Contents
- What is a hysterectomy
- How long does it take to recover from a hysterectomy?
- Will the doctor remove my ovaries during the hysterectomy?
- Will having a hysterectomy send me into menopause?
- What changes can I expect after a hysterectomy?
- Will I have emotional problems after a hysterectomy?
- Will having a hysterectomy have an effect on my enjoyment of sex?
- Do I still need to have cervical screening tests (Pap test) after hysterectomy?
- What are some alternatives to hysterectomy?
- The female reproductive system
- Hysterectomy types
- Reasons for hysterectomy
- How you prepare for a hysterectomy
- What you can expect during the hysterectomy procedure
- Hysterectomy recovery
- What to expect after a hysterectomy
- Hysterectomy side effects
What is a hysterectomy
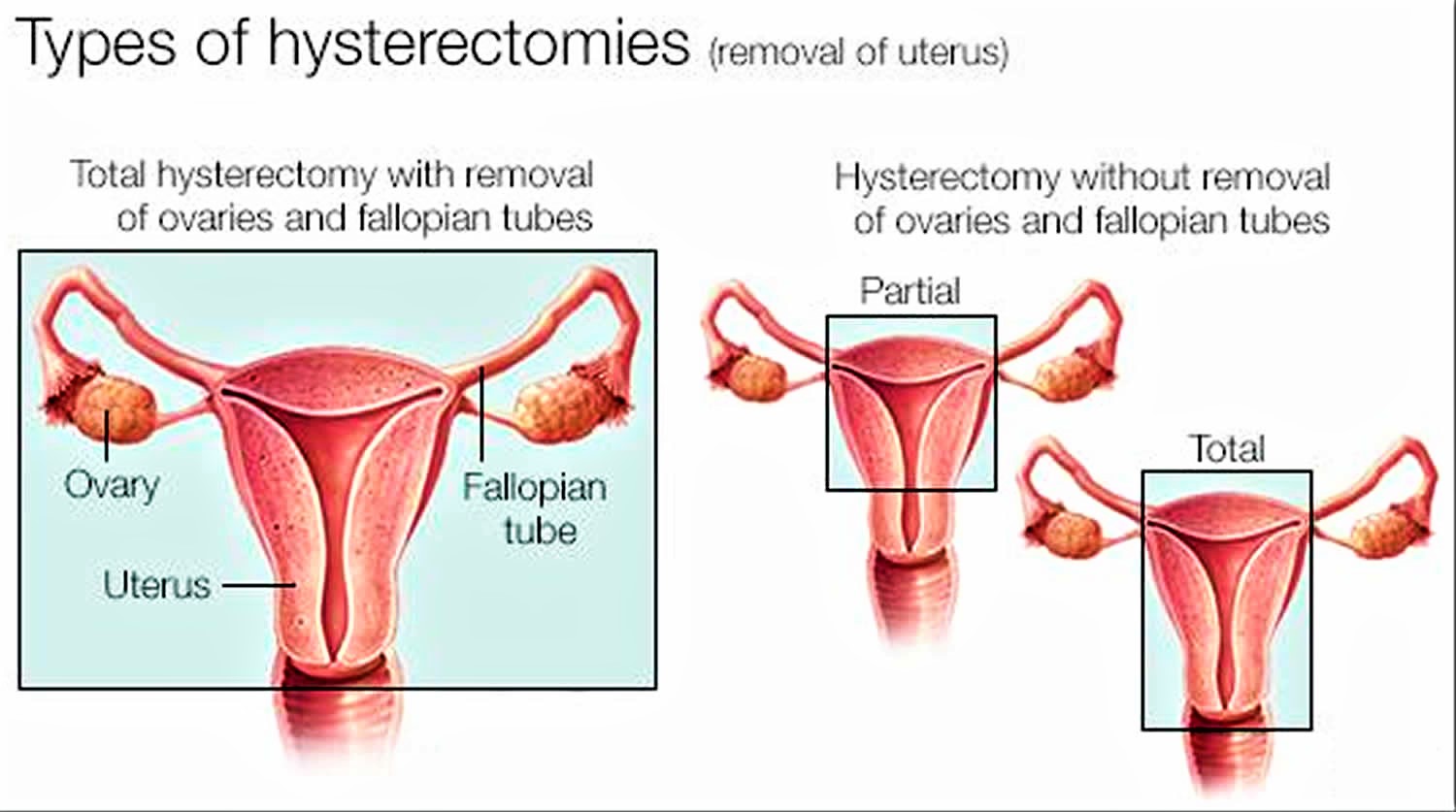
A hysterectomy is a surgery to remove a woman’s uterus (womb). The uterus is where a baby grows when a woman is pregnant. During a hysterectomy surgery the whole uterus is usually removed. The lower part of your uterus (cervix) is usually removed (total hysterectomy) but may sometimes the cervix is left in place (partial hysterectomy). When the surgeon also remove your fallopian tubes and one or both ovaries, it’s called a total hysterectomy with salpingo-oophorectomy. All these organs are part of your reproductive system and are located in your pelvis. After a hysterectomy, you no longer have menstrual periods and cannot become pregnant. You and your doctor should discuss ahead of time whether you need this procedure, which results in what’s known as surgical menopause in the case where both of your ovaries are also removed.
With surgical menopause, menopause symptoms often begin suddenly for women after having the procedure done. Depending on how much these symptoms affect your quality of life, you may need short-term treatment with hormones.
Each year in the United States, nearly 500,000 women get hysterectomies 1. A hysterectomy is the second most common surgery among women in the United States. The most common surgery in women is childbirth by cesarean delivery (C-section).
A hysterectomy ends your ability to become pregnant. If you think you might want to become pregnant, ask your doctor about alternatives to hysterectomy. In the case of cancer, a hysterectomy might be the only option. But for other conditions — including uterine fibroids, endometriosis and uterine prolapse — you may be able to try less invasive treatments first.
A hysterectomy can also be performed through an incision in the vagina (vaginal hysterectomy) or an abdominal hysterectomy where your uterus is removed through an incision in your lower abdomen. Both procedures can be performed by a laparoscopic or robotic surgical approach — which uses long, thin instruments passed through small abdominal incisions.
The conditions that may lead to a hysterectomy can have an immense influence on a woman’s quality of life, affecting your general health, daily routine or sense of wellbeing. These conditions may include:
- Heavy menstrual bleeding (menorrhagia) that has not responded to other treatments.
- An enlarged uterus that may be pressing on other organs.
- Uterine fibroids
- Uterine prolapse
- Cancer of the cervix, uterus, or ovary.
Make sure that you are clear on the reason for hysterectomy by talking with your gynecologist.
Your recovery time
It takes about six to eight weeks to fully recover after having an abdominal hysterectomy. Recovery times are often shorter after a vaginal or laparoscopy hysterectomy.
During this time, you should rest as much as possible and not lift anything heavy, such as bags of shopping. Your abdominal muscles and the surrounding tissues need time to heal.
How long does it take to recover from a hysterectomy?
Recovering from a hysterectomy takes time. Most women stay in the hospital one to two days after surgery. Some doctors may send you home the same day of your surgery. Some women stay in the hospital longer, often when the hysterectomy is done because of cancer.
Your doctor will likely have you get up and move around as soon as possible after your hysterectomy. This includes going to the bathroom on your own. However, you may have to pee through a thin tube called a catheter for one or two days after your surgery.
The time it takes for you to return to normal activities depends on the type of surgery:
- Abdominal hysterectomy can take from four to six weeks to recover.
- Vaginal, laparoscopic, or robotic hysterectomy can take from three to four weeks to recover.
You should get plenty of rest and not lift heavy objects for four to six weeks after surgery. At that time, you should be able to take tub baths and resume sexual intercourse. How long it takes for you to recover will depend on your surgery and your health before the surgery. Talk to your doctor.
Will the doctor remove my ovaries during the hysterectomy?
Whether your ovaries are removed during the hysterectomy may depend on the reason for your hysterectomy.
Ovaries may be removed during hysterectomy to lower the risk for ovarian cancer. However, women who have not yet gone through menopause also lose the protection of estrogen, which helps protect women from conditions such as heart disease and osteoporosis.
Recent studies suggest that removing only the fallopian tubes but keeping the ovaries may help lower the risk for the most common type of ovarian cancer, which is believed to start in the fallopian tubes 2.
The decision to keep or remove your ovaries is one you can make after talking about the risks and benefits with your doctor.
Will having a hysterectomy send me into menopause?
Menopause happens when women no longer release eggs from the ovaries. Unless both ovaries are removed as part of the hysterectomy, menopause will not happen at the time of the hysterectomy surgery.
If you keep your ovaries during the hysterectomy, you should not have other menopausal symptoms right away. But you may have symptoms a few years younger than the average age for menopause (52 years).
Because your uterus is removed, you no longer have periods and cannot get pregnant. But your ovaries might still make hormones, so you might not have other signs of menopause. You may have hot flashes, a symptom of menopause, because the surgery may have blocked blood flow to the ovaries. This can prevent the ovaries from releasing estrogen.
If both ovaries are removed during the hysterectomy, you will no longer have periods and you may have other menopausal symptoms right away. Because your hormone levels drop quickly without ovaries, your symptoms may be stronger than with natural menopause. Ask your doctor about ways to manage your symptoms.
What changes can I expect after a hysterectomy?
Hysterectomy is a major surgery, so recovery can take a few weeks. But for most women, the biggest change is a better quality of life. You should have relief from the symptoms that made the surgery necessary.
Other changes that you may experience after a hysterectomy include:
- Menopause. You will no longer have periods. If your ovaries are removed during the hysterectomy, you may have other menopause symptoms.
- Change in sexual feelings. Some women have vaginal dryness or less interest in sex after a hysterectomy, especially if the ovaries are removed.
- Increased risk for other health problems. If both ovaries are removed, this may put you at higher risk for certain conditions such as: bone loss, heart disease, and urinary incontinence (leaking of urine). Talk to your doctor about how to prevent these problems.
- Sense of loss. Some women may feel grief or depression over the loss of fertility or the change in their bodies. Talk to your doctor if you have symptoms of depression, including feelings of sadness, a loss of interest in food or things you once enjoyed, or less energy, that last longer than a few weeks after your surgery.
Will I have emotional problems after a hysterectomy?
A hysterectomy is a major operation, so it is normal to have a period of recovery. During this time it is normal to experience tiredness, and sometimes tearfulness and a sense of depression. However, the great majority of women experience better moods and emotions once they have recovered because their medical concerns usually improve. Heavy menstrual bleeding, pain and discomfort, and prolapse are all unpleasant – once the hysterectomy has been performed these symptoms are usually better, and women very commonly feel much better as well.
Will having a hysterectomy have an effect on my enjoyment of sex?
Many women will have increased enjoyment of sex if hysterectomy improves problems such as heavy or painful periods, pain from fibroids, or discomfort from prolapse. Some women will find there is no change after hysterectomy. Very rarely, there may be decreased enjoyment of sex – however, this may not be directly due to the hysterectomy but to the repair operation to the vagina which is often performed at the same time as a vaginal hysterectomy for uterine prolapse.
If your hysterectomy causes you to have symptoms of menopause, you may experience vaginal dryness or a lack of interest in sex. Using a water-based lubricant can help with dryness. Talk to your partner and try to allow more time to get aroused during sex.
Do I still need to have cervical screening tests (Pap test) after hysterectomy?
If the cervix is removed and normal then you will not usually need to have any further Pap smears or Pap tests. If you have a ‘partial hysterectomy’ (where the cervix is not removed) then you should continue to have Pap smears as guided by the national screening program. Please check with your surgeon as to the recommendations for your own care.
What are some alternatives to hysterectomy?
Hysterectomy is major surgery. Sometimes a hysterectomy may be medically necessary, such as with prolonged heavy bleeding or certain types of cancer. But sometimes you can try other treatments first. These include:
- Watchful waiting. You and your doctor may wish to wait if you have uterine fibroids, which tend to shrink after menopause.
- Exercises. For uterine prolapse, you can try Kegel exercises (squeezing the pelvic floor muscles). Kegel exercises help restore tone to the muscles holding the uterus in place.
- Medicine. Your doctor may give you medicine to help with endometriosis. Over-the-counter pain medicines taken during your period also may help with pain and bleeding. Hormonal birth control, such as the pill, shot, or vaginal ring, or a hormonal intrauterine device (IUD) may help with irregular or heavy vaginal bleeding or periods that last longer than usual.
- Vaginal pessary (for uterine prolapse). A pessary is a rubber or plastic donut-shaped object, similar to a diaphragm used for birth control. The pessary is inserted into the vagina to hold the uterus in place. Uterine prolapse happens when the uterus drops or “falls out” because it loses support after childbirth or pelvic surgery.
- Surgery. You and your doctor may choose to try a surgery that involves smaller or fewer cuts than hysterectomy. The smaller cuts may help you heal faster with less scarring. Depending on your symptoms, these options may include:
- Surgery to treat endometriosis. Laparoscopic surgery uses a thin, lighted tube with a small camera. The doctor puts the camera and surgery tools into your pelvic area through very small cuts. This surgery can remove scar tissue or growths from endometriosis without harming the surrounding healthy organs such as ovaries. You may still get pregnant after this surgery.
- Surgery to help stop heavy or long-term vaginal bleeding.
- Dilation and curettage (D&C) removes the lining of the uterus that builds up every month before your period. Often, a hysteroscopy is done at the same time. Your doctor inserts the hysteroscope (a thin telescope) into your uterus to see the inside of the uterine cavity. D&C may also remove noncancerous growths or polyps from the uterus. After the D&C, a new uterine lining will build up during your next menstrual cycle as usual. You may still get pregnant after this surgery.
- Endometrial ablation destroys the lining of the uterus permanently. Depending on the size and condition of your uterus, your doctor may use tools that freeze, heat, or use microwave energy to destroy the uterine lining. This surgery should not be used if you still want to become pregnant or if you have gone through menopause.
- Surgery to remove uterine fibroids without removing the uterus. This is called a myomectomy. Depending on the location of your fibroids, the myomectomy can be done through the pelvic area or through the vagina and cervix. You may be able to get pregnant after this surgery. If your doctor recommends this surgery, ask your doctor if a power morecellator will be used. The FDA has warned against the use of power morcellators for most women.
- Surgery to shrink fibroids without removing the uterus. This is called myolysis. The surgeon heats the fibroids, which causes them to shrink and die. Myolysis may be done laparoscopically (through very small cuts in the pelvic area). You may still get pregnant after myolysis.
- Treatments to shrink fibroids without surgery. These treatments include uterine artery embolization (UAE) and magnetic resonance (MR)-guided focused ultrasound (MR[f]US). Uterine artery embolization (UAE) puts tiny plastic or gel particles into the vessels supplying blood to the fibroid. Once the blood supply is blocked, the fibroid shrinks and dies. MR(f)US sends ultrasound waves to the fibroids that heat and shrink the fibroids. After uterine artery embolization (UAE) or magnetic resonance (MR)-guided focused ultrasound (MR[f]US), you will not be able to get pregnant.
The female reproductive system
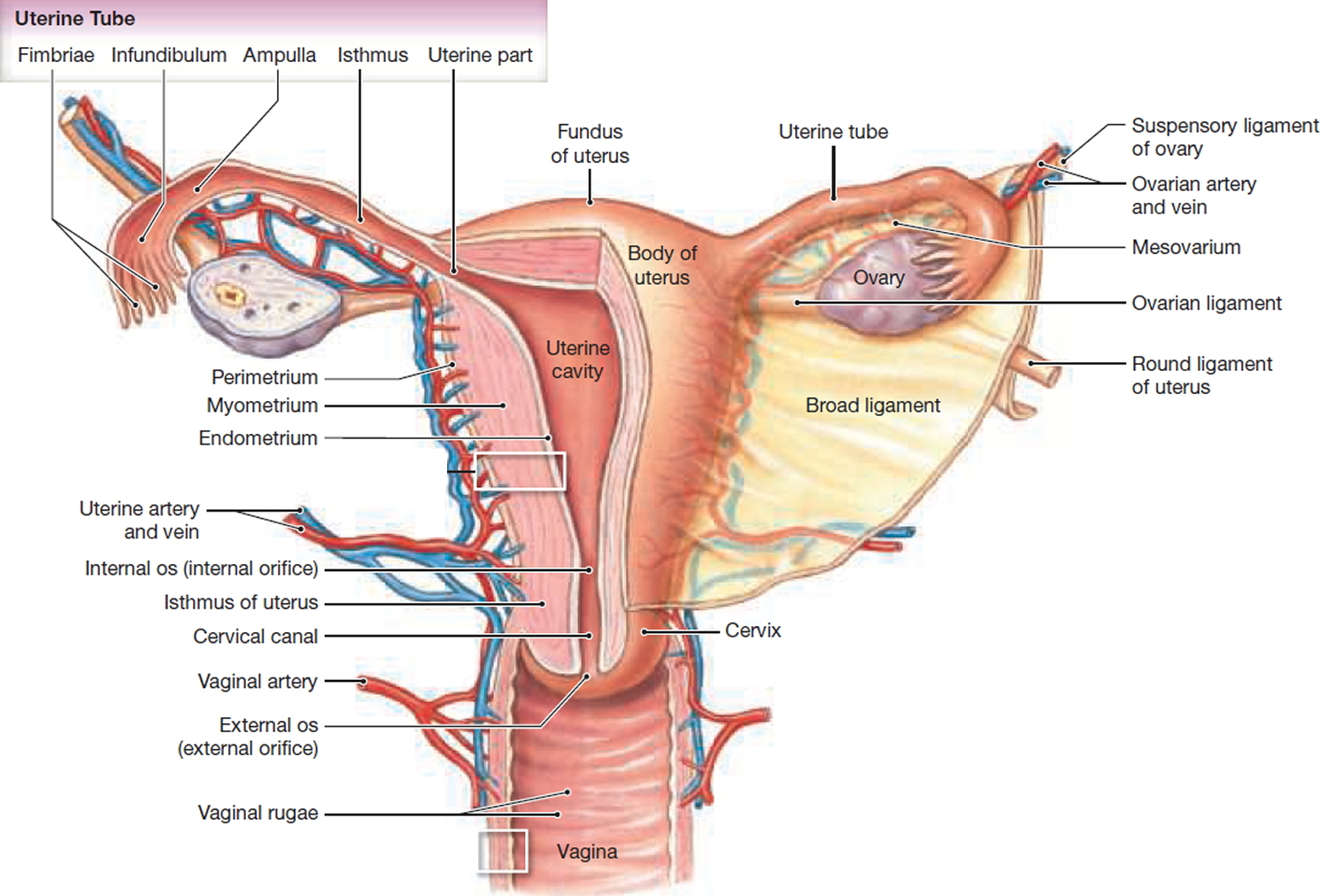
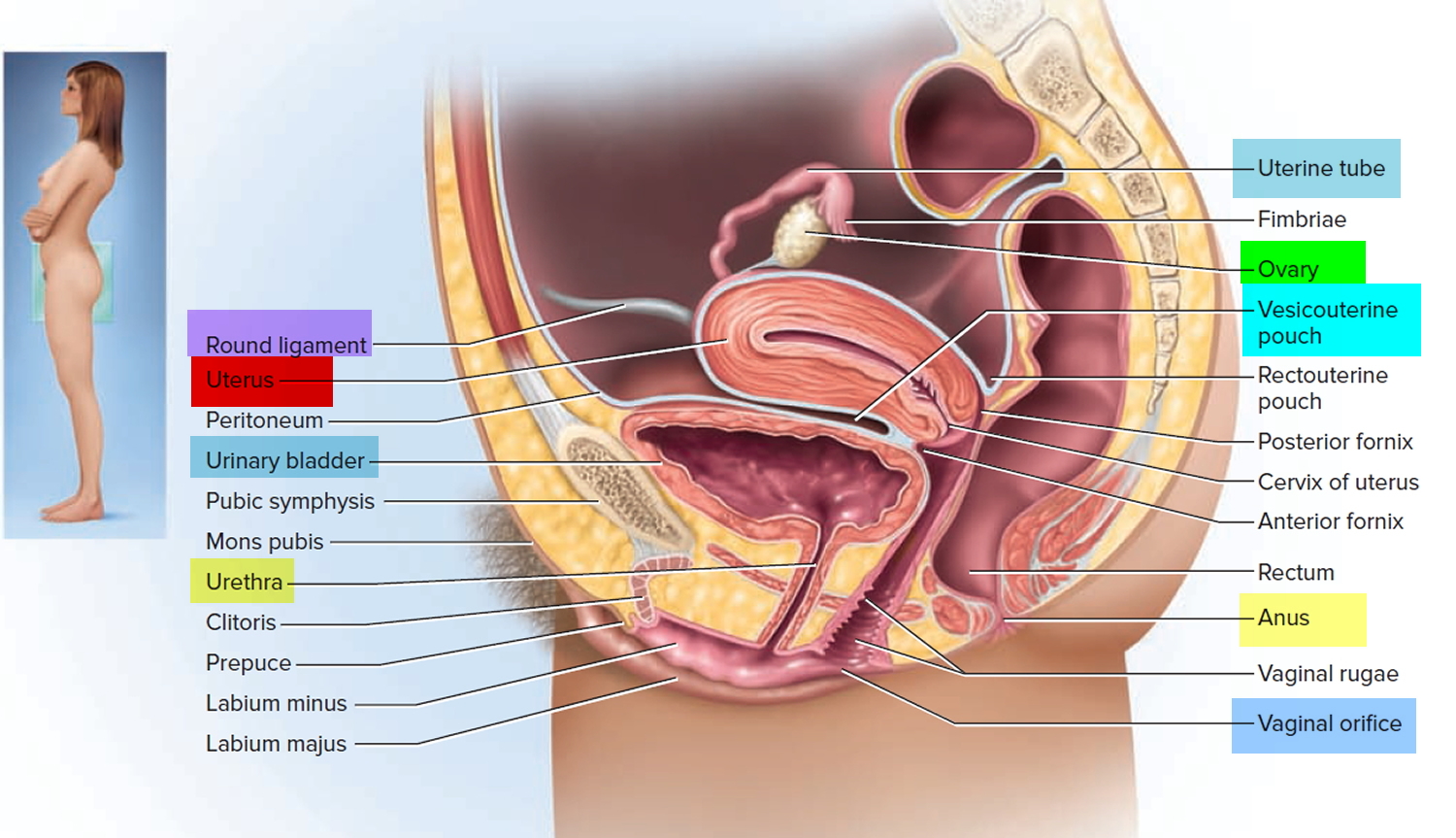
The female reproductive system is made up of the:
- womb (uterus) – a pear-shaped organ in the middle of your pelvis where a baby develops; the lining of the womb is shed during a period
- cervix – the neck of the womb, where the womb meets the vagina; the cervix is the lower part of the womb and not separate
- vagina – a muscular tube below the cervix
- fallopian tubes – tubes that connect the womb to the ovaries
- ovaries – small organs by the fallopian tubes that release an egg each month
Figure 1. Uterus anatomy
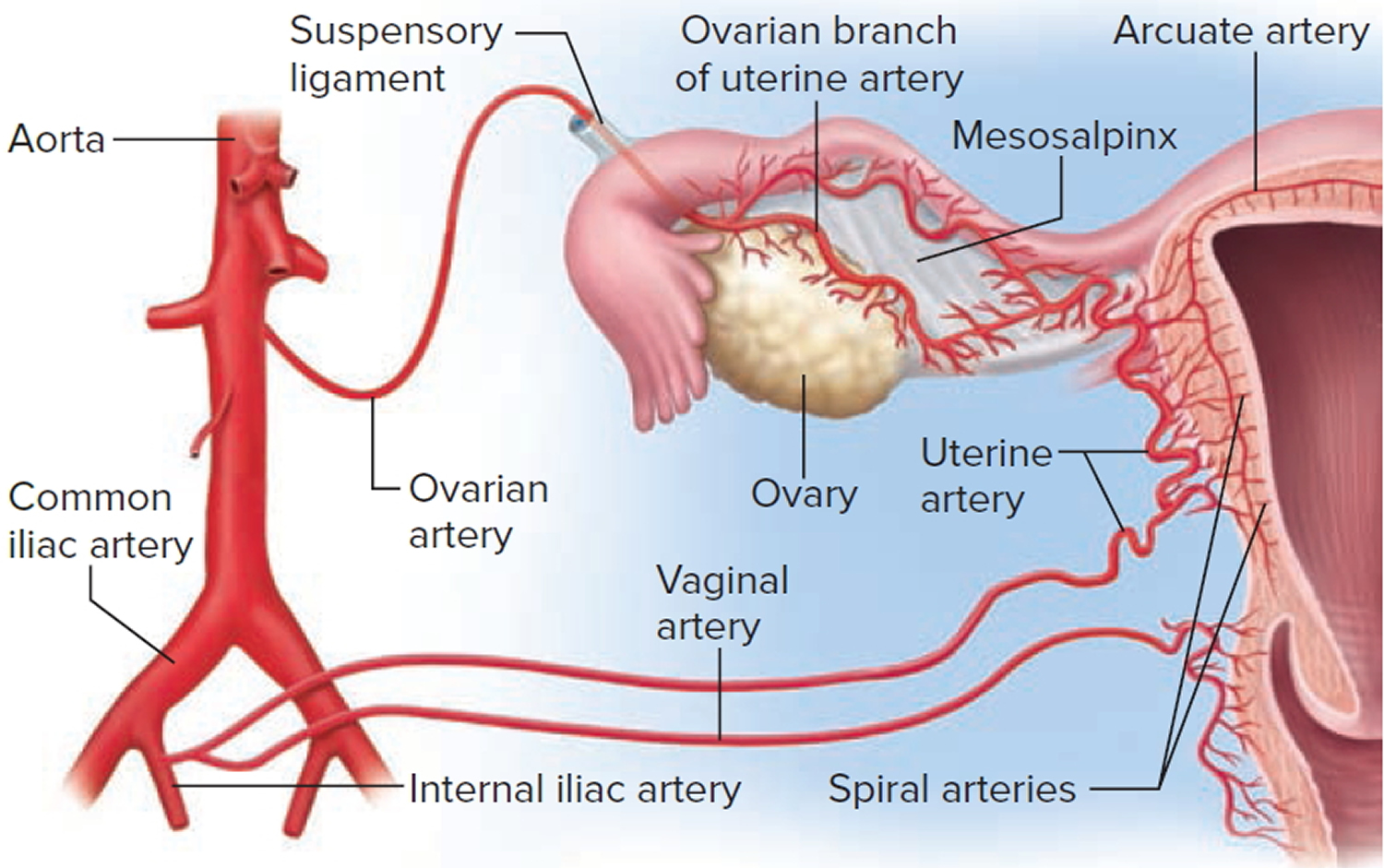
Figure 2. Blood supply to the uterus
Figure 3. Uterus location
Hysterectomy types
There are various types of hysterectomy. The type you have depends on why you need the operation and how much of your womb and surrounding reproductive system can safely be left in place.
The main types of hysterectomy are:
- Total hysterectomy – the womb and cervix (neck of the womb) are removed; this is the most common type of hysterectomy.
- Partial hysterectomy (subtotal hysterectomy or supracervical hysterectomy) – the main body of the womb is removed, leaving the cervix in place – this is a less common operation.
- Total hysterectomy with bilateral salpingo-oophorectomy – the womb, cervix, fallopian tubes (salpingectomy) and the ovaries (oophorectomy) are removed
- Radical hysterectomy – the womb and surrounding tissues are removed, including the fallopian tubes, part of the vagina, ovaries, lymph glands and fatty tissue
Figure 4. Types of hysterectomy
There are three ways to carry out a hysterectomy:
- Vaginal hysterectomy – where the womb is removed through a cut in the top of the vagina
- Abdominal hysterectomy – where the womb is removed through a cut in the lower abdomen
- Laparoscopic hysterectomy (keyhole surgery) – where the womb is removed through several small cuts in the abdomen
It is important that you are clear about the type of hysterectomy that might be performed, and whether the ovaries or fallopian tubes are to be removed as well.
The type of hysterectomy and whether the ovaries or fallopian tubes are removed will depend on your personal circumstances and will be discussed with you by your gynecologist before your operation.
Total hysterectomy
During a total hysterectomy, your womb and cervix (neck of the womb) is removed. A total hysterectomy is usually the preferred option over a subtotal hysterectomy, because removing the cervix means there’s no risk of you developing cervical cancer at a later date.
Partial or Subtotal hysterectomy
A partial or subtotal hysterectomy involves removing the main body of the womb and leaving the cervix in place.
This procedure isn’t performed very often. If the cervix is left in place, there’s still a risk of cervical cancer developing and regular cervical screening will still be needed.
Some women want to keep as much of their reproductive system as possible, including their cervix. If you feel this way, talk to your surgeon about any risks associated with keeping your cervix.
Total hysterectomy with bilateral salpingo-oophorectomy
A total hysterectomy with bilateral salpingo-oophorectomy is a hysterectomy that also involves removing:
- the fallopian tubes (salpingectomy)
- the ovaries (oophorectomy)
The National Institute for Health and Care Excellence (NICE) recommends that the ovaries should only be removed if there’s a significant risk of further problems – for example, if there’s a family history of ovarian cancer.
Your surgeon can discuss the pros and cons of removing your ovaries with you.
Radical hysterectomy (removal of the cervix + uterus + part of the vagina + ovaries + lymph glands and fatty tissue)
If you have cancer of the cervix, ovarian cancer or womb (uterus) cancer, you may be advised to have your cervix removed to stop the cancer spreading.
- A radical hysterectomy is usually carried out to remove and treat cancer when other treatments such as chemotherapy and radiotherapy aren’t suitable or haven’t worked.
Even if you don’t have cancer, removing the cervix means there’s no risk of developing cervical cancer in the future.
Many women are concerned that removing the cervix will lead to a loss in sexual function, but there’s no evidence to support this.
Some women are reluctant to have their cervix removed because they want to retain as much of their reproductive system as possible. If you feel this way, ask your surgeon whether there are any risks associated with keeping your cervix.
If you have your cervix removed, you’ll no longer need to have cervical screening tests. If you don’t have your cervix removed, you’ll need to continue having regular screening for cervical cancer (cervical smears).
During the radical hysterectomy procedure, the body of your womb and cervix is removed, along with:
- your fallopian tubes
- part of your vagina
- ovaries
- lymph glands
- fatty tissue
Removal of the ovaries (salpingo-oophorectomy)
The National Institute for Health and Care Excellence (NICE) recommends that a woman’s ovaries should only be removed if there’s a significant risk of associated disease, such as ovarian cancer.
If you have a family history of ovarian or breast cancer, removing your ovaries (an oophorectomy) may be recommended to prevent cancer occurring in the future.
Your surgeon can discuss the pros and cons of removing your ovaries with you. If your ovaries are removed, your fallopian tubes will also be removed.
If you’ve already gone through the menopause or you’re close to it, removing your ovaries may be recommended regardless of the reason for having a hysterectomy. This is to protect against the possibility of ovarian cancer developing.
Some surgeons feel it’s best to leave healthy ovaries in place if the risk of ovarian cancer is small – for example, if there’s no family history of the condition.
This is because the ovaries produce several female hormones that can help protect against conditions such as osteoporosis (weak and brittle bones). They also play a part in feelings of sexual desire and pleasure.
If you would prefer to keep your ovaries, make sure you’ve made this clear to your surgeon before your operation. You may still be asked to give consent to treatment in regards to having your ovaries removed if an abnormality is found during the operation.
Think carefully about this and discuss any fears or concerns that you have with your surgeon.
Reasons for hysterectomy
A hysterectomy is a major operation for a woman that’s only recommended if other treatment options have been unsuccessful.
The most common reasons for having a hysterectomy include:
- Uterine fibroids. Many hysterectomies are done to permanently treat uterine fibroids — benign tumors in your uterus that can cause persistent bleeding, anemia, pelvic pain, pain during intercourse and bladder pressure. If you have large uterine fibroids, you may need an abdominal hysterectomy — surgery that removes your uterus through an incision in your lower abdomen. Nonsurgical treatments of uterine fibroids are a possibility, depending on your discomfort level and tumor size. Many women with fibroids have minimal symptoms and require no treatment.
- Endometriosis. In endometriosis, the tissue lining the inside of your uterus (endometrium) grows outside the uterus on your ovaries, fallopian tubes, or other pelvic or abdominal organs. When medication or conservative surgery doesn’t improve endometriosis, you might need a hysterectomy along with removal of your ovaries and fallopian tubes (bilateral salpingo-oophorectomy). Most women with endometriosis have an abdominal hysterectomy, but sometimes a vaginal hysterectomy is possible.
- Gynecologic cancer (e.g., ovarian cancer, uterine cancer, cervical cancer or cancer of the fallopian tubes). If you have cancer of the uterus, cervix, endometrium or ovaries, your doctor may recommend a hysterectomy to treat it. Most of the time, an abdominal hysterectomy is done during treatment for ovarian cancer, but sometimes vaginal hysterectomy may be appropriate for women with cervical cancer or endometrial cancer. And depending on the specific cancer you have and how advanced it is, your other treatment options might include radiation or chemotherapy.
- Uterine prolapse. When pelvic supporting tissues and ligaments get stretched out or weak, the uterus can lower or sag into the vagina, causing urinary incontinence, pelvic pressure or difficulty with bowel movements. Removing the uterus with hysterectomy and repairing pelvic relaxation may relieve those symptoms.
- Abnormal vaginal bleeding. When medication or a less invasive surgical procedure doesn’t control irregular, heavy or very long periods, hysterectomy can solve the problem.
- Chronic pelvic pain. If you have chronic pelvic pain clearly caused by a uterine condition, hysterectomy may help, but only as a last resort. Chronic pelvic pain can have several causes, so an accurate diagnosis of the cause is critical before having a hysterectomy for pelvic pain. However, a hysterectomy provides no relief from many forms of pelvic pain, and an unnecessary hysterectomy may create new problems. Seek careful evaluation before proceeding with such major surgery.
For most of these conditions — with the possible exception of cancer — hysterectomy is just one of several treatment options. You may not even need to consider hysterectomy if your doctor recommends hormonal medications or other less invasive gynecologic procedures that are successful in managing your symptoms.
You cannot become pregnant after you’ve had a hysterectomy. If you’re less than completely sure that you’re ready to give up your fertility, explore other treatments.
Heavy periods
Many women lose a large amount of blood during their monthly periods. They may also experience other symptoms, such as pain and stomach cramps.
For some women, the symptoms can have a significant impact on their quality of life. Sometimes heavy periods can be caused by uterine fibroids, but in many cases there’s no obvious cause.
In some cases, removing the womb may be the only way of stopping persistent heavy menstrual bleeding when:
- other treatments haven’t worked
- the bleeding has a significant impact on quality of life and it’s preferable for periods to stop
- the woman no longer wishes to have children
Pelvic inflammatory disease (PID)
Pelvic inflammatory disease (PID) is a bacterial infection of the female reproductive system.
If detected early, the infection can be treated with antibiotics. However, if it spreads, it can damage the womb and fallopian tubes, resulting in long-term pain.
A hysterectomy to remove the womb and fallopian tubes may be recommended if a woman has severe pain from pelvic inflammatory disease (PID) and no longer wants children.
Endometriosis
Endometriosis is a condition where cells that line the womb are also found in other areas of the body and reproductive system, such as the ovaries, fallopian tubes, bladder and rectum.
If the cells that make up the lining of the womb become trapped in other areas of the body, it can cause the surrounding tissue to become inflamed and damaged. This can lead to pain, heavy and irregular periods, and infertility.
A hysterectomy may remove the areas of endometrial tissue causing the pain. However, it will usually only be considered if other less invasive treatments haven’t worked and the woman decides not to have any more children.
Uterine fibroids
Uterine fibroids are non-cancerous tumors that grow in or around the womb (uterus). The growths are made up of muscle and fibrous tissue, and vary in size.
The symptoms of fibroids can include:
- heavy or painful periods
- pelvic pain
- frequent urination or constipation
- pain or discomfort during sex
A hysterectomy may be recommended if you have large fibroids or severe bleeding and you don’t want to have any more children.
Adenomyosis
Adenomyosis is a common condition where the tissue that normally lines the womb starts to grow within the muscular wall of the womb. This extra tissue can make your periods particularly painful and cause pelvic pain.
A hysterectomy can cure adenomyosis, but will only be considered if all other treatments have failed and you don’t want to have any more children.
Prolapse of the uterus
A prolapsed uterus happens when the tissues and ligaments that support the womb become weak, causing it to drop down from its normal position.
Symptoms can include:
- back pain
- a feeling that something is coming down out of your vagina
- leaking urine (urinary incontinence)
- difficulty having sex
A prolapsed uterus can often occur as a result of childbirth.
A hysterectomy resolves the symptoms of a prolapse because it removes the entire womb. It may be recommended if the tissues and ligaments that support the womb are severely weakened and the woman doesn’t want any more children.
Gynecologic cancer
A hysterectomy may be recommended for the following cancers:
- cervical cancer
- ovarian cancer
- cancer of the fallopian tubes
- cancer of the womb (uterus)
If the cancer has spread and reached an advanced stage, a hysterectomy may be the only possible treatment option.
Deciding to have a hysterectomy
If you have cancer, a hysterectomy may be the only treatment option. For other conditions, it’s a good idea to ask yourself the questions listed below before deciding to have the procedure.
- Are my symptoms seriously affecting my quality of life?
- Have I explored all other alternative treatment options?
- Am I prepared for the possibility of an early menopause?
- Do I still want to have children?
Don’t be afraid to ask your doctor as many questions as you want.
How you prepare for a hysterectomy
It’s normal to feel anxious about having a hysterectomy. Talk with your doctor about what to expect during and after a hysterectomy, including physical and emotional effects.
Here’s what you can do to prepare:
- Gather information. Before the surgery, get all the information you need to feel confident about it. Ask your doctor and surgeon questions. Learn about the procedure, including all the steps involved if it makes you feel more comfortable.
- Follow your doctor’s instructions about medication. Find out whether you should change your usual medication routine in the days leading up to your hysterectomy. Be sure to tell your doctor about any over-the-counter medications, dietary supplements or herbal preparations that you’re taking.
- Discuss what type of anesthesia you’ll have. You may prefer general anesthesia, which makes you unconscious during surgery, but regional anesthesia — also called spinal block or epidural block — may be an option. If you’re having a vaginal hysterectomy, regional anesthesia will block the sensation in the lower half of your body.
- Plan for a hospital stay. How long you’ll be in the hospital depends on what type of hysterectomy you have and what your doctor recommends. Generally, abdominal hysterectomy requires a hospital stay of at least one to two days.
- Arrange for help. Although you’re likely to recover sooner after a vaginal hysterectomy than after an abdominal one, it still takes time. Ask someone to help you out at home for the first week or so. Full recovery could take several weeks. Your doctor may recommend restricting your activities during your recovery, such as avoiding driving or lifting heavy objects. Arrange for help at home if you think you’ll need it.
If you need to have a hysterectomy, it’s important to be as fit and healthy as possible.
Good health before your operation will reduce your risk of developing complications and speed up your recovery.
As soon as you know you’re going to have a hysterectomy, take the following steps:
- stop smoking
- eat a healthy, balanced diet
- exercise regularly
- lose weight (if you are overweight)
Before the hysterectomy procedure
Before surgery, you may have tests done to check for cancer, which could change your surgeon’s approach to surgery. Tests may include:
- Cervical cytology (Pap test), which detects the presence of abnormal cervical cells or cervical cancer
- Endometrial biopsy, which detects abnormal cells in the uterine lining or endometrial cancer
- Pelvic ultrasound, which may show the size of uterine fibroids, endometrial polyps or ovarian cysts
The day before and morning of your surgery, you will be instructed to shower using soap provided by your surgeon to reduce your risk of infection. A preoperative cleansing of your vagina (vaginal douche) or preoperative cleansing of your rectum (enema) also may be done. Immediately before surgery, you’ll receive an intravenous antibiotic medication to minimize your risk of infection after the procedure.
What you can expect during the hysterectomy procedure
You may have general anesthesia, so you won’t be awake for the surgery. Alternatively, you may choose a spinal block (regional anesthesia) with a medication that makes you drowsy, or you may remain awake during your surgery. The hysterectomy procedure itself generally lasts about one to two hours, although you’ll spend some time beforehand getting ready to go into the operating room.
You’ll lie on your back, in a position similar to the one you’re in for a Pap test. To begin the procedure, a member of your surgical team passes a urinary catheter through your urethra to empty your bladder. The catheter remains in place during surgery and for a short time afterward. Your abdomen and vagina are cleaned with a sterile solution before surgery.
Performing a hysterectomy
There are three ways a hysterectomy can be performed. These are:
- vaginal hysterectomy
- abdominal hysterectomy
- laparoscopic hysterectomy
Vaginal hysterectomy
Vaginal hysterectomy is a surgical procedure to remove the uterus through the vagina. During a vaginal hysterectomy, the womb and cervix are removed through an incision that’s made in the top of the vagina. During a vaginal hysterectomy, the surgeon detaches the uterus from the ovaries, fallopian tubes and upper vagina, as well as from the blood vessels and connective tissue that support it. The uterus is then removed through the vagina. The operation usually takes about an hour to complete.
Vaginal hysterectomy involves a shorter time in the hospital, lower cost and faster recovery than an abdominal hysterectomy, which requires an incision in your lower abdomen. However, if your uterus is enlarged, vaginal hysterectomy may not be possible and your doctor will talk to you about other surgical options, such as an abdominal hysterectomy.
A vaginal hysterectomy can either be carried out using:
- general anaesthetic – where you’ll be unconscious during the procedure
- local anaesthetic – where you’ll be awake, but won’t feel any pain
- spinal anaesthetic – where you’ll be numb from the waist down
A vaginal hysterectomy is usually preferred over an abdominal hysterectomy, because it’s less invasive and involves a shorter stay in hospital. The recovery time also tends to be quicker.
To perform the vaginal hysterectomy
- Your surgeon makes an incision inside your vagina to get to the uterus
- Using long instruments, your surgeon clamps the uterine blood vessels and separates your uterus from the connective tissue, ovaries and fallopian tubes
- Your uterus is removed through the vaginal opening, and absorbable stitches are used to control any bleeding inside the pelvis
Except in cases of suspected uterine cancer, the surgeon may cut an enlarged uterus into smaller pieces and remove it in sections (morcellation).
Laparoscopic or robotic assisted vaginal hysterectomy
You may be a candidate for a laparoscopically assisted vaginal hysterectomy or robotic hysterectomy. Both procedures allow your surgeon to remove the uterus vaginally while being able to see your pelvic organs through a laparoscope, a slender viewing instrument.
Your surgeon performs most of the procedure through small abdominal incisions aided by long, thin surgical instruments inserted through the incisions. Your surgeon then removes the uterus through an incision made in your vagina.
Your surgeon might recommend laparoscopically assisted vaginal hysterectomy or robotic hysterectomy if you have scar tissue (pelvic adhesions) on your pelvic organs from prior surgeries or from endometriosis.
Abdominal hysterectomy
An abdominal hysterectomy is a surgical procedure that removes your uterus through an incision in your lower abdomen. Your uterus — or womb — is where a baby grows if you’re pregnant. A partial hysterectomy removes just the uterus, leaving the cervix intact. A total hysterectomy removes the uterus and the cervix.
Sometimes a hysterectomy includes removal of one or both ovaries and fallopian tubes, a procedure called a total hysterectomy with salpingo-oophorectomy.
An abdominal hysterectomy may be recommended if your womb is enlarged by fibroids or pelvic tumors and it’s not possible to remove it through your vagina.
It may also be recommended if your ovaries need to be removed.
An abdominal hysterectomy may be recommended over other types of hysterectomy if:
- You have a large uterus.
- Your doctor wants to check other pelvic organs for signs of disease.
- Your surgeon feels it’s in your best interest to have an abdominal hysterectomy.
During an abdominal hysterectomy, an incision will be made in your abdomen (tummy). It will either be made horizontally along your bikini line, or vertically from your belly button to your bikini line.
After your womb has been removed, the incision is stitched up. The operation takes about an hour to perform and a general anaesthetic is used.
To perform the abdominal hysterectomy
Your surgeon makes a cut (incision) in your lower abdomen, using one of two approaches:
- A vertical incision, which starts in the middle of your abdomen and extends from just below your navel to just above your pubic bone. A vertical incision will usually be used if there are large fibroids (non-cancerous growths) in your womb, or for some types of cancer.
- A horizontal bikini-line incision, which lies about an inch above your pubic bone
The type of incision depends on many factors, including the reason for your hysterectomy, the need to explore the upper abdomen, the size of your uterus and the presence of any scars from prior abdominal surgeries. For instance, hysterectomies performed for endometriosis, large fibroids and gynecologic cancers are done mainly through a vertical incision.
Laparoscopic hysterectomy
Laparoscopic surgery is also known as keyhole surgery. Nowadays, a laparoscopic hysterectomy is the preferred treatment method for removing the organs and surrounding tissues of the reproductive system. Laparoscopic hysterectomies are usually carried out under general anaesthetic.
During the procedure, a small tube containing a telescope (laparoscope) and a tiny video camera will be inserted through a small incision in your abdomen. Laparoscopic hysterectomy is performed under the guidance of a special camera passed through a ‘keyhole’ in the abdomen, and with other instruments passed through separate ‘keyholes.’ The uterus is most commonly removed through the vagina, although sometimes it might be removed in small pieces (‘morcellated’) through the keyholes. In some cases, the entire operation is performed through the keyholes (‘total laparoscopic hysterectomy’). In other cases, part of the operation is done as a vaginal hysterectomy (this procedure is known as a ‘laparoscopically-assisted hysterectomy.’).
Hysterectomy recovery
After surgery, you’ll be in a recovery room for a few hours and in the hospital for one to two days, possibly longer.
Your health care team will:
- Monitor you for signs of pain
- Give you medicine for pain and to prevent infection
- Encourage you to get up and walk around soon after surgery.
An abdominal hysterectomy usually requires a hospital stay of one to two days, but it could be longer. You’ll need to use sanitary pads for vaginal bleeding and discharge. It’s normal to have bloody vaginal drainage for several days to weeks after a hysterectomy. However, let your surgeon know if you have bleeding that’s as heavy as a menstrual period or bleeding that’s persistent.
The abdominal incision will gradually heal, but a visible scar on your abdomen will remain.
It’s normal to have bloody vaginal discharge for several days to weeks after a hysterectomy, so you’ll need to wear sanitary pads.
- After a hysterectomy, you’ll no longer have periods or be able to get pregnant.
- If you had your ovaries removed, you’ll begin menopause immediately after surgery. You may experience symptoms such as vaginal dryness, hot flashes and night sweats. Your doctor can recommend medications for these symptoms, if you need treatment.
- If your ovaries weren’t removed during surgery — and you still had periods before your surgery — your ovaries continue producing hormones and eggs until you reach menopause.
Length of hospital stay
In most cases you will be admitted to hospital on the day of your operation. The length of time it will take before you’re well enough to leave hospital depends on your age and your general level of health.
If you’ve had a vaginal or laparoscopic hysterectomy, you may be able to leave between one and four days later. If you’ve had an abdominal hysterectomy, it will usually be up to five days before you’re discharged.
Most women can go home from hospital within a couple of days of hysterectomy, depending on the type of hysterectomy, and whether other procedures were performed at the same time (for example, a vaginal operation to repair prolapse). For laparoscopic and vaginal hysterectomies, there is usually little or no pain within a week.
Anaesthesia and pain relief
The anaesthetist will provide the most appropriate form of anaesthesia suited to you during the operation. After a hysterectomy you can expect pain and discomfort for a few days but this can usually be managed well with medications. The anaesthetist will provide you with a number of options to help control your pain. Taking regular pain relief is very important to your recovery and will enable you to get out of bed sooner and walk around. This will help speed up your recovery and reduce the risks of thrombosis.
Urinary catheter
After your operation you may have a catheter (tube) in your bladder to drain urine until you are able to walk to the toilet. This may stay in for up to 24 hours after your operation. If you have difficulty passing urine, the catheter may need to stay in for a few days.
Care of your wound
If you have had an abdominal or laparoscopic hysterectomy, you will have a cut(s) on your abdomen. Your wound will be closed by stitches, staples or glue. Some stitches and glue dissolve by themselves. Staples, and some types of stitches will need to be removed. This usually occurs either prior to discharge from hospital, or by your gynecologist, general practitioner or district nurse five to seven days after your operation. Your incision will be covered by a dressing which the nurses will often remove before you leave hospital. If this cannot be done before discharge, they will talk to you about how to care for it. Keep your wound clean and dry. Wear loose clothing and look for signs of infection (such as redness, pain, swelling of the wound or bad smelling discharge). Report these to your doctor or nurse. If you have had a vaginal hysterectomy, any stitches within your vagina will be dissolvable and will not need to be removed. You may notice stitches coming away after a few weeks. This is normal and nothing to worry about.
Bleeding after hysterectomy
It is normal to experience some vaginal bleeding for one to two weeks after your hysterectomy, like a light period, as the stitches (sutures) dissolve and the tissue heals. You’ll likely need to wear sanitary pads during that time.
Generally, vaginal bleeding after hysterectomy should be light. You may notice occasional spotting or a pink discharge. If bleeding after hysterectomy is as heavy as a menstrual period or lasts longer than six weeks, consult your doctor for an evaluation.
Some women have no initial bleeding at all but will then experience a gush of old blood or fluid after a week. This will usually stop quickly. You should use sanitary pads rather than tampons to reduce the chance of infection. Any heavy bleeding should be reported to your doctor.
Activity
It is important to be as active as possible, but to get adequate rest if tired. It is also important to avoid dehydration, so drinking enough fluid is advisable. To avoid the complication of hernia (a weakness in the incision), women should not do heavy lifting or straining for four to six weeks. Depending on the type of hysterectomy, and the type of work a woman does, it might be usual to need between two and six weeks away from work. This can be discussed with your gynecologist.
Hysterectomy recovery time
For healthy women who have a hysterectomy that goes well, recovery is often complete within two to six weeks. Your own recovery will depend on a number of things:
- Your health and fitness before the operation
- The reasons for having a hysterectomy
- The type of hysterectomy you have – when an incision is made on the abdomen, recovery often takes a couple of weeks more.
- If the operation is more complex or has any complications, recovery may be slower.
It takes time to get back to your usual self after an abdominal hysterectomy — about six weeks for most women. During that time:
- Get plenty of rest.
- Don’t lift anything heavy for a full six weeks after the operation.
- Stay active after your surgery, but avoid strenuous physical activity for the first six weeks.
- Wait six weeks to resume sexual activity.
- Follow your doctor’s recommendations about returning to your other normal activities.
What to expect after a hysterectomy
Life after a hysterectomy
A hysterectomy permanently changes some aspects of your life. For instance:
- You’ll no longer have menstrual periods.
- Most of the time, you’ll get relief from the symptoms that made your surgery necessary.
- You won’t be able to become pregnant.
- If you’re premenopausal, having your ovaries removed along with a hysterectomy starts menopause.
- If you have a hysterectomy before menopause and you remove your ovaries, you may experience menopause at a younger than average age.
- If you have a partial hysterectomy, your cervix remains in place, so you’re still at risk of cervical cancer. You need regular Pap tests to screen for cervical cancer.
Other parts of your life will likely return to normal or perhaps improve once you’ve recovered from your hysterectomy. For example:
- If you had a good sex life before a hysterectomy, chances are you’ll maintain it afterward. Some women even experience more sexual pleasure after a hysterectomy. This may be due to relief from the chronic pain or heavy bleeding that was caused by a uterine problem.
- The relief of symptoms may greatly enhance your quality of life. You may have an improved sense of well-being and a chance to get on with your life.
On the other hand, you may feel a sense of loss after hysterectomy. Premenopausal women who must have a hysterectomy to treat gynecologic cancer may experience grief and possibly depression over the loss of fertility. If sadness or negative feelings begin to interfere with your enjoyment of everyday life, talk with your doctor.
How you’ll feel physically
Recovery after vaginal hysterectomy is shorter and less painful than after an abdominal hysterectomy. A full recovery may take three to four weeks.
Even if you feel like you’re back to normal, don’t lift anything heavy — more than 20 pounds (9.1 kilograms) — or have vaginal intercourse until six weeks after surgery.
Contact your doctor if pain worsens or if you develop nausea, vomiting or bleeding that’s heavier than a menstrual period.
How you’ll feel emotionally
After a hysterectomy, you may have an improved mood and increased sense of well-being. You may be relieved to no longer experience signs and symptoms such as heavy bleeding or pelvic pain.
For most women, there’s no change in sexual function after hysterectomy. But for some women, heightened sexual satisfaction occurs after hysterectomy — perhaps because they no longer fear becoming pregnant or no longer have pain during intercourse.
You may feel a sense of loss and grief after hysterectomy, which is normal. Or you may experience depression related to the loss of your fertility, especially if you’re young and hoped for a future pregnancy.
If sadness or negative feelings begin to interfere with your enjoyment of everyday life, talk to your doctor.
Getting back to normal
Returning to work
How long it will take for you to return to work depends on how you feel and what sort of work you do.
If your job doesn’t involve manual work or heavy lifting, it may be possible to return after four to eight weeks.
Driving
Don’t drive until you’re comfortable wearing a seatbelt and can safely perform an emergency stop.
This can be anything from three to eight weeks after your operation. You may want to check with your doctor that you are fit to drive before you start.
Some car insurance companies require a certificate from a doctor stating that you’re fit to drive. Check this with your car insurance company.
Exercise and lifting
After a hysterectomy, the hospital where you were treated should give you information and advice about suitable forms of exercise while you recover.
Walking is always recommended, and you can swim after your wounds have healed. Don’t try to do too much, because you’ll probably feel more tired than usual.
Don’t lift any heavy objects during your recovery period. If you have to lift light objects, make sure your knees are bent and your back is straight.
Sex
After a hysterectomy, it’s generally recommended that you don’t have sex until your scars have healed and any vaginal discharge has stopped, which usually takes at least four to six weeks. As long as you’re comfortable and relaxed, it’s safe to have sex.
You may experience some vaginal dryness, particularly if you’ve had your ovaries removed and you’re not taking HRT.
Many women also experience an initial loss of sexual desire (libido) after the operation, but this usually returns once they’ve fully recovered.
At this point, studies show that pain during sex is reduced and that strength of orgasm, libido and sexual activity all improve after a hysterectomy.
Contraception
You no longer need to use contraception to prevent pregnancy after having a hysterectomy. However, you’ll still need to use condoms to protect yourself against sexually transmitted infections (STIs).
Surgical menopause
If you have a total or radical hysterectomy that removes your ovaries, you’ll experience the menopause immediately after your operation, regardless of your age. This is known as a surgical menopause.
If a hysterectomy leaves one or both of your ovaries intact, there’s a chance that you’ll experience the menopause within five years of having the operation.
Although your hormone levels decrease after the menopause, your ovaries continue producing testosterone for up to 20 years. Testosterone is a hormone that plays an important part in stimulating sexual desire and sexual pleasure.
Your ovaries also continue to produce small amounts of the hormone oestrogen after the menopause. It’s a lack of oestrogen that causes menopausal symptoms such as:
- hot flushes
- depression
- vaginal dryness
- insomnia (sleep problems)
- fatigue
- night sweats
Hormone replacement therapy (HRT) is usually used to help with menopausal symptoms that occur after a hysterectomy.
Hormone replacement therapy (HRT)
You may be offered HRT after having your ovaries removed. This replaces some of the hormones your ovaries used to produce and relieves any menopausal symptoms you may have.
It’s unlikely that the HRT you’re offered will exactly match the hormones your ovaries previously produced.
The amount of hormones a woman produces can vary greatly, and you may need to try different doses and brands of HRT before you find one that feels suitable.
Not everyone is suitable for HRT. For example, it’s not recommended for women who have had a hormone-dependent type of breast cancer or liver disease. It’s important to let your surgeon know about any such conditions that you’ve had.
If you’re able to have HRT and both of your ovaries have been removed, it’s important to continue with the treatment until you reach the normal age for the menopause (51 is the average age).
Cervical screening
If your cervix is removed during a hysterectomy, you’ll no longer need to have cervical screening.
If your cervix is left in place after having a subtotal hysterectomy, you’ll need to continue to go for regular cervical screening tests.
Hysterectomy side effects
After having a hysterectomy, you may experience some temporary side effects, as outlined below.
Bowel and bladder disturbances
After your operation, there may be some changes in your bowel and bladder functions when going to the toilet.
Some women develop urinary tract infections or constipation. Both can easily be treated. It’s recommended that you drink plenty of fluids and increase the fruit and fiber in your diet to help with your bowel and bladder movements.
For the first few bowel movements after a hysterectomy, you may need laxatives to help you avoid straining. Some people find it more comfortable to hold their abdomen to provide support while passing a stool.
Vaginal discharge
After a hysterectomy, you’ll experience some vaginal bleeding and discharge. This will be less discharge than during a period, but it may last up to six weeks.
Visit your doctor if you experience heavy vaginal bleeding, start passing blood clots, or have a strong-smelling discharge.
Menopausal symptoms
If your ovaries are removed, you’ll usually experience severe menopausal symptoms after your operation. These may include:
- hot flushes
- anxiety
- weepiness
- sweating
You may have hormone replacement therapy (HRT) after your operation. This can be given in the form of an implant, injections or tablets. It usually takes around a week before having an effect.
Emotional effects
You may feel a sense of loss and sadness after having a hysterectomy. These feelings are particularly common in women with advanced cancer, who have no other treatment option.
Some women who haven’t yet experienced the menopause may feel a sense of loss because they’re no longer able to have children. Others may feel less “womanly” than before.
In some cases, having a hysterectomy can be a trigger for depression. See your doctor if you have feelings of depression that won’t go away, as they can advise you about the available treatment options.
Talking to other women who have had a hysterectomy may help by providing emotional support and reassurance. Your doctor or the hospital staff may be able to recommend a local support group.
Potential risks or complications with hysterectomy
Although hysterectomy is generally safe, however all operations have potential risks. Every operation is different, and no two patients are alike. All surgical procedures carry a small amount of risk. Some operations will be more difficult. It is important to discuss your own individual risks with your gynecologist.
Surgical risks are higher in women who are obese or who have high blood pressure.
There is a risk of injury to other pelvic and abdominal organs during vaginal hysterectomy, including the bladder, ureters or bowel. Severe endometriosis or scar tissue (pelvic adhesions) may force your surgeon to switch from a vaginal hysterectomy to abdominal hysterectomy during the surgery.
Long term, you may also face an increased risk of heart and blood vessel (cardiovascular) diseases and certain metabolic conditions after a hysterectomy, especially if you have the surgery before age 35, according to recent research. Talk with your doctor about treatment options for your condition, to see if there are any alternatives that you might consider.
Risks associated with vaginal hysterectomy
- Heavy bleeding
- Blood clots in the legs or lungs
- Infection
- Damage to surrounding organs
- Adverse reaction to anesthesia
- Rarely, death.
Risks associated with an abdominal hysterectomy
- Blood clots
- Infection
- Excessive bleeding
- Adverse reaction to anesthesia
- Damage to your urinary tract, bladder, rectum or other pelvic structures during surgery, which may require further surgical repair
- Earlier onset of menopause even if the ovaries aren’t removed
- Rarely, death.
General anaesthetic
It’s very rare for serious complications to occur after having a general anaesthetic (1 in 10,000 anaesthetics given).
Serious complications can include nerve damage, allergic reaction and death. However, death is very rare – there’s 1 in 100,000 to 1 in 200,000 chance of dying after having a general anaesthetic.
Being fit and healthy before you have an operation reduces your risk of developing complications.
Thrombosis and embolism
Thrombosis is a clot that forms in a blood vessel, commonly known as a DVT (Deep Venous Thrombosis). It occurs in the blood vessels of the legs, but may occur elsewhere. In rare circumstances, part of the clot can break off and travel to the heart and lungs. This is called an embolism. The risk of developing thrombosis depends on the type of hysterectomy, the length of the surgery, and whether other underlying risk factors are present. Every effort is made to reduce the risk of thrombosis and embolism. For example, special stockings might be fitted during or after your surgery, and you might have injections of a blood-thinning (anticoagulant) agent. You’ll also be encouraged to start moving around as soon as possible after your operation. However, nothing will completely eliminate this risk. The risk of embolism for a healthy woman having a hysterectomy is estimated to be less than 1 in 100.
Infection
The most common infection is a urinary infection, usually associated with catheter drainage at the time of the hysterectomy. However, infection of the skin or vaginal wounds can occur. Fortunately, this happens less than 5 in 100 women. Rarely infection can gain access to the deeper tissues in the area where the uterus was removed. These aren’t usually serious and can be treated with antibiotics.
Bleeding
Most surgical procedures cause a small amount of bleeding. In some cases, bleeding can be heavier than expected and in rare cases a transfusion with blood (or blood products) may be necessary. Most commonly the excessive bleeding begins during the operation but sometimes it can begin after the hysterectomy is completed, and a collection of blood in the body wall or deeper tissues may form. Transfusion is needed in less than 1 in 100 of routine hysterectomies.
Injury to surrounding organs
The uterus and ovaries lie close to a number of important structures in the abdomen. The bladder lies to the front. The ureters – connecting the kidneys to the bladder – lie on each side of the uterus. There is bowel close to the pelvic organs. Whenever surgery is performed on the organs of the pelvis, there is a small possibility of damage to other organs. This risk depends on the complexity of the operation, and whether scarring is present from previous operations or infections. In general, the risk of an injury to the adjacent organs in the pelvis is estimated at less than 1 in 100.
Ureter damage
The ureter (the tube that urine is passed through) may be damaged during surgery, which happens in around 1% of cases. This is usually repaired during the hysterectomy.
Bladder or bowel damage
In rare cases, damage to abdominal organs such as the bladder or bowel can occur. This can cause problems such as:
- infection
- incontinence
- a frequent need to urinate
It may be possible to repair any damage during the hysterectomy. You may need a temporary catheter to drain your urine or a colostomy to collect your bowel movements.
Vaginal problems
If you have a vaginal hysterectomy, there’s a risk of problems at the top of your vagina where the cervix was removed. This could range from slow wound healing after the operation to prolapse in later years.
Ovary failure
Even if one or both of your ovaries are left intact, they could fail within five years of having your hysterectomy. This is because your ovaries receive some of their blood supply through the womb, which is removed during the operation.
Early menopause
If you’ve had your ovaries removed, you’ll usually have menopausal symptoms soon after the operation, such as:
- hot flushes
- sweating
- vaginal dryness
- disturbed sleep
This is because the menopause is triggered once you stop producing eggs from your ovaries (ovulating).
This is an important consideration if you’re under the age of 40, because early onset of the menopause can increase your risk of developing brittle bones (osteoporosis). This is because estrogen levels decrease during the menopause.
Depending on your age and circumstances, you may need to take additional medication to prevent osteoporosis.
Other potential risks
If the hysterectomy is performed as a laparoscopy, or keyhole procedure, carbon dioxide gas is used to fill the abdomen and allow access to the tissues. There is a very small possibility of this gas entering the body wall, or very rarely a blood vessel. Very rarely, the incisions may be weakened, allowing the organs of the abdomen to bulge through – this is called a hernia.
- CDC. (2010). National Hospital Discharge Survey. Procedures by selected patient characteristics – Number by procedure category and age. https://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf[↩]
- American College of Obstetricians and Gynecologists. (2013). Growing Acceptance of Removing Fallopian Tubes But Keeping Ovaries to Lower Ovarian Cancer Risk. https://www.acog.org/Patients/FAQs/Hysterectomy[↩]