Contents
Hailey Hailey disease
Hailey–Hailey disease also known as benign familial pemphigus is a rare hereditary blistering skin disease that usually appears in the third or fourth decade, although it can occur at any age. Hailey-Hailey disease is characterized by red, raw, and blistered areas of skin that occur most often in skin folds, such as the groin, armpits, neck, and under the breasts. These inflamed areas can become crusty or scaly and may itch and burn. The skin problems tend to worsen with exposure to moisture (such as sweat), friction, and hot weather. Hailey–Hailey disease then tends to persist life-long. It can affect people of all races.
The lesions are most commonly seen in the sides of the neck, armpit, and groin areas and under the breast. These patients may complain of a heavy odor and itching, which may be a social distress to patients’ lives.
The initial lesion may be a red, scaly area or a fluid filled blister which ruptures easily and becomes macerated or crusted. These lesions seem to come and go and leave no scars. The lesions may be localized to an area or may become widespread.
Many affected patients with Hailey-Hailey disease also have white lines running the length of their fingernails called ‘longitudinal leukonychia’ which are longitudinal white bands on the fingernails. These lines do not cause any problems, but they can be useful for diagnosing Hailey Hailey disease.
The severity of Hailey Hailey disease or benign chronic pemphigus varies from relatively mild episodes of skin irritation to widespread, persistent areas of raw and blistered skin that interfere with daily activities. Affected skin may become infected with bacteria or fungi, leading to pain and odor. Although the condition is described as “benign” (noncancerous), in rare cases the skin lesions may develop into a form of skin cancer called squamous cell carcinoma.
Hailey Hailey disease is a rare condition; its prevalence is unknown.
Complications of Hailey-Hailey disease include risk of secondary bacterial, fungal, and viral infections, which may require antimicrobial agents. There is no cure for Hailey-Hailey disease since it is a genetic disorder. Treating patients for the symptoms does provide patients with relief and reduces the microbial infections.
The first part of treatment is to avoid friction and sweating by wearing lightweight clothes. Avoiding direct sun and using sunscreen may also be helpful. Applying soothing compresses followed by topical corticosteroids and topical antibiotics are often effective for localized lesions. Generalized lesions may require oral antibiotics in addition to the above treatments.
Resistant cases that fail topical treatment have responded well to the following; oral corticosteroids, dapsone, topical tacrolimus, and photodynamic therapy. Dermabrasion, laser treatment and surgical skin grafting can also be used in severe cases.
Figure 1. Hailey Hailey skin disorder
Hailey Hailey skin disease cause
Hailey–Hailey disease or benign chronic pemphigus results from mutations in the ATP2C1 gene found on chromosome 3q21-24. This gene provides instructions for producing a protein called hSPCA1 (Secretory Pathway Calcium/manganese-ATPase), which is found in many types of cells. The hSPCA1 protein helps cells store calcium until it is needed. Calcium has several critical functions in cells, including regulating cell growth and division and helping cells stick to one another (cell adhesion). The hSPCA1 protein appears to be particularly important for the normal function of cells called keratinocytes, which are found in the outer layer of the skin (the epidermis).
Mutations in the ATP2C1 gene reduce the amount of functional hSPCA1 protein in cells. This abnormality impairs cells’ ability to store calcium normally. For unknown reasons, this abnormal calcium storage affects keratinocytes more than other types of cells. The abnormal regulation of calcium impairs many cell functions, including cell adhesion. As a result, keratinocytes do not stick tightly to one another, which causes the epidermis to become fragile and less resistant to minor trauma. Because the skin is easily damaged, it develops raw, blistered areas, particularly in skin folds where there is moisture and friction.
The genetic defect in Hailey–Hailey disease or benign chronic pemphigus causes the skin cells to become unstuck from one another. Normally the cells are packed together tightly in much the same way as bricks and mortar. Patients with Hailey-Hailey disease have defective ´mortar´ and the cells fall apart, like a dilapidated brick wall.
Hailey Hailey disease inheritance pattern
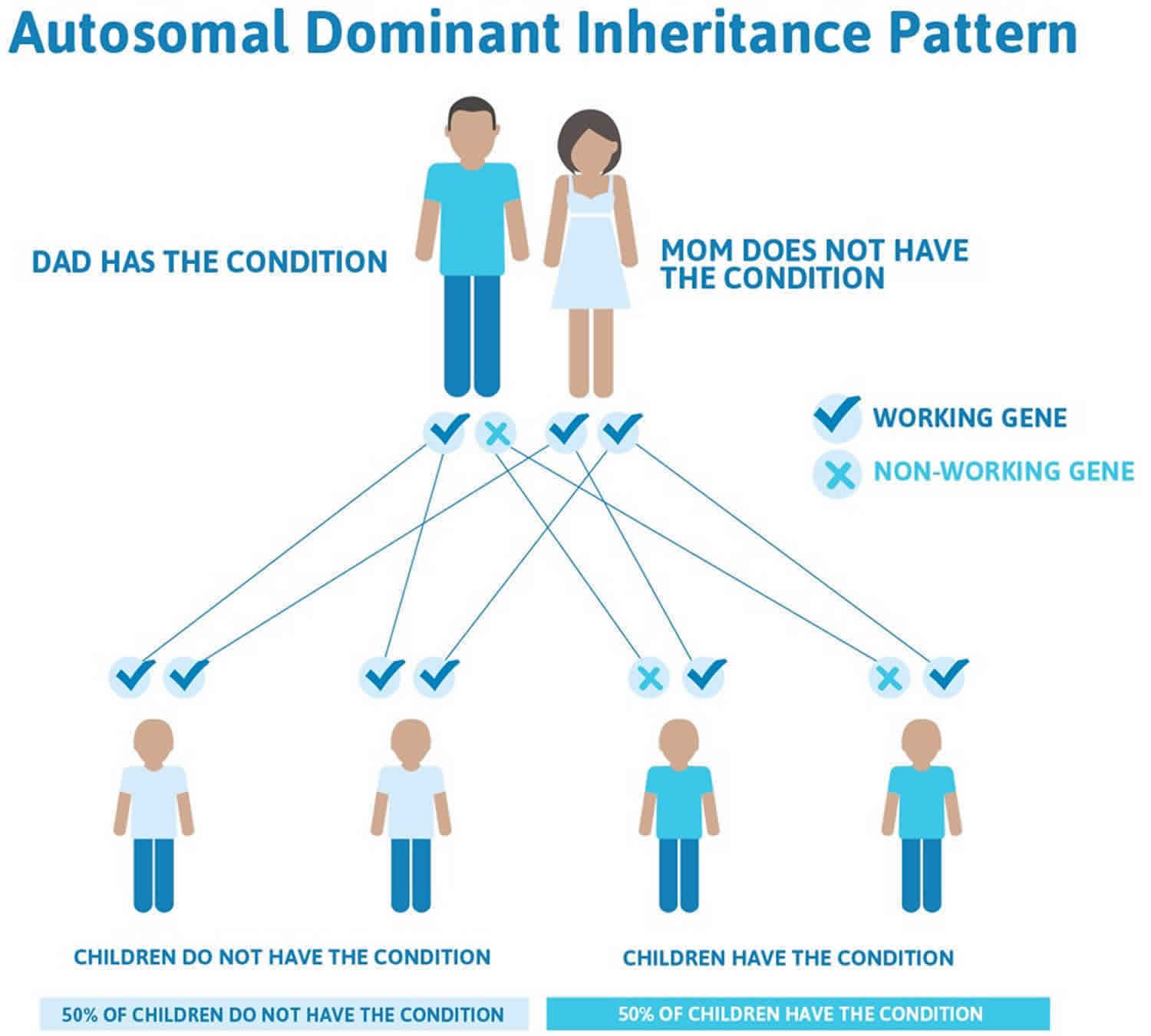
Hailey Hailey disease is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
There are cases of autosomal dominant gene changes, or mutations, where no one in the family has it before and it appears to be a new thing in the family. This is called a de novo mutation. For the individual with the condition, the chance of their children inheriting it will be 50%. However, other family members are generally not likely to be at increased risk.
Figure 2 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 2. Hailey Hailey disease autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Hailey Hailey skin disease symptoms
Hailey Hailey disease or benign familial pemphigus typically begins as a symmetrical painful erosive and crusted skin rash in the skin folds. Common sites include the armpits, groins, and neck, under the breasts and between the buttocks. The lesions tend to come and go and leave no scars. As the lesions get bigger the center clears leaving a typical ring shape. If the lesions are present for some time they may become thickened. The skin then tends to macerate leaving quite painful cracks.
Heat, sweating and friction often exacerbate the disease, and most patients have worse symptoms during the summer months.
Rarely, Hailey Hailey disease can be unilateral or have a linear arrangement, or it may involve mucous membranes. White bands on the fingernails and pits in the palms can also occur.
Hailey Hailey skin disease complications
For many patients Hailey Hailey disease (benign familial pemphigus) is a mild condition, but for others, the pain and smell can be serious problems. Secondary bacterial infection, which is not uncommon, can give rise to an unpleasant smell. Herpes simplex can infect blistered sites and may evolve to widespread, painful viral infection (eczema herpeticum).
Hailey Hailey skin disease diagnosis
Usually, Hailey Hailey disease or benign familial pemphigus is diagnosed by its appearance and family history, but it is often is mistaken for other skin problems. Impetigo, thrush, tinea (jock itch) and other blistering conditions look similar.
Diagnosis may require a skin biopsy. The histology is characteristic, with layers of detached skin cells (‘acantholysis’) lining up like ‘a row of tombstones’. Unlike pemphigus vulgaris, the immunofluorescence test for antibodies is negative.
As yet there is no diagnostic test available to family members.
Hailey Hailey skin disease treatment
There is no cure for Hailey-Hailey disease. Treatment is aimed at reducing symptoms and preventing flares.
General advice
- Avoid trigger factors such as sunburn, sweating and friction where possible; when hot, stay indoors with a fan or air conditioning, and limit the amount of exercise taken.
- Wash and dry skin folds carefully, once or twice daily using mild soap and water.
- Wear soft, loose clothing, with absorbent pads in underwear.
- If overweight, try to decrease body fat to minimise friction.
- Apply wet compresses, eg with 1:40 diluted aluminium acetate or vinegar, to dry up oozing patches.
- Take bleach baths twice weekly reduce superficial infections.
- Apply zinc paste to inflamed patches.
- Use antiperspirants such as roll-on and cream forms of aluminium salts and dusting powder containing the anticholinergic drug, diphemanil 2%.
Topical prescriptions
- Corticosteroid (cortisone) creams used short-term (eg one to two weeks) are effective in treating inflamed lesions; they work best if started early.
- Topical antibiotics such as clindamycin or mupirocin are used short-term for localized infection but are best avoided long-term due to the risk of inducing bacterial resistance, eg MRSA.
- Short-term use of combination corticosteroid/ antibiotic creams may also be helpful.
- Benzoyl peroxide is a useful antiseptic available as cream or wash.
- Ketoconazole cream can be used in case of fungal infection.
- Calcipotriol cream is useful for some patients.
- Fluorouracil cream has been reported effective in at least one patient.
- Topical calcineurin inhibitors such as pimecrolimus cream or tacrolimus ointment have been reported to reduce the need for topical steroids.
Oral prescriptions
- Prolonged courses of oral antibiotics, such as tetracycline may be useful.
- If herpes virus infection is a recurrent problem, oral antivirals such as aciclovir are prescribed.
- Anticholinergic medications such as glycopyrrolate may be prescribed to reduce hyperhidrosis (excessive sweating).
- A number of other oral medications (retinoids, ciclosporin, dapsone, and methotrexate) have been reported in single cases as partially effective, but large trials have not been performed.
Other treatments
- Corticosteroid injections into inflamed plaques
- Botulinum toxin to reduce sweating in axillae and groins, thus reducing colonisation by microorganisms and flare-ups
- Phototherapy (ultraviolet light) has also been used.
- Photodynamic therapy has had varying success.
- Lasers have been reported to be useful in one study, eg CO2laser or Er:YAG laser vaporising the affected skin, or pulsed dye laser enhancing wound healing.
- In severe cases, surgery can be performed to remove the affected skin. Skin grafts are usually necessary to repair the wounds.
- Dermabrasion has been reported to give excellent long-term results.
- Afamelanotide implants cleared Hailey-Hailey disease in 2 patients 1.
- Several patients have been reported that have had improvement in Hailey-Hailey disease when treated with low-dose naltrexone 2.
Hailey Hailey skin disease prognosis
Many patients have long remissions and an improvement with age does occur. Hailey Hailey disease or benign familial pemphigus causes discomfort but is not life threatening. Hailey Hailey disease or benign familial pemphigus lesions often begin during the teenage years and manifest as itchy and malodorous plaques. Patients with Hailey Hailey disease or benign familial pemphigus live long and productive lives. The skin disorder is more of a nuisance than a serious health threat. New treatment options are under study and offer hope for better treatments in the future.
- Biolcati G, Aurizi C, Barbieri L, Cialfi S, Screpanti I, Talora C. Efficacy of the melanocortin analogue Nle4-D-Phe7-α-melanocyte-stimulating hormone in the treatment of patients with Hailey-Hailey disease. Clin Exp Dermatol 2014; 39: 168–75. doi: 10.1111/ced.12203[↩]
- BENIGN CHRONIC PEMPHIGUS. https://omim.org/entry/169600?search=Hailey%20Hailey%20disease&highlight=disease%20hailey[↩]