Contents
- What is hyperostosis
- Diffuse idiopathic skeletal hyperostosis
- Diffuse idiopathic skeletal hyperostosis causes
- Risk factors for diffuse idiopathic skeletal hyperostosis
- Diffuse idiopathic skeletal hyperostosis symptoms
- Diffuse idiopathic skeletal hyperostosis complications
- Diffuse idiopathic skeletal hyperostosis diagnosis
- Diffuse idiopathic skeletal hyperostosis treatment
- Hyperostosis frontalis interna
- Infantile cortical hyperostosis
- Diffuse idiopathic skeletal hyperostosis
What is hyperostosis
Hyperostosis is a benign (non-cancerous) overgrowth of bones. Hyperostosis occurs in many musculoskeletal disorders.
Diffuse idiopathic skeletal hyperostosis
Diffuse idiopathic skeletal hyperostosis (DISH) also known as Forestier disease or senile ankylosing spondyliyis, is a bony hardening of ligaments in areas where they attach to your spine. Diffuse idiopathic skeletal hyperostosis might not cause symptoms or require treatment. If it does cause symptoms, the most common are mild to moderate pain and stiffness in your upper back. Diffuse idiopathic skeletal hyperostosis can also affect your neck and lower back, and some people have diffuse idiopathic skeletal hyperostosis in other areas, such as shoulders, elbows, knees and heels.
Diffuse idiopathic skeletal hyperostosis can be progressive. As it worsens, it can cause serious complications.
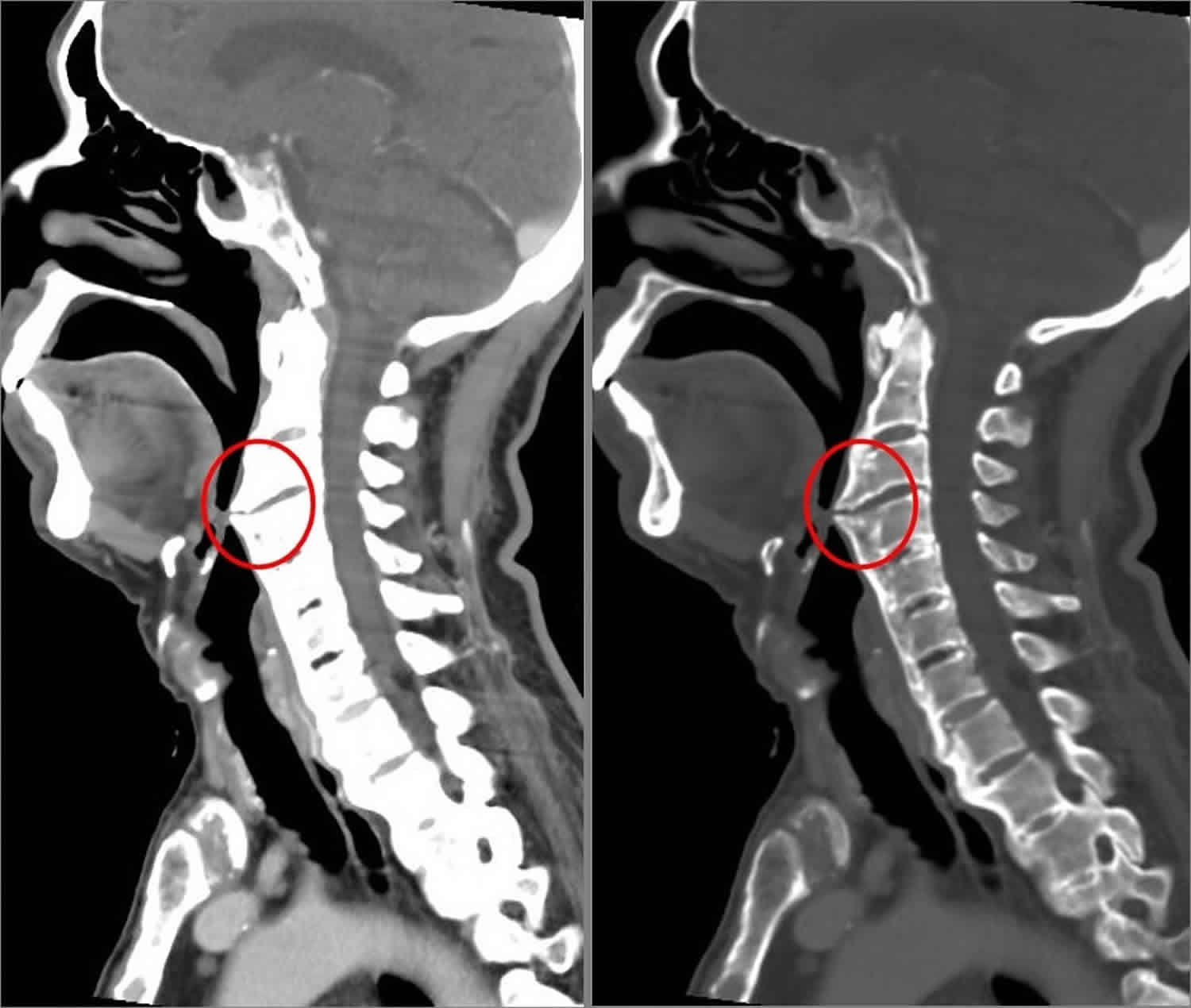
Figure 1. Diffuse idiopathic skeletal hyperostosis
Footnote: (Circles) Florid, flowing ossification is noted along the anterior aspects of the cervical vertebrae merging with bridging anterior osteophytes that encroach upon the oropharynx anteriorly (mainly at the left side).
Diffuse idiopathic skeletal hyperostosis causes
Diffuse idiopathic skeletal hyperostosis is caused by the buildup of calcium salts in the ligaments and tendons and a hardening and overgrowth of bone. But what causes these to occur is unknown.
Risk factors for diffuse idiopathic skeletal hyperostosis
Doctors have some idea of what can increase your risk of the condition. Risk factors include:
- Sex. Men are more likely to develop diffuse idiopathic skeletal hyperostosis .
- Older age. Diffuse idiopathic skeletal hyperostosis is most common in older adults, especially in people older than 50.
- Diabetes and other conditions. People with type 2 diabetes might be more likely to develop DISH than are those who don’t have diabetes. Other conditions that can raise insulin levels in your body may also increase your risk, including hyperinsulinemia, prediabetes and obesity.
- Certain medications. Long-term use of medications called retinoids, such as isotretinoin (Amnesteem, Claravis, others), which are used to treat skin conditions such as acne, can increase your risk.
Diffuse idiopathic skeletal hyperostosis symptoms
You might have no signs or symptoms with diffuse idiopathic skeletal hyperostosis. For those who have signs and symptoms, the upper portion of the back is most commonly affected. Signs and symptoms might include:
- Stiffness. Stiffness may be most noticeable in the morning.
- Pain. You might feel pain in your back or in other affected areas, such as your shoulder, elbow, knee or heel.
- Loss of range of motion. You might notice this most when stretching side to side.
- Difficulty swallowing or a hoarse voice. You might have these if you have DISH in your neck.
Diffuse idiopathic skeletal hyperostosis complications
People with diffuse idiopathic skeletal hyperostosis are at risk of certain complications, such as:
- Disability. Loss of range of motion in the affected joint can make it difficult to use that joint. For instance, DISH in your shoulder can make it difficult to use your arm.
- Difficulty swallowing. Bone spurs in the neck can put pressure on your esophagus. The pressure from bone spurs can also cause a hoarse voice or sleep apnea, a sleep disorder in which you stop breathing repeatedly during sleep. Rarely, this can become serious and might require surgery to remove the bone spurs.
- Spinal fracture. Diffuse idiopathic skeletal hyperostosis can increase your risk of breaking bones in your spine, especially if you have moderate to severe disease. Even minor injuries can cause fractures. Breaks might require surgery to repair.
Diffuse idiopathic skeletal hyperostosis diagnosis
To determine whether you have diffuse idiopathic skeletal hyperostosis, your doctor might begin with a physical examination of your spine and joints. He or she will press lightly on your spine and joints to feel for abnormalities and check your range of motion.
Your doctor will also order imaging tests, such as X-rays, CT scans or MRIs, to look for changes in your spine.
Diffuse idiopathic skeletal hyperostosis treatment
While there’s no cure for diffuse idiopathic skeletal hyperostosis, you can take steps to reduce pain and stiffness. Treatment is also aimed at keeping the condition from worsening and at preventing complications.
Because of the relationship between diffuse idiopathic skeletal hyperostosis and conditions such as obesity, insulin resistance and type 2 diabetes, treating those conditions might slow or halt the progression of diffuse idiopathic skeletal hyperostosis.
Medications
Your doctor might recommend over-the-counter pain relievers, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others). More-severe pain can be treated with corticosteroid injections.
Physical therapy
Physical therapy can reduce the stiffness associated with diffuse idiopathic skeletal hyperostosis. Exercises might also increase the range of motion in your joints. Ask your doctor about specific exercises you can do. He or she might refer you to a physical therapist for further guidance.
Lifestyle and home remedies
To help you manage pain and stiffness and to halt progression of the disease, try these self-care measures:
- Exercise regularly. Regular aerobic exercise, such as walking or swimming, can increase your endurance, keep your body more nimble and help you cope with diffuse idiopathic skeletal hyperostosis. Talk with your doctor before starting an exercise program.
- Achieve and maintain a desirable weight. Since obesity is associated with diffuse idiopathic skeletal hyperostosis, losing weight might help keep the disease from progressing and lower your risk of complications.
- Apply heat. Use a heating pad on affected areas of your body to reduce pain. Set the heating pad to low to reduce the risk of burns.
Surgery
Surgery might be needed in rare cases when diffuse idiopathic skeletal hyperostosis causes severe complications. People who have difficulty swallowing due to large bone spurs in the neck might need surgery to remove the bone spurs. Surgery might also relieve pressure on the spinal cord caused by diffuse idiopathic skeletal hyperostosis.
Hyperostosis frontalis interna
Hyperostosis frontalis interna is characterized benign overgrowth of the inner table of the frontal bone of the skull. Some clinicians believe that hyperostosis frontalis interna may be a common abnormality found in as many as 12 percent of the female population. Hyperostosis frontalis interna affects females 9 times more often than males. This disorder presents itself most often among the middle-aged and elderly but has also been found in adolescents. Hyperostosis frontalis interna is generally of no clinical significance and an incidental finding. It is typically bilateral and symmetrical, and may extend to involve the parietal bones. The skull thickening may be sessile or nodular, and may affect the bone in a focal or diffuse manner. Hyperostosis frontalis interna may also be found associated with a variety of conditions such as seizures, headaches, obesity, diabetes insipidus, excessive hair growth and sex gland disturbances 1. Increased serum alkaline phosphatase and elevated serum calcium may occur.
Hyperostosis frontalis interna may be a part of the triad of Morgagni syndrome. Morgagni-Stewart-Morel syndrome consists of the triad of:
- hyperostosis frontalis interna
- obesity
- excessive hair growth (virilism/hirsutism)
- and is also associated with neuropsychiatric conditions.
The cause of Morgagni syndrome is unclear.
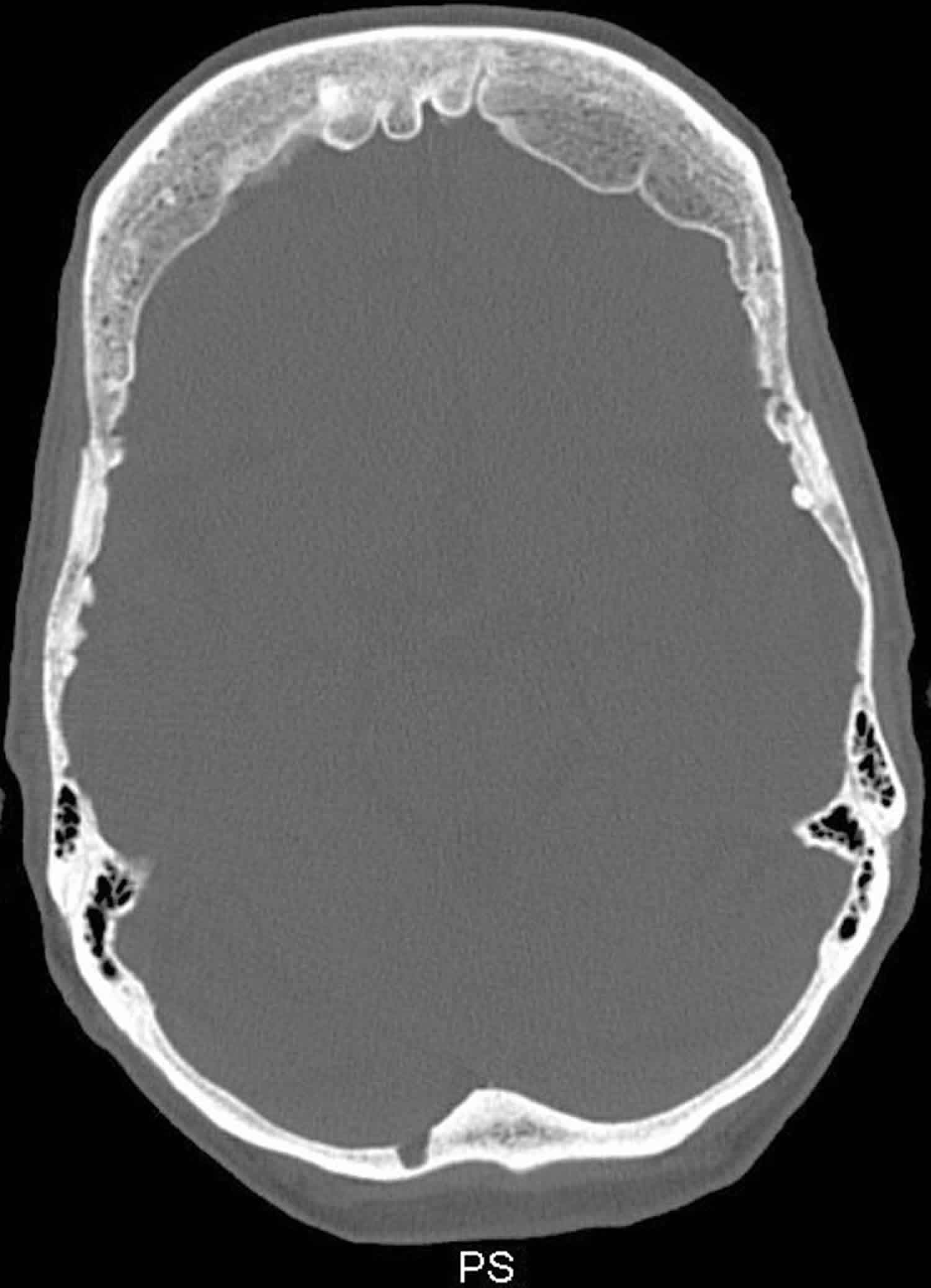
Figure 2. Hyperostosis frontalis interna
Hyperostosis frontalis interna causes
Hyperostosis Frontalis Interna has been found in multiple generations suggesting that the disorder may be inherited as a dominant trait. It is not known if the disorder is autosomal dominant or X-linked. There are no known cases of male-to-male (father to son) transmission.
Human traits, including the classic genetic diseases, are the product of the interaction of two genes, one received from the father and one from the mother.
In dominant disorders, a single copy of the disease gene (received from either the mother or father) will be expressed “dominating” the other normal gene and resulting in the appearance of the disease. The risk of transmitting the disorder from affected parent to offspring is 50 percent for each pregnancy regardless of the sex of the resulting child.
Hyperostosis frontalis interna signs and symptoms
The major feature of hyperostosis frontalis interna is excessive growth or thickening of the frontal bone of the head. This excess growth can only be seen in an x-ray. As a result, scientists feel that this condition may be much more prevalent than suspected, but often goes undetected. Many people have no apparent symptoms.
Other conditions that may be found in patients with this disorder are: obesity, a condition in which secondary male sexual traits are acquired by a female (virilization); a central nervous system disorder characterized by a sudden, aimless, uncontrollable discharge of electrical energy in the brain causing a convulsion or loss of consciousness (epilepsy); decreased vision; headaches; disturbances of the ovaries and testes (sex glands or gonads); excessive body hair; and/or diabetes.
Hyperostosis frontalis interna treatment
There is no known treatment for Hyperostosis Frontalis Interna. Seizures and headaches can be treated with standard medications.
Genetic counseling may be of benefit for patients and their families. Other treatment is symptomatic and supportive.
Infantile cortical hyperostosis
Infantile cortical hyperostosis also known as Caffey disease, is a disorder affecting the skeletal system of babies around 9 weeks of age 2. Infantile cortical hyperostosis most commonly affects the jawbone (70% to 90% of cases), shoulder blades (scapulae), collarbones (clavicles), and the shafts (diaphyses) of long bones in the arms and legs and rarely the ilia, parietal bones, and metatarsals 3. Usually unilateral when involving the scapula. Affected bones may double or triple in width, which can be seen by x-ray imaging. In some cases two bones that are next to each other, such as two ribs or the pairs of long bones in the forearms (radius and ulna) or lower legs (tibia and fibula) become fused together. Infantile cortical hyperostosis can affect all bones except cuboidal bones, vertebral bodies, and phalanges. Primary bone lesions are commonly asymmetric and localized to the diaphysis with sparing of the metaphysis and epiphysis resulting in spindle-shaped bones. Babies with infantile cortical hyperostosis (Caffey disease) also have swelling of joints and of soft tissues such as muscles, with pain and redness in the affected areas. Affected infants can also be feverish and irritable.
The signs and symptoms of infantile cortical hyperostosis are usually apparent by the time an infant is 5 months old. In rare cases, skeletal abnormalities can be detected by ultrasound imaging during the last few weeks of development before birth. Lethal prenatal cortical hyperostosis, a more severe disorder that appears earlier in development and is often fatal before or shortly after birth, is sometimes called lethal prenatal Caffey disease; however, it is generally considered to be a separate disorder.
For unknown reasons, the swelling and pain associated with Caffey disease typically go away within a few months. Through a normal process called bone remodeling, which replaces old bone tissue with new bone, the excess bone is usually reabsorbed by the body and undetectable on x-ray images by the age of 2. Infantile cortical hyperostosis usually spontaneously resolves within 2 years 4. However, if two adjacent bones have fused, they may remain that way, possibly resulting in complications. For example, fused rib bones can lead to curvature of the spine (scoliosis) or limit expansion of the chest, resulting in breathing problems.
Most people with infantile cortical hyperostosis have no further problems related to the disorder after early childhood. Occasionally, another episode of hyperostosis occurs years later. In addition, some adults who had Caffey disease in infancy have other abnormalities of the bones and connective tissues, which provide strength and flexibility to structures throughout the body. Affected adults may have loose joints (joint laxity), stretchy (hyperextensible) skin, or be prone to protrusion of organs through gaps in muscles (hernias).
Infantile cortical hyperostosis has been estimated to occur in approximately 3 per 1,000 infants worldwide. A few hundred cases have been described in the medical literature. Researchers believe this condition is probably underdiagnosed because it usually goes away by itself in early childhood.
Infantile cortical hyperostosis causes
A mutation in the COL1A1 gene causes infantile cortical hyperostosis (Caffey disease) 5. The COL1A1 gene provides instructions for making part of a large molecule called type I collagen. Collagens are a family of proteins that strengthen and support many tissues in the body, including cartilage, bone, tendon, and skin. In these tissues, type I collagen is found in the spaces around cells. The collagen molecules are cross-linked in long, thin, fibrils that are very strong and flexible. Type I collagen is the most abundant form of collagen in the human body.
The COL1A1 gene mutation that causes Caffey disease replaces the protein building block (amino acid) arginine with the amino acid cysteine at protein position 836 (written as Arg836Cys or R836C). This mutation results in the production of type I collagen fibrils that are variable in size and shape, but it is unknown how these changes lead to the signs and symptoms of infantile cortical hyperostosis.
Infantile cortical hyperostosis inheritance pattern
Infantile cortical hyperostosis (Caffey disease) is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is usually sufficient to cause the disorder. About 20 percent of people who have the mutation that causes Caffey disease do not experience its signs or symptoms; this phenomenon is called incomplete penetrance.
In some cases, an affected person inherits the mutation that causes Caffey disease from a parent. Other cases result from new mutations in the gene and occur in people with no history of the disorder in their family.
Infantile cortical hyperostosis symptoms
Infantile cortical hyperostosis is characterized by excessive new bone formation (hyperostosis). The bone abnormalities mainly affect the jawbone, shoulder blades, collarbones, and the shafts of long bones in the arms and legs. Affected bones may double or triple in width. In some cases, two bones in the forearms or lower legs become fused together. Babies with this condition may also develop swelling of joints and soft tissues with pain and redness in the affected areas. They may also be feverish and irritable 3.
The signs and symptoms of infantile cortical hyperostosis are usually apparent by the time an infant is 5 months old. In rare cases, skeletal abnormalities can be detected by ultrasound during the late stages of pregnancy. For unknown reasons, the swelling and pain associated with infantile cortical hyperostosis tend to go away within a few months. The excess bone also disappears as it is reabsorbed by the body through a normal process called bone remodeling. If two bones have been fused, they may remain that way, which can lead to complications such as scoliosis and breathing problems 3.
Most people with infantile cortical hyperostosis have no further problems related to the disorder after early childhood. Occasionally, another episode of hyperostosis occurs years later. In addition, some adults who had infantile cortical hyperostosis have other abnormalities of the bones and connective tissues, including loose joints, stretchy skin or hernias 3.
Infantile cortical hyperostosis diagnosis
Although no specific laboratory tests exist to diagnose infantile cortical hyperostosis (Caffey disease), laboratory studies may be performed to help exclude other diagnoses. The erythrocyte sedimentation rate (ESR) and the alkaline phosphatase (ALP) level are often elevated. Anemia and leukocytosis may be present.
Infantile cortical hyperostosis treatment
No specific treatment exists for infantile cortical hyperostosis (Caffey disease). Infantile cortical hyperostosis is self-limited and usually resolves without complications 6. Some periods of exacerbation and remission may occur during the course of this condition.
Infantile cortical hyperostosis prognosis
Infantile cortical hyperostosis usually runs its course and resolves without complications in 6-9 months. However, the possibility of recurrence should not be ruled out.
Navarre et al 7 reported the case of a 12-year-old female patient who presented with symptoms of pain and swelling of both forearms and legs. These symptoms were similar to symptoms present at the age of 1 month, at which time she was diagnosed as having cortical hyperostosis. Genetic analysis confirmed the COL1A1 mutation. Radiologic investigation revealed new periosteal bone formation of the right and left ulnae and the left fibula, suggesting a recurrence of cortical hyperostosis.
Navarre et al 7 conducted a review of the literature, using the Medline database between 1948 and 2011, and found that the literature confirmed the possibility of recurrence. They concluded that the diagnosis of recurrent cortical hyperostosis should be considered for patients who experienced cortical hyperostosis in infancy and who present with similar symptoms during adolescence 7.
- Hyperostosis Frontalis Interna. https://rarediseases.org/rare-diseases/hyperostosis-frontalis-interna/[↩]
- CAFFEY J. Infantile cortical hyperostosis; a review of the clinical and radiographic features. Proc. R. Soc. Med. 1957 May;50(5):347-54.[↩]
- Caffey disease. https://ghr.nlm.nih.gov/condition/caffey-disease[↩][↩][↩][↩]
- Shandilya R, Gadre KS, Sharma J, Joshi P. Infantile cortical hyperostosis (Caffey disease): a case report and review of the literature–where are we after 70 years? J. Oral Maxillofac. Surg. 2013 Jul;71(7):1195-201[↩]
- Gensure RC, Mäkitie O, Barclay C, Chan C, Depalma SR, Bastepe M, Abuzahra H, Couper R, Mundlos S, Sillence D, Ala Kokko L, Seidman JG, Cole WG, Jüppner H. A novel COL1A1 mutation in infantile cortical hyperostosis (Caffey disease) expands the spectrum of collagen-related disorders. J. Clin. Invest. 2005 May;115(5):1250-7.[↩]
- Rodríguez M, Martínez LE, Cortés J, de Uña A, Vega V, Acosta M. [Infantile cortical hyperostosis: Case report]. Rev Chil Pediatr. 2016 Sep – Oct. 87 (5):401-405.[↩]
- Navarre P, Pehlivanov I, Morin B. Recurrence of infantile cortical hyperostosis: a case report and review of the literature. J Pediatr Orthop. 2013 Mar. 33(2):e10-7.[↩][↩][↩]