Contents
Hypopnea
Hypopnea is defined as reduction in ventilation of at least 50% that results in a decrease in arterial saturation of 4% or more due to partial airway obstruction 1.
Apnea refers to a pause in respiration for more than 10 seconds and is seen in both central sleep apnea (CSA) and obstructive sleep apnea (OSA) 2. Central sleep apnea (CSA) and obstructive sleep apnea (OSA) are differentiated by a lack of respiratory effort in central sleep apnea versus continued but ineffective respiratory effort in obstructive sleep apnea.
Hypopnea causes
Apnea and hypopnea are caused by the airway being sucked close on inspiration during sleep. This occurs as the upper airway dilating muscles, which are also striated muscles, normally relax during sleep.
Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing. These muscles support structures including the back of the roof of your mouth (soft palate), the triangular piece of tissue hanging from the soft palate (uvula), the tonsils and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in and breathing may be inadequate for 10 seconds or longer. This may lower the level of oxygen in your blood and cause a buildup of carbon dioxide.
Your brain senses this impaired breathing and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don’t remember it.
You can awaken with shortness of breath that corrects itself quickly, within one or two deep breaths. You may make a snorting, choking or gasping sound.
This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you’ll probably feel sleepy during your waking hours.
People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, many people with this type of sleep apnea think they slept well all night.
Risk factors for developing obstructive sleep apnea
Anyone can develop obstructive sleep apnea. However, certain factors put you at increased risk, including:
- Excess weight. Most but not all people with obstructive sleep apnea are overweight. Fat deposits around the upper airway may obstruct breathing. Medical conditions that are associated with obesity, such as hypothyroidism and polycystic ovary syndrome, also can cause obstructive sleep apnea. However, not everyone with obstructive sleep apnea is overweight and vice versa. Thin people can develop the disorder, too.
- Narrowed airway. You may inherit naturally narrow airways. Or your tonsils or adenoids may become enlarged, which can block your airway.
- High blood pressure (hypertension). Obstructive sleep apnea is relatively common in people with hypertension.
- Chronic nasal congestion. Obstructive sleep apnea occurs twice as often in those who have consistent nasal congestion at night, regardless of the cause. This may be due to narrowed airways.
- Smoking. People who smoke are more likely to have obstructive sleep apnea.
- Diabetes. Obstructive sleep apnea may be more common in people with diabetes.
- Sex. In general, men are twice as likely as premenopausal women to have obstructive sleep apnea. The frequency of obstructive sleep apnea increases in women after menopause.
- A family history of sleep apnea. If you have family members with obstructive sleep apnea, you may be at increased risk.
- Asthma. Research has found an association between asthma and the risk of obstructive sleep apnea.
Hypopnea symptoms
Signs and symptoms of obstructive sleep apnea include:
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of stopped breathing during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Experiencing mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
Consult a medical professional if you experience, or if your partner observes, the following:
- Snoring loud enough to disturb your sleep or that of others
- Waking up gasping or choking
- Intermittent pauses in your breathing during sleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you’re working, watching television or even driving a vehicle
Many people may not think of snoring as a sign of something potentially serious, and not everyone who snores has obstructive sleep apnea.
Be sure to talk to your doctor if you experience loud snoring, especially snoring that’s punctuated by periods of silence. With obstructive sleep apnea, snoring usually is loudest when you sleep on your back, and it quiets when you turn on your side.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as narcolepsy.
Hypopnea diagnosis
To diagnose your condition, your doctor may make an evaluation based on your signs and symptoms, an examination, and tests. Your doctor may refer you to a sleep specialist in a sleep center for further evaluation.
You’ll have a physical examination, and your doctor will examine the back of your throat, mouth and nose for extra tissue or abnormalities. Your doctor may measure your neck and waist circumference and check your blood pressure.
A sleep specialist may conduct additional evaluations to diagnose your condition, determine the severity of your condition and plan your treatment. The evaluation may involve overnight monitoring of your breathing and other body functions as you sleep.
Tests to detect dyssomnias include:
- Polysomnography. During this sleep study, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep. You may have a full-night study, in which you’re monitored all night, or a split-night sleep study. In a split-night sleep study, you’ll be monitored during the first half of the night. If you’re diagnosed with obstructive sleep apnea, staff may wake you and give you continuous positive airway pressure for the second half of the night. Polysomnography can help your doctor diagnose obstructive sleep apnea and adjust positive airway pressure therapy, if appropriate. This sleep study can also help rule out other sleep disorders that can cause excessive daytime sleepiness but require different treatments, such as leg movements during sleep (periodic limb movements) or sudden bouts of sleep during the day (narcolepsy).
- Home sleep apnea testing. Under certain circumstances, your doctor may provide you with an at-home version of polysomnography to diagnose obstructive sleep apnea. This test usually involves measurement of airflow, breathing patterns and blood oxygen levels, and possibly limb movements and snoring intensity.
Your doctor also may refer you to an ear, nose and throat doctor to rule out any anatomic blockage in your nose or throat.
Hypopnea treatment
Lifestyle changes
For milder cases of obstructive sleep apnea, your doctor may recommend lifestyle changes:
- Lose weight if you’re overweight.
- Exercise regularly.
- Drink alcohol moderately, if at all, and don’t drink several hours before bedtime.
- Quit smoking.
- Use a nasal decongestant or allergy medications.
- Don’t sleep on your back.
- Avoid taking sedative medications such as anti-anxiety drugs or sleeping pills.
If these measures don’t improve your sleep or if your apnea is moderate to severe, then your doctor may recommend other treatments. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary.
Positive airway pressure therapy
If you have obstructive sleep apnea, you may benefit from positive airway pressure. In this treatment, a machine delivers air pressure through a piece that fits into your nose or is placed over your nose and mouth while you sleep. Positive airway pressure reduces the number of respiratory events that occur as you sleep, reduces daytime sleepiness and improves your quality of life.
The most common type is called continuous positive airway pressure (CPAP). With CPAP treatment, the pressure of the air breathed is continuous, constant and somewhat greater than that of the surrounding air, which is just enough to keep your upper airway passages open. This air pressure prevents obstructive sleep apnea and snoring.
Although CPAP is the most consistently successful and most commonly used method of treating obstructive sleep apnea, some people find the mask cumbersome, uncomfortable or loud. However, newer machines are smaller and less noisy than older machines and there are a variety of mask designs for individual comfort.
Also, with some practice, most people learn to adjust the mask to obtain a comfortable and secure fit. You may need to try different types to find a suitable mask. Several options are available, such as nasal masks, nasal pillows or face masks.
If you’re having particular difficulties tolerating pressure, some machines have special adaptive pressure functions to improve comfort. You also may benefit from using a humidifier along with your CPAP system.
CPAP may be given at a continuous (fixed) pressure or varied (autotitrating) pressure. In fixed CPAP, the pressure stays constant. In autotitrating CPAP, the levels of pressure are adjusted if the device senses increased airway resistance.
Bilevel positive airway pressure (BPAP), another type of positive airway pressure, delivers a preset amount of pressure when you breathe in and a different amount of pressure when you breathe out.
CPAP is more commonly used because it’s been well studied for obstructive sleep apnea and has been shown to effectively treat obstructive sleep apnea. However, for people who have difficulty tolerating fixed CPAP, BPAP or autotitrating CPAP may be worth a try.
Don’t stop using your positive airway pressure machine if you have problems. Check with your doctor to see what adjustments you can make to improve its comfort.
In addition, contact your doctor if you still snore despite treatment, if you begin snoring again or if your weight goes up or down by 10% or more.
Mouthpiece (oral device)
Though positive airway pressure is often an effective treatment, oral appliances are an alternative for some people with mild or moderate obstructive sleep apnea. These devices may reduce your sleepiness and improve your quality of life.
These devices are designed to keep your throat open. Some devices keep your airway open by bringing your lower jaw forward, which can sometimes relieve snoring and obstructive sleep apnea. Other devices hold your tongue in a different position.
If you and your doctor decide to explore this option, you’ll need to see a dentist experienced in dental sleep medicine appliances for the fitting and follow-up therapy. A number of devices are available. Close follow-up is needed to ensure successful treatment.
Surgery or other procedures
Surgery is usually considered only if other therapies haven’t been effective or haven’t been appropriate options for you. Surgical options may include:
- Surgical removal of tissue. Uvulopalatopharyngoplasty (UPPP) is a procedure in which your doctor removes tissue from the back of your mouth and top of your throat. Your tonsils and adenoids may be removed as well. Uvulopalatopharyngoplasty usually is performed in a hospital and requires a general anesthetic. Doctors sometimes remove tissue from the back of the throat with a laser (laser-assisted uvulopalatoplasty) or with radiofrequency energy (radiofrequency ablation) to treat snoring. These procedures don’t treat obstructive sleep apnea, but they may reduce snoring.
- Upper airway stimulation. This new device is approved for use in people with moderate to severe obstructive sleep apnea who can’t tolerate CPAP or BPAP. A small, thin impulse generator (hypoglossal nerve stimulator) is implanted under the skin in the upper chest. The device detects your breathing patterns and, when necessary, stimulates the nerve that controls movement of the tongue. Studies have found that upper airway stimulation leads to significant improvement in obstructive sleep apnea symptoms and improvements in quality of life.
- Jaw surgery (maxillomandibular advancement). In this procedure, the upper and lower parts of your jaw are moved forward from the rest of your facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
- Surgical opening in the neck (tracheostomy). You may need this form of surgery if other treatments have failed and you have severe, life-threatening obstructive sleep apnea. During a tracheostomy, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. Air passes in and out of your lungs, bypassing the blocked air passage in your throat.
- Implants. This minimally invasive treatment involves placement of three tiny polyester rods in the soft palate. These inserts stiffen and support the tissue of the soft palate and reduce upper airway collapse and snoring. This treatment is recommended only for people with mild obstructive sleep apnea.
Other types of surgery may help reduce snoring and sleep apnea by clearing or enlarging air passages, including:
- Nasal surgery to remove polyps or straighten a crooked partition between your nostrils (deviated septum)
- Surgery to remove enlarged tonsils (tonsillectomy) or adenoids (adenoidectomy)
Obstructive sleep apnea hypopnea syndrome
Obstructive sleep apnea-hypopnea syndrome is characterized by repeated episodes of reduction in airflow due to repetitive collapse of the upper airway during sleep, which may be either partial or total resulting in hypopnea or apnea 2 and can lead to respiratory failure due to lack of nocturnal oxygen exchange 3. Obstructive sleep apnea hypopnea syndrome is defined as night-time apnea, frequent night-time sleeplessness, or night-time mouth-breathing 4 .
Obstructive sleep apnea hypopnea syndrome can lead to respiratory failure, pulmonary hypertension, and cardiac failure, and may require positive airway pressure ventilation during sleep 5. Furthermore, during sleep apnea, nocturnal hypoxemia can exacerbate co-existing chronic or advanced pulmonary disease, including chronic obstructive pulmonary disease (COPD), and bronchial asthma 6.
Adenotonsillectomy is the most appropriate surgical treatment for obstructive sleep apnea hypopnea syndrome if the patient can tolerate surgery and general anesthesia 7. However, adenotonsillectomy may not be an acceptable treatment option for all patients 8. Studies have shown that patients who suffer from obstructive sleep apnea hypopnea syndrome can have elevated levels of serum inflammatory cytokines 9. Therefore, corticosteroid treatment has been proposed as a possible effective treatment for patients with obstructive sleep apnea hypopnea syndrome 10.
Recent studies have shown that treatment with intranasal mometasone furoate can improve the symptoms of obstructive sleep apnea hypopnea syndrome 11. Treatment with modafinil is also proposed for patients with obstructive sleep apnea hypopnea syndrome as modafinil acts as a mild selective dopamine reuptake inhibitor 12 and has an effect on neurotransmitter systems including histamine 13, γ-aminobutyric acid (GABA), noradrenergic, and serotonergic pathway, which explain the possible mode of action of modafinil in obstructive sleep apnea hypopnea syndrome 14.
The findings of this preliminary clinical study, in a Chinese population of 250 patients with obstructive sleep apnea-hypopnea syndrome (OSAHS) 4 showed that intranasal mometasone furoate had a greater beneficial effect after discontinuation of intervention when compared with modafinil treatment. These study findings are supported by the findings of previously published studies of intranasal corticosteroid therapy for the treatment of sleep apnea in children 15. In the post-study treatment findings of the present study 4, intranasal mometasone furoate treatment was preferred to modafinil by patients with obstructive sleep apnea hypopnea syndrome.
Obstructive sleep apnea hypopnea cause
Apnea and hypopnea are caused by the airway being sucked close on inspiration during sleep. This occurs as the upper airway dilating muscles, which are also striated muscles, normally relax during sleep. In patients with obstructive sleep apnea hypopnea syndrome, the dilating muscles can no longer successfully oppose negative pressure within the airway during inspiration 16. The patients have narrow upper airways. The airway is kept patent by the dilating muscles which have higher than normal activity during wakefulness. But during sleep, the muscle tone falls and airway narrows 17. Snoring may then occur; followed by airway occlusion and subsequent apnea. The characteristics of this condition include hypoxemia, hypercapnia, large intrathoracic pressure swings (to -120 mm Hg), and surges of systemic blood pressure of up to 250/150 mm Hg which is associated with arousals and sleep fragmentation, up to 100 times per hour 18.
Symptoms include excessive daytime somnolence, non-refreshed sleep, nocturia, loud snoring, apneas and choking during sleep, morning headaches, and sexual dysfunction.
Predisposing factors include all the factors which cause narrowing of pharynx, e.g. obesity (more than 50% of obese patients have body mass index (BMI) greater than 30 kg/m²), shortening of the mandible or maxilla. Change in jaw shape may be mild and familial. Hypothyroidism and acromegaly predispose to obstructive sleep apnea hypopnea syndrome by narrowing the upper airway with tissue infiltration. Other factors include male gender, middle age (40–65 years), myotonic dystrophy, Ehlers-Danlos syndrome, and possibly smoking 19. Obstructive sleep apnea hypopnea syndrome also occurs in childhood and is usually associated with tonsil or adenoid enlargement.
Obstructive sleep apnea hypopnea complications
Neurobehavioral and social
Excessive daytime sleepiness, impaired vigilance, mood disturbances, and cognitive dysfunctions are the features of obstructive sleep apnea hypopnea syndrome. The sleepiness may result in inability to work efficiently and may damage interpersonal relationship and prevent socializing. The somnolence is dangerous when driving and causes three- to sixfold increase in road accidents or when operating machinery 19. Partners of patients with obstructive sleep apnea hypopnea syndrome experience poor sleep, and often it is the partner who prompts the evaluation, seeking relief from loud snoring.
Cardiovascular
The intermittent hypoxia, negative intrathoracic pressure variations, and arousals characteristic of apneas and hypopneas lead to increase in blood pressure at the termination of disordered breathing events evolving into sustained hypertension via chronically heightened sympathetic nervous system activity and arterial baroreceptor dysfunction 20. Hypertension in the setting of obstructive sleep apnea hypopnea syndrome may be more difficult to treat. Large population-based studies have associated obstructive sleep apnea hypopnea syndrome with cardiovascular and cerebrovascular diseases 20. Observational studies suggest an increase in the risk of myocardial infarction and stroke in untreated obstructive sleep apnea hypopnea syndrome 21. Cardiac arrhythmias and cor pulmonale are commoner in these patients 20.
Diabetes mellitus
Recent data suggest obstructive sleep apnea hypopnea syndrome is associated with insulin resistance, independent of obesity 16. The association of obstructive sleep apnea hypopnea syndrome with diabetes mellitus is not just due to obesity being common in both conditions. Obesity is associated with diabetes mellitus, and diabetes mellitus may cause vascular and neuropathic damage to the dilator pharyngeal muscles and reduced upper airway sensation; this needs to be further investigated 22.
Liver
Hepatic dysfunction has also been associated with irregular breathing during sleep. Nonalcoholic subjects with apnea and hypopnea during sleep were found to have raised liver enzymes and fibrosis on liver biopsy, independent of body weight 16.
Perioperative and postoperative
Patients with obstructive sleep apnea hypopnea syndrome may have an increased perioperative risks. In such patients, endotracheal intubation may be more difficult and recovery may be more prolonged postoperatively 16.
Obstructive sleep apnea hypopnea syndrome differential diagnosis
The differential diagnoses of obstructive sleep apnea hypopnea syndrome include the following:
- Insufficient sleep: A good history taking can always reveal this diagnosis.
- Shift work: This is a major cause of sleepiness in workers either on rotating shift or with night work patterns.
- Psychological conditions: Depression is a major cause of sleepiness.
- Drugs: This is common with sedatives and stimulant drugs.
- Narcolepsy: Is much less common than obstructive sleep apnea hypopnea syndrome and usually commences from childhood.
- Idiopathic hypersomnolence: This is a term used to define long duration of sleep and sleepiness.
Obstructive sleep apnea hypopnea syndrome diagnosis
Medical history
The history focuses on breathing disturbances during sleep, unsatisfactory sleep quality, and daytime somnolence. History should be obtained from both patients and sleeping partners. History of habitual socially disruptive snoring and witnessed apneas terminated by gasps increases the diagnostic accuracy. Obstructive sleep apnea hypopnea syndrome is 2–3 times greater in men. This sex protective effect is diminished in premenopausal overweight women (BMI ≥ 32 kg/m²), menopausal women not on replacement therapy, and overweight women on hormone replacement therapy 23. Other factors include smoking, alcohol, drugs, and nasal congestion 24.
Physical examination
The physical examination may reveal craniofacial and soft tissue enlargement associated with upper airway resistance such as retrognathia, deviated nasal septum, low-lying soft palate, enlarged uvula and base of the tongue. Other clinical pointers include a causal role for obesity (BMI≥28 kg/m²) and neck circumferences of ≥43 cm 19. Obstructive sleep apnea hypopnea syndrome patients with other co-morbidities may predispose to severe pulmonary hypertension.
Investigations
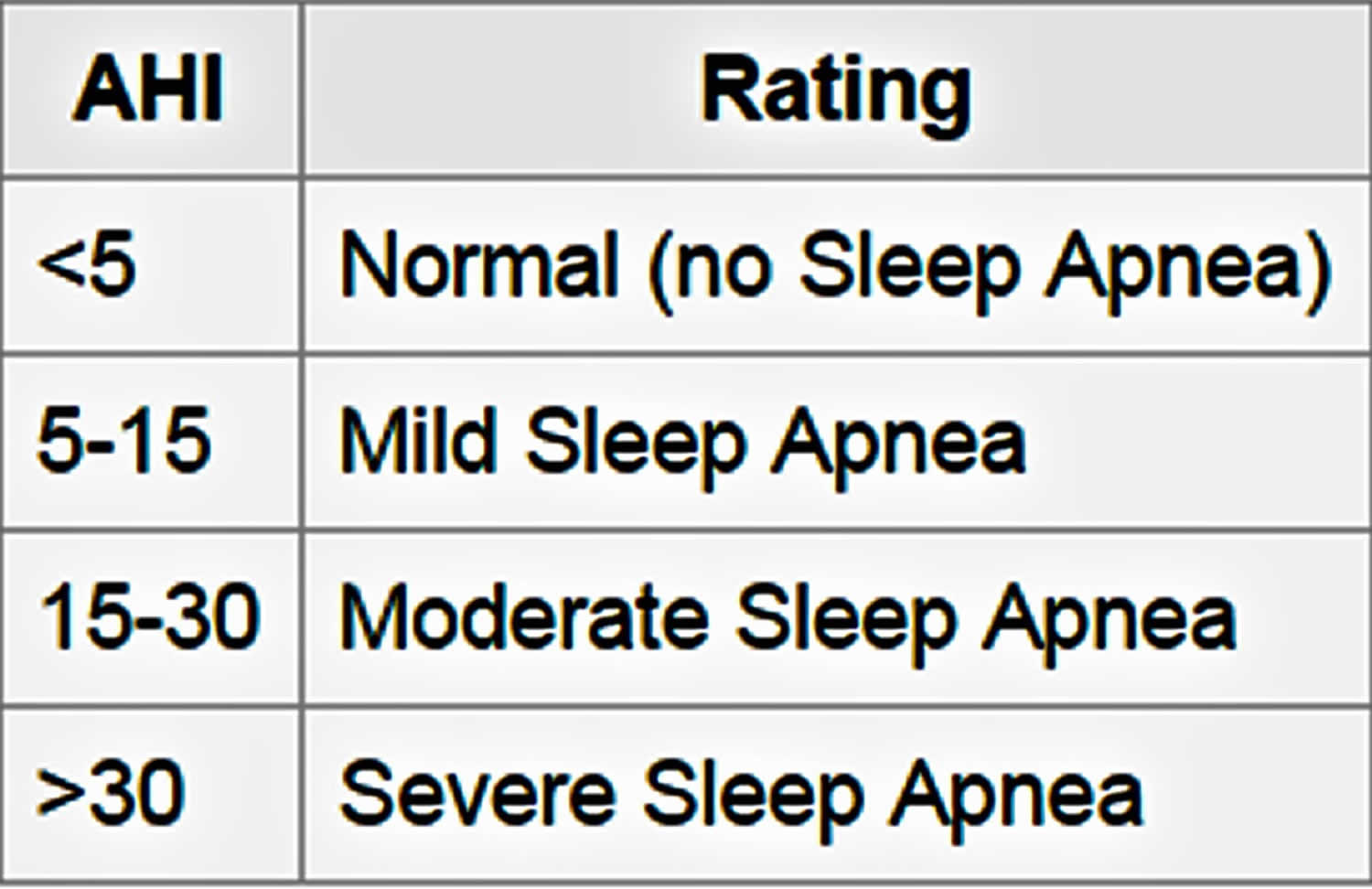
A patient with obstructive sleep apnea hypopnea syndrome should be admitted. Sleep study should be performed on such a patient. Ideally, full somnographic studies should be done with recording of multiple respiratory and neurophysiologic signals during sleep. But in most centers, especially outside the USA, only “limited studies” are done which involve recording respiratory and oxygenation patterns overnight without neurophysiologic recording 19. Episode of apnea/hypopneas occurring more than five times and lasting for ≥10 seconds is regarded as significant. This is called Apnea-Hypopnea Index (AHI) (Figure 1).
- Apnea-Hypopnea Index (AHI) measures sleep apnea severity. The Apnea-Hypopnea Index (AHI) is the sum of the number of apneas (pauses in breathing) plus the number of hypopneas (periods of shallow breathing) that occur, on average, each hour.
- To count in the index apneas and hypopneas, collectively called events, must have a duration of at least 10 seconds.
- The Apnea-Hypopnea Index (AHI), as with the separate Apnea Index and Hypopnea Index, is calculated by dividing the number of events by the number of hours of sleep.
The obstructive sleep apnea hypopnea syndrome is arbitrarily defined by greater than five apneas/hypopneas per hour plus symptoms of daytime sleepiness or when Apnea-Hypopnea Index (AHI) is >15. Apnea-Hypopnea Index (AHI) has been used to grade the degree of severity of obstructive sleep apnea hypopnea syndrome. Apnea-Hypopnea Index (AHI) of 5–14 is regarded as mild, 15–30 as moderate, and greater than 30 as severe obstructive sleep apnea hypopnea syndrome 18.
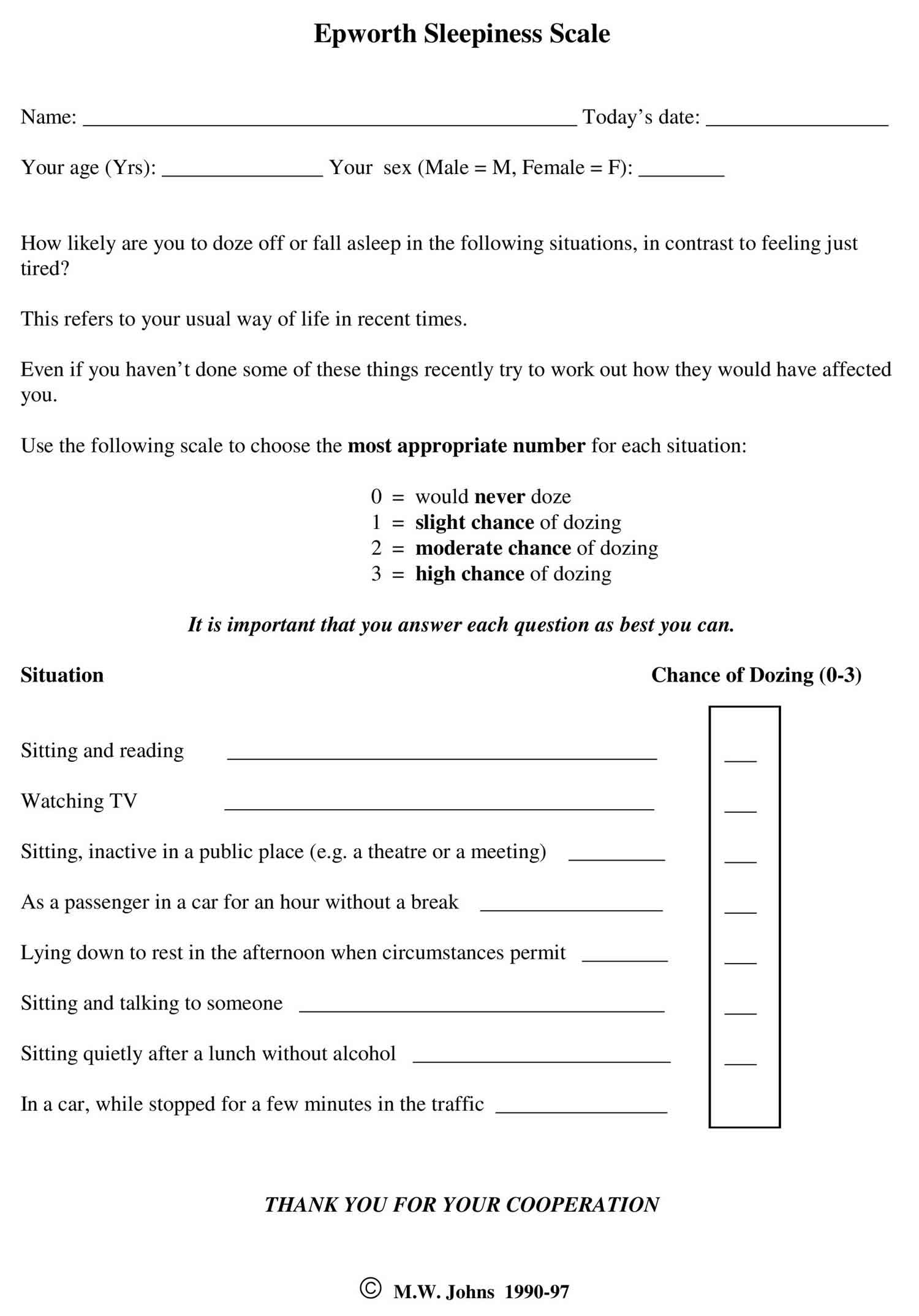
The Epworth Sleepiness Scale first published in 1991 and revised in 1997 25, has been used to assess patients with obstructive sleep apnea hypopnea syndrome (see Figure 2). Patients with scores ≥11 and experiencing sleepiness during work or driving are regarded as having obstructive sleep apnea hypopnea syndrome. Both the patients and the partner should be assessed and, in this case, the higher of two scores should be accepted. Epworth Sleepiness Scale is a self-administered questionnaire with 8 questions. The questionnaire asks the subject to rate his or her probability of falling asleep on a scale of increasing probability from 0 to 3 (0 = no chance of dozing 1 = slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing) for eight different situations that most people engage in during their daily lives, though not necessarily every day. The scores for the eight questions are added together to obtain a single number. A number in the 0–9 range is considered to be normal while a number in the 10–24 range indicates that expert medical advice should be sought. For instance, scores of 11-15 are shown to indicate the possibility of mild to moderate sleep apnea, where a score of 16 and above indicates the possibility of severe sleep apnea or narcolepsy. Certain questions in the scale were shown to be better predictors of specific sleep disorders, though further tests may be required to provide an accurate diagnosis.
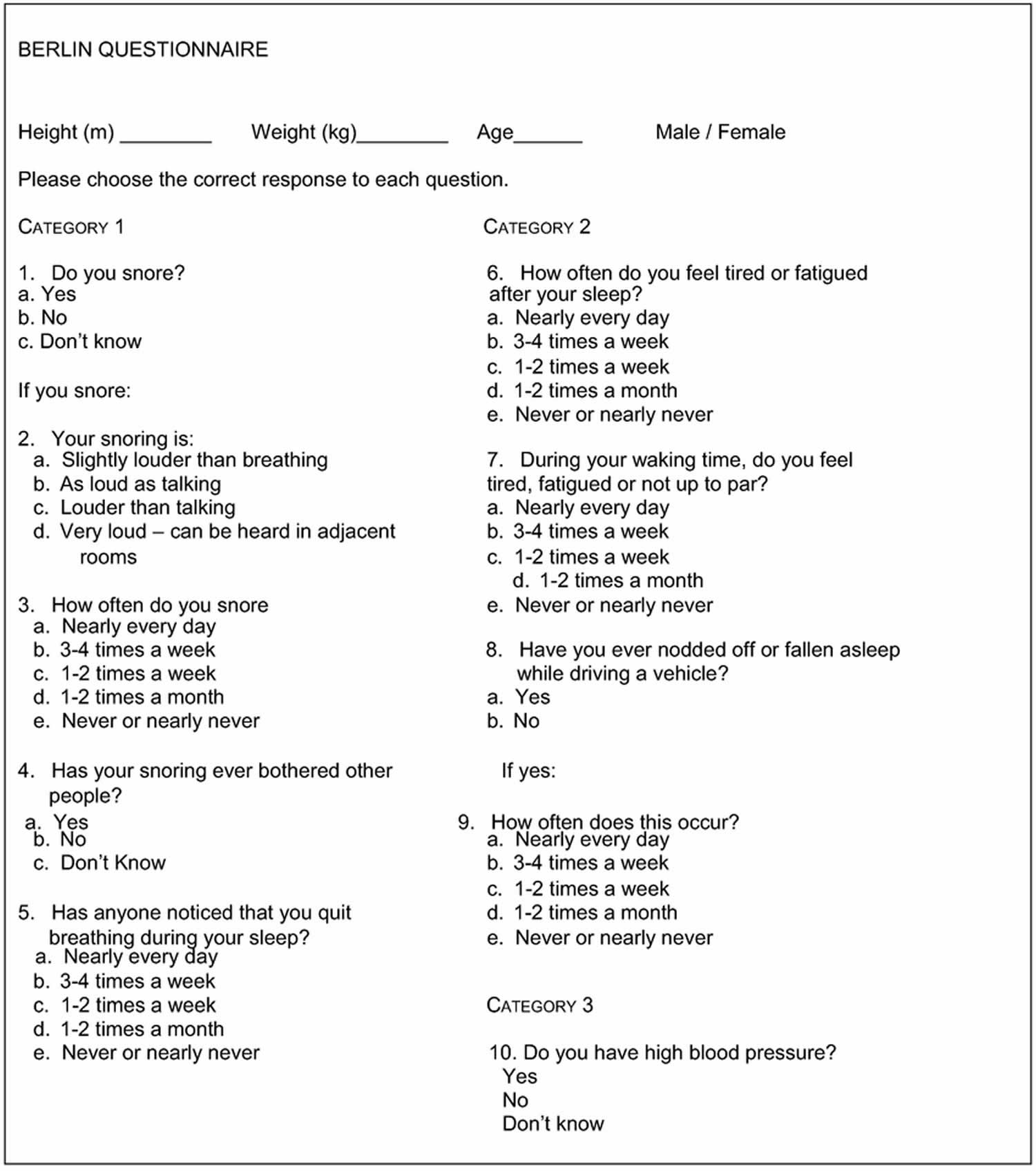
The Berlin questionnaire 26 is a good assessment tool for initial screening of patients suspected of having obstructive sleep apnea hypopnea syndrome (see Figure 3). Berlin questionnaire has three parts. The first part focuses on snoring, the second part on breathing pauses and daytime sleepiness, and the third part focuses on the presence of obesity and hypertension.
Figure 1. Apnea-Hypopnea Index (AHI)
Figure 2. Epworth Sleepiness Scale
Figure 3. Berlin questionnaire
[Source 27 ]Pulse Oximetry
Obstructive sleep apnea and hypopnea results in repetitive “saw tooth” oscillations in the oxyhemoglobin saturation on a time-compressed profile 18. It shows marked and progressive hypopneas over the period with evidence of fragmented sleep. For diagnosing obstructive sleep apnea hypopnea syndrome, pulse oximetry is not considered a single alternative to polysomnography.
Obstructive sleep apnea hypopnea syndrome treatment
Obstructive sleep apnea hypopnea syndrome is a chronic condition; therefore, patient education, alleviation of airway obstruction, and follow-up are important in the optimal management of patients.
Conservative management
Lifestyle modification is important in the management of patients with obstructive sleep apnea hypopnea syndrome. Co-morbidities should be identified and also treated. Lifestyle modification includes weight reduction, reduction of alcohol intake, withdrawal of drugs and sedatives which affect airway tone, smoking cessation, avoidance of sleep deprivation, and adjustment of sleeping positions. Longitudinal data from Wisconsin sleep cohort study indicate that a 10% weight reduction predicts a 26% decrease in the AHI 19.
Continuous positive airway pressure (CPAP)
Once decision has been made to treat obstructive sleep apnea hypopnea syndrome, continuous positive airway pressure (CPAP) is the preferred treatment of choice. It is a device that pneumatically splints the upper airway during inspiration and expiration while the patient is asleep. CPAP is titrated to a level that eliminates snoring, usually 5–20 cm Hg. A randomized placebo-controlled trial showed that CPAP can improve breathing during sleep, sleep quality, blood pressure, vigilance, cognition, and driving ability as well as mood and quality of life in patients with obstructive sleep apnea hypopnea syndrome. Problems are encountered during initiation and use of CPAP.
The following questions should be asked by the clinician during assessment of patients on CPAP:
- Does anything interfere with your use of CPAP?
- Do you feel sleepy during the day?
- Does your bed partner observe snoring or breathing pauses when you use CPAP?
- Have you observed any change in weight since CPAP therapy was prescribed or last adjusted?
- When was your CPAP equipment assessed last?
Mandibular repositioning splint
Mandibular repositioning splints or oral devices work by holding lower jaw and the tongue forward, thereby increasing the pharyngeal airway 16.
Medication
Modafinil has been shown to offer a marginal improvement in sleepiness in patients with obstructive sleep apnea hypopnea syndrome who remain sleepy despite CPAP 16. The clinical value and cost implication are debatable. Modafinil is contraindicated in pregnancy and lactation.
Surgery
Four forms of surgery benefit patients with obstructive sleep apnea hypopnea syndrome 28.
Bariatric surgery can be curative in patients with morbid obesity. Tonsillectomy is highly effective in children. Tracheostomy is curative but rarely used because of increased morbidity. Jaw advancement surgery, especially maxilla-mandibular osteotomy, is effective in patients with retrognathia.
- Sleep apnoea: What Is Sleep Apnoea? NHLBI: Health information for the public. U S Department of Health and Human services. 2009 May; Assessed from internet on 20th November, 2010[↩]
- Mbata G, Chukwuka J. Obstructive sleep apnea hypopnea syndrome. Ann Med Health Sci Res. 2012;2(1):74–77. doi:10.4103/2141-9248.96943 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3507119[↩][↩]
- Obstructive sleep apnea-hypopnea syndrome in patients with severe chronic respiratory insufficiency. Hernández Voth A, Sayas Catalán J, Benavides Mañas P, de Pablo Gafas A, Díaz Cambriles T, Villena Garrido V. Med Clin (Barc). 2017 May 23; 148(10):449-452.[↩]
- Zhang S, Fu J, Duan Z. Comparison of the Efficacy, Side Effects, and Cost of Modafinil and Intranasal Mometasone Furoate in Obstructive Sleep Apnea-Hypopnea Syndrome: A Preliminary Clinical Study. Med Sci Monit. 2018;24:3084–3092. Published 2018 May 11. doi:10.12659/MSM.907565 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5973497[↩][↩][↩]
- Impact of CPAP use and age on mortality in patients with combined COPD and obstructive sleep apnea: the overlap syndrome. Stanchina ML, Welicky LM, Donat W, Lee D, Corrao W, Malhotra A. J Clin Sleep Med. 2013 Aug 15; 9(8):767-72.[↩]
- Review: Quality of Life in Children with Non-cystic Fibrosis Bronchiectasis. Nathan AM, de Bruyne JA, Eg KP, Thavagnanam S. Front Pediatr. 2017; 5():84.[↩]
- A randomized trial of adenotonsillectomy for childhood sleep apnea. Marcus CL, Moore RH, Rosen CL, Giordani B, Garetz SL, Taylor HG, Mitchell RB, Amin R, Katz ES, Arens R, Paruthi S, Muzumdar H, Gozal D, Thomas NH, Ware J, Beebe D, Snyder K, Elden L, Sprecher RC, Willging P, Jones D, Bent JP, Hoban T, Chervin RD, Ellenberg SS, Redline S, Childhood Adenotonsillectomy Trial (CHAT). N Engl J Med. 2013 Jun 20; 368(25):2366-76.[↩]
- Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130:e714–55.[↩]
- Kim J, Bhattacharjee R, Dayyat E, et al. Increased cellular proliferation and inflammatory cytokines in tonsils derived from children with obstructive sleep apnea. Pediatr Res. 2009;66:423–28.[↩]
- Rezaeetalab F, Rezaeitalab F, Dehestani V. Inhaled steroids reduce apnea-hypopnea index in overlap syndrome. Pneumologia. 2013;62:212–14.[↩]
- Jung YG, Kim HY, Min JY, et al. Role of intranasal topical steroid in pediatric sleep-disordered breathing and influence of allergy, sinusitis, and obesity on treatment outcome. Clin Exp Otorhinolaryngol. 2011;4:27–32.[↩]
- Madras BK, Lin Z, Jassen A, et al. Modafinil occupies dopamine and norepinephrine transporters in vivo and modulates the transporters and trace amine activity in vitro. J Pharmacol Exp Ther. 2006;319:561–69.[↩]
- Ishizuka T, Murakami M, Yamatodani A. Involvement of central histaminergic systems in modafinil-induced but not methylphenidate-induced increases in locomotor activity in rats. Eur J Pharmacol. 2008;578:209–15.[↩]
- Morgenthaler TI, Kapen S, Lee-Chiong T, et al. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29:1031–35.[↩]
- Kheirandish-Gozal L, Gozal D. Intranasal budesonide treatment for children with mild obstructive sleep apnea syndrome. Pediatrics. 2008;122:149–55.[↩]
- Dauglas NJ. Sleep Apnoea. In: Fausi AS, Kasper DL, Longo LD, Braunwald E, Hauser SL, Jameson JL, et al., editors. Harrisons Principles of Internal Medicine. New York: Mc Graw –Hill; 2008. pp. 1665–7.[↩][↩][↩][↩][↩][↩]
- Eckert DJ, Jordan AS, Merchia P, Malhotra A. Central Sleep Apnoea: Pathophysiology and treatment. Chest. 2007;131:595–607.[↩]
- Crummy F, Piper AJ, Naughton MT. Obesity and the lung: Obesity and sleep disordered breathing. Thorax. 2008;63:738–46.[↩][↩][↩]
- Olson EJ, Moore WR, Morgenthaler TI, Gay PC, Staats BA. Obstructive sleep apnoea hypopnoea syndrome. Mayo Clin Proc. 2003;78:1545–52.[↩][↩][↩][↩][↩]
- Leung RS. Sleep–disordered breathing, autonomic mechanisms and arrhythmias. Prog Cardiovasc Dis. 2009;51:324–38.[↩][↩][↩]
- Leung RS, Bradley TD. Sleep apnoea and cardiovascular disease. Am J Respir Crit Care Med. 2001;164:2147–65.[↩]
- Bottini P, Redolfi S, Dottorini ML, Tantucci C. Autonomic neuropathy increases the risk of obstructive sleep apnoea in obese diabetes. Respiration. 2008;75:265–71.[↩]
- Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep disordered breathing in women: Effects of gender. Am J Respir Crit Care Med. 2001;163:608–13.[↩]
- Young T, Preppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnoea: A population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39.[↩]
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5.[↩]
- Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at for the sleep apnoea syndrome. Ann Intern Med. 1999;131:485–91.[↩]
- Maurer JT. Early diagnosis of sleep related breathing disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2008;7:Doc03. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199834[↩]
- Sundaram S, Bridgman SA, Lim J, Lasserson TJ. Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev. 2005;4:CD001004[↩]