Contents
Causes of groin pain
Groin pain also called pelvic pain or perineal pain refers to discomfort in the area where the abdomen ends and the legs begin. The terms “groin” and “testicle” are sometimes used interchangeably for groin pain in men. But what causes pain in one area does not always cause pain in the other.
Groin pain female / women
Acute groin pain is generally defined as pain in the lower abdomen or pelvis lasting less than three months. Diagnosis of groin pain in women can be challenging because many symptoms and physical examination findings are often insensitive and nonspecific and the clinical presentation of each condition can vary widely 1. As the first priority, urgent life-threatening conditions (e.g., ectopic pregnancy, appendicitis, ruptured ovarian cyst) and fertility-threatening conditions (e.g., pelvic inflammatory disease (PID), ovarian torsion) must be considered. A careful history focusing on pain characteristics, review of systems, and gynecologic, sexual, and social history, in addition to physical examination helps narrow the differential diagnosis.
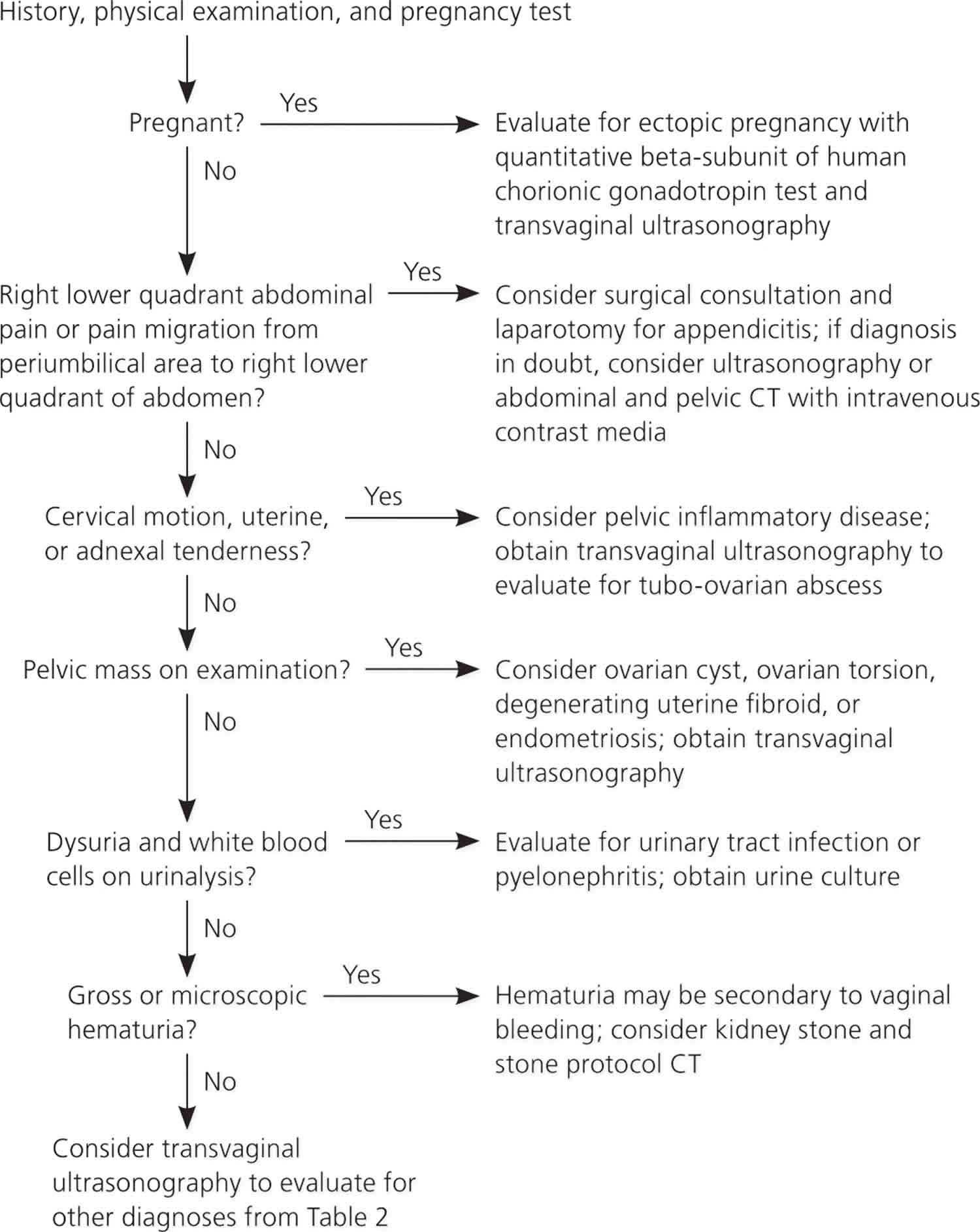
Figure 1 is an algorithm for the evaluation of acute groin pain in women 2. The physician’s first priority is to rule out emergent life-threatening conditions, such as ectopic pregnancy, ruptured tubo-ovarian abscess, and appendicitis. A thorough history, physical examination, and point-of-care pregnancy test and urinalysis should either produce a diagnosis or point to the proper imaging study. Rarely, diagnostic laparoscopy is needed to make the diagnosis.
Figure 1. Approach to a Woman with Acute Groin Pain
[Source 1 ]In a randomized trial of women of reproductive age presenting with nonspecific abdominal pain, a diagnosis during hospitalization was established in only 45 percent of the women randomized to the observation arm compared with 79 percent of the women randomized to the laparoscopy arm 3. In a study of 161 women undergoing laparoscopy for clinical appendicitis (based on history, examination, and transvaginal ultrasonography by a gynecologist), only 88 women were found to have appendicitis 2. These trials exemplify the diagnostic challenge of acute groin pain in women.
The most common urgent causes of groin pain are pelvic inflammatory disease (PID), ruptured ovarian cyst, and appendicitis 1; however, many other causes may mimic these conditions, and imaging is often needed. Transvaginal ultrasound should be the initial imaging test because of its sensitivities across most causes and its lack of radiation exposure. A high index of suspicion should be maintained for pelvic inflammatory disease (PID) when other causes are ruled out, because the presentation is variable and the prevalence is high. Multiple studies have shown that 20 to 50 percent of women presenting with groin pain have pelvic inflammatory disease (PID). Adolescents and pregnant and postpartum women require unique considerations.
Early diagnosis of groin pain is important to prevent complications of delayed diagnosis, such as appendiceal perforation, infertility from pelvic inflammatory disease (PID) and ovarian torsion, or hemoperitoneum from an ectopic pregnancy. Right-sided groin pain is especially challenging and can be confusing because of the close proximity of the appendix, uterus, right fallopian tube, and right ovary. Typically, right-sided groin pain requires imaging to determine the cause.
Pelvic inflammatory disease (PID) should be considered in young women who are sexually active and in other women at risk of sexually transmitted diseases (STDs) when they experience pelvic or lower abdominal pain and no other cause is apparent. This is especially true if the patient has cervical motion, uterine, or adnexal tenderness.
Causes of groin pain in women
The differential diagnosis of groin pain in women is most logically divided by the age and pregnancy status of the patient (see Table 1). Age separates patients into three groups: adolescents, women of reproductive age, and postmenopausal women. Adolescents will be discussed in a separate section below. Women of reproductive age and postmenopausal women obviously differ in their potential for pregnancy-related conditions, but share risks for non–pregnancy-related conditions. In postmenopausal women, endometriosis and ovarian torsion occur less often; however, there have been case reports of ovarian torsion in postmenopausal women 4.
Urgent conditions are the first causes to be considered and include ectopic pregnancy, ruptured ovarian cyst, ovarian torsion, appendicitis, and pelvic inflammatory disease (PID). Pelvic inflammatory disease (PID), appendicitis, and ruptured ovarian cysts are the most common among these conditions. Table 2 lists the frequencies of the most common acute groin pain causes 5. Less urgent conditions span many other organ systems, requiring the physician to consider a large differential diagnosis.
Table 1. Possible causes of acute groin pain in female
Women of reproductive age | |
| Gastrointestinal | |
| |
Gynecologic | |
| |
Urinary | |
| |
Other | |
| |
Pregnant women | |
| |
Adolescents | |
| |
Postmenopausal women | |
| |
Table 2. Frequency of common acute groin pain diagnoses
| Study (n) | Diagnosis | ||||||
|---|---|---|---|---|---|---|---|
| Appendicitis | Ectopic pregnancy | Endometriosis | Ovarian cyst | Ovarian torsion | Pelvic inflammatory disease | No diagnosis | |
Morino (104) 3 | 18% | 1%* | 2% | 12% | — | 19% | 37% |
Anteby (223) 6 | 3% | 17% | 3% | 27% | 10% | 21% | 12% |
Gaitán (110) 7 | 2% | 9% | 7% | 14% | — | 55% | 8% |
Kontoravdis (736) 8 | † | 19% | 16% | 2% | — | 23% | 8% |
Annual incidence in the United States (multiple sources) | 130,000 per year 9 ‡ | 60,000 per year 10 | NA | 65,000 per year 11 § | NA | 1,000,000 per year 5 | — |
Footnote:
NA = not available.
*— Pregnant women excluded.
† — Only gynecologic etiologies recorded.
‡ — Women only.
§ — Inpatient data.
[Source 1 ]Groin pain in female diagnosis
The history and physical examination narrow the differential diagnosis and allow the physician to choose the proper imaging test, because many of the diagnoses considered in acute pelvic pain require confirmatory testing. The patient should be asked about the location, intensity, radiation, timing, duration, and exacerbating and mitigating factors of the pain. Table 3 matches pertinent history and physical examination findings with their respective conditions 2.
Table 3. History and Physical Examination Clues to the Diagnosis of Acute Groin Pain in Female
| Clinical clues | Suggested diagnosis |
|---|---|
History | |
Bilateral pelvic pain | Pelvic inflammatory disease |
Dysmenorrhea | Endometriosis, uterine fibroid |
Dyspareunia | Endometriosis, ovarian cyst |
Dysuria | Pelvic inflammatory disease, urinary tract infection (UTI) |
Gross hematuria | Kidney stone, urinary tract infection (UTI) |
Left-sided pelvic pain | Diverticulitis, kidney stone, ruptured ovarian cyst |
Midcycle pain | Mittelschmerz |
Nausea and vomiting | Appendicitis, ovarian torsion |
Pain migration from periumbilical area to right lower quadrant of abdomen | Appendicitis |
Radiation of pain to groin | Kidney stone, ovarian torsion |
Right-sided pelvic pain | Appendicitis, kidney stone, ovarian torsion, ruptured ovarian cyst |
Urinary frequency | Urinary tract infection (UTI) |
Vaginal bleeding | Ectopic pregnancy, uterine fibroid |
Vaginal discharge | Pelvic inflammatory disease |
Physical examination | |
Adnexal mass | Corpus luteum cyst, diverticula of colon, ectopic pregnancy, endometriosis, follicular cyst, pelvic inflammatory disease, uterine fibroids |
Bilateral abdominal tenderness | Pelvic inflammatory disease |
Cervical motion, uterine, or adnexal tenderness | Pelvic inflammatory disease |
Fever | Appendicitis, pelvic inflammatory disease, pyelonephritis |
Hypotension | Ectopic pregnancy, ruptured hemorrhagic ovarian cyst |
Left lower quadrant abdominal tenderness | Diverticulitis |
Right lower quadrant abdominal tenderness | Appendicitis |
Vaginal mucopurulent discharge | Pelvic inflammatory disease |
The medical history should include previous abdominal and gynecologic surgeries. Past gynecologic problems should be elicited; in one study, 53 percent of patients with ovarian torsion had a known history of ovarian cyst or mass 12.
A comprehensive social history should include the patient’s sexual and sexually transmitted infection (STI or STD) history and her sex partner’s symptoms to help stratify risks for pelvic inflammatory disease (PID) and ectopic pregnancy. Recent intrauterine device (IUD) use should also be ascertained. In one review of 22,908 IUD insertions during 51,399 woman-years of follow-up, 1.6 cases of pelvic inflammatory disease (PID) per 1,000 woman-years were found, with risk more than six times higher during the first 20 days after insertion 13. After these first 20 days, the incidence of pelvic inflammatory disease (PID) in women with IUDs is similar to that in the general population.
Physical Examination
The physical examination should focus on the vital signs, and abdominal and pelvic examination. The pelvic examination is the most important part and is required for any woman with abdominal or pelvic pain. Physicians should acknowledge the limitations of a pelvic examination when assessing the adnexa 14.
There are few studies on the validity and reliability of the pelvic examination. A study of 186 women undergoing pelvic examination in two different emergency departments showed poor interexaminer reliability 15. The percentage of positive agreement between two physician examiners ranged from 17 to 33 percent 15. In another study of women examined preoperatively under anesthesia, the sensitivity of detecting an adnexal mass was 28 percent for the attending physician and 16 percent for a resident 14.
Table 4 lists the Centers for Disease Control and Prevention (CDC) criteria for pelvic inflammatory disease (PID) 16. The physician must be cognizant that pelvic inflammatory disease (PID) often presents with subtle and vague symptoms. In approximately 70 percent of patients with infertility because of obstructed fallopian tubes, chlamydia antibodies were detected, presumably from a missed diagnosis of pelvic inflammatory disease (PID) 17.
Table 4. Centers for Disease Control and Prevention (CDC) Criteria for Diagnosis of pelvic inflammatory disease
At least one of the following criteria must be present: |
|
|
|
Additional diagnostic criteria (enhances specificity if present): |
|
|
|
|
|
|
The most specific criteria for diagnosing PID include: |
|
|
|
Laboratory Testing
Physicians should obtain a urine pregnancy test and urinalysis. Urine beta-subunit of human chorionic gonadotropin (β-hCG) tests are sensitive to 25 mIU per mL (25 IU per L) and positive three to four days after implantation. By seven days after implantation, or the time of the expected menstrual period, 98 percent of the tests will be positive 18. A vaginal wet mount should be obtained, and cervical chlamydia and gonorrhea testing should be performed. White blood cells on vaginal wet mount support pelvic inflammatory disease (PID).
Most physicians are now using nucleic acid amplification tests (NAATs) to detect chlamydia and gonorrhea. These tests amplify and detect DNA and RNA sequences and are much more sensitive than previous chlamydia and gonorrhea tests. Urine NAATs have sensitivities and specificities similar to those of cervical samples 19. Based on the history and physical examination, other tests that should be considered include Rh blood typing (if pregnant), urine culture, complete blood count, erythrocyte sedimentation rate, and a fecal occult blood test. Erythrocyte sedimentation rate is a nonspecific marker of inflammation that can be associated with ectopic pregnancy 20.
Imaging
The goal of imaging is to make the most accurate diagnosis using the least amount of radiation; therefore, transvaginal ultrasonography is the imaging modality of choice in the initial evaluation of groin pain 21. A prospective study of 1,011 patients evaluated for urgent abdominal and groin pain found that ultrasonography, followed by computed tomography (CT) for negative or inconclusive ultrasonography, resulted in the most sensitive strategy with the least amount of radiation exposure (abdominal or pelvic CT exposes a woman to a radiation dose equivalent to 200 radiographs) 21.
For pregnant women with groin pain, transvaginal ultrasonography should be conducted immediately to evaluate for ectopic pregnancy. When the serum β-hCG level is greater than 1,500 mIU per mL (1,500 IU per L; often referred to as the discriminatory zone), a gestational sac should be visible on ultrasonography; if not, ectopic pregnancy should be suspected 22. However, one half of women presenting with ectopic pregnancy have β-hCG levels less than 2,000 mIU per mL (2,000 IU per L), which can make the distinction between early pregnancy and ectopic pregnancy difficult when an empty uterus is seen on transvaginal ultrasonography 22. A pseudo sac, which mimics intrauterine pregnancy, will be seen in 5 to 10 percent of ectopic pregnancies 5. An intrauterine pregnancy can be distinguished from a pseudo sac of an ectopic pregnancy by double echogenic rings (double decidual sac sign). A pseudo sac is characterized by only a single echogenic ring. Rarely, an ectopic pregnancy can occur simultaneously with an intrauterine pregnancy (one in 7,000 pregnancies); however, in patients undergoing assisted reproduction, the risk increases to one in 100 pregnancies 5.
Appendicitis, the most common cause of nongynecologic pain, can be diagnosed by ultrasonography, with a sensitivity of 75 to 90 percent compared with 87 to 98 percent for CT 5. Thus, normal ultrasonography makes appendicitis less likely, but does not rule it out. As the most common gynecologic cause of acute pelvic pain, early pelvic inflammatory disease (PID) changes may not be apparent on ultrasonography; however, later changes, such as pyosalpinx and tubo-ovarian abscess, will be seen. Ultrasonography is also a sensitive diagnostic tool for other urgent conditions, including hemorrhagic ovarian cysts, uterine fibroids, and ovarian torsion. When ultrasonography is indeterminate, CT or magnetic resonance imaging should be considered.
Adolescents and pregnant and postpartum women with groin pain
Adolescents and pregnant and postpartum women represent populations that deserve special attention. Adolescents can be uniquely challenging; issues to consider include confidentiality, local laws pertaining to consent, and high-risk behavior.
The differential diagnosis of groin pain in adolescents is similar to that for adults. Anatomic anomalies that prevent menstruation, such as imperforate hymen and transverse vaginal septum, must also be considered in adolescents. Compared with older patients, adolescents are at higher risk of pelvic inflammatory disease (PID) because of unsafe behaviors. In a study of 4,598 adolescents 15 to 19 years of age, 13.3 percent had been treated for an sexually transmitted infection (STI) or pelvic inflammatory disease (PID) 23. Another study reported that 48 percent of new cases of sexually transmitted diseases occurred in persons 15 to 24 years of age 24.
A detailed discussion on pelvic pain in pregnant and postpartum women is beyond the scope of this article. In addition to many of the same conditions as nonpregnant women, special considerations in pregnant women include corpus luteum hematoma and uterine impaction in the first trimester, and placental abruption and preterm labor in the third trimester. In the first trimester, there is an increased risk of ovarian torsion (25 percent of all cases of ovarian torsion) 5. In postpartum women, the diagnoses of endometritis and ovarian vein thrombosis must be considered 5.
Groin pain male
The most common cause of groin pain in men is a muscle, tendon or ligament strain, particularly in athletes who play sports such as hockey, soccer and football. Groin pain might occur immediately after an injury, or pain might come on gradually over a period of weeks or even months. Groin pain might be worsened by continued use of the injured area.
Less commonly, a bone injury or fracture, a hernia, or even kidney stones might cause groin pain. Although testicle pain and groin pain are different, a testicle condition can sometimes cause pain that spreads to the groin area.
Common causes of groin pain in men include:
- Pulled muscle, tendon, or ligaments in the leg. This problem often occurs in people who play sports such as hockey, soccer, and football. This condition is sometimes called “sports hernia” although the name is misleading since it is not an actual hernia. It may also involve pain in the testicles. Pain most often improves with rest and medications.
- Hernia. This problem occurs when there is a weak spot in the wall of the abdominal muscle that allows internal organs to press through. Surgery is needed to correct the weak spot.
- Disease or injury to the hip joint.
Less common causes of groin pain male include:
- Inflammation of the testicle or epididymitis and related structures
- Twisting of the spermatic cord that attaches to the testicle (testicular torsion)
- Tumor of the testicle
- Kidney stone
- Inflammation of the small or large intestine
- Skin infection
- Enlarged lymph glands
- Urinary tract infection
Direct and indirect causes of groin pain in men can include:
- Avascular necrosis (death of bone tissue due to limited blood flow)
- Avulsion fracture (ligament or tendon pulled from the bone)
- Bursitis (joint inflammation)
- Epididymitis (testicle inflammation)
- Hydrocele (fluid buildup that causes swelling of the scrotum)
- Inguinal hernia
- Kidney stones
- Mumps
- Muscle strain
- Orchitis (inflamed testicle)
- Osteoarthritis (disease causing the breakdown of joints)
- Pinched nerve
- Piriformis syndrome
- Retractile testicle (testicle that moves between the scrotum and abdomen)
- Sciatica
- Scrotal masses
- Spermatocele (fluid buildup in the testicle)
- Sprains
- Stress fractures
- Swollen lymph nodes
- Tendinitis
- Testicular cancer
- Testicular torsion (twisted testicle)
- Urinary tract infection (UTI)
- Varicocele (enlarged veins in the scrotum)
If your groin pain is caused by a strain or sprain, these self-care measures might help:
- Take an over-the-counter pain reliever such as ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others).
- Place an ice pack or bag of frozen peas, wrapped in a protective layer such as a towel, on the sore area for 20 to 30 minutes two to four times a day.
- Temporarily stop participation in athletic activities. Rest is essential to heal any strains or sprains to your groin.
Seek immediate medical attention if you have:
- Groin pain associated with back, abdomen or chest pain
- Sudden, severe testicle pain
- Testicle pain and swelling accompanied by nausea, vomiting, fever, chills or blood in the urine
Schedule a doctor’s visit if you have:
- Severe groin pain
- You have ongoing groin pain for no reason.
- Groin pain that doesn’t improve with home treatment within a few days
- Pain affects only one testicle for more than 1 hour, especially if it came on suddenly.
- A lump or swelling in or around a testicle
- You have pain with swelling of the scrotum
- You have noticed changes such as a testicular growth or change in skin color
- You have burning pain.
- Intermittent intense pain along the lower side of your abdomen (flank) that may radiate along your groin and into your testicle
- Blood in your urine
What to expect at your doctor’s visit
Your doctor will do an exam of the groin area and ask questions about your medical history and symptoms, such as:
- Have you had a recent injury?
- Has there been a change in your activity, especially a recent strain, heavy lifting, or similar activity?
- When did the groin pain start? Is it getting worse? Does it come and go?
- What other symptoms do you have?
- Have you been exposed to any sexually transmitted diseases?
Tests that may be performed include:
- Blood tests such as a complete blood count (CBC) or blood differential
- Ultrasound or other scan
- Urinalysis
- Evaluation of Acute Pelvic Pain in Women. https://www.aafp.org/afp/2010/0715/p141.html[↩][↩][↩][↩][↩][↩]
- Morishita K, Gushimiyagi M, Hashiguchi M, Stein GH, Tokuda Y. Clinical prediction rule to distinguish pelvic inflammatory disease from acute appendicitis in women of childbearing age. Am J Emerg Med. 2007;25(2):152–157.[↩][↩][↩]
- Morino M, Pellegrino L, Castagna E, Farinella E, Mao P. Acute nonspecific abdominal pain: A randomized, controlled trial comparing early laparoscopy versus clinical observation. Ann Surg. 2006;244(6):881–888.[↩][↩]
- Ding DC, Hsu S, Kao SP. Isolated torsion of the hydrosalpinx in a post-menopausal woman. JSLS. 2007;11(2):252–254.[↩]
- Vandermeer FQ, Wong-You-Cheong JJ. Imaging of acute pelvic pain. Clin Obstet Gynecol. 2009;52(1):2–20.[↩][↩][↩][↩][↩][↩][↩]
- Anteby SO, Schenker JG, Polishuk WZ. The value of laparoscopy in acute pelvic pain. Ann Surg. 1975;181(4):484–486.[↩]
- Gaitán H, Angel E, Sánchez J, Gómez I, Sánchez L, Agudelo C. Laparoscopic diagnosis of acute lower abdominal pain in women of reproductive age. Int J Gynaecol Obstet. 2002;76(2):149–158.[↩]
- Kontoravdis A, Chryssikopoulos A, Hassiakos D, Liapis A, Zourlas PA. The diagnostic value of laparoscopy in 2365 patients with acute and chronic pelvic pain. Int J Gynaecol Obstet. 1996;52(3):243–248.[↩]
- 2006 National Hospital Discharge Survey. National Health Statistics Reports Number 5, 30 July 2008. https://www.cdc.gov/nchs/data/nhsr/nhsr005.pdf[↩]
- Centers for Disease Control and Prevention. Ectopic pregnancy—United States, 1990–1992. MMWR Morb Mortal Wkly Rep. 1995;44(3):46–48.[↩]
- Merrill CT, Elixhauser A. Hospitalization in the United States, 2002. Rockville, Md.: Agency for Healthcare Research and Quality; 2005.[↩]
- Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med. 2001;38(2):156–159.[↩]
- Farley TM, Rosenberg MJ, Rowe PJ, Chen JH, Meirik O. Intrauterine devices and pelvic inflammatory disease: an international perspective. Lancet. 1992;339(8796):785–788.[↩]
- Padilla LA, Radosevich DM, Milad MP. Accuracy of the pelvic examination in detecting adnexal masses. Obstet Gynecol. 2000;96(4):593–598.[↩][↩]
- Close RJ, Sachs CJ, Dyne PL. Reliability of bimanual pelvic examinations performed in emergency departments. West J Med. 2001;175(4):240–245.[↩][↩]
- Centers for Disease Control and Prevention, Workowski KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006 [published correction appears in MMWR Morb Mortal Wkly Rep. 2006;55(36):997]. MMWR Morb Mortal Wkly Rep. 2006;55(RR-11):1–94[↩][↩]
- McCormack WM. Pelvic inflammatory disease. N Engl J Med. 1994;330(2):115–119.[↩]
- Chard T. Pregnancy tests: a review. Hum Reprod. 1992;7(5):701–710.[↩]
- Cook RL, Hutchison SL, Østergaard L, Braithwaite RS, Ness RB. Systematic review: noninvasive testing for Chlamydia trachomatis and Neisseriagonorrhoeae Ann Intern Med. 2005;142(11):914–925.[↩]
- Gaitán H, Angel E, Diaz R, Parada A, Sanchez L, Vargas C. Accuracy of five different diagnostic techniques in mild-to-moderate pelvic inflammatory disease. Infect Dis Obstet Gynecol. 2002;10(4):171–180.[↩]
- Laméris W, van Randen A, van Es HW, et al.; OPTIMA study group. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ. 2009;338:b2431.[↩][↩]
- Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy [published correction appears in Am Fam Physician. 2007;75(3):312]. Am Fam Physician. 2005;72(9):1707–1714.[↩][↩]
- Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005;(25):1–160.[↩]
- Weinstock H, Berman S, Cates W Jr. Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36(1):6–10.[↩]