Contents
Hereditary coproporphyria
Hereditary coproporphyria (HCP) is a rare inherited form of liver (hepatic) porphyria, that involve defects in heme or ‘haem’ biosynthetic pathway caused by mutations (changes) in the CPOX gene which results in deficiency of the enzyme coproporphyrinogen oxidase or coproporphyrinogen-III oxidase (CPOX), the sixth enzyme in the heme biosynthetic pathway that produces porphyrins and heme. Hereditary coproporphyria (HCP) is characterized by neurological symptoms in the form of episodes (acute attacks) of stomach pain, nausea, vomiting, weakness, numbness, and pain in the hands and feet (neuropathy) 1, 2, 3, 4, 5, 6, 7, 8, 9, 10. The porphyrias are a group of blood conditions caused by a lack of an enzyme in the body that makes heme or haem, an important molecule that carries oxygen throughout the body and is vital for all of the body’s organs 11.
Hereditary coproporphyria (HCP) is caused by mutations in the CPOX (coproporphyrinogen oxidase) gene that provides instructions for making an enzyme known as coproporphyrinogen oxidase (CPOX). The enzyme coproporphyrinogen oxidase or coproporphyrinogen-III oxidase (CPOX) enzyme is involved in the production of a molecule called heme (haem). Heme is vital for all of the body’s organs, although it is most abundant in the blood, bone marrow, and liver. Heme or haem is an essential component of iron (Fe) containing proteins called hemoproteins, including hemoglobin (the protein that carries oxygen in the blood), which is necessary to bind oxygen in the bloodstream and transport of oxygen in your body. Heme molecule also helps in respiration, detoxification of drugs, and other different biological functions. In hemoglobin (Hb), iron exists as ferrous (Fe2+) iron ion that is located at the center of the porphyrin ring, held in place by the four nitrogen atoms of the pyrrole rings. Normally, your body makes heme (haem) in a multi-step process that requires 8 different enzymes. Porphyrins are made during several steps of this process. Coproporphyrinogen oxidase (CPOX) enzyme is responsible for the sixth step in this process, the removal of carbon and oxygen atoms from coproporphyrinogen III (the product of the fifth step) to form protoporphyrinogen IX (PPIX). In subsequent steps, two other enzymes modify protoporphyrinogen IX (PPIX) and incorporate an iron atom to produce heme.
In people with hereditary coproporphyria (HCP), the coproporphyrinogen oxidase (CPOX) enzyme deficiency results in the accumulation of porphyrin precursors in their body. Symptoms usually begin around 20 to 30 years of age, but have been reported at younger ages. Signs and symptoms present during the attacks may include body pain, nausea and vomiting, increased heart rate (tachycardia) and high blood pressure 1. Less common symptoms include seizures, skin lesions, and paralysis of the arms and legs, body trunk, and respiratory muscles. Most individuals with hereditary coproporphyria do not have any signs or symptoms between attacks 12.
In hereditary coproporphyria (HCP) the CPOX gene mutation is inherited in an autosomal dominant manner meaning that a mutation is present in only one of the pair of coproporphyinogen oxidase (CPOX) genes. However, the enzyme coproporphyrinogen oxidase (CPOX) deficiency by itself is not sufficient to produce symptoms of the disease and most individuals with a CPOX gene mutation do not develop symptoms of hereditary coproporphyria (HCP). Additional factors such as endocrine factors (e.g. hormonal changes), the use of certain drugs, excess alcohol consumption, infections, and fasting or dietary changes are required to trigger the appearance of symptoms 11. Some affected individuals experience acute attacks or episodes that develop over a period of days. The course and severity of attacks is highly variable from one person to another. In some cases, particularly those without proper diagnosis and treatment, the disorder can cause life-threatening complications.
Hereditary coproporphyria (HCP) is rare. The exact incidence is unknown. One study suggested that about 0.02 per 10 million people per year have hereditary coproporphyria in Europe 13. Females are more commonly affected than males. Because hereditary coproporphyria is often misdiagnosed and many people who have CPOX gene mutations do not have symptoms, the incidence of hereditary coproporphyria may be higher.
Acute hepatic porphyria should be suspected in individuals with the following symptoms or findings 1:
- Nausea for at least 48 hours
- Abdominal, back, or extremity pain for at least 48 hours
- New-onset seizures
- Hyponatremia
- Family history of porphyria
Hereditary coproporphyria (HCP) diagnosis is based on the symptoms and specific blood, urine and stool testing. Treatment is based on preventing the symptoms. An acute attack requires hospitalization, medications, and treatment with heme therapy 14.
Figure 1. Hereditary coproporphyria (HCP)
Footnotes: In hereditary coproporphyria (HCP), coproporphyrinogen and uroporphyrinogen accumulate in patients, causing acute attacks, abdominal pain, and motor neuropathy. Skin signs and symptoms including photosensitivity also occur. Heme arginate is an effective treatment for hereditary coproporphyria (HCP), and Givosiran may also prevent the development of symptoms.
[Source 2 ]Figure 2. Porphyrin molecular structure
Footnote: Molecular structure of porphyrin (M represent metal ions, such as Mg, Cu, Fe, Zn, etc.).
[Source 15 ]Figure 3. Hemoglobin molecular structure
[Source 16 ]Figure 4. Heme biosynthesis pathway
Footnotes: The heme biosynthetic pathway requires 8 enzymatic steps. Heme synthesis pathway showing the enzymes involved in the heme synthesis pathway and the associated porphyrias with the disruption of each specific enzyme. Gain-of-function variants in ALAS2 result in X-linked protoporphyria (XLP), and loss-of-functions variants in FECH result in erythropoietic protoporphyria (EPP). In both X-linked protoporphyria (XLP) and erythropoietic protoporphyria (EPP), metal-free protoporphyrin IX (PPIX) accumulates in erythroblasts, erythrocytes, the plasma, and the biliary system. Metal-free protoporphyrin IX (PPIX) is photosensitive, particularly to visible light in the blue range, and the light-mediated activation of metal-free protoporphyrin IX (PPIX) produces free radicals that damage the surrounding tissues.
Enzymes, encoded by genes, catalyze each of the steps. Gene mutations cause deficient enzyme production. Disruptions are indicated by red lines connecting enzymes with the resultant porphyrias. ALAS (ALAS2) = aminolevulinate synthase (aminolevulinate synthase 2); ALAD = delta-aminolevulinic acid dehydratase; PBGD = porphobilinogen dehydratase; HMBS = hydroxymethylbilane synthase; UROS = uroporphyrinogen-III synthase; UROD = uroporphyrinogen III decarboxylase; CPOX = coproporphyrinogen-III oxidase; PPOX = protoporphyrinogen oxidase; FECH = ferrochelatase.
Porphyrias resulting from disruption of enzyme production. XLP (X-linked protoporphyria); ADP (aminolevulinic acid dehydratase porphyria); AIP (acute intermittent porphyria); CEP (congenital erythropoietic porphyria); PCT (porphyria cutanea tarda); HCP (hereditary coproporphyria); VP (variegate porphyria); EPP (erythropoietic protoporphyria).
Abbreviations: ALA = aminolevulinic acid; PBG = porphobilinogen; HMB = hydroxymethylbilane; URO III = uroporphyrinogen III; COPRO III = coproporphyrinogen III; PROTO’gen IX protoporphyrinogen IX; PPIX = protoporphyrin IX; Fe2+ = iron.
[Source 17 ]Hereditary coproporphyria causes
Hereditary coproporphyria is caused by a genetic change (mutation) in the CPOX (coproporphyrinogen oxidase) gene that provides instructions for making an enzyme known as coproporphyrinogen oxidase or coproporphyrinogen-III oxidase (CPOX), the sixth enzyme in the heme biosynthetic pathway that produces porphyrins and heme (haem). Heme is vital for all of the body’s organs, although it is most abundant in the blood, bone marrow, and liver. Heme or haem is an essential component of iron (Fe) containing proteins called hemoproteins, including hemoglobin (the protein that carries oxygen in the blood), which is necessary to bind oxygen in the bloodstream and transport of oxygen in your body. Heme molecule also helps in respiration, detoxification of drugs, and other different biological functions. In hemoglobin (Hb), iron exists as ferrous (Fe2+) iron ion that is located at the center of the porphyrin ring, held in place by the four nitrogen atoms of the pyrrole rings. Normally, your body makes heme (haem) in a multi-step process that requires 8 different enzymes. Porphyrins are made during several steps of this process. Coproporphyrinogen oxidase (CPOX) enzyme is responsible for the sixth step in this process, the removal of carbon and oxygen atoms from coproporphyrinogen III (the product of the fifth step) to form protoporphyrinogen IX (PPIX). In subsequent steps, two other enzymes modify protoporphyrinogen IX (PPIX) and incorporate an iron atom to produce heme.
More than 65 CPOX gene mutations have been identified in hereditary coproporphyria (HCP) patients 18. The majority of the hereditary coproporphyria (HCP) patients were heterozygous for the mutant and normal CPOX alleles.
However, having a CPOX gene mutation alone does not cause symptoms and most individuals with a CPOX gene mutation do not develop symptoms of hereditary coproporphyria (HCP). Additional factors such as endocrine factors (e.g. hormonal changes), the use of certain drugs, excess alcohol consumption, infections, and fasting or dietary changes are required to trigger the appearance of symptoms 11. Some people with CPOX gene mutations never have symptoms of hereditary coproporphyria 1.
The penetrance of CPOX gene mutations is unknown, as acute attacks are rare in comparison to acute intermittent porphyria (AIP), suggesting that clinical disease only manifests in a small number of CPOX gene heterozygotes 1. A study investigating a family with hereditary coproporphyria (HCP) found that of 14 members diagnosed with disease only 1 expressed clinical manifestations 1, 19.
Certain CPOX pathogenic alleles (notably D400-K404 in exon 6) in the homozygous state result in a disorder called harderoporphyria 20. Some pathogenic variants may affect the active site of the enzyme, possibly causing premature separation of CPOX from its substrate 1. The result is incomplete decarboxylation of COPROgen, yielding the tricarboxylic intermediate harderoporphyrinogen instead of dicarboxylic PROTOgen 1.
Heterozygotes for a CPOX pathogenic variant that is associated with harderoporphyria have no symptoms; those with biallelic pathogenic variants have large amounts of harderoporphyrin in the stool and neonatal onset of hemolytic anemia and jaundice, which can resemble congenital erythropoietic porphyria, an autosomal recessive condition with hemolysis and severe photosensitivity in infancy 1. They can also have acute porphyric attacks with high levels of urinary delta-aminolevulinic acid (ALA) and porphobilinogen (PBG). One infant died at age five months, apparently from complications of an acute attack 20. Some develop normally while others exhibit short stature 1.
A recent study investigating seven cases of hereditary coproporphyria (HCP) from a single family with a novel mutation found evidence contrasting current literature including a notably high disease penetrance, high rate of severe, recurrent attacks, and a high incidence of venous-thromboembolism, a phenomenon not known to be associated with acute porphyria 3.
If a question of drug safety arises, a physician or medical center specializing in porphyria should be contacted. A list of these institutions may be obtained from the American Porphyria Foundation. The American Porphyria Foundation offers a drug database with safety information about the interaction of specific drugs in patients with porphyria (https://porphyriafoundation.org/for-healthcare-professionals/ahp-drug-safety-database/) or https://porphyriafoundation.org/drugdatabase/drug-safety-database-search/.
The EPNET/NAPOS Database should also be consulted. The Norwegian Porphyria Centre (NAPOS), with the European Porphyria Network (EPNET), has created a list of medications that clinicians must avoid using in porphyria patients (https://drugsporphyria.net/). These drugs include ketamine, thiopental, chloramphenicol, erythromycin, nitrofurantoin, rifampicin, trimethoprim/sulfamethoxazole, spironolactone, methyldopa, valproic acid, carbamazepine, phenytoin, phenobarbital, primidone, and risperidone 21. For information on prescribing medication in the context of certain conditions (e.g., HIV, epilepsy, malaria), see https://porphyria.uct.ac.za/porphyria-professionals/prescribing-porphyria-treatment-specific-disorders-poprhyria/therapy-epilepsy.
Circumstances and risk factors associated with acute attacks
Circumstances commonly associated with acute attacks are caloric deprivation, changes in female reproductive hormones, and use of porphyria-inducing medications or drugs 1:
- Caloric deprivation. Fasting appears to sensitize the heme-synthetic pathway to an inducer, which could be external (i.e., a medication) or internal (ovarian hormones). The sensitizing effect of caloric deprivation was demonstrated in the 1960s in experimental animals and has been confirmed by clinical observation. People who fail to eat because of intercurrent illness or who undertake drastic weight loss are predisposed to an acute attack. First attacks have been reported after reduction gastroplasty for obesity 22. CPOX heterozygotes (having two different CPOX gene) undergoing surgery are at risk because of the routine preoperative fast. This and other anecdotal experience have led to consensus that the first line of treatment for an acute attack is intravenous glucose, which is occasionally helpful.
- Changes in female reproductive hormones. A role for female reproductive hormones can be inferred from the fact that acute attacks are infrequent prior to menarche and after menopause. Some women have monthly attacks that appear a few days before the onset of menstruation (when progestins peak). Attacks have been linked to use of oral contraceptives; the risk may be associated more with the progesterone component than the estrogen component.
- Use of porphyria-inducing medications or drugs. The American Porphyria Foundation offers a drug database with safety information about the interaction of specific drugs in patients with porphyria (https://porphyriafoundation.org/for-healthcare-professionals/ahp-drug-safety-database/) or https://porphyriafoundation.org/drugdatabase/drug-safety-database-search/. The EPNET/NAPOS Database should also be consulted. The Norwegian Porphyria Centre (NAPOS), with the European Porphyria Network (EPNET), has created a list of medications that clinicians must avoid using in porphyria patients (https://drugsporphyria.net/). These drugs include ketamine, thiopental, chloramphenicol, erythromycin, nitrofurantoin, rifampicin, trimethoprim/sulfamethoxazole, spironolactone, methyldopa, valproic acid, carbamazepine, phenytoin, phenobarbital, primidone, and risperidone 21. For information on prescribing medication in the context of certain conditions (e.g., HIV, epilepsy, malaria), see https://porphyria.uct.ac.za/porphyria-professionals/prescribing-porphyria-treatment-specific-disorders-poprhyria/therapy-epilepsy.
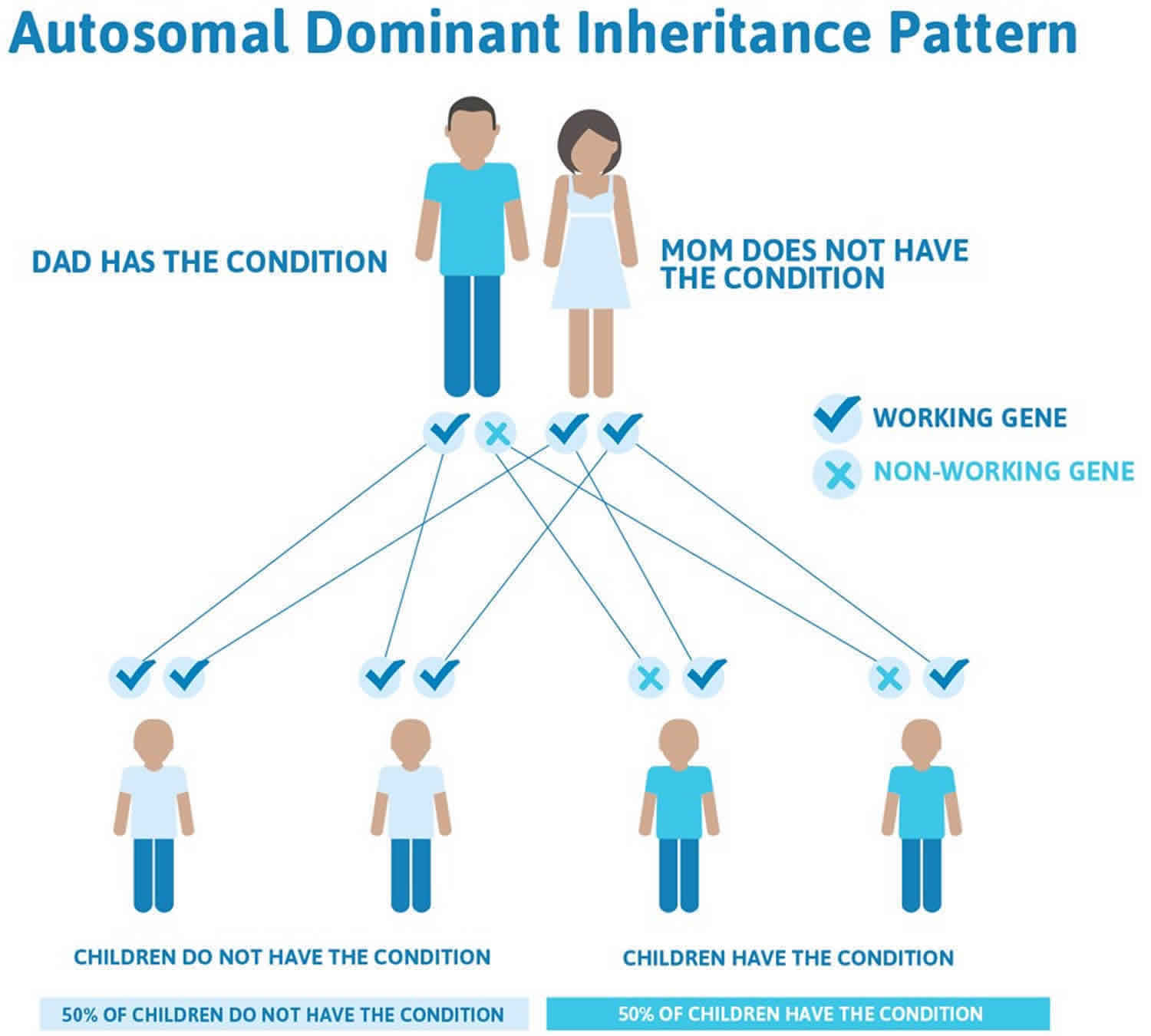
Hereditary coproporphyria inheritance pattern
Hereditary coproporphyria (HCP) is inherited in an autosomal dominant pattern 1. All individuals inherit two copies of each gene. In autosomal dominant conditions, having a mutation in just one copy of the CPOX gene causes the person to have hereditary coproporphyria. The mutation can be inherited from either parent. Some people are born with hereditary coproporphyria due to a new genetic mutation (de novo) and do not have a history of this condition in their family. There is nothing either parent can do, before or during pregnancy, to cause a child to have this.
Each child of an individual with an autosomal dominant condition has a 50% or 1 in 2 chance of inheriting the mutation and the condition. Offspring who inherit the mutation may develop hereditary coproporphyria, although they could be more or less severely affected than their parent. Sometimes a person may have a CPOX gene mutation for hereditary coproporphyria and show no signs or symptoms of it.
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
There are cases of autosomal dominant gene changes, or mutations, where no one in the family has it before and it appears to be a new thing in the family. This is called a de novo mutation. For the individual with the condition, the chance of their children inheriting it will be 50%. However, other family members are generally not likely to be at increased risk.
Genetic counseling is recommended for affected individuals and their families.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://abgc.learningbuilder.com/Search/Public/MemberRole/Verification) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (https://clinics.acmg.net/) has a searchable database of medical genetics clinic services in the United States.
Figure 5. Hereditary coproporphyria autosomal dominant inheritance pattern
Hereditary coproporphyria symptoms
The symptoms of hereditary coproporphyria may be different from person to person. Some people may be more severely affected than others and not everyone with hereditary coproporphyria will have the same symptoms. Many individuals with a CPOX gene mutation do not experience any symptoms of hereditary coproporphyria 12.
In people with hereditary coproporphyria, additional factors; such as hormonal changes, certain drugs, excess alcohol consumption, infections, and fasting or dietary changes; may trigger the appearance of symptoms. Symptoms appear as acute attacks or episodes that develop over the course of several hours or a few days. The timing and severity of attacks vary from one person to another 11. Some affected individuals experience acute attacks or episodes that develop over a period of days. The course and severity of attacks is highly variable from one person to another. In some cases, particularly those without proper diagnosis and treatment, the disorder can cause life-threatening complications.
Hereditary coproporphyria (HCP) is associated with neurovisceral symptoms i.e., acute attacks, severe abdominal pain, motor neuropathy and more rarely psychiatric symptoms, similar to acute intermittent porphyria (AIP) and variegate porphyria (VP) 23.
The symptoms of an acute attack include 1:
- Severe stomach pain leading to nausea and vomiting
- Back and leg pain
- High blood pressure
- Rapid heartbeat (tachycardia)
- Seizures (less common)
- Weakness, numbness in the arms and legs (peripheral neuropathy)
- Skin findings (in about 20% of people with hereditary coproporphyria)
- extreme sensitivity to sunlight (photosensitivity)
- fragile skin
In between attacks, people with hereditary coproporphyria are often symptom-free.
The episodes or “attacks” that characterize hereditary coproporphyria usually develop over the course of several hours or a few days. Affected individuals usually recover from an attack within days 24. However, if an acute attack is not diagnosed and treated promptly recovery can take much longer, even weeks or months 24. Most affected individuals do not exhibit any symptoms in between episodes 24. Onset of attacks usually occurs in the 20s or 30s, but may occur at or just after puberty. Onset before puberty is extremely rare 24. Attacks are more common in women than men.
Intermittent, recurrent body pain, usually affecting the abdomen and the lower back may occur chronically. Pain in these areas is often the initial sign of an attack. Pain usually begins as low-grade, vague pain in the abdomen and slowly over a few days worsens eventually causing severe abdominal pain. Pain may radiate to affect the lower back, neck, buttocks, or arms and legs. Pain is usually not well localized, but in some cases can be mistaken for inflammation of the gallbladder, appendix or another intra-abdominal organ. In a minority of cases, pain primarily affects the back and the arms and legs and is usually described as deep and aching. Abdominal pain is often described as colicky and is usually associated with nausea and vomiting. Vomiting may be severe enough that affected individuals vomit after eating or drinking any food or liquid. The absence of bowel sounds (ileus), which indicates a lack of intestinal activity may be noted. Constipation may also occur and can be severe (obstipation). Affected individuals may also experience a faster than normal heart rate (tachycardia), high blood pressure (hypertension), irregular heartbeats (cardiac arrhythmias), and a sudden fall in blood pressure upon standing (orthostatic hypotension). Hypertension may persist in between acute attacks.
Neurologic symptoms, including seizures, may be associated with hereditary coproporphyria. In some cases, new-onset seizures may be the initial sign of the disorder. Abnormally low sodium levels in the blood (hyponatremia) may occur during an attack and contribute to the onset of seizures. Affected individuals may also develop damage to the nerves in the extremities (peripheral neuropathy). Peripheral neuropathy may be preceded by the loss of deep tendon reflexes. Peripheral neuropathy is characterized by numbness or tingling and burning sensations that, in hereditary coproporphyria, usually begin in the upper legs and arms. Affected individuals may develop muscle weakness initially in the feet and legs that progresses to affect and paralyze all extremities and the body trunk (motor paralysis) and the respiratory muscles (respiratory paralysis and failure).
This ascending paralysis in hereditary coproporphyria can mimic the ascending paralysis seen in Guillain-Barre syndrome, a disorder in which the body’s immune system attacks the nerves. Differentiating hereditary coproporphyria (HCP) from Guillain-Barre syndrome (GBS) is extremely important to ensure prompt treatment of hereditary coproporphyria and the avoidance of medications that can precipitate or worsen an acute attack.
Some individuals develop psychological symptoms, although such symptoms are highly variable. Such symptoms can include irritability, depression, anxiety, and insomnia. Less often, more acute psychiatric symptoms can develop including hallucinations, paranoia, disorientation, mental confusion, delirium, and psychosis.
In some cases, affected individuals may develop skin (cutaneous) lesions affecting the sun-exposed areas of skin such as the hands and face. Affected individuals may develop severe pain, burning, and itching of such areas (photosensitivity). Eventually, the skin may become fragile and develop fluid-filled blisters (bullae). Affected areas may also exhibit darkly discolored (hyperpigmented) scars and excessive hair growth.
Acute Attacks
The initial symptoms of an acute attack are nonspecific, consisting of low-grade abdominal pain that slowly increases over a period of days (not hours) with nausea progressing to vomiting of all oral intake 1.
Typically the pain is not well localized but in some instances does mimic acute inflammation of the gallbladder, appendix, or other intra-abdominal organ 1. In most instances the abdominal examination is unremarkable except for diminished bowel sounds consistent with ileus, which is common and can be seen on abdominal radiography. Typically fever is absent. In a young woman of reproductive age, the symptoms may raise the question of early pregnancy.
Prior to the widespread use of abdominal imaging in the emergency room setting, some individuals with abdominal pain and undiagnosed acute porphyria underwent urgent exploratory surgery. Therefore, a history of abdominal surgery with negative findings was considered characteristic of acute porphyria 1.
A minority of affected individuals has predominantly back or extremity pain, which is usually deep and aching, not localized to joints or muscle groups.
Neurologic signs and symptoms
Seizures may occur early in an attack and be the problem that brings the affected individual to medical attention 1. In a young woman with abdominal pain and new-onset seizures, it is critical to consider acute porphyria because of the implications for seizure management.
When an attack is unrecognized as such or treated with inappropriate medications, it may progress to a motor neuropathy, which typically occurs many days to a few weeks after the onset of symptoms 2. The neuropathy first appears as weakness proximally in the arms and legs, then progresses distally to involve the hands and feet 2. Neurosensory function remains largely intact.
In some individuals the motor neuropathy eventually involves nerves serving the diaphragm and muscles of respiration. Ventilator support may be needed 2.
Tachycardia and bowel dysmotility (manifest as constipation) are common in acute attacks and believed to represent involvement of the autonomic nervous system 1, 23.
Of note, when the acute attack is recognized early and treated appropriately, the outlook for survival and eventual complete recovery is good 1. Individuals with frequent recurrent acute attacks defined as more than four attacks per year have historically been at highest risk for development of chronic neurologic manifestations 1. In November 2019, Givosiran, an siRNA that works directly against ALAS1, was approved in the US after demonstrating effectiveness in preventing acute attacks in these individuals. Effective prevention of acute attacks with givosiran may reduce or prevent the development of neurologic sequelae in persons with hereditary coproporphyria (HCP) with frequent recurrent attacks, though this remains to be determined with long-term study 1.
Psychosis
The mental status of people presenting with an acute attack of porphyria varies widely and can include psychosis 1. Commonly the predominant feature is distress including pain that may seem hysterical or feigned, given a negative examination, absence of fever, and abdominal imaging showing some ileus only. Incessant demands for relief may be interpreted as drug-seeking behavior.
Because of the altered affect in acute porphyria, it has been speculated that mental illness is a long-term consequence of an attack and that mental institutions may house disproportionately large numbers of individuals with undiagnosed acute porphyria 1. Screening of residents in mental health facilities by urinary porphobilinogen (PBG) and/or PBG deaminase activity in blood which diagnoses acute intermittent porphyria has been performed, with mixed results 25. The experience of those who have monitored affected individuals over many years suggests that heterozygotes who are at risk for one of the acute porphyrias are no more prone to chronic mental illness than individuals in the general population; however, a prospective study is needed 1.
Kidney and liver disease
In people with any type of acute porphyria, the kidneys and liver may develop chronic changes that often are subclinical. One complication of the liver problem is excess primary liver cancer (hepatocellular carcinoma). The risk is greatest in women older than age 60 with acute intermittent porphyria (AIP) 160-fold increased risk above the general population risk; for men there is a 37-fold increase in risk 26. Liver cancer and the kidney disease may be restricted largely to heterozygotes with chronically elevated plasma or urine delta-aminolevulinic acid (ALA). Hypertension may be chronic in those with frequent symptoms and may contribute to kidney disease.
In as much as delta-aminolevulinic acid (ALA) and porphobilinogen (PBG) tend to be minimally elevated or normal in hereditary coproporphyria (HCP) heterozygotes, the risk of liver and kidney complications may be less in hereditary coproporphyria (HCP) than in acute intermittent porphyria (AIP).
Chronic skin signs and symptoms
Photocutaneous damage is present in only a small minority of those with acute attacks. Specifically, uroporphyrinogen and coproporphyrinogen result in bullae (skin blisters) and fragility in light-exposed skin 1. It has been reported that 20% of patients experiencing acute attacks also experience photosensitivity 1. Bullae (skin blisters) and skin fragility of light-exposed skin, in particular the backs of the hands, result in depigmented scars, erosion, and disfigurement. Facial skin damage also occurs, with excess hair growth (hypertrichosis) on the temples, ears, and cheeks; this is more noticeable in women than in men. Hyperpigmentation and hypopigmentation may also occur in sun-exposed skin. High levels of circulating porphyrins promote brown and reddish discoloration of teeth (erythrodontia) due to the deposition of porphyrins in the enamel layer of the developing tooth 27.
The skin findings in hereditary coproporphyria (HCP) resemble those in porphyria cutanea tarda (PCT) and in variegate porphyria (VP).
Hereditary coproporphyria diagnosis
The diagnosis of hereditary coproporphyria is suspected first based on the characteristic clinical signs and symptoms, usually during an acute attack. The observation of reddish brown urine that is free of blood is indicative, but not conclusive, of an acute porphyria. The intolerance of medications such as oral contraceptives is also suggestive of an acute porphyria. Once a person is suspected of having hereditary coproporphyria, examination of urine, blood, and stool (fecal) samples is typically done. These lab tests are usually done at the time of the acute attack and look for elevated levels of compounds found to be associated with several different types of porphyria 28.
Acute hepatic porphyria should be suspected in individuals with the following symptoms or findings 1:
- Nausea for at least 48 hours
- Abdominal, back, or extremity pain for at least 48 hours
- New-onset seizures
- Hyponatremia
- Family history of porphyria
Screening tests can help diagnose hereditary coproporphyria by measuring the levels of certain porphyrin precursors (e.g. porphobilinogen [PBG] and delta-aminolevulinic acid [ALA] in the urine. Acute attacks are always accompanied by markedly increased excretion of porphobilinogen. During a potential acute attack in an individual suspected of an acute porphyria, a random (spot) urine sample can be tested. If urinary porphobilinogen is sufficiently increased, then a qualitative 24-hour urine analysis for both porphobilinogen and delta-aminolevulinic acid should be performed and compared to urine sample results from when the individual did not exhibit symptoms. Although porphobilinogen and delta-aminolevulinic acid may be increased during an acute attack, they return to normal on recovery.
Individuals with hereditary coproporphyria may have elevated porphyrin levels such as coproporphyrin in the urine, but this finding is nonspecific (e.g. it can also be associated with other conditions) and therefore does not conclusively confirm a diagnosis of hereditary coproporphyria.
The hallmark biochemical feature of hereditary coproporphyria (HCP) is elevated porphyrins, most notably coproporphyrinogen II and uroporphyrinogen, in the urine and feces of affected individuals 1, 23.
Further testing is necessary to exclude hereditary coproporphyria from variegate porphyria or acute intermittent porphyria. Fecal coproporphyrin analysis can be extremely helpful in obtaining the diagnosis. This test can reveal markedly increased levels of coproporphyrin in stool samples, which is characteristic of hereditary coproporphyria.
To identify the specific type of porphyria an individual has, molecular genetic testing can be performed to look for mutations in the CPOX gene 1. Family members of an individual positive for a CPOX mutation can be offered testing for this mutation. Molecular genetic testing is available in certain laboratories specializing in porphyria diagnosis.
At least one study suggesting diagnostic criteria for the acute dominantly inherited forms of porphyria has been published 29.
Individuals and family members who have inherited hereditary coproporphyria should be counseled on how to limit their risk of any future acute attacks. This should include information about hereditary coproporphyria and what causes attacks, how to check if a prescribed medication is safe or unsafe, and details of relevant patient support groups. Membership in the American Porphyria Foundation is very helpful to affected individuals.
Hereditary coproporphyria differential diagnosis
Symptoms of the following disorders can be similar to those of hereditary coproporphyria (HCP). Comparisons may be useful for a differential diagnosis.
Three other forms of porphyria, specifically variegate porphyria (VP), acute intermittent porphyria (AIP), and ALA dehydratase deficiency porphyria (ADP), may develop acute attacks that characterize hereditary coproporphyria (HCP). Collectively, hereditary coproporphyria (HCP), variegate porphyria (VP), acute intermittent porphyria (AIP), and ALA dehydratase deficiency porphyria (ADP) are classified as the acute porphyrias. The skin symptoms that affect some individuals with hereditary coproporphyria (HCP) resemble those seen in variegate porphyria (VP) and porphyria cutanea tarda (PCT), one of the nonacute porphyrias.
Guillain-Barre syndrome (GBS) is a rare, rapidly progressive autoimmune disorder where the body’s immune system mistakenly attacks the peripheral nerves. Guillain-Barre syndrome (GBS) consists of inflammation of the nerves (polyneuritis) causing muscle weakness, ascending paralysis and potentially complete paralysis and sensory problems. Although the precise cause of Guillain-Barre syndrome (GBS) is unknown, a viral or respiratory infection precedes the onset of the syndrome in about half of the cases. The following variants of Guillain-Barre syndrome (GBS) (acute inflammatory neuropathy or acute inflammatory demyelinating polyradiculoneuropathy) are recognized: Miller Fisher syndrome, acute motor-sensory axonal neuropathy, acute motor axonal neuropathy. Most people recover from GBS, but some may experience long-term complications.
Hereditary coproporphyria treatment
There is no specific treatment for hereditary coproporphyria (HCP). Treatment is aimed at managing the symptoms of hereditary coproporphyria that occur during an acute attack. Hospitalization is often necessary for acute attacks, and medications for pain, nausea and vomiting, and close observation are generally required. Initial treatment steps include stopping any medications that can potentially worsen hereditary coproporphyria or cause an attack. All triggering factors should be identified, if possible, and discontinued. In addition, ensuring proper intake of carbohydrate, either orally or intravenously, is essential. Wearing a Medic Alert bracelet or the use of a wallet card is advisable in individuals who have hereditary coproporphyria.
Recommended evaluations following initial diagnosis of hereditary coproporphyria (HCP) 1:
- Review of medications for those thought to induce attacks. The American Porphyria Foundation offers a drug database with safety information about the interaction of specific drugs in patients with porphyria (https://porphyriafoundation.org/for-healthcare-professionals/ahp-drug-safety-database/) or https://porphyriafoundation.org/drugdatabase/drug-safety-database-search/. The EPNET/NAPOS Database should also be consulted. The Norwegian Porphyria Centre (NAPOS), with the European Porphyria Network (EPNET), has created a list of medications that clinicians must avoid using in porphyria patients (https://drugsporphyria.net/). These drugs include ketamine, thiopental, chloramphenicol, erythromycin, nitrofurantoin, rifampicin, trimethoprim/sulfamethoxazole, spironolactone, methyldopa, valproic acid, carbamazepine, phenytoin, phenobarbital, primidone, and risperidone 21. For information on prescribing medication in the context of certain conditions (e.g., HIV, epilepsy, malaria), see https://porphyria.uct.ac.za/porphyria-professionals/prescribing-porphyria-treatment-specific-disorders-poprhyria/therapy-epilepsy.
- Detailed neurologic exam for signs of motor neuropathy (indicating a more advanced attack and the need for early treatment with Panhematin® (hemin for injection). Inquiry into possibility of seizures 30.
- Measurement of serum sodium concentration. Hyponatremia is characteristic and may be profound (serum sodium concentration <110 mEq/L), requiring urgent correction with special precaution for risk of central pontine myelinolysis.
- Quantitation of urinary excretion of porphobilinogen (PBG) on several occasions over a few months to establish baseline. In an acute attack urinary excretion of porphobilinogen (PBG) is substantially elevated over the baseline. For future use in determining if a new symptom or drug reaction is due to an acute attack.
Some attacks may be managed by giving the person a large amount of glucose or other carbohydrates. More severe attacks are treated with heme therapy, given through a vein (intravenously). Panhematin® (hemin for injection), an enzyme inhibitor derived from red blood cells that is potent in suppressing acute attacks of porphyria, is currently the only commercially available heme therapy for treatment and prevention of acute porphyria attacks in the United States. Heme arginate (Normosang®), which is marketed in some other countries, is another type of heme therapy 14. Panhematin® (hemin for injection) almost always returns porphyrin and porphyrin precursor levels to normal values. The U.S. Food and Drug Administration (FDA) originally approved panhematin for the treatment of recurrent attacks of acute intermittent porphyria (AIP) related to the menstrual cycle in susceptible women. Numerous symptoms including pain, hypertension, tachycardia and altered mental status, and neurologic signs have improved in individuals with acute porphyria after treatment with panhematin. Because of its potency, it is usually given after a trial of high-dose carbohydrate of any sort, including glucose therapy and should be administered only by physicians experienced in the management of porphyrias in a hospital setting. Responses to hematin infusion can include reduced urine concentration of porphobilinogen (PBG) (the 1st sign) after 2 doses; clinical improvement after 3 to 4 doses (typically dramatic) with no further need of narcotic analgesia 1. Hemin treatment withdrawal triggered a rapid return of clinical symptoms 23, 31. Furthermore, heme arginate (Normosang®) has been demonstrated as an effective maintenance therapy for patients with hereditary coproporphyria (HCP), and can significantly improve quality of life 1, 23.
Some individuals who experience recurrent attacks may benefit from chronic hematin infusion. This is sometimes recommended for women with severe symptoms during the time of their menses.
Attacks can also be avoided by avoiding the ‘trigger’ for the attack. The trigger can be different for different people. Triggers include certain medications, alcohol, dieting, and hormonal changes in the body. Sometimes, however, the trigger is unknown. If the person with hereditary coproporphyria has skin symptoms, avoiding excess sun exposure can reduce the blisters and skin lesions 32.
In 2019, the FDA approved Givosiran (Givlaari) to treat adults with acute hepatic porphyria, including hereditary coproporphyria (HCP). Givosiran (Givlaari) is a small interfering RNA (siRNA) that targets the mRNA of the enzyme aminolevulinate synthase 1 (ALAS1). By doing so, it reduces the production of aminolevulinic acid (ALA) and porphobilinogen (PBG), the toxic substances that accumulate in acute hepatic porphyria. Givlaari aims to prevent attacks from occuring and may reduce or prevent the development of neurologic symptoms in persons with hereditary coproporphyria (HCP); however, this remains to be determined with long-term studies 1. In a phase 3 trial of Givosiran, only one individual with hereditary coproporphyria (HCP) was included in the study, although reports indicate clinical response 33.
Other treatments include glucose administration to reverse fasting state, dextrose rehydration for hyponatremia, and anti-seizure medications 1.
Treatment for hereditary coproporphyria may also include drugs to treat specific symptoms such as certain pain medications (analgesics), anti-anxiety drugs, anti-hypertensive drugs, and drugs to treat nausea and vomiting, tachycardia, or restlessness. Medications to treat any infections that may occur at the same time as an attack (intercurrent infection) may also be necessary. Seizures may require treatment with anti-seizure (anti-convulsant) medications, but many of the common options can worsen an attack and are contraindicated. A short-acting benzodiazepine or magnesium may be recommended. Gabapentin and propofol are considered effective and safe for prolonged control of seizures.
Although many types of drugs are believed to be safe in individuals with hereditary coproporphyria, recommendations about drugs for treating hereditary coproporphyria are based upon experience and clinical study. Since many commonly used drugs have not been tested for their effects on porphyria, they should be avoided if at all possible. If a question of drug safety arises, a physician or medical center specializing in porphyria should be contacted. The American Porphyria Foundation offers a drug database (https://porphyriafoundation.org/drugdatabase/drug-safety-database-search) with safety information about the interaction of specific drugs in patients with porphyria.
Additional treatment for individuals undergoing an attack includes monitoring for muscle weakness and respiratory issues and monitoring fluid and electrolyte balances. For example, if affected individuals develop low blood sodium level (hyponatremia), which can induce seizures, they should be treated by restricting the intake of water (water deprivation). If serum sodium is decreased severely, e.g. from normal (>134 meq/dl) to very low (100-115 meq/dl), then saline infusion is indicated.
Premenstrual attacks often resolve quickly with the onset of menstruation. Hormone manipulation may be effective in preventing such attacks. Some affected women have been treated with gonadotropin-releasing hormone analogues to suppress ovulation and prevent frequent cyclic attacks.
In some cases, an attack is precipitated by a low intake of carbohydrates in an attempt to lose weight. Consequently, dietary counseling is very important. Affected individuals who are prone to attacks should eat a normal carbohydrate diet and should not greatly restrict their intake of carbohydrates or calories, even for short periods of time. If weight loss is desired, it is advisable to contact a physician and dietitian.
In individuals who develop skin complications, avoidance of sunlight will be of benefit and can include the use of double layers of clothing, long sleeves, wide brimmed hats, gloves, and sunglasses. Topical sunscreens are generally ineffective. Affected individuals will also benefit from window tinting and the use of vinyl or films to cover the windows of their homes and cars. Avoidance of sunlight can potentially cause vitamin D deficiency and some individuals may require supplemental vitamin D.
A liver transplant has been used to treat some individuals with acute forms of porphyria, specifically individuals with severe disease who have failed to respond to other treatment options. A liver transplant in individuals with hereditary coproporphyria is an option of last resort.
Hereditary coproporphyria diet
In some cases, an attack is precipitated by a low intake of carbohydrates in an attempt to lose weight. Consequently, dietary counseling is very important. Affected individuals who are prone to attacks should eat a normal carbohydrate diet and should not greatly restrict their intake of carbohydrates or calories, even for short periods of time. If weight loss is desired, it is advisable to contact a physician and dietitian.
Because glucose is used to treat acute attacks, its use in preventing attacks has been suggested and is in fact touted in lay discussions of porphyria; however, there is no evidence that heterozygotes can protect themselves by overeating or adopting a high-carbohydrate diet, and they risk becoming obese 28. Heterozygotes should adhere to a healthful diet with the usual balance of protein, fat, and carbohydrate. Weight loss is possible but only by incremental restriction of calories combined with exercise. Extreme diets (e.g., all bacon, all brown rice, starvation) are risky and should be avoided.
Pregnancy management
The effect of pregnancy on inducing acute attacks is unpredictable. In general, serious problems during pregnancy are unusual. In fact, some women with recurrent symptoms associated with the menstrual cycle report improvement during pregnancy. Attacks, if they occur, are usually in the first trimester. The women most at risk are those with hyperemesis gravidarum and inadequate caloric intake 34. Among antiemetics, ondansetron is not expected to precipitate or exacerbate acute attacks, although several studies have suggested that ondansetron exposure in the first trimester of pregnancy could lead to an increased risk of cleft palate and/or congenital heart defects in the fetus. These suggested risks have not been confirmed. However, metoclopramide should be avoided, as it may precipitate acute attacks 35.
The experience with administration of hematin (or heme arginate, which is not available in the US) during pregnancy is limited. Badminton and Deybach 36 published an anecdotal report of successful heme arginate treatment (without adverse fetal effect) in several women experiencing attacks of variegate porphyria or other acute porphyrias during pregnancy. Based on the absence of reported adverse effects, use of hematin to control exacerbations of acute intermittent porphyria during pregnancy has been recommended 37.
Prenatal testing and preimplantation genetic diagnosis
Once the CPOX pathogenic variant has been identified in an affected family member, prenatal testing for a pregnancy at increased risk and preimplantation genetic diagnosis for hereditary coproporphyria are possible.
Differences in perspective may exist among medical professionals and within families regarding the use of prenatal testing, particularly if the purpose is pregnancy termination rather than early diagnosis. While most centers would consider decisions regarding prenatal testing to be the choice of the parents, discussion of these issues is appropriate. Parents are encouraged to seek genetic counseling before reaching a decision on the use of prenatal testing.
Note: The presence of a CPOX pathogenic variant detected by prenatal testing does not predict whether individuals will be symptomatic, or if they are, what the severity of the clinical manifestations will be. It is common for the offspring who inherit the CPOX pathogenic variant from a severely affected individual to be completely asymptomatic.
Hereditary coproporphyria prognosis
The prognosis is usually good if the disease is recognized and treated promptly, before nerve damage develops. Although symptoms usually resolve after an attack, recovery of neuromuscular function (in a severe case) may require several months or longer. Mental symptoms may occur during attacks but are not chronic. Premenstrual attacks often resolve quickly with the onset of menses.
Can attacks be prevented?
Yes, particularly with regard to drugs and diet. Genetic hereditary coproporphyria carriers should become informed on drugs and other factors that can lead to symptoms (see above). They should be prepared to point their healthcare providers to drugs and medications to avoid. A Medic Alert bracelet is useful for a situation in which the patient is incapacitated. Very frequent premenstrual attacks can be prevented by a gonadotropin-releasing hormone (GnRH) analogue administered with expert guidance. In selected cases, frequent noncyclic attacks can be prevented by once- or twice-weekly infusions of hemin.
Individuals who are prone to attacks should consume a normal balanced diet. Despite online discussion, there is no evidence that pushing carbohydrate prevents attacks, and it has the side effect of weight gain, which is undesirable for most people. Fasting, fad diets (for example, high protein) and gastric reduction surgery should be avoided. If weight loss is desired, it is advisable to consult a physician and a dietitian about an individualized diet with modest caloric restriction, which will produce gradual weight loss without increasing the risk of an attack of porphyria. Exercise is safe in porphyria, and recommended.
Hereditary coproporphyria life expectancy
Most patients (60-80%) with hereditary coproporphyria who have an acute attack of porphyria never have another. Avoiding precipitating factors also helps prevent attacks. Researchers consider coproporphyria a less severe disease than Acute Intermittent Porphyria.
The long term outlook for people with hereditary coproporphyria varies with the severity of the symptoms. With early diagnosis and treatment, hereditary coproporphyria is rarely life-threatening. Some people with hereditary coproporphyria may have long-term pain and may be at increased risk for liver and kidney disease 28.
- Wang B, Bissell DM. Hereditary Coproporphyria. 2012 Dec 13 [Updated 2022 May 19]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK114807[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Balogun O, Nejak-Bowen K. Understanding Hepatic Porphyrias: Symptoms, Treatments, and Unmet Needs. Semin Liver Dis. 2024 May;44(2):209-225. doi: 10.1055/s-0044-1787076[↩][↩][↩][↩][↩]
- Towns C, Balakrishnan S, Florkowski C, Davies A, Barrington-Ward E. High penetrance, recurrent attacks and thrombus formation in a family with hereditary coproporphyria. JIMD Rep. 2022 Mar 18;63(3):211-215. doi: 10.1002/jmd2.12281[↩][↩]
- Kaftory R, Edel Y, Snast I, Lapidoth M, Mamet R, Elis A, Hodak E, Levi A. Greater disease burden of variegate porphyria than hereditary coproporphyria: An Israeli nationwide study of neurocutaneous porphyrias. Mol Genet Metab Rep. 2021 Jan 13;26:100707. doi: 10.1016/j.ymgmr.2021.100707[↩]
- Eroglu S, Birsenogul I. Delirium with delayed diagnosis of hereditary coproporphyria. Clin Case Rep. 2022 Jun 2;10(6):e05937. doi: 10.1002/ccr3.5937[↩]
- Edel Y, Mamet R, Sagy I, Snast I, Kaftory R, Mimouni T, Levi A. A 25-Hour Fast Among Quiescent Hereditary Coproporphyria and Variegate Porphyria Patients is Associated With a Low Risk of Complications. Rambam Maimonides Med J. 2023 Jan 29;14(1):e0003. doi: 10.5041/RMMJ.10490[↩]
- Whatley SD, Mason NG, Woolf JR, Newcombe RG, Elder GH, Badminton MN. Diagnostic strategies for autosomal dominant acute porphyrias: retrospective analysis of 467 unrelated patients referred for mutational analysis of the HMBS, CPOX, or PPOX gene. Clin Chem. 2009 Jul;55(7):1406-14. doi: 10.1373/clinchem.2008.122564[↩]
- Anderson KE, Bloomer JR, Bonkovsky HL, Kushner JP, Pierach CA, Pimstone NR, Desnick RJ. Recommendations for the diagnosis and treatment of the acute porphyrias. Ann Intern Med. 2005 Mar 15;142(6):439-50. doi: 10.7326/0003-4819-142-6-200503150-00010. Erratum in: Ann Intern Med. 2005 Aug 16;143(4):316.[↩]
- Valle, G. , Carmine Guida, C. , Nasuto, M. , Totaro, M. , Aucella, F. , Frusciante, V. , Di Mauro, L. , Potenza, A. , Savino, M. , Stanislao, M. , Popolizio, T. , Guglielmi, G. , Giagulli, V. A. , Guastamacchia, E. , & Triggiani, V. (2016). Cerebral hypoperfusion in hereditary coproporphyria (HCP): A single photon emission computed tomography (SPECT) study. Endocrine, Metabolic & Immune Disorders‐Drug Targets, 16, 39–46. 10.2174/1871530316666151218151101[↩]
- Liu A, Zhou L, Zhu H, Li Y, Yang J. Systemic Lupus Erythematosus and Hereditary Coproporphyria: Two Different Entities Diagnosed by WES in the Same Patient. Biomed Res Int. 2022 May 28;2022:9096999. doi: 10.1155/2022/9096999[↩]
- Hereditary coproporphyria. https://rarediseases.org/rare-diseases/hereditary-coproporphyria[↩][↩][↩][↩]
- Wang B, Rudnick S, Cengia B, Bonkovsky HL. Acute Hepatic Porphyrias: Review and Recent Progress. Hepatol Commun. 2018;3(2):193–206. Published 2018 Dec 20. doi:10.1002/hep4.1297 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6357830[↩][↩]
- Elder G, Harper P, Badminton M, Sandberg S, Deybach JC. The incidence of inherited porphyrias in Europe. J Inherit Metab Dis. 2013 Sep;36(5):849-57. https://doi.org/10.1007/s10545-012-9544-4[↩]
- Balwani M, Wang B, Anderson KE, Bloomer JR, Bissell DM, Bonkovsky HL, Phillips JD, Desnick RJ, et al.. Acute hepatic porphyrias: recommendations for evaluation and long-term management. Hepatology. 2017; 66:1314-1322. https://www.ncbi.nlm.nih.gov/pubmed/28605040[↩][↩]
- Lin, Jou & Shi, Donglu. (2021). Photothermal and photovoltaic properties of transparent thin films of porphyrin compounds for energy applications. Applied Physics Reviews. 8. 011302. https://doi.org/10.1063/5.0036961[↩]
- Panawala, Lakna. (2017). What is the Function of Hemoglobin in the Human Body. https://www.researchgate.net/publication/313841668_What_is_the_Function_of_Hemoglobin_in_the_Human_Body[↩]
- Edel Y, Mamet R. Porphyria: What Is It and Who Should Be Evaluated? Rambam Maimonides Med J. 2018 Apr 19;9(2):e0013. doi: 10.5041/RMMJ.10333[↩]
- Lamoril J., Puy H., Whatley S.D., Martin C., Woolf J.R., Da Silva V., Deybach J.C., Elder G.H. Characterization of mutations in the CPO gene in British patients demonstrates absence of genotype-phenotype correlation and identifies relationship between hereditary coproporphyria and harderoporphyria. Am. J. Hum. Genet. 2001;68:1130–1138. doi: 10.1086/320118[↩]
- Blake D, McManus J, Cronin V, Ratnaike S. Fecal coproporphyrin isomers in hereditary coproporphyria. Clin Chem. 1992 Jan;38(1):96-100.[↩]
- Hasanoglu A, Balwani M, Kasapkara CS, Ezgü FS, Okur I, Tümer L, Cakmak A, Nazarenko I, Yu C, Clavero S, Bishop DF, Desnick RJ. Harderoporphyria due to homozygosity for coproporphyrinogen oxidase missense mutation H327R. J Inherit Metab Dis. 2011 Feb;34(1):225-31. doi: 10.1007/s10545-010-9237-9[↩][↩]
- Roveri G, Nascimbeni F, Rocchi E, Ventura P. Drugs and acute porphyrias: reasons for a hazardous relationship. Postgrad Med. 2014 Nov;126(7):108-20. doi: 10.3810/pgm.2014.11.2839[↩][↩][↩]
- Bonkovsky HL, Siao P, Roig Z, Hedley-Whyte ET, Flotte TJ. Case records of the Massachusetts General Hospital. Case 20-2008. A 57-year-old woman with abdominal pain and weakness after gastric bypass surgery. N Engl J Med. 2008 Jun 26;358(26):2813-25. doi: 10.1056/NEJMcpc0803190. Erratum in: N Engl J Med. 2008 Oct 23;359(17):1859[↩]
- Ma E, Mar V, Varigos G, Nicoll A, Ross G. Haem arginate as effective maintenance therapy for hereditary coproporphyria. Australas J Dermatol. 2011 May;52(2):135-8. doi: 10.1111/j.1440-0960.2011.00747.x[↩][↩][↩][↩][↩]
- Hereditary Coproporphyria. https://rarediseases.org/rare-diseases/hereditary-coproporphyria/[↩][↩][↩][↩]
- Jara-Prado A, Yescas P, Sánchez FJ, Ríos C, Garnica R, Alonso E. Prevalence of acute intermittent porphyria in a Mexican psychiatric population. Arch Med Res. 2000 Jul-Aug;31(4):404-8. doi: 10.1016/s0188-4409(00)00092-8[↩]
- Sardh E, Wahlin S, Björnstedt M, Harper P, Andersson DE. High risk of primary liver cancer in a cohort of 179 patients with Acute Hepatic Porphyria. J Inherit Metab Dis. 2013 Nov;36(6):1063-71. doi: 10.1007/s10545-012-9576-9[↩]
- Rudnick S, Phillips J, Bonkovsky H; Porphyrias Consortium of the Rare Diseases Clinical Research Network. Hepatoerythropoietic Porphyria. 2013 Oct 31 [Updated 2022 Dec 22]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK169003[↩]
- Wang B, Bissell DM. Hereditary Coproporphyria. 2012 Dec 13 [Updated 2018 Nov 8]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK114807[↩][↩][↩]
- Whatley SD, Mason NG, Woolf JR, Newcombe RG, Elder GH, Badminton MN. Diagnostic strategies for autosomal dominant acute porphyrias: retrospective analysis of 467 unrelated patients referred for mutational analysis of the HMBS, CPOX, or PPOX gene. Clin Chem. 2009; 55:1406-1414. https://www.ncbi.nlm.nih.gov/pubmed/19460837[↩]
- Tran TP, Leduc K, Savard M, Dupré N, Rivest D, Nguyen DK. Acute porphyria presenting as epilepsia partialis continua. Case Rep Neurol. 2013 Jun 29;5(2):116-24. doi: 10.1159/000353279[↩]
- Kühnel A, Gross U, Doss MO. Hereditary coproporphyria in Germany: clinical-biochemical studies in 53 patients. Clin Biochem. 2000 Aug;33(6):465-73. doi: 10.1016/s0009-9120(00)00159-4[↩]
- Stein PE, Badminton MN, Rees DC.. Update review of the acute porphyrias. Br Jl Hemot. 2017; 176(4):527-538. https://www.ncbi.nlm.nih.gov/pubmed/27982422[↩]
- Balwani M, Sardh E, Ventura P, Peiró PA, Rees DC, et al. ENVISION Investigators. Phase 3 Trial of RNAi Therapeutic Givosiran for Acute Intermittent Porphyria. N Engl J Med. 2020 Jun 11;382(24):2289-2301. doi: 10.1056/NEJMoa1913147[↩]
- Aggarwal N, Bagga R, Sawhney H, Suri V, Vasishta K. Pregnancy with acute intermittent porphyria: a case report and review of literature. J Obstet Gynaecol Res. 2002;28:160–2.[↩]
- Shenhav S, Gemer O, Sassoon E, Segal S. Acute intermittent porphyria precipitated by hyperemesis and metoclopramide treatment in pregnancy. Acta Obstet Gynecol Scand. 1997;76:484–5.[↩]
- Badminton MN, Deybach JC. Treatment of an acute attack of porphyria during pregnancy. Eur J Neurol. 2006;13:668–9.[↩]
- Farfaras A, Zagouri F, Zografos G, Kostopoulou A, Sergentanis TN, Antoniou S. Acute intermittent porphyria in pregnancy: a common misdiagnosis. Clin Exp Obstet Gynecol. 2010;37:256–60.[↩]