Contents
What is audiometry
A hearing test is also called audiometry, is a test to measure your ability to hear sounds. Sounds vary, based on their loudness (intensity or decibels [dB]) and the speed of sound wave vibrations (tone or frequency measured in cycles per second [Hertz]). Hearing occurs when sound waves stimulate the nerves of the inner ear. The sound then travels along nerve pathways to the brain. Sound waves can travel to the inner ear through the ear canal, eardrum, and bones of the middle ear (air conduction). They can also pass through the bones around and behind the ear (bone conduction).
There are several methods that can be used to test hearing, depending on your age, development, and health status. Newborn hearing tests and some hearing tests for children are different to adult hearing tests, these are discussed below under newborn baby and toddler hearing test.
Common adult hearing tests include:
| Test | What happens |
|---|---|
| Pure tone audiometry | you listen to different sounds through headphones and press a button or raise your hand each time you hear something |
| Speech perception test | similar to a pure tone audiometry test but you listen to speech rather than sounds |
| Tympanometry | a small device is placed in your ear to check for fluid behind your eardrum |
In adults and older children, several hearing tests may be done:
- Pure tone testing (audiogram) — For this test, you wear earphones attached to the audiometer. Pure tones are delivered to one ear at a time. You are asked to signal when you hear a sound. The minimum volume required to hear each tone is graphed. A device called a bone oscillator is placed against the mastoid bone to test bone conduction.
- Speech audiometry — This tests your ability to detect and repeat spoken words at different volumes heard through a head set.
- Immittance audiometry — This test measures the function of the ear drum and the flow of sound through the middle ear. A probe is inserted into the ear and air is pumped through it to change the pressure within the ear as tones are produced. A microphone monitors how well sound is conducted within the ear under different pressures.
- Tuning fork testing — To determine if there are any conductive or nerve issues, the audiologist uses a tuning fork to make a sound. The tuning fork is placed behind your ear or on your head. As it vibrates, you observe when the sound fades and if the sound is louder on one side or the other.
In a conventional audiometry (pure tone testing), usually you’ll listen through headphones to sounds of different tones and volumes and be asked to press a button or raise your hand each time you hear something. The noises will gradually become quieter to find the softest sounds that you can hear and the results recorded on a chart called on an audiogram.
You may also be given a headband with a vibrating pad. The pad sends sound through the bones in your head directly to the cochlea (hearing organ) in both your ears. Again, you’ll be asked to signal each time you hear a sound. This test checks whether the cochlea and/or the hearing nerve are working or damaged.
At some point, the audiologist may play a rushing noise into one ear to cover up sounds while they test the other ear.
The tests may vary and you may be asked to come back for more tests to find out more about your ears and hearing.
The INTENSITY of sound is measured in decibels (dB):
- A whisper is about 20 dB.
- Loud music (some concerts) is around 80 to 120 dB.
- A jet engine is about 140 to 180 dB.
Sounds greater than 85 dB can cause hearing loss after a few hours. Louder sounds can cause immediate pain, and hearing loss can develop in a very short time.
The TONE of sound is measured in cycles per second or Hertz:
- Low bass tones range around 50 to 60 Hz.
- Shrill, high-pitched tones range around 10,000 Hz or higher.
The normal range of human hearing is about 20 to 20,000 Hz. Human speech is usually 500 to 3,000 Hz.
Your hearing threshold levels (the quietest sounds you can hear) are measured in decibels (dB) at different frequencies from low (500 Hz) to high (8000 Hz).
In detailed audiometry, hearing is normal if you can hear tones from 250 to 8,000 Hz at 25 decibels (dB) or lower.
An audiogram is a chart used to plot out hearing sensitivity and visually display the results of an audiogram hearing test. The quietest sounds a person can hear—thresholds—are measured across a broad range of pitches.
The numbers on the top of the audiogram represent pitch. When reading them from left to right, pitch changes from low to high (bass to treble).
The numbers running down the side of the audiogram represent loudness level. When reading from top to bottom, the loudness changes from soft to loud.
The symbols on an audiogram represent the quietest sounds which a person can detect. Where the symbols fall on the audiogram indicate the degree of hearing loss (how much hearing loss is present in each ear) as well as the type of hearing loss (conductive, sensorineural, or mixed). Once the audiogram is completed, your audiologist will explain to you in depth your hearing sensitivity.
The following is a generic audiogram that displays pitch, loudness level, and the degrees of hearing loss.
Figure 1. Audiogram
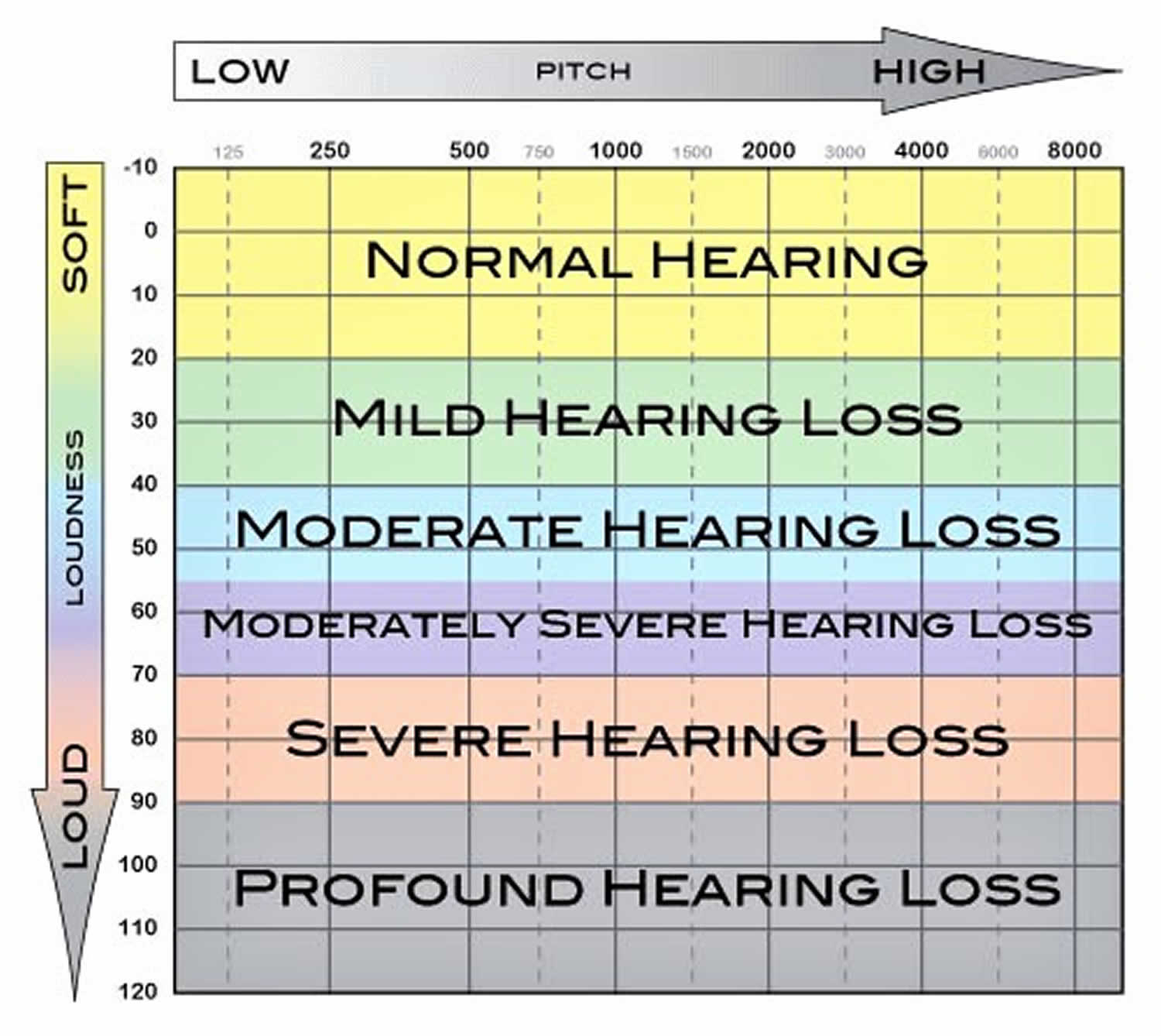 Compare your hearing threshold levels to this scale:
Compare your hearing threshold levels to this scale:- -10 (minus 10) – 25 dB Normal hearing
- 26 – 40 dB Mild hearing loss
- 41 – 55 dB Moderate hearing loss
- 56 – 70 dB Moderate/severe hearing loss
- 71 – 90 dB Severe hearing loss
- 91 – 100 dB Profound hearing loss
Normal Results
Normal results include:
- The ability to hear a whisper, normal speech, and a ticking watch is normal.
- The ability to hear a tuning fork through air and bone is normal.
- In detailed audiometry, hearing is normal if you can hear tones from 250 to 8,000 Hz at 25 dB or lower.
What abnormal results mean
There are many kinds and degrees of hearing loss. In some types, you only lose the ability to hear high or low tones, or you lose only air or bone conduction. The inability to hear pure tones below 25 dB indicates some hearing loss.
The amount and type of hearing loss may give clues to the cause, and chances of recovering your hearing.
The following conditions may affect your hearing test results:
- Acoustic neuroma
- Acoustic trauma from a very loud or intense blast sound
- Age-related hearing loss
- Alport syndrome
- Chronic ear infections
- Labyrinthitis
- Ménière disease
- Ongoing exposure to loud noise, such as at work or from music
- Abnormal bone growth in the middle ear, called otosclerosis
- Ruptured or perforated eardrum
Other tests may be used to determine how well the inner ear and brain pathways are working. One of these is otoacoustic emission testing (OAE) that detects sounds given off by the inner ear when responding to sound. This test is often done as part of a newborn screening. A head MRI may be done to help diagnose hearing loss due to an acoustic neuroma.
Other ways to get a hearing test
You can do a simple online hearing test on the Action on Hearing Loss website here (https://www.actiononhearingloss.org.uk/hearing-health/check-your-hearing/).
This can tell you if you need to have a face-to-face hearing test.
How hearing works
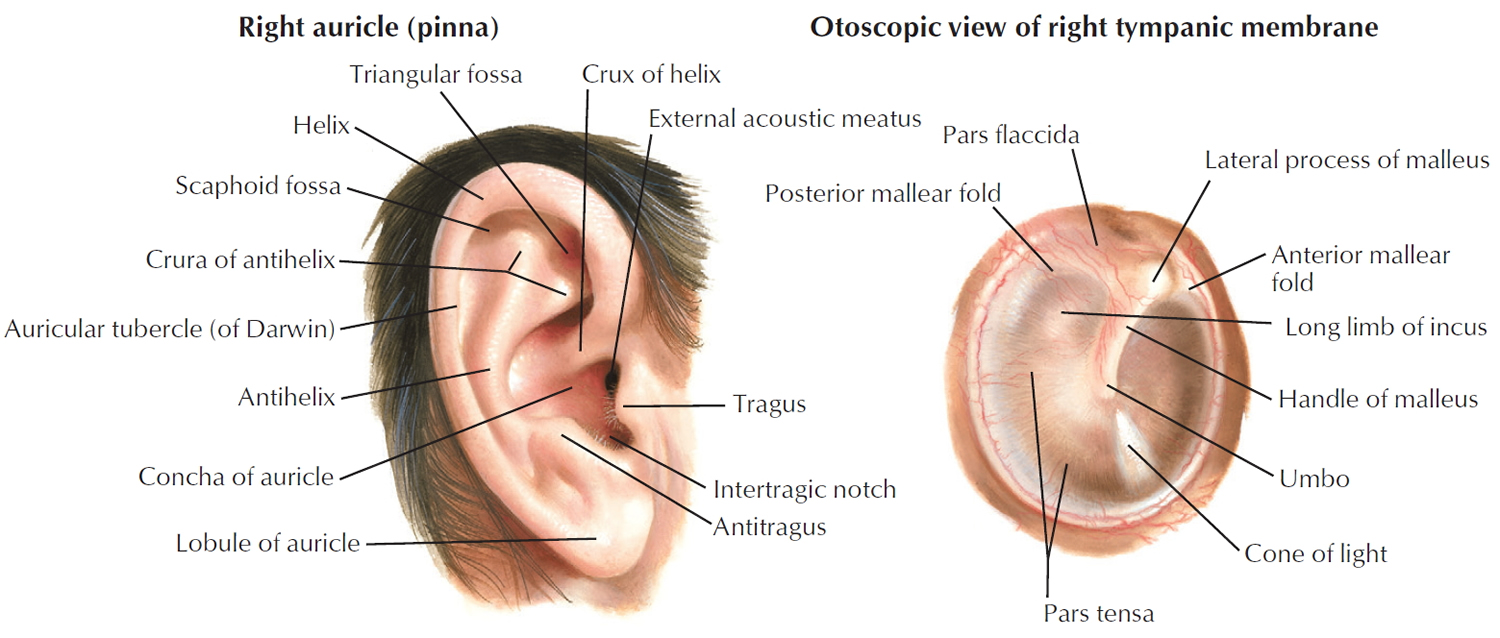
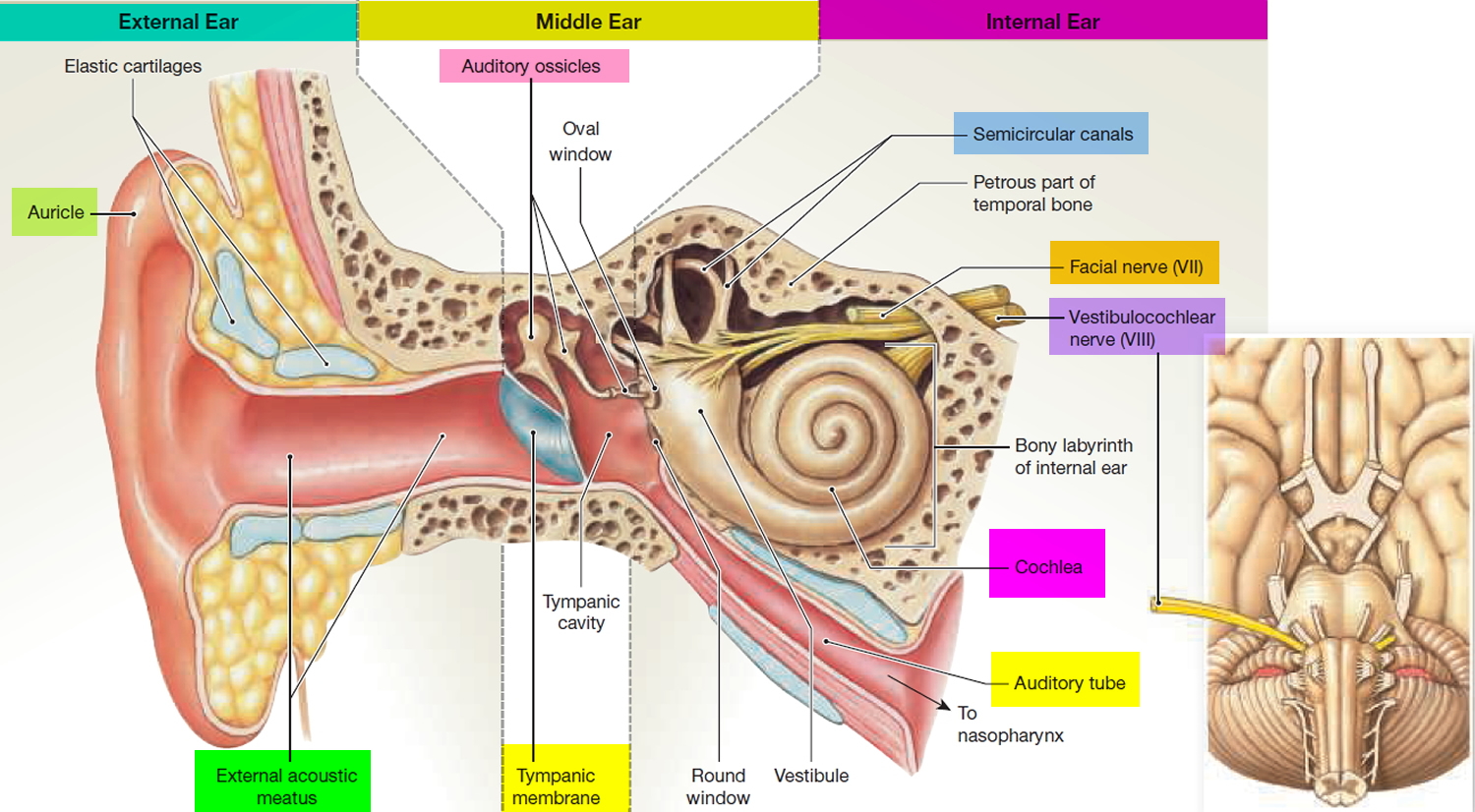
To understand how and why hearing loss happens, it helps to know how the ear works. The ear is made up of three different sections: the outer ear, the middle ear, and the inner ear. These parts work together so you can hear and process sounds. The outer ear, or pinna (the part you can see), picks up sound waves and the waves then travel through the outer ear canal (Figure 1 and 2).
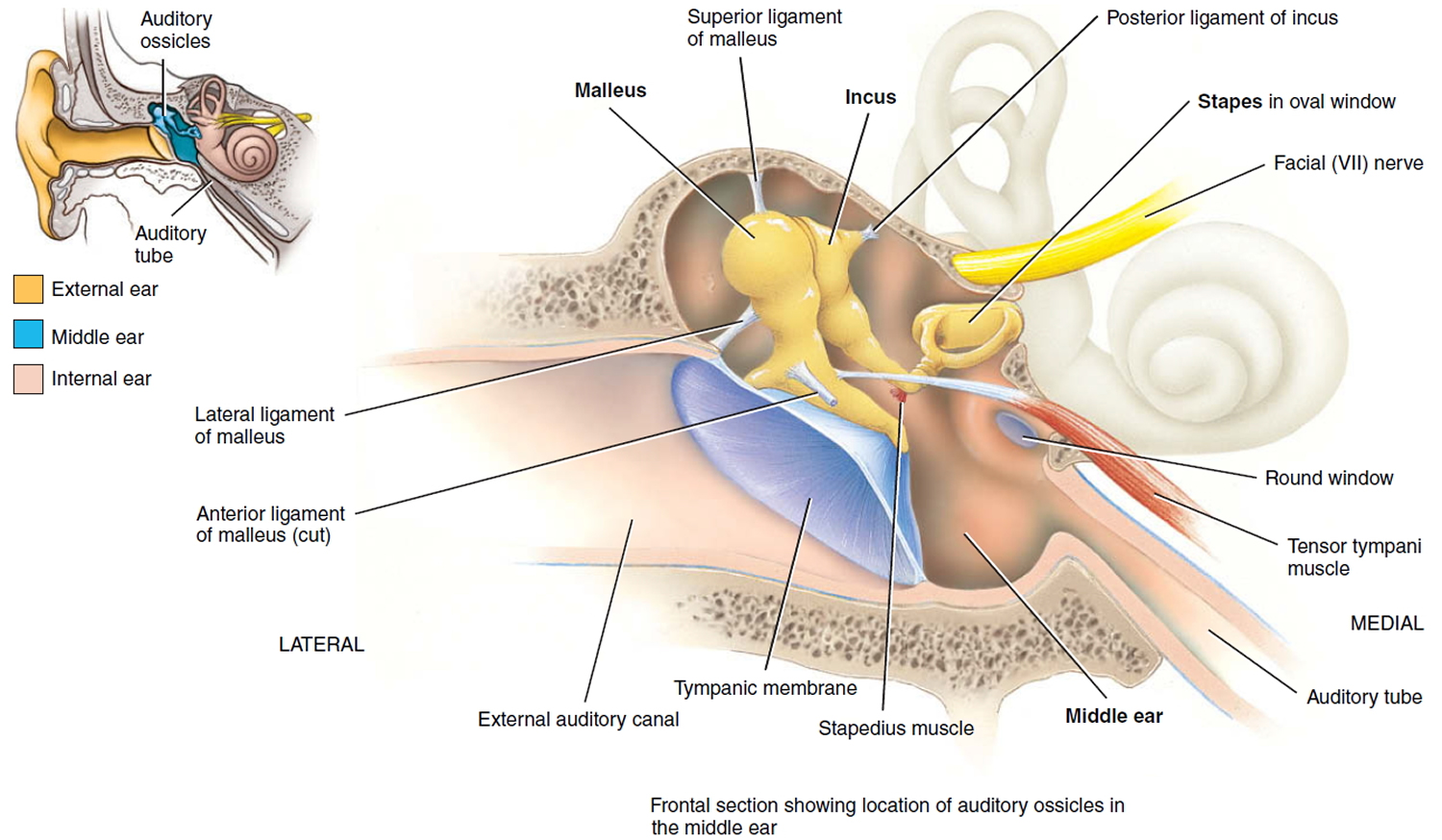
When the sound waves hit the eardrum in the middle ear, the eardrum starts to vibrate (see Figure 3). When the eardrum vibrates, it moves three tiny bones in your ear. These bones are called the hammer (or malleus), anvil (or incus), and stirrup (or stapes). They help sound move along on its journey into the inner ear (Figure 4).
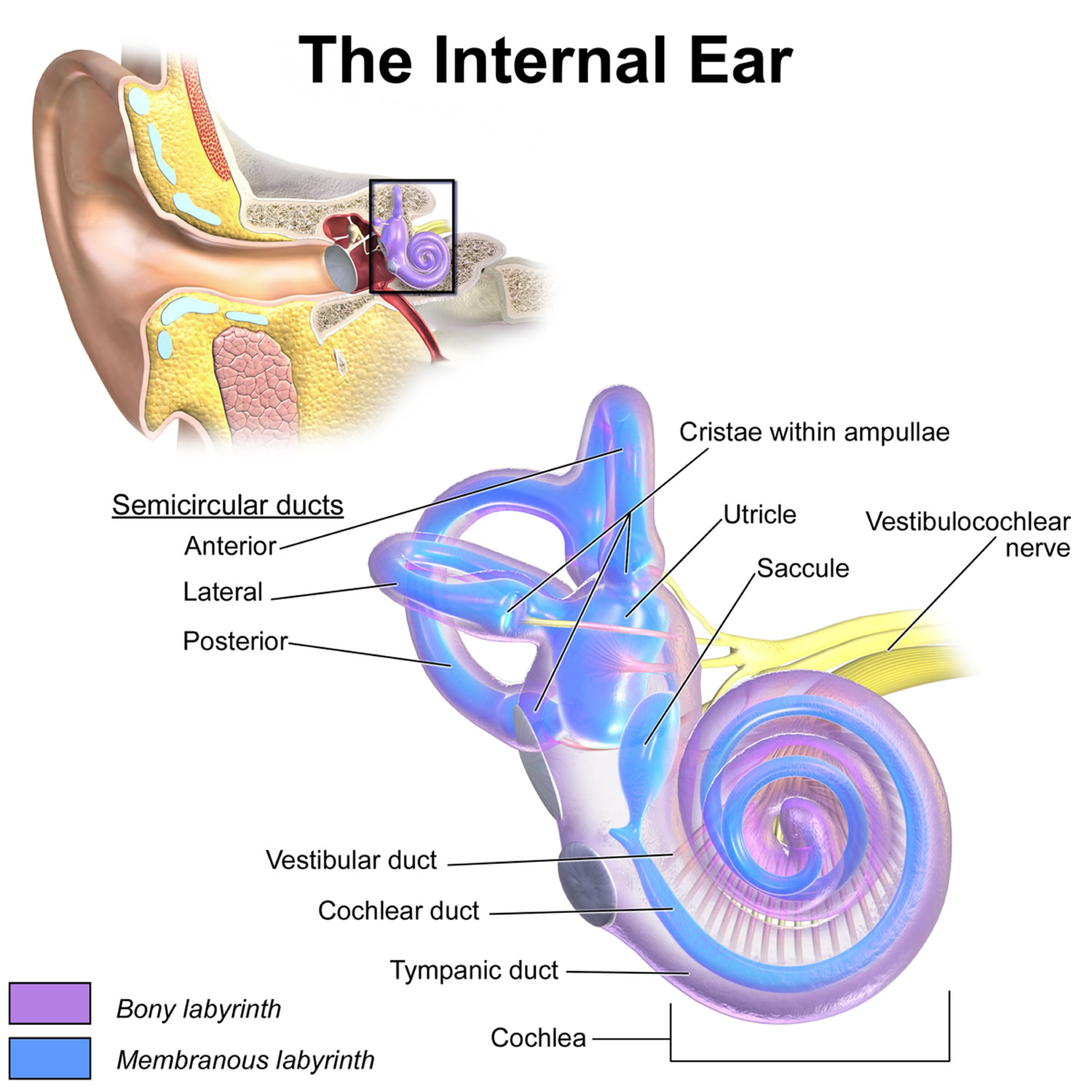
The vibrations then travel to the cochlea, which is filled with liquid and lined with cells that have thousands of tiny hairs on their surfaces. There are two types of hair cells: the outer and inner cells. The sound vibrations make the tiny hairs move. The outer hair cells take the sound information, amplify it (make it louder), and tune it. The inner hair cells send the sound information to your hearing nerve, which then sends it to your brain, allowing you to hear.
Figure 1. Ear structure
Figure 2. Ear anatomy
Figure 3. Middle ear and auditory ossicles
Figure 4. Parts of the inner ear
What is hearing loss
Hearing loss or deafness can be temporary or permanent, partial or complete. Hearing loss often comes on gradually as you get older (presbycusis), but hearing loss can sometimes happen suddenly. You may also have other symptoms, such as earache, unusual noises in your ear (tinnitus) or a spinning sensation (vertigo).
It can be hard to tell if you’re losing your hearing. Other people may notice it before you do.
About 25 percent of people in the United States between the ages of 55 and 64 have some degree of hearing loss. For those older than 65, the number of people with some hearing loss is almost 1 in 2.
Early signs of hearing loss include:
- difficulty hearing other people clearly and misunderstanding what they say, especially in noisy places
- asking people to repeat themselves
- listening to music or watching TV with the volume higher than other people need
- difficulty hearing on the phone
- finding it hard to keep up with a conversation
- feeling tired or stressed from having to concentrate while listening
Aging and chronic exposure to loud noises are significant factors that contribute to hearing loss. Other factors, such as excessive earwax, can temporarily prevent your ears from conducting sounds as well as they should.
See your doctor if you notice any problems with your hearing so you can find out the cause and get advice on treatment.
If you have a sudden loss of hearing, particularly in one ear, seek immediate medical attention.
See your doctor if difficulty hearing is interfering with your daily life. Your hearing may have deteriorated if:
- You find that it’s harder to understand everything that’s said in conversation, especially when there’s background noise
- Sounds seem muffled
- You find yourself having to turn the volume higher when you listen to music, the radio or television
Types of hearing loss
There are a few different types of hearing loss: conductive, sensorineural, mixed (conductive and sensory combined), neural, and central.
- Conductive hearing loss. This happens when there is a problem with a part of the outer or middle ear that is blocking sound from going to the inner ear. Ear infections are the most common cause of this type of hearing loss in infants and young children. This type of hearing loss is usually mild, temporary, and treatable with medicine or surgery.
- Sensorineural hearing loss. This happens when there is a problem in the inner ear — the sensitive inner ear (cochlea) has damage or a structural problem or with the connection from the inner ear to the brain responsible for hearing (problems with the auditory cortex). Cochlear hearing loss, the most common type, may involve a specific part of the cochlea such as the inner hair cells, outer hair cells, or both. It usually exists at birth, and can be inherited or come from other medical problems, though sometimes the cause is unknown. This type of hearing loss is usually permanent and a child’s ability to talk normally may be affected. Sometimes the loss is progressive (gets worse over time) and sometimes unilateral (one ear only). Because the hearing loss can get worse over time, audiologic testing should be repeated later on. Although medicines and surgeries cannot cure this type of hearing loss, hearing aids can help children hear better.
- The degree of sensorineural hearing loss can be:
- mild (a person cannot hear certain sounds)
- moderate (a person cannot hear many sounds)
- severe (a person cannot hear most sounds)
- profound (a person cannot hear any sounds)
- The degree of sensorineural hearing loss can be:
- Central hearing loss. This happens when the cochlea is working properly, but parts of the brain are not. This rare type of hearing loss is difficult to treat. Auditory processing disorder is a condition in which the ears and brain cannot fully coordinate. People with auditory processing disorder usually hear well when it is quiet, but cannot hear well when it is noisy. In most cases, speech-language therapy can help kids with auditory processing disorder.
- Mixed hearing loss happens when a person has both conductive and sensorineural hearing loss.
What causes hearing loss?
Hearing loss can happen because a person was born with parts of the ear that didn’t form correctly and don’t work well. Other problems can happen later because of an injury or illness, including:
- middle ear fluid
- serious infections, such as meningitis
- head injury
- listening to very loud music, especially through headphones or ear buds
- repeated exposure to loud sounds, such as machinery
Lots of kids have had ear infections, which also can cause hearing loss. Permanent hearing loss from an ear infection is rare, though.
Hearing loss in children
Your child may have a problem with their hearing if they:
- are slow to learn to talk, or aren’t clear when they speak
- fails to respond to his or her name or easily frustrated when there’s a lot of background noise
- fails to respond to conversation-level speech or answers inappropriately to speech
- talk very loudly
- ask you to repeat yourself or respond inappropriately to questions
- turn up the volume of the TV very high
- frequently inattentive
- difficulty learning
See your doctor if you’re worried about your child’s hearing.
Hearing loss in children can be caused by a build-up of fluid in the ear (glue ear or middle ear effusion or otitis media), which tends to get better over time and can be treated.
Hearing loss in babies
Hearing loss is a common birth defect, affecting about 1 to 3 out of every 1,000 babies. Although many things can lead to hearing loss, about half the time, no cause is found.
Babies have a hearing check in the first few weeks after birth, but speak to your health visitor or see your doctor if you think they might have difficulty hearing. Newborn hearing screening identifies most children born with a hearing loss. But in some cases, the hearing loss is caused by things like infections, trauma, and damaging noise levels, and the problem doesn’t emerge until later in childhood. Researchers believe that the number of people who have hearing loss doubles between birth and the teen years. So it’s important to have kids’ hearing checked regularly as they grow.
Your newborn should have a hearing screening before being discharged from the hospital. Every state and territory in the United States has now established an Early Hearing Detection and Intervention program; the program identifies every child with permanent hearing loss before 3 months of age, and provides intervention services before 6 months of age. If your baby doesn’t have this screening, or was born at home or a birthing center, it’s important to have a hearing screening within the first 3 weeks of life.
If your baby does not pass the hearing screening, it doesn’t necessarily mean there’s a hearing loss. Because debris or fluid in the ear can interfere with the test, it’s often redone to confirm a diagnosis.
If your newborn doesn’t pass the initial hearing screening, it’s important to get a retest within 3 months so treatment can begin right away. Treatment for hearing loss can be the most effective if it’s started before a child is 6 months old.
Kids who seem to have normal hearing should continue to have their hearing evaluated at regular doctors’ appointments. Hearing tests are usually done at ages 4, 5, 6, 8, and 10, and any other time if there’s a concern.
But if your child seems to have trouble hearing, if speech development seems abnormal, or if your child’s speech is difficult to understand, talk with your doctor.
Hearing loss can occur if a baby:
- was born prematurely
- stayed in the neonatal intensive care unit (NICU)
- had newborn jaundice with bilirubin level high enough to require a blood transfusion
- was given medications that can lead to hearing loss
- has family members with childhood hearing loss
- had certain complications at birth
- had many ear infections
- had infections such as meningitis or cytomegalovirus
- was exposed to very loud sounds or noises, even briefly
Babies may have a problem with their hearing if they:
- aren’t startled by loud noises
- seem to hear some sounds but not others
- notice you when they see you, but not when you call their name
- don’t turn towards voices by four months of age
- haven’t started to say any recognizable words by around 15 months
Babies Reaction to Sounds Checklist
This list give pointers about what to look for as your baby grows to check if he/she can hear. Babies differ widely in what they can do at any given age. The ages presented here are an approximate guide only.
- Shortly after birth – a baby: Is startled by a sudden loud noise such as a hand clap or a door slamming. Blinks or opens eyes widely to such sounds or stops sucking or starts to cry.
- 1 month – a baby: Starts to notice sudden prolonged sounds like the noise of a vacuum cleaner and may turn towards the noise. Pauses and listens to the noises when they begin.
- 4 months – a baby: Quietens or smiles to the sounds of familiar voice even when unable to see speaker and turns eyes or head towards voice. Shows excitement at sounds (e.g. voices, footsteps etc).
- 7 months – a baby: Turns immediately to familiar voice across the room or to very quiet noises made on each side (if not too occupied with other things).
- 9 months – a baby: Listens attentively to familiar everyday sounds and searches for very quiet sounds made out of sight.
- 12 months – a baby: Shows some response to own name. May also respond to expressions like ‘no’ and ‘bye bye’ even when any accompanying gesture cannot be seen.
If at any stage in the baby or child’s development you think he/she may have difficulties hearing, contact your family doctor.
Babies Making Sounds Checklist
Babies Making Sounds Checklist and Babies Reaction to Sounds Checklist give pointers about what to look for as your baby grows to check if he/she can hear. Babies do differ in what they can do at any given age. The ages presented here are approximate only.
- 4 months – a baby: Makes soft sounds when awake. Gurgles and coos.
- 6 months – a baby: Makes laughter-like sounds. Starts to make sing-song vowel sounds (e.g., a-a, muh, goo, der, aroo, adah).
- 9 months – a baby: Makes sounds to communicate in friendliness or annoyance. Babbles (e.g., ‘dada da’, ‘ma ma ma’, ‘ba ba ba’). Shows pleasure in babbling loudly and tunefully. Starts to imitate other sounds like coughing or smacking lips.
- 12 months – a baby: Babbles loudly, often in a conversational-type rhythm. May start to use one or two recognizable words.
- 15 months – a baby: Makes lots of speech-like sounds. Uses 2-6 recognizable words meaningfully (e.g., ‘teddy’ when seeing or wanting the teddy bear).
- 18 months – a baby: Makes speech-like sounds with conversational-type rhythm when playing. Uses 6-20 recognizable words. Tries to join in nursery rhymes and songs.
- 24 months – a child: Uses 50 or more recognizable words appropriately. Puts 2 or more words together to make simple sentences (for example: more milk). Joins in nursery rhymes and songs. Talks to self during play (may be incomprehensible to others).
- 30 months – a child: Uses 200 or more recognisable words. Uses pronouns (e.g., I, me, you). Uses sentences but many will lack adult structure. Talks intelligibly to self during play. Asks questions. Says a few nursery rhymes.
- 36 months – a child: Has a large vocabulary intelligible to everyone.
Newborn hearing screening
The newborn hearing screening test helps identify babies who have permanent hearing loss as early as possible. This means parents can get the support and advice they need right from the start.
One to two babies in every 1,000 are born with permanent hearing loss in one or both ears.
This increases to about 1 in every 100 babies who have spent more than 48 hours in intensive care.
Most of these babies are born into families with no history of permanent hearing loss.
Permanent hearing loss can significantly affect babies’ development.
Finding out early can give these babies a better chance of developing language, speech, and communication skills.
It’ll also help them make the most of relationships with their family or carers from an early age.
When’s the newborn hearing test done?
If you give birth in hospital, you may be offered a newborn hearing test for your baby before you’re discharged. Otherwise it’ll be done by a health professional, healthcare assistant or health visitor within the first few weeks.
You’ll be contacted by your local newborn hearing screening service to arrange a suitable time and venue. Ideally, the test is done in the first 4 to 5 weeks, but it can be done at up to 3 months of age.
If you aren’t offered a screening test, ask your health visitor, local audiology department or doctor to arrange an appointment, or contact your local newborn hearing screening service.
Newborn baby hearing test
All babies born in the United States receive a hearing screening prior to being discharged from the hospital. If your baby does not pass the screening test, further diagnostic testing will be needed to determine the presence and degree of hearing loss.
Ideally, all babies with hearing loss will be identified by 3 months of age so treatment can begin before the baby is 6 months old. These early months are an important time for your child’s speech and language development.
Some of the different hearing tests your baby may receive include:
Auditory brainstem response
Auditory brainstem response (ABR) test measures the response of your baby’s hearing nerve to sounds played through earphones. Responses are measured through small sticker electrodes placed on your baby’s skin. Testing is conducted while your baby sleeps. For this test, tiny earphones are placed in the ear canals and small electrodes (sensors which look like small stickers) are placed behind the ears and on the forehead. Usually, clicking sounds are sent through the earphones, and the electrodes measure the hearing nerve’s response to the sounds. It can take a few minutes for a simple screening test or more than an hour for more detailed diagnostic testing. The auditory brainstem response (ABR) test is painless for your baby. Young infants under 6 months can sleep for the entire test, but older infants may need sedation for this test. Older cooperative kids can do this testing in a silent environment while they’re visually occupied.
If your child is:
- Younger than 6 months, the auditory brainstem response (ABR) can usually be done without sedation. Your baby must sleep during the entire test. To help your baby stay asleep:
- In the hours before the test, don’t feed your baby or let your baby sleep.
- Arrive for the test when your baby is hungry and tired but awake.
- Before the test begins, the audiologist (hearing specialist) will ask you to feed your baby and get your little one comfortable. Your baby can sleep in your arms or a crib for the test.
- 6 months or older, the auditory brainstem response (ABR) might be done with sedation. This will help your child stay completely still and quiet during the test.
The audiologist will discuss the test with you when it’s done. A final report with recommendations will be available in a few weeks. If a hearing loss is found, the report also will go to the newborn hearing screening coordinator in your state.
Normal hearing has a certain appearance when test results are measured on a chart. Because of this, a normal auditory brainstem response suggests that a baby’s inner ear and lower part of the auditory system (brainstem) are working normally for typical speech. An abnormal auditory brainstem response may be a sign of hearing loss, but it may also be due to some medical problems or measurement problems.
Otoacoustic emissions
Otoacoustic emission (OAE) test uses a small earphone will play sounds into your baby’s ears. A healthy inner ear will respond with otoacoustic emissions (responses), which can be recorded with a tiny microphone inside the earphone. Otoacoustic emission testing takes only a few minutes and is painless.
A sleeping infant or an older child who may be able to sit quietly can do this quick test. A tiny probe is placed in the ear canal, then many pulsing sounds are sent and the probe records an “echo” response from the outer hair cells in the inner ear. These recordings are averaged by a computer.
A normal recording suggests that the outer hair cells are working well. But in some cases, a hearing loss may still happen if other hearing pathways are not working normally.
Hospitals use auditory brainstem response or otoacoustic emission to screen newborns. If a baby fails a screening, the test is usually repeated. If the screening is failed again, the baby is sent to an audiologist for a full hearing evaluation.
Auditory steady state response test
Auditory steady state response (ASSR) test is similar to the auditory brainstem response, though an infant usually needs to be sleeping or sedated for the auditory steady state response test.
Sound passes into the ear canals, and a computer picks up the brain’s response to the sound and automatically decides whether hearing loss is mild, moderate, severe, or profound. Auditory steady state response (ASSR) test has to be done with (and not instead of) auditory brainstem response (ABR) to check for hearing.
Central auditory evoked potential test
Central auditory evoked potential (CAEP) test is similar to the auditory brainstem response (ABR), and uses the same tiny earphones and small electrodes. Central auditory evoked potential (CAEP) test allows the audiologist to see if the pathways from the brainstem to the auditory cortex are working properly. The audiologist may recommend a central auditory evoked potential (CAEP) test for some specific types of hearing loss. This test can be done at any age and does not require participation from the child.
Tympanometry
Tympanometry is not a hearing test but is a test of middle ear function — the mobility of the eardrum and health of the middle ear space. A tympanometry procedure that can show how well the eardrum moves when a soft sound and air pressure are introduced in the ear canal. Tympanometry test can help determine how your child’s middle ear is functioning. Tympanometry is helpful in identifying middle ear problems, such as fluid collecting behind the eardrum.
Tympanometry does not measure your baby’s hearing, but it can detect any changes in pressure in the middle ear, fluid behind the eardrum, or a hole in the eardrum – all of which can affect your baby’s hearing.
Typically the child sits in a parent’s lap, a small rubber probe is inserted into the ear, and results are obtained within seconds. The results from tympanometry can help assess impacted earwax, middle ear fluid, eustachian tube dysfunction, eardrum perforations, and the status of pressure equalization tubes.
A tympanogram puts the tympanometry results into a graph. A “flat” line on a tympanogram may indicate that the eardrum can’t move, while a “peaked” pattern usually suggests that the ear drum is moving normally. Doctors who do this exam should also do a visual ear examination and see the ear drum.
Middle ear muscle reflex
The middle ear muscle reflex (MEMR) (also called acoustic reflex test) tests how well the ear responds to loud sounds by evoking a reflex. In a healthy ear, this reflex helps protect the ear against loud sounds.
For the middle ear muscle reflex (MEMR), a soft rubber tip is placed in the ear canal. A series of loud sounds are sent through the tips into the ears and a machine records whether the sound has triggered a reflex. Sometimes the test is done while the child is sleeping.
What does it mean if my baby’s referred to a hearing specialist?
If the screening test results don’t show a clear response from one or both of your baby’s ears, an appointment will be made with a hearing specialist at an audiology clinic. Even if this happens, it doesn’t necessarily mean your baby has permanent hearing loss.
A hearing specialist should see you within 4 weeks of your baby’s hearing test. It’s important that you attend the appointment in case your baby does have permanent hearing loss.
The appointment will usually take about 1 to 2 hours. This includes time to settle your baby. If possible, feed your baby shortly before the hearing test. Make sure you have everything you need to keep them comfortable and happy.
The tests give more detailed information about your baby’s hearing. They won’t hurt or be uncomfortable for your baby, and you’ll be able to stay with them while the tests are done.
You may want to take your partner or a friend or relative with you to the appointment.
Your audiologist will usually be able to explain the results at the end of the appointment. They’ll explain what the results mean for your baby’s hearing and whether they need any more tests.
Toddler hearing test
Evaluating hearing in infants and toddlers may include the use of the above tests, as well as a behavioral test called visual reinforcement audiometry. In this test, your child is trained to look toward a toy or short video in response to a sound source. Visual reinforcement audiometry testing is possible once your child is able to sit independently and is most often performed with children between 6 months and 30 months of age.
Preschoolers hearing test
Hearing evaluation in preschoolers may include any of the above tests, as well as conditioned play audiometry. During a conditioned play audiometry test, your child is asked to respond to sounds by playing a simple game, such as throwing a block or stacking a tower. Testing is usually performed through earphones and requires your child’s cooperation. This testing is most often performed with children between 30 months and 4 years of age.
School-age children hearing test
Evaluating hearing in school-age children may include the above tests, but most often is similar to the hearing test used for adults, called conventional audiometry. In this test, your child is asked to respond to sounds played through earphones. Testing resembles adult hearing testing (e.g., raise your hand when you hear a beep) and requires your child’s cooperation. This testing is most often performed on children 4 years of age and older.