What is glossitis
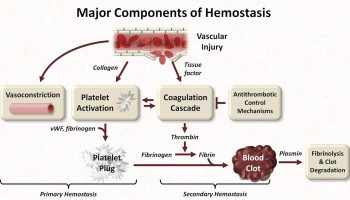
Glossitis can mean soreness of the tongue, or more usually inflammation with depapillation of the dorsal surface of the tongue (loss of the lingual papillae), leaving a smooth and erythematous (reddened) surface 1, sometimes specifically termed atrophic glossitis. In a wider sense, glossitis can mean inflammation of the tongue generally 2. Glossitis is often caused by nutritional deficiencies and may be painless or cause discomfort. Glossitis usually responds well to treatment if the cause is identified and corrected. Tongue soreness caused by glossitis is differentiated from burning mouth syndrome, where there is no identifiable change in the appearance of the tongue, and there are no identifiable causes 3.
Atrophic glossitis
Atrophic glossitis is also known as ‘smooth tongue’ because of the smooth, glossy appearance with a red or pink background (Figure 1). The smooth quality is caused by the atrophy of the filiform and fungiform papillae of the tongue. Atrophic glossitis presents with considerable loss of taste buds under a red or pink background. Atrophic glossitis is primarily a manifestation of underlying conditions and warrants thorough diagnostic evaluation. Nutritional deficiencies of iron, folic acid, vitamin B12, riboflavin, and niacin are common causes 4. Other causes include candida, immunosuppression due to HIV, celiac disease, malignancy, xerostomia triggered by some medications and Sjogren’s syndrome, and amyloidosis. Atrophic glossitis caused by nutritional deficiency often causes a painful or burning sensation in the tongue 4. Atrophic glossitis mainly affects elderly and debilitated patients. Treatment includes replacement of the missing nutrient or treatment of the underlying condition 5.
Iron deficiency. Oral effects of iron deficiency on oropharyngeal region varies from mucosal pallor, atrophic glossitis, generalized oral mucosal atrophy, anemic stomatitis, angular cheilitis, tenderness or burning sensation of oral mucosa, to various types of oral candidiasis, recurrent aphthous ulcers, dry mouth, and dysguesia. Severe prolonged iron deficiency may result in Plummer Vinson Syndrome 6.
Conditions associated with atrophic glossitis 7:
- Amyloidosis
- Celiac disease
- Chemical irritants
- Drug reactions
- Local infections (especially candidiasis)
- Nutritional deficiencies (e.g., iron, folic acid, vitamin B12, riboflavin, niacin)
- Pernicious anemia
- Protein-calorie malnutrition
- Sarcoidosis
- Sjögren syndrome
- Systemic infections (e.g., syphilis)
- Vesiculoerosive diseases (e.g., pemphigoid, pemphigus vulgaris, erythema multiforme, Stevens-Johnson syndrome)
Figure 1. Atrophic glossitis
Median rhomboid glossitis
Median rhomboid glossitis is the term used to describe a smooth, sharply circumscribed, asymptomatic, red, flat or raised nodular area on the top part (dorsum) of the middle or back of the tongue. The affected area of the tongue is missing its normal coating of finger-like projections called filiform papilla, which normally cover the entire top surface of the tongue. Other surfaces of the mouth are characteristically spared. Median rhomboid glossitis reflects its location and describes it. Median implies that the affected area is located near the center of the tongue, rhomboid refers to the shape of the affected area, and glossitis means inflammation.
Median rhomboid glossitis is present in about 1% of the population and most often affects men between the ages of 30 – 50 years of age. Men are affected three times more often than women 8. Median rhomboid glossitis typically presents as an ovoid area about 2 –3 centimeters long in its longest dimension (see Figure 2). As most cases of median rhomboid glossitis are without symptoms, it is often first noticed by the dentist during a routine examination. However, some patients may experience a burning sensation when eating certain foods 9. Median rhomboid glossitis is currently thought to represent a chronic fungal (candidiasis) infection in this area of the tongue. Sometimes a “kissing” lesion develops on the palate, directly opposite from the tongue lesion. This is more common in people whose immune system is suppressed and is believed to result from the fungal organisms on the top of tongue being transferred to the palate during swallowing and similar movements.
Median rhomboid glossitis is not contagious and cannot be transmitted.
In general, no treatment is necessary for median rhomboid glossitis. For those with symptoms (pain or burning sensation), antifungals (e.g., nystatin, fluconazole [Diflucan], clotrimazole) delivered as a suspension or oral troche 10 may be prescribed to kill the yeast and thereby reduce the symptoms. For cases of median rhomboid glossitis that do not respond to antifungal therapy, the dentist may recommend a biopsy be performed. Finally, while the lesion may resolve completely after using antifungal medication, it may recur once the medication is stopped.
Figure 2. Median rhomboid glossitis
Benign migratory glossitis
With benign migratory glossitis, the dorsal tongue develops areas of papillary atrophy that appear smooth and are surrounded by raised serpiginous borders. Benign migratory glossitis is also known as geographic tongue or erythema migrans, is common affecting up to 14% of the US population, and is of unknown cause 11. The prevalence is higher among white and black persons compared with Mexican Americans, and it has an association with fissured tongue and an inverse association with cigarette smoking 12. Benign migratory glossitis appears more commonly in females than males and more frequently in adults.
Benign migratory glossitis is characterized by irregularly shaped red, map-like smooth swollen patches on the tongue, the appearance is constantly changing. A white border sometimes surrounds them, giving rise to a map-like appearance. These regions of atrophy spontaneously resolve and migrate, giving the tongue a variegated appearance.
Often there are no symptoms but burning or irritation of the tongue is common, particularly with hot or spicy foods. The discomfort may come and go over time and may worsen at certain times of a women’s menstrual cycle or during pregnancy.
Lesions are usually confined to the tongue but they sometimes arise elsewhere in the mouth or on the lips.
The exact cause of benign migratory glossitis is unknown but the following factors have been linked with the condition:
- Benign migratory glossitis occurs more commonly in patients with psoriasis, especially pustular psoriasis
- There are also associations with diabetes, anemia, atopy (asthma and/or eczema) and stress
- In some patients particular foods seem to be a trigger, especially cheese
- Clustering within a family suggests genetic involvement
- Variation with the menstrual cycle suggests hormonal factors.
Benign migratory glossitis (geographic tongue) is a benign (harmless) condition that usually resolves itself without causing any problems for the patient so most people do not require treatment 13. There is no known cure, it may persist for months or longer, and often recurs. If there are associated medical conditions, treatment of these may improve the appearance of the tongue.
Discomfort may be treated with a mouth gargle or rinse containing antiseptic and anesthetic agents. Topical corticosteroids may also be helpful for occasional use e.g., triamcinolone in dental paste applied several times a day when required. Antihistamine mouth rinses (e.g., diphenhydramine elixir [Banophen], 12.5 mg per 5 mL diluted in a 1:4 ratio with water) can reduce tongue sensitivity 10.
Figure 3. Benign migratory glossitis
Glossitis causes
Conditions associated with atrophic glossitis 7:
- Amyloidosis
- Celiac disease
- Chemical irritants
- Drug reactions
- Local infections (especially candidiasis)
- Nutritional deficiencies (e.g., iron, folic acid, vitamin B12, riboflavin, niacin)
- Pernicious anemia
- Protein-calorie malnutrition
- Sarcoidosis
- Sjögren syndrome
- Systemic infections (e.g., syphilis)
- Vesiculoerosive diseases (e.g., pemphigoid, pemphigus vulgaris, erythema multiforme, Stevens-Johnson syndrome)
Other causes
Many conditions can cause glossitis via malnutrition or malabsorption 14, which creates the nutritional deficiencies described above, although other mechanisms may be involved in some of those conditions listed.
- Alcoholism 14
- Sprue (celiac disease or tropical sprue), secondary to nutritional deficiencies 14
- Crohn’s disease 14
- Whipple disease 14
- Glucagonoma syndrome 14
- Cowden disease 14
- Acquired immunodeficiency syndrome (AIDS) 14
- Carcinoid syndrome 14
- Kwashiorkor amyloidosis 14
- Veganism and other specialized diets 15
- Poor hydration and low saliva in the mouth, which allows bacteria to grow more readily
- Mechanical irritation or injury from burns, rough edges of teeth or dental appliances, or other trauma
- Tongue piercing 16. Glossitis can be caused by the constant irritation by the ornament and by colonization of Candida albicans in site and on the ornament 17
- Exposure to irritants such as tobacco, alcohol, hot foods, or spices
- Allergic reaction to toothpaste, mouthwash, breath fresheners, dyes in confectionery, plastic in dentures or retainers, or certain blood-pressure medications (ACE inhibitors)
- Administration of ganglion blockers (e.g., Tubocurarine, Mecamylamine).
- Oral lichen planus, erythema multiforme, aphthous ulcer, pemphigus vulgaris
- Heredity
- Albuterol (bronchodilator medicine)
A painful tongue may be an indication of an underlying serious medical condition and nearly always merits assessment by a physician or dental surgeon.
Glossitis treatment
The goal of treatment is to reduce inflammation. Treatment usually does not require hospitalization unless tongue swelling is severe. Good oral hygiene is necessary, including thorough tooth brushing at least twice a day, and flossing at least daily. Corticosteroids such as prednisone may be given to reduce the inflammation of glossitis. For mild cases, topical applications (such as a prednisone mouth rinse that is not swallowed) may be recommended to avoid the side effects of swallowed or injected corticosteroids. Antibiotics, antifungal medications, or other antimicrobials may be prescribed if the cause of glossitis is an infection. Anemia and nutritional deficiencies (such as a deficiency in iron, folic acid, vitamin B12, riboflavin, niacin) must be treated, often by dietary changes or other supplements. Avoid irritants (such as hot or spicy foods, alcohol, and tobacco) to minimize the discomfort.
- Rogers, K, eds. (2010). The digestive system (1st ed.). New York, NY: Britannica Educational Pub., in association with Rosen Educational Services. p. 146. ISBN 978-1615301317.[↩]
- Frank J. Domino (editor-in-chief), Robert A. Baldor, associate editors, eds. (2012-03-07). The 5-minute clinical consult 2012 (20th ed.). Philadelphia, Pa.: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 532–33. ISBN 978-1451103038.[↩]
- McMillan, Roddy; Forssell, Heli; Buchanan, John Ag; Glenny, Anne-Marie; Weldon, Jo C.; Zakrzewska, Joanna M. (2016). “Interventions for treating burning mouth syndrome”. The Cochrane Database of Systematic Reviews. 11: CD002779. doi:10.1002/14651858.CD002779.pub3 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002779.pub3/full[↩]
- Common Tongue Conditions in Primary Care. Am Fam Physician. 2010 Mar 1;81(5):627-634. https://www.aafp.org/afp/2010/0301/p627.html[↩][↩]
- Lee HJ, Jo DY. Images in clinical medicine. A smooth, shiny tongue. N Engl J Med. 2009;360(6):e8.[↩]
- Bhattacharya, Preeti Tomar & Misra, Satya. (2017). Effects of Iron Deficiency on the Oropharyngeal Region: Signs, Symptoms, and Biological Changes. 10.1007/978-3-319-40007-5_4-1.[↩]
- Shulman JD, Beach MM, Rivera-Hidalgo F. The prevalence of oral mucosal lesions in U.S. adults: data from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Dent Assoc. 2004;135(9):1279–1286.[↩][↩]
- Byrd JA, Bruce AJ, Rogers RS III. Glossitis and other tongue disorders. Dermatol Clin. 2003;21(1):123–134.[↩]
- Joseph BK, Savage NW. Tongue pathology. Clin Dermatol. 2000;18(5):613–618.[↩]
- Gonsalves WC, Chi AC, Neville BW. Common oral lesions: Part I. Superficial mucosal lesions. Am Fam Physician. 2007;75(4):501–507.[↩][↩]
- Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M. Benign migratory glossitis or geographic tongue: an enigmatic oral lesion. Am J Med. 2002;113(9):751–755.[↩]
- Shulman JD, Carpenter WM. Prevalence and risk factors associated with geographic tongue among US adults. Oral Dis. 2006;12(4):381–386.[↩]
- Samad A, Mohan N, Balaji RV et al (2015) Oral manifestations of Plummer-Vinson syndrome: a classic report with literature review. J Int Oral Health 7(1):1–4[↩]
- Tadataka Yamada, David H. Alpers, et al., eds. (2009). Textbook of gastroenterology (5th ed.). Chichester, West Sussex: Blackwell Pub. pp. 1717–1744. ISBN 978-1-4051-6911-0.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Scully, Crispian (2008). Oral and maxillofacial medicine : the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone. p. 356. ISBN 978-0443068188.[↩]
- Oral piercing: complications and side effects. Am J Dent. 2007 Oct;20(5):340-4. https://www.ncbi.nlm.nih.gov/pubmed/17993034[↩]
- Colonization of Candida: prevalence among tongue-pierced and non-pierced immunocompetent adults. Oral Dis. 2010 Mar;16(2):172-5. doi: 10.1111/j.1601-0825.2009.01618.x. Epub 2009 Aug 28. https://www.ncbi.nlm.nih.gov/pubmed/19732353[↩]