Contents
- What is hydatidiform mole pregnancy
What is hydatidiform mole pregnancy
Hydatidiform mole also called molar pregnancy is a rare growth or mass that forms inside the womb (uterus) at the beginning of a pregnancy 1, 2. Hydatidiform mole is a rare complication of pregnancy. Hydatidiform mole is one of the most common complications of gestational trophoblastic diseases (cells that help an embryo attach to the uterus and help form the placenta) 3, 4, 5. The incidence of hydatidiform moles varies in different ethnic groups, with an estimated incidence of 2.43 to 13 per 1000 pregnancies in Asians and 0.5 to 1.84 per 1000 pregnancies in Caucasians 6, 7, 8, 9. Women from 21 to 35 years of age have a lower risk of complete hydatidiform mole than women older than 35 years and younger than 21 years 10. Women with a history of prior spontaneous miscarriage have a two- to three-fold risk of molar pregnancy in comparison with the general population 11. Furthermore, women with previous hydatidiform mole have a 10- to 20-fold risk of developing a second hydatidiform mole in the next pregnancy 12.
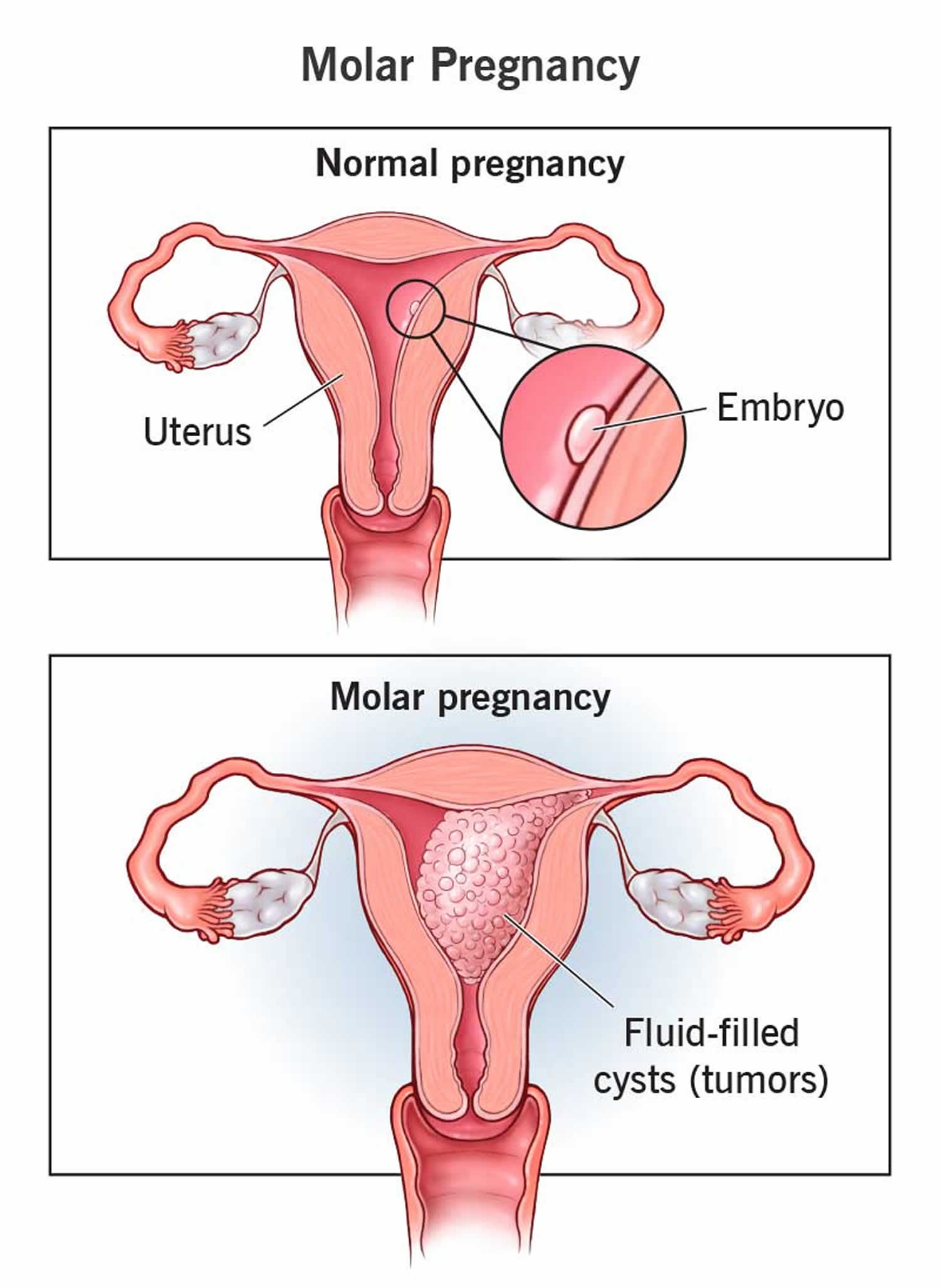
Hydatidiform mole pregnancy can be of two types. The absence or presence of a fetus or embryo is used to distinguish the complete from partial moles 13, 14:
- Partial molar pregnancy: There is an abnormal placenta where the placenta might have both regular and irregular tissue and some fetal development, but the fetus can’t survive. The fetus usually is miscarried early in the pregnancy.
- Complete molar pregnancy: There is an abnormal placenta where the placental tissue swells and appears to form fluid-filled cysts and no fetus.
A hydatidiform mole pregnancy or molar pregnancy may not have any symptoms or you may have some symptoms of pregnancy. You may find out about a hydatidiform mole pregnancy during your first pregnancy ultrasound scan at around 8 to 14 weeks. Some people find out after their pregnancy ends with a miscarriage.
Some people don’t have any symptoms of a molar pregnancy. For those who do, the most common include:
- Vaginal bleeding within the first three months of pregnancy.
- Severe nausea and vomiting.
- Grape-like cysts coming out of your vagina.
- Preeclampsia (extremely high blood pressure).
- Abnormally high human chorionic gonadotropin (HCG or hCG) hormone levels.
- Abdominal swelling.
- Anemia.
These symptoms are similar to many other conditions. It’s best to report any unusual symptoms to your doctor.
Although more than 80% of hydatidiform mole has spontaneous remission, 10 to 15% of cases may develop into invasive moles and 2 to 3% of cases may develop into a rare form of cancer called choriocarcinoma 15. Choriocarcinoma also called chorionic carcinoma, chorioblastoma or chorioepithelioma is a fast-growing cancer that develops from trophoblastic cells. Almost all choriocarcinomas form in the uterus after fertilization of an egg by a sperm, but a small number form in a testis or an ovary. Choriocarcinomas spread through the blood to other organs, especially the lungs. Therefore, hydatidiform mole needs to be closely followed up in clinical practice and requires early treatment. About 20% of patients will develop malignant transformation after evacuation of hydatidiform mole 16.
Figure 1. Hydatidiform mole pregnancy
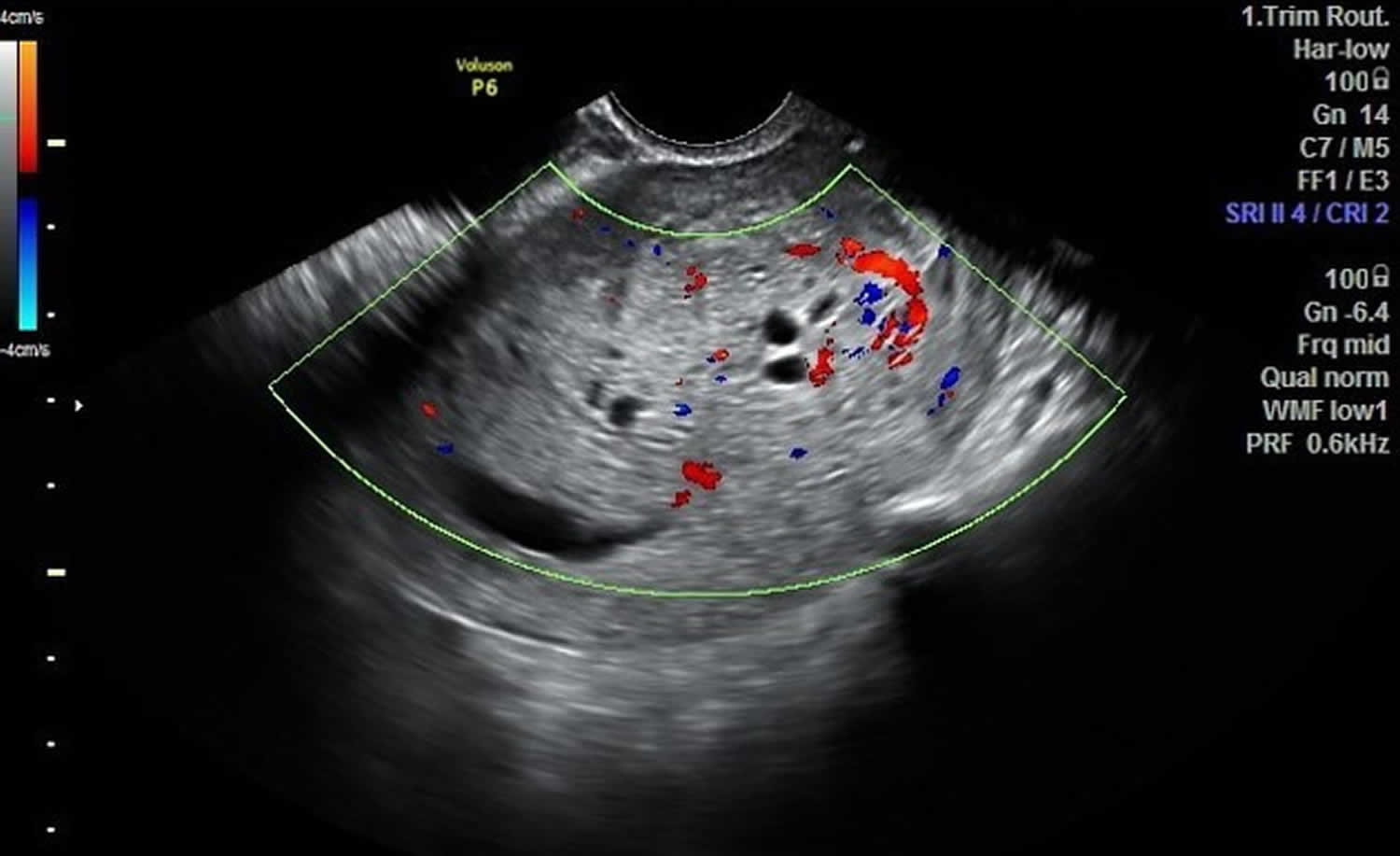
Figure 2. Partial hydatidiform mole pregnancy
Footnote: Pregnant uterus with large irregular gestational sac containing small non viable embryo. There is evident discrepancy between the size of sac and that of the embryo. The placenta is thickened, hyperreflective with multiple small cystic spaces inside and increased internal vascularity on Doppler scan.
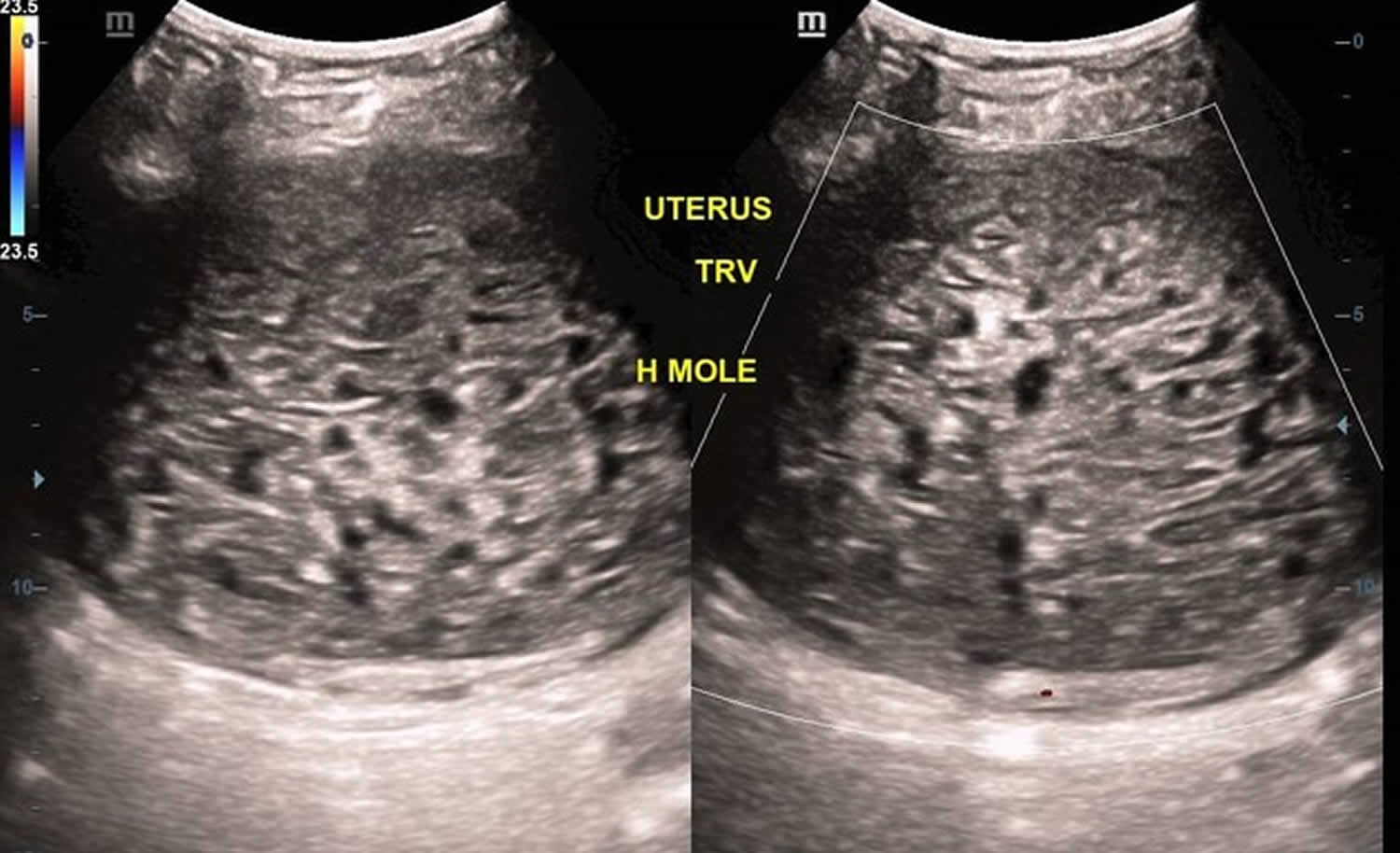
[Source 17 ]Figure 3. Complete hydatidiform mole pregnancy
Footnote: A bulky anteverted uterus with a volumetric quantity of 1105.5 ml demonstrating a large amount of heterogeneous luminal material with characteristic honey-comb appearance composed of echogenic solid areas and non-vascular multi-focal cystic vesicles. The endometrial-myometrial interface is obliterated with resultant infiltration of the myometrial parenchyma. Both ovaries shows small sized luteal follicles however, with no gross enlargement as yet.
[Source 18 ]Figure 4. Hydatidiform mole and live fetus
Footnote: (a-c) Hydatidiform mole. (d) Live fetus
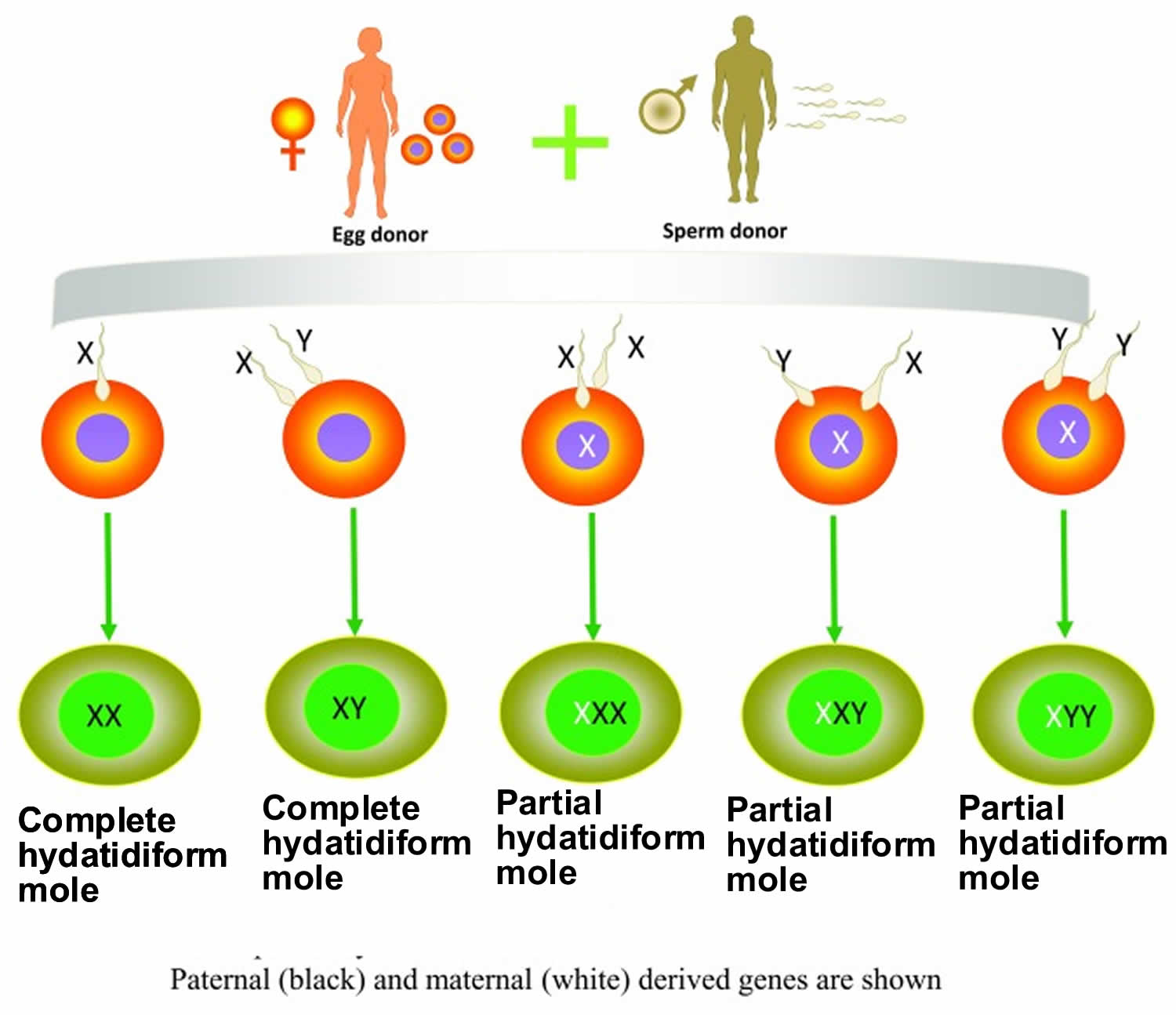
[Source 19Figure 5. Complete and partial hydatidiform moles genetics
Footnote: Complete and partial hydatidiform moles complete set of chromosomes or karyotypes
[Source 20)) ]See your doctor immediately when you’re pregnant and:
- you have any bleeding or a dark discharge from your vagina
- you’re feeling or being sick often (severe morning sickness)
- you think your bump looks bigger than it should for your stage of pregnancy
- you’re passing grape-like cysts from your vagina
- you have any other symptoms you’re worried about.
Prompt evaluation and treatment are necessary to prevent complications.
Can a hydatidiform mole pregnancy lead to a normal pregnancy?
No. A hydatidiform mole pregnancy results in the loss of the pregnancy. 10 to 15% of molar pregnancy cases may develop into invasive moles and 2 to 3% of cases may develop into a rare form of cancer called choriocarcinoma 15. Choriocarcinoma also called chorionic carcinoma, chorioblastoma or chorioepithelioma is a fast-growing cancer that develops from trophoblastic cells. Almost all choriocarcinomas form in the uterus after fertilization of an egg by a sperm, but a small number form in a testis or an ovary. Choriocarcinomas spread through the blood to other organs, especially the lungs. Therefore, hydatidiform mole needs to be closely followed up in clinical practice and requires early treatment.
It’s normal to have questions about what went wrong and to be fearful about future pregnancies. Talk to your healthcare provider about your concerns, ask them any questions you have and let your family and friends support you during this time. Most people go on to have healthy pregnancies.
Is a hydatidiform mole pregnancy a type of miscarriage?
A hydatidiform mole pregnancy usually results in the loss of the pregnancy. It’s normal to be disappointed and sad that you aren’t pregnant. Take time to grieve the loss. Look for support from your family, friends or support groups that deal with losing a pregnancy. If you’ve had a hydatidiform mole pregnancy in the past, you’re likely to have a healthy pregnancy in the future.
Does a hydatidiform mole pregnancy cause infertility?
No, hydatidiform mole pregnancy doesn’t cause infertility. However, you should avoid becoming pregnant for up to 12 months. This allows your human chorionic gonadotropin (hCG or HCG) hormone levels to return to prepregnancy levels. Ask your pregnancy care provider about when you can begin trying for another pregnancy.
How is a hydatidiform mole pregnancy diagnosed?
Your doctor diagnose a hydatidiform mole pregnancy during routine prenatal tests usually in the first trimester. An ultrasound of your uterus often shows several fluid-filled sacs instead of a placenta. There’s usually no embryo or fetus in your uterus, but sometimes pregnancy tissue remains.
Your doctor can also measure human chorionic gonadotropin (hCG or HCG) hormone levels in your blood. A healthy placenta produces human chorionic gonadotropin (hCG or HCG) hormone during pregnancy. It’s the hormone that at-home pregnancy tests measure in your urine (pee) to confirm a pregnancy. In molar pregnancies, HCG is produced at abnormally high levels. A blood test can detect these high levels and suggest a molar pregnancy has occurred.
Some people won’t have any symptoms of a molar pregnancy, and the diagnosis can be quite shocking. Just know that you did nothing to cause a molar pregnancy. In most cases, you can subsequently become pregnant with a healthy pregnancy if you chose to.
Hydatidiform mole types
Hydatidiform mole pregnancies fall into two categories: complete and partial. The absence or presence of a fetus or embryo is used to distinguish the complete from partial moles. The ratio of partial to complete hydatidiform mole is approximately 1.5 to 1.8.
Rarely, hydatidiform mole co-exist with a normal pregnancy (co-existent molar pregnancy), in which a normal fetus and placenta are seen separate from the molar gestation (see Figure 4).
Complete hydatidiform mole pregnancy
In complete hydatidiform mole pregnancies, no embryo forms. It happens when a sperm fertilizes an empty egg that does not contain the mother’s DNA. Approximately 90% of complete hydatidiform moles have a 46XX diploid chromosomal pattern with ~10% having a 46XY composition 10, 21, 22, 23, 24, 25, 26. All the chromosomes are derived from the sperm, suggesting fertilization of a single egg that has lost its chromosomes.
Because the egg is empty, the embryo can’t grow. The placental tissue grows but is abnormal and contains fluid-filled cysts (or tumors). This tissue produces the pregnancy human chorionic gonadotropin (HCG or hCG) hormone, which is made by a healthy placenta during pregnancy. This can make you feel like you’re pregnant and give you a positive pregnancy test.
Partial hydatidiform mole pregnancy
A partial hydatidiform mole pregnancy occurs when an abnormal placenta forms along with an embryo, and two sperm fertilize one egg. A partial hydatidiform mole forms when two sperms fertilize a normal egg and there are two sets of DNA from the father in the fertilized egg. In these cases, the growing embryo has an extra set of chromosomes (70% are 69 XXY, 27% are 69 XXX, and 3% are 69 XYY) 10, 21, 22, 23, 24, 25, 26. The embryo may start to develop but generally can’t survive and the cells that were meant to become the placenta are abnormal.
Hydatidiform mole pregnancy causes
Hydatidiform mole pregnancy is caused by genetic errors that occur during the fertilization of an egg (oocyte) by a sperm 27, 28, 29. Human cells usually have 23 pairs of chromosomes for a total of 46 chromosomes. In a typical fertilization and normal pregnancy, one set of chromosomes (23) comes from the father, the other from the mother for a total of 46 chromosomes (23 pairs of chromosomes). Chromosomes are structures that contain genes. Genes tell your body how to work.
- In a complete molar pregnancy, one or two sperm fertilize an egg. The chromosomes from the mother’s egg are missing or don’t work. The father’s chromosomes are copied. There’s none from the mother. Ninety percent of complete hydatidiform moles have a 46XX diploid chromosomal pattern. All the chromosomes are derived from a single sperm in 90% or less likely two sperms, suggesting fertilization of a single egg that has lost its chromosomes.
- In a partial or incomplete molar pregnancy, the mother’s chromosomes are present, but the father supplies two sets of chromosomes. The embryo then has 69 chromosomes known as triploid (69XXY) instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father’s genes, one bearing a 23X chromosomal pattern and the other a 23Y chromosomal pattern.
This genetic error leads to an unsuccessful pregnancy. Hydatidiform mole results in an abnormal fetus. The placenta grows normally with little or no growth of the fetal tissue. The placental tissue forms a mass in the uterus. On ultrasound, this mass often has a grape-like appearance, as it contains many small cysts. The chance of mole formation is higher in older women. A history of mole in earlier years is also a risk factor.
Risk factors for developing hydatidiform mole pregnancy
Although hydatidiform mole pregnancies are rare, anyone can have a molar pregnancy. You’re more likely to have a hydatidiform mole pregnancy if you:
- Have a history of molar pregnancy. If you’ve had one molar pregnancy, you’re more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 people.
- Age of the mother. A molar pregnancy is more likely in people older than age 40 or younger than age 15.
- Have had two or more miscarriages.
- Are of Asian descent.
- Dietary factors including patients that have diets deficient in carotene (vitamin A precursor) and animal fats
- Smoking
Hydatidiform mole pathophysiology
Hydatidiform mole pregnancy is caused by genetic errors that occur during the fertilization of an egg (oocyte) by a sperm 27, 28, 29. Several studies reveal a severe vasculogenic deficit in trophoblastic diseases, with significantly retarded angiogenesis in early complete mole, progressive accumulation of fluids, and subsequent formation of cystic spaces (“cistern”) 30, 31, 32, 33, 34. In complete hydatidiform moles an enucleated egg is fertilized either by two sperm or, more commonly, monospermic arising from a haploid sperm which endoreduplicates, resulting in only paternal DNA being expressed; this aberration lacks mitochondria, as mitochondrial DNA is maternally derived. Conversely, in a partial hydatiform mole, a haploid ovum either duplicates and fertilized by normal sperm, or a haploid ovum is fertilized by two sperm, resulting in both the expression of both maternal and paternal DNA 35. In brief, complete hydatidiform moles are diploid (46,XX; 46,XY) while most partial hydatidiform moles are triploid (69,XXY; XXX; XYY). Triploid or tetraploid complete moles are androgenetic (since they lack maternal chromosomes) while tetraploid partial moles have maternal contributions. Hydatiform mole is characterized by chromosomal abnormalities, which allow for malignant transformation in choriocarcinoma. The most common alteration leading to malignant transformation are the activation of oncogenes, inactivation of tumor suppressors, and the alteration of telomerase regulation 1.
Hydatidiform mole pregnancy prevention
There’s no way to prevent a hydatidiform mole pregnancy. If you’ve had a hydatidiform mole pregnancy, talk to your pregnancy care provider before trying to get pregnant again. You might want to wait six months to one year after your initial molar pregnancy. The risk of having another molar pregnancy is low, but it’s higher once you’ve had a molar pregnancy.
During future pregnancies, your doctor may do early ultrasounds to check your condition and make sure the baby is developing.
Hydatidiform mole signs and symptoms
A hydatidiform mole pregnancy may seem like a regular pregnancy at first. But most molar pregnancies cause symptoms that can include:
- Abnormal growth of your uterus (womb), either bigger or smaller than usual
- Dark brown to bright red bleeding from your vagina during the first 3 months of pregnancy
- Severe nausea and vomiting
- Sometimes grapelike cysts that pass from the vagina
- Pelvic pressure or pain
Because of improved ways of detecting a molar pregnancy, most are found in the first trimester.
If it is not found in the first three months, symptoms of a hydatidiform mole might include:
- A uterus growing quickly and being too large early in the pregnancy
- Symptoms similar to preeclampsia that occur in the first trimester or early second trimester (before 20 weeks of pregnancy) — a condition that causes high blood pressure and protein in the urine and swelling in the feet, ankles, and legs (this is almost always a sign of a hydatidiform mole, because preeclampsia is extremely rare this early in a normal pregnancy)
- Ovarian cysts
- Overactive thyroid also known as hyperthyroidism. Symptoms of overactive thyroid (hyperthyroidism), including heat intolerance, loose stools, rapid heart rate, restlessness or nervousness, warm and moist skin, trembling hands, or unexplained weight loss.
Hydatidiform mole complications
After removing a molar pregnancy, parts of the molar tissue might remain and continue to grow. This is called persistent gestational trophoblastic neoplasia. Gestational trophoblastic neoplasia happens more often in complete molar pregnancies than it does in partial molar pregnancies. If this happens, abnormal cells may grow into the muscle layer around your uterus (also called an invasive mole). This is rare and happens in less than 15% of people who’ve had a molar pregnancy removed.
One sign of persistent gestational trophoblastic neoplasia is a high level of human chorionic gonadotropin (hCG or HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, the mole that causes the molar pregnancy goes deep into the middle layer of the uterine wall. This causes bleeding from the vagina.
Persistent gestational trophoblastic neoplasia is usually treated with chemotherapy. Another treatment possibility is surgical removal of the uterus also known as hysterectomy.
In very rare cases, a cancerous form of gestational trophoblastic neoplasia known as choriocarcinoma develops and spreads to other parts of your body. Choriocarcinoma is usually successfully treated with chemotherapy or radiation. A complete molar pregnancy is more likely to have this complication than is a partial molar pregnancy.
Other potential complications of a hydatidiform mole pregnancy include:
- Infection of the blood (sepsis).
- Uterine infection.
- Preeclampsia (very high blood pressure).
- Shock (very low blood pressure).
Hydatidiform mole diagnosis
Your doctor who suspects a hydatidiform mole pregnancy is likely to order blood tests and an ultrasound. During early pregnancy, an transvaginal ultrasound where you lie on an exam table while a doctor or a medical technician puts a wandlike device, known as a transducer, into your vagina. Sound waves from the transducer create images of the uterus, ovaries and fallopian tubes.
Complete hydatidiform moles usually occupy the uterine cavity and are rarely located in fallopian tubes or ovaries. The chorionic villi are converted into a mass of clear vesicles that resemble a cluster of grapes.
As early as eight or nine weeks of pregnancy, an ultrasound of a complete molar pregnancy might show:
- No embryo or fetus
- No amniotic fluid
- A thick cystic placenta nearly filling the uterus
- Ovarian cysts
An ultrasound of a partial molar pregnancy might show:
- A fetus that’s smaller than expected
- Low amniotic fluid
- Placenta that appears unusual
MRI can be used to determine if there is an extension of molar tissue outside the uterus.
After finding a molar pregnancy, your doctor might check for other medical issues, including:
- Preeclampsia
- Hyperthyroidism (overactive thyroid)
- Anemia (low red blood cells)
Hydatidiform mole histopathology
Hydatiform mole is characterized by an overgrown villous trophoblast with cystic “swollen” villi 1. Macroscopically can be visible, the second trimester, as clusters of vesicles (similar to small grapes) developed from the transformation of chorionic villi. Complete mole differs from partial mole, in cytogenetic and microscopical appearance. Important is a complete lack of embryonic/fetal tissue in complete moles and the presence of-of embryonic tissue in partial moles.
Microscopically, a complete hydatidiform mole has markedly hydropic and deformed chorionic villi with the formation of “cisterns” containing stromal fluid; there is a peripheral proliferation of both cytotrophoblast and syncytiotrophoblast, arranged in lace-like structures, papillary formation, or circumferential 1. In normal early placenta the cytotrophoblast and syncytiotrophoblast are polarized 1. There is the absence of fetal stromal blood vessels 1. An immature vascular network is otherwise present, positive for CD31, with dysmorphic features such as a complete lack of lumen 1. In partial hydatidiform mole there are hydropic chorionic villi surrounded by hyperplastic trophoblasts with variable degrees of central cistern formation, with an irregular maze-like pattern; also, there are normal chorionic villi and embryonic or fetal tissue mixed with hydropic villi. There are recognizable fetal blood vessels containing fetal red blood cells. The curettage material should be examined carefully, especially in first trimester pregnancies, and if a partial mole is suspected the whole specimen should be examined. The main differential diagnosis is with a hydropic abortion, where the main clue is the presence of villous edema only with microscopical evaluation and lacks cistern formation or trophoblastic proliferation. A pitfall in hydropic abortion is the presence of polar stratification of anchoring trophoblast in a first-trimester placenta. The villous size in hydropic abortion ranges from small, to medium and large.
An important marker that aids in the diagnosis of the complete hydatidiform mole is the presence or absence of p57 in immunohistochemistry. This marker is a paternal-imprint inhibitor gene so its expression implies the maternal contribution; in brief, the absence of p57 expression supports the diagnosis of androgenetic gestational disease with complete hydatidiform mole 36, 37, 38. Hydatidiform moles also express p53, p21, cyclin E, and MCM7 1.
Hydatidiform mole treatment
Because of the risk of complications such as persistent gestational trophoblastic neoplasia or choriocarcinoma, a hydatidiform mole pregnancy can’t be allowed to continue. To prevent complications, the affected placental tissue must be removed. Treatment usually consists of one or more of the following steps:
- Dilation and curettage (D&C). This procedure removes the molar tissue from the uterus. You lie on a table on your back with your legs in stirrups. You’ll receive general anesthesia to put you to sleep. After opening the cervix, your doctor removes uterine tissue with a suction device. A D&C for a molar pregnancy usually is done in a hospital or surgery center.
- In some cases, medication to help your uterus contract and expel the contents of your uterus is used instead of D&C. Talk to your healthcare provider about the best treatment option for you as urgent treatment is recommended for molar pregnancies to help prevent complications.
- Surgical removal of the uterus (hysterectomy). This occurs rarely if there’s increased risk of gestational trophoblastic neoplasia (GTN) and there’s no desire for future pregnancies.
- Human chorionic gonadotropin (HCG or hCG) monitoring. After the molar tissue is removed, your doctor keeps measuring the human chorionic gonadotropin (hCG or HCG) hormone level until it goes down. A continuing high level of human chorionic gonadotropin (hCG or HCG) hormone in the blood might require more treatment. After treatment for the molar pregnancy is complete, your doctor might check HCG levels for six months to make sure no molar tissue is left. For people with gestational trophoblastic neoplasia (GTN), HCG levels are checked for one year after chemotherapy is completed. Because pregnancy HCG levels also increase during a regular pregnancy, your doctor might recommend that you wait 6 to 12 months before trying to become pregnant again. Your doctor can recommend a reliable form of birth control during this time.
Hydatidiform mole prognosis
Although hydatiform moles are usually considered benign, they are premalignant and do have the potential to become malignant and invasive 39, 40, 16. Most people who receive treatment for a hydatidiform mole pregnancy have no further complications. If you have a hydatidiform mole pregnancy, your risk for miscarriage doesn’t increase. You’re only at a slightly higher risk of a second molar pregnancy.
Some people find it helpful to seek genetic counseling before conceiving again. There aren’t any indications that a hydatidiform mole pregnancy should affect your decision to try to conceive again if you wish to do so.
- Ghassemzadeh S, Farci F, Kang M. Hydatidiform Mole. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459155[↩][↩][↩][↩][↩][↩][↩][↩]
- Richardson MV, Hertig AT. New England’s first recorded hydatidiform mole; a historical note. N Engl J Med. 1959;260(11):544–545. doi: 10.1056/NEJM195903122601107[↩]
- Leenharattanarak P, Lertkhachonsuk R: Quality of life in gestational trophoblastic neoplasia patients after treatment in Thailand. Asian Pac J Cancer Prev. 2015;15(24):10871–4. 10.7314/APJCP.2014.15.24.10871[↩]
- Nadhan R, Vaman JV, C N, et al.: Insights into dovetailing GTD and Cancers. Crit Rev Oncol Hematol. 2017;114:77–90. 10.1016/j.critrevonc.2017.04.001[↩]
- Berkowitz RS, Goldstein DP. Current management of gestational trophoblastic diseases. Gynecol Oncol. 2009;112(3):654–662. doi: 10.1016/j.ygyno.2008.09.005[↩]
- Altieri A, Franceschi S, Ferlay J, et al.: Epidemiology and aetiology of gestational trophoblastic diseases. Lancet Oncol. 2003;4(11):670–8. 10.1016/S1470-2045(03)01245-2[↩]
- Newlands ES, Paradinas FJ, Fisher RA: Recent advances in gestational trophoblastic disease. Hematol Oncol Clin North Am. 1999;13(1):225–44, x. 10.1016/S0889-8588(05)70162-3[↩]
- Jacobs PA, Hunt PA, Matsuura JS, Wilson CC, Szulman AE. Complete and partial hydatidiform mole in Hawaii: cytogenetics, morphology and epidemiology. Br J Obstet Gynaecol. 1982;89(4):258–266. doi: 10.1111/j.1471-0528.1982.tb04693.x[↩]
- Hui P, Buza N, Murphy KM, Ronnett BM. Hydatidiform moles: genetic basis and precision diagnosis. Annu Rev Pathol. 2017;12:449–485. doi: 10.1146/annurev-pathol-052016-100237[↩]
- Seckl MJ, Sebire NJ, Berkowitz RS: Gestational trophoblastic disease. Lancet. 2010;376(9742):717–29. 10.1016/S0140-6736(10)60280-2[↩][↩][↩]
- Parazzini F, Mangili G, La Vecchia C, et al.: Risk factors for gestational trophoblastic disease: a separate analysis of complete and partial hydatidiform moles. Obstet Gynecol. 1991;78(6):1039–45.[↩]
- Sebire NJ, Fisher RA, Foskett M, Rees H, Seckl MJ, Newlands ES. Risk of recurrent hydatidiform mole and subsequent pregnancy outcome following complete or partial hydatidiform molar pregnancy. BJOG. 2003;110(1):22–26. doi: 10.1046/j.1471-0528.2003.02388.x[↩]
- Tham BW, Everard JE, Tidy JA, Drew D, Hancock BW. Gestational trophoblastic disease in the Asian population of northern England and North Wales. BJOG. 2003;110(6):555–559. doi: 10.1046/j.1471-0528.2003.01413.x[↩]
- Colgan TJ, Chang MC, Nanji S, Kolomietz E. A reappraisal of the incidence of placental Hydatidiform mole using selective molecular genotyping. Int J Gynecol Cancer. 2016;26(7):1345–1350. doi: 10.1097/IGC.0000000000000754[↩]
- Tang Y, Zhu C, Zhu C, Liang F, Lee A, Yao X, Chen Q. The impact of pre-evacuation ultrasound examination in histologically confirmed hydatidiform mole in missed abortion. BMC Womens Health. 2020 Sep 10;20(1):196. doi: 10.1186/s12905-020-01064-9[↩][↩]
- Ning F, Hou H, Morse AN, Lash GE. Understanding and management of gestational trophoblastic disease. F1000Res. 2019 Apr 10;8:F1000 Faculty Rev-428. doi: 10.12688/f1000research.14953.1[↩][↩]
- Partial molar pregnancy. https://radiopaedia.org/cases/partial-molar-pregnancy-2?lang=us[↩]
- Complete hydatidiform molar pregnancy. https://radiopaedia.org/cases/complete-hydatidiform-molar-pregnancy-1?lang=us[↩]
- Kle, E., Kle, M., & Ycesoy, G. (2018). A Rare Case Report: Partial Molar Pregnancy with a Live Fetus.[↩]
- ((Ning F, Hou H, Morse AN, Lash GE. Understanding and management of gestational trophoblastic disease. F1000Res. 2019 Apr 10;8:F1000 Faculty Rev-428. doi: 10.12688/f1000research.14953.1[↩]
- Brown J, Naumann RW, Seckl MJ, et al.: 15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage. Gynecol Oncol. 2017;144(1):200–7. 10.1016/j.ygyno.2016.08.330[↩][↩]
- Mello JB, Ramos Cirilo PD, Michelin OC, et al.: Genomic profile in gestational and non-gestational choriocarcinomas. Placenta. 2017;50:8–15. 10.1016/j.placenta.2016.12.009[↩][↩]
- Schmid P, Nagai Y, Agarwal R, et al.: Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study. Lancet. 2009;374(9683):48–55. 10.1016/S0140-6736(09)60618-8[↩][↩]
- Zhao J, Lv WG, Feng FZ, et al.: Placental site trophoblastic tumor: A review of 108 cases and their implications for prognosis and treatment. Gynecol Oncol. 2016;142(1):102–8. 10.1016/j.ygyno.2016.05.006[↩][↩]
- Pradjatmo H, Dasuki D, Dwianingsih EK, et al.: Malignancy risk scoring of hydatidiform moles. Asian Pac J Cancer Prev. 2015;16(6):2441–5. 10.7314/APJCP.2015.16.6.2441[↩][↩]
- Karimi-Zarchi M, Mortazavizadeh MR, Soltani-Gerdefaramrzi M, Rouhi M, Yazdian-Anari P, Ahmadiyeh MH. Investigation of Risk Factors, Stage and Outcome in Patients with Gestational Trophoblastic Disease since 2001 to 2011 in Iran-Yazd. Int J Biomed Sci. 2015 Dec;11(4):166-72. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4699131[↩][↩]
- Braga A, Mora P, de Melo AC, Nogueira-Rodrigues A, Amim-Junior J, Rezende-Filho J, Seckl MJ. Challenges in the diagnosis and treatment of gestational trophoblastic neoplasia worldwide. World J Clin Oncol. 2019 Feb 24;10(2):28-37. doi: 10.5306/wjco.v10.i2.28[↩][↩]
- Yuk JS, Baek JC, Park JE, Jo HC, Park JK, Cho IA. Incidence of gestational trophoblastic disease in South Korea: a longitudinal, population-based study. PeerJ. 2019 Feb 20;7:e6490. doi: 10.7717/peerj.6490[↩][↩]
- Li X, Xu Y, Liu Y, Cheng X, Wang X, Lu W, Xie X. The management of hydatidiform mole with lung nodule: a retrospective analysis in 53 patients. J Gynecol Oncol. 2019 Mar;30(2):e16. doi: 10.3802/jgo.2019.30.e16[↩][↩]
- Kim MJ, Kim KR, Ro JY, Lage JM, Lee HI. Diagnostic and pathogenetic significance of increased stromal apoptosis and incomplete vasculogenesis in complete hydatidiform moles in very early pregnancy periods. Am J Surg Pathol. 2006 Mar;30(3):362-9. doi: 10.1097/01.pas.0000194299.27463.21[↩]
- Lisman BA, Boer K, Bleker OP, van Wely M, Exalto N. Vasculogenesis in complete and partial hydatidiform mole pregnancies studied with CD34 immunohistochemistry. Hum Reprod. 2005 Aug;20(8):2334-9. doi: 10.1093/humrep/dei039[↩]
- Kim KR, Park BH, Hong YO, Kwon HC, Robboy SJ. The villous stromal constituents of complete hydatidiform mole differ histologically in very early pregnancy from the normally developing placenta. Am J Surg Pathol. 2009 Feb;33(2):176-85. doi: 10.1097/PAS.0b013e31817fada1[↩]
- Novac L, Niculescu M, Manolea MM, Iliescu D, Georgescu CV, Comănescu A, Cernea N, Enache A. The vasculogenesis–a possible histological identification criterion for the molar pregnancy. Rom J Morphol Embryol. 2011;52(1):61-7. https://www.rjme.ro/RJME/resources/files/520111061067.pdf[↩]
- Hussein MR. Analysis of the vascular profile and CD99 protein expression in the partial and complete hydatidiform moles using quantitative CD34 immunohistochemistry. Exp Mol Pathol. 2010 Dec;89(3):343-50. doi: 10.1016/j.yexmp.2010.07.002[↩]
- Kar A, Mishra C, Biswal P, Kar T, Panda S, Naik S. Differential expression of cyclin E, p63, and Ki-67 in gestational trophoblastic disease and its role in diagnosis and management: A prospective case-control study. Indian J Pathol Microbiol. 2019 Jan-Mar;62(1):54-60. doi: 10.4103/IJPM.IJPM_82_18[↩]
- Giacometti C, Bellan E, Ambrosi A, Dei Tos AP, Cassaro M, Ludwig K. “While there is p57, there is hope.” The past and the present of diagnosis in first trimester abortions: Diagnostic dilemmas and algorithmic approaches. A review. Placenta. 2021 Dec;116:31-37. doi: 10.1016/j.placenta.2021.02.010[↩]
- Xing D, Adams E, Huang J, Ronnett BM. Refined diagnosis of hydatidiform moles with p57 immunohistochemistry and molecular genotyping: updated analysis of a prospective series of 2217 cases. Mod Pathol. 2021 May;34(5):961-982. doi: 10.1038/s41379-020-00691-9[↩]
- Takahashi S, Okae H, Kobayashi N, Kitamura A, Kumada K, Yaegashi N, Arima T. Loss of p57KIP2 expression confers resistance to contact inhibition in human androgenetic trophoblast stem cells. Proc Natl Acad Sci U S A. 2019 Dec 26;116(52):26606-26613. doi: 10.1073/pnas.1916019116[↩]
- Mittal S, Menon S. Interstitial pregnancy mimicking an invasive hydatidiform mole. Am J Obstet Gynecol. 2019 May;220(5):501. doi: 10.1016/j.ajog.2018.10.024[↩]
- Sarmadi S, Izadi-Mood N, Sanii S, Motevalli D. Inter-observer variability in the histologic criteria of diagnosis of hydatidiform moles. Malays J Pathol. 2019 Apr;41(1):15-24. https://www.mjpath.org.my/2019/v41n1/hydatidiform-moles.pdf[↩]