Contents
- Gastroesophageal reflux disease
- Gastroesophageal reflux disease causes
- Gastroesophageal reflux disease pathophysiology
- Gastroesophageal reflux disease prevention
- Gastroesophageal reflux disease symptoms
- Gastroesophageal reflux disease complications
- Gastroesophageal reflux disease diagnosis
- Gastroesophageal reflux disease differential diagnosis
- Gastroesophageal reflux disease treatments
- Gastroesophageal reflux disease diet
Gastroesophageal reflux disease
Gastroesophageal reflux disease also called GERD, gastro-oesophageal reflux disease (GORD), acid reflux or heartburn, is a condition that develops when there is a backward flow or reflux of stomach contents (acid from the food and liquid in your stomach) back up into your throat and esophagus causing troublesome symptoms and/or complications 1, 2, 3, 4, 5. Gastroesophageal reflux disease can present as non-erosive reflux disease or erosive esophagitis. It can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux.
The main symptoms of gastroesophageal reflux disease (GERD) are:
- Heartburn – a burning sensation in the middle of your chest, usually after eating, which might be worse after eating, when lying down or when bending over.
- An unpleasant sour taste in your mouth, caused by stomach acid
You may also have:
- Cough or hiccups that keep coming back
- Hoarse voice
- Bad breath
- Bloating and feeling sick
If you have nighttime acid reflux, you might also experience:
- An ongoing cough
- Inflammation of the vocal cords (laryngitis)
- New or worsening asthma
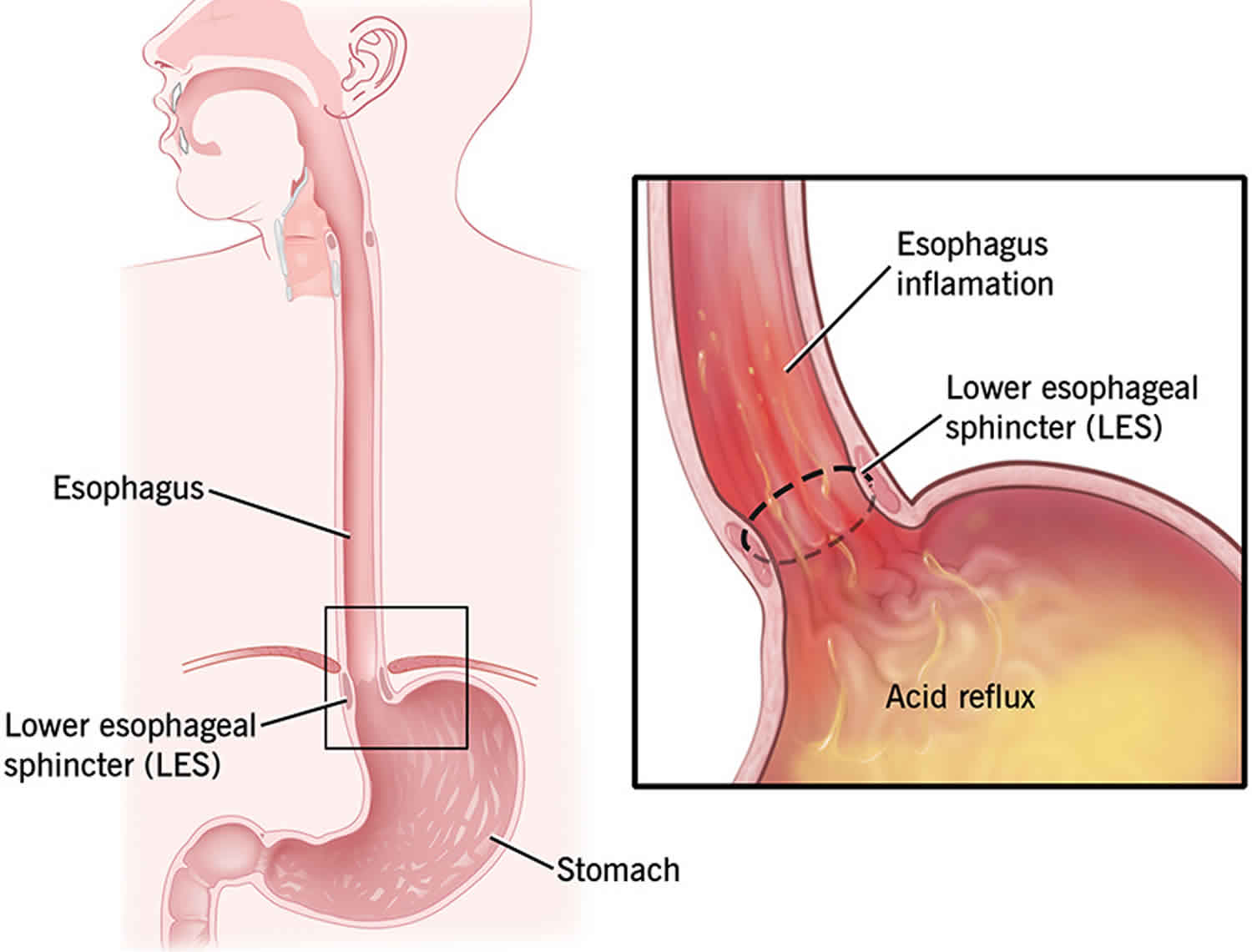
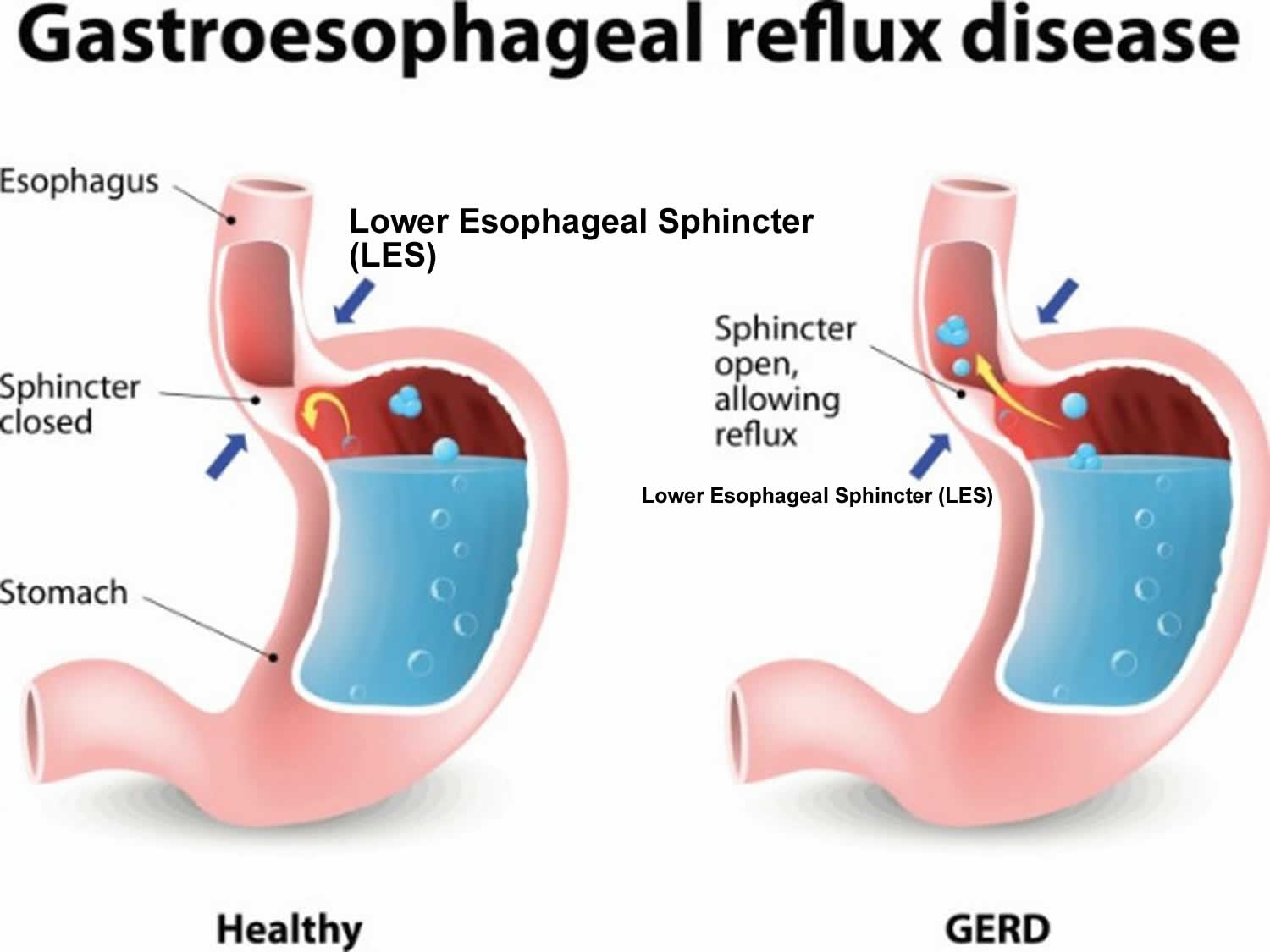
Gastroesophageal reflux disease is caused by a weakened muscle at the end of your esophagus where it connects to your stomach called the lower esophageal sphincter (LES). The lower esophageal sphincter (LES) muscle doesn’t close properly, which allows acid to back up into your throat. Typically, when food is swallowed, the lower esophageal sphincter (a band of muscle around the bottom of the esophagus) relaxes to allow food and liquid to flow down into the stomach. Then the muscle tightens again. If the lower esophageal sphincter isn’t working as it should, stomach acid can flow back up into the esophagus (acid reflux) and cause heartburn. The acid backup may be worse when you’re bent over or lying down.
Sometimes gastroesophageal reflux disease is caused or made worse by:
- certain food and drink – such as coffee, tomatoes, alcohol, chocolate and fatty or spicy foods
- being overweight
- smoking
- pregnancy
- stress and anxiety
- an increase in some types of hormones, such as progesterone and estrogen
- taking certain medicines such as anti-inflammatory painkillers like ibuprofen
- a hiatus hernia – when part of your stomach moves up into your chest
- a stomach ulcer
- a bacterial infection in your stomach
In the United States, 20% of the population experience gastroesophageal reflux disease-related symptoms weekly and 7% daily 6, 7. The prevalence of gastroesophageal reflux disease is slightly higher in men compared to women 8. Several studies have demonstrated that patients with gastroesophageal reflux disease (GERD) have reduced health-related quality of life and work productivity 9.
The danger of untreated gastroesophageal reflux disease (GERD) is that it can cause health problems such as inflammation of the esophagus (esophagitis), which is a risk factor for esophageal cancer. Gastroesophageal reflux disease (GERD) also may lead to breathing problems such as asthma, fluid in the lungs, chest congestion, as well as damaging teeth.
Not everyone who has an episode of acid reflux has gastroesophageal reflux disease (GERD). Your doctor may have you undergo testing to see if you have gastroesophageal reflux disease (GERD). Such tests could include:
- Ambulatory acid (pH) probe test: This test measures the acid in your stomach for 24 hours. Your doctor will insert a small, thin tube into your nose and down into your throat. The tube is connected to a small computer you strap around your waist. Another version of this involves a small probe placed in your throat. The probe transmits a signal for a period of time. After 2 days, the probe falls off and is passed in your stool.
- X-ray of the upper digestive system: The X-ray will look at the inside your upper digestive system (throat, stomach, and upper intestine). For this test, you will you be given a chalky liquid to swallow. This liquid coats your digestive tract to provide better views of the inside.
- Endoscopy or gastroscopy: This is where a thin tube with a camera inside it is passed down your throat and into your stomach. This allows your doctor to look inside your upper digestive tract. He or she may also take a sample of the tissue inside your tract for further testing, for example, tests to check for bacteria that can cause heartburn
- Esophageal motility test (manometry): This test measures the movement and pressure of your esophagus. It involves inserting small, thin tube through your nose and down your throat.
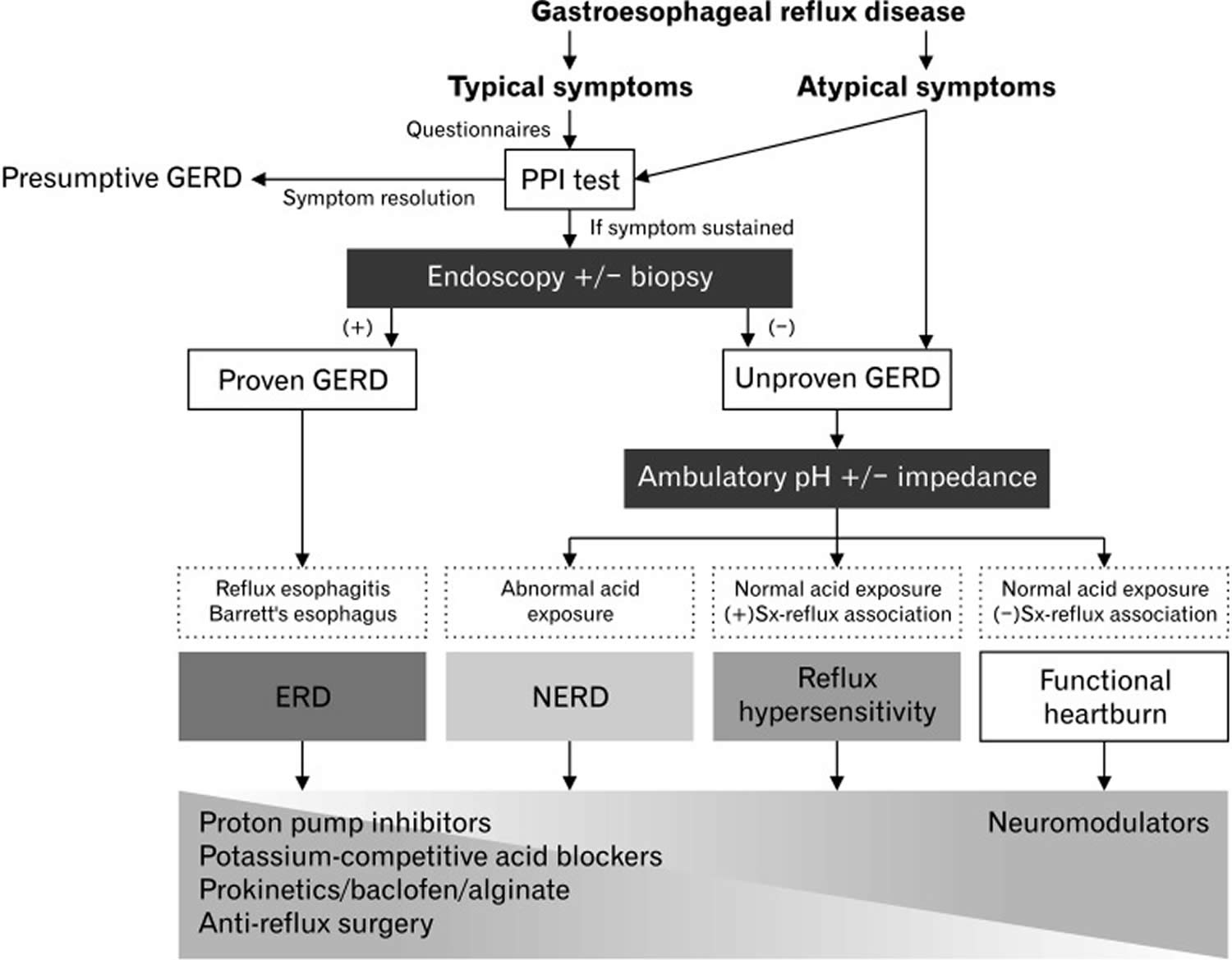
Based on endoscopic and histopathologic appearance, gastroesophageal reflux disease (GERD) is classified into three different types 10:
- Non-erosive reflux disease (NERD). Non-erosive reflux disease (NERD) is a subcategory of gastroesophageal reflux disease (GERD). It is characterized by troublesome reflux symptoms with abnormally increased gastroesophageal reflux observed on 24-hour ambulatory pH-impedance monitoring in the absence of esophageal mucosal injury confirmed on endoscopy.
- Erosive esophagitis. Erosive esophagitis is characterized by erosions or ulcers of the esophageal mucosa 11. Patients may be asymptomatic or can present with worsening symptoms of gastroesophageal reflux disease (GERD). The degree of esophagitis is endoscopically graded using the Los Angeles esophagitis classification system, which employs the A, B, C, D grading system based on variables that include length, location, and circumferential severity of mucosal breaks in the esophagus 12.
- Barrett’s esophagus. Barrett’s esophagus occurs as a result of chronic pathological acid exposure to the distal esophageal mucosa. It leads to a histopathological change of the distal esophageal mucosa, which is normally lined by stratified squamous epithelium to metaplastic columnar epithelium. Barrett’s esophagus is more commonly seen in Caucasian males above 50 years, obesity, and history of smoking and predisposes to the development of esophageal adenocarcinoma 11. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 13.
Non-erosive reflux disease (NERD) is the most prevalent type seen in 60-70% of patients followed by erosive esophagitis and Barrett’s esophagus seen in 30% and 6-12% of patients with gastroesophageal reflux disease (GERD), respectively 10, 9, 14.
If you have acid reflux, your doctor may prescribe a medicine called a proton pump inhibitor (PPI) or H-2 receptor blockers (Histamine-2 Receptor Antagonists) that reduces how much acid your stomach makes. You’ll usually need to take this type of medicine for 4 or 8 weeks, depending on how serious your acid reflux is.
Go back to your doctor if your symptoms return after stopping your medicine. You may need a long-term prescription.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Figure 1. Gastroesophageal reflux disease causes
Figure 2. Gastroesophageal reflux disease diagnostic algorithm
Chest pain may be a symptom of a heart attack. Seek immediate medical care if you have severe chest pain or pressure, especially when combined with pain in the arm or jaw or difficulty breathing. These may be signs and symptoms of a heart attack.
Make an appointment with your doctor if:
- Heartburn occurs more than twice a week
- Symptoms persist despite use of nonprescription medications
- Take over-the-counter medications for heartburn more than twice a week
- Experience severe or frequent gastroesophageal reflux disease (GERD) symptoms
- You have difficulty swallowing
- You have persistent nausea or vomiting
- You have weight loss because of poor appetite or difficulty eating
Is acid reflux the same as gastroesophageal reflux disease (GERD)?
Acid reflux and gastroesophageal reflux disease (GERD) are closely related, but the terms don’t necessarily mean the same thing.
Gastroesophageal reflux disease (GERD) is defined as “a condition that develops when the reflux of stomach contents into the esophagus causes troublesome symptoms and/or complications” 16. The Montreal Definition of gastroesophageal reflux disease (GERD) encapsulates most complications from patients with reflux esophagitis with or without symptoms (the latter actually accounting for close to 40% of such patients in Western populations, and possibly a much higher proportion in Asian populations) to those with symptoms but no other findings 17, 18. The most common symptom of gastroesophageal reflux disease (GERD) is frequent heartburn — two or more times a week. Other symptoms can include regurgitation of food or sour liquid, difficulty swallowing, coughing, wheezing, and chest pain — especially while lying down at night.
Acid reflux also known as gastroesophageal reflux (GER) is the backward flow of stomach acid into the tube that connects your throat to your stomach called the esophagus. During an episode of acid reflux, you might feel a burning sensation in your chest, commonly called heartburn. This can happen after eating a big meal or drinking coffee or alcohol.
Sometimes acid reflux progresses to gastroesophageal reflux disease (GERD), a more severe form of acid reflux.
Can acid reflux be prevented or avoided?
There are many lifestyle changes you can make to reduce or eliminate acid reflux, including:
- Not drinking alcohol
- Not eating too close to bedtime
- Losing weight
- Not wearing tight clothing
- Cutting back on foods known to trigger gastroesophageal reflux disease (GERD), such as chocolate, caffeine, peppermints, and greasy, spicy, and acidic foods
- Eating smaller meals or avoiding overeating
Gastroesophageal reflux disease causes
Currently, there is no known cause to explain the development of gastroesophageal reflux disease 5. Over the years, several risk factors have been identified and implicated in the pathogenesis of gastroesophageal reflux disease 19. Gastroesophageal reflux disease is caused by frequent acid reflux or reflux of nonacidic content from the stomach. When you swallow, a circular band of muscle around the bottom of your esophagus called the lower esophageal sphincter relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again. If the lower esophageal sphincter does not relax as it should or it weakens, stomach acid can flow back into your esophagus. This constant backwash of acid irritates the lining of your esophagus, often causing it to become inflamed.
A meta-analysis by Hampel H et al. 20 concluded that obesity was associated with an increased risk of developing gastroesophageal reflux disease (GERD) symptoms, erosive esophagitis, and esophageal cancer. The study by Malfertheiner et al. 21 evaluated the predictive factors for erosive reflux disease in more than 6000 patients with GERD and noted that the odds ratio for the erosive disease increased with the body mass index (BMI). Several other risk factors have been independently associated with the development of GERD symptoms that include age ≥50 years, low socioeconomic status, tobacco use, consumption of excess alcohol, connective tissue disorders, pregnancy, postprandial supination, and different classes of drugs which include anticholinergic drugs, benzodiazepines, NSAID or aspirin use, nitroglycerin, albuterol, calcium channel blockers, antidepressants, and glucagon 22, 23, 4.
Risk factors for gastroesophageal reflux disease
The following factors can lead to the onset of gastroesophageal reflux disease or aggravate acid reflux:
- Certain diseases, such as Zollinger-Ellison syndrome or scleroderma.
- Increased abdominal pressure due to obesity or pregnancy.
- Increased production of gastrin, a hormone that regulates the release of stomach acid.
- Hiatal hernia, a condition where the upper part of the stomach moves up into the chest through an opening in the diaphragm. This condition lowers the pressure in the esophageal sphincter.
- Certain medications, including asthma medicine, calcium channel blockers, antihistamines, painkillers, sedatives, and antidepressants.
- Certain foods and beverages, such as fried, spicy, or fatty foods, chocolate, peppermint, coffee, or alcoholic beverages.
- Smoking or inhaling second-hand smoke.
- Delayed stomach emptying.
Factors that can aggravate acid reflux include:
- Smoking
- Eating large meals or eating late at night
- Eating certain foods (triggers) such as fatty or fried foods
- Drinking certain beverages, such as alcohol or coffee
- Taking certain medications, such as aspirin, ibuprofen and naproxen.
Gastroesophageal reflux disease pathophysiology
The pathophysiology of gastroesophageal reflux disease is multifactorial and is best explained by various mechanisms involved including the influence of the tone of the lower esophageal sphincter, the presence of a hiatal hernia, esophageal mucosal defense against the refluxate and esophageal motility.
Impaired Lower Esophageal Sphincter (LES) Function
The lower esophageal sphincter (LES) is a 3-4 cm tonically contracted smooth muscle segment located at the esophagogastric junction (EGJ) and, along with the crural diaphragm forms the physiological esophagogastric junction (EGJ) barrier, which prevents the retrograde migration of acidic gastric contents into the esophagus 24. In otherwise healthy individuals, lower esophageal sphincter (LES) maintains a high-pressure zone above intragastric pressures with transient relaxation of the lower esophageal sphincter that occurs physiologically in response to a meal facilitating the passage of food into the stomach. Patients with symptoms of gastroesophageal reflux disease may have frequent transient lower esophageal sphincter relaxations (TLESRs) not triggered by swallowing, resulting in exceeding the intragastric pressure more than lower esophageal sphincter pressures permitting reflux of gastric contents into the esophagus 25. The exact mechanism of increased transient relaxation is unknown, but transient lower esophageal sphincter relaxations (TLESRs) account for 48-73% of gastroesophageal reflux disease symptoms 26. The lower esophageal sphincter (LES) tone and transient lower esophageal sphincter relaxations (TLESRs) are influenced by factors such as alcohol use, smoking, caffeine, pregnancy, certain medications like nitrates, and calcium channel blockers 25.
Hiatal hernia
Hiatal hernia is frequently associated with gastroesophageal reflux disease and can exist independently without causing any symptoms. The presence of hiatal hernia plays a vital role in the pathogenesis of gastroesophageal reflux disease as it hinders the lower esophageal sphincter (LES) function 27. Patti et al. 28 reported that patients with proven gastroesophageal reflux disease with or without a small hiatal hernia had similar lower esophageal sphincter (LES) function abnormalities and acid clearance. However, patients with large hiatal hernias were noted to have shorter and weaker lower esophageal sphincter (LES) resulting in increased reflux episodes. It was also pointed out that the degree of esophagitis was worse in patients with large hiatal hernias 28. A study evaluating the relationship between hiatal hernia and reflux esophagitis by Ott et al. 29 demonstrated the presence of hiatal hernia in 94% of patients with reflux esophagitis.
Impaired esophageal mucosal defense against the gastric refluxate
The esophageal mucosa comprises various structural and functional constituents that function as a protective defense barrier against the luminal substances encountered with gastroesophageal reflux disease25. This defensive barrier can be breached by prolonged exposure to the refluxate, which consists of both acidic gastric contents (hydrochloric acid and pepsin) and alkaline duodenal contents (bile salts and pancreatic enzymes) leading to mucosal damage. The influence of gastroparesis on gastroesophageal reflux disease is unknown. It is believed that delayed gastric emptying contributes to gastroesophageal reflux disease symptoms due to gastric distention and increased exposure to the gastric refluxate 25.
Defective esophageal peristalsis
Normally, the acidic gastric contents that reach the esophagus are cleared by frequent esophageal peristalsis and neutralized by salivary bicarbonate 25, 30. In a prospective study by Diener et al. 31, 21% of patients with gastroesophageal reflux disease were noted to have impaired esophageal peristalsis leading to decreased clearance of gastric reflux resulting in severe reflux symptoms and mucosal damage.
Gastroesophageal reflux disease prevention
There are ways to prevent gastroesophageal reflux disease and acid reflux. To start, you need to know your body and how it reacts to different food and drinks. Spicy and acidic foods and carbonated drinks can trigger acid reflux. Try to avoid those things when possible. Eat smaller meals throughout the day, and don’t eat too late at night. Don’t lie down too soon after eating. Limit the use of alcohol. If you use tobacco, try to quit. Stress and lack of sleep also can worsen symptoms.
There are many dietary and lifestyle changes you can make to reduce or eliminate acid reflux, including:
- Not drinking alcohol
- Not smoking
- Avoid these foods and drinks that are commonly known to be heartburn triggers
- Fried foods
- Fast foods
- Pizzas
- Potato chips and other processed snacks
- Chili powder and pepper (white, black, cayenne)
- Fatty meats such as bacon and sausage
- Cheese
- Alcohol
- Carbonated beverages
- Caffeine
- Acidic foods
- Peppermints
- Not eating too close to bedtime
- Losing weight
- Not wearing tight clothing
- Eating smaller meals or avoiding overeating
Foods that help prevent acid reflux
Ginger is one of the best digestive aids because of its medicinal properties. Ginger is alkaline in nature and anti-inflammatory, which eases irritation in the digestive tract. Try sipping ginger tea when you feel heartburn coming on.
High-fiber foods
Fibrous foods make you feel full so you’re less likely to overeat, which may contribute to heartburn. So, load up on healthy fiber from these foods:
- Whole grains such as oatmeal, couscous and brown rice.
- Root vegetables such as sweet potatoes, carrots and beets.
- Green vegetables such as asparagus, broccoli and green beans.
Alkaline foods
Foods that have a low pH are acidic and more likely to cause reflux. Those with higher pH are alkaline and can help offset strong stomach acid. Alkaline foods include:
- Bananas
- Melons
- Cauliflower
- Fennel
- Nuts
Watery foods
Eating foods that contain a lot of water can dilute and weaken stomach acid. Choose foods such as:
- Celery
- Cucumber
- Lettuce
- Watermelon
- Broth-based soups
- Herbal tea
Gastroesophageal reflux disease symptoms
The main symptom of gastroesophageal reflux disease (GERD) is heartburn, often described as a burning feeling in the back of your throat, in the middle of your chest, or behind the sternum (breastbone), and regurgitating sour or bitter liquid to the throat or mouth 5, 11. The combination of heartburn and regurgitation is such a common characteristic of gastroesophageal reflux disease (GERD) that formal testing may be unnecessary 32.
Other symptoms of gastroesophageal reflux disease include 33, 34, 16:
- An acid taste in your mouth.
- A dry cough, asthma, and difficulty swallowing (these may occur without the burning sensation)
- Excessive saliva and a sore throat that doesn’t go away
You may also have:
- Non-burning chest pain, which is usually located in the middle of the chest and radiates to the back
- Difficulty swallowing (dysphagia)
- Atypical reflux symptoms relating to the throat, larynx or lungs:
- Sore throat
- Coughing or hiccups that keep coming back
- Increased salivation
- Shortness of breath
- A hoarse voice
- Bad breath
- Bloating and feeling sick
Symptoms are often worse after eating, when lying down or when bending over.
Gastroesophageal reflux disease complications
Gastroesophageal reflux disease can sometimes lead to the following complications:
- Swelling of the vocal cords, also known as reflux laryngitis
- Inflammation of the tissue in the esophagus (esophagitis). Stomach acid can break down tissue in the esophagus, causing inflammation, bleeding, and sometimes an open sore (ulcer). Esophagitis can cause pain and make swallowing difficult.
- Narrowing of the esophagus (esophageal stricture), caused by scar tissues that develop due to repeated ulcerations. Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing. American College of Gastroenterology guidelines recommend esophageal dilation and continue proton pump inhibitor (PPI) therapy to prevent the need for repeated dilations 35.
- Barrett’s esophagus, a precancerous changes to the esophagus tissue caused by long-lasting gastroesophageal reflux disease which increases the risk of esophageal cancer. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 13.
- Lung damage which may include pulmonary fibrosis and bronchiectasis
- Ulcers in the esophagus, caused by burning from stomach acid.
Gastroesophageal reflux disease diagnosis
A diagnosis of gastroesophageal reflux disease (GERD) starts with a thorough medical history during which you describe your signs and symptoms and physical examination. If the typical symptoms of acid reflux disease are present, including heartburn and regurgitation, your doctor may begin treatment without performing specific diagnostic tests.
However, tests may be performed if:
- Your symptoms are atypical
- The severity of acid reflux raises concerns about esophageal damage
- Symptoms do not respond to initial treatment
- Your doctor is considering anti-reflux surgery
To confirm a diagnosis of gastroesophageal reflux disease (GERD) or to check for complications, your doctor might recommend:
- Upper endoscopy or gastroscopy. Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat. The endoscope helps your provider see inside your esophagus and stomach. Test results may not show problems when reflux is present, but an endoscopy may detect inflammation of the esophagus (esophagitis) or other complications. An endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications such as Barrett esophagus. In some instances, if a narrowing is seen in the esophagus, it can be stretched or dilated during this procedure. This is done to improve trouble swallowing (dysphagia).
- Transnasal esophagoscopy. This test is done to look for any damage in your esophagus. A thin, flexible tube with a video camera is put through your nose and moved down your throat into the esophagus. The camera sends pictures to a video screen.
- Reflux testing (wireless pH/pH impedance). Ambulatory acid (pH) probe is placed in your esophagus to identify when, and for how long, stomach acid regurgitates there. The monitor connects to a small computer that you wear around your waist or with a strap over your shoulder. The monitor might be a thin, flexible tube (catheter) that’s threaded through your nose into your esophagus. Or it might be a clip that’s placed in your esophagus during an endoscopy. The clip passes into your stool after about two days.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- Your doctor performs an endoscopy and places a small chip in your lower esophagus
- The chip records the acid level in your esophagus for 48 hours.
- The chip transmits your acid level to a wireless recording device that you wear around your belt.
- The data from the recording device can gauge your reflux severity.
- 24-Hour pH Impedance. Your doctor may order this procedure to evaluate your reflux. This procedure monitors your pH level (level of acidity) for a prolonged period. During pH impedance:
- Your doctor places a thin, flexible catheter with an acid-sensitive tip through your nose into your esophagus. The catheter is placed in separate recording spots to evaluate the flow of liquid from your stomach into your esophagus.
- The catheter stays in your nose for a period of 24 hours.
- Your doctor is able to evaluate whether you have GERD, the severity of your reflux, the presence of non-acid reflux and the correlation between your reflux and symptoms. This procedure helps in the design of a course of treatment for you.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- X-ray of the upper digestive system. X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus and stomach. This is particularly useful for people who are having trouble swallowing. You may also be asked to swallow a barium pill that can help diagnose a narrowing of the esophagus that may interfere with swallowing.
- Esophageal manometry also known as esophageal motility (movement) studies. This test measures the rhythmic muscle contractions in your esophagus when you swallow. Esophageal manometry also measures the coordination and force exerted by the muscles of your esophagus. This is typically done in people who have trouble swallowing. An esophageal manometry is an essential part of the assessment process prior to anti-reflux surgery.
- During an esophageal manometry your doctor places a pressure-sensitive catheter into the esophagus. This may be performed right before esophageal pH impedance studies, as it determines where your doctor should place the catheter. The catheter evaluates the strength and coordination of your muscle contractions. It also tests the strength and relaxation function of the lower esophageal sphincter.
- Barium esophagram also called barium swallow, is an imaging test that checks for problems in your upper gastrointestinal tract. Your upper gastrointestinal tract includes your mouth, back of the throat, esophagus, stomach, and first part of your small intestine. The test uses a special type of x-ray called fluoroscopy. Fluoroscopy is a kind of X-ray “movie.” A barium esophagram also evaluates the coordination of your esophageal motor function. While it does not test for the presence of reflux, it is useful for evaluating injury to your esophagus.
- During barium contrast radiography:
- You swallow a contrast solution called barium.
- The barium coats your esophagus and gastrointestinal tract, making it easier for the doctor to detect abnormalities.
- An X-ray is taken.
- During the X-ray, your doctor looks for a narrowing in the esophagus called a stricture.
- During barium contrast radiography:
Gastroesophageal reflux disease differential diagnosis
Gastroesophageal reflux disease differential diagnosis include:
- Coronary artery disease
- Achalasia
- Eosinophilic esophagitis (EoE)
- Non-ulcer dyspepsia
- Rumination syndrome
- Esophageal diverticula
- Gastroparesis
- Esophageal and gastric neoplasm
- Peptic ulcer disease (PUD)
Gastroesophageal reflux disease treatments
If your symptoms are mild, treatment may not be necessary. Your doctor is likely to recommend that you first try lifestyle changes and nonprescription medications. If you don’t experience relief within a few weeks, your doctor might recommend prescription medication and additional testing.
Over-the-counter medicine is effective for treating mild cases of acid reflux. These medicines include:
- Antacids: This is a quick-acting medicine that reduces stomach acid. Unfortunately, antacids alone won’t heal the damage stomach acid causes in your esophagus. Sometimes, overusing antacids can cause diarrhea or constipation.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists): These medicines reduce acid production. They don’t work as quickly as antacids. However, they provide longer relief (up to 12 hours). Stronger versions of these medications are available by prescription from your doctor.
- Proton pump inhibitors (PPIs): These medicines block acid production and heal the damage in your throat. They are stronger than H2-receptor blockers.
If these medicines are not providing relief after a few weeks, contact your doctor. Your doctor may give you a prescription version of H2 receptor blockers or proton pump inhibitors. Additionally, your doctor may prescribe medicine to strengthen the lower esophageal sphincter. The medicine may decrease the number of times your muscle relaxes. It is often used for severe reflux. Side effects include fatigue or confusion. Another medicine your doctor may prescribe helps your stomach empty faster. This will cause the food to move along the digestive tract and not back up into your throat. Your doctor may combine more than one medicine, depending upon the severity of your reflux.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Lifestyle and home remedies for acid reflux
You can ease, stop or reduce heartburn and acid reflux yourself by doing the following:
- Eat smaller, more frequent meals.
- Eat food slowly and chew thoroughly. Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Lose weight if you’re overweight. Excess weight put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Try to find ways to relax
- Avoid foods or drinks that trigger your heartburn — such as alcohol, fried or fatty foods, chocolate, and peppermint.
- Don’t eat within 3 or 4 hours before bed. Wait at least three hours after eating before lying down or going to bed.
- Avoid tight-fitting clothing that are tight around your waist or abdomen. Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Don’t smoke or use tobacco. Smoking decreases the lower esophageal sphincter’s ability to function properly.
- Don’t drink alcohol
- Don’t stop taking any prescribed medicine without speaking to a doctor first
Elevate the head of your bed. You may find that using wood, bricks or books under the feet at the head end of your bed to raise the head of your bed by around 10 to 20 cm, so your chest and head are above your waist, helps relieve symptoms. This can help stop stomach acid traveling up towards your throat. If you can’t elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows isn’t effective as this can increase pressure on your abdomen and make your symptoms worse. When you go to bed, start by lying on your left side to help make it less likely that you will have reflux.
Alternative medicine
Some complementary and alternative therapies, such as ginger, chamomile and slippery elm, may be recommended to treat gastroesophageal reflux disease. However, none have been proved to treat gastroesophageal reflux disease or reverse damage to the esophagus. Talk to your doctor if you’re considering taking alternative therapies to treat GERD.
Nonprescription medications
If necessary, occasional acid reflux can be treated with nonprescription medication, options include:
- Antacids that neutralize stomach. Antacids containing calcium carbonate such as Mylanta, Rolaids and Tums, may provide quick relief. But antacids alone won’t heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or sometimes kidney problems.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists) to reduce acid production, such as cimetidine (Tagamet HB), famotidine (Pepcid AC) or nizatidine (Axid AR). H-2 blockers don’t act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours. Stronger versions are available by prescription.
- Proton pump inhibitors (PPIs) block acid production and heal the esophagus. Proton pump inhibitors are stronger acid blockers than H-2 blockers and allow time for damaged esophageal tissue to heal. Nonprescription proton pump inhibitors include lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24 HR).
If you suspect that you have gastroesophageal reflux disease (GERD), your symptoms worsen, or you have nausea, vomiting or difficulty swallowing, talk to your doctor. Prescription medications might help. In a few cases, gastroesophageal reflux disease (GERD) might be treated with surgery or other procedures.
Prescription medications
Prescription-strength treatments for gastroesophageal reflux disease (GERD) include:
- Prescription-strength proton pump inhibitors. Prescription-strength proton pump inhibitors include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), rabeprazole (Aciphex) and dexlansoprazole (Dexilant). Although generally well tolerated, prescription-strength proton pump inhibitors might cause diarrhea, headaches, nausea, or in rare instances, low vitamin B-12 or magnesium levels.
- Prescription-strength H-2 blockers. Prescription-strength H-2 blockers include prescription-strength famotidine and nizatidine. Side effects from these medications are generally mild and well tolerated.
Multiple studies have demonstrated that proton-pump inhibitors (PPIs) provide superior therapeutic efficacy in the management of GERD than other antireflux medications such as H-2 receptor antagonists 36. Overall, proton-pump inhibitors (PPIs) demonstrate an unsurpassed rates of symptomatic relief and healing of esophageal inflammation as well as significant improvement in health-related quality of life in patients with erosive esophagitis 37, 38.
Surgery and other procedures
Gastroesophageal reflux disease (GERD) can usually be controlled with medication. But if medications don’t help or you wish to avoid long-term medication use, your doctor might recommend:
- Fundoplication. The surgeon wraps the top of your stomach around the lower esophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. The wrapping of the top part of the stomach can be complete (Nissen fundoplication) or partial. The most common partial procedure is the Toupet fundoplication. Your surgeon will recommend the type that is best for you.
- LINX device. A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The LINX device can be implanted using minimally invasive surgery. The magnetic beads do not have an effect on airport security or magnetic resonance imaging.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Because obesity can be a risk factor for gastroesophageal reflux disease (GERD), your doctor may suggest weight-loss surgery as an option for treatment. Talk with your doctor to find out if you’re a candidate for weight-loss surgery.
Gastroesophageal reflux disease diet
Diet plays a major role in controlling acid reflux symptoms and is the first line of therapy used for people with gastroesophageal reflux disease.
Foods that help prevent acid reflux
Ginger is one of the best digestive aids because of its medicinal properties. Ginger is alkaline in nature and anti-inflammatory, which eases irritation in the digestive tract. Try sipping ginger tea when you feel heartburn coming on.
High-fiber foods
Fibrous foods make you feel full so you’re less likely to overeat, which may contribute to heartburn. So, load up on healthy fiber from these foods:
- Whole grains such as oatmeal, couscous and brown rice.
- Root vegetables such as sweet potatoes, carrots and beets.
- Green vegetables such as asparagus, broccoli and green beans.
Alkaline foods
Foods that have a low pH are acidic and more likely to cause reflux. Those with higher pH are alkaline and can help offset strong stomach acid. Alkaline foods include:
- Bananas
- Melons
- Cauliflower
- Fennel
- Nuts
Watery foods
Eating foods that contain a lot of water can dilute and weaken stomach acid. Choose foods such as:
- Celery
- Cucumber
- Lettuce
- Watermelon
- Broth-based soups
- Herbal tea.
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x[↩]
- Hungin APS, Molloy-Bland M, Scarpignato C. Revisiting Montreal: new insights into symptoms and their causes, and implications for the future of GERD. Am J Gastroenterol. 2019;114:414–421. doi: 10.1038/s41395-018-0287-1[↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589[↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018 Mar;67(3):430-440. doi: 10.1136/gutjnl-2016-313589[↩][↩]
- Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441938[↩][↩][↩]
- Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997 May;112(5):1448-56. doi: 10.1016/s0016-5085(97)70025-8[↩]
- Nebel OT, Fornes MF, Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976 Nov;21(11):953-6. doi: 10.1007/BF01071906[↩]
- Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Prevalence of gastro-oesophageal reflux symptoms and the influence of age and sex. Scand J Gastroenterol. 2004 Nov;39(11):1040-5. doi: 10.1080/00365520410003498[↩]
- Fass R, Frazier R. The role of dexlansoprazole modified-release in the management of gastroesophageal reflux disease. Therap Adv Gastroenterol. 2017 Feb;10(2):243-251. doi: 10.1177/1756283X16681701[↩][↩]
- Fass R, Ofman JJ. Gastroesophageal reflux disease–should we adopt a new conceptual framework? Am J Gastroenterol. 2002 Aug;97(8):1901-9. doi: 10.1111/j.1572-0241.2002.05912.x[↩][↩]
- Kellerman R, Kintanar T. Gastroesophageal Reflux Disease. Prim Care. 2017 Dec;44(4):561-573. doi: 10.1016/j.pop.2017.07.001[↩][↩][↩]
- Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ, Tytgat GN, Wallin L. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999 Aug;45(2):172-80. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1727604/pdf/v045p00172.pdf[↩]
- Wang KK, Sampliner RE; Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett’s esophagus. Am J Gastroenterol. 2008 Mar;103(3):788-97. doi: 10.1111/j.1572-0241.2008.01835.x[↩][↩]
- Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007 Feb;41(2):131-7. doi: 10.1097/01.mcg.0000225631.07039.6d[↩]
- Jung HK, Tae CH, Song KH, et al. Korean Society of Neurogastroenterology and Motility. 2020 Seoul Consensus on the Diagnosis and Management of Gastroesophageal Reflux Disease. J Neurogastroenterol Motil. 2021 Oct 30;27(4):453-481. doi: 10.5056/jnm21077[↩]
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006 Aug;101(8):1900-20; quiz 1943. doi: 10.1111/j.1572-0241.2006.00630.x[↩][↩]
- Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Graffner H, Vieth M, Stolte M, Engstrand L, Talley NJ, Agréus L. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005 Mar;40(3):275-85. doi: 10.1080/00365520510011579[↩]
- Zou D, He J, Ma X, Chen J, Gong Y, Man X, Gao L, Wang R, Zhao Y, Yan X, Liu W, Wernersson B, Johansson S, Dent J, Sung JJ, Li Z. Epidemiology of symptom-defined gastroesophageal reflux disease and reflux esophagitis: the systematic investigation of gastrointestinal diseases in China (SILC). Scand J Gastroenterol. 2011 Feb;46(2):133-41. doi: 10.3109/00365521.2010.521888[↩]
- Argyrou A, Legaki E, Koutserimpas C, Gazouli M, Papaconstantinou I, Gkiokas G, Karamanolis G. Risk factors for gastroesophageal reflux disease and analysis of genetic contributors. World J Clin Cases. 2018 Aug 16;6(8):176-182. doi: 10.12998/wjcc.v6.i8.176[↩]
- Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005 Aug 2;143(3):199-211. doi: 10.7326/0003-4819-143-3-200508020-00006[↩]
- Malfertheiner P, Nocon M, Vieth M, Stolte M, Jaspersen D, Koelz HR, Labenz J, Leodolter A, Lind T, Richter K, Willich SN. Evolution of gastro-oesophageal reflux disease over 5 years under routine medical care–the ProGERD study. Aliment Pharmacol Ther. 2012 Jan;35(1):154-64. doi: 10.1111/j.1365-2036.2011.04901.x[↩]
- El-Serag HB, Hashmi A, Garcia J, Richardson P, Alsarraj A, Fitzgerald S, Vela M, Shaib Y, Abraham NS, Velez M, Cole R, Rodriguez MB, Anand B, Graham DY, Kramer JR. Visceral abdominal obesity measured by CT scan is associated with an increased risk of Barrett’s oesophagus: a case-control study. Gut. 2014 Feb;63(2):220-9. doi: 10.1136/gutjnl-2012-304189[↩]
- Mohammed I, Nightingale P, Trudgill NJ. Risk factors for gastro-oesophageal reflux disease symptoms: a community study. Aliment Pharmacol Ther. 2005 Apr 1;21(7):821-7. doi: 10.1111/j.1365-2036.2005.02426.x[↩]
- Savarino E, Bredenoord AJ, Fox M, Pandolfino JE, Roman S, Gyawali CP; International Working Group for Disorders of Gastrointestinal Motility and Function. Expert consensus document: Advances in the physiological assessment and diagnosis of GERD. Nat Rev Gastroenterol Hepatol. 2017 Nov;14(11):665-676. doi: 10.1038/nrgastro.2017.130. Epub 2017 Sep 27. Erratum in: Nat Rev Gastroenterol Hepatol. 2018 Apr 06;[↩]
- De Giorgi F, Palmiero M, Esposito I, Mosca F, Cuomo R. Pathophysiology of gastro-oesophageal reflux disease. Acta Otorhinolaryngol Ital. 2006 Oct;26(5):241-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2639970[↩][↩][↩][↩][↩]
- Mittal RK, McCallum RW. Characteristics and frequency of transient relaxations of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology. 1988 Sep;95(3):593-9. doi: 10.1016/s0016-5085(88)80003-9[↩]
- Kahrilas PJ, Lin S, Chen J, Manka M. The effect of hiatus hernia on gastro-oesophageal junction pressure. Gut. 1999 Apr;44(4):476-82. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1727465/pdf/v044p00476.pdf[↩]
- Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW. Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg. 1996 Jan;171(1):182-6. doi: 10.1016/S0002-9610(99)80096-8[↩][↩]
- Ott DJ, Gelfand DW, Chen YM, Wu WC, Munitz HA. Predictive relationship of hiatal hernia to reflux esophagitis. Gastrointest Radiol. 1985;10(4):317-20. doi: 10.1007/BF01893120[↩]
- Richter J. Do we know the cause of reflux disease? Eur J Gastroenterol Hepatol. 1999 Jun;11 Suppl 1:S3-9.[↩]
- Diener U, Patti MG, Molena D, Fisichella PM, Way LW. Esophageal dysmotility and gastroesophageal reflux disease. J Gastrointest Surg. 2001 May-Jun;5(3):260-5. doi: 10.1016/s1091-255x(01)80046-9[↩]
- Gastroesophageal Reflux Disease (GERD). https://www.hopkinsmedicine.org/health/conditions-and-diseases/gastroesophageal-reflux-disease-gerd[↩]
- Sandhu DS, Fass R. Current Trends in the Management of Gastroesophageal Reflux Disease. Gut Liver. 2018 Jan 15;12(1):7-16. doi: 10.5009/gnl16615[↩]
- Hom C, Vaezi MF. Extraesophageal manifestations of gastroesophageal reflux disease. Gastroenterol Clin North Am. 2013 Mar;42(1):71-91. doi: 10.1016/j.gtc.2012.11.004[↩]
- Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013 Mar;108(3):308-28; quiz 329. doi: 10.1038/ajg.2012.444. Epub 2013 Feb 19. Erratum in: Am J Gastroenterol. 2013 Oct;108(10):1672.[↩]
- Chiba N, De Gara CJ, Wilkinson JM, Hunt RH. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology. 1997 Jun;112(6):1798-810. doi: 10.1053/gast.1997.v112.pm9178669[↩]
- Hershcovici T, Fass R. Pharmacological management of GERD: where does it stand now? Trends Pharmacol Sci. 2011 Apr;32(4):258-64. doi: 10.1016/j.tips.2011.02.007[↩]
- Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease–where next? Aliment Pharmacol Ther. 2005 Jul 15;22(2):79-94. doi: 10.1111/j.1365-2036.2005.02531.x[↩]