Contents
- What is interstitial cystitis
- Interstitial cystitis causes
- Interstitial cystitis symptoms
- Interstitial cystitis complications
- Interstitial cystitis diagnosis
- Interstitial cystitis treatment
What is interstitial cystitis
Interstitial cystitis is also called painful bladder syndrome or urinary bladder pain syndrome, refers to a chronic, or long-lasting condition (more than 6 months duration) affecting the bladder that causes pain in your bladder and pelvic area. Symptoms of interstitial cystitis may be different from person to person. For example, some people feel mild discomfort, bladder pressure, or tenderness in the pelvic area. Other people may have intense pain in the bladder or struggle with urinary urgency, the sudden need to urinate, or frequency, the need to urinate more often.
Interstitial cystitis is common. Interstitial cystitis tends to first affect people in their 30s and 40s, and is much more common in women than men. The condition may affect between 3 million and 8 million women and between 1 million and 4 million men in the United States 1.
Interstitial cystitis usually represents a diagnosis of exclusion. There is no one test to tell if you have it. Health care professionals diagnose interstitial cystitis by ruling out other conditions with similar symptoms.
Researchers don’t know the exact cause of interstitial cystitis. Some researchers believe interstitial cystitis may result from conditions that cause inflammation in various organs and parts of the body. Traditionally, interstitial cystitis has been defined as a chronic sterile inflammatory disease of the bladder of unknown cause 2.
Interstitial cystitis can cause discomfort or pain in the bladder and a need to urinate frequently and urgently. Interstitial cystitis is far more common in women than in men. The symptoms vary from person to person. Some people may have pain without urgency or frequency. Others have urgency and frequency without pain. Women’s symptoms often get worse during their periods. They may also have pain with sexual intercourse.
Interstitial cystitis signs and symptoms include:
- Pain in your pelvis or between the vagina and anus in women
- Pain between the scrotum and anus in men (perineum)
- Chronic pelvic pain
- A persistent, urgent need to urinate
- Frequent urination, often of small amounts, throughout the day and night (up to 60 times a day)
- Pain or discomfort while the bladder fills and relief after urinating.
- Pain during sexual intercourse.
Symptoms severity is different for everyone, and some people may experience symptom-free periods.
Although signs and symptoms of interstitial cystitis may resemble those of a chronic urinary tract infection, there’s usually no infection. However, symptoms may worsen if a person with interstitial cystitis gets a urinary tract infection.
Severe interstitial cystitis symptoms can affect your quality of life. You may feel like you can’t exercise or leave your home because you have to use the bathroom too often, or perhaps your relationship is suffering because sex is painful.
Working with health care professionals, including a urologist or urogynecologist, along with a pain specialist, may help improve your interstitial cystitis symptoms.
There is no cure for interstitial cystitis, but treatments can help most people feel better. No simple treatment eliminates the signs and symptoms of interstitial cystitis, and no one treatment works for everyone. You may need to try various treatments or combinations of treatments before you find an approach that relieves your symptoms.
They include:
- Distending, or inflating, the bladder
- Bathing the inside of the bladder with a drug solution
- Oral medicines
- Electrical nerve stimulation
- Physical therapy
- Lifestyle changes
- Bladder training
- In rare cases, surgery
Natural remedies for interstitial cystitis
Some people with interstitial cystitis find symptom relief from these strategies:
Dietary changes
Eliminating or reducing foods in your diet that irritate your bladder may help to relieve the discomfort of interstitial cystitis.
Common bladder irritants — known as the “four Cs” — include:
- carbonated beverages,
- caffeine in all forms (including chocolate),
- citrus products and
- food containing high concentrations of vitamin C.
Consider avoiding similar foods, such as tomatoes, pickled foods, alcohol and spices. Artificial sweeteners may aggravate symptoms in some people.
If you think certain foods may irritate your bladder, try eliminating them from your diet. Reintroduce them one at a time and pay attention to which, if any, worsen symptoms.
Bladder training
Bladder training involves timed urination — going to the toilet according to the clock rather than waiting for the need to go. You start by urinating at set intervals, such as every half-hour — whether you have to go or not. Then you gradually wait longer between bathroom visits.
During bladder training, you may learn to control urinary urges by using relaxation techniques, such as breathing slowly and deeply or distracting yourself with another activity.
These self-care measures also may help:
- Wear loose clothing. Avoid belts or clothes that put pressure on your abdomen.
- Reduce stress. Try methods such as visualization and biofeedback.
- If you smoke, stop. Smoking may worsen any painful condition, and smoking contributes to bladder cancer.
- Exercise. Easy stretching exercises may help reduce interstitial cystitis symptoms.
Who is more likely to develop interstitial cystitis?
Interstitial cystitis can occur at any age, including during childhood, but is most common in adult women and men. About twice as many women are affected as men 1. However, more men may struggle with interstitial cystitis than researchers originally thought.
Some research suggests that women are more likely to develop interstitial cystitis if they have a history of being sexually abused or physically traumatized 3.
What other health problems do people with interstitial cystitis have?
Many women with interstitial cystitis are more likely to have other conditions such as irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome 4. Allergies and some autoimmune diseases are also associated with interstitial cystitis 5.
Vulvodynia, which is chronic pain in the vulva that often causes a burning or stinging feeling, or rawness, is commonly associated with interstitial cystitis 3. Vulvodynia has symptoms that overlap with interstitial cystitis.
What are the complications of interstitial cystitis?
The symptoms of interstitial cystitis—such as urgency, frequency, and pain—may lead you to decrease your physical and social activity and negatively affect your quality of life.
Women with pelvic pain or vulvodynia often have pain during sexual intercourse, which can damage your relationships and self-image. Men also can experience pelvic pain that causes uncomfortable or painful sex. Sometimes sex can increase bladder pain attacks, also called symptom flares.
Sexual complications may cause people to avoid further intimacy, possibly leading to depression and guilt. Like many people who deal with chronic pain, people with interstitial cystitis are more likely to struggle with sleep loss due to the frequent need to urinate, and with anxiety and depression 6.
Medical tests such as pelvic exams and Pap tests often are painful for women with interstitial cystitis symptoms, especially those who may have pelvic floor muscle spasm. Don’t avoid these tests. Talk with a health care professional about how to make pelvic exams and Pap tests more comfortable and how often you should have them.
Interstitial cystitis causes
Researchers are working to understand the causes of interstitial cystitis and to find treatments that work. In some people with interstitial cystitis, the bladder is inflamed, ulcerated, scarred or stiff. It’s likely that many factors contribute to interstitial cystitis. For instance, people with interstitial cystitis may also have a defect in the protective lining (epithelium) of the bladder. A leak in the epithelium may allow toxic substances in urine to irritate your bladder wall. Other possible but unproven contributing factors include an autoimmune reaction, heredity, infection or allergy.
There are several theories about the possible cause of interstitial cystitis.
These include:
- damage to the bladder lining, which may mean urine can irritate the bladder and surrounding muscles and nerves
- a problem with the pelvic floor muscles used to control urination
- your immune system mistakenly attacking your bladder
- an allergic reaction
It’s also been suggested that interstitial cystitis may be a symptom of a more widespread problem, as it’s been associated with conditions such as fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome (IBS) and lupus.
Even though the exact cause of interstitial cystitis is unknown, you may find that certain events or factors start, or trigger, your symptom flares. Symptom flares can make your interstitial cystitis feel worse. Some people have reported that their symptom flares happen when they 7:
- are stressed, or have certain emotions, such as anger or sadness
- have sex
- have a menstrual cycle
- have a urinary tract infection
- urinate or hold urine for too long
- skip meals or are dehydrated
- feel changes in the seasons or the weather
- have allergies
- go through sudden or bumpy movements
- take certain medicines or forget to take their medicines
- wear tight pants and undergarments
- use laundry detergents with certain chemicals or are in pool water with certain chemicals
- use certain brands of toilet paper
- do certain physical activities, like pushing or lifting heavy objects
- stand for long periods of time
- have a Pap smear
- take antidepressants, sinus medicines, or pain relievers
Talk with your health care professional about flare management. If you know which factors make your symptoms flare, you may wish to avoid them. However, if factors that affect your health—like having sex, having a Pap smear, or taking certain medicines—make your symptom flares occur, talk with your health care professional right away.
Risk factors for interstitial cystitis
These factors are associated with a higher risk of interstitial cystitis:
- Your sex. Women are diagnosed with interstitial cystitis more often than men. Symptoms in men may mimic interstitial cystitis, but they’re more often associated with an inflammation of the prostate gland (prostatitis).
- Your skin and hair color. Having fair skin and red hair has been associated with a greater risk of interstitial cystitis.
- Your age. Most people with interstitial cystitis are diagnosed during their 30s or older.
- Having a chronic pain disorder. Interstitial cystitis may be associated with other chronic pain disorder, such as irritable bowel syndrome or fibromyalgia.
Interstitial cystitis symptoms
People with interstitial cystitis have repeat discomfort, pressure, tenderness or pain in the bladder, lower abdomen, and pelvic area. Symptoms vary from person to person, may be mild or severe, and can even change in each person as time goes on. If you have interstitial cystitis, your symptoms may vary over time, periodically flaring in response to common triggers, such as menstruation, sitting for a long time, stress, exercise and sexual activity.
The main symptoms of interstitial cystitis are:
- intense pelvic pain (felt below your bellybutton)
- sudden strong urges to pee
- needing to pee more often than normal
- waking up several times during the night to go to the toilet
The pain may be worse when your bladder is full and may be temporarily relieved when you go to the toilet.
You might also find the pain is worse during periods or after having certain foods or drinks.
The symptoms will often come and go in phases. You may have episodes lasting days, weeks or months where your symptoms improve, followed by times when they’re worse.
Symptoms may include a combination of these symptoms:
Urgency
Urgency is the feeling that you need to urinate right now. A strong urge is normal if you haven’t urinated for a few hours or if you have been drinking a lot of liquids. With interstitial cystitis, you may feel pain or burning along with an urgent need to urinate before your bladder has had time to fill.
Frequency
Frequency is urinating more often than you think you should need to, given the amount of liquid you are drinking. Most people urinate between four and seven times a day. Drinking large amounts of liquid can cause more frequent urinating. Taking blood pressure medicines called diuretics, or water pills, can also cause more frequent urinating. Some people with interstitial cystitis feel a strong, painful urge to urinate many times a day.
Pain
As your bladder starts to fill, you may feel pain—rather than just discomfort—that gets worse until you urinate. The pain usually improves for a while once you empty your bladder. People with interstitial cystitis rarely have constant bladder pain. The pain may go away for weeks or months and then return. People with interstitial cystitis sometimes refer to an attack of bladder pain as a symptom flare.
Some people may have pain without urgency or frequency. This pain may come from a spasm in the pelvic floor muscles, the group of muscles that is attached to your pelvic bones and supports your bladder, bowel, and uterus or prostate. Pain from pelvic floor muscle spasm may get worse during sex.
Interstitial cystitis complications
Interstitial cystitis can result in a number of complications, including:
- Reduced bladder capacity. Interstitial cystitis can cause stiffening of the bladder wall, which allows your bladder to hold less urine.
- Lower quality of life. Frequent urination and pain may interfere with social activities, work and other activities of daily life.
- Sexual intimacy problems. Frequent urination and pain may strain your personal relationships, and sexual intimacy may suffer.
- Emotional troubles. The chronic pain and interrupted sleep associated with interstitial cystitis may cause emotional stress and can lead to depression.
Interstitial cystitis diagnosis
Health care professionals will use your medical history, a physical exam, and lab tests to diagnose interstitial cystitis.
A health care professional will ask if you have a history of health problems related to interstitial cystitis. He or she will ask questions about your symptoms and other questions to help find the cause of your bladder problems.
If you are a woman who has interstitial cystitis symptoms, a health care professional may also perform a pelvic exam. During the pelvic exam, the health care professional will check your pelvic floor muscles to see if any of your painful symptoms are related to spasm in your pelvic floor muscles.
For men, a health care professional may perform a digital rectal exam to check for prostate problems and to check your pelvic floor muscles.
Doctors diagnose interstitial cystitis based on:
- pain in or near the bladder, usually with urinary frequency and urgency
- the absence of other diseases and conditions that could cause similar symptoms, such as urinary tract infections (UTIs), bladder cancer, endometriosis in women, or prostatitis—infection or inflammation of the prostate—in men.
Interstitial cystitis tests
A health care professional may use the following tests to look inside your urethra and bladder, and may even take a tissue sample from inside your bladder. The health care professional will use tests to rule out certain diseases and conditions, such as urinary tract infection and bladder cancer. If the test results are normal and all other diseases and conditions are ruled out, your doctor may diagnose interstitial cystitis.
Urinalysis and urine culture
At the doctor’s office, you may be given a cup to take into the bathroom. A health care professional will give you instructions for collecting urine in the cup. White and red blood cells and bacteria in the urine may indicate a UTI (urinary tract infection), which can be treated with an antibiotic.
Cystoscopy
Doctors may use cystoscopy to look inside the urethra and bladder. Doctors use a cystoscope, a tubelike instrument, to look for bladder ulcers, cancer, swelling, redness, and signs of infection.
Biopsy. During cystoscopy under anesthesia, your doctor may remove a sample of tissue (biopsy) from the bladder and the urethra for examination under a microscope. This is to check for bladder cancer and other rare causes of bladder pain.
Potassium sensitivity test
Your doctor places (instills) two solutions — water and potassium chloride — into your bladder, one at a time. You’re asked to rate on a scale of 0 to 5 the pain and urgency you feel after each solution is instilled. If you feel noticeably more pain or urgency with the potassium solution than with the water, your doctor may diagnose interstitial cystitis. People with normal bladders can’t tell the difference between the two solutions.
Interstitial cystitis treatment
Unfortunately, there’s currently no cure for interstitial cystitis and it can be difficult to treat, although a number of treatments can be tried. Researchers have not found one treatment for interstitial cystitis that works for everyone.
No single treatment works for everyone, however, and there’s disagreement about how effective some of them are.
You may need to try several treatments to find one that works for you.
Lifestyle changes will usually be recommended first. Medications and other therapies may be used if these don’t help, and surgery may be necessary as a last resort.
A health care professional will work with you to find a treatment plan that meets your needs. Your plan may include:
- lifestyle changes
- bladder training
- physical therapy
- medicines
- bladder procedures
Some treatments may work better for you than others. You also may need to use a combination of these treatments to relieve your symptoms.
A health care professional may ask you to fill out a form, called a symptom scale, with questions about how you feel. The symptom scale may allow a health care professional to better understand how you are responding to treatment.
You may have to try several different treatments before you find one that works for you. Your symptoms may disappear with treatment, a change in what you eat, or without a clear reason. Even when your symptoms go away, they may return after days, weeks, months, or even years. Researchers do not know why. With time, you and your doctor should be able to find a treatment that gives you some relief and helps you cope with interstitial cystitis.
Lifestyle changes
Change your eating and drinking habits. Some people with interstitial cystitis find that certain foods or drinks trigger their symptoms. Others find no link between symptoms and what they eat. However, be sure to drink enough water to stay hydrated. Talk with your health care professional about how much liquid you should drink to prevent dehydration based on your health, how active you are, and where you live.
Quit smoking. Some people feel that smoking makes their interstitial cystitis symptoms worse. Researchers don’t know exactly how tobacco affects interstitial cystitis. However, smoking is a major cause of bladder cancer . If you smoke, one of the best things you can do for your bladder and overall health is to quit.
If you smoke or use other tobacco products, stop. Ask for help so you don’t have to do it alone.
Reduce stress
Researchers don’t think stress causes interstitial cystitis, yet stress can trigger painful symptom flares in some people with interstitial cystitis.
When you feel stress, your body responds by releasing hormones that increase your blood pressure and raise your heart rate. This is called the stress response.
Relaxation techniques can help your body relax and lower your blood pressure and heart rate. This is called a relaxation response. There are several exercises you can try. See which ones work best for you.
If you feel stressed, try relaxation techniques and other activities that might soothe you, such as:
- looking at nature around you
- listening to soft music
- noticing smells around you
- savoring each bite of a special treat
- breathing gently
Be physically active
If you have interstitial cystitis, you may feel that the last thing you want to do is be physically active. However, many people feel that easy activities like walking or gentle stretching exercises help relieve symptoms.
Get support
Having the emotional support of family, friends, and other people with interstitial cystitis is a very important part of helping you cope. People who learn about the disorder and become involved in their own care do better than people who do not.
Interstitial cystitis diet
Most people with interstitial cystitis report that food sensitivities – they find that certain foods or drinks trigger or worsen their symptoms. Coffee, soda, alcohol, tomatoes, hot and spicy foods, chocolate, caffeinated beverages, citrus juices and drinks, MSG, and high-acid foods can trigger interstitial cystitis symptoms or make them worse. Some people also note that their symptoms get worse after eating or drinking products with artificial sweeteners, or sweeteners that are not found naturally in foods and beverages. However, trigger foods and beverages are different for different people. In addition, many with interstitial cystitis have other health conditions (e.g., constipation or irritable bowel syndrome) requiring them to limit or avoid specific foods related to these health problems.
No research consistently links certain foods or drinks to interstitial cystitis. However, some research strongly suggests a relationship between diet and symptoms. Healthy eating and staying hydrated are important for your overall health, including bladder health.
Most bothersome foods 8:
There are certain items that are more likely to trigger interstitial cystitis flares 9:
- Coffee (caffeinated and decaffeinated),
- Tea (caffeinated and decaffeinated),
- Soda,
- Alcohol,
- Citrus juices,
- Foods and beverages containing artificial sweeteners
- Hot peppers and spicy foods
- Carbonated drinks (cola, non-cola, diet, and caffeine-free)
- Cranberry juice,
- Grapefruit and grapefruit juice,
- Lemons,
- Oranges and orange juice,
- Pineapple and pineapple juice,
- Strawberries
- Chili peppers,
- Pickles,
- Sauerkraut,
- Tomato and tomato products
- Processed sandwich meats (salami, bologna), soy products
- Yogurt
- Chili,
- Horseradish,
- Ketchup,
- Salad dressings,
- Soy sauce,
- Vinegar,
- Worcester sauce
- Chocolate
- Indian food,
- Mexican food,
- Thai food,
- Pizza,
- Spicy foods
- Artificial sweeteners (Equal® (sweetener), NutraSweet®, Saccharin, and Sweet’N Low®)
- Monosodium glutamate (MSG)
Restricting intake of the foods and beverages listed above help some individuals control interstitial cystitis symptoms. However, others may need to limit even more foods and beverages.
Learning which foods trigger your symptoms or make them worse may take some effort. Keep a food diary and note the times you have bladder pain. For example, the diary might show that your symptom flares always happen after you eat tomatoes or oranges. If you find that certain foods make your symptoms worse, your health care professional and dietitian can help you avoid them with an eating plan. Find an expert to advise you on how to use nutrition and ingredient information on a food label. You can use this information to help you avoid eating or drinking things that trigger pain in your bladder.
Stopping certain foods and drinks—and then adding them back to what you normally eat and drink one at a time—may help you figure out which foods or drinks, if any, affect your symptoms. Talk with your health care professional about how much liquid you should drink to prevent dehydration based on your health, how active you are, and where you live. Water is the best liquid for bladder health.
Some doctors recommend taking an antacid with meals. This medicine reduces the amount of acid that gets into the urine.
Bladder training
Bladder training may help your bladder hold more urine. People with bladder pain often get in the habit of using the bathroom as soon as they are aware of any need to go to avoid pain or urgency. They then feel the need to go before the bladder is really full. The body may get used to urinating often. Bladder training helps your bladder hold more urine before your body tells you to urinate.
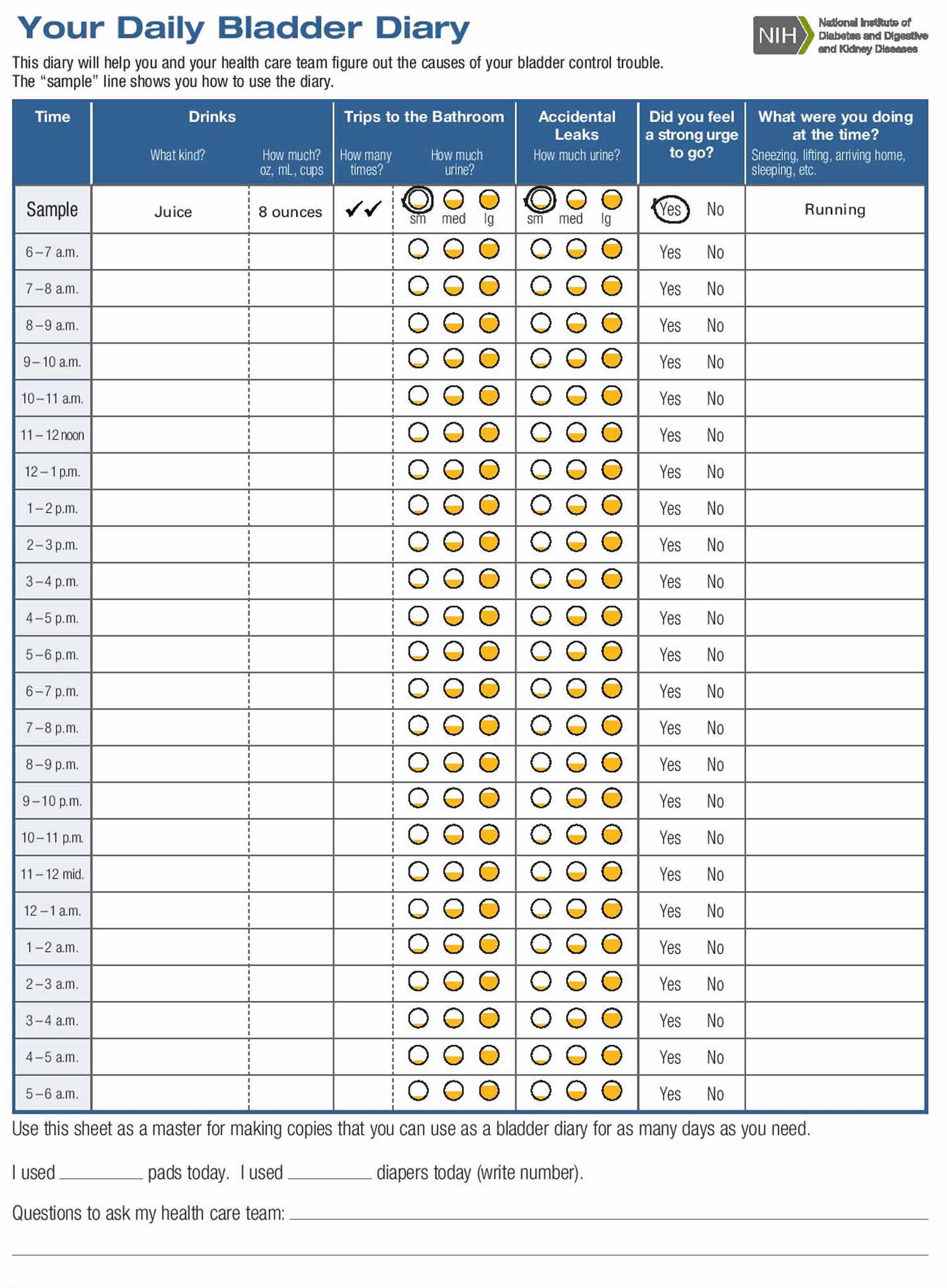
Keep a bladder diary (Figure 1) to track how you are doing. Start by writing down the times when you urinate. For example, you may find that you return to the bathroom every 40 minutes. Try to wait a few more minutes and gradually stretch out the time between urinating. This may be easier if you are well hydrated.
If your bladder becomes painful, use the bathroom. You may find that your first urge to use the bathroom goes away if you ignore it. Find ways to relax or distract yourself when the first urge strikes.
After a week or two, you may be able to stretch the time out to 50 or 60 minutes, and you may find that the urge to urinate does not return as soon
Figure 1. Interstitial cystitis bladder training diary
Bowel training
Your doctor may suggest that you try to train yourself to have a bowel movement at the same time each day to help you become more regular, also called bowel training. Consider keeping track of your bowel movements. Some people report that having regular bowel movements helps their interstitial cystitis symptoms. Talk with your health care professional if you are having bowel control problems, such as
- diarrhea
- constipation
- fecal incontinence
Physical therapy
If you have interstitial cystitis symptoms or pelvic floor muscle spasm, your doctor may suggest that you work with a physical therapist who specializes in pelvic floor problems. The physical therapist will work to stretch tight pelvic floor muscles and help you keep them relaxed.
Relaxation techniques for stress
Chronic stress can be bad for your body and mind. It can put you at risk for health problems such as high blood pressure, stomachaches, headaches, anxiety, and depression. Using relaxation techniques can help you feel calm. These exercises can also help you manage stress and ease the effects of stress on your body.
Deep Breathing
One of the simplest ways to relax is by practicing deep breathing. You can do deep breathing almost anywhere.
- Sit still or lie down and place one hand on your stomach. Put your other hand over your heart.
- Inhale slowly until you feel your stomach rise.
- Hold your breath for a moment.
- Exhale slowly, feeling your stomach fall.
There are also many other types of breathing techniques you can learn. In many cases, you do not need much instruction to do them on your own.
Meditation
Meditation involves focusing your attention to help you feel more relaxed. Practicing meditation may help you react in a calmer way to your emotions and thoughts, including those that cause stress. Meditation has been practiced for thousands of years, and there are several different styles.
Most types of meditation usually include:
- Focused attention. You might focus on your breath, an object, or a set of words.
- Quiet. Most meditation is done in a quiet area to limit distractions.
- Body position. Most people think of meditation done while sitting, but it can also be done lying down, walking, or standing.
- An open attitude. This means that you stay open to thoughts that come into your mind during meditation. Instead of judging these thoughts, you let them go by bringing your attention back to your focus.
- Relaxed breathing. During meditation, you breathe slowly and calmly. This also helps you relax.
Biofeedback
Biofeedback teaches you how to control some of your body’s functions, such as your heart rate or certain muscles.
In a typical session, a biofeedback therapist attaches sensors to different areas of your body. These sensors measure your skin temperature, brain waves, breathing, and muscle activity. You can see these readings on a monitor. Then you practice changing your thoughts, behaviors, or emotions to help control your body’s responses. Over time, you can learn to change them without using the monitor.
Progressive Relaxation
This is another simple technique that you can do almost anywhere. Starting with your toes and feet, focus on tightening your muscles for a few moments and then releasing them. Continue with this process, working your way up your body, focusing on one group of muscles at a time.
Yoga
Yoga is an ancient practice rooted in Indian philosophy. The practice of yoga combines postures or movements with focused breathing and meditation. The postures are meant to increase strength and flexibility. Postures range from simple poses lying on the floor to more complex poses that may require years of practice. You can modify most yoga postures based on your own ability.
There are many different styles of yoga that range from slow to vigorous. If you are thinking about starting yoga, look for a teacher who can help you practice safely. Make sure to tell your teacher about any injuries.
Tai Chi
Tai chi was first practiced in ancient China for self-defense. Today, it is used mainly to improve health. It is a low-impact, gentle type of exercise that is safe for people of all ages.
There are many styles of tai chi, but all involve the same basic principles:
- Slow, relaxed movements. The movements in tai chi are slow, but your body is always moving.
- Careful postures. You hold specific postures as you move your body.
- Concentration. You are encouraged to put aside distracting thoughts while you practice.
- Focused breathing. During tai chi, your breathing should be relaxed and deep.
If you are interested in tai chi for stress relief, you may want to start with a class. For many people, it is the easiest way to learn the proper movements. You can also find books and videos about tai chi.
Coping and support
Interstitial cystitis can worsen your quality of life. Support from family and friends is important, but because the condition is a urinary problem, you may find the topic difficult to discuss.
Find a supportive doctor who is concerned about your quality of life as well as your condition. Seek someone who will work with you to help relieve your urinary frequency, urgency and bladder pain.
You might also benefit from joining a support group. A support group can provide sympathetic listening and useful information. Ask your doctor for information on support groups or see the Interstitial Cystitis Association (https://www.ichelp.org/).
Interstitial cystitis medication
Your doctor may suggest that you take over-the-counter (OTC) pain medicine to help control mild bladder pain, including:
- acetaminophen (Tylenol)
- aspirin (Bayer)
- ibuprofen (Advil, Motrin)
Talk with your doctor if you feel you need a stronger pain medicine. If you have severe pain, you may need your doctor to prescribe narcotic analgesics, or pain-relieving medicines, such as acetaminophen with codeine or longer-acting narcotics.
In some people, however, certain antidepressants , sinus medicines, and pain relievers may trigger symptom flares. Talk with your health care professional if these medicines make your interstitial cystitis worse.
Long-term use of pain medicines can be dangerous. Talk with your doctor about how to safely manage your chronic, or long-term, pain—possibly with the help of a pain specialist, a doctor who diagnoses, treats, and manages pain. You may also want to discuss alternatives to pain medicines or complementary pain medicines.
If lifestyle changes, bladder training, physical therapy, and pain medicines don’t do enough to relieve your interstitial cystitis symptoms, your doctor may prescribe other medicines, including:
- Pentosan polysulfate sodium (Elmiron), which is approved by the Food and Drug Administration specifically for treating interstitial cystitis. How it works is unknown, but it may restore the inner surface of the bladder, which protects the bladder wall from substances in urine that could irritate it. It may take two to four months before you begin to feel pain relief and up to six months to experience a decrease in urinary frequency.
- Tricyclic antidepressants, such as amitriptyline or imipramine (Tofranil), to help relax your bladder and block pain.
- Antihistamines, such as loratadine (Claritin, others), which may reduce urinary urgency and frequency and relieve other symptoms.
- Cyclosporine
- Stronger painkillers available on prescription – such as gabapentin and pregabalin
- Tolterodine, solifenacin or mirabegron – these help relax the bladder muscles
- Cimetidine – a prescription medicine that may help by blocking the effect of a substance called histamine on cells in the bladder
- Botulinum toxin injections – where a substance called botulinum toxin (such as Botox) is injected directly into your bladder to temporarily relieve your symptoms
All medicines, even OTC (over-the-counter) medicines, have side effects. Always consult a doctor before using any medicine or supplement for more than a few days.
Interstitial cystitis natural treatment
A growing body of evidence suggests that some complementary approaches, such as acupuncture, hypnosis, massage, mindfulness meditation, spinal manipulation, tai chi, and yoga, may help to manage some painful conditions.
Guided imagery
This type of therapy employs visualization and direct suggestions using imagery to help you imagine healing, with the hope that the body will follow the mind’s suggestions.
Acupuncture
During an acupuncture session, a practitioner places numerous thin needles in your skin at specific points on your body. According to traditional Chinese medicine, precisely placed acupuncture needles relieve pain and other symptoms by rebalancing the flow of life energy. Western medical practitioners tend to believe that acupuncture boosts the activity of your body’s natural painkillers.
There’s some evidence that cannabis (marijuana)-based medicines (i.e., cannabinoids) may be helpful for chronic nerve (neuropathic) pain and perhaps other types of chronic pain, but it’s unclear whether the potential benefits are greater than the potential harms. Further research is needed that meets U.S. Food and Drug Administration (FDA) requirements for determining the safety and efficacy of cannabinoids for the management of pain.
- It’s unclear whether kratom has an effect on chronic pain because of a lack of studies of this substance in people.
- There’s a lack of high-quality research to definitively evaluate whether Reiki is of value for pain relief.
- Although static magnets are widely marketed for pain control, the evidence does not support their use.
NOTE: These treatments have not been well-studied for interstitial cystitis, so be sure to discuss the use of these therapies with your doctor.
Nerve stimulation
Nerve stimulation techniques include:
Transcutaneous electrical nerve stimulation (TENS)
With TENS, mild electrical pulses relieve pelvic pain and, in some cases, reduce urinary frequency. TENS may increase blood flow to the bladder. This may strengthen the muscles that help control the bladder or trigger the release of substances that block pain.
Electrical wires placed on your lower back or just above your pubic area deliver electrical pulses — the length of time and frequency of therapy depends on what works best for you.
Sacral nerve stimulation
Your sacral nerves are a primary link between the spinal cord and nerves in your bladder. Stimulating these nerves may reduce urinary urgency associated with interstitial cystitis.
With sacral nerve stimulation, a thin wire placed near the sacral nerves sends electrical impulses to your bladder, similar to what a pacemaker does for your heart. If the procedure decreases your symptoms, you may have a permanent device surgically implanted. This procedure doesn’t manage pain from interstitial cystitis, but may help to relieve some symptoms of urinary frequency and urgency.
Bladder instillation
Some people who have interstitial cystitis find relief after a treatment in which a doctor puts a small amount of liquid medicine into the bladder, called bladder instillation or a bladder wash or bath. The doctor guides a tube called a catheter into your bladder and slowly adds a liquid that eases irritation of the bladder wall. The liquid may be a compound called dimethyl sulfoxide (DMSO) or a solution that contains heparin, steroids, and a topical anesthetic, such as short-acting lidocaine or long-acting marcaine.
In bladder instillation, your doctor places the prescription medication dimethyl sulfoxide (Rimso-50) into your bladder through a thin, flexible tube (catheter) inserted through the urethra. The solution sometimes is mixed with other medications, such as a local anesthetic. You will be asked to keep the liquid in your bladder for about 15 minutes and then release it. You can have this treatment once every week or every other week for 1 or 2 months. You may not feel any better until the third or fourth treatment.
- You might receive dimethyl sulfoxide (DMSO) — treatment weekly for six to eight weeks, and then have maintenance treatments as needed — such as every couple of weeks, for up to one year.
A newer approach to bladder instillation uses a solution containing the medications lidocaine, sodium bicarbonate, and either pentosan or heparin.
Bladder stretching
A doctor may use a procedure called bladder stretching, or hydrodistention, to treat your bladder pain, if only for a short time. Bladder stretching occurs when a doctor stretches your bladder by filling it with fluid. You will be given a local or general anesthesia to help you tolerate the bladder stretching.
Some people have temporary relief of their symptoms after this treatment. Researchers are not exactly sure why bladder stretching helps some people. Stretching may temporarily block pain signals sent by nerves in the bladder.
Sometimes your pain symptoms may temporarily get worse 4 to 48 hours after bladder stretching. However, your pain levels should return to your previous level or improve within 2 to 4 weeks.
Surgery
Doctors rarely use surgery to treat interstitial cystitis because removing the bladder doesn’t relieve pain and can lead to other complications.
People with severe pain or those whose bladders can hold only very small volumes of urine are possible candidates for surgery, but usually only after other treatments fail and your pain is still unbearable and affect quality of your life. You and your doctor may consider surgery to either:
- Fulguration. This minimally invasive method involves insertion of instruments through the urethra to burn off ulcers that may be present with interstitial cystitis.
- Cauterisation – where ulcers inside the bladder are sealed using an electrical current or laser. This is another minimally invasive method that involves insertion of instruments through the urethra to cut around any ulcers.
- Bladder augmentation. In this procedure, a surgeon increases the capacity of your bladder by putting a patch of intestine on the bladder. However, this is performed only in very specific and rare instances. The procedure doesn’t eliminate pain and some people need to empty their bladders with a catheter many times a day.
- Reroute the normal flow of urine, called urinary diversion.
- Remove the bladder, called cystectomy. In very rare cases, it may be necessary to remove the bladder completely. If this is done, your surgeon will need to create an alternative way for urine to leave your body. This will usually be through a small hole in your tummy called a stoma, but might involve making a new bladder using part of your small intestine (bladder reconstruction).
Talk with your doctor and family about the possible benefits and side effects of bladder surgery. Surgery does not cure the pain of interstitial cystitis in all cases.
- What is interstitial cystitis? 4 to 12 million may have IC. https://www.ichelp.org/about-ic/what-is-interstitial-cystitis/4-to-12-million-may-have-ic/[↩][↩]
- Kelada E, Jones A. Interstitial cystitis. (2007) Archives of gynecology and obstetrics. 275 (4): 223-9. doi:10.1007/s00404-006-0247-7[↩]
- Mayson BE, Teichman JM. The relationship between sexual abuse and interstitial cystitis/painful bladder syndrome. Current Urology Reports. 2009;10(6):441–447.[↩][↩]
- Nickel JC, Tripp DA, Pontari M, et al. Interstitial cystitis/painful bladder syndrome and associated medical conditions with an emphasis on irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome. The Journal of Urology. 2010;184(4):1358–1363.[↩]
- Ruutu M, Leppilahti M, and Sairanen J. Epidemiology. In: Nordling J, Wyndaele JJ, van de Merwe JP, Bouchelouche P, Cervigni M, Fall M, eds. Bladder Pain Syndrome: A Guide for Clinicians. New York, NY: Springer US; 2013:11–19.[↩]
- Chuang YC, Weng SF, Hsu YW, Huang CL, Wu MP. Increased risks of healthcare-seeking behaviors of anxiety, depression and insomnia among patients with bladder pain syndrome/interstitial cystitis: a nationwide population-based study. International Urology and Nephrology. 2015;47(2):275–281.[↩]
- Sutcliffe S, Bradley CS, Clemens JQ. Urological chronic pelvic pain syndrome flares and their impact: qualitative analysis in the MAPP network. International Urogynecology Journal. 2015;26(7):1047–1060.[↩]
- Foods to Avoid. https://www.ichelp.org/living-with-ic/interstitial-cystitis-and-diet/foods-to-avoid/[↩]
- Urological and Gynecological Chronic Pelvic Pain: Current Therapies [Moldwin R, ed]. Springer Publishing: USA.[↩]