Contents
What is hoarseness
Hoarseness is also called dysphonia, is an abnormal change in the quality of your voice, making it sound raspy, strained, breathy, weak, higher or lower in pitch, inconsistent, or fatigued, often making it harder to talk 1. Your vocal sounds may be weak, breathy, scratchy, or husky, and the pitch or quality of the voice may change.
Hoarseness is most often caused by a problem with your vocal cords (or folds) of your voice box (larynx) that produce sound. The vocal cords are part of your voice box (larynx) located in the throat. Your vocal cords are separated when you breathe, but when you make sound, they come together and vibrate as air leaves your lungs. Anything that alters the vibration or closure of the vocal cords results in hoarseness. When the vocal cords become inflamed or infected, they swell. This can cause hoarseness.
The most common cause of hoarseness is a cold or sinus infection, which most often goes away on its own within 2 weeks.
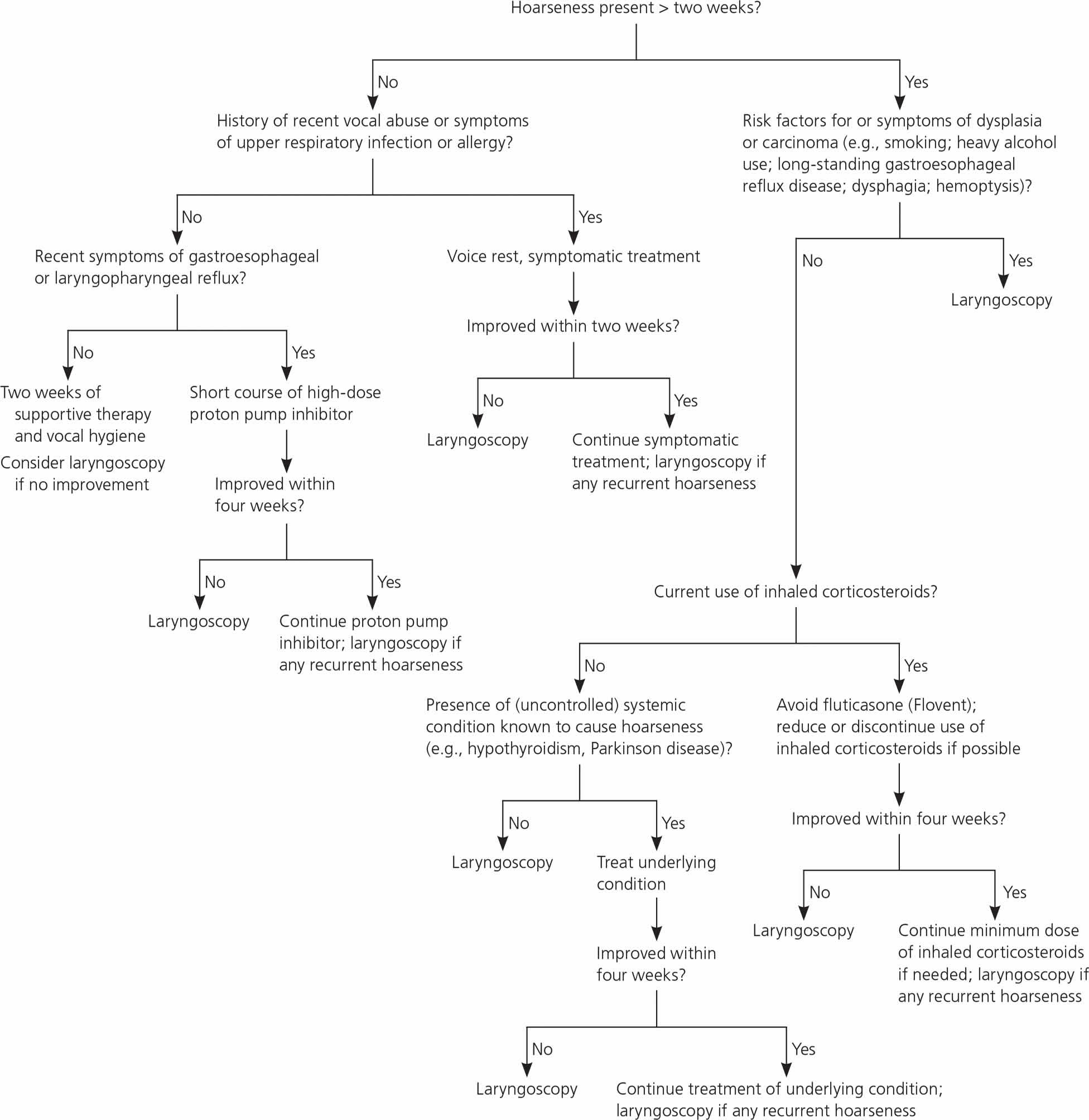
A rare but serious cause of hoarseness that does not go away in a few weeks is cancer of the voice box. Figure 3 below outlines a suggested approach to the primary care management of hoarseness 2.
Hoarseness is a symptom common to many diseases. Most dysphonia (hoarseness) is related to upper respiratory tract infection and goes away on its own in 7 to 10 days 3. See your health care provider if your hoarseness does not go away or get better in 4 weeks. You may have a serious medical condition that requires further evaluation by an otolaryngologist. An otolaryngologist is often called an ear, nose, and throat doctor, or ENT for short 4.
Some causes of hoarseness:
- Common cold, upper respiratory tract infection
- Voice overuse (using your voice too much, too loudly, or for a long period of time)
- Acid reflux
- Allergic laryngitis, which is inflammation of the larynx due to allergies
- Smoking and secondhand smoke
- Head and neck cancer
- Medication side effects
- Age-related changes
- Neurological conditions (examples: Parkinson’s disease, amyotrophic lateral sclerosis)
- Intubation (process of inserting a tube through the mouth and into the airway) and postsurgical injury
Who is at risk of hoarseness?
Hoarseness affects people of all ages and sexes but is more common in people who use their voice in their work. Singers, teachers, and call-center operators are some examples. Boys in the 8- to 14-year age range, adults over the age of 65 years, and people who smoke are also more likely to develop hoarseness.
See your doctor if:
- You have trouble breathing or swallowing.
- Hoarseness occurs with drooling, particularly in a small child.
- Hoarseness occurs in a child less than 3 months old.
- Hoarseness has lasted for more than 1 week in a child, or 2 to 3 weeks in an adult.
- Your hoarseness does not go away or get better in 7 to 10 days, especially if you smoke.
- You do not have a cold or flu.
- You are coughing up blood.
- You have difficulty swallowing.
- You feel a lump in your neck.
- You observe loss or severe changes in your voice that lasts longer than a few days.
- You experience pain when speaking or swallowing.
- Your voice change comes with uneasy breathing.
- Your hoarseness makes your work hard to do.
- You are a vocal performer (singer, teacher, public speaker) and cannot do your job.
Home remedies for hoarseness
Hoarseness may be short-term (acute) or long-term (chronic). Rest and time may improve hoarseness. Hoarseness that continues for weeks or months should be checked by a health care provider.
Things you can do at home to help relieve hoarseness include:
- Talk only when you need to until hoarseness goes away.
- Drink plenty of fluids to help keep your airways moist. (Gargling does not help.)
- Use a vaporizer to add moisture to the air you breathe.
- Avoid actions that strain the vocal cords such as whispering, shouting, crying, and singing.
- Take medicines to reduce stomach acid if hoarseness is due to gastroesophageal reflux disease (GERD).
- DO NOT use decongestants which can dry out the vocal cords.
- If you smoke, cut down, or stop at least until hoarseness goes away.
Are there potential dangers or complications?
Depending on the cause of your hoarseness, long-term concerns range from permanent hoarseness, inability to effectively communicate with others, loss of work for vocal professionals, to major surgery or, in severe cases, death from cancer and cancer-related treatments. That’s why it’s very important to see an ENT specialist to be evaluated for persistent hoarseness.
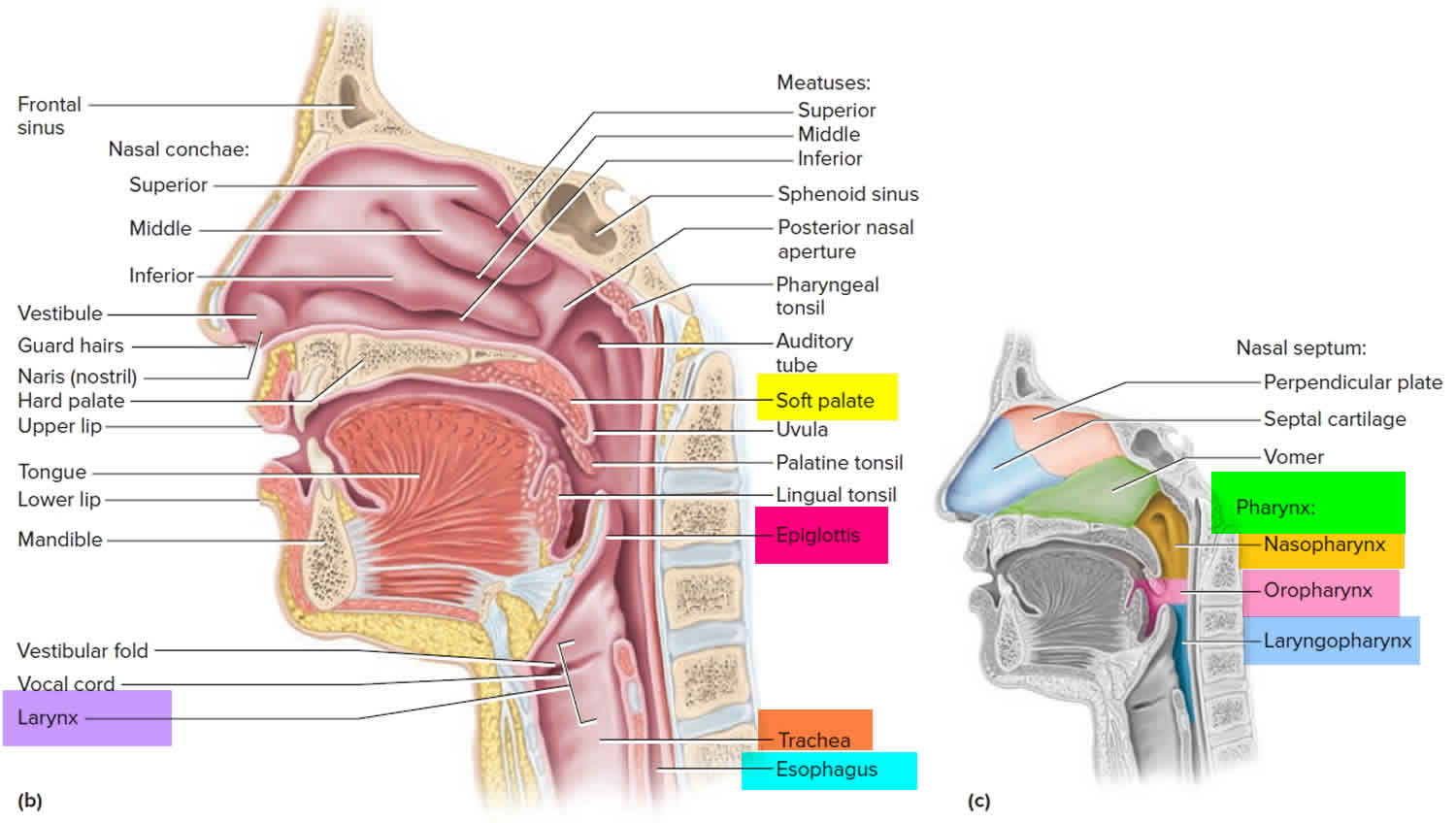
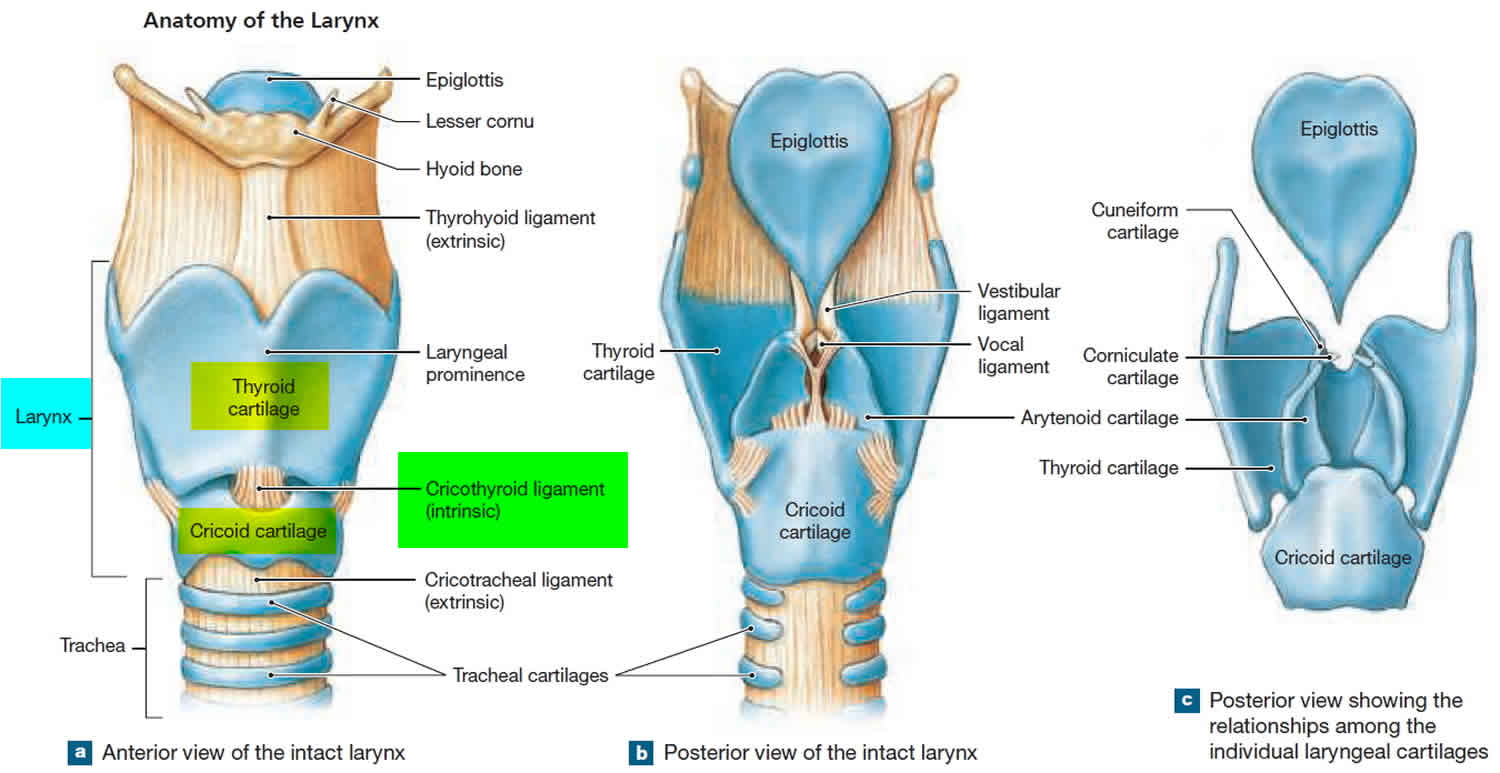
Laryngeal Anatomy and Function
The larynx functions in vocalization, deglutition, and respiration. It consists of an inner, mucosal-lined soft tissue framework protected by cartilaginous and bony structures (Figures 1 and 2). Extending from tongue base to trachea, it can be divided into three sections: supraglottic, glottic, and subglottic. The supraglottis, protected by the hyoid bone and thyroid cartilage, ranges from the tongue base to just above the true vocal folds (commonly mislabeled as vocal cords), and contains the epiglottis, false vocal folds, and arytenoids. The glottis, protected by the thyroid cartilage, extends inferiorly 1 cm below the true vocal folds. The subglottis extends from the inferior glottis to just below the cricoid cartilage.
The larynx contains extrinsic and intrinsic muscles innervated by two nerves branching from the vagus on each side: the superior laryngeal nerve and the recurrent (or inferior) laryngeal nerve. The internal branch of the superior laryngeal nerve enters the supraglottis between the hyoid and thyroid cartilage, and the external branch enters the glottis laterally through the cricothyroid membrane. The recurrent laryngeal nerves ascend lateral to the trachea after recurring upward around the aortic arch on the left and the subclavian artery on the right to ultimately enter the glottis through the cricothyroid membrane. The extrinsic muscles elevate and lower the position of the larynx in the neck. The intrinsic muscles produce fine movements of the vocal folds for phonation, and except for the cricothyroid muscles, are innervated by the recurrent laryngeal nerves.
The larynx produces sounds by forcing air through partially closed vocal folds to create vibrations of the folds. The intrinsic muscles control the tension of the vocal folds to create a wide range of sound waves, and the positioning of other speech organs such as the lips, tongue, and soft palate modifies these waves to increase the range of sounds.
Figure 1. Larynx and pharynx anatomy
Figure 2. Larynx (voice box) anatomy
Figure 3. Initial assessment and management of hoarseness
Footnote: Algorithm for the initial assessment and management of hoarseness.
[Source 5 ]What causes hoarseness
Causes of hoarseness can be grouped into four categories: irritant/inflammatory, neoplastic, neuromuscular/psychiatric, and associated systemic disease. Common and important causes are listed in Table 1 6.
Timing, onset, duration, and exacerbating or remitting factors can be key to determining the cause. The presence of any associated symptoms, especially for gastroesophageal reflux disease (GERD), laryngopharyngeal reflux, or postnasal drip, should be elicited. Symptoms of laryngopharyngeal reflux include dysphagia, burning in the throat, globus sensation, throat clearing, or a sensation of postnasal drainage. GERD (gastroesophageal reflux disease) and laryngopharyngeal reflux can occur together or separately. A review of medications is imperative because multiple drug classes have been associated with hoarseness (Table 2) 7. Acute onset is more suggestive of infection, inflammation, injury, or vocal abuse (e.g., singing or screaming at a sporting event or concert), whereas a chronic or progressive change in phonation can indicate more severe illness.
Hoarseness may be caused by:
- Acid reflux (gastroesophageal reflux)
- Allergies
- Breathing in irritating substances
- Cancer of the throat or larynx
- Chronic coughing
- Colds or upper respiratory infections
- Heavy smoking or drinking, particularly together
- Overuse or abuse of the voice (as in shouting or singing), which may cause swelling or growths on the vocal cords
- Medications. Inhaled corticosteroids, notably fluticasone (Flovent), budesonide (Rhinocort), and beclomethasone, can cause hoarseness in up to 58% of persons, more so in women (3:2 ratio) and individuals older than 65 years 7. Gargling, rinsing the mouth, or drinking water, as well as using a spacer, may be tried if hoarseness develops, and the corticosteroids can be discontinued or given at a reduced dosage if the hoarseness fails to resolve with these simple measures
- 7.
Acute laryngitis —The most common cause of hoarseness is acute laryngitis. A cold, viral infection in your breathing tract, or voice strain can make your vocal cords swell. You can seriously damage your vocal cords if you talk while you have laryngitis.
Non-cancerous vocal cord lesions —Nodules, polyps, and cysts usually develop after prolonged trauma to the vocal cords from talking too much, too loudly, or with bad technique.
Pre-cancerous or cancerous lesions —Pre-cancer or cancerous lesions on the vocal cords can also cause hoarseness. If it lasts four weeks or more, or if you are at a higher risk of developing throat cancer (i.e., you smoke), you should have your voice box evaluated by an ENT specialist.
Acid reflux (gastroesophageal reflux) — Acid reflux is when acidic or non-acidic stomach contents move from the stomach up into your swallowing tube (the esophagus). Classic heartburn and indigestion are symptoms of gastroesophageal reflux disease (GERD), which is caused by acid. If the stomach acid travels up the esophagus and spills into the throat or voice box (called the pharynx/larynx), it is known as laryngopharyngeal reflux.
Smoking —Most importantly, smoking increases the risk of developing throat cancer. Smoking can also cause permanent changes to your vocal cords that can lead to swelling, which lowers the pitch of your voice and can block the airway in severe cases. Smokers who develop hoarseness should see an otolaryngologist right away.
Neurological diseases or disorders —Hoarseness can occur with Parkinson’s disease or after a stroke. A rare disorder called spasmodic dysphonia can also create hoarseness or uneasy breathing. A paralyzed vocal cord, usually after surgery, viral illness, or injury, may also cause a weak, breathy voice.
Vocal cord atrophy —As you age, your vocal cords become thinner (decreased bulk) and floppy (decreased tone). This is not due to talking too much or too little, it’s just a fact of life. A raspy voice that changes from day to day with decreased power is common.
Vocal cord hemorrhage —You can lose your voice after yelling or other strenuous vocal activity if a blood vessel/blood blister breaks, filling the vocal cord with blood. This is a vocal emergency and should be treated with complete voice rest and examination by an otolaryngologist.
Less common causes of hoarseness include:
- Injury or irritation from a breathing tube or bronchoscopy
- Damage to the nerves and muscles around the voice box (from trauma or surgery)
- Foreign object in the esophagus or trachea
- Swallowing a harsh chemical liquid
- Changes in the larynx during puberty
- Thyroid or lung cancer
- Underactive thyroid gland
- Occasionally, menstruation can contribute to hoarseness
Table 1. Common or Important Causes of Hoarseness
Inflammatory or irritant |
Allergies and irritants (alcohol, tobacco) |
Direct trauma (intubation) |
Environmental irritants |
Infections (upper respiratory infection, fungal laryngitis) |
Laryngopharyngeal or gastroesophageal reflux |
Medications |
Vocal abuse |
Neoplasia or physical lesions |
Benign vocal fold lesions |
Dysplasia |
Laryngeal papillomatosis |
Squamous cell carcinoma |
Neuromuscular and psychiatric |
Age-related vocal atrophy |
Multiple sclerosis |
Muscle tension dysphonia |
Myasthenia gravis |
Nerve injury (vagus or recurrent laryngeal nerve) |
Parkinson disease |
Psychogenic (including conversion aphonia) |
Spasmodic dysphonia (laryngeal dystonia) |
Stroke |
Associated systemic diseases |
Acromegaly |
Amyloidosis |
Hypothyroidism |
Inflammatory arthritis |
Lupus |
Sarcoidosis |
Inflammatory and irritant causes
The most common cause of hoarseness in adults is laryngitis, which is classified as acute or chronic. Acute laryngitis is a common, self-limited condition lasting less than three to four weeks. Common causes include acute vocal strain or upper respiratory infection. Short-term vocal abuse (e.g., singing, screaming) or protracted coughing can cause microtrauma and focal vocal fold edema. Hoarseness is often part of a constellation of upper respiratory symptoms caused by viruses and less commonly by bacterial or fungal sources 8. Allergic rhinitis is another common cause of acute laryngitis.
Chronic laryngitis is diagnosed when symptoms persist for more than three to four weeks. Long-term inhalation of irritants (usually through smoking), reflux, chronic vocal strain, and postnasal drip are common causes. Irritation of vocal fold mucosa by reflux can be caused by laryngopharyngeal reflux or gastroesophageal reflux disease (GERD). Medications are another common cause of chronic laryngitis 9, 7, particularly those classes listed in Table 2 10.
Table 2. Medications that may cause hoarseness
| Medication | Mechanism of impact on voice |
|---|---|
Angiotensin-converting enzyme inhibitors | Cough |
Antihistamines, diuretics, anticholinergics | Drying effect on mucosa |
Antipsychotics, including atypical antipsychotics | Laryngeal dystonia |
Bisphosphonates | Chemical laryngitis |
Danazol, testosterone | Sex hormone production/utilization alteration |
Inhaled corticosteroids | Dose-dependent mucosal irritation, candidal or fungal laryngitis |
Warfarin (Coumadin), thrombolytics, phosphodiesterase-5 inhibitors | Vocal fold hematoma |
Neoplasia and physical lesions
Vocal fold lesions may be benign or malignant. More common benign lesions include Reinke edema (also known as polypoid chorditis), cysts, pseudocysts, polyps, and nodules (also known as midfold masses) 11. Some benign lesions have a higher prevalence based on factors such as age and sex (Table 3) 11.
Premalignant or malignant vocal fold lesions include laryngeal leukoplakia, dysplasia, and squamous cell carcinoma. Smoking, alcohol abuse, laryngopharyngeal reflux, and GERD are risk factors for more serious underlying causes such as malignant lesions 10. Hoarseness alone or other related symptoms (e.g., dysphagia, odynophagia, otalgia, hemoptysis, unilateral throat pain) may be the initial presentation of these lesions, particularly in middle-aged or older persons who smoke 12.
Table 3. Characteristics of Benign Vocal Fold Lesions
| Lesion type | Laryngoscopic findings | Common characteristics and associations | Causes |
|---|---|---|---|
Bilateral midfold masses (includes nodules) | Subepithelial fibrous thickening at vocal fold midpoint | Female, 18 to 39 years of age | Vocal abuse |
Contact lesion (ulceration or granuloma) | Mucosal irregularity over vocal process of arytenoid cartilage | Male, unilateral or bilateral | Direct trauma (intubation), inhaled corticosteroid use, laryngopharyngeal reflux, vocal abuse |
Cyst | Encapsulated subepithelial mass | Unilateral | Vocal abuse |
Hemorrhage | Subepithelial extravasated blood | Unilateral | Vocal abuse, direct trauma, anticoagulant use |
Leukoplakia | White-appearing epithelia of vocal fold | Male, older age (60 years and older) | Benign leukoplakia, carcinoma, dysplasia |
Polyp | Well-defined sessile or pedunculated midpoint mass | Male, unilateral | Allergy, tobacco and other irritants, vocal abuse |
Pseudocyst | Translucent lesion on vibratory margin | Female, 18 to 39 years of age, unilateral | Vocal abuse, vocal fold paresis |
Reactive lesion | Focal mucosal thickening in vocal fold midpoint | Unilateral, contralateral lesion | Trauma by contralateral vocal fold lesion |
Reinke edema (polypoid chorditis) | Proliferation of superficial mucosa over entire length of one or both vocal folds | Female, middle-aged (40 to 59 years) or older age (60 years and older), bilateral more common | GERD, laryngopharyngeal reflux, tobacco and other irritants, vocal abuse |
Sulcus | Focal epithelial invagination | Male, bilateral | Congenital |
Unilateral midfold masses (includes nodules) | Subepithelial fibrous thickening at vocal fold midpoint | Male, less common than bilateral | Vocal abuse |
Abbreviations: GERD = gastroesophageal reflux disease; LPR = laryngopharyngeal reflux.
[Source 6 ]Neuromuscular and psychiatric causes
Vocal fold paralysis is a common neurologic cause of hoarseness. Unilateral paralysis is typically caused by recurrent laryngeal nerve injury during neck, thyroid, or cardiothoracic surgery, but many times it is idiopathic 13. Unilateral paralysis can also be associated with infiltrating thyroid or apical lung cancers 14. Bilateral vocal fold paralysis is typically associated with bilateral thyroid surgery or neck trauma resulting in bilateral recurrent laryngeal nerve injury. Prolonged or traumatic endotracheal intubation can cause vocal fold inflammation and paralysis. Presbylaryngis, or age-related vocal atrophy, is increasingly common with an aging population, and can mimic fold paralysis as laryngeal muscles atrophy despite intact innervation 15. Less common neurologic causes include myasthenia gravis, Parkinson disease, amyotrophic lateral sclerosis, and multiple sclerosis.
Spasmodic dysphonia (or laryngeal dystonia) is the episodic, uncontrolled contraction of laryngeal intrinsic muscles to create a halting, strangled voice. Once considered psychogenic because of its relation to stress, the underlying neuromuscular etiology remains unknown 16. Considered neuropsychiatric in nature, muscle tension dysphonia results from excessive tension of the intrinsic or extrinsic muscles, and is associated with lack of breath control and stress 17. Psychiatric or functional voice disorders include functional dysphonia, laryngeal conversion disorder, paradoxical vocal fold motion, and malingering. Functional dysphonia occurs in patients with job-related chronic vocal stress without organic cause. Conversion disorder and paradoxical fold motion are psychogenic responses to stress 18.
Systemic diseases
Less commonly, hoarseness occurs secondary to systemic illnesses. Autoimmune diseases, such as inflammatory arthritis and lupus, can affect the cricoarytenoid joints. Endocrine disorders, including hypothyroidism and acromegaly, can cause hoarseness. Sarcoidosis and laryngeal amyloidosis are rare causes that strain voice quality from infiltration of the vocal folds and supraglottic structures 19.
Hoarseness prevention
- Quit smoking, if you use any type of tobacco product
- Avoid beverages that can dehydrate the body, such as alcohol (beer, wine, liquor) and caffeine (soft drinks, coffee)
- Avoid secondhand smoke
- Drink plenty of water, especially in dry areas
- Humidify your home
- Watch your diet—avoid spicy foods
- Avoid excessive throat clearing or coughing
- Try not to use your voice too long or too loudly
- Use a microphone if possible in situations where you need to talk louder than normal speech
- Avoid drying medications such as some antihistamines and diuretics (water pills)
- Seek professional help if your voice is injured or hoarse
Hoarseness symptoms
If you have any of these symptoms for hoarseness, you should see an ENT (ear, nose, and throat) specialist, or otolaryngologist, as soon as you can:
- Hoarseness that lasts more than four weeks, especially if you smoke
- Severe changes in voice lasting more than a few days
- Voice changes, such as raspy, strained, breathy, weak, higher or lower in pitch, inconsistent, fatigued, or shaky voice
- Difficult breathing
- Pain when speaking
- Vocal professionals (singer, teacher, public speaker) who cannot do their job
Table 4. Clinical Clues Suggesting Specific Causes of Hoarseness: Vocal Quality
| Vocal quality | Suggested diagnoses |
|---|---|
Breathy | Inflammatory arthritis, spasmodic or functional dysphonia, vocal fold mass, vocal fold paralysis |
Halting, strangled | Spasmodic dysphonia |
Hoarse, husky, muffled, or nasal-sounding | Parkinson disease |
Hoarseness worse early in the day | GERD, laryngopharyngeal reflux |
Hoarseness worse later in the day | Myasthenia gravis, vocal abuse |
Low pitched | GERD, hypothyroidism, laryngopharyngeal reflux, leukoplakia, muscle tension dysphonia, Reinke edema, vocal fold edema, age-related vocal atrophy in women |
Raspy or harsh | GERD, laryngopharyngeal reflux, muscle tension dysphonia, vocal fold lesion |
Scanning speech and dysarthria | Multiple sclerosis |
Soft (loss of volume) | Vocal fold paralysis, Parkinson disease, age-related vocal atrophy |
Spoken voice lost, but whispered voice maintained | Conversion aphonia |
Strained | GERD, laryngopharyngeal reflux, muscle tension dysphonia, spasmodic dysphonia |
Strained, effortful phonation | Muscle tension dysphonia |
Thick, deep voice and slowed speech | Acromegaly |
Vocal fatigue | Muscle tension dysphonia, myasthenia gravis, Parkinson disease, vocal abuse, age-related vocal atrophy |
Abbreviations: GERD = gastroesophageal reflux disease; LPR = laryngopharyngeal reflux.
[Source 20 ]Hoarseness diagnosis
Your health care provider will complete a physical examination and ask about your medical history. Your doctor may ask how long you have had the hoarseness, if you have other symptoms (fever, fatigue), how the hoarseness is affecting your life, medications you are currently taking, and lifestyle questions (alcohol use, smoking). If your hoarseness persists (does not go away) after 4 weeks or has no clear cause, you should be evaluated by an otolaryngologist. Otolaryngologists who specialize in voice disorders are called laryngologists.
Your doctor will examine your throat, neck, and mouth and ask you some questions about your symptoms and medical history. These may include:
- To what extent have you lost your voice (all or partially)?
- What kind of vocal problems are you having (making scratchy, breathy, or husky vocal sounds)?
- When did hoarseness start?
- Does hoarseness come and go or get worse over time?
- Have you been shouting, singing, or overusing your voice, or crying a lot (if a child)?
- Have you been exposed to harsh fumes or liquids?
- Do you have allergies or a post nasal drip?
- Have you ever had throat surgery?
- Do you smoke or use alcohol?
- Do you have other symptoms such as fever, cough, sore throat, difficulty swallowing, weight loss, or fatigue?
The physical exam should include a full head and neck examination. Your provider may feel your neck for any lumps or other problem signs. He or she may examine your voice box and nearby tissue with a mirror or laryngoscope (a small lighted instrument that bends when placed in the back of your throat) 21. Your doctor will listen to your voice to evaluate your voice quality. Depending on your symptoms, your health care provider may order additional tests such as a biopsy, computed tomography (CT) scan, or magnetic resonance imaging (MRI).
You may have one or more of the following tests:
- Laryngoscopy
- Throat culture
- Throat examination with a small mirror
- X-rays of the neck or CT scan
- Blood tests such as a complete blood count (CBC) or blood differential
Table 5. Clinical Clues Suggesting Specific Causes of Hoarseness: History and Physical Examination
| Findings | Suggested causes |
|---|---|
Cough | Allergy, GERD, inhaled irritants, laryngopharyngeal reflux, tobacco, upper respiratory infection |
Dysphagia | Carcinoma, GERD, inflammatory arthritis, laryngopharyngeal reflux |
Heartburn | Carcinoma, GERD, laryngopharyngeal reflux |
Hemoptysis | Carcinoma |
History of heavy alcohol use | Carcinoma, GERD, laryngopharyngeal reflux |
History of smoking or tobacco use | Carcinoma, chronic laryngitis, leukoplakia, Reinke edema |
Odynophagia | Carcinoma, inflammatory arthritis, upper respiratory infection |
Palpable lymph nodes | Carcinoma, upper respiratory infection |
Professional vocalist or untrained singer | Vocal abuse |
Recent head, neck, or chest surgery | Vagus or recurrent laryngeal nerve injury |
Recent intubation or laryngeal procedure | Direct trauma with vocal fold paralysis |
Rhinorrhea, sneezing, watery eyes | Allergy, upper respiratory infection |
Sensitivity to heat, spicy foods, other irritants | Leukoplakia |
Stridor, symptoms of airway obstruction | Carcinoma, laryngeal papillomatosis |
Throat clearing | Allergy, GERD, inhaled corticosteroids, laryngopharyngeal reflux |
Weight loss | Carcinoma |
Wheezing, other signs of asthma | Allergy, inhaled corticosteroids |
Abbreviations: GERD = gastroesophageal reflux disease; LPR = laryngopharyngeal reflux; URI = upper respiratory infection.
[Source 22 ]Diagnostic studies
Hoarseness of acute onset with a duration of less than 14 days and an apparent benign cause requires no further initial evaluation. Laryngoscopy should be performed if serious pathology is suspected, or it can be considered if dysphonia persists longer than two weeks, especially in patients with risk factors for dysplasia such as tobacco use, heavy alcohol use, or hemoptysis 10. Visualization by direct or indirect methods should not be delayed beyond three months for patients who remain symptomatic. Table 3 and Table 6 highlight laryngoscopic findings for a variety of conditions. Figure 3 (see above) outlines a suggested approach to the primary care management of hoarseness 2. Referral for imaging studies (computed tomography or magnetic resonance imaging) or biopsy may be indicated if laryngoscopy is nondiagnostic 10. Laryngoscopy and pH monitoring are not reliable tests for diagnosing laryngopharyngeal reflux. Videostroboscopy, which uses strobe lighting during laryngoscopy, can further visualize mucosal vibration disorders (e.g., scar, sulcus) if conventional laryngoscopy is inconclusive 23. Speech-language pathology offers perceptual, acoustic, and aerodynamic evaluations if examination and imaging are insufficient for making a diagnosis 24.
Table 6. Laryngoscopic Findings Associated with Causes of Hoarseness
| Findings | Causes |
|---|---|
Cysts | Vocal abuse |
Exophytic or ulcerated lesions | Carcinoma |
Granulomas | Direct trauma (intubation), GERD, inhaled corticosteroids, laryngopharyngeal reflux, vocal abuse |
Laryngeal inflammation | Allergy, direct trauma (intubation), GERD, infection, inhaled corticosteroids, laryngopharyngeal reflux, tobacco and other irritants |
Leukoplakia | Benign leukoplakia, carcinoma, dysplasia |
Loss of vocal fold adduction during phonation, but normal adduction with coughing or throat clearing | Conversion aphonia |
Nodules | Vocal abuse |
Papillomas | Laryngeal papillomatosis (human papillomavirus infection) |
Polyps | Allergy, tobacco and other irritants, vocal abuse |
Reinke edema (polypoid chorditis) | GERD, laryngopharyngeal reflux, tobacco and other irritants, vocal abuse |
Translucent, yellow, waxy deposits on vocal folds | Laryngeal amyloidosis |
Ulceration and laceration | Direct trauma (intubation) |
Vocal fold in paramedian or lateralized position | Vagus or recurrent laryngeal nerve injury, stroke |
Abbreviations: GERD = gastroesophageal reflux disease; LPR = laryngopharyngeal reflux
[Source 22 ]Hoarseness treatment
An ENT specialist needs to obtain your medical history and look at the voice box (larynx) with special equipment before they can determine what’s causing your hoarseness and recommend treatment options. They may pass a very small, lighted flexible tube with a camera (called a fiberoptic scope) through your nose to view your vocal cords. Most patients tolerate these procedures well. Sometimes, it helps to measure voice irregularities, how the voice sounds, airflow, and other characteristics to help decide how to treat your hoarseness.
Appropriate treatment depends on the cause of your hoarseness.
Botulinum toxin can be used for the management of adductor spasmodic dysphonia 25. Vocal fold paralysis can be treated with laryngeal reinnervation or vocal fold medialization procedures 26.
Acute laryngitis
Supportive care and voice rest are usually the recommended courses of action for acute laryngitis. Antibiotics and steroids are often not needed, and your primary care physician can manage this. If your hoarseness lasts beyond typical cold symptoms, however, you should see an ENT specialist.
Non-cancerous vocal cord lesions
Treatment for non-cancerous vocal cord lesions includes learning proper voicing technique with voice therapy, adequate hydration, and sometimes surgery.
Pre-cancerous or cancerous lesions
Surgery is needed to diagnose and treat pre-cancerous or cancerous lesions. Sometimes, other cancer treatments are needed, such as radiation therapy or chemotherapy.
Neurological diseases or disorders
Determining why your vocal cords are paralyzed helps your doctor decide the best course of action. Sometimes, vocal cord augmentation is needed. For patients with Parkinson’s disease, special voice techniques can help, but evaluation is also very important. Mumbled speech (called dysarthria) after a stroke or from a degenerative neurologic disorder can be addressed with speech therapy or the use of assistive communicative devices. Other disorders can be treated with botulinum toxin, or Botox®, injections.
Vocal cord atrophy
Treatment for vocal cord atrophy includes voice therapy and, sometimes, vocal cord injection, but reassurance from your doctor that your hoarseness is not due to cancer may be all that you need for peace of mind.
Vocal cord hemorrhage
Treatment usually includes resting your voice and avoiding blood thinners. Surgery is rarely needed.
Voice therapy, or voice training
Voice therapy, or voice training, is strongly recommended for patients with hoarseness who have significantly impaired vocal quality of life, especially those with dysphonia of nonorganic origins, benign vocal fold lesions, or age-related vocal atrophy 18. It can also be preventive in high-risk individuals such as vocalists and public speakers 27. Therapy regimens consist of vocal behavior modification to reduce laryngeal trauma during weekly 30- to 60-minute sessions for eight to 10 weeks. Compliance with vocal hygiene (e.g., avoiding irritants and alcohol, using a humidifier, controlling vocal volume, limiting large or spicy meals), vocal and physical exercises, and behavior change are imperative 28.
General vocal wellness tips
General vocal wellness tips include:
- Avoid speaking in loud environments.
- Be aware of how much and how loudly you are talking.
- Use a microphone or other type of voice amplification if your job requires a lot of talking (like teaching or public speaking).
- Drink plenty of water, usually around 60 ounces daily. This helps thin out mucus.
- Avoid large amounts of caffeine, such as caffeinated coffee, tea, and soda.
- Stop smoking and avoid secondhand smoke. This is a good idea for all smoked products.
- Krouse, H. J., W., C. (Charlie), Stachler, R. J., Francis, D. O., & O’Connor, S. (2018). Plain Language Summary: Hoarseness (Dysphonia). Otolaryngology–Head and Neck Surgery, 158(3), 427–431. https://doi.org/10.1177/0194599817751137[↩]
- Feierabend RH, Malik SN. Hoarseness in adults. Am Fam Physician. 2009;80(4):363–370.[↩][↩]
- Stachler, RJ, Francis, DO, Schwartz, SR. Clinical practice guideline: hoarseness (dysphonia) (update). Otolaryngol Head Neck Surg. 2018;158(suppl):S1-S42.[↩]
- What is Otolaryngology? http://entcolumbia.org/about-us/what-otolaryngology[↩]
- Feierabend RH, Malik SN. Hoarseness in adults. Am Fam Physician . 2009;80(4):368.[↩]
- Hoarseness in Adults. Am Fam Physician. 2017 Dec 1;96(11):720-728. https://www.aafp.org/afp/2017/1201/p720.html[↩][↩][↩]
- Galván CA, Guarderas JC. Practical considerations for dysphonia caused by inhaled corticosteroids. Mayo Clin Proc. 2012;87(9):901–904.[↩][↩][↩][↩]
- Dworkin JP. Laryngitis: types, causes, and treatments. Otolaryngol Clin North Am. 2008;41(2):419–436, ix.[↩]
- Adams NP, et al. Fluticasone versus placebo for chronic asthma in adults and children. Cochrane Database Syst Rev. 2008;(4):CD003135.[↩]
- Schwartz SR, Cohen SM, Dailey SH, et al. Clinical practice guideline: hoarseness (dysphonia). Otolaryngol Head Neck Surg. 2009;141(3 suppl 2):S1–S31.[↩][↩][↩][↩][↩]
- Zhukhovitskaya A, et al. Gender and age in benign vocal fold lesions. Laryngoscope. 2015;125(1):191–196.[↩][↩]
- Qadeer MA, et al. Gastroesophageal reflux and laryngeal cancer: causation or association? A critical review. Am J Otolaryngol. 2006;27(2):119–128.[↩]
- Sulica L. The natural history of idiopathic unilateral vocal fold paralysis: evidence and problems. Laryngoscope. 2008;118(7):1303–1307.[↩]
- Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007;117(10):1864–1870.[↩]
- Davids T, Klein AM, Johns MM III. Current dysphonia trends in patients over the age of 65: is vocal atrophy becoming more prevalent? Laryngoscope. 2012;122(2):332–335.[↩]
- Persaud R, et al. An evidence-based review of botulinum toxin (Botox) applications in non-cosmetic head and neck conditions. JRSM Short Rep. 2013;4(2):10.[↩]
- Altman KW, Atkinson C, Lazarus C. Current and emerging concepts in muscle tension dysphonia: a 30-month review. J Voice. 2005;19(2):261–267.[↩]
- Ruotsalainen J, Sellman J, Lehto L, Verbeek J. Systematic review of the treatment of functional dysphonia and prevention of voice disorders. Otolaryngol Head Neck Surg. 2008;138(5):557–565.[↩][↩]
- Bartels H, et al. Laryngeal amyloidosis: localized versus systemic disease and update on diagnosis and therapy. Ann Otol Rhinol Laryngol. 2004;113(9):741–748.[↩]
- Feierabend RH, Malik SN. Hoarseness in adults. Am Fam Physician. 2009;80(4):366.[↩]
- Hoarseness: Frequently Asked Questions. https://my.clevelandclinic.org/health/diseases/17105-hoarseness-frequently-asked-questions[↩]
- Feierabend RH, Malik SN. Hoarseness in adults. Am Fam Physician. 2009;80(4):367.[↩][↩]
- Sulica L. Laryngoscopy, stroboscopy and other tools for the evaluation of voice disorders. Otolaryngol Clin North Am. 2013;46(1):21–30.[↩]
- Cohen SM, Dinan MA, Kim J, Roy N. Otolaryngology utilization of speech-language pathology services for voice disorders. Laryngoscope. 2016;126(4):906–912.[↩]
- Truong DD, Bhidayasiri R. Botulinum toxin therapy of laryngeal muscle hyperactivity syndromes: comparing different botulinum toxin preparations. Eur J Neurol. 2006;13(suppl 1):36–41.[↩]
- Siu J, Tam S, Fung K. A comparison of outcomes in interventions for unilateral vocal fold paralysis: a systematic review. Laryngoscope. 2016;126(7):1616–1624.[↩]
- Havas T, Lowinger D, Priestley J. Unilateral vocal fold paralysis: causes, options and outcomes. Aust N Z J Surg. 1999;69(7):509–513.[↩]
- Yun YS, Kim MB, Son YI. The effect of vocal hygiene education for patients with vocal polyp. Otolaryngol Head Neck Surg. 2007;137(4):569–575.[↩]