Contents
- What is a hole in heart
- Atrial septal defect
- Ventricular septal defect
What is a hole in heart
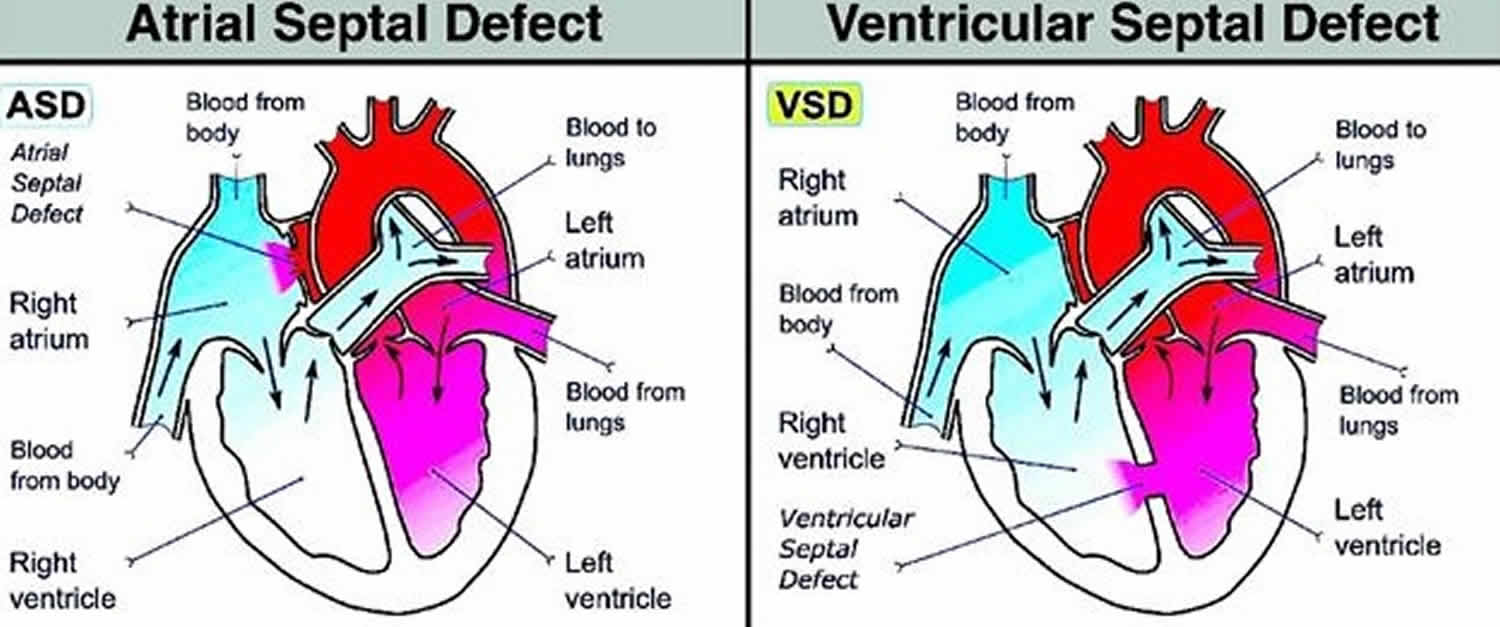
A hole in heart is also known septal defect is a type of congenital heart defect, which means the baby is born with a hole in his/her heart. A hole in heart or a septal defect is where there’s an abnormality in the wall (septum) between the main chambers of the heart. The two main types of septal defect are outlined below.
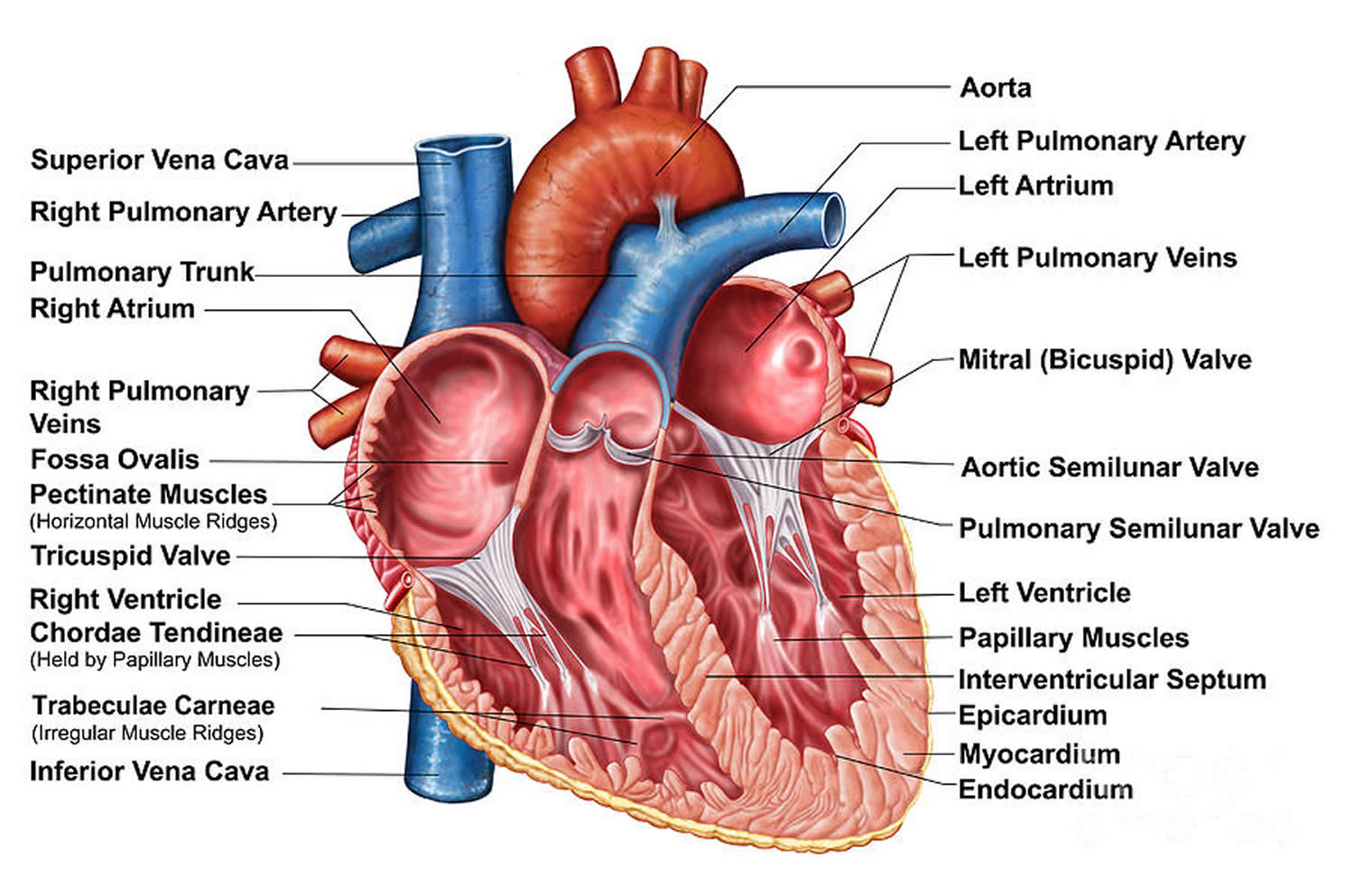
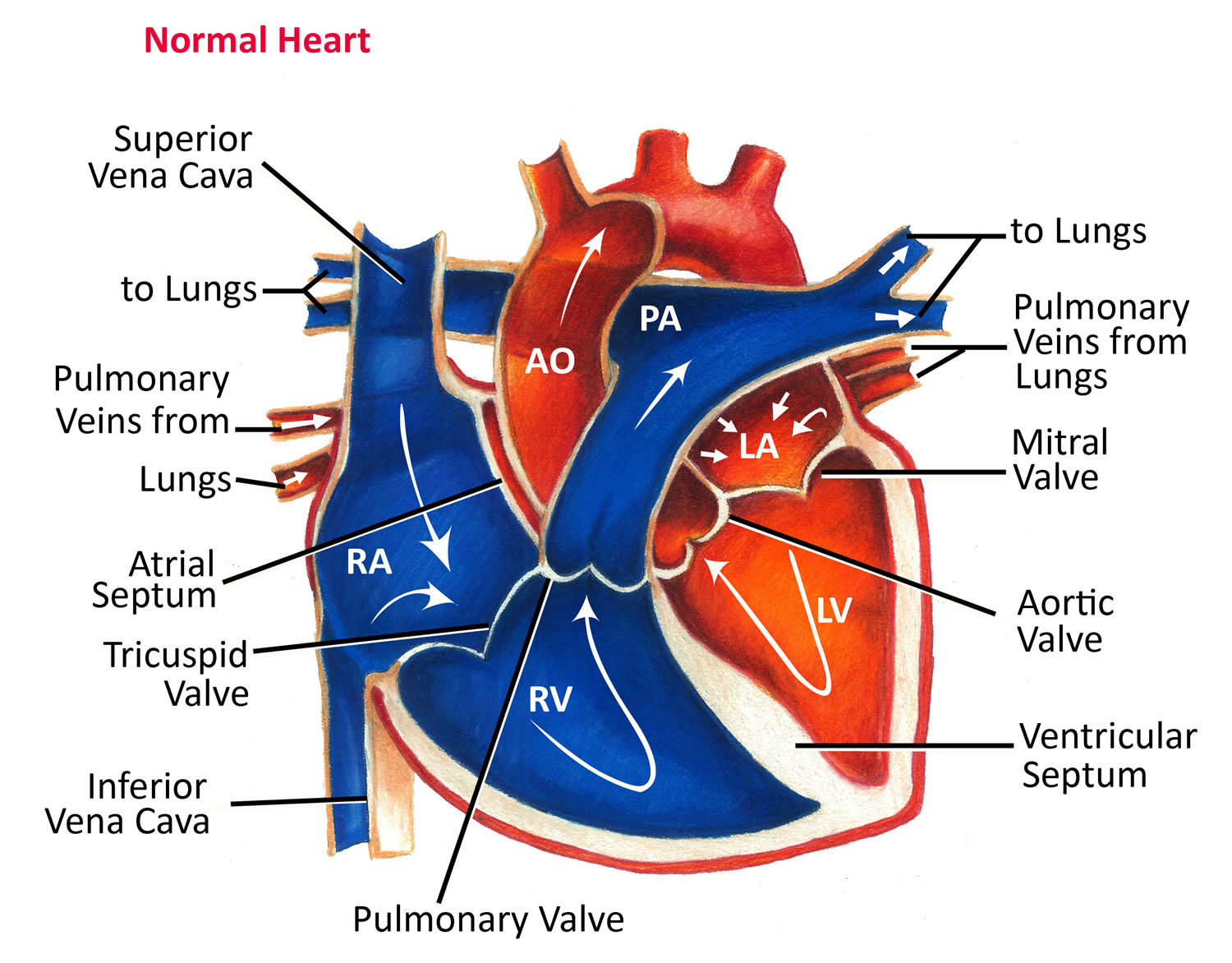
The heart has 4 chambers: 2 upper (atria) and 2 lower (ventricles) (see Figures 1 and 2). Blood that is high in oxygen flows from the left atrium to the left ventricle and out to the body, where the vital organs use the oxygen. Blood with less oxygen flows from the right atrium to the right ventricle and out to the lungs. There, it picks up more oxygen. Normally, a wall (septum) is present between the left and right atria and between the left and right ventricles.
Atrial septal defects
An atrial septal defect (ASD) is where there’s a hole between the two upper chambers of the heart known as the right atrium and left atrium. When there’s an atrial septal defect (ASD), extra blood flows through the defect into the right side of the heart, causing it to stretch and enlarge.
Ventricular septal defects
A ventricular septal defect (VSD) is a common form of congenital heart disease. It occurs when there’s a hole between the 2 pumping chambers of the heart (the left and right ventricles).
This means that extra blood flows through the hole from the left to the right ventricle, due to the pressure difference between them. The extra blood goes to the lungs, causing high pressure in the lungs and a stretch on the left- sided pumping chamber.
Small holes often eventually close by themselves, but larger holes need to be closed using surgery.
Atrial septal defect
An atrial septal defect (ASD) is a congenital (present at birth) heart defect where there is a hole between the two upper chambers of the heart known as the right atrium and left atrium. In fetal circulation there is normally an opening between the two atria (the upper chambers of the heart) to allow blood to bypass the lungs. This opening usually closes about the time your baby is born. If the opening is persistent it is called a atrial septal defect, and thus blood continues to bypass the lungs. This is called a shunt. Because pressure in the left atrium of the heart is much higher, the atrial septal defect allows blood from the left atrium to pass to the right atrium. Atrial septal defect can also occur with other heart defects.
An atrial septal defect (ASD) allows freshly oxygenated blood to flow from the left upper chamber of the heart (left atrium) into the right upper chamber of the heart (right atrium). There, it mixes with deoxygenated blood and is pumped to the lungs, even though it’s already refreshed with oxygen. If the atrial septal defect is large, this extra blood volume can overfill the lungs and overwork the right side of the heart. If not treated, the right side of the heart eventually enlarges and weakens. If this process continues, the blood pressure in your lungs may increase as well, leading to pulmonary hypertension.
Atrial septal defect affects about 1 in 1,966 babies in the United States 1. Females outnumber males 3:1 in incidence.
Some atrial septal defects are very small and may never cause any problems or require treatment. However, a large atrial septal defect can result in the right side of your child’s heart being overloaded with blood. Atrial septal defect may only cause mild symptoms, such as breathlessness when being active. However, if a large atrial septal defect is left untreated, over a period of many years it can eventually lead to permanent damage to your child’s heart and sometimes to their lungs.
Figure 3. Atrial septal defect
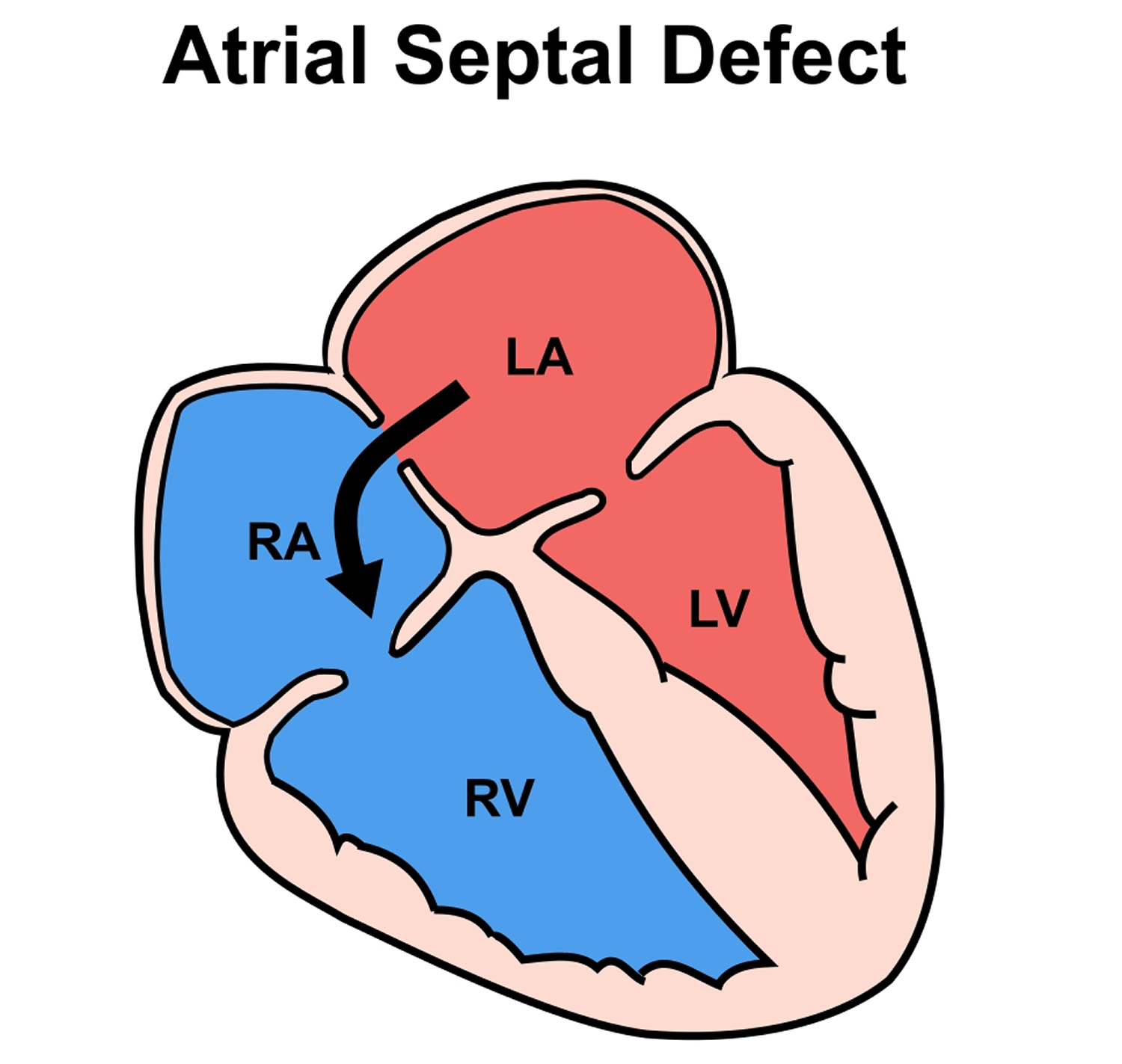 Note: RA = right atrium; LA = left atrium; RV= right ventricle; LV = left ventricle
Note: RA = right atrium; LA = left atrium; RV= right ventricle; LV = left ventricleThere are generally three main types of atrial septal defect
- Secundum atrial septal defect (ostium secundum atrial septal defect), this is the most common type of atrial septal defect. The hole is near the center of your atrial septum, related to the foramen ovale. It results from the inadequate closure of the central hole in the septum primum by the septum secundum – this also produces the fossa ovalis defect.
- Primum atrial septal defect (ostium primum atrial septal defect) occurs when there is interference with the development of the septum primum at its lower margin, associated with abnormal development of the endocardial cushions – there is no inferior rim of atrial septal tissue. This defect is often associated with abnormalities of the mitral and tricuspid valves as well as abnormalities of the upper portion of the interventricular septum.
- Sinus venosus atrial septal defect is a hole that extends into the superior vena cava where the main vein carrying oxygen – poor blood back to the body enters the heart.
- Coronary sinus atrial septal defect. In this rare defect, part of the wall between the coronary sinus — which is part of the vein system of the heart — and the left atrium is missing.
Usually, the only test that is needed to make the diagnosis is an echocardiogram. This is an ultrasound scan of the heart. It won’t hurt your baby at all. Because babies and young children often show no symptoms, atrial septal defect may not be found until they are older, sometimes even in teenage and adult years.
Atrial septal defects may occur in isolation or may be associated with other malformations:
- Spontaneous closure of atrial septal defects is rare after the first 2 years of life;
- Atrial septal defects allow shunting of blood from one side of the circulation to the other. There are no great pressure differentials across the two atria and shunting is usually from left to right due to the greater compliance of the right heart chambers. Flow rates across the defect are usually not high;
- Increased flow to the pulmonary circulation eventually leads to pulmonary hypertension, usually by the 4th decade. Atrial arrhythmias, particularly atrial fibrillation (AF) are common due to the physical distention of the atria;
- In severe cases the shunt can eventually reverse so that blood bypasses the lungs – this is termed Eisenmenger’s syndrome and is a poor prognostic factor.
You may have your atrial septal defect closed by open heart surgery. Small holes can be closed by suturing, which means sewing the edges of the hole together. Bigger holes are covered with patches, either made of pieces of the pericardium, which is the membrane that covers the heart, or instead the patches can be made of a synthetic material. The scar on your chest will heal and fade to a paler color over time. Your child’s cardiologist will talk to you about which type of surgery is best for your child.
Atrial septal defect complications
A small atrial septal defect may never cause any problems. Small atrial septal defects often close during infancy.
Larger defects can cause serious problems, including:
- Right-sided heart failure
- Heart rhythm abnormalities (arrhythmias)
- Increased risk of a stroke
- Shortened life span
Less common serious complications may include:
- Pulmonary hypertension. If a large atrial septal defect goes untreated, increased blood flow to your lungs increases the blood pressure in the lung arteries (pulmonary hypertension).
- Eisenmenger syndrome. Pulmonary hypertension can cause permanent lung damage. This complication, called Eisenmenger syndrome, usually develops over many years and occurs uncommonly in people with large atrial septal defects.
Treatment can prevent or help manage many of these complications.
What happens as my child grows up?
Most children, after atrial septal defect repair, will remain completely well and lead a normal, active life after treatment. There is no need to restrict your child’s physical activity and no special precautions are necessary.
Atrial septal defect and pregnancy
Most women with an atrial septal defect can tolerate pregnancy without any problems. However, having a larger atrial septal defect or having complications such as heart failure, arrhythmias or pulmonary hypertension can increase your risk of complications during pregnancy. Doctors strongly advise women with Eisenmenger syndrome not to become pregnant because it can endanger their lives.
The risk of congenital heart disease is higher for children of parents with congenital heart disease, whether in the father or the mother. Anyone with a congenital heart defect, repaired or not, who is considering starting a family should carefully discuss it beforehand with a doctor. Some medications may need to be stopped or adjusted before you become pregnant because they can cause serious problems for a developing fetus.
Atrial septal defect causes
The cause of congenital heart defects is not understood but several factors are known to be associated:
- Maternal drug abuse, alcohol abuse and radiation exposure;
- Maternal infection, particularly rubella;
- Genetic abnormalities;
- Chromosomal abnormalities (septal defects are associated with Trisomy 21- Down’s syndrome).
Risk factors for atrial septal defect
It’s not known why atrial septal defects occur, but congenital heart defects appear to run in families and sometimes occur with other genetic problems, such as Down syndrome. If you have a heart defect, or you have a child with a heart defect, a genetic counselor can estimate the odds that any future children will have one.
Some conditions that you have or that occur during pregnancy may increase your risk of having a baby with a heart defect, including:
- Rubella (German measles) infection. Becoming infected with rubella (German measles) during the first few months of your pregnancy can increase the risk of fetal heart defects.
- Drug, tobacco or alcohol use, or exposure to certain substances. Use of certain medications, tobacco, alcohol or drugs, such as cocaine, during pregnancy can harm the developing fetus.
- Diabetes or lupus. If you have diabetes or lupus, you may be more likely to have a baby with a heart defect.
- Obesity. Being extremely overweight (obese) may play a role in increasing the risk of having a baby with a birth defect.
- Phenylketonuria (PKU). If you have PKU and aren’t following your PKU meal plan, you may be more likely to have a baby with a heart defect.
What is the risk of having another child with a congenital heart condition?
If you have one child with a congenital heart condition, there is around a 1 in 40 chance that if you have another child, they will have a heart condition too 2. However, this risk may be higher (or lower) depending on the type of congenital heart condition your child has. Because your risk of having another child with congenital heart condition is higher than it is for other people, your doctor may offer you a special scan at an early stage in future pregnancies, to look at the baby’s heart.
Do ask your obstetrician or doctor for more information on having a scan earlier than usual. Do be aware that if you have more than one child with congenital heart condition, the specific condition may not always be the same.
Atrial septal defect prevention
In most cases, atrial septal defects can’t be prevented. If you’re planning to become pregnant, schedule a preconception visit with your health care provider. This visit should include:
- Getting tested for immunity to rubella. If you’re not immune, ask your doctor about getting vaccinated.
- Going over your current health conditions and medications. You’ll need to carefully monitor certain health problems during pregnancy. Your doctor may also recommend adjusting or stopping certain medications before you become pregnant.
- Reviewing your family medical history. If you have a family history of heart defects or other genetic disorders, consider talking with a genetic counselor to determine what the risk might be before getting pregnant.
Atrial septal defect symptoms
Many babies born with atrial septal defects don’t have associated signs or symptoms. Most commonly symptoms don’t develop until the twenties when evidence of pulmonary vascular disease becomes apparent. With increasing age, risk of developing cardiac rhythm disturbances increases. In adults, signs or symptoms may begin around age 30, but in some cases signs and symptoms may not occur until decades later. By the age of 40 most patients are severely symptomatic. Cardiac failure is the most common cause of death. Others include emboli and infections.
Atrial septal defect signs and symptoms may include:
- Heart murmur, a whooshing sound that can be heard through a stethoscope;
- Susceptibility to chest infections is common;
- Subtle failure to thrive may occur in some children;
- Tiring when feeding (infants);
- Shortness of breath when being active or exercising and weakness are sometimes reported;
- Difficulty breathing;
- Fatigue;
- Swelling of legs, feet or abdomen;
- Heart palpitations or skipped beats;
- Swelling of legs, feet, or stomach area
- Stroke;
- Later in life, palpitations associated with atrial fibrillation and congestive heart failure are common with exertional dyspnea and orthopnea.
Atrial septal defect diagnosis
An atrial septal defect may be diagnosed during pregnancy or after the baby is born. In many cases, it may not be diagnosed until adulthood.
Your or your child’s doctor may first suspect an atrial septal defect or other heart defect during a regular checkup if he or she hears a heart murmur while listening to the heart using a stethoscope.
During Pregnancy
During pregnancy, there are screening tests (prenatal tests) to check for birth defects and other conditions. An atrial septal defect might be seen during an ultrasound (which creates pictures of the body), but it depends on the size of the hole and its location. If an atrial septal defect is suspected, a specialist will need to confirm the diagnosis.
If your doctor suspects you or your child has a heart defect, the doctor may request one or more of the following tests:
- Echocardiogram. This is the most commonly used test to diagnose an atrial septal defect. Some atrial septal defects can be found during an echocardiogram done for another reason. During an echocardiogram, sound waves are used to produce a video image of the heart. It allows your doctor to see your heart’s chambers and measure their pumping strength. This test also checks heart valves and looks for any signs of heart defects. Doctors may use this test to evaluate your condition and determine your treatment plan.
- Chest X-ray. An X-ray image helps your doctor to see the condition of your heart and lungs. An X-ray may identify conditions other than a heart defect that may explain your signs or symptoms.
- Electrocardiogram (ECG). This test records the electrical activity of your heart and helps identify heart rhythm problems.
- Cardiac catheterization. In this test, a thin, flexible tube (catheter) is inserted into a blood vessel at your groin or arm and guided to your heart. Through catheterization, doctors can diagnose congenital heart defects, test how well your heart is pumping and check the function of your heart valves. Using catheterization, the blood pressure in your lungs also can be measured. However, this test usually isn’t needed to diagnose an atrial septal defect. Doctors may also use catheterization techniques to repair heart defects.
- Magnetic resonance imaging (MRI). An MRI is a technique that uses a magnetic field and radio waves to create 3-D images of your heart and other organs and tissues within your body. Your doctor may request an MRI if echocardiography can’t definitively diagnose an atrial septal defect.
- Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create detailed images of your heart. A CT scan may be used to diagnose an atrial septal defect if echocardiography hasn’t definitely diagnosed an atrial septal defect.
Atrial septal defect treatment
Many atrial septal defects close on their own during childhood. For those that don’t close, some small atrial septal defects don’t cause any problems and may not require any treatment. But mny persistent atrial septal defects eventually require surgery to be corrected.
Large atrial septal defects (where pulmonary blood flow is greater than 150% normal) should be repaired surgically as early as possible, preferably before 10 years. The outlook is good if pulmonary hypertension (high blood pressure in the lungs) has not developed. Otherwise, medical management of heart failure and other complications such as arrhythmias should be instigated.
Medical monitoring
If your child has an atrial septal defect, your child’s cardiologist may recommend monitoring it for a period of time to see if it closes on its own. Your child’s doctor will decide when your child needs treatment, depending on your child’s condition and whether your child has any other congenital heart defects.
Medications
Medications won’t repair the hole, but they may be used to reduce some of the signs and symptoms that can accompany an atrial septal defect. Drugs may also be used to reduce the risk of complications after surgery. Medications may include those to keep the heartbeat regular (beta blockers) or to reduce the risk of blood clots (anticoagulants).
Atrial septal defect surgery
Many doctors recommend repairing an atrial septal defect diagnosed during childhood to prevent complications as an adult. Doctors may recommend surgery to repair medium- to large-sized atrial septal defects. However, surgery isn’t recommended if you have severe pulmonary hypertension because it might make the condition worse.
For adults and children, surgery involves sewing closed or patching the abnormal opening between the atria. Doctors will evaluate your condition and determine which procedure is most appropriate. Atrial septal defects can be repaired using two methods:
Atrial septal defect is treated with:
- Keyhole surgery, or
- Open-heart surgery.
The aim of both these surgeries is to close the atrial septal defect and stop blood from the left atrium of the heart passing to the right atrium. The type of treatment will depend on the size of the atrial septal defect and its exact position.
Keyhole surgery for atrial septal defect
Your child will be given a general anesthetic. A small tube will be inserted into your child’s food pipe (esophagus) through their mouth. The doctors will use this tube to do a scan called a transesophageal echocardiogram (TEE) to see the heart, and in particular the atrial septal defect, clearly. Then, a long thin tube called a catheter will be inserted into a vein at the top of their leg and guided to their heart. The atrial septal defect is closed using a special device, which is folded up and pushed through the catheter to the heart. Once it is in the correct position, the device is unfolded so that the atrial septal defect hole is closed. The catheter will then be removed. The device will stay inside your child’s heart and become covered over by their own tissue during the healing process.
After the operation, you will need to take your child to the outpatient department to see the cardiologist for a check-up about a month later.
Your child will need to take aspirin for a few months after the treatment. This reduces the risk of a blood clot forming on the device while it is healing over.
What are the risks of keyhole surgery?
Keyhole treatment to repair an atrial septal defect is usually very successful and carries a very low risk of fatality. Most children will not experience any major complications. There is a small risk of bleeding around the heart and a small risk that the device could move out of place after the surgery. If this happens your child may need an operation to remove the device and to close the hole at the same time.
Sometimes the device might not completely close the hole. If this happens your child may need another operation to close the hole around the device. There is a very small risk that the device could become infected and an operation would be needed to remove it.
It’s very rare, but there is also a very small risk of blood clots forming inside the heart during the surgery which could cause a stroke. The risk of dying as a result of this treatment is very small. Your doctor will talk you through all these risks before your child’s treatment.
Some children who suffered from migraines in the past may find that their migraine is worse for a few months after keyhole closure of their atrial septal defect. However, some find that their migraine disappears after keyhole surgery. The reasons for this are not fully understood at the moment.
Open-heart surgery for atrial septal defect
Sometimes open-heart surgery is required to close the atrial septal defect. This procedure is the preferred treatment for certain types of atrial septal defects (primum, sinus venosus and coronary sinus), and these types of atrial defects can only be repaired through open-heart surgery. If your child has surgery, they will be given a general anesthetic. The surgeon will make a cut in their breastbone to get access to their heart. Their heart will be stopped and a ‘heart-lung machine’ will be used to take over the function of the heart and lungs. The surgeon will sew the atrial septal defect closed. They will start the heart beating again and the heart-lung machine will be turned off. Your child’s chest will be sewn closed.
After the operation your child will have a scar, usually in the center of the chest along their breastbone. They will need to stay in hospital for a few days and return to the out-patient department a few weeks later for a check-up.
What are the risks of open-heart surgery?
Open-heart surgery to repair atrial septal defect is usually very successful and the fatality risks are very low. There are small risks of complications such as brain damage, kidney damage, or serious lung diseases such as pneumonia. Your child’s doctor will talk you through all these risks before the operation.
Follow-up care
Follow-up care depends on the type of defect and whether other defects are present. Repeated echocardiograms are done after hospital discharge, one year later and then as requested by your or your child’s doctor. For simple atrial septal defects closed during childhood, only occasional follow-up care is generally needed.
Adults who’ve had atrial septal defect repair need to be monitored throughout life to check for complications, such as pulmonary hypertension, arrhythmias, heart failure or valve problems. Follow-up exams are typically done on a yearly basis.
Home remedies
If you find out you have a congenital heart defect, or you’ve had surgery to correct one, you may wonder about limitations on activities and other issues.
- Exercise. Having an atrial septal defect usually doesn’t restrict you from activities or exercise. If you have complications, such as arrhythmias, heart failure or pulmonary hypertension, you may not be able to do some activities or exercises. Your cardiologist can help you learn what is safe.
If you have an unrepaired defect, your doctor will likely advise you to avoid scuba diving and high altitude climbing.
- Preventing infection. Some heart defects and the repair of defects create changes to the surface of the heart in which bacteria can become stuck and grow into an infection (infective endocarditis). Atrial septal defects generally aren’t associated with infective endocarditis, though your doctor will likely recommend preventive antibiotics for about six months after closure whenever you have dental work done.
But if you have other heart defects in addition to an atrial septal defect, or if you’ve had atrial septal defect repair within the last six months, you may need to take antibiotics before certain dental or surgical procedures.
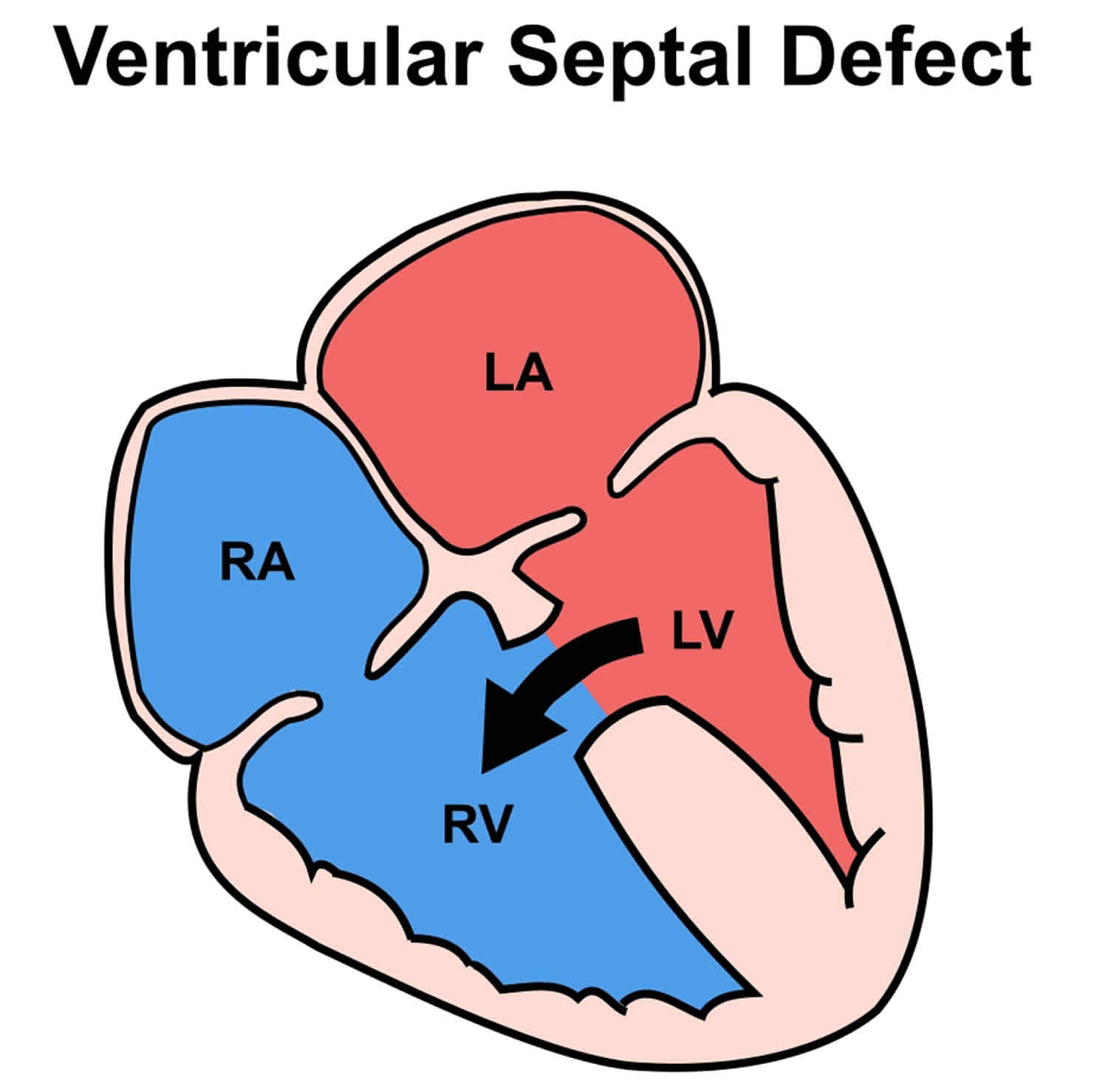
Ventricular septal defect
A ventricular septal defect (VSD) is a common congenital heart defect. Ventricular septal defect occurs when there’s a hole between the 2 pumping chambers of the heart (the left and right ventricles). Blood may flow from the left ventricle and mix with blood in the right ventricle, instead of going to the rest of the body. If the hole is large, this may make the heart and lungs work harder and may cause fluid to build up in the lungs.
Before a baby is born, the right and left ventricles of the heart are not separate. As the fetus grows, a septal wall forms to separate these 2 ventricles. If the wall does not completely form, a hole remains. This hole is known as a ventricular septal defect, or a ventricular septal defect. The hole can occur in different locations along the septal wall. There can be a single hole or multiple holes.
The baby may have no symptoms and the hole can close over time as the wall continues to grow after birth. If the hole is large, too much blood will be pumped to the lungs. This can lead to heart failure.
The cause of ventricular septal defect is not yet known. This defect often occurs along with other congenital heart defects.
In adults, ventricular septal defects are a rare, but serious complication of heart attacks. These holes do not result from a birth defect.
A small ventricular septal defect (VSD) may cause no problems, and many small small ventricular septal defects close on their own. By age 1, most small ventricular septal defects close on their own. However, those ventricular septal defects that do stay open after this age may need to be closed.
Medium or larger ventricular septal defects may need surgical repair early in life to prevent complications, such as ventricular septal defects in certain parts of the ventricular septum, or ventricular septal defects that cause heart failure or endocarditis, (inflammation) need open-heart surgery. The hole in the septum is most often closed with a patch.
Some ventricular septal defects can be closed without surgery. The procedure involves passing a small wire into the heart and placing a small device to close the defect.
Figure 4. Ventricular septal defect
Note: RA = right atrium; LA = left atrium; RV= right ventricle; LV = left ventricle
Ventricular septal defect prognosis
Many small ventricular septal defects will close on their own. Surgery can repair ventricular septal defects that do not close. In most cases, a person will not have any ongoing medical issues related to the ventricular septal defect if it is closed with surgery or closes on its own. Complications may occur if a large ventricular septal defect is not treated and there is permanent damage to the lungs.
Ventricular septal defect complications
A small ventricular septal defect may never cause any problems. Medium or large ventricular septal defect can cause a range of disabilities — from mild to life-threatening. Treatment can prevent many complications.
- Delayed growth and development (failure to thrive in infancy)
- Heart failure. In a heart with a medium or large ventricular septal defect, the heart needs to work harder to pump enough blood to the body. Because of this, heart failure can develop if medium to large ventricular septal defects aren’t treated.
- Pulmonary hypertension (high blood pressure in the lungs). Increased blood flow to the lungs due to the ventricular septal defect causes high blood pressure in the lung arteries (pulmonary hypertension), which can permanently damage them and cause failure of the right side of the heart. This complication can cause reversal of blood flow through the hole (Eisenmenger syndrome).
- Infective endocarditis (bacterial infection of the heart). This heart infection is an uncommon complication.
- Other heart problems. These include abnormal heart rhythms and valve problems.
- Aortic insufficiency (leaking of the valve that separates the left ventricle from the aorta)
- Damage to the electrical conduction system of the heart during surgery (causing an irregular or slow heart rhythm)
Ventricular septal defect symptoms
People with ventricular septal defects may not have symptoms. However, if the hole is large, the baby often has symptoms related to heart failure.
Signs and symptoms of serious heart defects often appear during the first few days, weeks or months of a child’s life.
Ventricular septal defect symptoms in a baby may include:
- Poor eating, failure to thrive or gain weight
- Fast breathing or breathlessness
- Easy tiring
- Paleness
- Fast heart rate
- Sweating while feeding
- Frequent respiratory infections
You and your doctor may not notice signs of a ventricular septal defect at birth. If the defect is small, symptoms may not appear until later in childhood — if at all. Signs and symptoms vary depending on the size of the hole and other associated heart defects.
Your doctor may first suspect a heart defect during a regular checkup if he or she hears a murmur while listening to your baby’s heart with a stethoscope. Sometimes ventricular septal defects can be detected by ultrasound before the baby is born.
Sometimes a ventricular septal defect isn’t detected until a person reaches adulthood. Symptoms and signs can include shortness of breath or a heart murmur your doctor hears when listening to your heart with a stethoscope.
When to see a doctor
See your doctor if your baby or child:
- Tires easily when eating or playing
- Is not gaining weight
- Becomes breathless when eating or crying
- Breathes rapidly or is short of breath
See your doctor if you develop:
- Shortness of breath when you exert yourself or when you lie down
- Rapid or irregular heartbeat
- Fatigue or weakness
Ventricular septal defect causes
Except for ventricular septal defect that is caused by a heart attack, this condition is always present at birth. Congenital heart defects arise from problems early in the heart’s development, but there’s often no clear cause. Genetics and environmental factors may play a role. ventricular septal defects can occur alone or with other congenital heart defects.
During fetal development, a ventricular septal defect occurs when the muscular wall separating the heart into left and right sides (septum) fails to form fully between the lower chambers of the heart (ventricles).
Normally, the right side of the heart pumps blood to the lungs to get oxygen; the left side pumps the oxygen-rich blood to the rest of the body. A ventricular septal defect allows oxygenated blood to mix with deoxygenated blood, causing the heart to work harder to provide enough oxygen to the body’s tissues.
ventricular septal defects may be various sizes, and they can be present in several locations in the wall between the ventricles. There may be one or more ventricular septal defect.
It’s also possible to acquire a ventricular septal defect later in life, usually after a heart attack or as a complication following certain heart procedures.
Risk factors for developing ventricular septal defect
Ventricular septal defects may run in families and sometimes may occur with other genetic problems, such as Down syndrome. If you already have a child with a heart defect, a genetic counselor can discuss the risk of your next child having one.
Ventricular septal defect prevention
Drinking alcohol and using the anti-seizure medicines depakote and dilantin during pregnancy may increase the risk for ventricular septal defects. Other than avoiding these things during pregnancy, there is no known way to prevent a ventricular septal defect.
In most cases, you can’t do anything to prevent having a baby with a ventricular septal defect. However, it’s important to do everything possible to have a healthy pregnancy. Here are the basics:
- Get early prenatal care, even before you’re pregnant. Talk to your doctor before you get pregnant about your health and discuss any lifestyle changes that your doctor may recommend for a healthy pregnancy. Also, be sure you talk to your doctor about any medications you’re taking.
- Eat a balanced diet. Include a vitamin supplement that contains folic acid. Also, limit caffeine.
- Exercise regularly. Work with your doctor to develop an exercise plan that’s right for you.
- Avoid risks. These include harmful substances such as alcohol, tobacco and illegal drugs.
- Avoid infections. Be sure you’re up to date on all of your vaccinations before becoming pregnant. Certain types of infections can be harmful to a developing fetus.
- Keep diabetes under control. If you have diabetes, work with your doctor to be sure it’s well-controlled before getting pregnant.
If you have a family history of heart defects or other genetic disorders, consider talking with a genetic counselor before getting pregnant.
Ventricular septal defect diagnosis
Ventricular septal defects (ventricular septal defects) often cause a heart murmur that your doctor can hear using a stethoscope. If your doctor hears a heart murmur or finds other signs or symptoms of a heart defect, he or she may order several tests including:
- Echocardiogram. In this test, sound waves produce a video image of the heart. Doctors may use this test to diagnose a ventricular septal defect and determine its size, location and severity. It may also be used to see if there are any other heart problems. Echocardiography can be used on a fetus (fetal echocardiography).
- Electrocardiogram (ECG). This test records the electrical activity of the heart through electrodes attached to the skin and helps diagnose heart defects or rhythm problems.
- Chest X-ray. An X-ray image helps the doctor view the heart and lungs. This can help doctors see if the heart is enlarged and if the lungs have extra fluid.
- MRI of the heart is used to find out how much blood is getting to the lungs
- Cardiac catheterization. In this test, a thin, flexible tube (catheter) is inserted into a blood vessel at the groin or arm and guided through the blood vessels into the heart. Through cardiac catheterization, doctors can diagnose congenital heart defects and determine the function of the heart valves and chambers.
- Pulse oximetry. A small clip on the fingertip measures the amount of oxygen in the blood.
Ventricular septal defect treatment
Many babies born with a small ventricular septal defect won’t need surgery to close the hole. After birth, your doctor may want to observe your baby and treat symptoms while waiting to see if the defect closes on its own. This is to make sure that the hole eventually closes properly and signs of heart failure do not occur.
Babies with a large ventricular septal defect who have symptoms related to heart failure may need medicine to control the symptoms and surgery to close the hole. Diuretic medicines are often used to relieve symptoms of congestive heart failure.
If symptoms continue, even with medicine, surgery to close the defect with a patch is needed. Babies who need surgical repair often have the procedure in their first year.
Children and adults who have a medium or large ventricular septal defect or one that’s causing significant symptoms may need surgery to close the defect.
Having surgery for a ventricular septal defect with no symptoms is controversial, especially when there is no evidence of heart damage. Discuss this carefully with your provider.
Some ventricular septal defects can be closed with a special device during a cardiac catheterization, which avoids the need for surgery. This is called transcatheter closure. However, only certain types of defects can successfully be treated this way.
Some smaller ventricular septal defects are closed surgically to prevent complications related to their locations, such as damage to heart valves. Many people with small ventricular septal defects have productive lives with few related problems.
Babies who have large ventricular septal defects or who tire easily during feeding may need extra nutrition to help them grow. Some babies may require tube feeding.
Medications
Medications for ventricular septal defect may include those to:
- Decrease the amount of fluid in circulation and in the lungs. Doing so reduces the volume of blood that must be pumped. These medications, called diuretics, include furosemide (Lasix).
- Keep the heartbeat regular. Examples include beta blockers, such as metoprolol (Lopressor), propranolol (Inderal LA) and others, and digoxin (Lanoxin, Lanoxin Pediatric).
Ventricular septal defect procedures
Surgical treatment for ventricular septal defects involves plugging or patching the abnormal opening between the ventricles. If you or your child is having surgery to repair a ventricular defect, consider having surgery performed by surgeons and cardiologists with training and expertise in conducting these procedures.
Procedures may include:
- Surgical repair. This procedure of choice in most cases usually involves open-heart surgery under general anesthesia. The surgery requires a heart-lung machine and an incision in the chest. The doctor uses a patch or stitches to close the hole.
- Catheter procedure. Closing a ventricular septal defect during catheterization doesn’t require opening the chest. Rather, the doctor inserts a thin tube (catheter) into a blood vessel in the groin and guides it to the heart. The doctor then uses a specially sized mesh device to close the hole.
- Hybrid procedure. A hybrid procedure uses surgical and catheter-based techniques. Access to the heart is usually through a small incision, and the procedure may be performed without stopping the heart and using the heart-lung machine. A device closes the ventricular septal defect via a catheter placed through the incision.
After repair, your doctor will schedule regular medical follow-up to ensure that the ventricular septal defect remains closed and to look for signs of complications. Depending on the size of the defect and the presence of other problems, your doctor will tell you how frequently you or your child will need to be seen.
Post-op care
After your ventricular septal defect (ventricular septal defect) is repaired, you or your child will need follow-up care throughout life for doctors to monitor your condition and check for any signs of complications.
Your doctor may suggest that you or your child have regular follow-up appointments with a doctor who specializes in congenital heart disease. In follow-up appointments, your doctor may evaluate you or your child and order imaging tests to monitor your or your child’s condition.
Here are a few tips for managing your or your child’s condition:
- Consider pregnancy carefully. Before becoming pregnant, talk to a doctor trained in heart conditions (cardiologist) to determine if you can undergo pregnancy safely. This is especially important if you’re taking medications. It’s also important to see both an obstetrician and a cardiologist during pregnancy. Having a repaired ventricular septal defect without complications or having a small defect doesn’t pose an additional pregnancy risk. However, having an unrepaired, larger defect; heart failure; pulmonary hypertension; abnormal heart rhythms; or other heart defects poses a high risk to both mother and fetus. Doctors strongly advise women with Eisenmenger syndrome not to become pregnant because of the high risk of complications.
- Prevent endocarditis. You or your child usually won’t need to take antibiotics before certain dental procedures to prevent an infection of the heart’s inner lining (endocarditis). However, your doctor may recommend antibiotics if you’ve had prior endocarditis, a heart valve replacement, if you have had a recent ventricular septal defect repair with artificial material, if you still have leaks through the ventricular septal defect, if the repaired ventricular septal defect is next to a defect that’s been repaired with artificial material, or if you have a large ventricular septal defect that’s causing low oxygen levels. For most people with a ventricular septal defect, good oral hygiene and regular dental checkups can prevent endocarditis.
- Follow exercise recommendations. Your doctor can advise you about which activities are safe for you or your child. If some activities pose special dangers, encourage your child to engage in other, safer activities. Keep in mind that many children with ventricular septal defects can lead healthy, fully active, productive lives.
Children with small defects or a repaired hole in the heart will usually have few or no restrictions on activity or exercise. Children whose hearts don’t pump as normally will need to follow some limits. A child with irreversible pulmonary hypertension (Eisenmenger syndrome) has the greatest number of restrictions.
- Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, et al; for the National Birth Defects Prevention Network. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88(12):1008-16.[↩]
- Gill HR, Splitt M, Sharland GK, Simpson JM. 2003. Patterns of recurrence of congenital heart disease: An analysis of 6,640 consecutive pregnancies evaluated by detailed fetal echocardiography. Journal of the American College of Cardiology; 42: 923-9.[↩]