Contents
What is Harlequin ichthyosis
Harlequin ichthyosis is a rare severe genetic skin disorder that affects infants before birth. The newborn infant is covered with very hard plates of thick skin that crack and split apart. The skin forms large, diamond-shaped plates that are separated by deep cracks (fissures). These skin abnormalities affect the shape of the eyelids, nose, mouth, and ears, and limit movement of the arms and legs. Restricted movement of the chest can lead to breathing difficulties and respiratory failure. The thick plates can pull at and distort facial features and can restrict breathing and eating. Harlequin ichthyosis baby needs to be cared for in the neonatal intensive care unit immediately.
The skin abnormalities associated with harlequin ichthyosis disrupt this barrier, making it more difficult for affected infants to control water loss, regulate their body temperature, and fight infections. Infants with harlequin ichthyosis often experience an excessive loss of fluids (dehydration) and develop life-threatening infections in the first few weeks of life. It used to be very rare for affected infants to survive the newborn period. However, with intensive medical support and improved treatment, people with this disorder now have a better chance of living into childhood and adolescence.
Harlequin ichthyosis is inherited as an autosomal recessive trait. Males and females are affected in equal numbers. Harlequin ichthyosis affects approximately one in 500,000 persons. Harlequin type ichthyosis occurs in about seven births annually in the United States.
There is no cure for harlequin ichthyosis, and treatment is centred around protecting the skin and preventing infection.
In the past, harlequin ichthyosis infants rarely survived beyond the first few days of life. With advancements in neonatal care, the survival rate has improved, with worldwide figures approaching 50% 1. With intensive medical support and improved treatment, people with Harlequin ichthyosis now have a better chance of living into childhood and adolescence. Several surviving children are now in their teenage years, with several in their twenties 2. The surviving children display dry, reddened skin, which may be covered by large thin scales, and sparse hair. Physical development may be delayed by the enormous calorie needs their skin function demands, but mental and intellectual developments are expected to be normal. Harlequin ichthyosis demands a meticulous skin care regimen to keep the skin moisturized and pliable and to prevent cracking and fissuring that may lead to infection.
Figure 1. Harlequin ichthyosis baby
Harlequin ichthyosis causes
Harlequin ichthyosis is caused by mutations in the ABCA12 gene located on chromosome 2 (2q34). ABCA12 gene provides instructions for making a protein that is essential for the normal development of skin cells. This protein plays a major role in the transport of fats (lipids) in the outermost layer of skin (the epidermis). Some mutations in the ABCA12 gene prevent the cell from making any ABCA12 protein, while others lead to the production of an abnormally small version of the protein that cannot transport lipids properly. A loss of functional ABCA12 protein disrupts the normal development of the epidermis, resulting in the hard, thick scales characteristic of harlequin ichthyosis.
Chromosomes, which are present in the nucleus of human cells, carry the genetic information for each individual. Each chromosome has a short arm designated “p” and a long arm designated “q”. Chromosomes are further sub-divided into many bands that are numbered. For example, “chromosome 2q34” refers to band 34 on the long arm of chromosome 2. The numbered bands specify the location of the thousands of genes that are present on each chromosome.
Harlequin ichthyosis inheritance pattern
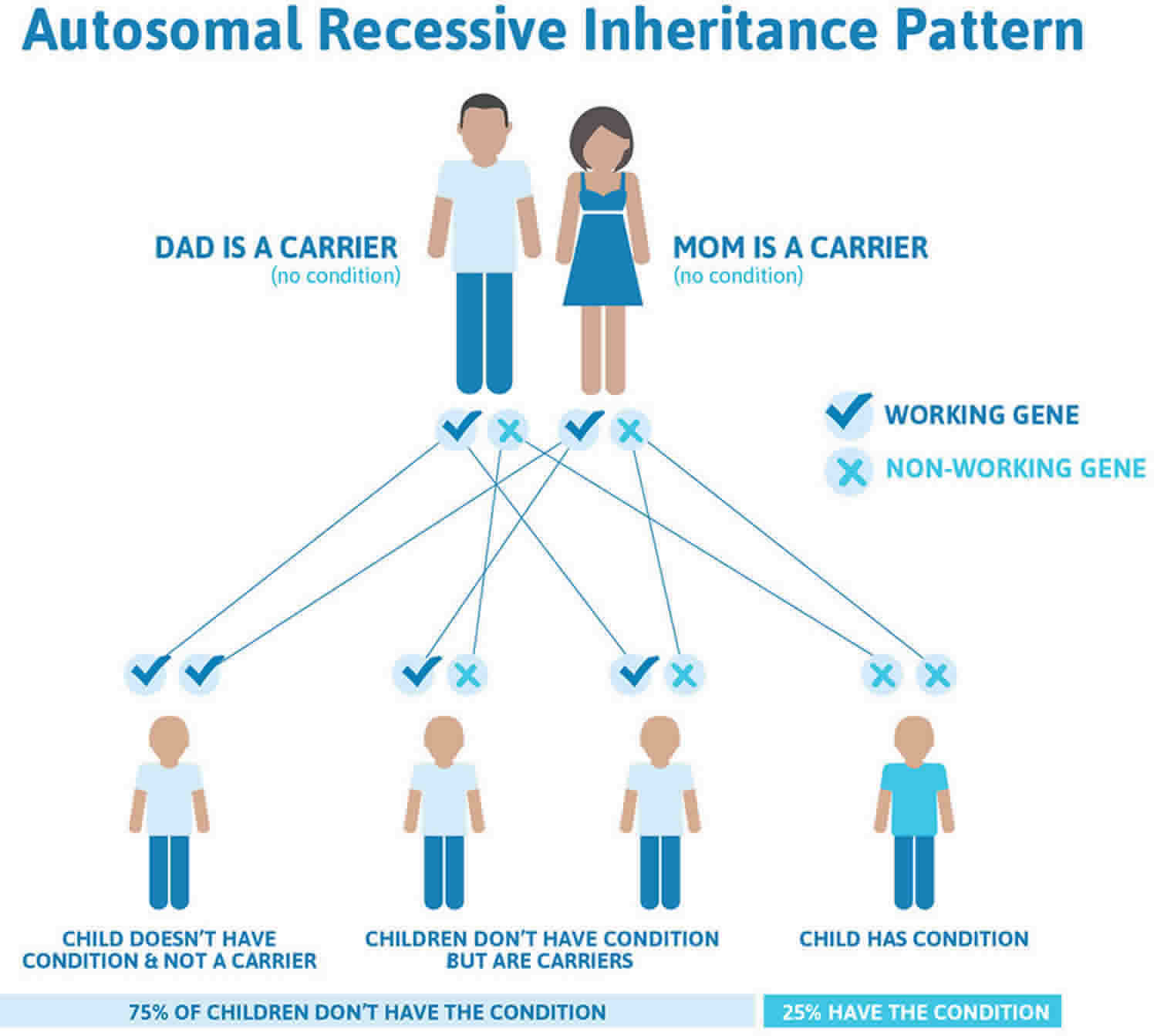
Harlequin type ichthyosis is a hereditary disorder transmitted through autosomal recessive genes. In recessive disorders, the condition appears when the person inherits the same defective gene for the same trait from each parent. If the individual receives one normal gene and one gene for the disease, the person will be a carrier for the disease but will not show the condition. The risk of transmitting the disease to the children of a couple, both of whom are carriers for the recessive disorder, is approximately 25 percent per pregnancy.
Figure 2. Harlequin ichthyosis autosomal recessive inheritance pattern
Harlequin ichthyosis signs and symptoms
Infants born with Harlequin ichthyosis are covered in thick plate-like scales of skin. The tightness of the skin pulls around the eyes and the mouth, forcing the eyelids and lips to turn inside out, revealing the red inner linings. The chest and abdomen of the infant may be severely restricted by the tightness of the skin, making breathing and eating difficult. The hands and feet may be small and swollen, and partially flexed. The ears may appear to be misshapen or missing, but are really fused to the head by the thick skin.
Premature birth is typical, leaving the infants at risk for complications from early delivery. These infants are also at high risk for difficulty breathing, infection, low body temperature, dehydration, and hypernatremia (elevated levels of sodium in the blood). Constriction and swelling of the mouth may interfere with the suck response and infants may need tube feeding. The baby’s corneas need to be lubricated and protected if the eyelids are forced open by the tightness of the skin.
Medical monitoring is difficult because of the abnormal skin; electrodes cannot be placed effectively and blood vessels cannot be seen under the skin. Placing lines in the artery and vein of the umbilical cord can aid in monitoring the infant and delivering fluids and nutrition. These infants may have problems maintaining normal levels of electrolytes, especially sodium in their blood. They are particularly prone to develop hypernatremia (high sodium levels in the blood). The baby’s corneas need to be lubricated and protected if the eyelids are forced open by the tightness of the skin. A high, humidity environment in a heated incubator is necessary to help maintain body temperature and to prevent the skin from cracking.
What are the clinical features of Harlequin ichthyosis?
The clinical features of Harlequin ichthyosis are described below.
Cutaneous features
- Skin changes are present at birth.
- The patient’s skin is severely thickened with large, shiny plates of hyperkeratotic scale.
- Deep erythematous fissures separate the scales.
Face
- Severe ectropion affecting the patient’s eyelids leaves the conjunctivae and cornea at risk of desiccation, infection, and trauma.
- The nose may be poorly developed, with the patient exhibiting nasal hypoplasia, eroded nasal alae, and obstructed nares.
- The ears may be poorly developed, flattened, or absent.
- The retroauricular folds and the pinnae of the ears may be small or absent, and the external auditory canal may be obstructed by scale.
- The traction of the lips causes eclabium.
Extremities
- The patient’s limbs are encased in thick, hyperkeratotic skin.
- Hypoplasia and extra fingers and toes may occur.
Thermal dysregulation
- The patient’s thickened skin prevents normal sweat gland function and heat loss.
- Excessive fluid loss leads to dehydration.
- The rise in body temperature can cause heat stroke.
What are the complications of harlequin ichthyosis?
- The cutaneous abnormalities associated with harlequin ichthyosis disrupt the normal skin barrier.
- The patient’s poor immunity to infections may be life threatening.
- Thick, hyperkeratotic skin may cause contractures (muscle shortening) and constriction of the limbs (including the fingers and toes) leading to swelling, necrosis, and autoamputation.
- The patient’s respiration is also restricted. The rigid skin impedes chest wall expansion, leading to hypoventilation and respiratory failure.
Harlequin ichthyosis diagnosis
Doctors frequently use genetic testing to help define which ichthyosis a person actually has. This may help them to treat and manage the patient. Another reason to have a genetic test is if you or a family member wants to have children. Genetic testing, which would ideally be performed first on the person with ichthyosis, is often helpful in determining a person’s, and their relative’s, chances to have a baby with ichthyosis. Genetic testing may be recommended if the inheritance pattern is unclear or if you or a family member is interested in reproductive options such as genetic diagnosis before implantation or prenatal diagnosis.
Genetic testing for a loss of function mutation on the ABCA12 gene is the most specific diagnostic test for harlequin ichthyosis.
- Mutations in the gene may cause impaired transport of lipids in the skin and shrunken versions of proteins responsible for skin development.
- Less severe mutations result in a collodion membrane and congenital ichthyosiform erythroderma-like presentation 3.
Results of genetic tests, even when they identify a specific mutation, can rarely tell you how mild or how severe a condition will be in any particular individual. There may be a general presentation in a family or consistent findings for a particular diagnosis, but it’s important to know that every individual is different. The result of a genetic test may be “negative,” meaning no mutation was identified. This may help the doctor exclude certain diagnoses, although sometimes it can be unsatisfying to the patient. “Inconclusive” results occur occasionally, and this reflects the limitation in our knowledge and techniques for doing the test. But we can be optimistic about understanding more in the future, as science moves quickly and new discoveries are being made all the time. You can receive genetic testing through the Yale University’s Disorders of Keratinization study with Dr. Keith Choate (http://www.firstskinfoundation.org/calling-all-ichthyosis-patients-gene-discovery-opportunity) or for more information about genetic tests performed you can visit GeneDx (https://www.genedx.com/).
Harlequin ichthyosis treatment
There is no cure for harlequin ichthyosis, and treatment is centred around protecting the skin and preventing infection. The thick, plate-like skin of Harlequin type ichthyosis will gradually split and peel off over several weeks. Antibiotic treatment may be necessary to prevent infection at this time. Administration of oral etretinate (1 mg/kg body weight) may accelerate shedding of the thick scales. Most Harlequin infants will need one-on-one nursing care for the first several weeks of life. It takes a week or two for etretinate to work loosening the scales. Because most of the fatalities from this condition occur in the first few days of life, many of the successes attributed to etretinate use in the medical literature may be equally due to the high quality of care in the immediate newborn period and to a less severely affected newborn. Some newborns with harlequin ichthyosis will not survive, even with the best of care, because of the severity of their condition.
After the thick plates peel off, the skin is left dry and reddened, and may be covered in large thin scales. The skin symptoms are treated by applying skin softening emollients. This can be particularly effective after bathing while the skin is still moist. Skin barrier repair formulas containing ceramides or cholesterol, moisturizers with petrolatum or lanolin, and mild keratolytics (products containing alpha-hydroxy acids or urea) can all work to keep the skin moisturized and pliable, and prevent cracking and fissuring that can lead to infection.
Severe cases of ichthyosis can be treated systemically with oral retinoids (e.g., acitretin or isotretinoin). Retinoids are used only in severe cases of ichthyosis due to their known toxicity and other complications. Early systemic treatment with oral retinoids (eg, acitretin or isotretinoin) has also been shown to heal skin fissures, soften or resolve plate-like scales, and improve overall survival 4.
Harlequin ichthyosis life expectancy
In the past, harlequin ichthyosis infants rarely survived beyond the first few days of life. With advancements in neonatal care, the survival rate has improved, with worldwide figures approaching 50% 1. With intensive medical support and improved treatment, people with Harlequin ichthyosis now have a better chance of living into childhood and adolescence. Several surviving children are now in their teenage years, with several in their twenties 2.
Children who survive the neonatal period usually evolve to a less severe phenotype of icthyosis but continue to develop fish-like scales, and have retention of waxy, yellowing material in seborrhoeic areas, generalised poor hair growth and scarring alopecia. Harlequin ichthyosis survivors may continue to suffer from temperature dysregulation, have contractures of the digits, arthralgias, failure to thrive, hypothyroidism, and short stature.
- Rajpopat S, Moss C, Mellerio J, et al. Harlequin ichthyosis: a review of clinical and molecular findings in 45 cases. Arch Dermatol 2011; 147: 681–6. DOI: 10.1001/archdermatol.2011.9[↩][↩]
- Harlequin Ichthyosis: A Patient’s Perspective. http://www.firstskinfoundation.org/types-of-ichthyosis/harlequin-ichthyosis[↩][↩]
- Akiyama, M. ABCA12 mutations and autosomal recessive congenital ichthyosis: a review of genotype/phenotype correlations and of pathogenetic concepts. Hum Mutat 2010; 31: 1090–6. DOI: 10.1002/humu.21326[↩]
- Chang LM, Reyes M. A case of harlequin ichthyosis treated with isotretinoin. Dermatol Online J 2014; 20 (2): 7[↩]