Contents
- What is sleep ?
- Why is Sleep Important ?
- Regulation of sleep-wake cycles
- Sleep mechanisms
- Sleep functions
- Sleep Stages
What is sleep ?
Sleep can be defined as a temporary state of unconsciousness from which (in contrast to coma) one can awaken when stimulated. Sleep is an active state of unconsciousness produced by the body where the brain is in a relative state of rest and is reactive primarily to internal stimulus 1. Sleep is one of many bodily functions that occur in cycles called circadian rhythms, so named because they are marked by events that reoccur at intervals of about 24 hours. Sleep is characterized by a stereotyped posture (usually lying down with the eyes closed) and inhibition of muscular activity (sleep paralysis). It superficially resembles other states of prolonged unconsciousness such as coma and animal hibernation, except that individuals cannot be aroused from those states by sensory stimulation.
However, the exact purpose of sleep has not been fully elucidated 1. There are several prominent theories currently which have explored the brain and attempt to identify a purpose for why you sleep which includes the Inactivity theory, Energy conservation theory, Restoration theory, and the Brain plasticity theory.
Inactivity theory is based on the concept of evolutionary pressure where creatures that were inactive at night were less likely to die from the predation of injury in the dark, thus creating an evolutionary and reproductive benefit to be inactive at night.
Energy conservation theory posits that the main function of sleep is to reduce a person’s energy demand during part of the day and night when it is least efficient to hunt for food. This theory is supported by the fact that the body has decreased metabolism of up to 10% during sleep.
The restorative theory states that sleep allows for the body to repair and replete cellular components necessary for biological functions that become depleted throughout an awake day. This is backed by the findings many functions in the body such as muscle repair, tissue growth, protein synthesis, and release of many of the important hormones for growth occur primarily during sleep.
Brain plasticity theory is that sleep is necessary for neural reorganization and growth of the brain’s structure and function. It is clear that sleep plays a role in the development of the brain in infants and children and explains why it is necessary that infants sleep upwards of 14 hours per day.
These theories are not exhaustive or all-inclusive of the prevalent ideas; rather, they serve to frame the concept that scientists do not fully understand sleep yet. It is more accepted that no single theory explains it all, and a combination of these ideas is more likely to hold the key to sleep 1.
Although sleep is essential to the normal functioning of the body, the exact functions of sleep are still unclear. Studies have shown that sleep deprivation impairs attention, memory, performance, and immunity; if the lack of sleep lasts long enough, it can lead to mood swings, hallucinations, and even death.
There has been considerable debate in the scientific community about the importance of sleep, but some proposed functions of sleep are widely accepted:
- Restoration, providing time for the body to repair itself;
- Consolidation of memories;
- Enhancement of immune system function; and
- Maturation of the brain.
Sleep deprivation impairs attention, learning, and performance.
Why is Sleep Important ?
Sleep plays a vital role in good health and well-being throughout your life. Getting enough quality sleep at the right times can help protect your mental health, physical health, quality of life, and safety 2.
The way you feel while you’re awake depends in part on what happens while you’re sleeping 2. During sleep, your body is working to support healthy brain function and maintain your physical health. In children and teens, sleep also helps support growth and development.
The damage from sleep deficiency can occur in an instant (such as a car crash), or it can harm you over time. For example, ongoing sleep deficiency can raise your risk for some chronic health problems. It also can affect how well you think, react, work, learn, and get along with others.
Healthy Brain Function and Emotional Well-Being
Sleep helps your brain work properly. While you’re sleeping, your brain is preparing for the next day. It’s forming new pathways to help you learn and remember information.
Studies show that a good night’s sleep improves learning 2. Whether you’re learning math, how to play the piano, how to perfect your golf swing, or how to drive a car, sleep helps enhance your learning and problem-solving skills. Sleep also helps you pay attention, make decisions, and be creative.
Studies also show that sleep deficiency alters activity in some parts of the brain. If you’re sleep deficient, you may have trouble making decisions, solving problems, controlling your emotions and behavior, and coping with change. Sleep deficiency also has been linked to depression, suicide, and risk-taking behavior 2.
Children and teens who are sleep deficient may have problems getting along with others. They may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation. They also may have problems paying attention, and they may get lower grades and feel stressed 2.
Physical Health
Sleep plays an important role in your physical health. For example, sleep is involved in healing and repair of your heart and blood vessels. Ongoing sleep deficiency is linked to an increased risk of heart disease, kidney disease, high blood pressure, diabetes, and stroke 2.
A lack of sleep also puts your body under stress and may trigger the release of more adrenaline, cortisol, and other stress hormones during the day. These hormones keep your blood pressure from dipping during sleep, which increases your risk for heart disease. Lack of sleep also may trigger your body to produce more of certain proteins thought to play a role in heart disease. For example, some studies find that people who repeatedly don’t get enough sleep have higher than normal blood levels of C-reactive protein, a sign of inflammation. High levels of this protein may indicate an increased risk for a condition called atherosclerosis, or hardening of the arteries.
Sleep deficiency also increases the risk of obesity. For example, one study of teenagers showed that with each hour of sleep lost, the odds of becoming obese went up. Sleep deficiency increases the risk of obesity in other age groups as well 2.
Sleep helps maintain a healthy balance of the hormones that make you feel hungry (ghrelin) or full (leptin) 2. When you don’t get enough sleep, your level of ghrelin goes up and your level of leptin goes down. This makes you feel hungrier than when you’re well-rested 2.
Evidence is growing that sleep is a powerful regulator of appetite, energy use, and weight control. During sleep, the body’s production of the appetite suppressor leptin increases and the appetite stimulant grehlin decreases. Studies find that the less people sleep, the more likely they are to be overweight or obese and prefer eating foods that are higher in calories and carbohydrates. People who report an average total sleep time of 5 hours a night, for example, are much more likely to become obese, compared with people who sleep 7–8 hours a night.
Sleep also affects how your body reacts to insulin, the hormone that controls your blood glucose (sugar) level. Sleep deficiency results in a higher than normal blood sugar level, which may increase your risk for diabetes 2. One study found that, when healthy young men slept only 4 hours a night for 6 nights in a row, their insulin and blood sugar levels matched those seen in people who were developing diabetes. Another study found that women who slept less than 7 hours a night were more likely to develop diabetes over time than those who slept between 7 and 8 hours a night.
Sleep also supports healthy growth and development 2. Deep sleep triggers the body to release the hormone that promotes normal growth in children and teens. This hormone also boosts muscle mass and helps repair cells and tissues in children, teens, and adults. Sleep also plays a role in puberty and fertility.
Your immune system relies on sleep to stay healthy 2. This system defends your body against foreign or harmful substances. Ongoing sleep deficiency can change the way in which your immune system responds. For example, if you’re sleep deficient, you may have trouble fighting common infections.
During sleep, your body creates more cytokines—cellular hormones that help the immune system fight various infections. Lack of sleep can reduce your body’s ability to fight off common infections. Research also reveals that a lack of sleep can reduce the body’s response to the flu vaccine. For example, sleep-deprived volunteers given the flu vaccine produced less than half as many flu antibodies as those who were well rested and given the same vaccine.
Daytime Performance and Safety
Getting enough quality sleep at the right times helps you function well throughout the day. People who are sleep deficient are less productive at work and school 2. They take longer to finish tasks, have a slower reaction time, and make more mistakes.
After several nights of losing sleep—even a loss of just 1–2 hours per night—your ability to function suffers as if you haven’t slept at all for a day or two.
Lack of sleep also may lead to microsleep 2. Microsleep refers to brief moments of sleep that occur when you’re normally awake.
You can’t control microsleep and you might not be aware of it 2. For example, have you ever driven somewhere and then not remembered part of the trip ? If so, you may have experienced microsleep.
Even if you’re not driving, microsleep can affect how you function. If you’re listening to a lecture, for example, you might miss some of the information or feel like you don’t understand the point. In reality, though, you may have slept through part of the lecture and not been aware of it.
Some people aren’t aware of the risks of sleep deficiency. In fact, they may not even realize that they’re sleep deficient. Even with limited or poor-quality sleep, they may still think that they can function well.
Several studies show that lack of sleep causes thinking processes to slow down. Lack of sleep also makes it harder to focus and pay attention. Lack of sleep can make you more easily confused. Studies also find that a lack of sleep leads to faulty decision making and more risk taking. A lack of sleep slows down your reaction time, which is particularly important to driving and other tasks that require quick response. When people who lack sleep are tested on a driving simulator, they perform just as poorly as people who are drunk.
For example, drowsy drivers may feel capable of driving. Yet, studies show that sleep deficiency harms your driving ability as much as, or more than, being drunk. It’s estimated that driver sleepiness is a factor in about 100,000 car accidents each year, resulting in about 1,500 deaths 2.
Drivers aren’t the only ones affected by sleep deficiency. It can affect people in all lines of work, including health care workers, pilots, students, lawyers, mechanics, and assembly line workers.
As a result, sleep deficiency is not only harmful on a personal level, but it also can cause large-scale damage. For example, sleep deficiency has played a role in human errors linked to tragic accidents, such as nuclear reactor meltdowns, grounding of large ships, and aviation accidents.
Regulation of sleep-wake cycles
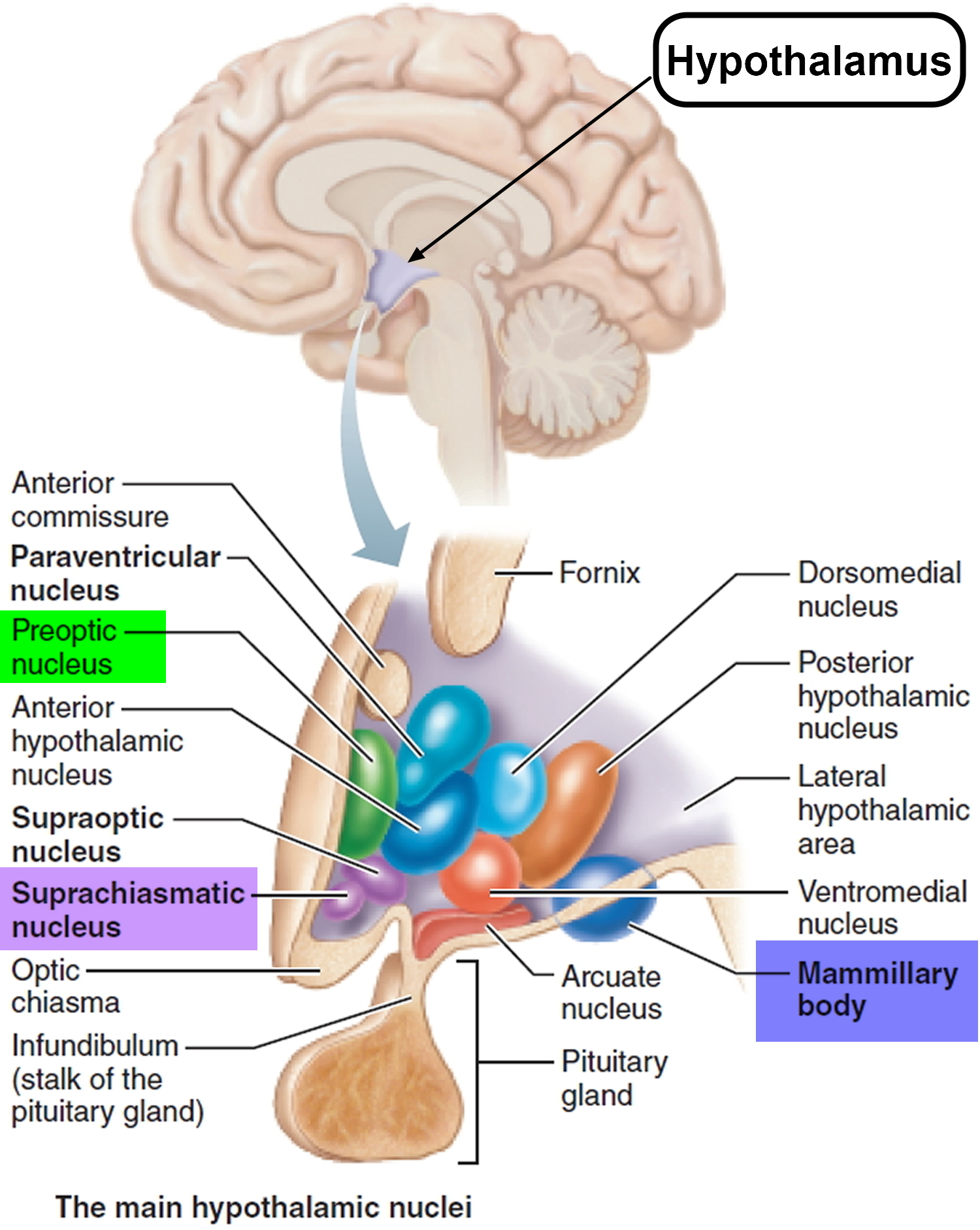
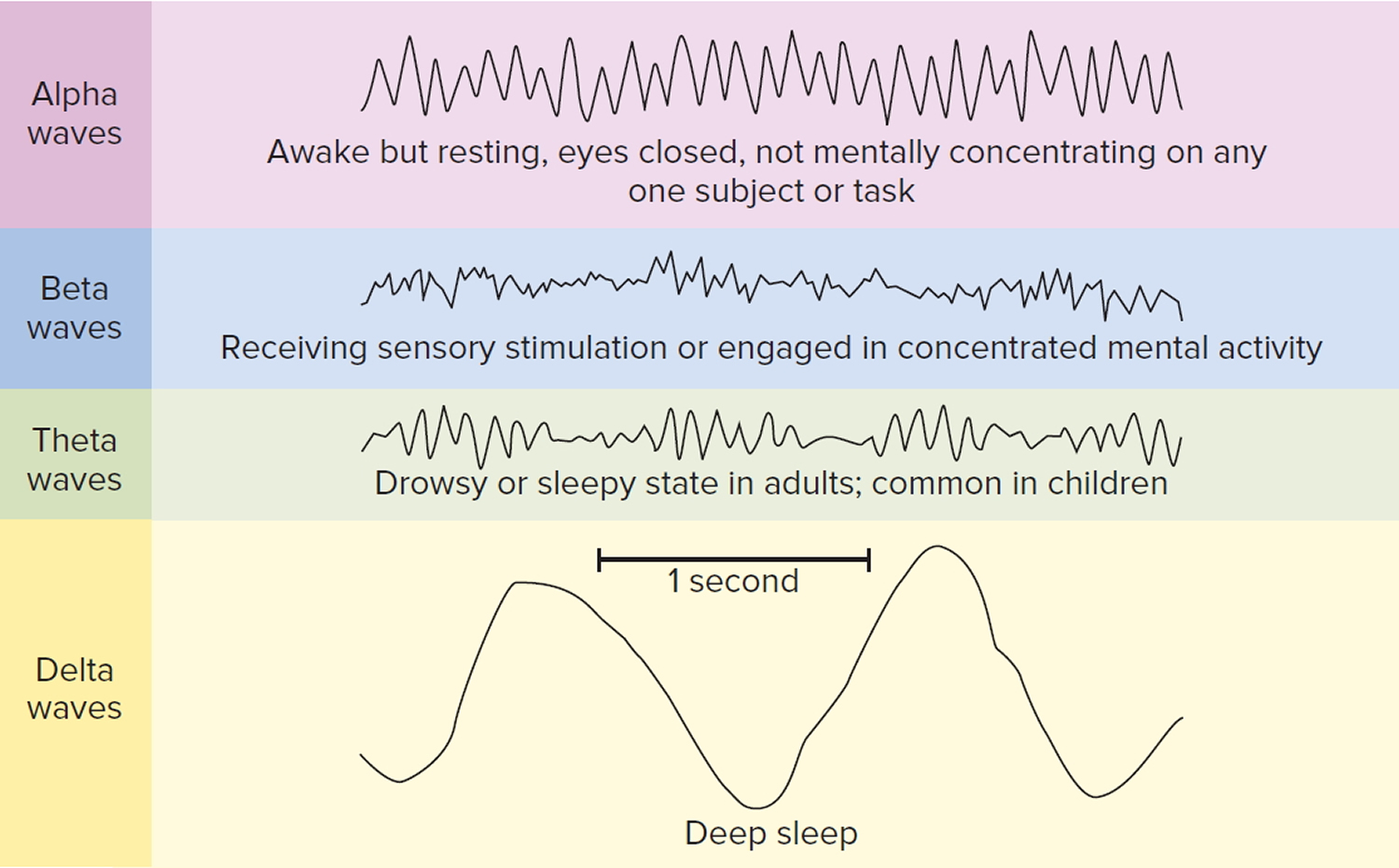
Humans sleep and awaken in a 24-hour cycle called a circadian rhythm that is established by the suprachiasmatic nucleus of the hypothalamus (see Figure 1). A person who is awake is in a state of readiness and is able to react consciously to various stimuli. EEG (electroencephalogram, a test that detects electrical activity in your brain using small, flat metal discs (electrodes) attached to your scalp) recordings show that the cerebral cortex is very active during wakefulness; fewer impulses arise during most stages of sleep.
How does your nervous system make the transition between these sleep-wake states ?
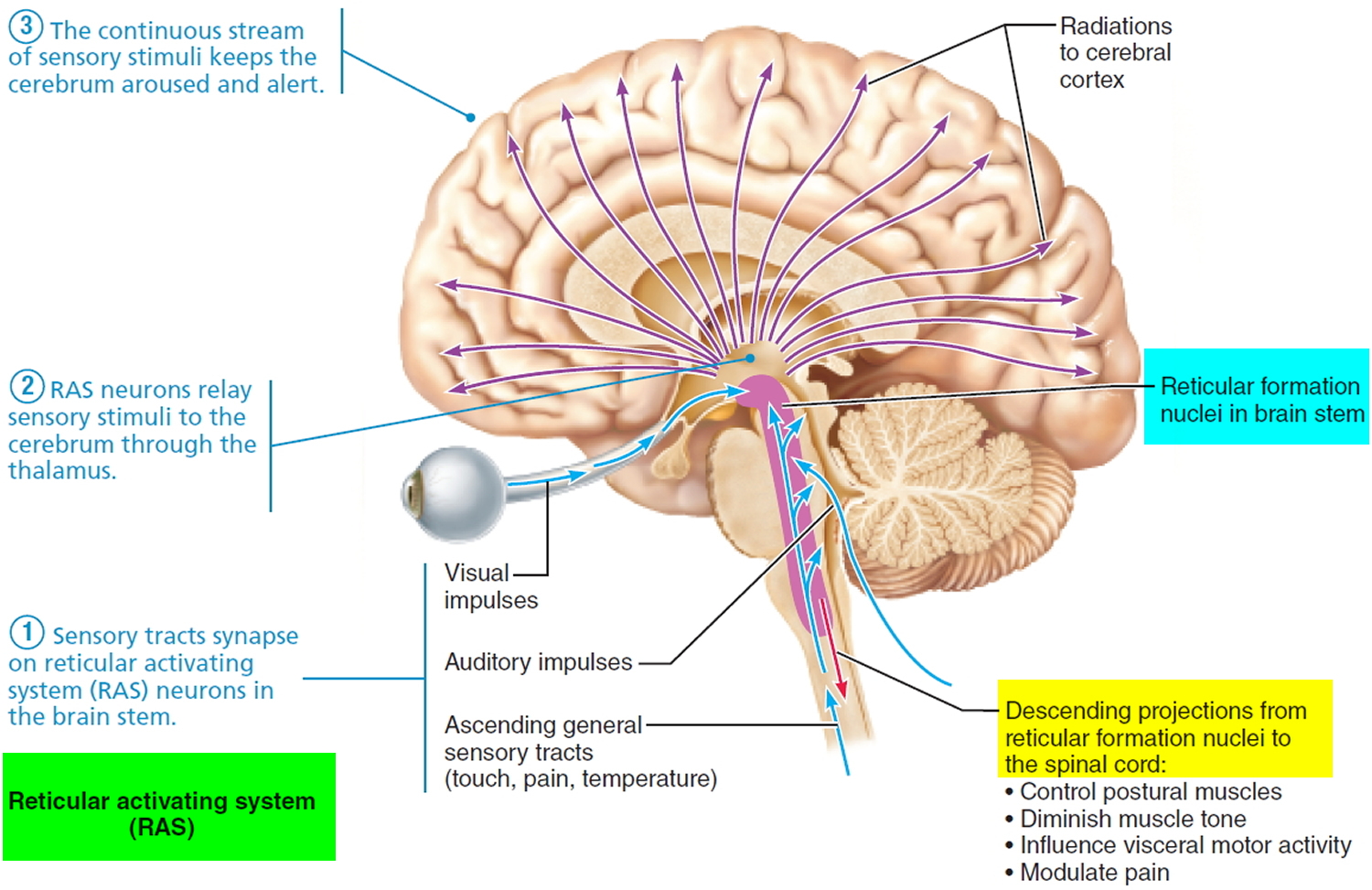
Because stimulation of some parts of the brain and the nervous system increases activity of the cerebral cortex, a portion of the reticular formation known as the reticular activating system (RAS) (see Figure 3), when the reticular activating system (RAS) area is active, many nerve impulses are transmitted to widespread areas of the cerebral cortex, both directly and via the thalamus. The effect is a generalized increase in cortical activity.
Arousal, or awakening from sleep, also involves increased activity in the reticular activating system (RAS). For arousal to occur, the RAS must be stimulated. Many sensory stimuli can activate the RAS: painful stimuli detected by nociceptors, touch and pressure on the skin, movement of the limbs, bright light, or the buzz of an alarm clock. Once the RAS is activated, the cerebral cortex is also activated, and arousal occurs. The result is a state of wakefulness called consciousness. Notice in Figure 3 that even though the reticular activating system (RAS) receives input from somatic sensory receptors, the eyes, and the ears, there is no input from olfactory receptors; even strong odors may fail to cause arousal. People who die in house fires usually succumb to smoke inhalation without awakening. For this reason, all sleeping areas should have a nearby smoke detector that emits a loud alarm. A vibrating pillow or flashing light can serve the same purpose for those who are hearing impaired.
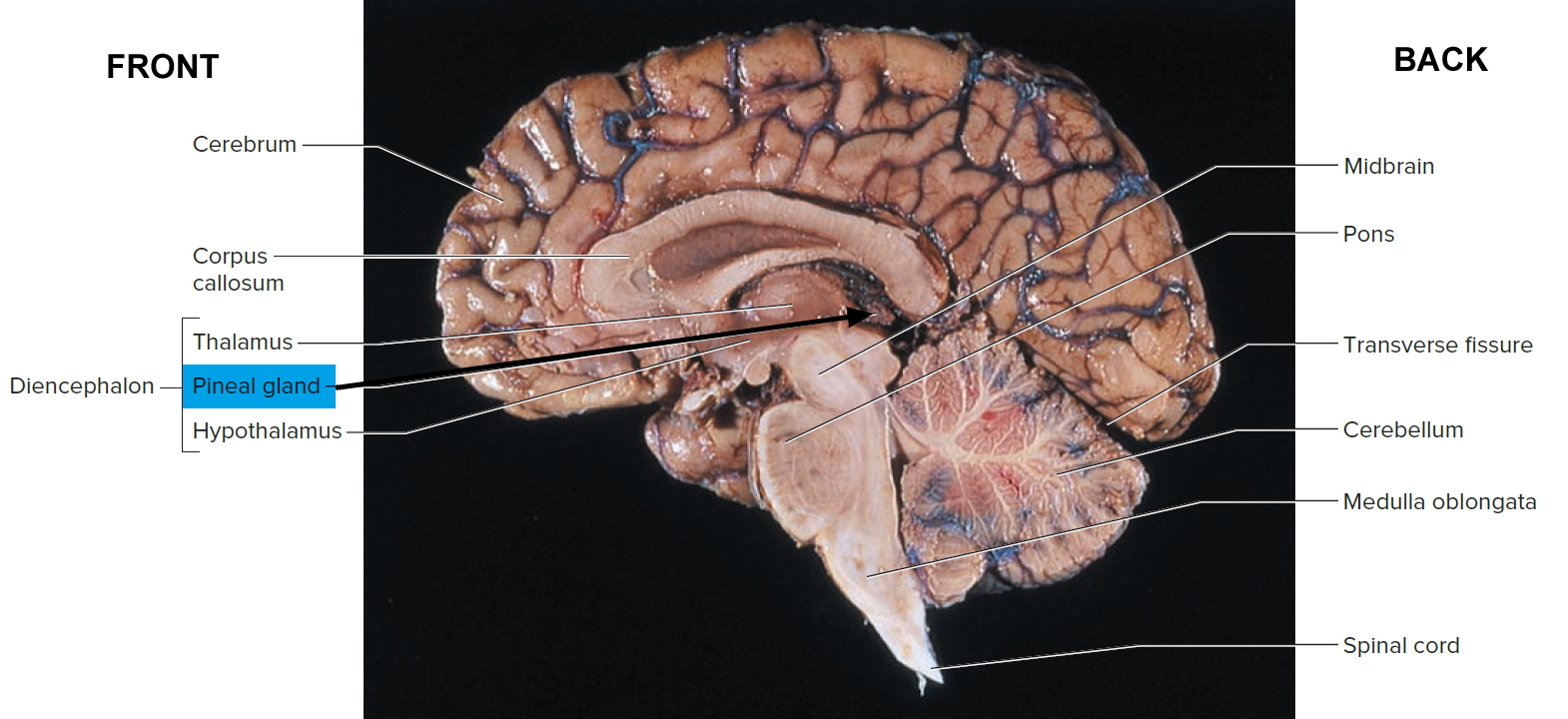
Acting with other brain regions, the hypothalamus helps regulate the complex phenomenon of sleep. The suprachiasmatic nucleus (Figure 1) is the body’s biological clock. It generates the daily circadian rhythms and synchronizes these cycles in response to dark-light information sensed via the optic nerve. In response to such signals, the preoptic nucleus induces sleep. Other hypothalamic nuclei near the mammillary body mediate arousal from sleep. Under the influence of the hypothalamus, the pineal gland secretes the hormone melatonin, which signals the body to prepare for the nighttime stage of the sleep-wake cycle. The pineal gland (pineal body) is a small, pine cone-shaped structure at the end of a short stalk on the roof of the diencephalon (epithalamus) (see Figure 2). During the darkness of night, the suprachiasmatic nucleus of the hypothalamus responds to a lack of visual input from the retina by sending signals to the preganglionic sympathetic neurons in the upper thoracic spinal cord. The signals then go to postganglionic neurons in the superior cervical ganglion, whose axons run on the internal carotid artery to stimulate the pineal gland to secrete melatonin. Increased melatonin levels promote sleepiness.
Elevated melatonin levels get the body ready for sleep. The timing of the rise in melatonin levels changes during a lifetime. In youth and childhood, melatonin levels rise in the early evening hours, and thus young children tire early in the night. In adolescence, the time at which melatonin levels rise shifts to much later in the night. As a result, teenagers are not sleepy until quite late in the night. This physiological shift makes it difficult for teenagers to fall asleep at a reasonable hour. The sleep deficit is compounded by the fact that most secondary schools start early in the morning. A few school systems have recognized this biological constraint and have changed the start of high school to later in the morning, allowing their students to get their needed sleep.
The reticular activating system (RAS) that is located mainly in the medial nuclear group of the pons and medulla in the brain stem also functions in sleep and in
arousal from sleep (see Figure 3). Axons from all the major ascending sensory nerve tracts synapse on reticular activating system (RAS) neurons, keeping these reticular neurons active and enhancing their arousing effect on the cerebrum. The fact that visual, auditory, and touch stimuli keep people awake and mentally alert explains why many students like to study in a crowded room: they are stimulated by the bustle of such an environment. General anesthesia, alcohol, tranquilizers, and sleep-inducing drugs depress the RAS and lead to a loss of alertness or consciousness. Severe injury to the RAS is a cause of coma.
Descending pathways of the reticular formation send axons to the spinal cord via the reticulospinal tracts. Certain descending pathways from the reticular formation influence somatic motor neurons to postural muscles. Others diminish muscle tone by inhibiting motor neurons, as when the person is sleeping. Axons from the reticular formation influence the autonomic neurons that regulate visceral functions such as heart rate, blood pressure, and respiration. Another group of descending fibers from the reticular fromation influence our perception of pain by inhibiting the transmission of pain impulses.
The brain stem, at the base of the brain, communicates with the hypothalamus to control the transitions between wake and sleep. (The brain stem includes structures called the pons, medulla, and midbrain.) Sleep-promoting cells within the hypothalamus and the brain stem produce a brain chemical called GABA, which acts to reduce the activity of arousal centers in the hypothalamus and the brain stem. The brain stem (especially the pons and medulla) also plays a special role in rapid eye movement (REM) sleep; it sends signals to relax muscles essential for body posture and limb movements, so that we don’t act out our dreams.
The basal forebrain, near the front and bottom of the brain, also promotes sleep and wakefulness, while part of the midbrain acts as an arousal system. Release of adenosine (a chemical by-product of cellular energy consumption) from cells in the basal forebrain and probably other regions supports your sleep drive. Caffeine counteracts sleepiness by blocking the actions of adenosine.
In addition, two related brain neuropeptides called orexins act as an important “sleep switch.” Produced by the hypothalamus, orexins stimulate increased activity in neurons of the reticular formation, leading to arousal and waking. Blocking orexin receptors induces sleep. Orexins are absent or at low levels in a disorder called narcolepsy, in which a person experiences excessive daytime sleepiness and fatigue and may often fall asleep at work or school, with abnormally quick onset of REM sleep. Narcolepsy seems to be an autoimmune disease caused by antibody-mediated destruction of the orexin-producing neurons.
What about melatonin ?
Your body produces this hormone that may cause some drowsiness and cues the brain and body that it is time to fall asleep. Melatonin builds up in your body during the early evening and into the first 2 hours of your sleep period, and then its release stops in the middle of the night.
Melatonin is available as an over-the-counter supplement. Because melatonin is considered safe when used over a period of days or weeks and seems to help people feel sleepy, it has been suggested as a treatment for jet lag. But melatonin’s effectiveness is controversial, and its safety when used over a prolonged period is unclear. Some studies find that taking melatonin supplements before bedtime for several days after arrival in a new time zone can make it easier to fall asleep at the proper time. Other studies find that melatonin does not help relieve jet lag.
Figure 1. Hypothalamus (suprachiasmatic nucleus) – regulation of sleep-wake cycles
Figure 2. Pineal gland
Figure 3. Reticular activating system & Reticular formation- regulation of sleep-wake cycles
Sleep mechanisms
Two internal biological mechanisms–circadian rhythm and homeostasis–work together to regulate when you are awake and sleep.
The mechanism through which sleep is generated and maintained is more of a balance between two systems located within the brain: the homeostatic processes which are functionally the body’s “need for sleep” center and the circadian rhythm which is an internal clock for the sleep-wake cycle 1.
Sleep Generation is initiated within the ventrolateral preoptic nucleus (VLPO) of the anterior hypothalamus and acts to inhibit the arousal regions of the brain including the tuberomammillary nucleus, lateral hypothalamus, locus coeruleus, dorsal raphe, laterodorsal tegmental nucleus, and pedunculopontine tegmental nucleus. Hypocretin (orexin) neurons in the lateral hypothalamus help to facilitate this process in a synergistic effect.
Non-rapid eye movement (NREM) sleep is a functional disconnection between the brain stem and the thalamus and cortex maintained with hyperpolarizing GABA neurons in the reticular activating center of the thalamus and the cortex. Corticothalamic neurons signal the thalamus which causes hyperpolarization of the thalamic reticular neurons. This process produces delta waves from both thalamic reticular and cortical pyramidal sources. Thus correlating with the varying stages 1 to 3 of non-rapid eye movement (NREM).
Rapid eye movement (REM) sleep is generated by “REM-on neurons” in the mesencephalic and pontine cholinergic neurons. The pedunculopontine tegmental nucleus and the lateral dorsal tegmental neurons trigger desynchronized cortical waveforms. The tonic component of rapid eye movement (REM) sleep is parasympathetically medicated, and the phasic component is sympathetically mediated.
Circadian rhythms
Circadian rhythm regulates sleep, which tends to change over the course of human lives 3. Circadian rhythms direct a wide variety of functions from daily fluctuations in wakefulness to body temperature, metabolism, and the release of hormones. They control your timing of sleep and cause you to be sleepy at night and your tendency to wake in the morning without an alarm. Your body’s biological clock, which is based on a roughly 24-hour day, controls most circadian rhythms. Circadian rhythms synchronize with environmental cues (light, temperature) about the actual time of day, but they continue even in the absence of cues.
Newborns spend about 50% of their total sleep in REM sleep, usually directly entering REM sleep. Newborns also tend to initially sleep in short intervals, obtaining around 12 to 18 hours of sleep. As children reach 5 to 10 years of age, their sleep demand decreases to 10 hours. The demand further decreases as teenagers require 8 to 9 hours and adults need 7 to 8 hours. Your circadian rhythm also controls the nocturnal release of adrenocorticotropic hormone (ACTH), prolactin, melatonin, and norepinephrine, which are all essentials hormones for normal body functioning 4.
Circadian rhythm is the body’s cyclical nature for the desire for sleep. The hypothalamus controls it via the suprachiasmatic nucleus with sensory input from the retinohypothalamic tract based on light levels detected from the retina 1. The circadian rhythm is approximately 24.2 hours per cycle 1. Melatonin, produced in the pineal gland, has also been shown to be a modulator of the circadian rhythm that has concentrations varied based on light level. Melatonin levels are greatest in the night and decreased during the daytime. Finally, body temperature has been associated as part of the circadian rhythm. The exact set point varies among different people, but it is expected to have generally lower temperatures in the morning and higher temperatures in the evening 1.
Sleep-wake homeostasis
Sleep-wake homeostasis keeps track of your need for sleep. The homeostatic sleep drive reminds the body to sleep after a certain time and regulates sleep intensity. This sleep drive gets stronger every hour you are awake and causes you to sleep longer and more deeply after a period of sleep deprivation.
Factors that influence your sleep-wake needs include medical conditions, medications, stress, sleep environment, and what you eat and drink. Perhaps the greatest influence is the exposure to light. Specialized cells in the retinas of your eyes process light and tell the brain whether it is day or night and can advance or delay our sleep-wake cycle. Exposure to light can make it difficult to fall asleep and return to sleep when awakened.
Night shift workers often have trouble falling asleep when they go to bed, and also have trouble staying awake at work because their natural circadian rhythm and sleep-wake cycle is disrupted. In the case of jet lag, circadian rhythms become out of sync with the time of day when people fly to a different time zone, creating a mismatch between their internal clock and the actual clock.
Sleep functions
Sleep functions in a relatively predictable cyclical pattern between 2 major phases: Non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep 1. Non-rapid eye movement (NREM) sleep is subdivided into several stages numbered 1 to 3. Each phase and stage represents the relative depth of sleep and offers unique characteristics in the brain wave, muscle tones, and eye movement patterns. As the name implies, non-rapid eye movement (NREM) is characterized by an absence of eye movements and REM (rapid eye movement) is characterized by rapid eye movements.
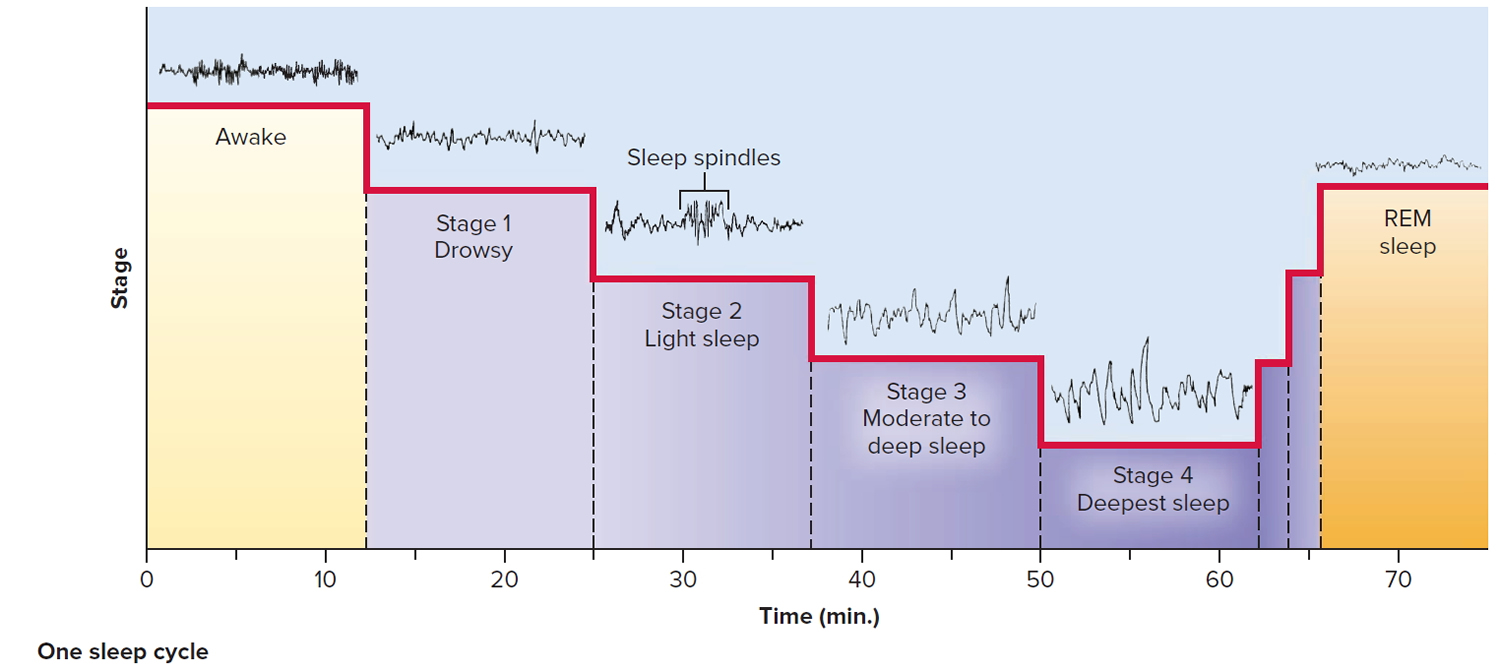
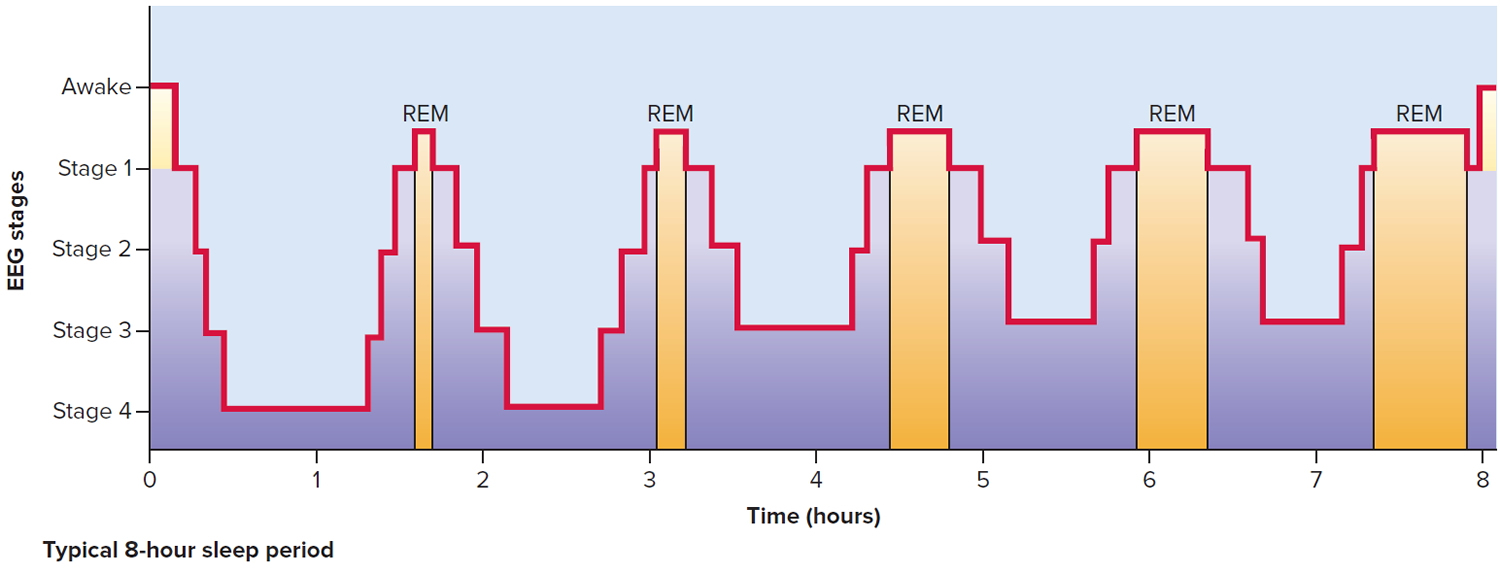
Sleep begins with a short NREM stage 1 phase, followed by NREM stage 2, then NREM stage 3, then finally into REM sleep. NREM accounts for approximately 75% to 80% of total sleep and REM accounts for the remaining 20% to 25% of sleep 1. This progression through the stages of sleep occurs in this order of events on repeat throughout the night for varying lengths of time. The initial cycle lasts 70 to 100 minutes to complete fully. However, the remaining cycles last 90 to 120 minutes each. The amount of REM in each cycle progresses throughout the night from being minimal on initiation of sleep, but eventually is up to 30% of the cycle later in the night. A total of 4 to 5 cycles through this progression is typical in a night.
NREM stage 1 is the shallow stage of sleep where a person is still easily awoken. It lasts 1 to 7 minutes. Rhythmical alpha waves characterize electroencephalogram (EEG) at a frequency of 8 to 13 cycles per second.
NREM stage 2 lasts approximately 10 to 25 minutes in the initial cycle of sleep but progresses to consume 50% of the total sleep cycle later in the night. Stage 2 is a much deeper sleep state than stage 1, but individuals are still awoken with heavy stimulation. Brainwave activity on EEG is low voltage “sleep spindles and K-complexes.” Current theories suggest that memory consolidation occurs primarily during this stage.
NREM stage 3 lasts about 20 to 40 minutes, initially. EEG characterized by high-voltage, slow wave frequency.
REM is the phase of sleep responsible for dreaming. It is characterized by total body voluntary muscle paralysis (except for the extraocular muscles). This paralysis is thought to be a mechanism to prevent neural stimulus from dreams to manifest in actual muscular impulses during sleep. EEG in REM is “Sawtooth waveforms,” theta waves, and slow, alpha waves in a desynchronized pattern set.
Sleep Stages
Sleep is broken down into 5 distinct stages recognizable from changes in the EEG: Wake (Stage W), NREM stage 1, NREM stage 2, NREM stage 3, and REM sleep 3. In the first 30 to 45 minutes, the EEG waves drop in frequency but increase in amplitude as one passes through five sleep stages. Non-rapid eye movement (NREM) stages 1 to 3 are considered non-rapid eye movement sleep, each progressively going into deeper sleep. Sleep is staged in sequential 30-second epochs, and each of these epochs is assigned a specific sleep stage. The majority of sleep is spent in the NREM stage 2 5. During sleep, your body cycles through 4 different stages consisting of both rapid-eye-movement (REM) and non-rapid eye movement (NREM) sleep. Your body usually cycles through these stages on average 4 to 6 times, averaging 90 minutes in each stage. As the night progresses, fewer NREM stages occur, and the duration of REM sleep episodes increase 6.
Wake (Stage W)
Stage 1 is the wake stage or stage W, which further depends on whether the eyes are open or closed. During eye-open wakefulness, there are alpha and beta waves present, predominantly beta. As individuals become drowsy, and the eyes close, the alpha rhythm is the predominant pattern. An epoch is considered stage W if it contains greater than 50% alpha waves and eye movements associated with wakefulness 7.
Stage W is a transition stage between wakefulness and sleep that normally lasts 1–7 minutes. One feels drowsy, closes the eyes, and begins to relax. Thoughts come and go, often accompanied by a drifting sensation. One awakens easily if stimulated. The EEG is dominated by alpha waves. People awakened during this stage often say they have not been sleeping.
NREM Stage 1 (N1)
This is the lightest stage of sleep and starts when more than 50% of the alpha waves are replaced with low-amplitude mixed-frequency (LAMF) activity. There is muscle tone present in the skeletal muscle and breathing tends to occur at a regular rate. This stage tends to last 1 to 5 minutes, consisting of around 5% of the total cycle.
One passes into light sleep (first stage of “true sleep”). The EEG declines in frequency but increases in amplitude. Occasionally it exhibits 1 or 2 seconds of sleep spindles, high spikes resulting from interactions between neurons of the thalamus and cerebral cortex. In it, a person is easy to awaken. Fragments of dreams may be experienced and the eyes may slowly roll from side to side.
NREM Stage 2 (N2)
This stage represents deeper sleep as your heart rate and body temperate drop. It is characterized by the presence of sleep spindles, K-complexes or both. These sleep spindles will activate the superior temporal gyri, anterior cingulate, insular cortices and the thalamus. The K-complexes show a transition into deeper sleep. They are single, long delta waves only lasting for a second. As deeper sleep ensues and the individual moves into N3. All of their waves will be replaced with delta waves. Stage 2 sleep lasts around 25 minutes in the initial cycle and lengthens with each successive cycle, eventually consisting of about 50% of total sleep.
This is moderate to deep sleep, typically beginning about 20 minutes after stage 1. Sleep spindles occur less often, and theta and delta waves appear. The muscles relax, and the vital signs (body temperature, blood pressure, and heart and respiratory rates) fall.
NREM Stage 3 (N3)
This is considered the deepest stage of sleep, also called slow-wave sleep (SWS), because the EEG is characterized by a much slower frequency with high amplitude signals known as delta waves. The muscles are now very relaxed, vital signs are at their lowest levels, brain metabolism decreases significantly and body temperature drops slightly at this time and most reflexes are intact. During this stage, it is the most difficult to awaken from, and for some people, even loud noises (over 100 decibels) will not awaken them. As people get older, they tend to spend less time in this slow, delta wave sleep and more time stage N2 sleep. Although this stage has the greatest arousal threshold, if someone is awoken during this stage, they will have a transient phase of mental fogginess. This is known as sleep inertia. Cognitive testing shows that individuals awoken during this stage tend to have mental performance moderately impaired for 30 minutes to an hour. This is the stage when the body repairs and regrows its tissues, builds bone and muscle and strengthens the immune system.
REM Sleep
This is the stage associated with dreaming. Interestingly, the EEG is similar to an awake individual, but the skeletal muscles are atonic and without movement. The exception is the eye and diaphragmatic breathing muscles, which remain active. The breathing rate is altered though, being more erratic and irregular. This stage usually starts 90 minutes after you fall asleep, and each of your REM cycles gets longer throughout the night. The first period typically lasts 10 minutes, and the final one can last up to an hour 8.
Sleep studies
Your health care provider may recommend a polysomnogram or other test to diagnose a sleep disorder. A polysomnogram typically involves spending the night at a sleep lab or sleep center. It records your breathing, oxygen levels, eye movements, muscle movement of chin and legs, nasal pressure and airflow, chest and thorax movement, and pulse oximetry, heart rate, and EEG (brain waves) throughout the night. Your sleep is also video and audio recorded. These tests are performed overnight and usually require a minimum of 6 hours of monitoring. The data can help a sleep specialist determine if you are reaching and proceeding properly through the various sleep stages. Results may be used to develop a treatment plan or determine if further tests are needed.
Figure 4. Electroencephalogram (EEG)
Normal sleep consists of two components:
- Non-rapid eye movement (NREM) sleep and
- Rapid eye movement (REM) sleep.
Several physiological changes occur during non-rapid eye movement (NREM) sleep. There are decreases in heart rate, respiratory rate, and blood pressure. Muscle tone also decreases, out only slightly. As a result, there is a moderate amount of muscle tone during NREM sleep, which allows the sleeping person to shift body positions while in bed.
Dreaming sometimes takes place during NREM sleep but only occasionally. However, most dreaming occurs during rapid eye movement (REM) sleep. When dreaming does occur during NREM sleep, the dreams are usually less vivid, less emotional, and more logical than REM dreams. Most nightmares, however, occur during NREM sleep.
During rapid eye movement (REM) sleep, the eyes move rapidly back and forth under closed eyelids. REM sleep is also known as paradoxical sleep because electroencephalography (EEG) readings taken during this time show high-frequency, small amplitude waves, which are similar to those of a person who is awake. Surprisingly, neuronal activity is high during REM sleep—brain blood flow and oxygen use are actually higher during REM sleep than during intense mental or physical activity while awake!
In spite of this high amount of neuronal activity, it is even more difficult to awaken a person during REM sleep than during any of the stages of NREM sleep.
Rapid eye movement (REM) sleep is associated with several physiological changes. For example, heart rate, respiratory rate, and blood pressure increase during REM sleep. In addition, most somatic motor neurons are inhibited during REM sleep, which causes a significant decrease in muscle tone and even paralyzes the skeletal muscles. The main exceptions to this inhibition are those somatic motor neurons that govern breathing and eye movements. REM sleep is also the period when most dreaming occurs.
Brain imaging studies on people going through REM sleep reveal that there is increased activity in both the visual association area (which is involved in recognition of visual images) and limbic system (which plays a major role in generation of emotions) and decreased activity in the prefrontal cortex (which is concerned with reasoning). These studies help to explain why dreams during REM sleep are often full of vivid imagery, emotional responses, and situations that may be illogical or even bizarre. Erection of the penis and enlargement of the clitoris may also occur during REM sleep, even when dream content is not sexual. The presence of penile erections during REM sleep in a man with erectile dysfunction (inability to attain an erection while awake) indicates that his problem has a psychological, rather than a physical cause.
Intervals of NREM and REM sleep alternate throughout the night. Initially, a person falls asleep by sequentially going through the stages of NREM sleep (from stage 1 to stage 4) in about 45 minutes. Then the person goes through the stages of NREM sleep in reverse order (from stage 4 to stage 1) in about the same amount of time before entering a period of REM sleep. Afterward, the person again descends through the stages of NREM sleep, and then ascends back through the stages of NREM sleep to enter another period of REM sleep. During a typical 8-hour sleep period, there are four or five of these NREM-to-REM cycles. The first episode of REM sleep lasts 10–20 minutes. REM periods, which occur approximately every 90 minutes, gradually lengthen, with the final one lasting about 50 minutes. In adults, REM sleep totals 90–120 minutes during a typical 8-hour sleep period. As a person ages, the average total time spent sleeping decreases, and the percentage of REM sleep declines. As much as 50% of an infant’s sleep is REM sleep, as opposed to 35% for 2-year-olds and 25% for adults.
Figure 5. Sleep stages and brain activity – one sleep cycle
Figure 6. Sleep stages and brain activity – 8 hour sleep cycle
Although we do not yet understand the function of REM sleep, the high percentage of REM sleep in infants and children is thought to be important for the maturation of the brain.
Different parts of the brain mediate NREM and REM sleep. NREM sleep is induced by NREM sleep centers in the hypothalamus and basal forebrain, whereas REM sleep is promoted by a REM sleep center in the pons and midbrain. Several lines of evidence suggest the existence of sleep-inducing chemicals in the brain. One apparent sleep-inducer is adenosine, which accumulates during periods of high usage of ATP (adenosine triphosphate) by the nervous system. Adenosine inhibits neurons of the RAS that participate in arousal. Adenosine binds to specific receptors, called A1 receptors and inhibits certain cholinergic (acetylcholine-releasing) neurons of the RAS that participate in arousal. Thus, activity in the RAS during sleep is low due to the inhibitory effect of adenosine.
Caffeine (in coffee or chocolate) and theophylline (in tea)—substances known for their ability to maintain wakefulness—bind to and block the A1 receptors, preventing adenosine from binding and inducing sleep.
The Role of Genes and Neurotransmitters
Chemical signals to sleep
Clusters of sleep-promoting neurons in many parts of the brain become more active as we get ready for bed. Nerve-signaling chemicals called neurotransmitters can “switch off” or dampen the activity of cells that signal arousal or relaxation. GABA is associated with sleep, muscle relaxation, and sedation. Norepinephrine and orexin (also called hypocretin) keep some parts of the brain active while we are awake. Other neurotransmitters that shape sleep and wakefulness include acetylcholine, histamine, adrenaline, cortisol, and serotonin.
Genes and sleep
Genes may play a significant role in how much sleep we need. Scientists have identified several genes involved with sleep and sleep disorders, including genes that control the excitability of neurons, and “clock” genes such as Per, tim, and Cry that influence our circadian rhythms and the timing of sleep. Genome-wide association studies have identified sites on various chromosomes that increase our susceptibility to sleep disorders. Also, different genes have been identified with such sleep disorders as familial advanced sleep-phase disorder, narcolepsy, and restless legs syndrome. Some of the genes expressed in the cerebral cortex and other brain areas change their level of expression between sleep and wake. Several genetic models–including the worm, fruit fly, and zebrafish–are helping scientists to identify molecular mechanisms and genetic variants involved in normal sleep and sleep disorders. Additional research will provide better understand of inherited sleep patterns and risks of circadian and sleep disorders.
How Much Sleep Do You Need ?
The amount of sleep you need each day will change over the course of your life, your sleep patterns change as you age. Despite variations in sleep quantity and quality, both related to age and between individuals, studies suggest that the optimal amount of sleep needed to perform adequately, avoid a sleep debt, and not have problem sleepiness during the day is about 7–8 hours for adults and at least 10 hours for school-aged children and adolescents. Similar amounts seem to be necessary to avoid an increased risk of developing obesity, diabetes, or cardiovascular diseases.
Quality of sleep and the timing of sleep are as important as quantity. People whose sleep is frequently interrupted or cut short may not get enough of both non-REM sleep and REM sleep. Both types of sleep appear to be crucial for learning and memory—and perhaps for the restorative benefits of healthy sleep, including the growth and repair of cells.
The table below shows general recommendations for different age groups. This table reflects recent American Academy of Sleep Medicine recommendations that the American Academy of Pediatrics has endorsed.
Table 1. Recommended Amount of Sleep
| Age | Recommended Amount of Sleep |
|---|---|
| Infants aged 4-12 months | 12-16 hours a day (including naps) |
| Children aged 1-2 years | 11-14 hours a day (including naps) |
| Children aged 3-5 years | 10-13 hours a day (including naps) |
| Children aged 6-12 years | 9-12 hours a day |
| Teens aged 13-18 years | 8-10 hours a day |
| Adults aged 18 years or older | 7–8 hours a day |
Babies initially sleep as much as 16 to 18 hours per day, which may boost growth and development (especially of the brain). School-age children and teens on average need about 9.5 hours of sleep per night. Most adults need 7-9 hours of sleep a night, but after age 60, nighttime sleep tends to be shorter, lighter, and interrupted by multiple awakenings. Elderly people are also more likely to take medications that interfere with sleep.
For example, some older people complain of difficulty falling asleep, early morning awakenings, frequent and long awakenings during the night, daytime sleepiness, and a lack of refreshing sleep. Many sleep problems, however, are not a natural part of sleep in the elderly. Their sleep complaints may be due, in part, to medical conditions, illnesses, or medications they are taking—all of which can disrupt sleep. In fact, one study found that the prevalence of sleep problems is very low in healthy older adults. Other causes of some of older adults’ sleep complaints are sleep apnea, restless legs syndrome, and other sleep disorders that become more common with age. Also, older people are more likely to have their sleep disrupted by the need to urinate during the night.
There is no evidence that indicates older people can get by with less sleep than younger people. There is some evidence showing that the biological clock shifts in older people, so they are more apt to go to sleep earlier at night and wake up earlier in the morning. Poor sleep in older people may result in excessive daytime sleepiness, attention and memory problems, depressed mood, and overuse of sleeping pills.
Across the lifespan, the sleep period tends to advance, namely relative to teenagers; older adults tend to go to bed earlier and wake earlier. The quality—but not necessarily the quantity—of deep, NREM sleep also changes, with a trend toward lighter sleep. The relative percentages of stages of sleep appear to stay mostly constant after infancy. From midlife through late life, people awaken more throughout the night. These sleep disruptions cause older people to lose more and more of stages 1 and 2 non-REM sleep as well as REM sleep.
In general, people are getting less sleep than they need due to longer work hours and the availability of round-the-clock entertainment and other activities 9.
If you routinely lose sleep or choose to sleep less than needed, the sleep loss adds up. The total sleep lost is called your sleep debt. For example, if you lose 2 hours of sleep each night, you’ll have a sleep debt of 14 hours after a week. Many people feel they can “catch up” on missed sleep during the weekend but, depending on how sleep-deprived they are, sleeping longer on the weekends may not be adequate 9.
Some people nap as a way to deal with sleepiness. Naps may provide a short-term boost in alertness and performance. However, napping doesn’t provide all of the other benefits of night-time sleep. Thus, you can’t really make up for lost sleep.
Some people sleep more on their days off than on work days. They also may go to bed later and get up later on days off.
Sleeping more on days off might be a sign that you aren’t getting enough sleep. Although extra sleep on days off might help you feel better, it can upset your body’s sleep–wake rhythm.
Bad sleep habits and long-term sleep loss will affect your health. If you’re worried about whether you’re getting enough sleep, try using a sleep diary for a couple of weeks.
Sleeping when your body is ready to sleep also is very important. Sleep deficiency can affect people even when they sleep the total number of hours recommended for their age group.
For example, people whose sleep is out of sync with their body clocks (such as shift workers) or routinely interrupted (such as caregivers or emergency responders) might need to pay special attention to their sleep needs.
If your job or daily routine limits your ability to get enough sleep or sleep at the right times, talk with your doctor. You also should talk with your doctor if you sleep more than 8 hours a night, but don’t feel well rested. You may have a sleep disorder or other health problem.
Who Is at Risk for Sleep Deprivation and Deficiency ?
Sleep deficiency, which includes sleep deprivation, affects people of all ages, races, and ethnicities. Certain groups of people may be more likely to be sleep deficient. Examples include people who:
- Have limited time available for sleep, such as caregivers or people working long hours or more than one job
- Have schedules that conflict with their internal body clocks, such as shift workers, first responders, teens who have early school schedules, or people who must travel for work
- Make lifestyle choices that prevent them from getting enough sleep, such as taking medicine to stay awake, abusing alcohol or drugs, or not leaving enough time for sleep
- Have undiagnosed or untreated medical problems, such as stress, anxiety, or sleep disorders
- Have medical conditions or take medicines that interfere with sleep
Certain medical conditions have been linked to sleep disorders. These conditions include heart failure, heart disease, obesity, diabetes, high blood pressure, stroke or transient ischemic attack (mini-stroke), depression, and attention-deficit hyperactivity disorder (ADHD).
If you have or have had one of these conditions, ask your doctor whether you might benefit from a sleep study.
A sleep study allows your doctor to measure how much and how well you sleep. It also helps show whether you have sleep problems and how severe they are.
If you have a child who is overweight, talk with the doctor about your child’s sleep habits.
What Are the Signs and Symptoms of Problem Sleepiness ?
Sleep deficiency can cause you to feel very tired during the day. You may not feel refreshed and alert when you wake up. Sleep deficiency also can interfere with work, school, driving, and social functioning.
How sleepy you feel during the day can help you figure out whether you’re having symptoms of problem sleepiness. You might be sleep deficient if you often feel like you could doze off while:
- Sitting and reading or watching TV
- Sitting still in a public place, such as a movie theater, meeting, or classroom
- Riding in a car for an hour without stopping
- Sitting and talking to someone
- Sitting quietly after lunch
- Sitting in traffic for a few minutes
Sleep deficiency can cause problems with learning, focusing, and reacting. You may have trouble making decisions, solving problems, remembering things, controlling your emotions and behavior, and coping with change. You may take longer to finish tasks, have a slower reaction time, and make more mistakes.
The signs and symptoms of sleep deficiency may differ between children and adults. Children who are sleep deficient might be overly active and have problems paying attention. They also might misbehave, and their school performance can suffer.
Sleep-deficient children may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation.
You may not notice how sleep deficiency affects your daily routine. A common myth is that people can learn to get by on little sleep with no negative effects. However, research shows that getting enough quality sleep at the right times is vital for mental health, physical health, quality of life, and safety.
To find out whether you’re sleep deficient, try keeping a sleep diary for a couple of weeks. Write down how much you sleep each night, how alert and rested you feel in the morning, and how sleepy you feel during the day.
Compare the amount of time you sleep each day with the average amount of sleep recommended for your age group, as shown in Table 1. Recommended Amount of Sleep (see above).
Many people try to make up for lost sleep during the week by sleeping more on the weekends. But if you have lost too much sleep, sleeping in on a weekend does not completely erase your sleep debt. Certainly, sleeping more at the end of a week won’t make up for any poor performance you had earlier in that week. Just one night of inadequate sleep can negatively affect your functioning and mood during at least the next day.
Daytime naps are another strategy some people use to make up for lost sleep during the night. Some evidence shows that short naps (up to an hour) can make up, at least partially, for the sleep missed on the previous night and improve alertness,mood, and work performance. But naps don’t substitute for a good night’s sleep. One study found that a daytime nap after a lack of sleep at night did not fully restore levels of blood sugar to the pattern seen with adequate nighttime sleep. If a nap lasts longer than 20 minutes, you may have a hard time waking up fully. In addition, late afternoon naps can make falling asleep at night more difficult.
If you often feel very sleepy, and efforts to increase your sleep don’t help, see your doctor.
How to get better sleep at night
You can take steps to improve your sleep habits. First, make sure that you allow yourself enough time to sleep. With enough sleep each night, you may find that you’re happier and more productive during the day.
Sleep often is the first thing that busy people squeeze out of their schedules. Making time to sleep will help you protect your health and well-being now and in the future.
Getting enough sleep is good for your health. Here are a few tips to improve your sleep:
- Set a schedule. Go to bed and wake up at the same time every day. For children, have a set bedtime and a bedtime routine. Don’t use the child’s bedroom for timeouts or punishment.
- Try to keep the same sleep schedule on weeknights and weekends. Limit the difference to no more than about an hour. Staying up late and sleeping in late on weekends can disrupt your body clock’s sleep–wake rhythm.
- Use the hour before bed for quiet time. Avoid strenuous exercise and bright artificial light, such as from a TV or computer screen. The light may signal the brain that it’s time to be awake.
- Create a room for sleep – avoid bright lights and loud sounds, keep the room at a comfortable temperature, and don’t watch TV or have a computer in your bedroom.
- Avoid nicotine (for example, cigarettes) and caffeine (including caffeinated soda, coffee, tea, and chocolate). Nicotine and caffeine are stimulants, and both substances can interfere with sleep. The effects of caffeine can last as long as 8 hours. So, a cup of coffee in the late afternoon can make it hard for you to fall asleep at night.
- Avoid heavy and/or large meals within a couple hours of bedtime. (Having a light snack is okay.) Also, avoid alcoholic drinks before bed.
- Exercise 20 to 30 minutes a day but no later than a few hours before going to bed.
- Relax before bed – try a warm bath, reading, or another relaxing routine.
- Don’t lie in bed awake. If you can’t get to sleep, do something else, like reading or listening to music, until you feel tired.
- Spend time outside every day (when possible) and be physically active.
- Keep your bedroom quiet, cool, and dark (a dim night light is fine, if needed).
Napping during the day may provide a boost in alertness and performance. However, if you have trouble falling asleep at night, limit naps or take them earlier in the afternoon. Adults should nap for no more than 20 minutes.
Napping in preschool-aged children is normal and promotes healthy growth and development.
See a doctor if you have a problem sleeping or if you feel unusually tired during the day. Most sleep disorders can be treated effectively.
How to Sleep Better if You Are a Shift Worker
Some people have schedules that conflict with their internal body clocks. For example, shift workers and teens who have early school schedules may have trouble getting enough sleep. This can affect how they feel mentally, physically, and emotionally.
If you’re a shift worker, you may find it helpful to:
- Increase your total amount of sleep by adding naps and lengthening the amount of time you allot for sleep.
- Keep the lights bright at work
- Minimize the number of shift changes so that your body’s biological clock has a longer time to adjust to a nighttime work schedule.
- Limit caffeine use to the first part of your shift to promote alertness at night.
- Remove sound and light distractions in your bedroom during daytime sleep (for example, use light-blocking curtains)
If you’re still not able to fall asleep during the day or have problems adapting to a shift-work schedule, talk with your doctor about other options to help you sleep.
When possible, employers and schools might find it helpful to consider options to address issues related to sleep deficiency.
Here are some potentially life-saving tips for avoiding drowsy driving
- Be well rested before hitting the road. If you have several nights in a row of fewer than 7–8 hours of sleep, your reaction time slows. Restoring that reaction time to normal can take more than one night of good sleep, because a sleep debt accumulates after each night you lose sleep. It may take several nights of being well rested to repay that sleep debt and make you ready for driving on a long road trip.
- Avoid driving between midnight and 7 a.m. Unless you are accustomed to being awake then, this period of time is when we are naturally the least alert and most tired.
- Don’t drive alone. A companion who can keep you engaged in conversation might help you stay awake while driving.
- Schedule frequent breaks on long road trips. If you feel sleepy while driving, pull off the road and take a nap for 15–20 minutes.
- Don’t drink alcohol. Just one beer when you are sleep deprived will affect you as much as two or three beers when you are well rested.
- Don’t count on caffeine or other tricks. Although drinking a cola or a cup of coffee might help keep you awake for a short time, it won’t over come extreme sleepiness or relieve a sleep debt.
Top 10 Sleep Myths
- Myth 1: Sleep is a time when your body and brain shut down for rest and relaxation.
No evidence shows that any major organ (including the brain) or regulatory system in the body shuts down during sleep. Some physiological processes actually become more active while you sleep. For example, secretion of certain hormones is boosted, and activity of the pathways in the brain linked to learning and memory increases.
- Myth 2: Getting just 1 hour less sleep per night than needed will not have any effect on your daytime functioning.
This lack of sleep may not make you noticeably sleepy during the day. But even slightly less sleep can affect your ability to think properly and respond quickly, and it can impair your cardiovascular health and energy balance as well as your body’s ability to fight infections, particularly if lack of sleep continues. If you consistently do not get enough sleep, a sleep debt builds up that you can never repay. This sleep debt affects your health and quality of life and makes you feel tired during the day.
- Myth 3: Your body adjusts quickly to different sleep schedules.
Your biological clock makes you most alert during the daytime and least alert at night. Thus, even if you work the night shift, you will naturally feel sleepy when nighttime comes. Most people can reset their biological clock, but only by appropriately timed cues—and even then, by 1–2 hours per day at best. Consequently, it can take more than a week to adjust to a substantial change in your sleep–wake cycle—for example, when traveling across several time zones or switching from working the day shift to the night shift.
- Myth 4: People need less sleep as they get older.
Older people don’t need less sleep, but they may get less sleep or find their sleep less refreshing. That’s because as people age, the quality of their sleep changes. Older people are also more likely to have insomnia or other medical conditions that disrupt their sleep.
- Myth 5: Extra sleep for one night can cure you of problems with excessive daytime fatigue.
Not only is the quantity of sleep important, but also the quality of sleep. Some people sleep 8 or 9 hours a night but don’t feel well rested when they wake up because the quality of their sleep is poor. A number of sleep disorders and other medical conditions affect the quality of sleep. Sleeping more won’t lessen the daytime sleepiness these disorders or conditions cause. However, many of these disorders or conditions can be treated effectively with changes in behavior or with medical therapies. Additionally, one night of increased sleep may not correct multiple nights of inadequate sleep.
- Myth 6: You can make up for lost sleep during the week by sleeping more on the weekends.
Although this sleeping pattern will help you feel more rested, it will not completely make up for the lack of sleep or correct your sleep debt. This pattern also will not necessarily make up for impaired performance during the week or the physical problems that can result from not sleeping enough. Furthermore, sleeping later on the weekends can affect your biological clock, making it much harder to go to sleep at the right time on Sunday nights and get up early on Monday mornings.
- Myth 7: Naps are a waste of time.
Although naps are no substitute for a good night’s sleep, they can be restorative and help counter some of the effects of not getting enough sleep at night. Naps can actually help you learn how to do certain tasks quicker. But avoid taking naps later than 3 p.m., particularly if you have trouble falling asleep at night, as late naps can make it harder for you to fall asleep when you go to bed. Also, limit your naps to no longer than 20 minutes, because longer naps will make it harder to wake up and get back in the swing of things. If you take more than one or two planned or unplanned naps during the day, you may have a sleep disorder that should be treated.
- Myth 8: Snoring is a normal part of sleep.
Snoring during sleep is common, particularly as a person gets older. Evidence is growing that snoring on a regular basis can make you sleepy during the day and increase your risk for diabetes and heart disease. In addition, some studies link frequent snoring to problem behavior and poorer school achievement in children. Loud, frequent snoring also can be a sign of sleep apnea, a serious sleep disorder that should be evaluated and treated.
- Myth 9: Children who don’t get enough sleep at night will show signs of sleepiness during the day.
Unlike adults, children who don’t get enough sleep at night typically become hyperactive, irritable, and inattentive during the day. They also have increased risk of injury and more behavior problems, and their growth rate may be impaired. Sleep debt appears to be quite common during childhood and may be misdiagnosed as attention-deficit hyperactivity disorder.
- Myth 10: The main cause of insomnia is worry.
Although worry or stress can cause a short bout of insomnia, a persistent inability to fall asleep or stay asleep at night can be caused by a number of other factors. Certain medications and sleep disorders can keep you up at night. Other common causes of insomnia are depression, anxiety disorders, and asthma, arthritis, or other medical conditions with symptoms that tend to be troublesome at night. Some people who have chronic insomnia also appear to be more “revved up” than normal, so it is harder for them to fall asleep.
- Brinkman JE, Sharma S. Physiology, Sleep. [Updated 2018 Dec 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482512[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Why Is Sleep Important ? National Heart, Lung and Blood Institute. https://www.nhlbi.nih.gov/health/health-topics/topics/sdd/why[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Patel AK, Araujo JF. Physiology, Sleep Stages. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526132[↩][↩]
- Zajac A, Skowronek-Bała B, Wesołowska E, Kaciński M. [Sleep paroxysmal events in children in video/polysomnography]. Prz. Lek. 2010;67(9):762-9[↩]
- Malik J, Lo YL, Wu HT. Sleep-wake classification via quantifying heart rate variability by convolutional neural network. Physiol Meas. 2018 Aug 20;39(8):085004.[↩]
- Memar P, Faradji F. A Novel Multi-Class EEG-Based Sleep Stage Classification System. IEEE Trans Neural Syst Rehabil Eng. 2018 Jan;26(1):84-95.[↩]
- Varga B, Gergely A, Galambos Á, Kis A. Heart Rate and Heart Rate Variability during Sleep in Family Dogs (Canis familiaris). Moderate Effect of Pre-Sleep Emotions. Animals (Basel). 2018 Jul 02;8, 7[↩]
- Della Monica C, Johnsen S, Atzori G, Groeger JA, Dijk DJ. Rapid Eye Movement Sleep, Sleep Continuity and Slow Wave Sleep as Predictors of Cognition, Mood, and Subjective Sleep Quality in Healthy Men and Women, Aged 20-84 Years. Front Psychiatry. 2018;9:255.[↩]
- Brain Basics: Understanding Sleep. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep[↩][↩]