/article/000274.htm[↩]
- Virgile J, Marathi R. Cholangitis. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558946[↩]
- Lan Cheong Wah D, Christophi C, Muralidharan V. Acute cholangitis: current concepts. ANZ J Surg. 2017 Jul;87(7-8):554-559. doi: 10.1111/ans.13981[↩]
- Viriyaroj V, Rookkachart T. Predictive Factors for Choledocholithiasis in Symptomatic Gallstone Patients. J Med Assoc Thai. 2016 Nov;99 Suppl 8:S112-S117.[↩]
- Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999 Sep;117(3):632-9. doi: 10.1016/s0016-5085(99)70456-7[↩]
- Duncan CB, Riall TS. Evidence-based current surgical practice: calculous gallbladder disease. J Gastrointest Surg. 2012 Nov;16(11):2011-25. doi: 10.1007/s11605-012-2024-1[↩]
- Jinfeng Z, Yin Y, Chi Z, Junye G. Management of impacted common bile duct stones during a laparoscopic procedure: A Retrospective Cohort Study of 377 Consecutive Patients. Int J Surg. 2016 Aug;32:1-5. doi: 10.1016/j.ijsu.2016.06.006[↩]
- van Dijk AH, de Reuver PR, Besselink MG, van Laarhoven KJ, Harrison EM, Wigmore SJ, Hugh TJ, Boermeester MA. Assessment of available evidence in the management of gallbladder and bile duct stones: a systematic review of international guidelines. HPB (Oxford). 2017 Apr;19(4):297-309. doi: 10.1016/j.hpb.2016.12.011[↩]
- European Association for the Study of the Liver (EASL). Electronic address: [email protected]. EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016 Jul;65(1):146-181. doi: 10.1016/j.jhep.2016.03.005[↩][↩]
- Parikh MP, Gupta NM, Thota PN, Lopez R, Sanaka MR. Temporal trends in utilization and outcomes of endoscopic retrograde cholangiopancreatography in acute cholangitis due to choledocholithiasis from 1998 to 2012. Surg Endosc. 2018 Apr;32(4):1740-1748. doi: 10.1007/s00464-017-5856-7.[↩][↩]
- de Clemente Junior CC, Bernardo WM, Franzini TP, Luz GO, Dos Santos MEL, Cohen JM, de Moura DTH, Marinho FRT, Coronel M, Sakai P, de Moura EGH. Comparison between endoscopic sphincterotomy vs endoscopic sphincterotomy associated with balloon dilation for removal of bile duct stones: A systematic review and meta-analysis based on randomized controlled trials. World J Gastrointest Endosc. 2018 Aug 16;10(8):130-144. doi: 10.4253/wjge.v10.i8.130[↩][↩]
- Benites Goñi HE, Palacios Salas FV, Asencios Cusihuallpa JL, Aguilar Morocco R, Segovia Valle NS. Rendimiento de los criterios predictivos de la ASGE en el diagnóstico de coledocolitiasis en el Hospital EdgardoRebagliati Martins [Performance of ASGE predictive criteria in diagnosis of choledocholithiasis in the Edgardo Rebagliati Martins Hospital]. Rev Gastroenterol Peru. 2017 Apr-Jun;37(2):111-119. Spanish.[↩][↩]
- Gallstones. https://www.mayoclinic.org/diseases-conditions/gallstones/symptoms-causes/syc-20354214[↩][↩]
- Frybova B, Drabek J, Lochmannova J, Douda L, Hlava S, Zemkova D, Mixa V, Kyncl M, Zeman L, Rygl M, Keil R. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS One. 2018 May 15;13(5):e0196475. doi: 10.1371/journal.pone.0196475[↩]
- Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care. 2017 Dec;44(4):575-597. doi: 10.1016/j.pop.2017.07.002[↩]
- Chung AY, Duke MC. Acute Biliary Disease. Surg Clin North Am. 2018 Oct;98(5):877-894. doi: 10.1016/j.suc.2018.05.003[↩]
- Yoo KS. [Management of Gallstone]. Korean J Gastroenterol. 2018 May 25;71(5):253-259. Korean. doi: 10.4166/kjg.2018.71.5.253[↩]
- Rebholz C, Krawczyk M, Lammert F. Genetics of gallstone disease. Eur J Clin Invest. 2018 Jul;48(7):e12935. doi: 10.1111/eci.12935[↩]
- Ibrahim M, Sarvepalli S, Morris-Stiff G, Rizk M, Bhatt A, Walsh RM, Hayat U, Garber A, Vargo J, Burke CA. Gallstones: Watch and wait, or intervene? Cleve Clin J Med. 2018 Apr;85(4):323-331. doi: 10.3949/ccjm.85a.17035[↩]